Abstract
A case of ocular (bulbar) rhinosporidiosis is described; its unusual features included a) the rapid development of a primary, rhinosporidial lesion with a scleral staphyloma, close to but noncontiguous with the rhinosporidial lesion, 3 weeks after exposure to a lacustrine reservoir, the putative source of the pathogen Rhinosporidium seeberi; b) ocular coherence tomography which revealed no retinal abnormalities unlike in previous cases reported from Sri Lanka; c) atypical histopathology that resulted in an initial mis-diagnosis of chronic inflammation with mucus cysts and a missed diagnosis of rhinosporidiosis; the rhinosporidial etiology was confirmed on replicate histopathological sections of the ocular mass. The pitfalls of histopathological diagnosis of rhinosporidiosis are pointed out.
Keywords: rhinosporidiosis, staphyloma, missed diagnosis
Introduction
Ocular rhinosporidiosis is known to occur in approximately 15% of all cases of rhinosporidiosis in humans while bulbar (scleral) rhinosporidiosis occurred in approximately 68% of 27 ocular cases in our series of 143 cases of rhinosporidiosis. A rare complication of bulbar rhinosporidiosis is scleral-thinning and a bulbous herniation of intraocular contents leading to staphyloma formation, which could lead to rupture and loss of intraocular contents, infection, and loss of the eye. A previous report, the first from Sri Lanka,1 described 4 cases of bulbar rhinosporidiosis with staphyloma formation; the present report describes the fifth case which had several unusual features.
Results
Case report
A male aged 20 years presented with a red-colored, granular mass on the superotemporal bulbar conjunctiva of the right eye (Figure 1), of 3 weeks’ duration. He had no tearing, photophobia, pain, or itching. He bathed regularly in a domestic well but had a 1-year history of bathing in a lacustrine reservoir in the Sri Lanka dry-zone which is a known rhinosporidiosis-endemic region. He gave no history of trauma to the affected eye; his vision was 6/6 in both eyes.
Figure 1.
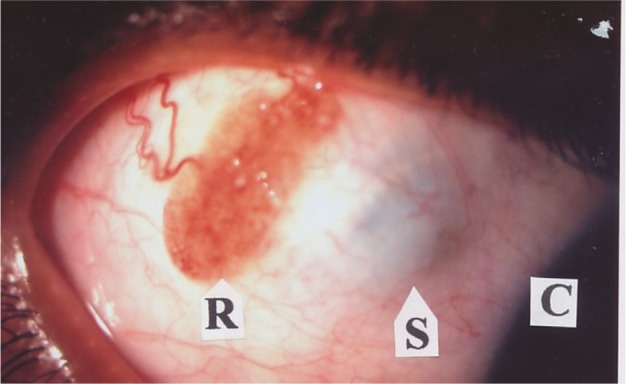
The bulbar rhinosporidial growth (R), showing vascularity and granularity with whitish spots on the surface, and the gray-bluish spherical staphyloma (S) with ill-defined margins; cornea (C).
A red-colored oval granular growth, 1 cm × 0.5 cm, was present on the right upper quandrant of the sclera of the right eye with a gray-bluish, flat, noncystic staphyloma, with ill-defined margins, a few millimeters medial to the rhinosporidial growth (Figure 1).
One week later, funduscopy showed mild peri-macular edema on the affected and normal eye but ocular (optical) coherence tomography (OCT) revealed no abnormalities (Figure 2). He had no concurrent nasal rhinosporidiosis, epistaxis, or obstruction to nasal breathing; the nasal passages were abnormal. Blood cell counts and other clinicopathological test results were normal. A clinical diagnosis of primary, bulbar rhinosporidiosis was made and the granular, red-colored growth was excised; the tissue was fixed in 10% formol-saline and paraffin sections at 5 µm were stained with hematoxylin and eosin (H&E).
Figure 2.
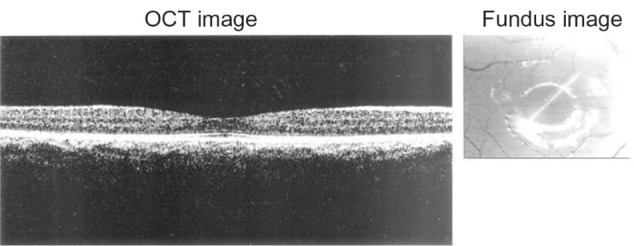
Pre-operative ocular (optical) coherence tomography image and fundus image of affected eye showing no abnormalities.
One percent prednisolone acetate drops were topically applied for 1 week. The patient, without a G6PD deficiency, was given dapsone 100 mg/daily, with which successful therapy of ocular rhinosporidiosis was reported,2,3 but the patient defaulted on the medication, which he discontinued after 1 week.
Six weeks later no recurrence was observed at the site of excision. Mild macular edema of the affected eye was suspected on admission but OCT, 1 month and 10 days after excision, showed no abnormality in both eyes. Follow-up 1 month later showed no retinal abnormalities in either eye.
Histopathologically, the lesion was initially reported as ‘chronic inflammation with mucous cysts’ on the presence of circular spaces without well-defined walls containing homogeneous eosinophilic material (Figure 3). Careful re-examination of several other sections stained with H&E showed spherical, cystic spaces that possessed thick, amorphous walls that resembled rhinosporidial sporangia containing amorphous, eosinophilic material without endospores (Figure 4), and other spherical cystic spaces that had no identifiable walls but contained deeply basophilic, spherical bodies approximately 10 µm in diameter compatible with rhinosporidial endospores (Figure 5); these histopathological appearances resembled the atypical appearances earlier described in rhinosporidiosis,4 and the clinical diagnosis of rhinosporidiosis of the bulbar conjunctiva was confirmed. Serum antirhinosporidial antibody levels were not assayed, as they were previously shown,5 when present in low titers, to have doubtful value in the diagnosis of rhinosporidiosis. Since Rhinosporidium seeberi is uncultivable in vitro, culture was not attempted.
Figure 3.
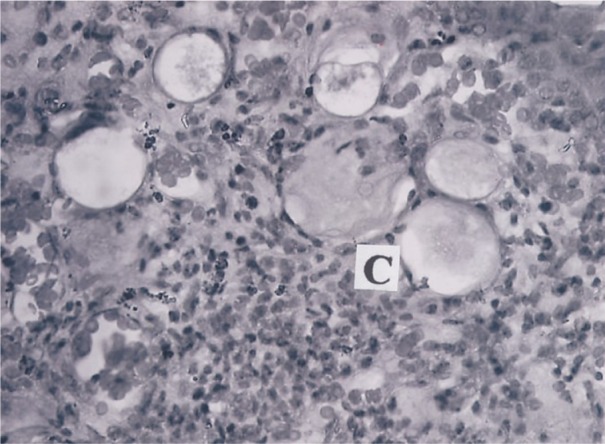
Histopathology of the rhinosporidial growth showing mononuclear cell infiltration and cystic areas (C) with thin, atypical, structureless walls enclosing amorphous eosinophilic material, which were initially identified as mucus cysts. Initial magnification × 400. H&E.
Figure 4.
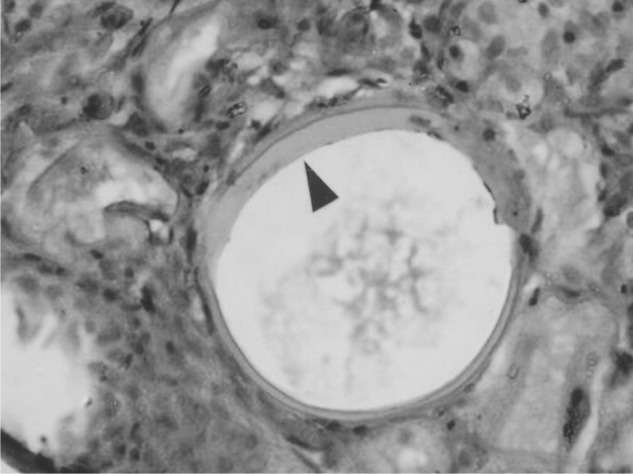
An empty rhinosporidial sporangium with abnormally thickened walls (arrow), containing amorphous eosinophilic material; rhinosporidial endospores are not seen. Initial magnification × 400. H&E.
Figure 5.
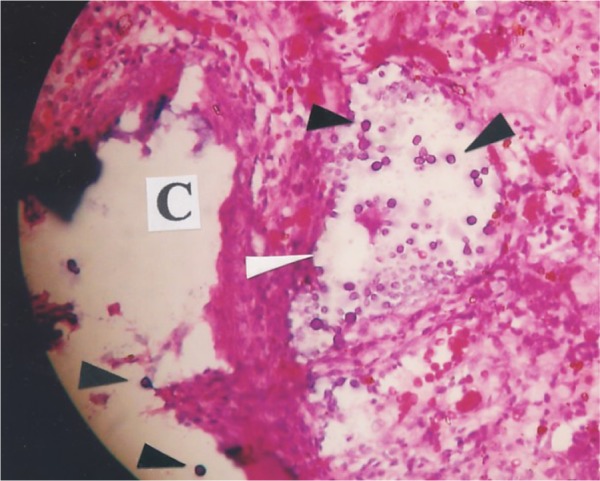
A mature rhinosporidial sporangium without typical walls (white arrow), containing basophilic rhinosporidial endospores (black arrows); the cystic space (C) without a wall represents an atypical sporangium with 2 free endospores (black arrows). Initial magnification × 400. H&E.
The patient was reviewed twice over the next 5 months, but no recurrence of the rhinosporidial lesions was observed, despite the abbreviated course of oral dapsone therapy. Four and a half months after his first visit, slit-lamp examination of the affected eye showed a gray-bluish scleral discoloration at the site of the original staphyloma, but was of lesser intensity (Figure 6). The left eye remained normal.
Figure 6.
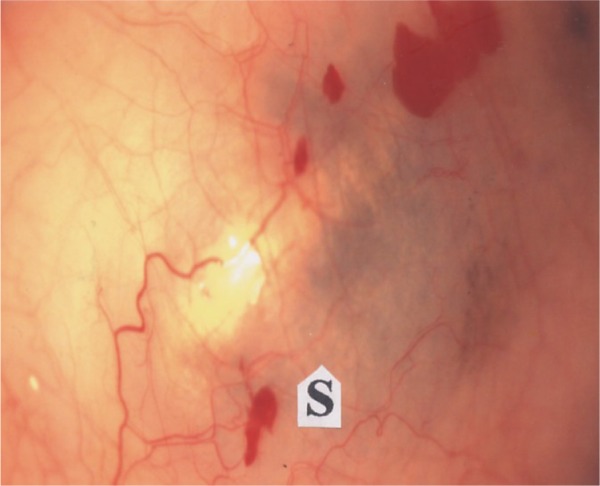
Slit-lamp photograph of the affected eye showing the site of original rhinosporidial growth, 5 months after excision showing residual staphyloma (S). The red patches are subconjunctival hemorrhages.
Discussion
Bulbar rhinosporidiosis with staphyloma formation was previously reported from India (8 cases), The Netherlands (1 case), and Sri Lanka (4 cases).1
The case described here had noteworthy features:
The ocular rhinosporidiosis was primary, and not secondary to rhinosporidiosis in nasal or other sites as in the previous 4 Sri Lankan cases, but was unlike the Indian1 and Netherlands cases reported previously.6
The patient gave a history of exposure to lacustrine waters for bathing, as in the previous 4 Sri Lankan cases.
The interval between the patient’s exposure to the lacustrine water in the rhinosporidiosis-endemic region and the development of the bulbar rhinosporidial growth with a concurrent staphyloma was, according to the patient’s history, as short as 3 weeks, the shortest period in Sri Lankan cases. Two previous Sri Lankan cases1 had an interval of 2 years and several years between the appearance of the rhinosporidial growth and the staphyloma, respectively, while 2 had simultaneous presentations of the rhinosporidial growth and the staphyloma of uncertain duration.
The staphyloma was near to and separated from but not contiguous with or under the rhinosporidial growth. This appearance differed from those recorded in previous cases from Sri Lanka in which the staphylomas were hemispherical, raised, cystic swellings with well-defined edges, adjacent to the rhinosporidial growth.1
There were no retinal abnormalities unlike in 2 previous Sri Lankan cases (one of which had a choroidal effusion, retinal detachment, a macular hole and a retinal fold), and in the cases reported from India1 and The Netherlands.6 The shorter history of 3 weeks and early management of the present case were the probable reasons for their absence.
The initial histopathological diagnosis was a mis-diagnosis of mucous cysts as well as a missed diagnosis of rhinosporidiosis; other replicate sections showed endosporulating sporangia amidst a chronic inflammatory cellular (lymphocytes, macrophages) infiltrate.
The thinning of the sclera and staphyloma formation were probably due to enzymic dissolution of scleral tissues by the pathogen, as first suggested by de Doncker et al6 and substantiated by Arseculeratne et al.4
Several H&E-stained sections of the specimen were available, but initially many of them had appearances shown in Figure 2 where no rhinosporidial entities (sporangia or endospores) were seen amidst the mononuclear cell infiltration, while circular bodies initially recognized as mucus cysts were visible. Other sections showed entities that were identified as rhinosporidial: a) the fragment of a mature sporangial wall (Figure 3), b) an atypical sporangium, without walls but containing endospores (Figure 4). These atypical appearances have previously been described as representing unusual features that could result in a missed or mis-diagnosis of rhinosporidiosis.4 Such appearances are important in the identification of rhinosporidial lesions in countries that are nonendemic for rhinosporidiosis, with histopathologists unfamiliar with the variations in rhinosporidial histopathology. In addition, wide sampling not only of the original lesion but also of histological sections needs to be made before a final diagnosis is made. The histopathological appearances of the pathogen are regarded as being diagnostic, and in this case were sufficiently diagnostic of rhinosporidiosis, eliminating the need for the use of molecular techniques; serum antibody titers are not sufficiently specific for diagnosis.
Footnotes
Disclosure
The authors declare no conflicts of interest in this work.
References
- 1.Senaratne T, Senanayake S, Edussuriya K, Wijenayake P, Arseculeratne S. Ocular rhinosporidiosis with staphyloma formation: The first report in Sri Lanka. J Infect Dis Antimicrob Agents. 2007;24:133–141. [Google Scholar]
- 2.Job A, Venkateswaran S, Mathan M, Krishnaswami H, Raman R. Medical therapy of rhinosporidiosis with dapsone. J Laryngol Otol. 1993;107:809–812. doi: 10.1017/s002221510012448x. [DOI] [PubMed] [Google Scholar]
- 3.John SS, Mohandas SG. Conjunctival oculosporidiosis with scleral thnning and staphyloma formation. Indian J Ophthalmol. 2005;53:272–274. doi: 10.4103/0301-4738.18912. [DOI] [PubMed] [Google Scholar]
- 4.Arseculeratne SN, Panabokke RG, Atapattu DN. Lymphadenitis, Trans-epidermal elimination and unusual histopathology in human rhinosporidiosis. Mycopathologia. 2002;153:57–69. doi: 10.1023/a:1014459100736. [DOI] [PubMed] [Google Scholar]
- 5.Arseculeratne SN, Kumarasiri PV, Rajapakse RP, Perera NA, Arseculeratne G, Atapattu DN. Anti-rhinosporidial antibody levels in patients with rhinosporidiosis and in asymptomatic persons in Sri Lanka. Mycopathologia. 2004;158:157–164. doi: 10.1023/b:myco.0000041903.48717.79. [DOI] [PubMed] [Google Scholar]
- 6.de Doncker RM, de Keizer RJ, Oosterhuis JA, Maes A. Scleral melting in a patient with conjunctival rhinosporidiosis. Br J Ophthalmol. 1990;74:635–637. doi: 10.1136/bjo.74.10.635. [DOI] [PMC free article] [PubMed] [Google Scholar]


