Abstract
A previously diagnosed child of persistent hyperplastic primary vitreous (PHPV) with painless blind eye remained clinically silent for about 3 years follow-up. The child suddenly presented as a case of orbital cellulitis and panopthalmitis with meningitis. No definite mass lesion was detected on ultrasonography, magnetic resonance imaging (MRI) and positron emission tomography (PET) scan. Histopathology of the enucleated eye revealed intra-ocular medulloepithelioma as the culprit of sterile panophthalmitis and orbital inflammation.
Keywords: Medulloepithelioma, Intra-ocular, PHPV, Cellulitis, Panophthalmitis
Introduction
Atypical presentation of medulloepithelioma in the absence of definite mass lesion is a diagnostic challenge for ophthalmologists and radiologists. Herein, we report one such case of medulloepithelioma in a child with persistent hyperplastic primary vitreous (PHPV) and its rare late presentation as panophthalmitis and orbital cellulitis.1, 2
Case report
A 5-year-old boy presented with pain, swelling, redness and restriction of movements of right eye for 3 days (Fig.1a). About 3 years back, patient had been admitted with leukocoria and buphthalmos (raised intra-ocular pressure) in a non-seeing eye with vitreous hemorrhage and retinal detachment on ultrasonography. No mass lesion or evidence of calcification was reported on ultrasonography. VER of the right eye showed extinguished response. On examination under anesthesia, a retrolental membrane or stalk was present and there was vitreous hemorrhage. No mass lesion or retinal detachment was seen due to media haze. Still atypical retinoblastoma was kept as an important differential because of age of presentation. Previous orbital imaging (CT and MRI) had showed enlarged globe without any mass lesion, calcification or retinal detachment but the presence of a retrolental membrane or stalk like structure connected to optic nerve head, was suggestive of PHPV (Fig. 2). Since then the patient was on regular follow-up as a case of PHPV. During follow-up, the patient was asymptomatic except for a single episode of hyphema at about one year after the initial presentation. On repeat MRI, right globe appeared small in size compared to fellow eye. It was suggestive of intra-ocular hemorrhage and no mass lesion was seen. No intervention was done and the hyphema resolved over few days. Presently, on examination, there was no perception of light in the right eye and visual acuity in left eye was 6/9. The child had severe lid edema, erythema and tenderness along with chemosis and congestion of conjunctiva. There was no purulent discharge or any evidence of keratitis and corneal ulcer. Diffuse corneal haze and band shaped keratopathy were present and therefore anterior chamber details could not be made out. There was no fundal glow. Extraocular movements were grossly restricted in all quadrants. Patient also had complaint of headache with signs of meningeal irritation. Ultrasonography of right eye showed disorganized intraocular structure with no definite mass lesion. MRI imaging showed thickening and marked enhancement of ocular coats with preseptal, tenons and retrobulbar inflammation (Fig.1b). It did not show any intraocular mass lesion or orbital pus pocket. Right globe size was decreased compared to previous imaging and fellow eye. PET scan was normal and blood culture was sterile. On the basis of clinical and radiological features a diagnosis of aseptic orbital cellulitis and panophthalmitis secondary to undetected atypical intraocular malignancy with pre-existing PHPV was made. Paediatric neurology opinion was sought for signs of meningeal irritation which was labeled as non-specific and secondary to orbital inflammation. Patient was treated with oral steroid (1 mg/kg/day) under empirical intravenous and topical antibiotics cover. A favorable response was noted over next 3–4 days and intravenous antibiotics were discontinued. Broad spectrum oral antibiotic was started in place of intravenous antibiotics and oral steroid was tapered over next one week (Fig.1c). After 3 weeks, once acute episode subsided, enucleation with primary implantation of Mules implant was performed. Histopathological examination of the right eye enucleated specimen revealed a tumor arising anteriorly from ciliary body which was present in form of cords, tubules, ribbons and Flexner-Wintersteiner rosettes (Fig.1d). The cords were lined by pseudostratified neuroepithelium. In addition, calcification, decalcified bone and small islands of undifferentiated neuroblastic cells were also seen. The number of mitotic figures ranged from 2 to 5 per 10 hpf (high power field). Multiple sections revealed that the entire eyeball was filled with large areas of necrosis, cholesterol clefts, giant cells and chronic inflammatory infiltrates. Sclera and optic nerve were not involved by the tumor and there was no extra-ocular extension or invasion. Immunohistochemical (IHC) stain was positive for glial fibrillary acid protein (GFAP) (Fig.1e). A pathological diagnosis of intra-ocular non-teratoid medulloepithelioma of the right eye was made. Six weeks after enucleation, prosthetic eye was offered to the patient. As there was the presence of small islands of undifferentiated neuroblastic cells (one of the criteria suggestive of malignant nature of the tumor) on histopathology, the patient was given 6 cycles of vincristine and carboplatin. On 3 years follow-up, the patient had no recurrence of the tumor.
Fig. 1.
(a)–(e): (a) Clinical photograph at presentation shows right orbital cellulitis. (b) Axial T2 W imaging shows small disorganized right globe with no intraocular mass lesion or orbital pus pocket. Marked hyperintense MR signals in the ocular coats, retrobulbar area and periorbital soft-tissue along with its thickening suggestive of orbital cellulitis. (c) Inflammatory membrane in anterior chamber with conjunctival hyperemia after subsidence of cellulitis. (d) Microphotograph showing a medulloepithelioma arranged in the form of cords, tubules, ribbons and rosettes, arising from ciliary body (H&E stain, 400×). (e) IHC stain for GFAP was positive in the tumor cells (400×),
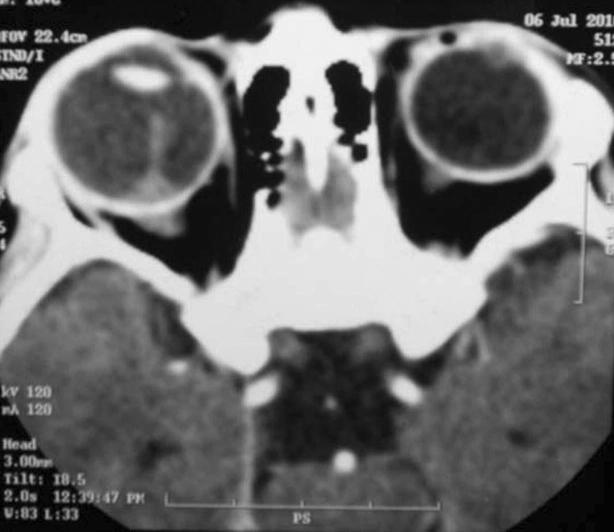
Fig. 2.
CECT (axial cut) done 3 years back show the presence of a retrolental stalk like structure connected to optic nerve head. No intra-ocular mass lesion or calcification was seen.
Discussion
Leukocoria, glaucoma, intra-ocular hemorrhage and retinal detachment in our case, all could be explained by PHPV in the absence of mass lesion, especially when retrolental membrane or stalk was visible.3 The presence of more than one unrelated pathology in the same eye is usually not expected unless there is evidence in favor of it or appearance of new features during follow-up which can be longer. Co-existence of PHPV and medulloepithelioma has been reported in 20% cases.1 Shields et al reported a similar case which clinically and radiologically appeared to be PHPV but there was no histopathological evidence of PHPV in enucleated specimen.4 Initial ‘Misdiagnosis’ and ‘delay in treatment’ are not uncommon with intra-ocular medulloepithelioma especially in the absence of classical features.5, 6 Reports on intra-ocular medulloepithelioma presented as orbital cellulitis or panophthalmitis are sparse. Although lid swelling was mentioned in few scattered cases in the literature, no case was documented as orbital cellulitis. Broughton WL et al reported two cases presented as panophthalmitis and endophthalmitis, while Zhao HS et al reported one case as endophthalmitis.1, 2 However, presentation of common pediatric intraocular tumor, i.e. retinoblastoma as aseptic inflammation is not uncommon and has been well documented.7 It has been hypothesized that the sterile inflammation is because of immune response to the necrotic material in the tumor. Beneficial role of systemic steroid is well established in such cases and one may repeat imaging after resolution of acute inflammation or can enucleate if there is no potential of vision in a disorganized globe.7, 8
Therefore we can conclude that child with PHPV and sterile orbital cellulitis or panopthalmitis in a blind disorganized eyeball in the absence of mass lesion on imaging, should be kept under high index of suspicion for tumor. Regular follow-up and early enucleation have key roles in preventing inadvertent adverse outcome.
Conflict of interest
The authors declared that there is no conflict of interest.
Patient consent
An informed consent was taken from legal guardian of the patient for publishing clinical photographs.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Broughton W.L., Zimmerman L.E. A clinicopathologic study of 56 cases of intraocular medulloepithelioma. Am J Ophthalmol. 1978;85:407–418. doi: 10.1016/s0002-9394(14)77739-6. [DOI] [PubMed] [Google Scholar]
- 2.Zhao H.S., Wei W.B. Dilemma in management of ocular medulloepithelioma in a child. Chin Med J (Engl) 2012;125(2):392–395. [PubMed] [Google Scholar]
- 3.Albert D.M., Miller J.W., Blodi B., Azar D. 3rd ed. Elsevier; London: 2008. Albert and Jakobiec’s Principles and Practice in Ophthalmology; pp. 2746–2747. [Google Scholar]
- 4.Shields J.A., Shields C.L., Schwartz R.L. Malignant teratoid medulloepithelioma of the ciliary body simulating persistent hyperplastic primary vitreous. Am J Ophthalmol. 1989;107(3):296–298. doi: 10.1016/0002-9394(89)90318-8. [DOI] [PubMed] [Google Scholar]
- 5.Earl J.B., Minckler D.S., Lee T.C., Murphree A.L. Malignant teratoid medulloepithelioma with retinoblastic and rhabdomyoblastic differentiation. J AAPOS. 2013;17(3):328–331. doi: 10.1016/j.jaapos.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Kaliki S., Shields C.L., Eagle R.C., Jr Ciliary body medulloepithelioma: analysis of 41 cases. Ophthalmology. 2013;120(12):2552–2559. doi: 10.1016/j.ophtha.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Walinjkar J., Krishnakumar S., Gopal L. Retinoblastoma presenting with orbital cellulitis. J AAPOS. 2013;17(3):282–286. doi: 10.1016/j.jaapos.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 8.Mullaney P.B., Karcioglu Z.A., Huaman A.M., al-Mesfer S. Retinoblastoma associated orbital cellulitis. Br J Ophthalmol. 1998;82(5):517–521. doi: 10.1136/bjo.82.5.517. [DOI] [PMC free article] [PubMed] [Google Scholar]