Abstract
Purpose
To determine whether saccadic eye movements are altered in glaucoma patients.
Patients and methods
Sixteen patients with glaucoma and 21 control subjects were prospectively studied. Patients participated in a pro-saccade step task. Saccades were recorded using a noninvasive infrared oculometric device with head-mounted target projection. Medians of saccade reaction time, duration, amplitude, and peak velocity; frequency of express saccades; and percentage of trials with direction error were recorded. t-tests were used to compare the glaucoma and age-matched control groups. A correlation analysis of saccade parameters with visual field loss was also performed.
Results
Median saccade reaction times were significantly prolonged in glaucoma patients compared with controls (220.9 ± 49.02 ms vs 192.1 ± 31.24 ms; t-test: P = 0.036). Median duration, median amplitude, and median peak velocity of saccades did not show significant differences between glaucoma and control groups (P > 0.05). Frequency of express saccades was significantly decreased in glaucoma patients compared with controls (1.75 ± 2.32 vs 7.0 ± 6.99; t-test: P = 0.007). Saccade parameters in glaucoma patients showed no significant correlation with visual field loss.
Conclusion
Saccadic eye movements are significantly delayed in patients with early, moderate, or advanced glaucoma. Determination of median saccade reaction time may offer a novel functional test to quantify visual function in glaucoma patients. Further studies are needed to determine pathological processes implicated in delayed initiation of saccades, and to assess whether alteration of saccades affects daily activities in glaucoma patients.
Keywords: visual field, latency, visual dysfunction, brain, superior colliculus, quality of life
Introduction
Glaucomatous optic neuropathy is a leading cause of irreversible blindness worldwide.1 Loss of sight in glaucoma is caused by death in retinal ganglion cells,2 and involves visual functions such as form, motion, and color.3–5 Functional tests for the diagnosis of glaucoma and for the assessment of progression are processed by retinal ganglion cells that project to the lateral geniculate nucleus,6 a relay station to the primary visual cortex. In glaucoma, neurodegeneration in this major retino-geniculo-cortical pathway has been demonstrated.7–15
The effect of glaucoma on other visual functions such as eye movements that are controlled by alternative visual pathways is not well studied. Saccades are rapid eye movements that redirect the fovea to visual targets, such as a suddenly appearing visual stimulus.16 They are generated by a complex network of brain structures, including the retinotectal pathway.17 Saccades can be measured precisely with reliable parameters such as saccade reaction time, saccade duration,18 amplitude,19,20 and peak velocity.21,22 Studies of these saccade parameters are used to assess the integrity of the saccade-generating neural network in various brain diseases.23–28 In addition, saccade parameters such as increased saccade reaction time are altered in various optic nerve pathologies affecting the nerve fibers that convey visual signals to the saccade-generating network.29,30 We hypothesize that eye movements may provide another functional marker of injury in glaucoma. The aim of this study was to determine whether saccadic eye movements are altered in glaucoma patients.
Material and methods
After study approval by St Michael’s Hospital Research Ethics Board, informed consent was obtained from glaucoma and age-matched participants between the ages of 40 and 80 years. Patients with primary open-angle glaucoma and a history of uncontrolled intraocular pressure (n = 16) were prospectively recruited from the practice of a glaucoma specialist (NG). Glaucoma was defined by characteristic optic nerve head findings with corresponding visual field changes assessed by white on white automated perimetry. Vision loss was estimated by the sum of mean deviations of right and left visual fields. Exclusion criteria included other nonglaucomatous eye disease, monocularity, incisional eye surgery within a month, central acuity of less than 20/50 OU, history of neurological disease, and use of psychotropic medications known to affect saccade velocity.31 Control subjects (n = 21) were recruited from visitors or personnel working at the institution and from relatives of patients. All control subjects had normal eye examinations. Glaucoma and age-matched control subjects underwent full eye examinations. Age and visual acuity were not different between glaucoma and age-matched controls (Tables 1–3). Mean ages of glaucoma patients and controls were 63.2 ± 8.70 years and 60.9 ± 8.13 years, respectively (P = 0.42). Glaucoma patients showed minimal to advanced visual field loss (Table 3).
Table 1.
Demographicsa
| Control | Glaucoma | Significance | |
|---|---|---|---|
| Number | 21 | 16 | |
| Percentage female | 57% | 44% | |
| Age (years) | 60.9 (8.05) | 63.2 (8.70) | P = 0.42 |
| Acuity OD | 0.737 (0.213) | 0.700 (0.212) | P = 0.61 |
| Acuity OS | 0.693 (0.227) | 0.616 (0.254) | P = 0.34 |
Note:
Visual acuity measured as the decimal equivalent of the Snellen number. Values in parentheses are standard deviations. Significance P-values represent the outcome of an independent-samples t-test.
Abbreviations: OD, right eye; OS, left eye.
Table 2.
Participant summary data for controls
| Age (years) | Gender |
|---|---|
| Control | |
| 46 | Male |
| 50 | Female |
| 53 | Female |
| 56 | Male |
| 56 | Male |
| 56 | Female |
| 57 | Male |
| 57 | Male |
| 57 | Female |
| 58 | Female |
| 58 | Female |
| 61 | Female |
| 61 | Female |
| 62 | Female |
| 63 | Female |
| 65 | Male |
| 68 | Female |
| 70 | Male |
| 71 | Female |
| 74 | Male |
| 79 | Male |
Table 3.
Participant summary data for glaucoma
| Age (years) | Gender | Total mean deviation (dB) |
|---|---|---|
| Glaucoma | ||
| 72 | Male | 0.07 |
| 63 | Male | −1.01 |
| 77 | Male | −7.68 |
| 62 | Female | −9.01 |
| 57 | Female | −10.54 |
| 68 | Male | −11.19 |
| 61 | Female | −11.68 |
| 70 | Female | −11.89 |
| 71 | Female | −14.1 |
| 56 | Male | −18.62 |
| 59 | Male | −20.29 |
| 54 | Male | −21.64 |
| 60 | Female | −23.16 |
| 42 | Male | −26.56 |
| 69 | Female | −27.21 |
| 70 | Male | −36.82 |
Eye movement recordings
All glaucoma and control participants were tested under similar conditions under constant observation. Participants were seated 1.5 m away from an evenly lit wall with luminance measured at 500 cd/m2 (Minolta Luminance Meter LS-100, Osaka, Japan). A noninvasive infrared oculometric device with a head-mounted system of low-power laser-target projections (saccadometer) (Ober Consulting, Poznan, Poland) projected three high-contrast (13 cd/m2) discs subtending 0.1° in diameter, at 0°, 10° left, and 10° right, along the frontal plane at eye level. Viewing and recording were performed binocularly. Prior to proceeding with testing, all participants were required to report clearly seeing the red stimuli located at 0°, 10° left, and 10° right. Calibrations were made for both left and right stimuli under binocular viewing.
After a random foreperiod (500–1000 ms), the central fixation point was extinguished, and a randomly chosen 10° left or 10° right stimulus was projected. There were no gaps or overlaps, and the stimuli remained projected until either the participant performed a saccade or 2000 msec had elapsed. Each session consisted of 200 trials, measured over the course of 15 minutes. Saccade reaction time, duration, amplitude, peak velocity, and direction were recorded with a sampling rate of 1 kHz and a linear range within 7% for up to ±30° (Ober Consulting).23 Blinks and head movements were automatically excluded by the Latency Meter Version 4.9 software (Ober Consulting), and analysis was performed on saccades made toward the stimulus. Trials with saccade reaction times between 50 ms and 600 ms were analyzed, removing anticipatory saccades (<50 ms) and latencies due to inattention (>600 ms).22,24–26 Trials with saccade reaction times between 50 ms and 100 ms were defined as express saccades,19,32–36 and their frequency was counted. Trials with direction error were analyzed separately.
Statistical analysis
Statistical analysis was performed using SPSS Version 14.0 (SPSS Inc, Chicago, IL) and SAS 9.2 (SAS Institute Inc, Cary, NC) with α level set at 0.05. Medians of saccade reaction time, duration, amplitude, and peak velocity, and frequency of express saccades were calculated. These variables in the glaucoma group were compared with age-matched controls using independent-samples t-tests. A P-value less than 0.05 was considered statistically significant. Bivariate correlations of the visual field loss (as measured by the sum of mean deviations of right and left visual fields) and various saccade variables were calculated using the Pearson correlation coefficient.
Results
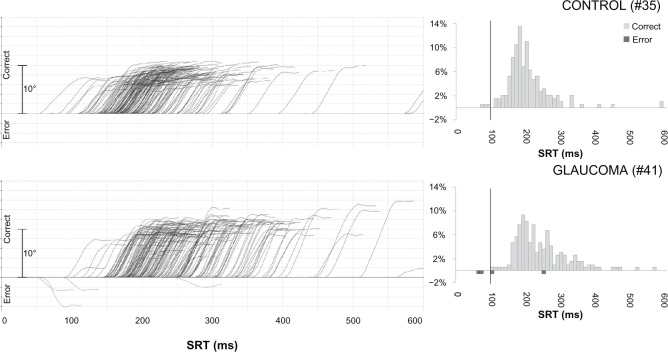
Figure 1 shows a series of saccade recordings and histograms of saccade reaction times of representative glaucoma and control subjects. Saccade reaction times were prolonged in glaucoma patients compared with controls (Figure 2). Median saccade reaction time was significantly increased in glaucoma patients compared with controls (220.9 ± 49.02 ms vs 192.1 ± 31.24 ms; P = 0.036) (Figure 3). Median duration, median amplitude, and median peak velocity were not statistically different between groups (54.7 ± 5.16 ms vs 52.8 ± 4.45 ms, P = 0.25; 10.4 ± 1.88° vs 9.5 ± 1.69°, P = 0.12; 349.4 ± 72.01°/s vs 345.0 ± 83.41°/s, P = 0.87) (Table 4).
Figure 1.
Traces of individual saccades for two subjects (left) and histograms of corresponding reaction times (right).a
Notes: aThe left column shows eye position (in degrees) as a function of time (in ms) after the onset of the stimulus. Traces above the x-axis show saccades made in the correct direction for the stimulus, whereas those below show direction errors. Each curve represents a single saccade. The right column shows histograms of reaction times for the two subjects (percentage of total responses on the y-axis, saccade reaction times [SRT] in ms on the x-axis). Light bars above the x-axis represent saccades made in the correct direction, whereas dark bars below the x-axis represent direction error. Data points to the left of the bolded vertical line represent express saccades (saccade reaction times < 100 ms).
Figure 2.
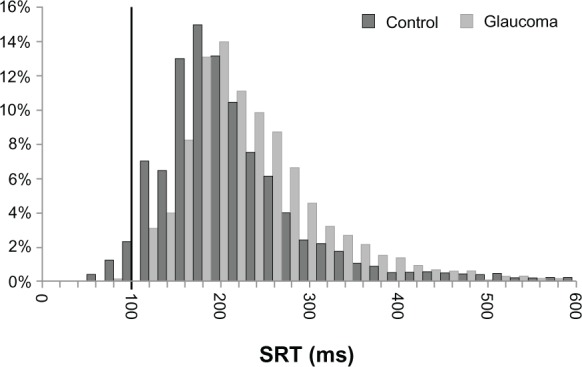
Saccade reaction times (SRT).a
Notes: aHistogram shows the distribution of SRT for each group (percentage of total responses on the y-axis, and in ms on the x-axis). Dark bars represent data from control subjects; light bars represent data from glaucoma patients. Data points to the left of the bolded vertical line at 100 ms represent express saccades.
Figure 3.
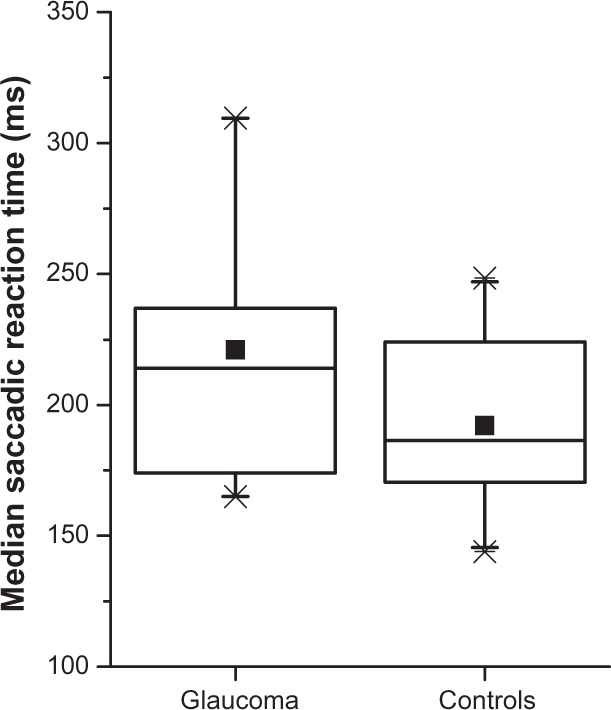
Box plots of median saccade reaction times per group.a
Notes: aThe horizontal bars across the boxes are the medians of the groups; small squares indicate group means. The boxes themselves delineate the 25th percentile to the 75th percentile of each group, the “whiskers” indicate the 5th and 95th percentiles, and the “X”s mark minima and maxima.
Table 4.
Saccade parameters in glaucoma and controls
| Saccade parameter | Control | Glaucoma | P-value | t-value |
|---|---|---|---|---|
| Median reaction time (ms) | 192.1 (31.24) | 220.9 (49.02) | P = 0.036 | t = 2.18 |
| Median duration (ms) | 52.8 (4.45) | 54.7 (5.16) | P = 0.25 | t = 1.17 |
| Median amplitude (°) | 9.5 (1.69) | 10.4 (1.88) | P = 0.12 | t = 1.57 |
| Median peak velocity (°/s) | 345.0 (83.41) | 349.4 (72.01) | P = 0.87 | t = 0.17 |
| Express saccades (frequency) | 7.0 (6.99) | 1.75 (2.32) | P = 0.007 | t = 2.88 |
| Trials with direction error (%) | 3.2 (5.89) | 1.72 (1.82) | P = 0.34 | t = 0.97 |
There was a significant reduction in the number of express saccades in the glaucoma patients compared with controls (1.75 ± 2.32 vs 7.0 ± 6.99; P = 0.007). The percentage of direction errors between the glaucoma and control groups was not statistically different (1.72 ± 1.82% vs 3.2 ± 5.89%; P = 0.34) (Table 4), and neither were direction errors significantly correlated with the degree of visual field loss in the glaucoma group (P = 0.54).
Median saccade reaction time, median duration, median amplitude, and median peak velocity were not statistically correlated with the degree of visual field loss (P = 0.64, P = 0.25, P = 0.14, and P = 0.38, respectively).
Discussion
This is the first study to demonstrate that saccade latencies are affected in glaucoma. Glaucoma patients were slower to initiate the saccade compared with age-matched controls. Normal saccade reaction times in control subjects in our study are consistent with previous work.25,27,34
The fact that other saccade parameters such as duration, amplitude, and peak velocity are not altered suggests that patients were able to detect the targets located at 10° to the right and to the left of the fixation point, and that once the saccades were initiated, the accuracy and the motor characteristics of the saccades were not significantly affected. Therefore, the glaucomatous pathological process seems to alter mainly the initiation of saccades that involve visual input as well as a complex saccade-generation network.
The neural network underlying saccade generation involves a multitude of structures, including superior colliculus, areas of the frontal lobe, and the basal ganglia.17 Visual input to the saccade-generating network is provided by a specific subpopulation of retinal ganglion cells that project directly to superior colliculus,6,37 and indirect visual input via the primary visual cortex also projects to the superior colliculus.38 In view of the fact that delayed saccades have been described in various optic nerve diseases,29,30 the delayed saccades observed in patients with glaucomatous optic neuropathy are likely due to damage to retinal ganglion cells that provide direct retinal input to superior colliculus6 and/or that drive the visual information through the visual cortex.38,39 It is interesting to note that delayed saccades are found in patients with mild visual field loss, as well as in advanced cases. It is not yet known whether the increased latency of nerve conduction in the retino-geniculate pathway40,41 and/or the decreased amplitude of retinal ganglion cell response42 reported in some glaucoma patients contribute to delayed saccades in glaucoma patients. Further studies are needed to determine whether the retinal ganglion cells conveying visual information to the saccade-generation network are affected in glaucoma.
The superior colliculus is critical to saccade generation, with a role in both visual and motor components.17 In addition to its sensory role as a visual information-recipient structure arranged in a retinotopic fashion, it plays an important role in influencing saccade generation through its direct projection to the brainstem reticular formation,43 which, in turn, projects to oculomotor neurons.44 Ablation of superior colliculus in nonhuman primates leads to increased saccade reaction times and eliminates a subpopulation of express saccades.45 Interestingly, in addition to prolonged saccade reaction time, we noted a reduced frequency of express saccades in glaucoma. Investigations in nonhuman primate experimental glaucoma may help to determine whether the retinal ganglion cells and superior colliculus involved in the generation of saccades are, indeed, affected in glaucoma.
Few studies have looked at eye movements in glaucoma. Other types of gaze-shifting eye movements such as smooth pursuit have not yet been studied. Among the gaze-stabilizing eye movements, optokinetic nystagmus has been investigated and shown to exhibit characteristic differences in glaucoma patients as compared with controls, eg, in pursuit eye movement and optokinetic nystagmus elicitation tasks.46,47 Other studies have examined the eye movements of glaucoma patients as either pedestrians or drivers. Gaze behavior has been shown to differ in a group of glaucoma patients compared with controls when crossing a street,48 whereas eye-tracking data have shown changes in the pattern of eye movements performed by glaucoma patients compared with controls while viewing a video of a driving scene.49 Further studies are needed to determine whether delayed saccades in glaucoma may contribute to these altered eye movements.
Certain pharmacological agents are known to alter sac-cade parameters. Patients on psychotropic medications, including benzodiazepines, antipsychotics, and anticonvulsants, which are known to decrease saccade velocity,31 were excluded in this study. This study shows that saccade reaction time is increased in glaucoma patients, and though topical treatment effects cannot be ruled out, no statistically significant difference in saccade reaction times (P = 0.42) was noted between glaucoma patients on topical β-blockers (n = 8) compared with those who were not (n = 8).
Glaucoma patients are known to be at increased risk for falls and motor vehicle collisions.50 These tasks are dependent on a person’s ability to attend to and respond to visual stimuli. Further studies are needed to determine whether delayed saccades observed in glaucoma patients have functional implications and contribute to an increased risk for falls and motor vehicle collisions.
Overall, this study provides the first insight into saccade alterations in glaucoma. Further studies are needed to investigate the possible locations of neural damage in pathways and centers involved in saccades, to determine whether saccade changes correlate with disease development and/or progression, and to evaluate their possible functional impact in patients with glaucoma.
Acknowledgments
The authors would like to thank Joyce Lo and Lalaine Songalia for their excellent research assistance, and Barbara Thomson MSc for statistical analysis. This study was supported by the Glaucoma Research Society of Canada (NG, YY), Dorothy Pitts Fund (NG), and the University of Toronto CREMS program.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Resnikoff S, Pascolini D, Etya’ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82(11):844–851. [PMC free article] [PubMed] [Google Scholar]
- 2.Quigley HA. Neuronal death in glaucoma. Prog Retin Eye Res. 1999;18(1):39–57. doi: 10.1016/s1350-9462(98)00014-7. [DOI] [PubMed] [Google Scholar]
- 3.Sample PA, Johnson CA. Functional assessment of glaucoma. J Glaucoma. 2001;10(5 Suppl 1):S49–S52. doi: 10.1097/00061198-200110001-00018. [DOI] [PubMed] [Google Scholar]
- 4.Sample PA, Medeiros FA, Racette L, et al. Identifying glaucomatous vision loss with visual-function-specific perimetry in the diagnostic innovations in glaucoma study. Invest Ophthalmol Vis Sci. 2006;47(8):3381–3889. doi: 10.1167/iovs.05-1546. [DOI] [PubMed] [Google Scholar]
- 5.Jampel HD, Singh K, Lin SC, et al. Assessment of visual function in glaucoma: a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118(5):986–1002. doi: 10.1016/j.ophtha.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 6.Perry VH, Cowey A. Retinal ganglion cells that project to the superior colliculus and pretectum in the macaque monkey. Neuroscience. 1984;12(4):1125–1137. doi: 10.1016/0306-4522(84)90007-1. [DOI] [PubMed] [Google Scholar]
- 7.Yucel YH, Zhang Q, Weinreb RN, Kaufman PL, Gupta N. Effects of retinal ganglion cell loss on magno-, parvo-, koniocellular pathways in the lateral geniculate nucleus and visual cortex in glaucoma. Prog Retin Eye Res. 2003;22(4):465–481. doi: 10.1016/s1350-9462(03)00026-0. [DOI] [PubMed] [Google Scholar]
- 8.Gupta N, Ang LC, Noel de Tilly L, Bidaisee L, Yucel YH. Human glaucoma and neural degeneration in intracranial optic nerve, lateral geniculate nucleus, and visual cortex. Br J Ophthalmol. 2006;90(6):674–678. doi: 10.1136/bjo.2005.086769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duncan RO, Sample PA, Weinreb RN, Bowd C, Zangwill LM. Retinotopic organization of primary visual cortex in glaucoma: comparing fMRI measurements of cortical function with visual field loss. Prog Retin Eye Res. 2007;26(1):38–56. doi: 10.1016/j.preteyeres.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garaci FG, Bolacchi F, Cerulli A, et al. Optic nerve and optic radiation neurodegeneration in patients with glaucoma: in vivo analysis with 3-T diffusion-tensor MR imaging. Radiology. 2009;252(2):496–501. doi: 10.1148/radiol.2522081240. [DOI] [PubMed] [Google Scholar]
- 11.Boucard CC, Hernowo AT, Maguire RP, et al. Changes in cortical grey matter density associated with long-standing retinal visual field defects. Brain. 2009;132(Pt 7):1898–1906. doi: 10.1093/brain/awp119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta N, Greenberg G, de Tilly LN, Gray B, Polemidiotis M, Yucel YH. Atrophy of the lateral geniculate nucleus in human glaucoma detected by magnetic resonance imaging. Br J Ophthalmol. 2009;93(1):56–60. doi: 10.1136/bjo.2008.138172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta N, Yucel YH. Glaucoma as a neurodegenerative disease. Curr Opin Ophthalmol. 2007;18(2):110–114. doi: 10.1097/ICU.0b013e3280895aea. [DOI] [PubMed] [Google Scholar]
- 14.Yucel Y, Gupta N. Glaucoma of the brain: a disease model for the study of transsynaptic neural degeneration. Prog Brain Res. 2008;173:465–478. doi: 10.1016/S0079-6123(08)01132-1. [DOI] [PubMed] [Google Scholar]
- 15.Yucel YH, Zhang Q, Gupta N, Kaufman PL, Weinreb RN. Loss of neurons in magnocellular and parvocellular layers of the lateral geniculate nucleus in glaucoma. Arch Ophthalmol. 2000;118(3):378–384. doi: 10.1001/archopht.118.3.378. [DOI] [PubMed] [Google Scholar]
- 16.Saslow MG. Effects of components of displacement-step stimuli upon latency for saccadic eye movement. J Opt Soc Am. 1967;57(8):1024–1029. doi: 10.1364/josa.57.001024. [DOI] [PubMed] [Google Scholar]
- 17.Munoz DP, Schall JD. Concurrent, distributed control of saccade initiation in the frontal eye field and superior colliculus. In: Hall WC, Moschovakis A, editors. The superior colliculus: new approaches for studying sensorimotor integration. Boca Raton, FL: CRC Press; 2004. pp. 34–52. [Google Scholar]
- 18.Warabi T, Kase M, Kato T. Effect of aging on the accuracy of visually guided saccadic eye movement. Ann Neurol. 1984;16(4):449–454. doi: 10.1002/ana.410160405. [DOI] [PubMed] [Google Scholar]
- 19.Fischer B, Weber H, Biscaldi M, Aiple F, Otto P, Stuhr V. Separate populations of visually guided saccades in humans: reaction times and amplitudes. Exp Brain Res. 1993;92(3):528–541. doi: 10.1007/BF00229043. [DOI] [PubMed] [Google Scholar]
- 20.Botzel K, Rottach K, Buttner U. Normal and pathological saccadic dysmetria. Brain. 1993;116(Pt 2):337–353. doi: 10.1093/brain/116.2.337. [DOI] [PubMed] [Google Scholar]
- 21.Pitt MC, Rawles JM. The value of measuring saccadic eye movement in the investigation of non-compressive myelopathy. J Neurol Neurosurg Psychiatry. 1989;52(10):1157–1161. doi: 10.1136/jnnp.52.10.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharpe JA, Zackon DH. Senescent saccades. Effects of aging on their accuracy, latency and velocity. Acta Otolaryngol. 1987;104(5–6):422–428. doi: 10.3109/00016488709128270. [DOI] [PubMed] [Google Scholar]
- 23.Ober JK, Przedpelska-Ober E, Gryncewicz W, et al. Handheld system for ambulatory measurement of saccadic durations of neurological patients. In: Gajda J, editor. Modelling and measurement in medicine. Warsaw, Poland: Komitet Biocybernityki i Inzyneierii Biomedycznej PAN; 2003. pp. 187–198. [Google Scholar]
- 24.Pierrot-Deseilligny C, Rivaud S, Gaymard B, Agid Y. Cortical control of reflexive visually-guided saccades. Brain. 1991;114(Pt 3):1473–1485. doi: 10.1093/brain/114.3.1473. [DOI] [PubMed] [Google Scholar]
- 25.Michell AW, Xu Z, Fritz D, et al. Saccadic latency distributions in Parkinson’s disease and the effects of L-dopa. Exp Brain Res. 2006;174(1):7–18. doi: 10.1007/s00221-006-0412-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rivaud S, Muri RM, Gaymard B, Vermersch AI, Pierrot-Deseilligny C. Eye movement disorders after frontal eye field lesions in humans. Exp Brain Res. 1994;102(1):110–120. doi: 10.1007/BF00232443. [DOI] [PubMed] [Google Scholar]
- 27.Antoniades CA, Altham PM, Mason SL, Barker RA, Carpenter R. Saccadometry: a new tool for evaluating presymptomatic Huntington patients. Neuroreport. 2007;18(11):1133–1136. doi: 10.1097/WNR.0b013e32821c560d. [DOI] [PubMed] [Google Scholar]
- 28.Pearson BC, Armitage KR, Horner CW, Carpenter RH. Saccadometry: the possible application of latency distribution measurement for monitoring concussion. Br J Sports Med. 2007;41(9):610–612. doi: 10.1136/bjsm.2007.036731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brigell MG, Goodwin JA, Lorance R. Saccadic latency as a measure of afferent visual conduction. Invest Ophthalmol Vis Sci. 1988;29(8):1331–1338. [PubMed] [Google Scholar]
- 30.Reulen JP. Latency of visually evoked saccadic eye movements. II. Temporal properties of the facilitation mechanism. Biol Cybern. 1984;50(4):263–271. doi: 10.1007/BF00337076. [DOI] [PubMed] [Google Scholar]
- 31.Reilly JL, Lencer R, Bishop JR, Keedy S, Sweeney JA. Pharmacological treatment effects on eye movement control. Brain Cogn. 2008;68(3):415–435. doi: 10.1016/j.bandc.2008.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Munoz DP, Broughton JR, Goldring JE, Armstrong IT. Age-related performance of human subjects on saccadic eye movement tasks. Exp Brain Res. 1998;121(4):391–400. doi: 10.1007/s002210050473. [DOI] [PubMed] [Google Scholar]
- 33.Shafiq-Antonacci R, Maruff P, Whyte S, Tyler P, Dudgeon P, Currie J. The effects of age and mood on saccadic function in older individuals. J Gerontol B Psychol Sci Soc Sci. 1999;54(6):P361–P368. doi: 10.1093/geronb/54b.6.p361. [DOI] [PubMed] [Google Scholar]
- 34.Irving EL, Steinbach MJ, Lillakas L, Babu RJ, Hutchings N. Horizontal saccade dynamics across the human life span. Invest Ophthalmol Vis Sci. 2006;47(6):2478–2484. doi: 10.1167/iovs.05-1311. [DOI] [PubMed] [Google Scholar]
- 35.Sparks D, Rohrer WH, Zhang Y. The role of the superior colliculus in saccade initiation: a study of express saccades and the gap effect. Vision Res. 2000;40(20):2763–2777. doi: 10.1016/s0042-6989(00)00133-4. [DOI] [PubMed] [Google Scholar]
- 36.Fischer B, Ramsperger E. Human express saccades: extremely short reaction times of goal directed eye movements. Exp Brain Res. 1984;57(1):191–195. doi: 10.1007/BF00231145. [DOI] [PubMed] [Google Scholar]
- 37.Mays LE, Sparks DL. Dissociation of visual and saccade-related responses in superior colliculus neurons. J Neurophysiol. 1980;43(1):207–232. doi: 10.1152/jn.1980.43.1.207. [DOI] [PubMed] [Google Scholar]
- 38.Schiller PH, Stryker M, Cynader M, Berman N. Response characteristics of single cells in the monkey superior colliculus following ablation or cooling of visual cortex. J Neurophysiol. 1974;37(1):181–194. doi: 10.1152/jn.1974.37.1.181. [DOI] [PubMed] [Google Scholar]
- 39.Abel PL, O’Brien BJ, Lia B, Olavarria JF. Distribution of neurons projecting to the superior colliculus correlates with thick cytochrome oxidase stripes in macaque visual area V2. J Comp Neurol. 1997;377(3):313–323. doi: 10.1002/(sici)1096-9861(19970120)377:3<313::aid-cne1>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 40.Parisi V. Impaired visual function in glaucoma. Clin Neurophysiol. 2001;112(2):351–358. doi: 10.1016/s1388-2457(00)00525-3. [DOI] [PubMed] [Google Scholar]
- 41.Rodarte C, Hood DC, Yang EB, et al. The effects of glaucoma on the latency of the multifocal visual evoked potential. Br J Ophthalmol. 2006;90(9):1132–1136. doi: 10.1136/bjo.2006.095158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sehi M, Grewal DS, Goodkin ML, Greenfield DS. Reversal of retinal ganglion cell dysfunction after surgical reduction of intraocular pressure. Ophthalmology. 2010;117(12):2329–2336. doi: 10.1016/j.ophtha.2010.08.049. [DOI] [PubMed] [Google Scholar]
- 43.Raybourn MS, Keller EL. Colliculoreticular organization in primate oculomotor system. J Neurophysiol. 1977;40(4):861–878. doi: 10.1152/jn.1977.40.4.861. [DOI] [PubMed] [Google Scholar]
- 44.Buttner-Ennever JA, Henn V. An autoradiographic study of the pathways from the pontine reticular formation involved in horizontal eye movements. Brain Res. 1976;108(1):155–164. doi: 10.1016/0006-8993(76)90171-2. [DOI] [PubMed] [Google Scholar]
- 45.Schiller PH, Sandell JH, Maunsell JH. The effect of frontal eye field and superior colliculus lesions on saccadic latencies in the rhesus monkey. J Neurophysiol. 1987;57(4):1033–1049. doi: 10.1152/jn.1987.57.4.1033. [DOI] [PubMed] [Google Scholar]
- 46.Severt WL, Maddess T, Ibbotson MR. Employing following eye movements to discriminate normal from glaucoma subjects. Clin Experiment Ophthalmol. 2000;28(3):172–174. doi: 10.1046/j.1442-9071.2000.00295.x. [DOI] [PubMed] [Google Scholar]
- 47.Tong J, Wang J, Sun F. Dual-directional optokinetic nystagmus elicited by the intermittent display of gratings in primary open-angle glaucoma and normal eyes. Curr Eye Res. 2002;25(6):355–362. doi: 10.1076/ceyr.25.6.355.14236. [DOI] [PubMed] [Google Scholar]
- 48.Geruschat DR, Hassan SE, Turano KA, Quigley HA, Congdon NG. Gaze behavior of the visually impaired during street crossing. Optom Vis Sci. 2006;83(8):550–558. doi: 10.1097/01.opx.0000232219.23362.a6. [DOI] [PubMed] [Google Scholar]
- 49.Crabb DP, Smith ND, Rauscher FG, et al. Exploring eye movements in patients with glaucoma when viewing a driving scene. PLoS One. 2011;5(3):e9710. doi: 10.1371/journal.pone.0009710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haymes SA, Leblanc RP, Nicolela MT, Chiasson LA, Chauhan BC. Risk of falls and motor vehicle collisions in glaucoma. Invest Ophthalmol Vis Sci. 2007;48(3):1149–1155. doi: 10.1167/iovs.06-0886. [DOI] [PubMed] [Google Scholar]