Abstract
Arrhythmogenesis in acute myocardial infarction (MI) is associated with depolarization of resting membraine potential (RMP) and decrease of inward rectifier potassium current (IK1) in cardiomyocytes. However, clinical anti-arrhythmic agents that primarily act on RMP by enhancing the IK1 channel are not currently available. We hypothesized that zacopride, a selective and moderate agonist of the IK1/Kir2.1 channels, prevents and cures acute ischemic arrhythmias. To test this viewpoint, adult Sprague-Dawley (SD) rats were subjected to MI by ligating the left main coronary artery. The antiarrhythmic effects of zacopride (i.v. infusion) were observed in the settings of pre-treatment (zacopride given 3 min prior to coronary occlusion), post-treatment (zacopride given 3 min after coronary occlusion) and therapeutic treatment (zacopride given 30 s after the onset of the first sustained ventricular tachycardia (VT)/ventricular fibrillation (VF) post MI). In all the three treatment modes, zacopride (15 μg/kg) inhibited MI-induced ventricular tachyarrhythmias, as shown by significant decreases in the premature ventricular contraction (PVC) and the duration and incidence of VT or VF. In Langendorff perfused rat hearts, the antiarrhythmic effect of 1 μmol/L zacopride were reversed by 1 μmol/L BaCl2, a blocker of IK1 channel. Patch clamp results in freshly isolated rat ventricular myocytes indicated that zacopride activated the IK1 channel and thereby reversed hypoxia-induced RMP depolarization and action potential duration (APD) prolongation. In addition, zacopride (1 μmol/L) suppressed hypoxia- or isoproterenol- induced delayed afterdepolarizations (DADs). In Kir2.x transfected Chinese hamster ovary (CHO) cells, zacopride activated the Kir2.1 homomeric channel but not the Kir2.2 or Kir2.3 channels. These results support our hypothesis that moderately enhancing IK1/Kir2.1 currents as by zacopride rescues ischemia- and hypoxia- induced RMP depolarization, and thereby prevents and cures acute ischemic arrhythmias. This study brings a new viewpoint to antiarrhythmic theories and provides a promising target for the treatment of acute ischemic arrhythmias.
Introduction
In the past three decades, elucidation of the structure and function of cardiac ion channels has contributed to our understanding of electrophysiological changes, arrhythmogenesis and the treatment of arrhythmias in cardiac diseases, including myocardial infarction (MI). Current clinical antiarrhythmic drugs primarily act on Na+, K+ and Ca2+ channels, and most of them are channel blockers. When producing therapeutic advantage against arrhythmias, these channel blockers may lead to unwanted electrophysiological abnormalities and proarrhythmic risks. Therefore, it is necessary to develop new antiarrhythmic agents based on new antiarrhythmic theory/mechanism. Cardiac inward rectifier potassium (Kir) channels constitute the IK1 channels which are present in all ventricular and atrial myocytes and are important for stabilizing the resting membrane potential (RMP). IK1 channels establish the excitation threshold and modulate the final repolarization phase of the action potential (AP) in cardiomyocytes, [1, 2] and thus exert profound effects on cardiac excitability and arrhythmogenesis.
Acute cardiac ischemia in coronary heart disease is a leading cause of sudden death primarily due to lethal arrhythmias, including ventricular tachycardia (VT), ventricular fibrillation (VF) and cardiac arrest [3]. In case of ischemia, diastolic potential decline [4–6] and catecholamine secretion [7–9] are two critical factors underlying the ventricular arrhythmias. Considering the key role of IK1 channel in maintaining the RMP, and the fact that IK1 is decreased by lysophosphatidylcholine (LPC) [6], intracellular acidosis [10, 11], and β-adrenergic receptor (β-AR) agonist [12], IK1 may probably be involved in the arrhythmogenesis in ischemic heart diseases. However, drugs that act mainly on RMP or IK1 channel are currently not available in the clinic. Zacopride is originally known as a 5-HT3 receptor antagonist and a 5-HT4 receptor agonist. In 2012 and 2013, we reported an alternative property of zacopride which is independent of 5-HT receptors, i.e., zacopride is proved a selective IK1 /Kir2.1 channel agonist and shows antiarrhythmic effect in an aconitine-treated rat model [13, 14]. Very recently, Elnakish and coworkers demonstrated that zacopride suppresses calcium overload- induced arrhythmias in human ventricular myocardium in vitro [15]. In the present study, we tested the potential preventative and curative effects of zacopride on cardiac ischemic arrhythmias in rat acute MI model, and further explored the underlying mechanisms mainly focusing on the IK1 channel and transmembrane potential (TMP), using native cardiomyocytes and Chinese hamster ovary (CHO) cells transfected with Kir2.x channels.
Materials and methods
Animals
Male Sprague-Dawley (SD) rats (age 2 months, weight 220–250 g) were provided by the National Institute for Food and Drug Control (Shijiazhuang, China). Rats were housed under standard conditions: room temperature 20–24°C, humidity 40–60%, 12:12 h light (200 lux)-dark (LD) cycles, chaw and water ad libitum. The investigation conformed to the guideline for the Care and Use of Laboratory Animals (NIH, No. 85–23, revised 1996) and followed the approval of Shanxi Medical University Bioethical Committee.
Induction of acute ischemic arrhythmias
In vivo study. Arrhythmias were induced by ligating the left main coronary artery as previously described [16]. Briefly, rats were anesthetized with sodium pentobarbital (65 mg/kg, i.p.), then were intubated and ventilated with room air using an animal respirator (DH-1, Chengdu Instrument Factory, Chengdu, China) with a tidal volume of 30 ml/kg body weight and a rate of 60 tidals/min to maintain normal blood pO2, pCO2 and pH. Body temperature was maintained with an air conditioner and an appropriate heating lamp. Left thoracotomy was performed in the fourth intercostal space, and lead II electrocardiogram (ECG) was recorded throughout the experiments. After opening the pericardium, a 6–0 suture was placed around the proximal portion of the left coronary artery, and the artery wasligated for 15 minutes (min). The treatment protocols are shown in Fig 1A. In the pre-treatment group, zacopride at 5, 15, 50 μg/kg or lidocaine at 7.5 mg/kg was dissolved in 0.2 ml of saline and administered intravenously (i.v.) 3 min before coronary artery occlusion. Post-treatment with zacopride (15 μg/kg) was executed 3 min after coronary occlusion. For the therapeutic treatment of ventricular tachyarrhythmias, zacopride (15 μg/kg) was i.v. infused after the onset of the first sustained VT or VF, which usually appeared over 30 seconds (s) after coronary occlusion in our model. Each control rat received 0.2 mL saline (i.v.). Lidocaine (7.5 mg/kg) was used as a positive control drug.
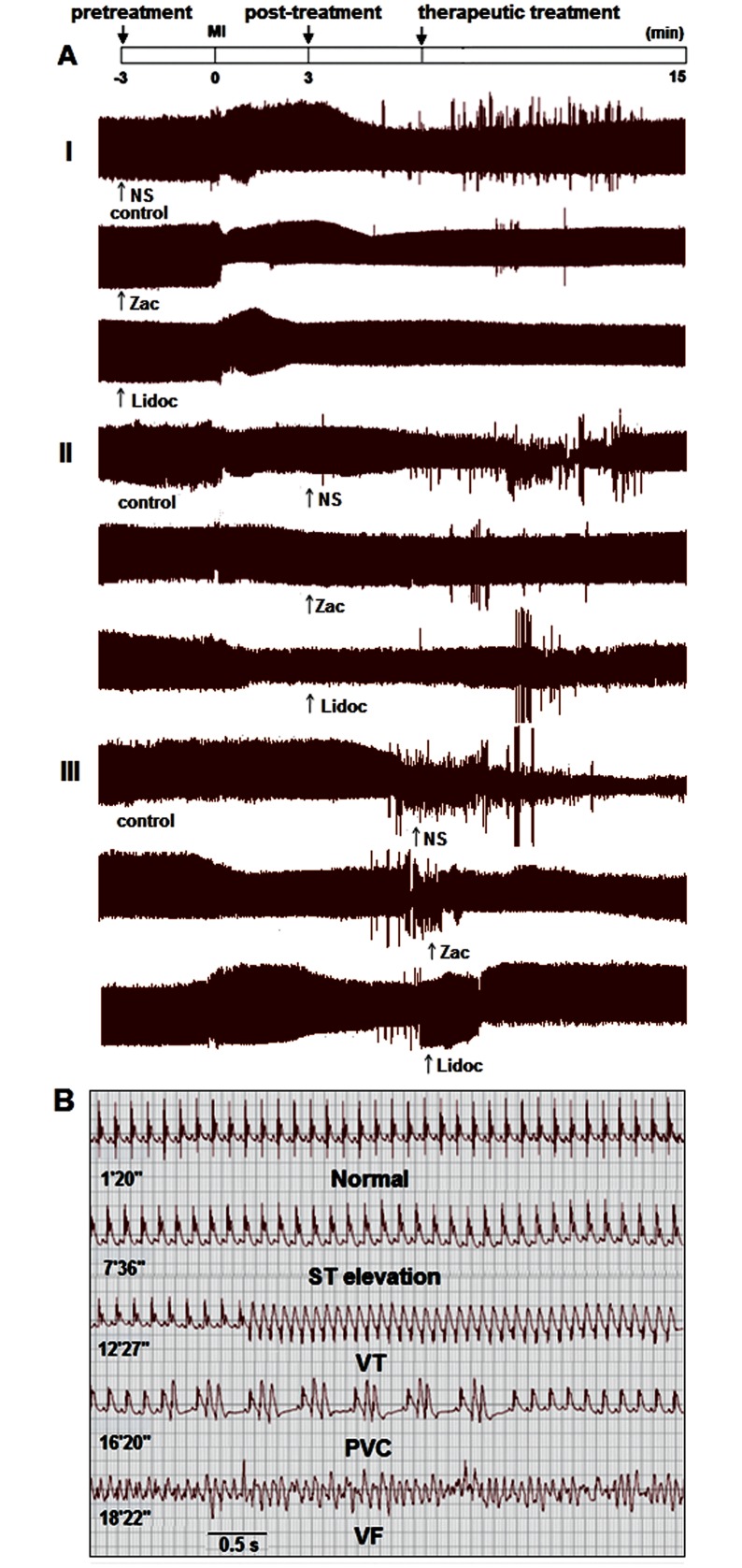
Fig 1. The preventative and curative effects of zacopride on MI- induced ventricular arrhythmias in anesthetized rats in vivo.
(A) Representative condensed ECGs (25 s/div). I, pretreatment; II, post-treatment; III, therapeutic treatment. (B) Time course of ECG traces for saline control rats (coronary occlusion + saline i.v.). Zac, zacopride, at 15 μg/kg. Lidoc, lidocaine, at 7.5 mg/kg.
Ex vivo study. Ventricular arrhythmias were induced by ligating the left main coronary artery in the isolated and Langendorff-perfused rat hearts as previously described [17]. In brief, rats were anesthetized with sodium pentobarbital (65 mg/kg, i.p.) and heparinized (1000 U/kg, i.p.) for 15 min. Hearts were then quickly harvested and mounted on an 80 cm H2O high Langendorff aortic retrograde perfusion system. Tyrode’s solution was bubbled with 100% O2, and the temperature was maintained at 37°C. Three ECG leads were placed on the cardiac apex, right auricule and ground to simulate ECG lead II. The ECGs were recorded with a BiopacSystem (RM6240, Chengdu Instrument Factory, Chengdu, China). All hearts were initially equilibrated for 1 hour before ECG recordings. The left main coronary artery was ligated across a small cotton roll for 15 min within 2 mm from the artery emergence and adjacent to the left atrium. Zacopride at 1 μmol/L or a combination of 1 μmol/L zacopride and 1 μmol/L BaCl2 was applied 3 min before coronary occlusion.
Evaluation of arrhythmias
Prior to and during ischemia, ECGs were continuously recorded with a waveform data analysis software (RM6240, BiopacSystem, Chengdu Instrument Factory, Chengdu, China). The ventricular ectopic activity was evaluated according to the diagnostic criteria advocated by Lambeth Convention [18]. The ECGs were analyzed to determine the onset of the individual episode of arrhythmias, total episodes and episode durations of ventricular tachyarrhythmias, including premature ventricular contraction (PVC), VT and VF. Sustained VT (susVT) or VF (susVF) was designated if the lasting time of individual episode was longer than 30 s.
Isolation of rat single ventricular myocytes
Single left ventricular myocytes were isolated using an enzymatic dissociation procedure described previously[19]. In brief, after appropriate anesthesia (sodium pentobarbital 65 mg/kg, i.p.), the rat heart was quickly harvested and placed into chilled (4°C), oxygenated (100% O2) and Ca2+-free Tyrode’s solution, then the heart was mounted onto a Langendorff retrograde perfusion apparatus via the aorta with a perfusion pressure of 80-cm H2O. The composition of Tyrode’s solution was (in mmol/L): NaCl 135.0, KCl 5.4, CaCl2 1.8, MgCl2 1.0, NaH2PO4 0.33, HEPES 10.0, and glucose 10.0 (pH 7.3–7.4 adjusted with NaOH). The heart was first perfused with oxygenated (100% O2) and Ca2+-free Tyrode’s solution at 37°C for approximately 10 min to wash out the blood. The perfusate was then switched to enzyme-containing Tyrode’s solution and the heart was perfused for about 20 min until the tissue was adequately digested. The enzyme-containing Tyrode’s solution was composed of (in mmol/L) NaCl 125.0, KCl 5.4, MgCl2 1.0, NaH2PO4 0.33, HEPES 10.0, glucose 10.0, taurine 20.0, as well as 5.0–8.0 mg/50 mL collagenase P (Boehringe Mannheim, Germany) depending on the enzyme activity. The left ventricle was then separated and minced in Krebs buffer (KB) solution which contained (in mmol/L) KOH 85.0, L-glutamic acid 50.0, KCl 30.0, MgCl2 1.0, KH2PO4 30.0, glucose 10.0, taurine 20.0, HEPES 10.0, and EGTA 0.5. The pH was adjusted to 7.4 with KOH. The dispersed cells were filtrated twice in KB solution using a 150 μm stainless steel mesh, and then stored in KB solution at room temperature (25°C) at least 4 hours before use.
Transfection of Kir2.x channels in Chinese hamster ovary (CHO) cells
Respective rat cardiac orthologs of Kir2.1, Kir2.2 and Kir2.3 were cloned via reverse transcriptase polymerase chain reaction (RT-PCR) and then subcloned into the eukaryotic expression vector, pEGFP-N1. CHO cells were cultured in Dulbecco’s modified Eagle’s medium supplemented with 10% fetal calf serum. Confluent CHO cells were then transiently transfected with the expression plasmids using a Lipofectamine 2000 kit (Invitrogen, USA).
Electrophysiology
Whole-cell recording of IK1 currents in rat native ventricular myocytes and Kir2.x channel currents in CHO cells were performed under normoxic or hypoxic condition.
Briefly, isolated cardiomyocytes or Kir2.x-transfected CHO cells were transferred to a special chamber mounted on an inverted microscope (Nikon Diaphot, Nikon Co., Tokyo, Japan). The chamber was enclosed except three admittance holes intended for bath solution, 100% N2 and microelectrode. To create a hypoxic condition, a separate reservoir of bath solution was bubbled with 100% N2, and the chamber was flooded with 100% N2 to guarantee the pO2 lower than 50 mmHg (40.6 ± 0.9 mmHg) in the bath solution. The pO2 was measured by a blood gas analyzer (ABL80, Denmark). The cells were superfused with bath solution at 36°C for recording RMP and AP, or at room temperature (22–23°C) for recording IK1, ATP-sensitive potassium current (IKATP) and Kir2.x channel currents. The perfusion flow rate was 2 ml/min. Voltage-clamp or current-clamp recordings were performed with a whole-cell configuration using the Axopatch-200B patch clamp amplifier (Axon Instrument, USA). Patch electrodes were made from thin-walled glass capillaries (1.5 mm OD, Beijing Brain Research Institute) using a two-stage vertical microelectrode puller (PP-83, Narishge Scientific Instrument, Japan) with resistance of 2–5 MΩ. The current signal was filtered at 2 kHz. In all experiments, the membrane current density was measured, normalized to cell capacitance and expressed as pA/pF. The cell capacitance was measured using a method described by Axon Guide. The pClampex 8.2 programme (Axon Instrument, USA) was utilized to produce clamping commands and to record channel currents.
Solutions
To measure the RMP and AP of ventricular myocytes, the bath solution contained (in mmol/L) NaCl 135.0, CaCl2 1.8, MgCl2 1.0, KCl 5.4, glucose 10.0, NaH2PO4 0.33, and HEPES 10.0, and the pH was adjusted to 7.4 with NaOH. The pipette solution contained (in mmol/L) KCl 150.0, MgCl2 1.0, EGTA 5.0, HEPES 5.0, ATP-K2 3.0, the pH was adjusted to 7.3 with KOH. The membrane potentials were corrected for the liquid junction potential. To record the IK1 of ventricular myocytes, the bath solution contained (in mmol/L) NaCl 135.0, CaCl2 1.8, MgCl2 1.0, KCl 5.4, glucose 10.0, NaH2PO4 0.33, HEPES 10.0, and CdCl2 0.5, the pH was adjusted to 7.4 with NaOH. BaCl2 (0.2 mmol/L in the bath solution) was used to block IK1 channels. IK1 was determined as Ba2+-sensitive current. The pipette solution contained (in mmol/L) KCl 150.0, MgCl2 1.0, EGTA 5.0, HEPES 5.0, ATP-K2 3.0, and 4-aminopyridine (4-AP) 5.0 (pH 7.4 adjusted with KOH). To measure the IKATP of ventricular myocytes, Tyrode’s solution was used as the bath solution. The pipette solution contained (in mmol/L) KCl 150.0, EGTA 10.0, HEPES 5.0, and the pH was adjusted to 7.3 with KOH. To measure the Kir2.x channel currents in CHO cells, the bath solution contained (in mmol/L): NaCl 136.0, KCl 5.0, CaCl2 1.8, MgCl2 1.0, glucose 10.0, HEPES 10.0 (pH 7.4). The pipette solution contained (in mmol/L) KCl 40.0, K-aspartate 80.0, KH2PO4 10.0, phosphocreatine 3.0, EGTA 5.0, HEPES 5.0, ATP-Mg 5.0 (pH 7.2 with KOH).
Induction of delayed afterdepolarization (DAD)
DAD is usually generated by intracellular Ca2+ overload in cardiomyocytes [20, 21]. We induced Ca2+ overload by hypoxia or isoproterenol (Iso) (1 μmol/L) (Sigma-Aldrich, USA). APs were elicited by a train of 5 depolarizing pulses with basic cycle length (BCL) of 100 ms, pulse duration of 2 ms and intensity of 0.8–1.2 nA delivered through the pipette. The incidence of DAD (the ratio of cells with DAD to total tested cells) was measured in the presence or absence of 1 μmol/L zacopride.
Statistical analyses
Quantitative data were presented as mean ± SEM, and were analyzed with the ANOVA (analysis of variance) function of SPSS 17.0 software, followed by Least-Significant Difference (LSD) test. Numerical data, such as the episodes of a certain type of arrhythmias, were compared using the chi square (χ2) test between groups. Difference was considered statistically significant if the P value was less than 0.05.
Results
Zacopride suppresses acute ischemic arrhythmias, irrespective of use in a preventative or therapeutic treatment setting
In vivo study. The protocol for zacopride treatment is depicted in Fig 1A. In the pilot experiment, we set the coronary occlusion time to 5, 15, 30, 45 or 60 min. Severe ventricular tachyarrhythmias usually appeared 5–6 min after coronary occlusion and peaked at 9–12 min (Fig 1B), and most acute ischemic arrhythmia occurred within 15 min after MI. Therefore, we set the ischemia time to 15 min in all rats in subsequent experiments. Zacopride i.v. administration significantly reduced or even eliminated ischemic ventricular arrhythmias both in episode number and duration compared with the saline control, irrespective of administration time, before MI (pre-treatment), after MI (post-treatment), or 30 s after the appearance of the first sustained VT/VF (therapeutic treatment) (Fig 1, Tables 1 and 2). Note that 15 μg/kg zacopride exerted the optimal antiarrhythmic efficacy, which compared favorably with that of lidocaine (7.5 mg/kg), a classical antiarrhythmic drug.
Table 1. The suppressive effects of zacopride pretreatment or post-treatment on acute ischemic arrhythmias in anesthetized rats in vivo (mean ± SEM).
| n | Arrhythmia latency time (s) | Total episodes of PVC | Duration of VT (s) | Incidence of VT (%) | Duration of VF (s) | Incidence of VF (%) | |
|---|---|---|---|---|---|---|---|
| Pretreatment | |||||||
| Control | 8 | 344.1 ± 21.1 | 149 ± 23 | 51.2 ± 16.1 | 100 | 6.9 ± 2.5 | 75 |
| Zac 5 μg/kg | 8 | 394.3 ± 18.2 | 157 ± 13 | 40.4 ± 5.2 | 100 | 0.7 ± 0.7 ** | 12.5 * |
| Zac 15 μg/kg | 8 | 475.6 ± 35.0 ** | 45 ± 15** | 2.1 ± 1.4** | 25** | 0 ** | 0 ** |
| Zac 50 μg/kg | 8 | 402.6 ± 36.7 | 38 ± 12** | 9.2 ± 2.9** | 75 | 0.2 ± 0.2 ** | 12.5 * |
| Lidoc 7.5 mg/kg | 8 | 518.8 ± 27.8 **# | 57 ± 17**# | 1.2 ± 0.9**# | 25**# | 0.2 ± 0.2 **# | 12.5 *# |
| Post-treatment | |||||||
| Control | 8 | 335.6 ± 11.8 | 105 ± 18 | 51.9 ± 12.3 | 100 | 4.4 ± 1.7 | 75 |
| Zac 15 μg/kg | 8 | 447.1 ± 26.1 ** | 14 ± 5** | 1.8 ± 0.9** | 37.5* | 0 ** | 0** |
| Lidoc 7.5 mg/kg | 8 | 430.6 ± 20.9**# | 53 ± 19**# | 1.8 ± 1.0**# | 50# | 0.3 ± 0.3 **# | 12.5 *# |
PVC, premature ventricular contraction. VT, ventricular tachycardia. VF, ventricular fibrillation. Zac, zacopride. Lidoc, lidocaine. Duration of VT, mean episode duration of VT. Duration of VF, mean episode duration of VF.
* P < 0.05,
** P < 0.01 vs. control.
# P > 0.05 vs. 15 μg/kg Zac.
Table 2. The suppressive effects of zacopride therapeutic treatment on acute ischemic arrhythmias in anesthetized rats in vivo (mean ± SEM).
| n | Latency time of the first susVT/VF (s) | Termination time of the first susVT/VF (s) | The remaining episodes of PVC | Total duration of the remaining VT (s) | Total duration of the remaining VF (s) | |
|---|---|---|---|---|---|---|
| Control | 8 | 428.9±30.3# | 129.8±54.5 | 110±21 | 191.4±55.5 | 30.1±11.0 |
| Zac 15 μg/kg | 8 | 465.1±53.3 | 27.5 ±5.5* | 26±10** | 51.9±10.9** | 0** |
| Lidoc 7.5 mg/kg | 8 | 494.1±44.0# | 26.5±7.3*# | 20±5**# | 40.4±11.8**# | 0.5±0.3**# |
Latency time of the first susVT/VF, the time from coronary occlusion to the onset of the first sustained VT or VF. Sustained VT or VF was designated a sustained time > 30 s. Termination time of the first susVT/VF, the time from drug administration to the termination of the first sustained VT or VF. Total duration of the remaining VT/VF (s), total duration (s) of the remaining VT/VF during the period from the termination of the first sustained VT/VF to the 15th min after coronary occlusion.
* P < 0.05,
** P < 0.01 vs. control,
# P > 0.05 vs.15 μg/kg Zac.
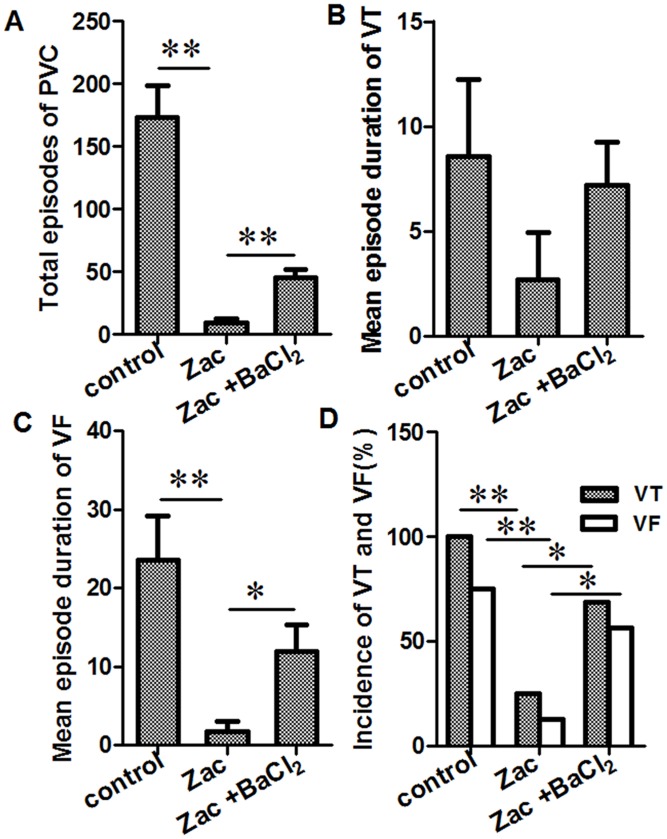
Ex vivo study. According to our previously published study [13], zacopride is a selective agonist of IK1, with the optimal concentration at 1 μmol/L. Additionally, BaCl2, a blocker of IK1 channel, roughly abolished zacopride-mediated enhancement of the IK1 current at 1 μmol/L [13]. In the present study, data from Langendorff- perfused hearts (Fig 2A) showed that, during the 15-min ischemia in saline control rats, the mean numbers of PVC were 173 ± 26, all rats (16/16, 100%) exhibited VT, the mean episode duration of VT was 8.6 ± 3.7 s, 75% (12/16) of rats exhibited unsustained VF with a mean episode duration of 23.5 ± 5.7 s. In rats pretreated with 1 μmol/L zacopride, the number of PVC episodes were reduced to 9 ± 4, and the incidence of VT and VF decreased to 25% and 12.5%, respectively; the episode durations of VT and VF decreased respectively to 2.7 ± 2.2 s and 1.7 ± 1.3 s. BaCl2 at 1 μmol/L blunted the anti-arrhythmic effects of zacopride, as shown by increases in the total number of PVC episodes (45 ± 7), the mean episode duration of VT (7.2 ± 2.0 s) and VF (11.9 ± 3.5 s), and the episode frequency of VT and VF (68.8% and 56.3%, respectively) relatively to zacopride treatment. Note that zacopride or BaCl2 per se had no effects on heart rhythm in normal rats (Fig A in S1 Dataset). These results indicate that zacopride pretreatment exerts significant anti-arrhythmic effects in MI rats, and these effects are mediated by the enhancement of IK1 currents.
Fig 2. Effects of zacopride on ischemia-induced ventricular tachyarrhythmias in the ex vivo rat hearts.
Zacopride at 1 μmol/L decreased the total number of PVC episodes (A), the mean episode duration of VT (B) or VF (C), and the incidence of VT or VF (D). BaCl2 at 1 μmol/L partially reversed the effect of zacopride. Zac, zacopride. * P < 0.05, ** P < 0.01.
Zacopride restores hypoxia-induced IK1 decline, RMP depolarization and APD prolongation in rat ventricular myocytes
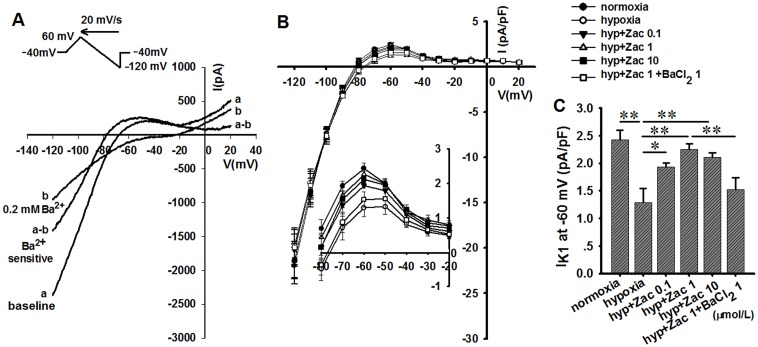
The electrophysiological experiments which carried out under hypoxic conditions were designed to clarify the cellular mechanisms of zacopride against arrhythmias. Glibenclamide (10 μmol/L) was used in the bath solution to prevent the opening of IKATP channel which usually occurs during hypoxia. Under the N2 mediated hypoxia, the IK1 current was measured with a ramp voltage-clamp pulse depolarized from a holding potential of –40 mV to +60 mV, then hyperpolarized to –120 mV at a rate of 20 mV/s. All current traces are presented as Ba2+-sensitive currents. As shown in Fig 3, soon after N2 overflowing, IK1 markedly decreased (from 2.4 ± 0.2 to 1.3 ± 0.3 pA/pF at –60 mV, n = 6, P < 0.01), and was restored by 1 μmol/L zacopride with a mean increase of 76.9% in the outward current (2.3 ± 0.1 pA/pF at –60 mV, n = 6, P < 0.01). The IK1 increase by zacopride was reversed to 1.5 ± 0.2 pA/pF at –60 mV by co-application of 1 μmol/L BaCl2. These results are consistent with our previous observation under normoxic condition [13].
Fig 3. The effect of zacopride on the IK1 of hypoxic native rat ventricular myocytes.
(A) A typical recording for IK1. (B) The current-voltage (I-V) curves of IK1. All traces indicated Ba2+-sensitive currents and were normalized for cell capacitance. The inset shows an enlarged outward portion of the I-V curves. (C) The outward IK1 currents (at –60 mV) decreased soon after the onset of hypoxia and were restored by zacopride. The maximal efficacy appeared at 1 μmol/L and attenuated by 1 μmol/L BaCl2. Zac, zacopride; hyp, hypoxia. * P < 0.05, ** P < 0.01.
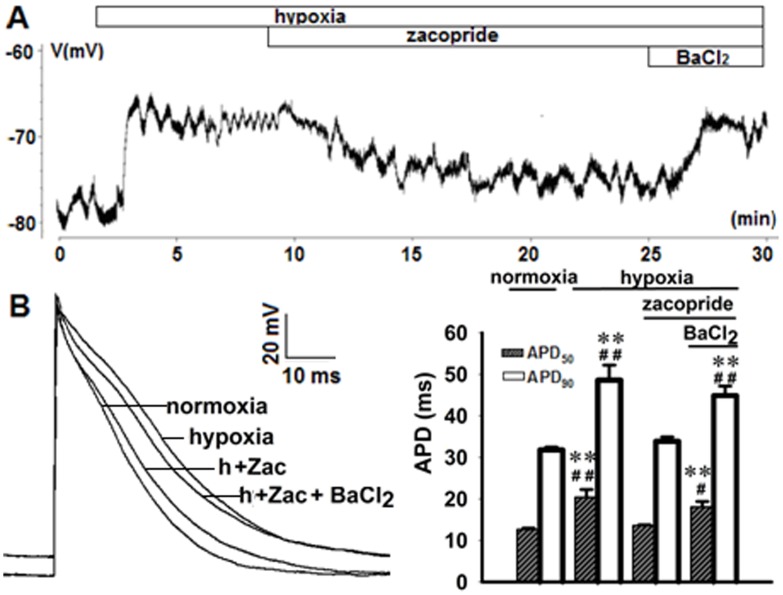
A sharp RMP depolarization occurred within the first 2 min of hypoxia, accompanying with prolongation of ADP50 and APD90 and fall of the AP amplitude (APA). Zacopride (1 μmol/L) moderately hyperpolarized the RMP and restored the ADP50, APD90 and APA. These effects were abolished by 1 μmol/L BaCl2 (Fig 4 and Table A in S1 Dataset).
Fig 4. Representative transmembrane potentials (TMPs) showing the effects of zacopride on the RMP (A) and AP (B) in rat ventricular myocytes under hypoxic conditions.
The right panel of B shows the statistical analysis of APD changes in response to zacopride (1 μmol/L) or zacopride (1 μmol/L) plus BaCl2 (1 μmol/L). Zac, zacopride. h, hypoxia. N = 6. ** P < 0.01, vs. normoxia. # P < 0.05, ## P < 0.01, vs. Zac.
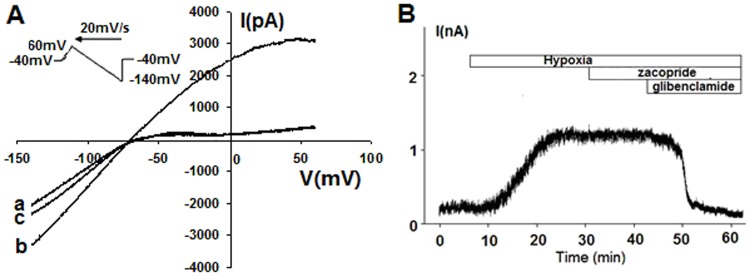
Zacopride does not affect hypoxia-activatated IKATP channel
The background membrane current in response to depolarizing or hyperpolarizing voltage was recorded with a ramp voltage-clamp pulse from a holding potential of –40 mV to +60 mV, followed by hyperpolarization to –140 mV at a rate of 20 mV/s (Fig 5A). When the cell was subjected to N2 overflow for approximately 15 min, the outward current evidently increased at potentials positive to the RMP. Activation of the IKATP channel was defined by a measurable increase in the outward current and inhibited by a specific IKATP blocker glibenclamide. Under the same hypoxic condition, the cardiomyocyte was clamped at potential of +20 mV (Fig 5B). After the activation of glibenclamide-sensitive current, zacopride at 1 μmol/L did not alter the value of this current (Fig 5B).
Fig 5. Zacopride did not affect hypoxia-induced and glibenclamide-sensitive currents in isolated rat ventricular myocytes.
(A) The I-V curves of the measured currents. a, baseline. b, hypoxia. c, 10 μmol/L glibenclamide. (B) Time course of the membrane currents measured at 20 mV under hypoxic condition. One μmol/L zacopride and 10 μmol/L glibenclamide were applied in succession.
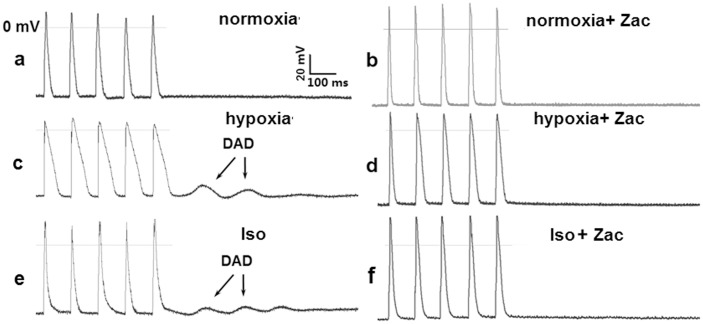
Zacopride suppresses hypoxia- or isoproterenol-induced DADs in rat cardiomyocytes
At in vitro condition, cardiomyocytes lack endogenous neurohumoral regulation. To mimic ischemia and adrenergic stimulation at the cellular level in vitro, isolated cardiomyocytes were exposed to hypoxia or 1 μmol/L Iso. In the current clamp mode, an electrical train of 5 stimuli at 100 ms BCL did not introduce DAD under normoxic condition, but did under hypoxia or Iso exposure (Fig 6). Pretreatment with 1 μmol/L zacopride decreased the incidence of DAD from 73.3% (11 of 15 preparations) to 20.0% (3 of 15 preparations) (P < 0.01) in the hypoxic model and from 66.6% (10 of 15 preparations) to 13.3% (2 of 15 preparations) (P < 0.01) under Iso treatment (Fig 6).
Fig 6. Representative transmembrane potential (TMP) traces showing hypoxia- or Iso-induced DADs in rat ventricular myocytes.
a, normoxia. b, normoxia + Zac (1 μmol/L). c, hypoxia. d, hypoxia + Zac (1 μmol/L). e, Iso (1 μmol/L). f, Iso (1 μmol/L) + Zac (1 μmol/L). Zac, zacopride. Iso, isoproterenol.
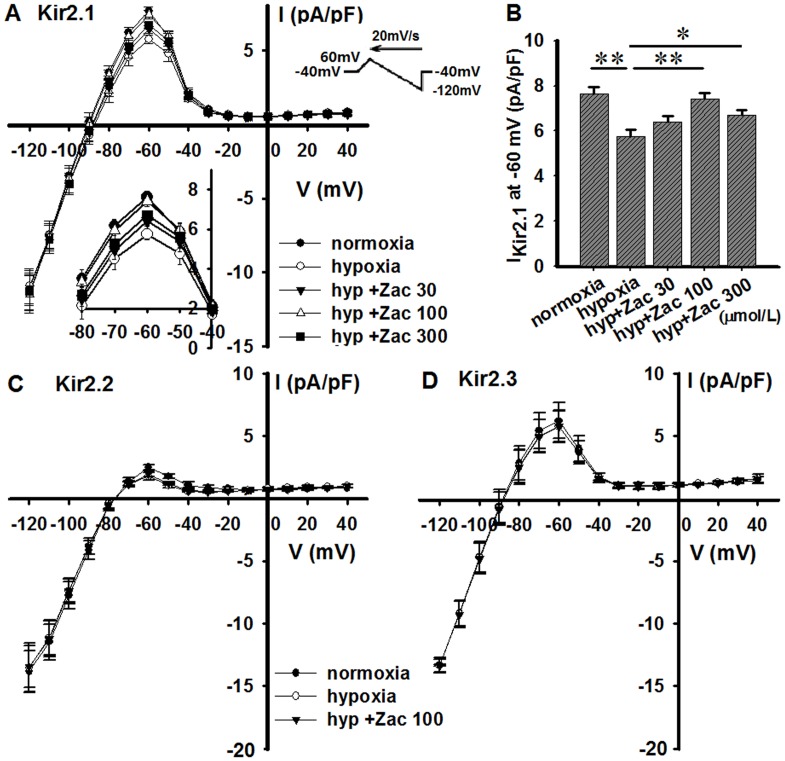
Zacopride rescues the hypoxia-induced decrease of IKir2.1, but not IKir2.2 and IKir2.3, in CHO cells
Soon after N2 overflow, the outward component of IKir2.1 decreased (from control 7.6 ± 0.3 pA/pF to 5.8 ± 0.3 pA/pF at –60 mV, n = 6, P < 0.05) in CHO cells transiently expressing Kir2.1 channels, and zacopride significantly attenuated this decrease (Fig 7A). The efficacy of zacopride was maximized at 100 μmol/L, with a mean increase of 28.8% in the outward current (from 5.8 ± 0.3 to 7.4 ± 0.3 pA/pF at –60 mV, n = 6, P < 0.01) (Fig 7B). Zacopride was likely less effective at 300 μmol/L than at 100 μmol/L (Fig 7B) and did not affect the inward component of IKir2.1. Hypoxia per se or zacopride (100 μmol/L) did not significantly affect the IKir2.2 or IKir2.3 (Fig 7C and 7D). Based on these results, zacopride is likely a selective agonist of the Kir2.1 channel.
Fig 7. Effects of zacopride on IKir2.x currents in hypoxic CHO cells.
(A) and (B), Kir2.1. (C) Kir2.2. (D) Kir2.3. The hypoxia-induced decrease of IKir2.1 was reversed by zacopride, whereas IKir2.2 and IKir2.3 were refractory to both hypoxia and zacopride treatment. Zac, zacopride. Hyp, hypoxia. N = 6. * P < 0.05, ** P < 0.01.
Discussion
In the present study, we demonstrated that zacopride, a selective IK1 channel agonist, significantly eliminated acute ischemic arrhythmias in MI rats, irrespective of the time of administration (before MI, after MI, or after the occurrence of malignant arrhythmias). The underlying mechanisms are ascribed to the activation of the IK1/Kir2.1 channel, maintenance of the RMP, moderate shortening of the APD and the suppression of DADs. This study is the first one to strengthen the hypothesis that enhancing the IK1 and thereby maintaining the RMP and shortening the APD is an effective and even powerful strategy to eliminate acute ischemic arrhythmias in both preventative and therapeutic aspects. The occurrence of lethal ventricular arrhythmias in acute MI is usually unpredictable. Thus, zacopride may potentially be developed as an anti-arrhythmic drug that prevents and treats arrhythmias in acute MI.
Zacopride restores the RMP and shortens the APD by activating the IK1/Kir2.1 channel during hypoxia or ischemia
During the acute stage of MI, K+ disturbance is an important event among variety of ion changes [22]. In the heart, [K+]o is frequently elevated due to accumulation of extracellular K+. Increased [K+]o and simultaneous inward currents involving Na+, Ca2+ and Cl−channels and exchangers depolarize the membrane [23, 24]. The conductance of the IK1 channel is increased by higher [K+]o [25] but decreased by lysophosphatidylcholine (LPC) [6], intracellular acidosis [10, 11] and adrenergic stimulation[12]. Eventually, the IK1 conductance may decrease and lead to membrane potential depolarization. During cardiac ischemia, changes in APD involve an initial lengthening followed by a marked shortening[26, 27]. The APD prolongation upon early ischemia is due to a reduction of electrogenic pump current, a fall of IK1 as a consequence of intracellular acidosis, and an acute inhibition of Ito[27]. The shortening of APD is partially attributable to activation of IKATP [27, 28].
In the present study, we created a hypoxic environment by N2 flux around patched cells in an enclosed chamber, and this manipulation reduced the pO2 of the bath solution to less than 50 mmHg. The RMP depolarization was well recognized within the first minute of hypoxia, along with IK1 reduction and APD prolongation during the early stage of hypoxia. Zacopride treatment enhanced the IK1, restored the depolarized RMP, and moderately shortened the APD. According to our previous work [13] and the present study, BaCl2 at 1 μmol/L could abolish zacopride (1 μmol/L)-induced IK1 increase under nomoxic or hypoxic conditions. It makes sense of subsequent results that 1 μmol/L BaCl2 diminished the effect of zacopride on RMP and APD during hypoxia. Because these experiments were all performed in the presence of glibenclamide (IKATP channel blocker), we excluded IKATP as a confounding factor when explaining the relationship between IK1 and RMP/APD.
Activation of the IKATP channel also hyperpolarizes the RMP and shortens the APD during hypoxia or ischemia, but it may be a relatively late event[29, 30]. In the present study, the IKATP channel opened at least 15 min after the onset of hypoxia (shown in Fig 5), an phenomenon consistent with the observation by Liu et al [30]. The subsequent application of 1.0 μmol/L zacopride did not affect the IKATP channel. Combining the observation that BaCl2 inhibited the effects of zacopride on the RMP and APD, we conclude that the effect of zacopride on RMP and APD is mediated by IK1, rather than by IKATP.
Enhancing RMP by activating the IK1 channel may represent a strategy to manipulate lethal arrhythmias in acute MI
Following coronary occlusion, ventricular arrhythmias are the critical cause of mortality in rats [31]. Re-entry, enhanced automaticity and triggered activity are likely the ultimate electrophysiological manifestation and the main underlying arrhythmogenic mechanisms in acute MI based on membrane damage and ionic imbalance [32]. We previously reported the ability of zacopride in attenuating aconitine-induced triggered arrhythmia [13]. In cardiac ischemia, myocardial substrates likely favor re-entry, but non-reentrant mechanisms, such as abnomal automaticity and triggered activity (TA) may be the most important initiators for lethal arrhythmias [33 – 35].
During cardiac ischemia, a burst of arrhythmias, including PVC, VT and VF, begins approximately 5 min after coronary occlusion and persists for at least 15 min in the rat model. These early arrhythmias are mainly attributable to disturbances in the RMP [4 – 6] and adrenergic activation (in vivo) [7 – 9]. For instance, there are an 100- fold increase in the catecholamine concentration within the extracellular space of the ischemic zone, a two fold increase in functionally coupled α-adrenoceptors and a 30% increase in β-adrenoceptors 15 min after myocardial ischemia [8]. Our hypothesis that enhancing the IK1 current attenuates arrhythmia in acute MI is based on the following three theoretical perspectives.
First, moderate enhancement of IK1 is a compensation for the reduction in this current and helps to maintain a normal RMP, the latter would likely eliminate any abnormal automaticity and improve the conductivity. During hypoxia or ischemia, cardiomyocytes are usually depolarized due to extracellular K+ accumulation [4] and intracellular acidosis [5]. Depolarization makes the membrane potential more prone to reach the threshold for Na+ channel activation and eventually generate propagated action potentials [35]. By enhancing the IK1, zacopride prevents RMP depolarization and consequently decreases cardiac excitability and autorhythmicity. Moreover, depolarization also inactivates voltage-gated Na+ channel. The recovery of RMP may increase Na+ channel availability and improve the conductivity in ischemic myocardium, and thus help to prevent or terminate re-entrant activity [36].
Second, IK1 channels determine the diastolic membrane conductance of cardiomocytes. Moderate IK1 enhancement increases the diastolic conductance and attenuates the fluctuation of membrane potential and thus to avoid aberrant action potentials aroused by a smaller depolarization [37].
Third, regarding the importance of the IK1 in maintaining the diastolic RMP and late phase 3 repolarization, enhancing IK1 is beneficial to abolishing or attenuating DADs or early afterdepolarizations (EADs). In vivo, Ca2+ overload due to ischemic membrane damage and adrenergic stimulation may initiate DADs [20]. As shown in the present study, zacopride increased the resting membrane conductance, which is a critical electrophysiological mechanism for diminishing the onset of DADs. By increasing the repolarizing current, zacopride moderately shortened the APD, which also helps to reduce Ca2+ influx and the development of DADs. In addition, moderate APD shortening alleviates AP triangulation and shrinks the vulnerable window for the reactivation of voltage-gated Ca2+ channel. Overall, both effects may alleviate the susceptibility of ventricular myocardium to EADs [38].
The IKATP channel operates only when the intracellular ATP concentration is significantly decreased (i.e., during hypoxia or ischemia). The openers/agonists of IKATP channel also hyperpolarize the RMP and shorten the APD, which are acknowledged to protect ischemic hearts. The emergence of the IKATP channel agonists constitutes an advance in anti-arrhythmia efforts albeit far from totally effective. The critical reason might be that the inward rectification of IKATP is markedly weaker than that of IK1. When the membrane potential is depolarized, activated IKATP permits generous potassium efflux during the plateau phase of AP. The resultant visible shortening of the APD associated with the shortening of the refractory period may even promote arrhythmia. Alternatively, the IK1 channel only slightly conducts current during the plateau phase due to the strong inward rectification, which helps to maintain a long-lasting plateau phase and prevents excessive potassium loss. Therefore, Lopatin et al [2] predicted that the ideal drug for suppressing ventricular arrhythmias ought to have the property of opening K+ channels at the resting potential, but not at the peak of the action potential, i.e., one that acts on the IK1. As a specific agonist of IK1, zacopride is the very candidate. Moreover, considering the time course of membrane damage and membrane potential disturbance during ischemia, zacopride may provide protection to cardiomyocytes during the very early stage of ischemia.
Special concerns about enhancing IK1
Upregulation of IK1 has been deemed to a risk factor for atrial arrhythmogenesis [39 – 41]. Increase of IK1 yields APD and ERP shortening, thus theoretically increases the curvature of spiral waves and thereby stabilizes rotors and re-entry arrhythmias [42, 43]. A concern remains that zacopride may increase the susceptibility to atrial fibrillation (AF) when used in the clinic for treating ischemic ventricular arrhythmias. But is that true? The native IK1 channels in the heart are assembled by Kir2.1 (KCNJ2), Kir2.2 (KCNJ12) and Kir2.3 (KCNJ4) channels, and these channels show tissue- and species-specific profiles [44, 45]. Based on the Western blot results from our previous work [14], Kir2.1 is the predominant isoform in rat ventricles, whereas Kir2.3 is the major isoform in the atrium. Kir2.1 expression in the atrium is only 25% of that in the ventricle. Our previous study in Kir2.x-transfected HEK-293 cells under normoxia [14] and the present results from the Kir2.x-cloned CHO cells under hypoxia indicate that the target channel of zacopride is IKir2.1, whereas IKir2.2 and IKir2.3 channels were refractory to zacopride (shown in Fig 7). These observations explain why zacopride did not affect the atrial IK1 or APD [14] and excluded the possibility of AF occurrence from a theoretical perspective. However, because the association between zacopride and AF has not been studied, the use of zacopride in cases of AF should be approached with caution.
A second concern is the risk of ventricular re-entry arrhythmias. A significant increase in IK1 may shorten APD and ERP, and thereby promote re-entry activities. For example, in two transgenic mice models [46, 47], the IK1 conductance was strikingly increased by approximately 12–14 fold, with resultant severe ventricular arrhythmias. It seems contradictory to advocate the development of anti-arrhythmic agents that enhance IK1. However, this discrepancy may stem from the extent of IK1 regulation, which should be limited. Conditions in transgenetic model usually significantly deviate from physiology. As reported by Li et a l [47], the ADP90 of cardiac myocytes in transgenetic mice was shortened from 21.8 ms (control) to 7.9 ms and accompanied by a more than 10 fold higher density of IK1. Excessive increases in IK1 do not further hyperpolarize the RMP due to the inward rectifying property of IK1, but may markedly accelerate repolarization and shorten the APD, which is undoubtedly pro-arrhythmic. In contrast, zacopride only evokes a 33% increase in IK1 at –60 mV under normoxic condition [13], and a 76.9% increase upon hypoxia. Such a moderate IK1 increment recovered the RMP from –64.4 ± 0.7 mV to –77.4 ± 1.2 mV, which is close to physiological levels (–79.1 ± 1.3 mV). Correspondingly, the shortening of APD50 and APD90 by zacopride were less than 40%. Modulating IK1 within the physiological range is important to minimize the pro-arrhythmic effects of anti-arrhythmic medications.
Limitations
A major limitation of the present study is species differences. The Ito current underlies the initial and rapid (phase 1) repolarization of the AP, and the IK is mainly responsible for subsequent phase 2 and phase 3 repolarization [48]. In adult rat ventricular myocytes, the IK current is smaller and its role is less pivotal, so larger Ito leads to a triangle-like AP morphology [49–51]. But IK is a major determinant of plateau phase duration and the rates of phases 2 and 3 AP repolarization in human and most nonrodent mammalian cardiomyocytes [50]. IK1 is primarily involved in late phase 3 repolarization towards the RMP. Heteromultimer formation among diverse Kir2 family subunits determines the properties of IK1 in different species and consequently influences IK1 contribution to AP configuration [52, 53]. Although the results in rats support our hypothesis, further studies in other species are warranted. Recently, zacopride was reported to exert anti-arrhythmic effects in human ventricular myocardium [15]. IK1 channel may be a promising target for treating human acute ischemic arrhythmias in the future if indication, dosage and administration time are appropriately designed.
Supporting information
The representative ECG traces before and after administration of zacopride (Zac) or BaCl2 respectively in normal isolated rat hearts. Table A. Effects of zacopride on the action potential parameters of rat ventricular myocytes.
(DOC)
(DOCX)
(XLSX)
Acknowledgments
The authors thank Rui-Ling Xu and Lu-Ying Zhao for their excellent technical assistance.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by grants from the National Natural Science Foundation of China (No. 31200864 to QL and No. 81670313 to JC) and Research Project Supported by Shanxi Scholarship Council of China (No. 2016-059 to QL).
References
- 1.Lopatin AN. and Anumonwo JM . Structural and Molecular Bases of Cardiac Inward Rectifier Potassium Channel Function In: Zipes DP, Jalife J, editors. Cardiac electrophysiology: from cell to bedside. 6th edition W.B. Saunders Co; Philadelphia, Pennsylvania, USA: 2014. pp.33 – 41. [Google Scholar]
- 2.Lopatin AN, Nichols CG. Inward rectifiers in the heart: an update on I(K1). J Mol Cell Cardiol. 2001; 33: 625–628. 10.1006/jmcc.2001.1344 [DOI] [PubMed] [Google Scholar]
- 3.Mackall JA, Carlson MD. Ventricular and supraventricular arrhythmias in acute myocardial infarction In: Allen J, Brown DL, editors. Cardiac intensive care. 2nded Philadelphia, PA: Saunders; 2010. pp. 3. [Google Scholar]
- 4.Shaw RM, Rudy Y. Electrophysiologic effects of acute myocardial ischemia: a theoretical study of altered cell excitability and action potential duration. Cardiovasc Res. 1997; 35(2): 256–272. [DOI] [PubMed] [Google Scholar]
- 5.Coraboeuf E, Deroubaix E, Coulombe A. Acidosisinduced abnormal repolarization and repetitive activity in isolated dog Purkinje fibers. J Physiol (Paris). 1980; 76: 97–106. [PubMed] [Google Scholar]
- 6.Clarkson CW and Ten Eick RE. On the mechanism of lysophosphatidylcholine- induced depolarization of cat ventricular myocardium. Circ Res. 1983; 52(5): 543–556. [DOI] [PubMed] [Google Scholar]
- 7.Sedlis SP. Mechanisms of ventricular arrhythmias in acute ischemia and reperfusion. Cardiovasc Clin. 1992; 22(1): 3–18. [PubMed] [Google Scholar]
- 8.Schömig A, Haass M, Richardt G. Catecholamine release and arrhythmias in acute myocardial ischaemia. Eur Heart J. 1991; 12 Suppl F: 38–47. [DOI] [PubMed] [Google Scholar]
- 9.Mill JG, Vassallo DV, Leite CM. Time course of changes in heart rate and sympathetic tone after coronary artery ligation in rats. Braz J Med Biol Res. 1991; 24: 855–858. [PubMed] [Google Scholar]
- 10.Collins A, Larson M. Regulation of inward rectifier K+ channels by shift of intracellular pH dependence. J Cell Physiol. 2005; 202(1): 76–86. 10.1002/jcp.20093 [DOI] [PubMed] [Google Scholar]
- 11.Ito H, Vereecke J,Carmeliet E Intracellular protons inhibit inward rectifier K1 channel of guinea-pig ventricular cell membrane. Pflugers Arch. 1992; 422(3): 280–286. [DOI] [PubMed] [Google Scholar]
- 12.Koumi S, Wasserstrom JA, Ten Eick RE. Beta-adrenergic and cholinergic modulation of inward rectifier K1 channel function and phosphorylation in guinea-pig ventricle. J Physiol (Lond.). 1995; 486: 661–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu QH, Li XL, Xu YW, Lin YY, Cao JM, Wu BW. A Novel Discovery of IK1 Channel Agonist: Zacopride Selectively Enhances IK1 Current and Suppresses Triggered Arrhythmias in the Rat. J Cardiovasc Pharmacol. 2012; 59(1): 37–48. 10.1097/FJC.0b013e3182350bcc [DOI] [PubMed] [Google Scholar]
- 14.Zhang L, Liu Q, Liu C, Zhai X, Feng Q, Xu R, et al. Zacopride selectively activates the Kir2.1 channel via a PKA signaling pathway in rat cardiomyocytes. Sci China Life Sci. 2013; 56(9): 788–796. 10.1007/s11427-013-4531-z [DOI] [PubMed] [Google Scholar]
- 15.Elnakish MT, Canan BD, Kilic A, Mohler PJ, Janssen PM. Effects of zacopride, a moderate IK1 channel agonist, on triggered arrhythmia and contractility in human ventricular myocardium. Pharmacol Res. 2017; 115: 309–318. 10.1016/j.phrs.2016.11.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang SS, Tsai SK,Chiang LY, Tsai LM. Cardioprotective effects of hexasulfobutylated C60 (FC4S) in anesthetized rats during coronary occlusion/ reperfusion injury. Drug Dev Res. 2001; 53: 244–253. [Google Scholar]
- 17.Li S, Wu J, Watanabe M, Li C, Okada T. Protective effects of ischemic postconditioning against hypoxia-reoxygenation injury and hydrogen peroxide-induced damage in isolated rat hearts. Exp Clin Cardiol. 2006; 11(4): 280–285. [PMC free article] [PubMed] [Google Scholar]
- 18.Curtis MJ, Hancox JC, Farkas A, Wainwright CL, Stables CL, Saint DA, et al. The Lambeth Conventions (II): guidelines for the study of animal and human ventricular and supraventricular arrhythmias. Pharmacol Ther. 2013; 139(2): 213–248. 10.1016/j.pharmthera.2013.04.008 [DOI] [PubMed] [Google Scholar]
- 19.Hamill OP, Marty A, Neher E, Sakmann B, Sigworth FJ. Improved patch-clamp techniques for high-resolution current recording from cells and cell-free membrane patches. PflÜgers Arch. 1981; 391: 85–100. [DOI] [PubMed] [Google Scholar]
- 20.Wit AL, Rosen MR. Afterdepolarizations and triggered activity: distinction from automaticity as an arrhythmogenic mechanism In: Fozzard HA, Haber E, Jennings RB, et al. The Heart and Cardiovascular System. 2nd ed New York, NY: Raven Press; 1992. pp. 2113–2163. [Google Scholar]
- 21.Jung CB, Moretti A, Mederos y Schnitzler M, Iop L, Storch U, Bellin M, et al. Dantrolene rescues arrhythmogenic RYR2 defect in a patient-specific stem cell model of catecholaminergic polymorphic ventricular tachycardia. EMBO Mol Med. 2012; 4(3): 180–191. 10.1002/emmm.201100194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris AS, Bisteni A, Russell RA, Brighan JC, Firestone JE. Excitatory factors in ventricular tachycardia resulting from myocardial ischemia. Potassium a major excitant. Science. 1954; 119(3085): 200–203. [DOI] [PubMed] [Google Scholar]
- 23.Sejersted OM, Sjogaard G. Dynamics and consequences of potassium shifts in skeletal muscle and heart during exercise. Physiol Rev. 2000; 80: 1411.–. [DOI] [PubMed] [Google Scholar]
- 24.Stanfield PR, Nakajima S, Nakajima Y. Constitutively active and G-protein coupled inward rectifier K+ channels: Kir2.0 and Kir3.0. Rev Physiol Biochem Pharmacol. 2002; 145: 47–179. [DOI] [PubMed] [Google Scholar]
- 25.Dhamoon AS, Jalife J. The inward rectifier current (IK1) controls cardiac excitability and is involved in arrhythmogenesis. Heart Rhythm. 2005; 2(3): 316–324. 10.1016/j.hrthm.2004.11.012 [DOI] [PubMed] [Google Scholar]
- 26.Watanabe I, Kanda A, Engle CL, Gettes LS. Comparison of the effects of regional ischemia and hyperkalemia on the membrane action potentials of the in situ pig heart. Experimental Cardiology Group, University of North Carolina at Chapel Hill. J Cardiovasc Electrophysiol. 1997; 8(11): 1229–1236. [DOI] [PubMed] [Google Scholar]
- 27.Verkerk AO, Veldkamp MW, van Ginneken AC, Bouman LN. Biphasic response of action potential duration to metabolic inhibition in rabbit and human ventricular myocytes: role of transient outward current and ATP-regulated potassium current. J Mol Cell Cardiol. 1996; 28: 2443–2456. 10.1006/jmcc.1996.0237 [DOI] [PubMed] [Google Scholar]
- 28.Terzic A, Jahangir A, Kurachi Y. Cardiac ATP-sensitive K+ channels: regulation by intracellular nucleotides and K+ channel-opening drugs. Am J Physiol. 1995; 269 (3 Pt 1): C525 –C545. [DOI] [PubMed] [Google Scholar]
- 29.Workman AJ, MacKenzie I, Northover BJ. Do KATP channels open as a prominent and early feature during ischaemia in the Langendorff-perfused rat heart? Basic Res Cardiol. 2000; 95(3): 250–260. [DOI] [PubMed] [Google Scholar]
- 30.Liu Y, Gao WD, O'Rourke B, Marban E. Priming effect of adenosine on K(ATP) currents in intact ventricular myocytes: implications for preconditioning. Am J Physiol. 1997; 273(4 Pt 2): H1637 –H1643. [DOI] [PubMed] [Google Scholar]
- 31.Baldo MP, Davel AP, Nicoletti-Carvalho JE, Bordin S, Rossoni LV, Mill JG. Granulocyte colony-stimulating factor reduces mortality by suppressing ventricular arrhythmias in acute phase of myocardial infarction in rats. J Cardiovasc Pharmacol. 2008; 52: 375–380. 10.1097/FJC.0b013e31818a2bb0 [DOI] [PubMed] [Google Scholar]
- 32.Carmeliet E. Cardiac ionic currents and acute ischemia: from channels to arrhythmias. Physiol Rev. 1999; 79(3): 917–1017. [DOI] [PubMed] [Google Scholar]
- 33.Pogwizd SM. Focal mechanism underlying ventricular tachycardia during prolonged ischemic cardiomyopathy. Circulation. 1994; 90: 1441–1458. [DOI] [PubMed] [Google Scholar]
- 34.Chung MK, Pogwizd SM, Miller DP, Cain ME. Three-dimensional mapping of the initiation of nonsustained ventricular tachycardia in the human heart. Circulation. 1997; 95: 2517–2527. [DOI] [PubMed] [Google Scholar]
- 35.Pogwizd SM, Chung MK, Cain ME (). Termination of ventricular tachycardia in the human heart: insights from three-dimensional mapping of nonsustained and sustained ventricular tachycardias. Circulation. 1997; 95: 2528–2540. [DOI] [PubMed] [Google Scholar]
- 36.Gómez R, Caballero R, Barana A, Amorós I, Calvo E, Lopez JA, et al. Nitric oxide increase cardiac IK1 by nitrosylation of cysteine 76 of Kir2.1 channels. Circ Res. 2009; 105(4): 83–92. [DOI] [PubMed] [Google Scholar]
- 37.Pogwizd SM, Schlotthauer K, Li L, Yuan W, Bers DM. Arrhythmogenesis and contractile dysfunction in heart failure: Roles of sodium-calcium exchange, inward rectifier potassium current, and residual beta-adrenergic responsiveness. Circ Res. 2001; 88: 1159–1167. [DOI] [PubMed] [Google Scholar]
- 38.January CT, Riddle JM. Early afterdepolarizations: mechanism of induction and block. A role for L-type Ca2+ current. Circ Res. 1989; 64(5): 977–990. [DOI] [PubMed] [Google Scholar]
- 39.Cha TJ, Ehrlich JR, Zhang L, Nattel S. Atrial ionic remodeling induced by atrial tachycardia in the presence of congestive heart failure. Circulation. 2004; 110(12): 1520–1526. 10.1161/01.CIR.0000142052.03565.87 [DOI] [PubMed] [Google Scholar]
- 40.Gaborit N, Steenman M, Lamirault G, Le Meur N, Le Bouter S, Lande G, et al. Human atrial ion channel and transporter subunit gene-expression remodeling associated with valvular heart disease and atrial fibrillation. Circulation. 2005; 112: 471–481. 10.1161/CIRCULATIONAHA.104.506857 [DOI] [PubMed] [Google Scholar]
- 41.Zhang H, Garratt CJ, Zhu J, Holden AV. Role of up-regulation of IK1 in action potential shortening associated with atrial fibrillation in humans. Cardiovasc Res. 2005; 66: 493–502. 10.1016/j.cardiores.2005.01.020 [DOI] [PubMed] [Google Scholar]
- 42.Samie FH, Berenfeld O, Anumonwo J, Mironov SF, Udassi S, Beaumont J, et al. Rectification of the background potassium current: a determinant of rotor dynamics in ventricular fibrillation. Circ Res. 2001; 89(12): 1216–1223. [DOI] [PubMed] [Google Scholar]
- 43.Cherry EM, Fenton FH. Suppression of alternans and conduction blocks despite steep APD restitution: electrotonic, memory, and conduction velocity restitution effects. Am J Physiol Heart Circ Physiol. 2004; 286: H2332 –H2341. 10.1152/ajpheart.00747.2003 [DOI] [PubMed] [Google Scholar]
- 44.Anumonwo JM, Lopatin AN. Cardiac strong inward rectifier potassium channels. J Mol Cell Cardiol. 2009; 48: 45–54. 10.1016/j.yjmcc.2009.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hibino H, Inanobe A, Furutani K, Murakami S, Findlay I, Kurachi Y. Inwardly rectifying potassium channels: their structure, function, and physiological roles. Physiol Rev. 2010; 90: 291–366. 10.1152/physrev.00021.2009 [DOI] [PubMed] [Google Scholar]
- 46.Piao L, Li J, McLerie M, Lopatin AN. Transgenic upregulation of IK1 in the mouse heart is proarrhythmic. Basic Res Cardiol. 2007; 102(5): 416–428. 10.1007/s00395-007-0659-y [DOI] [PubMed] [Google Scholar]
- 47.Li J, McLerie M, Lopatin AN. Transgenic upregulation of IK1 in the mouse heart leads to multiple abnormalities of cardiac excitability. Am J Physiol Heart Circ Physiol. 2004; 287: H2790 –H2802. 10.1152/ajpheart.00114.2004 [DOI] [PubMed] [Google Scholar]
- 48.Apkon M, Nerbonne JM. Characterization of two distinct depolarization- activated K+ currents in isolated adult rat ventricular myocytes. J Gen Physiol. 1991; 97: 973–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tande PM, Bjørnstad H, Yang T, Refsum H. Rate-dependent class III antiarrhythmic action, negative chronotropy, and positive inotropy of a novel IK blocking drug, UK68,798: Potent in guinea pig but no effect in rat myocardium. J Cardiovasc Pharmacol. 1990; 16: 401–410. [DOI] [PubMed] [Google Scholar]
- 50.Nerbonne JM. Molecuular basis of functional voltage-gated K diversity in the mammalian myocardium. J Physiol. 2000; 525 Pt 2: 285–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sun X, Wang HS. Role of the transient outward current (Ito) in shaping canine ventricular action potential—a dynamic clamp study. J physiol. 2005; 564: 411–419 10.1113/jphysiol.2004.077263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dhamoon AS, Pandit SV, Sarmast F, Parisian KR, Guha P, Li Y, et al. Unique Kir2.x properties determine regional and species differences in the cardiac inward rectifier K+ current. Circ Res. 2004; 94(10): 1332–1339. 10.1161/01.RES.0000128408.66946.67 [DOI] [PubMed] [Google Scholar]
- 53.de Boer TP, Houtman MJ, Compier M, van der Heyden MA. The mammalian K(IR)2.x inward rectifier ion channel family: expression pattern and pathophysiology. Acta Physiol (Oxf). 2010; 199(3): 243–256. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The representative ECG traces before and after administration of zacopride (Zac) or BaCl2 respectively in normal isolated rat hearts. Table A. Effects of zacopride on the action potential parameters of rat ventricular myocytes.
(DOC)
(DOCX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.