Abstract
A “cold” defect or an area of decreased radiotracer deposition is the less common appearance of acute hematogenous osteomyelitis (AHO) on a Tc99 m-methylene disphosphonate (Tc99 m-MDP) bone scan. Group A beta-hemolytic Streptococcus (GABHS) is a significantly less common cause of AHO than Staphylococcus aureus, particularly when the infection involves the pelvis or flat bones such as the ribs. Here, we present a case report of isolated acute “cold” hematogenous osteomyelitis in a rib of a child with GABHS bacteremia that was detected on 99Tc-MDP bone scan, with magnetic resonance imaging correlation, and pathologic confirmation after rib resection.
Keywords: Bone scan, cold, Group A beta-hemolytic Streptococcus, osteomyelitis, photopenic, Tc99 m-methylene disphosphonate
Disclaimer: The views expressed herein are those of the author(s) and do not necessarily reflect the official policy or position of the Department of Navy, Department of Defense, or the U.S. Government.
Introduction
A “cold” defect or an area of decreased radiotracer deposition on a Tc99 m-methylene disphosphonate (Tc99 m-MDP) bone scan may represent infection, neoplasm, infarction, foreign body, or artifact. “Cold” osteomyelitis is often a subperiosteal abscess resulting from underlying osteomyelitis. This often causes a disruption of small adjacent periosteal blood vessels resulting in a lack of Tc99 m-MDP accumulation in the area of infection. “Cold” osteomyelitis is associated with a higher severity of infection often requiring aggressive medical and surgical intervention, and is a less common appearance of osteomyelitis in pediatric patients.
Case Report
A 14-month-old male with history of a febrile urinary tract infection 3 weeks prior presented to the emergency department with fever up to 39.4°C and emesis for 3 days. Laboratory tests showed a white blood cell (WBC) count of 15 (normal range: 7.8–14.8). Two abdominal ultrasounds and a subsequent computed tomography of the abdomen were only notable for a small amount of free intraperitoneal fluid. Due to persistent fevers, blood cultures were drawn and grew Group A beta-hemolytic Streptococcus (GABHS). A 3-phase whole body Tc99 m-MDP bone scan showed a “cold” defect in the right 7th rib on the delayed images [Figure 1]. The blood flow and blood pool images were unremarkable. A subsequent magnetic resonance scan of the chest showed an extensive subperiosteal abscess along a majority of the right 7th rib, a small soft tissue abscess anteriorly, and signal abnormality with the rib consistent with osteomyelitis [Figures 2 and 3]. Despite successful interventional radiology percutaneous decompression and drainage of the abscesses, which grew GABHS, the patient continued to have fevers and an elevated WBC count. The patient then underwent resection of the entire right 7th rib, resulting in resolution of symptoms and subsequent down trending of the WBC count. Pathological analysis of the surgically resected rib confirmed osteomyelitis [Figure 4]. At the time of discharge, the patient was back to his baseline and sent home with a course oral antibiotics.
Figure 1.

Tc99 m-methylene disphosphonate bone scan with additional lateral planar images of the chest showing “cold” defect in the right 7th rib. Urine contamination accounts for the radiotracer accumulation over the right distal femur. The remainder of the uptake distribution is normal
Figure 2.

(a) Short-tau inversion recovery, (b) T2 (1250/70 [repetition time/echo time]), (c) T1 precontrast, (d) T1 postcontrast axial 3T magnetic resonance imaging of the right chest wall showing hyperintense T2 and hypointense T1 signal within the marrow space and beneath the periosteum surrounding the rib 7th rib (arrow) compatible with a subperiosteal abscess with underlying osteomyelitis. Note the relative lack of enhancement in the affected rib due to the compromised periosteal blood supply (d). A right pleural effusion is also present
Figure 3.

(a) Short-tau inversion recovery, (b) T2 (1250/70 [repetition time/echo time]), (c) T1 precontrast, (d) T1 postcontrast axial 3T magnetic resonance imaging of the right chest wall just inferior to the level of Figure 2 showing a small soft tissue abscess anterior to the subperiosteal abscess involving the right rib 7th (arrow)
Figure 4.
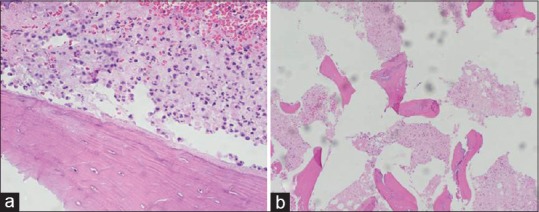
Two H and E-stained slides of the resected rib demonstrate dead bone marrow with an abnormally increased number of neutrophils (a), and dead bone with empty lacunae surrounded by dead bone marrow with a few inflammatory cells (b). These findings are consistent with osteomyelitis
Discussion
“Cold” osteomyelitis is an uncommon presentation of acute osteomyelitis in children. This term describes a subperiosteal abscess resulting from underlying osteomyelitis that causes a disruption of superficial periosteal blood vessels resulting in a lack of Tc99 m-MDP accumulation in the area of infection.[1] The thicker periosteum in children is more easily lifted from the bone.[1] This not only allows a subperiosteal abscess to form but enables the abscess, once formed, to spread along the bone disrupting the periosteal vessels.[1] A large portion of the blood supply to and from the bone in children is from these vessels.[2] Regardless of whether the subperiosteal vessels are compromised via compression or direct disruption, there is a resultant decrease in the blood supply to the underlying bone. Bone ischemia ensues and a consequent reduction in the flow of Tc99 m-MDP to the area of infection results. The most common cause of a subperiosteal abscess is underlying osteomyelitis. The subperiosteal abscess and its impact to the bone vasculature cause an area of decreased radiotracer deposition or “cold” defect on bone scintigraphy.[1]
The differential diagnosis for a “cold” defect on a bone scan is relatively short including infection, neoplasm, infarction, foreign body, or artifact. Several of these entities can usually be quickly excluded based on clinical findings. Among infectious causes, GABHS is only second to Staphylococcus aureus as the most common cause of acute hematogenous osteomyelitis (AHO) in children, representing approximately 10% of cases compared to 43% for S. aureus.[3] Tubular bones are the most common site of AHO regardless of the causative organism, with the femur involved in 23% of cases in one study.[3] In the same study, S. aureus was the most common causative organism (74% of cases) of infections involving the pelvis and flat bones (skull, ribs, sternum, scapula), whereas GABHS only accounted for 16% of cases.[3] Rib osteomyelitis is a rare infection, often a result of contiguous spread (62%), such as from an adjacent abscess or infected surgical bed, and less common via hematogenous spread (38%).[4]
Thus, this case is noteworthy in that the patient's infection was due to an organism (GABHS) that is an infrequent cause of AHO, particularly within a rib via hematogenous spread, with an uncommon presentation (”cold” defect) on 99 mTc-MDP bone scan.
“Cold” osteomyelitis is an important diagnosis to make in a timely manner because a subperiosteal abscess is an indication for surgery to prevent osteonecrosis and chronic osteomyelitis.[1] Children presenting with a cold defect on bone scintigraphy often have a more aggressive bone infection, requiring aggressive medical, and surgical intervention.[5]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of intrest.
References
- 1.Allwright SJ, Miller JH, Gilsanz V. Subperiosteal abscess in children: Scintigraphic appearance. Radiology. 1991;179:725–9. doi: 10.1148/radiology.179.3.2027982. [DOI] [PubMed] [Google Scholar]
- 2.Schauwecker DS. The scintigraphic diagnosis of osteomyelitis. AJR Am J Roentgenol. 1992;158:9–18. doi: 10.2214/ajr.158.1.1727365. [DOI] [PubMed] [Google Scholar]
- 3.Ibia EO, Imoisili M, Pikis A. Group A beta-hemolytic streptococcal osteomyelitis in children. Pediatrics. 2003;112(1 Pt 1):e22–6. doi: 10.1542/peds.112.1.e22. [DOI] [PubMed] [Google Scholar]
- 4.Bishara J, Gartman-Israel D, Weinberger M, Maimon S, Tamir G, Pitlik S. Osteomyelitis of the ribs in the antibiotic era. Scand J Infect Dis. 2000;32:223–7. doi: 10.1080/00365540050165839. [DOI] [PubMed] [Google Scholar]
- 5.Pennington WT, Mott MP, Thometz JG, Sty JR, Metz D. Photopenic bone scan osteomyelitis: A clinical perspective. J Pediatr Orthop. 1999;19:695–8. [PubMed] [Google Scholar]


