Abstract
Background
Recent reports have shown an expansion of Lassa virus from the area where it was first isolated in Nigeria to other areas of West Africa. Two Ghanaian soldiers on a United Nations peacekeeping mission in Liberia were taken ill with viral haemorrhagic fever syndrome following the death of a sick colleague and were referred to a military hospital in Accra, Ghana, in May 2013. Blood samples from the soldiers and five asymptomatic close contacts were subjected to laboratory investigations.
Objective
We report the results of these investigations to highlight the importance of molecular diagnostic applications and the need for heightened awareness about Lassa fever in West Africa.
Methods
We used molecular assays on sera from the two patients to identify the causative organism. Upon detection of positive signals for Lassa virus ribonucleic material by two different polymerase chain reaction assays, sequencing and phylogenetic analyses were performed.
Results
The presence of Lassa virus in the soldiers’ blood samples was shown by L-gene segment homology to be the Macenta and las803792 strains previously isolated in Liberia, with close relationships then confirmed by phylogenetic tree construction. The five asymptomatic close contacts were negative for Lassa virus.
Conclusions
The Lassa virus strains identified in the two Ghanaian soldiers had molecular epidemiological links to strains from Liberia. Lassa virus was probably responsible for the outbreak of viral haemorrhagic fever in the military camp. These data confirm Lassa fever endemicity in West Africa.
Introduction
Lassa virus is a single-stranded RNA virus and a member of the Arenaviridae family and the genus Arenavirus. The virus is the aetiologic agent of Lassa fever, which is an acute and often fatal illness, endemic in portions of West Africa.1 There are an estimated 300 000 to 500 000 cases of Lassa fever each year,2 with a reported mortality rate of 15% – 20% for hospitalised patients. Rodents of the genus Mastomys are the reservoir for the virus, which is transmitted through direct contact with materials contaminated with urine and/or droppings of infected rodents. Human-to-human transmission of the virus may give rise to nosocomial or community-based outbreaks. Subsequent to its first isolation in Lassa, Nigeria and its restricted endemicity to two geographical regions in West Africa, recent reports have shown expanded areas of spread.3,4 The upturn in global travel activities and international commitments in conflict and disaster situations have made the import of Lassa fever and other viral haemorrhagic fevers (VHFs) into non-endemic countries a more likely event than in the past, which has been well documented.5,6,7,8 Presently, an epidemic of another VHF, Ebola virus disease, has spread throughout Guinea and beyond its borders. As of December 6, 2014, a total of 17 895 Ebola virus cases, including 6394 deaths, had been reported in six West African countries (Guinea, Liberia, Sierra Leone, Nigeria, Senegal and Mali) and the Democratic Republic of the Congo.9
The use of molecular diagnostic tools has resulted in highly sensitive and specific tests for infectious organisms and genetic diseases. These tools, which include polymerase chain reaction (PCR) and molecular sequencing, have come in handy for the rapid identification of Lassa virus and other VHF agents from suspected cases.
In May 2013, an outbreak of acute febrile illness affecting three military personnel occurred in the Ghanaian United Nations Mission in Liberia military contingent in Zorzor, Liberia. Of the three cases, two were evacuated to a military hospital in Ghana, where molecular diagnostic methods were used to determine the causative agent. Two of the three cases were fatal.
Research method and design
Ethical considerations
Verbal consent was sought from the close relatives of the patients. The officers were also spoken to personally by the medical team at the 37 Military Hospital.
Setting and patients
The index case was a male soldier with severe symptoms of malaria who died on May 11, after admission to a Level II hospital for about a week. Two male colleagues, aged 27 years (Patient 1) and 33 years (Patient 2), who were living in the same camp, subsequently developed severe fever and myalgia on May 15 (Patient 1) and 21 (Patient 2). Their medical conditions deteriorated, necessitating their medical evacuation to the 37 Military Hospital, a Level IV facility, in Accra, Ghana, on May 26, 2013 after five days of illness for Patient 1 and 11 days for Patient 2. Patient 1 died two days after admission. At the military hospital in Accra, the medical staff ruled out malaria through microscopic examination of thick and thin blood smears and focused on the clinical manifestations, which were classified as VHF. A presumptive clinical diagnosis of Lassa fever was made on the strength of previous outbreaks of Lassa fever in Liberia.10 To investigate these clinical suspicions, blood samples from the patients and five asymptomatic close contacts were analysed.
Laboratory investigations
Five millilitres of blood were collected from each of the two patients (Patient 1 sample number: 60FSD_28052013; Patient 2 sample number: 59_PN_28052013) and five asymptomatic contacts (medical staff who had initially attended the two patients without barrier nursing). The samples were transported to the Virology Department of the Noguchi Memorial Institute for Medical Research at the University of Ghana in Legon, Ghana. The blood samples were processed into serum by low-speed centrifugation at 4 °C and the resultant 3 mL aliquots of sera were cryopreserved at -80 °C.
Real-time reverse transcription-PCR Pan Filoviridae assay for Marburg and Ebola
Viral RNA was extracted from 140 µL of the blood samples using the QIAamp viral RNA mini kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. A diagnostic assay developed by Panning et al.,11 for filovirus species and carried out with a OneStep RT-PCR reaction kit (Qiagen, Hilden, Germany) was used in a 25 µL total reaction volume, including 3 µL of the extracted RNA. The real-time diagnostic assay used five optimised large (L)-gene primers and three probes, as well as an internal control with a separate detection probe. Reactions were supplemented with 40 ng/mL bovine serum albumin and 400 mmol/L each dNTP. The primers and probes used were designed and published by Panning et al.11 (Table 1). All probes were synthesized by Tib-Molbiol (Berlin, Germany). Amplification in a 96-well ABI 7300 Real Time PCR System (Life Technology Holdings, Singapore) involved the following steps: 50 °C for 30 minutes; 95 °C for 15 minutes; and 45 cycles of denaturation at 95 °C for 15 seconds, annealing at 52 °C for 25 seconds and extension at 72 °C for 20 seconds. Fluorescence was measured at the end of each 52 °C annealing step.
TABLE 1.
Reverse transcription-PCR test assays used in the laboratory investigations, Ghana, 2013.
| Virus | Reagents; Primers and probes (sequence 5′ – 3′) | Target region | Reference |
|---|---|---|---|
| Filo† | OneStep RT-PCR kit (Qiagen); FiloA2.4, AAG CAT TTC CTA GCA ATA TGA TG-GT (200 nmol/L); FiloA2.2, AAG CCT TTC CTA GCA ACA TGA TGG T (200 nmol/L); FiloA2.3, AAG CAT TCC CTA GCA ACA TGA TGG T (200 nmol/L); FiloB, ATG TGG TGG GTT ATA ATA ATC ACT GAC ATG (300 nmol/L); FiloB-RAVN, GTG AGG AGG GCT ATA AAA GTC ACT GAC ATG (300 nmol/L); EBO Sud, FAM-CCG AAA TCA TCA CTI GTI TGG TGC CA-Black Hole Quencher 1 (BHQ1) (66.7 nmol/L); EBOg, FAM-CCA AAA TCA TCA CTI GTG TGG TGC-BHQ1 (66.7 nmol/L); Fam MBG, FAM-CCT ATG CTT GCT GAA TTG TGG TGC CA-BHQ1 (66.7 nmol/L) |
L-gene | 11 |
| Lassa | OneStep RT-PCR kit (Qiagen); 36E2, ACC GGG GAT CCT AGG CAT TT (10 μM); LVS-339-rev, GTT CTT TGT GCA GGA MAG GGG CAT KGT CAT (10 μM) |
S/GPC gene | 13 |
| Lassa | AgPath-ID One-Step RT-PCR kit (Ambion); LVL 3359D_Y+, AGA ATC AGT GAA AGG GAA AGC AAY TC (10 μM); LVL 3359G_Y+, AGA ATT AGT GAA AGG GAG AGT AAY TC (10 μM); LVL 3754A_R-, CAC ATC ATT GGT CCC CAT TTA CTA TGR TC (10 μM); LVL 3754D_R-, CAC ATC ATT GGT CCC CAT TTA CTG TGR TC (10 μM) |
L-gene | 18 |
| Lassa | Power SYBR® Green RNA-to-CT™ 1-Step Kit (Life Technologies); 36E2, ACC GGG GAT CCT AGG CAT TT (10 μM); LVS-339-rev, GTT CTT TGT GCA GGA MAG GGG CAT KGT CAT (10 μM) |
S/GPC gene | 13 |
Source: Various
Filoviruses including Ebola and Marburg virus.
Gel-based Pan Flaviviridae assay for Yellow fever and Dengue fever
An endpoint reverse transcription (RT)-PCR protocol for the detection and identification of flaviviruses, developed by Pierre, Drouet and Deubel in 199412 with a set of universal oligonucleotide primers, was used for laboratory investigation of flaviviruses present in the serum samples. These primers correspond to the 3’ non-coding region of the NS5 gene, which is highly conserved amongst the mosquito-borne flaviviruses. The OneStep RT-PCR kit (Qiagen, Hilden, Germany) was used with the following cycling conditions: reverse transcription at 50 °C for 30 minutes; initial activation step at 95 °C for 15 minutes; 45 cycles in a 3-step cycling of 95 °C for 30 seconds, 52 °C for 30 seconds and 72 °C for 30 seconds, with a cooling step of 30 seconds at 30 °C.
Gel-based Lassa fever S-gene segment assay
A gel-based conventional RT-PCR assay was performed using ABI 2720 Thermal Cycler (Life Technology Holdings, Singapore) for the detection of Lassa virus with primers specific for regions of the S RNA segment. The RT-PCR (45 cycles) contained OneStep RT-PCR kit reagents (Qiagen, Hilden, Germany) with the sense primer 36E2 and the antisense primer LVS-339-rev, as described by Ölschläger et al.13 (Table 1). Cycling conditions for the RT-PCR involved the following steps: 50 °C for 30 minutes; 95 °C for 15 minutes; and 45 cycles of 95 °C for 15 seconds, 52 °C for 30 seconds and 72 °C for 30 seconds. The amplification products (expected size: 320 bp) were electrophoresed on a 2% agarose gel (peqlab Biotechnologie, Erlangen, Germany), stained with ethidium bromide and viewed under a Kodak Gel Logic 100 Imaging System (Cole-Parmer Int., Chicago, Illinois, United States).
Lassa virus L-gene segment amplification by RT-PCR
An RT-PCR assay specific to the L-gene segment of the Lassa arenavirus on the RNA extracted from the processed blood samples. The 45 cycle RT-PCR used a AgPath-ID One-Step RT-PCR kit (Ambion, Life Technologies, Thermo Fisher Scientific, New York, New York, United States) with the primers as described by Vieth et al.14 (Table 1). The reaction solution consisted of: 2.5 μL nuclease-free H2O, 12 μL 2X RT-PCR buffer, 2 μL of the upstream and downstream primers (10 μM each), 1.5 μL 2X RT-PCR buffer enzyme mix and 5 µL DNA. Nucleic acid amplification started with a 30 minute RT step at 50 °C, then an initial denaturation step of 2 minutes at 95 °C and a 45-cycle amplification of 20 seconds at 98 °C, 30 seconds at 55 °C and 60 seconds at 72 °C. A gel was used to separate the products of the nucleic acid amplification. Images of the DNA bands were captured using a Gel Logic 100 imaging system (Eastman Kodak Company, Rochester, New York, United States). The DNA bands of nearly 400 bp in size were analysed and purified for sequencing.
Real-time RT-PCR assay for Lassa fever
A real-time RT-PCR assay was performed using the ABI 7300/7500 Real Time PCR System (Life Technology Holdings, Singapore) for the detection of Lassa virus with primers specific for regions of the small (S) RNA gene segment. The reagent used in the preparation of the master mix for the 45-cycle RT-PCR was the Power SYBR® Green RNA-to-CT™ 1-Step Kit (Life Technologies, Carlsbad, California, United States) with the sense primer 36E2 and the antisense primer LVS-339-rev, as described in detail by Ölschläger et al.13 (Table 1). The amplification protocol was as follows: 48 °C for 30 minutes; 95 °C for 10 minutes; and 45 cycles of 95 °C for 15 seconds, 60 °C for 1 minute. At the end of each cycle, fluorescence was measured at 60 °C.
Sequencing and phylogenetic analysis
The PCR products generated in the conventional RT-PCRs from the L-gene segment fragments were purified in accordance with the manufacturer’s instructions using a commercial kit (Big Dye XTerminator Purification Kit, Applied Biosystems, Carlsbad, California, United States). The purified products were sequenced on both strands using the L-gene PCR primers and an ABI Prism 3130 genetic analyser (Hitachi High Technology, Singapore). The sequences were assembled with Lasergene software (DNASTAR, Thermo Fisher Scientific, New York, New York, United States) and automated base calling was proofread by visual inspection of the electropherograms. Other published Lassa virus sequences were obtained from the National Center for Biotechnology Information’s15,16 GenBank (Table 2) to align with the generated sequences for phylogenetic analysis. With the use of the National Library of Medicine’s Basic Local Alignment Search Tool17 (BLAST) program, we compared the patients’ Lassa virus sequences with other reference Lassa virus sequences to locate regions that were similar. All sequences obtained were copied into BioEdit software (North Carolina State University, Raleigh, North Carolina, United States) and put together into an ideal sequence alignment file with the use of a multiple sequence alignment tool, ClustalW18 (version 2; EMBL-EBI, Cambridge, United Kingdom). We then used Molecular Evolutionary Genetics Analysis (MEGA) software (version 5.05) in a Kimura two-parameter model19 to infer a phylogenetic tree from the aligned nucleotide sequences following a neighbour-joining method. To establish reliability and to infer the strength of similarity between the patient’s sequence and the referenced sequences from the phylogenetic tree, a bootstrap analysis of 1000 replicates was used.
TABLE 2.
Lassa fever viral strains used for homology and phylogenetic analysis of Ghana case strains, 2013.
| Strain | Year submitted to GenBank | Location | Accession number |
|---|---|---|---|
| Las803792 | 2004 | Liberia | AY693638 |
| SL06-2057 | 2010 | Sierra Leone | GU979507 |
| Josiah | 2011 | Sierra Leone | JN650518 |
| Recom_Josiah | 2010 | Sierra Leone | HQ688675 |
| SL620 | 2003 | Nigeria | AY363905 |
| BA366 | 2010 | Guinea | GU979513 |
| CSF | 2002 | Nigeria | AY179174 |
| Nig04-010 | 2004 | Nigeria | AY693637 |
| AN21366 | 2003 | Germany | AY363904 |
| Nig08-A47 | 2010 | Nigeria | GU481079 |
| SL15 | 2003 | Germany | AY363906 |
| Soromba R | 2010 | Mali | GU573542 |
| AV | 2004 | Cote d’Ivoire | AF246121 |
| Nig11-205 | 2011 | Nigeria | JN651400 |
| BA377 | 2010 | Guinea | GU830840 |
| PB1 | 2005 | Nigeria | AJ969405 |
| Macenta | 2004 | Guinea | AY628200 |
| LP | 1996 | Lassa, Nigeria | U80004 |
Results
Detection and characterisation of nucleic acid in clinical specimens
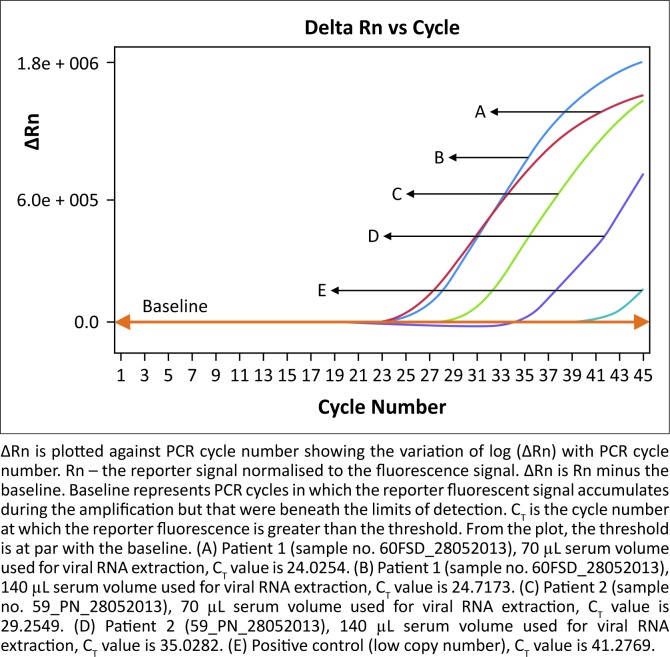
The gel-based RT-PCR flavivirus tests for Yellow fever and Dengue fever (types 1–4), as well as the real-time RT-PCR filovirus test for Marburg and Ebola, were negative (Table 3). However, the RT-PCR amplification of the S-gene segment of arenaviruses detected a 320 bp DNA band in the well with the patients’ clinical specimens. The length and position of these bands were on a par with the positive Lassa virus control (an inactivated culture supernatant of cells infected with Lassa virus strain CSF); no band was observed in the negative control (PCR-grade water) well. The real-time RT-PCR amplification of the S-gene segment of the arenavirus test produced a clear peak with a sigmoid-shaped curve for the patient’s samples, whereas no peak was observed for the negative control, which in the figure is covered by the threshold line, or baseline (Figure 1). This two-result signal indicated the presence of Lassa virus in the patients’ sera. The samples from the five asymptomatic close contacts were tested in the same assay run and no indication of the presence of Lassa virus was observed (data not shown).
TABLE 3.
Summary of suspected patient information and their test results, Ghana, 2013.
| Parameter | Patients | |
|---|---|---|
| Sample number | 59_PN_28052013 | 60FSD_28052013 |
| Gender | Male | Male |
| Age | 33 | 27 |
| Date of sample collection | May 26, 2013 | May 26, 2013 |
| Gel-based Pan Filoviridae (Marburg and Ebola) | Negative | Negative |
| Gel-based Pan Flaviviridae (Yellow fever and Dengue) | Negative | Negative |
| Gel-based Arenaviridae (L-gene segment) | Positive | Positive |
| Gel-based Lassa fever (S-gene segment) | Positive | Positive |
| Real-time Lassa fever | Positive | Positive |
FIGURE 1.
Real-time PCR amplification of patient sera and controls.
Lassa virus L-gene segment sequencing and homology analysis
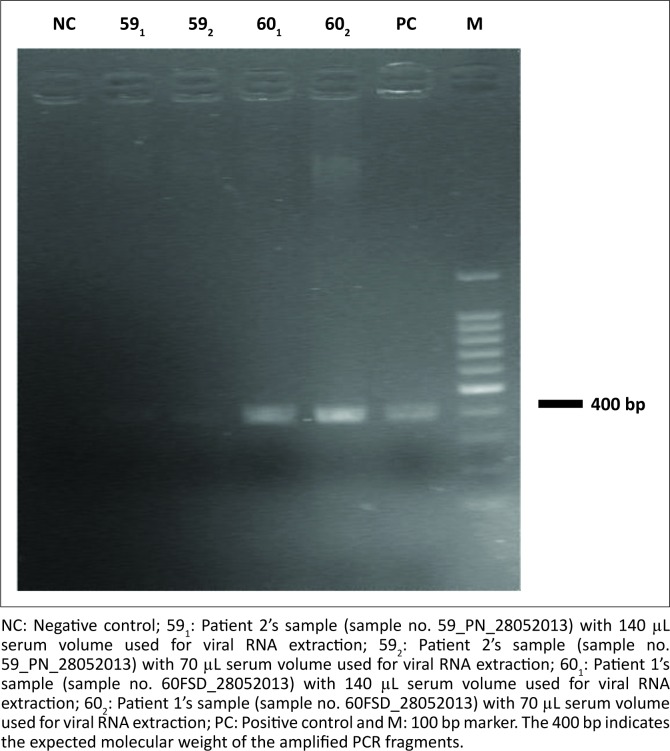
The gel-based RT-PCR amplification assay for the large L-gene segment of the arenavirus showed ~400 bp products that matched the expected size (Figure 2). The comparison of the nucleotide sequences from the amplified products with the GenBank database showed that the patients’ sequences had high similarities to known Lassa virus strains. Genetically, the sequences were close to strains that had originated in Guinea and been reported in Liberia. The highest similarity (85% maximum identity in nucleotides) was to Lassa virus strain Macenta20 and Lassa virus strain las803792.14
FIGURE 2.
Ethidium bromide-stained 2% agarose gel image of the PCR products generated from the two patients samples run in duplicate.
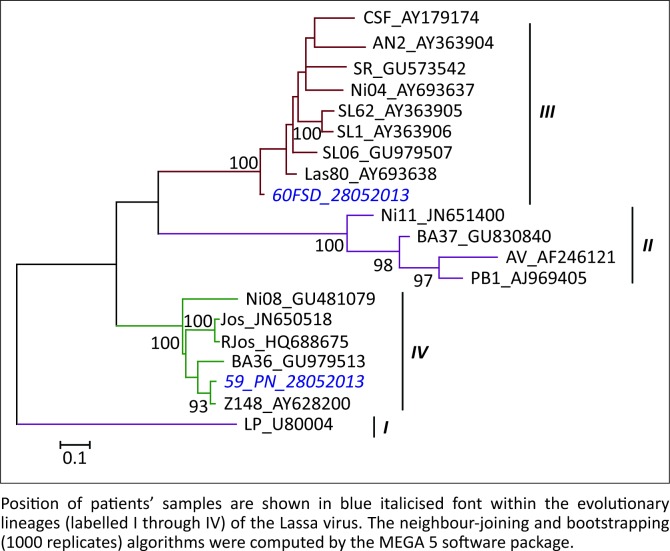
Phylogenetic tree analysis
The phylogenetic analysis with GenBank data revealed that the nucleotide sequences from the patients had close phylogenetic relationships with the reported Lassa virus strains Macenta20 (GenBank accession number: AY628200) and las80379214 (GenBank accession number: AY693638) (Figure 3). The sequence data from the patient who died (Patient 1, sample no. 60FSD_28052013) was sent to GenBank and assigned accession number KF425246.
FIGURE 3.
Phylogenetic relationship between the nucleotide sequences of reported Lassa virus strains and that of the two patients.
Discussion
We identified the aetiological agent responsible for suspected cases of VHF imported into Ghana. The patients were soldiers with the Ghanaian United Nations Mission in Liberia military contingent in Zorzor, Liberia, who had had close contact earlier with another soldier suspected of dying from VHF. These patients were medically evacuated, with deteriorating health conditions, to a Level IV military hospital in Ghana, where viral nucleic acid was detected and characterised from the patients’ blood specimens. The characteristic arenavirus signal indicated on both the gel-based and real time RT-PCRs was confirmed as Lassa virus by capillary DNA sequencing.
These results confirmed Lassa virus as the aetiological agent that caused the outbreak in Liberia, where Lassa fever is known to be endemic.21 It has been documented that Lassa fever seems to have two geographically-separate endemic areas: the Mano River region in the west (Guinea, Sierra Leone and Liberia) and Nigeria in the east.22 Moreover, literature indicates that, since the initial discovery of Lassa fever in Nigeria in 1969, nosocomial outbreaks have occurred repeatedly in three localities, specifically Zorzor, Phebe and Ganta in Liberia.23
Molecular analyses of patients’ samples from the outbreak we report are indicative of clues regarding the source of the aetiological agent. The nucleotide sequences from the samples aligned closely with the Lassa fever strain isolated in Guinea in 200424 and also reported subsequently in Liberia.21 The 85% proportion of alignment between GenBank-reported strains and sequences from the patients’ sera suggests a link between the source of the patients’ Lassa virus infection and the district of Zorzor in Liberia from which they were evacuated. In addition, this finding supports the assertion that persons participating in humanitarian missions or peacekeeping activities in the regions comprising Sierra Leone and Liberia are at risk for Lassa fever.23,24,25
Phylogenetic analysis of our patients’ sequences with GenBank-reported Lassa virus strains yielded a single parsimonious tree rooted with the prototype LP strain of Lassa virus. Our results indicate that our patients’ samples had close genetic relationships to the Macenta20 and las80379214 strains of Lassa virus, both of which were reported in Liberia but isolated in Guinea in 2004. The sequence data from the patient who died (Patient 1; sample no. 60FSD_28052013) had close homology with reported Lassa strain las803792, which was isolated from a fatal case in 2004.14 This observation is consistent with a study that suggested that Lassa virus strains differ in virulence potential.1
Limitations
Our report was limited by our inability to conduct a battery of tests, including serological assays, for either an ideal suspected case(s) of VHF or for the five asymptomatic close contacts of the evacuated patients. That notwithstanding, this report underscores the importance of preventive measures for all visitors and workers including peacekeeping forces to endemic regions in West Africa. This is because there is currently no effective Lassa fever vaccine is available.
Recommendations
It is recommended that medical support plans for peacekeeping operations should be built purposefully and in consideration of existing endemicity and history of endemicity in the host nations. Such support plans should be duly informed by frequently-updated research on endemic agents and other health concerns in the visiting country. Sensitisation of officers and other travellers to infectious agents in the host country and the importance of speedy reporting to health facilities when unwell should be given sufficient emphasis. This report of laboratory investigations of imported cases of Lassa fever and other documented medical fatalities on past peacekeeping operations supports the need for essential medical organisational changes in future operations. This would involve a good balance of proximity to medical care and transportation time for medical emergencies.
Conclusion
In conclusion, it is envisaged that the importation of VHFs into non-endemic countries will increase in likelihood as a result of increased travel and international commitments in conflict and disaster situations to VHF-endemic countries in West Africa. Thus, healthcare providers should: (1) have a high index (low threshold) of suspicion for VHF amongst travellers returning from endemic areas; (2) promptly implement appropriate infection prevention and control measures; and (3) rapidly report suspected cases to avert undue nosocomial transmission.
Acknowledgements
We are most grateful to the medical and para-medical staff of the Public Health Department of the 37 Military Hospital and the staff of Virology Department of the Noguchi Memorial Institute for Medical Research, College of Health Sciences, University of Ghana, Legon, particularly acknowledging the technical support by Juliana Naa Dedei Aryeequaye.
Competing interests
The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Sources of support
This work was supported by the Noguchi Memorial Institute for Medical Research, University of Ghana, Legon.
Authors’ contributions
J.H.K.B. performed the laboratory testing, analysed and interpreted the results and wrote the manuscript. E.O.N. coordinated sample collection and surveillance and edited the manuscript. S.-A.O. coordinated surveillance and edited the manuscript. J.A. supervised surveillance and edited the manuscript. R.K.A. was involved in surveillance and sample collection. S.C.N.-P. participated in sample testing and analysis and edited the manuscript. B.S. took part in the surveillance and edited the manuscript. P.A. participated in sample collection and surveillance. M.A. edited the manuscript and was involved in surveillance. N.N.A.K. was involved in surveillance and sample collection. S.B.-N. was involved in surveillance and edited the manuscript. W.K.A. supervised the design and implementation of the work and edited the manuscript.
Footnotes
How to cite this article: Bonney JHK, Nyarko EO, Ohene S-A, et al. Molecular confirmation of Lassa fever imported into Ghana. Afr J Lab Med. 2016;5(1), a288. http://dx.doi.org/10.4102/ajlm.v5i1.288
References
- 1.Günther S, Lenz O. Lassa virus. Crit Rev Clin Lab Sci. 2004; 41(4):339–390. http://dx.doi.org/10.1080/10408360490497456 [DOI] [PubMed] [Google Scholar]
- 2.McCormick JB. Epidemiology and control of Lassa fever. Curr Top Microbiol Immunol. 1987;134:69–78. http://dx.doi.org/10.1007/978-3-642-71726-0_3 [DOI] [PubMed] [Google Scholar]
- 3.Sogoba N, Feldmann H, Safronetz D. Lassa fever in West Africa: evidence for an expanded region of endemicity. Zoonoses Public Health. 2012;59(Suppl 2):43–47. http://dx.doi.org/10.1111/j.1863-2378.2012.01469.x [DOI] [PubMed] [Google Scholar]
- 4.Dzotsi EK, Ohene SA, Asiedu-Bekoe F, et al. The first cases of Lassa fever infection in Ghana. Ghana Med J. 2012;46(3):166–170. [PMC free article] [PubMed] [Google Scholar]
- 5.Unit for Surveillance and Communication, Unit for Preparedness and Response, Editorial team Case of Lassa fever imported into Germany from Sierra Leone. Euro Surveill. 24 July 2006;11(30):pii=3008. [PubMed] [Google Scholar]
- 6.Günther S, Emmerich P, Laue T, et al. Imported Lassa fever in Germany: molecular characterization of a new Lassa virus strain. Emerg Infect Dis. 2000;6(5):466–476. http://dx.doi.org/10.3201/eid0605.000504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Günther S, Weisner B, Roth A, et al. Lassa fever encephalopathy: Lassa virus in cerebrospinal fluid but not in serum. J Infect Dis. 2001;184(3):345–349. http://dx.doi.org/10.1086/322033 [DOI] [PubMed] [Google Scholar]
- 8.Schmitz H, Köhler B, Laue T, et al. Monitoring of clinical and laboratory data in two cases of imported Lassa fever. Microbes Infect. 2002;4(1):43–50. http://dx.doi.org/10.1016/S1286-4579(01)01508-8 [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization Ebola virus disease, West Africa – update [page on the Internet]. c2014 [cited 2014 Dec 06]. Available from: http://who.int/csr/don/2014_05_15_ebola/en/
- 10.Frame JD, Jahrling PB, Yalley-Ogunro JE, et al. Endemic Lassa fever in Liberia. II. Serological and virological findings in hospital patients. Trans R Soc Trop Med Hyg. 1984;78(5):656–660. http://dx.doi.org/10.1016/0035-9203(84)90232-3 [DOI] [PubMed] [Google Scholar]
- 11.Panning M, Laue T, Ölschlager S, et al. Diagnostic reverse-transcription polymerase chain reaction kit for filoviruses based on the strain collections of all European biosafety level 4 laboratories. J Infect Dis. 2007;196(Suppl 2):S199–204. http://dx.doi.org/10.1086/520600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pierre V, Drouet MT, Deubel V. Identification of mosquito-borne flavivirus sequences using universal primers and reverse transcription/polymerase chain reaction. Res Virol. 1994;145(2):93–104. http://dx.doi.org/10.1016/S0923-2516(07)80011-2 [DOI] [PubMed] [Google Scholar]
- 13.Ölschläger S, Lelke M, Emmerich P, et al. Improved detection of Lassa virus by reverse transcription-PCR targeting the 5’ region of S RNA. J Clin Microbiol. 2010;48(6):2009–2013. http://dx.doi.org/10.1128/JCM.02351-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vieth S, Drosten C, Lenz O, et al. RT-PCR assay for detection of Lassa virus and related Old World arenaviruses targeting the L gene. Trans R Soc Trop Med Hyg. 2007; 101(12):1253–1264. http://dx.doi.org/10.1016/j.trstmh.2005.03.018 [DOI] [PubMed] [Google Scholar]
- 15.Sayers EW, Barrett T, Benson DA, et al. Database resources of the National Center for Biotechnology Information. Nucleic Acids Res. 2009;40(Database issue):D13–D25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benson DA, Karsch-Mizrachi I, Clark K, et al. GenBank. Nucleic Acids Res. 2009;40(Database issue):D48–D53. http://dx.doi.org/10.1093/nar/gkn723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Altschul SF, Gish W, Miller W, et al. Basic local alignment search tool. J Mol Biol. 1990;215(3):403–410. http://dx.doi.org/10.1016/S0022-2836(05)80360-2 [DOI] [PubMed] [Google Scholar]
- 18.Larkin MA, Blackshields G, Brown NP, et al. ClustalW and ClustalX version 2. Bioinformatics. 2007;23(21):2947–2948. http://dx.doi.org/10.1093/bioinformatics/btm404 [DOI] [PubMed] [Google Scholar]
- 19.Tamura K, Peterson D, Peterson N, et al. MEGA5: Molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol. 2011;28(10):2731–2739. http://dx.doi.org/10.1093/molbev/msr121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hajjaj A, Chain PSG, Do LH, et al. Lassa virus strain Macenta segment L, complete sequence. Accession number: AY628200; 2004.
- 21.Jahrling PB, Frame JD, Smith SB, et al. Endemic Lassa fever in Liberia. III. Characterization of Lassa virus isolates. Trans R Soc Trop Med Hyg. 1985;79(3):374–379. http://dx.doi.org/10.1016/0035-9203(85)90386-4 [DOI] [PubMed] [Google Scholar]
- 22.Fichet-Calvet E, Rogers DJ. Risk maps of Lassa fever in West Africa. PLoS Negl Trop Dis. 2009;3(3):e388 http://dx.doi.org/10.1371/journal.pntd.0000388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ter Meulen J, Koulemou K, Wittekindt T, et al. Detection of Lassa virus antinucleoprotein immunoglobulin G (IgG) and IgM antibodies by a simple recombinant immunoblot assay for field use. J Clin Microbiol. 1998;36(11):3143–3148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fair J, Jentes E, Inapogui A, et al. Lassa virus-infected rodents in refugee camps in Guinea: a looming threat to public health in a politically unstable region. Vector Borne Zoonotic Dis. 2007;7(2):167–171. http://dx.doi.org/10.1089/vbz.2006.0581 [DOI] [PubMed] [Google Scholar]
- 25.Khan SH, Goba A, Chu M, et al. New opportunities for field research on the pathogenesis and treatment of Lassa fever. Antiviral Res. 2008;78(1):103–115. http://dx.doi.org/10.1016/j.antiviral.2007.11.003 [DOI] [PubMed] [Google Scholar]