A 12-year-old boy presented with poor vision and abnormal eye movements in his both eyes since birth. There were no systemic complaints. The visual acuity was light perception only in both eyes. The cycloplegic refraction revealed a hypermetropia of 6 and 7 diopters in right and left eye respectively, but the correction did not improve his visual acuity. The child had pendular nystagmus; enophthalmos and oculo-digital sign were present. The pupil reacted sluggishly to light in both the eyes. A dilated fundus examination revealed bilateral optic disc pallor, pigment spicules all over the fundus and vascular attenuation. In addition the right eye (Fig. 1) showed well-defined excavated area of chorio-retinal atrophy in macula and sclerosed vessels with scattered retinal hemorrhages in the temporal fundus. The left eye showed thick glial tissue with exudation in macula (Fig. 2). An area of retinal vascular telangiectasias and subretinal exudation was noted inferiorly and temporally in left fundus. Electroretinography (ERG) showed extinguished scotopic and photopic responses. A diagnosis of Leber’s Congenital Amaurosis (LCA) with “Coats like” response was made. Patient was advised for regular follow-up.
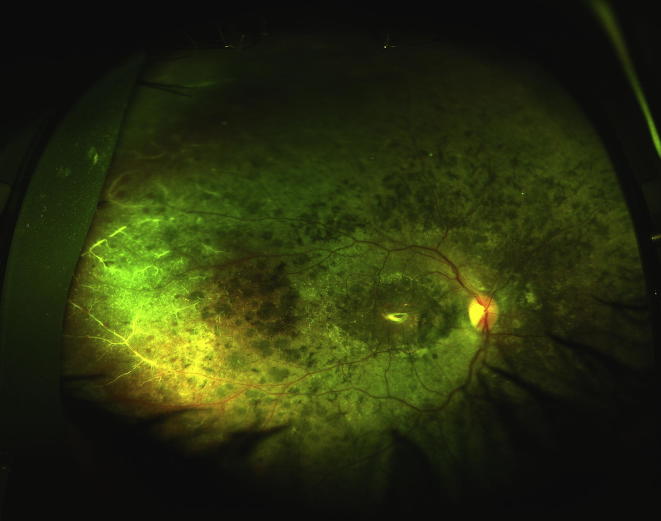
Figure 1.
Ultra wide field pseudo colour image of the right eye showing disc pallor, wide spread pigmentary changes, macular excavation and sclerosed vessels in temporal periphery.
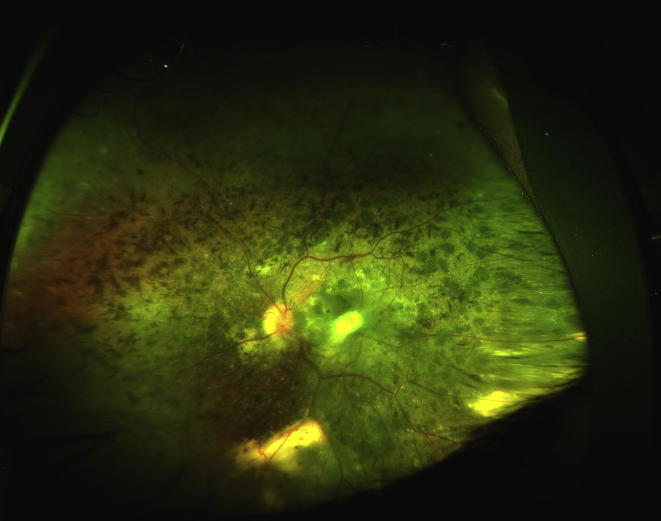
Figure 2.
Pseudo colour image of left eye showing disc pallor, pigmentary changes and fibro-glial nodule at macula. In addition subretinal and retinal exudations along with telangiectasia are seen in temporal and infero-temporal area.
Discussion
Leber’s congenital amaurosis is a severe hereditary retinal dystrophy that leads to blindness manifesting in infancy. It is believed to be a cause of childhood blindness in as many as 20% cases in blind institutes and accounts for 5% of all retinal dystrophies.1 It is mostly inherited as an autosomal recessive trait and to date around 19 genes have been implicated in the causation. Still, only around 70% or fewer cases are documented to have the detailed genetic defects.2
The fundus appearance in LCA can be extremely variable. Most cases initially present with a normal fundus appearance or with mild granularity and vascular attenuation, though in later life a number of changes have been described. Typical fundal changes include macular coloboma, typical retinitis pigmentosa, retinitis punctata albescens, optic atrophy, salt and pepper retinopathy, peripheral nummular pigmentation and vascular complications, such as optic disc oedema, retinal vasculitis, secondary angiomatosis and astrocytoma.
“Coats’ like response” is a clinical entity different from typical Coats disease and can be seen in a variety of clinical scenarios. It is typically described as a vascular alterations (telangiectasia and aneurysmal dilatation) with lipid exudation and has been documented with conditions such pars planitis,3 senile retinoschisis,4 pigmented paravenous retinochoroidal atrophy,5 linear en coup de sabre scleroderma6 and retinitis pigmentosa (RP).7, 8, 9 Coats’ like response is relatively common in RP associated with CRB1 mutation. Recently Hasan et al. described a case of LCA associated with CRBI gene mutation, which had coats’ like response. Their patient had lesser pigmentary changes, no macular coloboma and better visual acuity.10 A definitive common pathogenic mechanism has not been described for such a response. The clinical significance of such an observation arises from the fact that an exudative response like this may add to the visual disability of the pre-existing illness by extension of exudation to the posterior pole with ensuing macular oedema. In such a case, treating the Coats’ like response may help mitigate some visual disability.
In our case we found LCA to be associated with macular exudation and mid-peripheral telangiectasia associated with localized exudation. No intervention was performed and the patient was advised for regular follow-up as there were no recent complaints of decreased vision.
To our knowledge a “Coats’ like response” with LCA has never been documented before with the help of ultra-wide field (UWF) imaging and may well be another clinical feature in the already varied spectrum of fundus lesions associated LCA. UWF imaging is an useful tool as it provides panoramic images of retina in a single click despite poor fixation and cooperation from such patients.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Koenekoop R.K., Lopez I., den Hollander A.I., Allikmets R., Cremers F.P.M. Genetic testing for retinal dystrophies and dysfunctions: benefits, dilemmas and solutions. Clin Experiment Ophthalmol. 2007;35:473–485. doi: 10.1111/j.1442-9071.2007.01534.x. [DOI] [PubMed] [Google Scholar]
- 2.Den Hollander A.I., Roepman R., Koenekoop R.K., Cremers F.P.M. Leber congenital amaurosis: genes, proteins and disease mechanisms. Prog Retin Eye Res. 2008;27:391–419. doi: 10.1016/j.preteyeres.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Suh D.W., Pulido J.S., Jampol L.M., Chong L.P., Thomas M. Coats’-like response in pars planitis. Retina. 1999;19(79–8) doi: 10.1097/00006982-199901000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Gelisken F., Sherif Adel S., Inhoffen W., Bartz-Schmidt K.U. Coats’-like response in blood-filled senile retinoschisis. Ophthalmol J Int Ophtalmol Int J Ophthalmol. 2002;216:377–379. doi: 10.1159/000066181. [DOI] [PubMed] [Google Scholar]
- 5.Tandon M., Shukla D., Huda R., Ramasamy K. Pigmented paravenous chorioretinal atrophy with Coat’s like response. Indian J Ophthalmol. 2013;61:586–588. doi: 10.4103/0301-4738.121083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.George M.K., Bernardino C.R., Huang J.J. Coats-like response in linear en coup de sabre scleroderma. Retin Cases Brief Rep. 2011;5:275–278. doi: 10.1097/ICB.0b013e3181f66a04. [DOI] [PubMed] [Google Scholar]
- 7.Ghassemi F., Akbari-Kamrani M. Retinitis pigmentosa associated with vasoproliferative tumors and coats-like fundus. J Ophthalmic Vis Res. 2013;8:268–270. [PMC free article] [PubMed] [Google Scholar]
- 8.Kan E., Yilmaz T., Aydemir O., Güler M., Kurt J. Coats-like retinitis pigmentosa: reports of three cases. Clin Ophthalmol Auckl NZ. 2007;1:193–198. [PMC free article] [PubMed] [Google Scholar]
- 9.Khan J.A., Ide C.H., Strickland M.P. Coats’-type retinitis pigmentosa. Surv Ophthalmol. 1988;32(317–33):2. doi: 10.1016/0039-6257(88)90094-x. [DOI] [PubMed] [Google Scholar]
- 10.Hasan S.M., Azmeh A., Mostafa O., Megarbane A. Coat’s like vasculopathy in leber congenital amaurosis secondary to homozygous mutations in CRB1: a case report and discussion of the management options. BMC Res Notes. 2016;9:91. doi: 10.1186/s13104-016-1917-6. [DOI] [PMC free article] [PubMed] [Google Scholar]