Abstract
Nerve fibers are attracted by sutureless end-to-side nerve coaptation into the recipient nerve. Opening a window in the epineurium enhances axon attraction and myelination. The authors analyze the features of nerve repair by end-to-side coaptation. They highlight the known mechanisms of axon sprouting and different hypotheses of start up signals (presence or absence of an epineurial window, role of Schwann cells, signaling from the distal trunk). The clinical literature is also presented and differences between experimental and clinical applications are pointed out. The authors propose their point of view and perspectives deriving from recent experimental and clinical experiences.
Keywords: peripheral nerve repair, nerve coaptation, end-to-side nerve repair, side-to-side nerve repair, epineurial window, Schwann cells, nerve regeneration, nerve babysitter procedures, nerve transfer, nerve graft, glues in nerve repair
Introduction
The role of end-to-side (ETS) coaptation has been debated for a long time since first experience by Viterbo et al. (1982).
Several studies have been published proposing the theoretical bases for its clinical application. To date, experimental evidences can be considered as well-established scientific data, but a debate remains open about clinical utilization (Dvali and Myckatyn, 2008). Since the pioneering work from Terzis and Tzafetta (2009a, b) about distal babysitting of injured facial nerve through ETS coaptation and partial neurotomy, some authors are still wondering whether an important damage to the donor nerve could derive from this application.
Reviewing the whole literature reveals how this technique remains a domain of some experts (Al-Qattan and Al-Thunyan, 1998; Battiston and Lanzetta, 1999; Al-Qattan, 2001; Tung and Mackinnon, 2001; Mennen et al., 2003; Tung et al., 2003; Frey and Giovanoli, 2003a, b; Bertelli and Ghizoni, 2003; Amr and Moharram, 2005; Millesi and Schmidhammer, 2008); Magdi Sherif and Amr, 2010; Barbour et al., 2012) and is mostly performed by choosing selected donors for nerve transfers to protect distal effectors in cases of proximal trunk injuries.
Millesi and Schmidhammer (2008) published an interesting review and concluded that in case of high proximal injuries of nerve trunks in the upper extremity, more proximal nerve transfers failed to function, whereas choosing distal motor nerves gave the best results. These observations were supported by experimental evidences in the baboon (Mennen, 1998) and were confirmed by a clinical series of brachial plexus injuries.
We review the literature starting from the biological bases of ETS, and discuss the usefulness of this technique, relating experimental and clinical data from other scholars and from their own experience.
ETS Coaptation: An Effective Technique
Experimental
ETS nerve repair has proven an effective tool for repairing peripheral nerves in experimental microsurgery, from both functional and morphological points of view (Bontioti and Dahlin, 2009; Papalia et al., 2016).
Three mechanisms have been proposed: a) contamination from axons regenerating from the proximal stump of the recipient nerve, b) true collateral sprouting from healthy fibers of the donor nerve and c) true axonal regeneration from damaged fibers of the donor nerve (“terminal sprouting”) (Bontioti and Dahlin, 2009; Papalia et al., 2016).
“Simple” coaptation
Dealing with “simple coaptation”, few studies have been conducted without opening any window into the nerve connective tissue; a simple coaptation of a cut distal stump into a donor nerve trunk, is a stimulus for nerve repair by sutures passing through the donor nerve (see below, A. 2) (Kanje et al., 2000; Papalia et al., 2016).
Our original research about sutureless (cyanoacrylate glue) ETS nerve repair opened another scenario, demonstrating that simple glue coaptation without any window was capable to attract nerve fibers from the donor to the recipient trunk; however, from a morphological point of view, regenerating axons were smaller and less myelinated (Papalia et al., 2016).
Really, the presence of only a cut distal stump represents a powerful attraction for newly formed axons from a donor healthy trunk, maybe for its production of growth factors and signals, which have been shown also coming from distal effectors via retrograde transportation (Wood and Mackinnon, 2015).
How does a window opened into the connective nerve sheaths work?
Indeed, opening a window acts on Schwann cells and molecular components breaking the antineurotropic continuity of the wall constituted by epi- and/or perineurium (Bontioti and Dahlin, 2009; Kovačič et al., 2012); the effect of this breakthrough is a realignment of Schwann cells creating open gates both from a cellular and an ionic/molecular point of view. Through these gates acting as positive signals for axon outgrowth, neurite cones are attracted; moreover, attractive properties from degenerated distal axons together with retrograde chemiokinetic signals from distal effectors via the distal stump complete the job (Kovačič et al., 2012; Wood and MacKinnon, 2015).
Different sizes of epi-perineurial windows have been studied (Kovačič et al., 2012): enlarging the window from 1 to 4/5 mm produces an increased ingrowth of larger axons.
In these basic conditions, even a simple sutureless coaptation has proven effective in directing donor fibers to the recipient trunk (Papalia et al., 2016).
Other factors playing a positive role
Sutures have a role by an additional trauma represented by their passage through the connective tissue. Some authors suggested they could act through pressure and associated bleeding and inflammation (Kelly et al., 2007). Also glues have been shown to have a positive role through early inflammatory steps (Bontioti and Dahlin, 2009). As in wound healing process, where macrophages have been shown to play a critical role, early inflammation in nerve repair promotes Schwann cells activation (Papalia et al., 2016), and could be therefore defined as an “healthy” inflammation.
Disinhibition: let inhibitory factors shut up
Switching inhibitory factors off is a major task in nerve repair. To date, we know that the major inhibitory molecules are associated either with myelin or with scar tissue formation. NogoA, MAG, and OMgp are present in myelin debris and work through the Nogo receptor. In nerve scar tissue, chondroitin sulphate, proteoglycans, and semaphorins, together with the formation of a collagen-based membrane, act as inhibitory factors (Fawcett et al., 2012).
Time also runs against
Time has also been studied as an important factor in nerve regeneration, through both progressive increasing of inhibitory factors and decreasing activities (a true senescence) of Schwann cells. Peripheral nerve surgeons aware that for more proximal injuries, more time is required for nerve regeneration, with a finally negative outcome due to distal effectors atrophy (Papalia et al., 2016).
Do ETS procedures produce damage to the donor nerve?
Some studies found that ETS neurorrhaphy results in donor nerve injury and regeneration of the injured nerve (Okajima and Terzis, 2000; Brenner et al., 2007). In these experimental papers, it has been observed that ETS coaptation which epineurial window either alone or together with partial neurotomy produces a certain loss (“escape”) of nerve fibers from the donor nerve; this report ever restricts surgeon's choice keeping in mind that performing ETS coaptation will damage donor nerve function (Colonna et al., 2015). Since this point, investigators have been searching for the best donor: should it be agonist/antagonist, sensory even if recipient is motor (Papalia et al., 2007, 2016; Colonna et al., 2015; Nghiem et al., 2015)?
Which is the mechanism of fibers spreading through an ETS repair?
There is plenty of evidence on ETS about collateral sprouting of the donor nerve: surgical windows through neural connective tissue open the way for cathionic passageways and activate neuronal molecular pathways (by regulating expression of IGF-1 and TWEAK-Fn14) for regeneration from the donor nerve into the recipient one (Lundborg et al., 1994; Noah et al., 1997; Zhang et al., 1999; Xiong et al., 2003; Hayashi et al., 2004; Bontioti et al., 2005; Samal et al., 2006; Kovacic et al., 2007; Zhu et al., 2008; Liu et al., 2015, 2016b).
Which is the precise site from which new fibers spread out to enter ETS coaptation site?
A number of investigators (Bajrovic et al., 2002; Matsuda et al., 2005; Akeda et al., 2006; Bontioti et al., 2006) questioned the true origin of axons from the donor nerve: do they come from the axons closest to the coaptation site or from a more proximal site?
Morphological evidences have been reported of true regeneration from the Ranvier's nodes just close to the coaptation site (Zhu et al., 2008). However, in this study, only a qualitative analysis showing the sprouting of myelinated axons is reported. No further information about the amount of collateral sprouting fibers nor evidences of presence of unmyelinated fibers are described.
Other studies have proposed a more proximal origin, just from the dorsal ganglia or the spinal cord (Kim et al., 2012). To date, this question remains debated.
Fibers specificity: does it work?
Donor motor fibers have been proposed specifically for motor recipient trunks, as well as donor sensory fibers for sensory recipient trunks. As far as it concerns motor fibers, to regulate the number of spreading axons and the number of impulses, several authors have introduced partial neurectomy of the donor nerve (Terzis and Tzafetta, 2009a, b; Liu et al., 2015, 2016a). The use of sensory nerves as donors even in motor nerve injuries has been supported by a conspicuous report (Nghiem et al., 2015). To date, however, using sensory nerves for motor neurotization has not yet been proposed in the clinical field. But why not?
The choice for agonists in ETS nerve transfer
Even when choosing motor nerves as donors, their role as agonists of the recipient nerve has been debated; it has been concluded not to introduce conflict between agonists (Papalia et al., 2007). Millesi and Schmidhammer (2008) selected the trunk for the short head of Flexor Pollicis Brevis as donor for median thenar branch babysitting, as FPB acts as an agonist of thenarian muscles.
Double end-to-side: side-to-side. A look into clinical work and perspectives
A nerve graft can be coapted ETS as a bridge between the donor and the recipient trunk; Yüksel et al. (1999) in their experimental paper showed that babysitter procedure with side-to-side technique gave functional results superiors to ETS technique. In clinical studies, this kind of nerve fiber transfer has been proposed and used successfully in most distal nerve transfers for proximal nerve injuries (Magdi Sherif and Amr, 2010; Colonna et al., 2015, Gesslbauer et al., 2016).
Clinical: What have we learned from experimental research which can be translated to clinical practice?
To date, the peripheral nerve surgeons yet face challenging problems, especially with proximal nerve injuries produced by avulsion. A very small or no regeneration follows this dramatic event, producing anatomical changes in distal effectors, as well as severe functional deficits.
Even if direct or graft nerve repair between proximal and distal stump remains the gold standard, distal motor end-plate and sensory receptors hypotrophy will occur because of the long distance and time to be run by regenerating fibers from their proximal coaptation/graft site. Nerve fibers need to be brought distally as fast as possible and this is why we need short and quick motor nerve transfers (Bontioti and Dahlin, 2009; Colonna et al., 2015; Papalia et al., 2016).
However, we must remember that in the case of distal babysitter nerve transfers, clinical reports (MacKinnon et al., 2005; Moore et al., 2014; Sassu et al., 2015; Ray et al., 2016) agree that grading of the motor function cannot be achieved with the same precision (Isaacs, 1999) as for proximal techniques (Oberlin et al., 1994).
Indeed, opening a window in epiperineurium creates a sort of epineurial chamber similar to the experimental Lundborg chamber (Lundborg et al., 1982). It attracts all collateral and central axon sprouts towards empty endoneural tube on all recipient nerve stump surface. It should be reserved to an experienced microsurgeon trained in microsurgical peripheral nerve reconstruction.
Conclusions
New techniques and materials have been proposed as variants for ETS, and we expect novel reports regarding new materials to be used as conduits and gene therapy, too.
New techniques: reverse ETS
More recently, a new variant of ETS nerve coaptation has been described (Li et al., 2014), taking nerve fibers from a healthy trunk, which is severed distally and coapted ETS to the recipient injured nerve. This report seems very interesting as it couples the use of ETS with a donor sensory trunk to a recipient motor nerve.
Our experience
A recent study opened new perspectives for the comprehension of the mechanisms underlying ETS nerve regeneration. In this work, a sutureless technique for performing ETS neurorrhaphy was developed to verify whether axon regeneration can be induced by the biological lure coming from the damaged nerve without any trauma at the coaptation site (Papalia et al., 2016).
In adult female rats, the median nerve was glued to the ulnar nerve epineurium using N-butyl-2-cyanoacrylate. In one experimental group a small epineurial window was opened before coaptation while in another group gluing was performed without any intentional damage to the ulnar nerve epineurium.
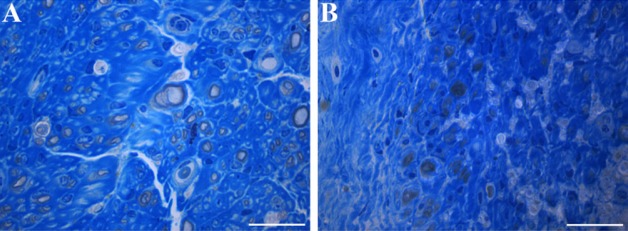
“Simple” gluing excludes trauma, inflammation and starts up signals for regeneration from sutures; nevertheless, regeneration and axons income from the donor to the recipient nerve occurred no matter epineurium was opened or not. Both from a quantitative and qualitative points of view, axons and fibers were more represented when the window was opened (Figure 1).
Figure 1.
Representative high resolution light microscopic images of toluidine-blue-stained transverse sections of median nerve 36 weeks after end-to-side coaptation with N-butyl-2-cyanoacrylate.
(A) Coaptation with an epineurial window; (B) coaptation without an epineurial window. With an epineurial window, the regenerated fibers are more numerous. Bars: 20 μm.
Thus, to date we can say that opening a window and gluing produces a valid regeneration through an ETS coaptation.
Moreover, even if epi-perineurial sheaths are not opened, a simple sutureless coaptation of a severed nerve trunk to the side of an healthy trunk is capable to attract axons from this last one.
Our group is on the way with further studies about the role of Schwann cells and attracting factors from the severed trunk, as well as stimulation with gene transfer, bioactive materials, and protecting the coaptation site (or sites when a graft is required) with wrapping.
Footnotes
Conflicts of interest: None declared.
References
- Akeda K, Hirata H, Matsumoto M, Fukuda A, Tsujii M, Nagakura T, Ogawa S, Yoshida T, Uchida A. Regenerating axons emerge far proximal to the coaptation site in end-to-side nerve coaptation without a perineurial window using a T-shaped chamber. Plast Reconstr Surg. 2006;117:1194–1203. doi: 10.1097/01.prs.0000201460.54187.d7. [DOI] [PubMed] [Google Scholar]
- Al-Qattan MM, Al-Thunyan A. Variables affecting axonal regeneration following end-to-side neurorrhaphy. Br J Plast Surg. 1998;51:238–242. doi: 10.1054/bjps.1997.0188. [DOI] [PubMed] [Google Scholar]
- Al-Qattan MM. Terminolateral neurorrhaphy: review of experimental and clinical studies. J Reconstr Microsurg. 2001;17:99–108. doi: 10.1055/s-2001-12698. [DOI] [PubMed] [Google Scholar]
- Amr SM, Moharram AN. Repair of brachial plexus lesions by end-to-side side-to-side grafting neurorrhaphy: experience based on 11 cases. Microsurgery. 2005;25:126–146. doi: 10.1002/micr.20036. [DOI] [PubMed] [Google Scholar]
- Bajrovic F, Kovacic U, Pavcnik M, Sketelj J. Interneuronal signaling is involved in induction of collateral sprouting of nociceptive axons. Neuroscience. 2002;111:587–596. doi: 10.1016/s0306-4522(01)00588-7. [DOI] [PubMed] [Google Scholar]
- Barbour J, Yee A, Kahn LC, Mackinnon SE. Supercharged end-to-side anterior interosseous to ulnar motor nerve transfer for intrinsic musculature reinnervation. J Hand Surg Am. 2012;37:2150–2159. doi: 10.1016/j.jhsa.2012.07.022. [DOI] [PubMed] [Google Scholar]
- Battiston B, Lanzetta M. Reconstruction of high ulnar nerve lesions by distal double median to ulnar nerve transfer. J Hand Surg Am. 1999;24:1185–1191. doi: 10.1053/jhsu.1999.1185. [DOI] [PubMed] [Google Scholar]
- Bertelli JA, Ghizoni MF. Nerve repair by end-to-side coaptation or fascicular transfer: a clinical study. J Reconstr Microsurg. 2003;19:313–318. doi: 10.1055/s-2003-42499. [DOI] [PubMed] [Google Scholar]
- Bontioti E, Kanje M, Lundborg G, Dahlin LB. End-to-side nerve repair in the upper extremity of rat. J Peripher Nerv Syst. 2005;10:58–68. doi: 10.1111/j.1085-9489.2005.10109.x. [DOI] [PubMed] [Google Scholar]
- Bontioti E, Dahlin LB, Kataoka K, Kanje M. End-to-side nerve repair induces nuclear translocation of activating transcription factor 3. Scand J Plast Reconstr Surg Hand Surg. 2006;40:321–328. doi: 10.1080/02844310600999956. [DOI] [PubMed] [Google Scholar]
- Bontioti E, Dahlin LB. Chapter 12: Mechanisms underlying the end-to-side nerve regeneration. Int Rev Neurobiol. 2009;87:251–268. doi: 10.1016/S0074-7742(09)87012-8. [DOI] [PubMed] [Google Scholar]
- Brenner MJ, Dvali L, Hunter DA, Myckatyn TM, Mackinnon SE. Motor neuron regeneration through end-to-side repairs is a function of donor nerve axotomy. Plast Reconstr Surg. 2007;120:215–223. doi: 10.1097/01.prs.0000264094.06272.67. [DOI] [PubMed] [Google Scholar]
- Colonna MR, Russo A, Galeano M, Delia G, Pajardi GE, d’Alcontres FS. “Babysitting” procedures in proximal nerve trunk injuries: two case reports and a review. Plast Aesthet Res. 2015;2:208–212. [Google Scholar]
- Dvali LT, Myckatyn TM. End-to-side nerve repair: review of the literature and clinical indications. Hand Clin. 2008;24:455–460. doi: 10.1016/j.hcl.2008.04.006. [DOI] [PubMed] [Google Scholar]
- Fawcett JW, Schwab ME, Montani L, Brazda N, Müller HW. Defeating inhibition of regeneration by scar and myelin components. Handb Clin Neurol. 2012;109:503–522. doi: 10.1016/B978-0-444-52137-8.00031-0. [DOI] [PubMed] [Google Scholar]
- Fortes WM, Noah EM, Liuzzi FJ, Terzis JK. End-to-side neurorrhaphy: evaluation of axonal response and upregulation of IGF-I and IGF-II in a non-injury model. J Reconstr Microsurg. 1999;15:449–457. doi: 10.1055/s-2007-1000126. [DOI] [PubMed] [Google Scholar]
- Frey M, Giovanoli P. End-to-side neurorrhaphy of sensory nerves. Eur J Plast Surg. 2003a;26:85–88. [Google Scholar]
- Frey M, Giovanoli P. End-to-side neurorrhaphy of motor nerves: reinnervation of free muscle transplants– first clinical application. Eur J Plast Surg. 2003b;26:89–94. [Google Scholar]
- Giovanoli P, Koller R, Meuli-Simmen C, Rab M, Haslik W, Mittlböck M, Meyer VE, Frey M. Functional and morphometric evaluation of end-to-side neurorrhaphy for muscle reinnervation. Plast Reconstr Surg. 2000;106:383–392. doi: 10.1097/00006534-200008000-00021. [DOI] [PubMed] [Google Scholar]
- Hayashi A, Yanai A, Komuro Y, Nishida M, Inoue M, Seki T. Collateral sprouting occurs following end-to-side neurorrhaphy. Plast Reconstr Surg. 2004;114:129–137. doi: 10.1097/01.prs.0000129075.96217.92. [DOI] [PubMed] [Google Scholar]
- Isaacs J. Commentary on ‘Nerve grafts bridging the thenar branch of the median nerve to the ulnar nerve to enhance nerve recovery: a report of three cases’. J Hand Surg Eur Vol. 2017;42:286–288. doi: 10.1177/1753193416675990. [DOI] [PubMed] [Google Scholar]
- Kanje M, Arai T, Lundborg G. Collateral sprouting from sensory and motor axons into an end to side attached nerve segment. Neuroreport. 2000;11:2455–2459. doi: 10.1097/00001756-200008030-00023. [DOI] [PubMed] [Google Scholar]
- Kelly EJ, Jacoby C, Terenghi G, Mennen U, Ljungberg C, Wiberg M. End-to-side nerve coaptation: a qualitative and quantitative assessment in the primate. J Plast Reconstr Aesthet Surg. 2007;60:1–12. doi: 10.1016/j.bjps.2005.12.059. [DOI] [PubMed] [Google Scholar]
- Kovačič U, Zele T, Tomšič M, Sketelj J, Bajrović FF. Influence of breaching the connective sheaths of the donor nerve on its myelinated sensory axons and on their sprouting into the end-to-side coapted nerve in the rat. J Neurotrauma. 2012;29:2805–2815. doi: 10.1089/neu.2011.2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Zhang P, Yin X, Han N, Kou Y, Jiang B. Early sensory protection in reverse end-to-side neurorrhaphy to improve the functional recovery of chronically denervated muscle in rat: a pilot study. J Neurosurg. 2014;121:415–422. doi: 10.3171/2014.4.JNS131723. [DOI] [PubMed] [Google Scholar]
- Liu HF, Chen ZG, Shen HM, Zhang H, Zhang J, Lineaweaver WC, Zhang F. Efficacy of the end-to-side neurorrhaphies with epineural window and partial donor neurectomy in peripheral nerve repair: an experimental study in rats. J Reconstr Microsurg. 2015;1:31–38. doi: 10.1055/s-0034-1382263. [DOI] [PubMed] [Google Scholar]
- Liu HF, Chen ZG, Lineaweaver WC, Zhang F. Can the babysitter procedure improve nerve regeneration and denervated muscle atrophy in the treatment of peripheral nerve injury? Plast Reconstr Surg. 2016a;1:122–131. doi: 10.1097/PRS.0000000000002292. [DOI] [PubMed] [Google Scholar]
- Liu HF, Chen ZG, Lineaweaver WC, Friel MT, Zhang F. Molecular mechanism of the “babysitter” procedure for nerve regeneration and muscle preservation in peripheral nerve repair in a rat model. Ann Plast Surg. 2016b doi: 10.1097/SAP.0000000000000952. doi: 10.1097/SAP.0000000000000952. [DOI] [PubMed] [Google Scholar]
- Lundborg G, Dahlin LB, Danielsen N, Hansson HA, Johannesson A, Longo FM, Varon S. Nerve regeneration across an extended gap: a neurobiological view of nerve repair and the possible involvement of neuronotrophic factors. J Hand Surg Am. 1982;6:580–587. doi: 10.1016/s0363-5023(82)80107-x. [DOI] [PubMed] [Google Scholar]
- Lundborg G, Zhao Q, Kanje M, Danielsen N, Kerns JM. Can sensory and motor collateral sprouting be induced from intact peripheral nerve by end-to-side anastomosis? J Hand Surg (Br) 1994;19:277–282. doi: 10.1016/0266-7681(94)90069-8. [DOI] [PubMed] [Google Scholar]
- Mackinnon SE, Novak CB, Myckatyn TM, Tung TH. Results of reinnervation of the biceps and brachialis muscles with a double fascicular transfer for elbow flexion. J Hand Surg Am. 2005;5:978–985. doi: 10.1016/j.jhsa.2005.05.014. [DOI] [PubMed] [Google Scholar]
- Magdi Sherif M, Amr AH. Intrinsic hand muscle reinnervation by median-ulnar end-to-side bridge nerve graft: case report. J Hand Surg Am. 2010;35:446–450. doi: 10.1016/j.jhsa.2009.10.033. [DOI] [PubMed] [Google Scholar]
- Matsuda K, Kakibuchi M, Fukuda K, Kubo T, Madura T, Kawai K, et al. End-to-side nerve grafts: experimental study in rats. J Reconstr Microsurg. 2005;21:581–591. doi: 10.1055/s-2005-922439. [DOI] [PubMed] [Google Scholar]
- Mennen U. End-to-side nerve suturing technique. J Hand Surg Br. 2004;29:514. doi: 10.1016/j.jhsb.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Mennen U, van der Westhuizen MJ, Eggers IM. Re-innervation of M. biceps by end-to-side nerve suture. Hand Surg. 2003;8:25–31. doi: 10.1142/s0218810403001340. [DOI] [PubMed] [Google Scholar]
- Millesi H, Schmidhammer R. Nerve fiber transfer by end-to-side coaptation. Hand Clin. 2008;24:461–483. doi: 10.1016/j.hcl.2008.04.007. [DOI] [PubMed] [Google Scholar]
- Moore AM, Franco M, Tung TH. Motor and sensory nerve transfers in the forearm and hand. Plast Reconstr Surg. 2014;4:721–730. doi: 10.1097/PRS.0000000000000509. [DOI] [PubMed] [Google Scholar]
- Nghiem BT, Sando IC, Hu Y, Urbanchek MG, Cederna PS. Sensory protection to enhance functional recovery following proximal nerve injuries: current trends. Plast Aesthet Res. 2015;2:202–207. [Google Scholar]
- Noah EM, Williams A, Jorgenson C, Skoulis TG, Terzis JK. End-to-side neurorrhaphy: a histologic and morphometric study of axonal sprouting into an end-to-side nerve graft. J Reconstr Microsurg. 1997;13:99–106. doi: 10.1055/s-2007-1000224. [DOI] [PubMed] [Google Scholar]
- Oberlin C, Beal D, Leechavengvongs S, Salon A, Dauge MC, Sarcy JJ. Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus: anatomical study and report of four cases. J Hand Surg Am. 1994;2:232–237. doi: 10.1016/0363-5023(94)90011-6. [DOI] [PubMed] [Google Scholar]
- Okajima S, Terzis JK. Ultrastructure of early axonal regeneration in an end-to-side neurorrhaphy model. J Reconstr Microsurg. 2000;16:313–323. doi: 10.1055/s-2000-7339. [DOI] [PubMed] [Google Scholar]
- Papalia I, Cardaci A, d’Alcontres FS, Lee JM, Tos P, Geuna S. Selection of the donor nerve for end-to-side neurorrhaphy. J Neurosurg. 2007;107:378–382. doi: 10.3171/JNS-07/08/0378. [DOI] [PubMed] [Google Scholar]
- Papalia I, Magaudda L, Righi M, Ronchi G, Viano N, Geuna S, Colonna MR. Epineurial window is more efficient in attracting axons than simple coaptation in a sutureless (cyanoacrylate-bound) model of end-to-side nerve repair in the rat upper limb: functional and morphometric evidences and review of the literature. PLoS One. 2016;11:e0148443. doi: 10.1371/journal.pone.0148443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray ZW, Chang J, Hawasli A, Wilson JT, Yang L. Motor nerve transfers: a comprehensive review. Neurosurgery. 2016;78:1–26. doi: 10.1227/NEU.0000000000001029. [DOI] [PubMed] [Google Scholar]
- Samal F, Haninec P, Raska O, Dubovwy P. Quantitative assessment of the ability of collateral sprouting of the motor and primary sensory neurons after the end-to-side neurorrhaphy of the rat musculocutaneous nerve with the ulnar nerve. Ann Anat. 2006;188:337–344. doi: 10.1016/j.aanat.2006.01.017. [DOI] [PubMed] [Google Scholar]
- Sassu P, Libberecht K, Nilsson A. Nerve transfers of the forearm and hand: a review of current indications. Plast Aesthet Res. 2015;2:195–201. [Google Scholar]
- Terzis JK, Tzafetta K. The “babysitter” procedure: mini hypoglossal to facial nerve transfer and cross-facial nerve grafting. Plast Reconstr Surg. 2009a;123:865–876. doi: 10.1097/PRS.0b013e31819ba4bb. [DOI] [PubMed] [Google Scholar]
- Terzis JK, Tzafetta K. “Babysitter” procedure with concomitant muscle transfer in facial paralysis. Plast Reconstr Surg. 2009b;124:1142–1156. doi: 10.1097/PRS.0b013e3181b2b8bc. [DOI] [PubMed] [Google Scholar]
- Tung TH, Mackinnon SE. Flexor digitorum superficialis nerve transfer to restore pronation: two case reports and anatomic study. J Hand Surg Am. 2001;26:1065–1072. doi: 10.1053/jhsu.2001.28427. [DOI] [PubMed] [Google Scholar]
- Tung TH, Novak CB, Mackinnon SE. Nerve transfers to the biceps and brachialis branches to improve elbow flexion strength after brachial plexus injuries. J Neurosurg. 2003;98:313–318. doi: 10.3171/jns.2003.98.2.0313. [DOI] [PubMed] [Google Scholar]
- Viterbo F, Trindade JC, Hoshino K, Mazzoni Neto A. Latero-terminal neurorrhaphy without removal of the epineural sheath. Experimental study in rats. Rev Paul Med. 1992;110:267–275. [PubMed] [Google Scholar]
- Wood MD, Mackinnon SE. Pathways regulating modality-specific axonal regeneration in peripheral nerve. Exp Neurol. 2015;265:171–175. doi: 10.1016/j.expneurol.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong G, Ling L, Nakamura R, Sugiura Y. Retrograde tracing and electrophysiological findings of collateral sprouting after end-to-side neurorrhaphy. Hand Surg. 2003;8:145–150. doi: 10.1142/s0218810403001637. [DOI] [PubMed] [Google Scholar]
- Yüksel F, Karacaoglu E, Güler MM. Nerve regeneration through side-to-side neurorrhaphy sites in a rat model: a new concept in peripheral nerve surgery. Plast Reconstr Surg. 1999;7:2092–2099. doi: 10.1097/00006534-199912000-00022. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Soucacos PN, Bo J, Beris AE. Evaluation of collateral sprouting after end-to-side nerve coaptation using a fluorescent double-labeling technique. Microsurgery. 1999;9:281–286. doi: 10.1002/(sici)1098-2752(1999)19:6<281::aid-micr5>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Johnson EO, Vekris MD, Zoubos AB, Bo J, Beris AE, Soucacos PN. Long-term evaluation of rabbit peripheral nerve repair with end-to-side neurorrhaphy in rabbits. Microsurgery. 2006;26:262–267. doi: 10.1002/micr.20237. [DOI] [PubMed] [Google Scholar]
- Zhu QT, Zhu JK, Chen GY. Location of collateral sprouting of donor nerve following end-to-side neurorrhaphy. Muscle Nerve. 2008;38:1506–1509. doi: 10.1002/mus.21116. [DOI] [PubMed] [Google Scholar]