Abstract
Objective
The objective of this study was to assess the costs associated with the hospitalization and the cumulative 30-, 60-, and 90-day readmission rates in a cohort of Medicare beneficiaries with heart failure (HF).
Methods
This was a retrospective, observational study based on data from the national 5% sample of Medicare beneficiaries. Inpatient data were gathered for Medicare beneficiaries with at least one HF-related hospitalization between July 1, 2005, and December 31, 2011. The primary end point was the average per-patient cost of hospitalization for individuals with HF. Secondary end points included the cumulative rate of hospitalization, the average length of hospital stay, and the cumulative 30-, 60-, and 90-day readmission rates.
Results
Data from 63,678 patients with a mean age of 81.8 years were included in the analysis. All costs were inflated to $2,015 based on the medical care component of the Consumer Price Index. The mean per-patient cost of an HF-related hospitalization was $14,631. The mean per-patient cost of a cardiovascular (CV)-related or all-cause hospitalization was $16,000 and $15,924, respectively. The cumulative rate of all-cause hospitalization was 218.8 admissions per 100 person-years, and the median length of stay for HF-related, CV-related, and all-cause hospitalizations was 5 days. Also, 22.3% of patients were readmitted within 30 days, 33.3% were readmitted within 60 days, and 40.2% were readmitted within 90 days.
Conclusion
The costs associated with hospitalization for Medicare beneficiaries with HF are substantial and are compounded by a high rate of readmission.
Keywords: heart failure, Medicare, health economics, hospitalization, costs
Introduction
Heart failure (HF) is a highly prevalent condition, associated with significant morbidity and a poor prognosis.1,2 Current estimates suggest that 6.2 million individuals are affected by HF in the USA, a number expected to rise to 8.5 million by 2030.3 The incidence of HF also increases significantly with age, with >60% of patients with HF aged ≥65 years.3 This is expected to have a significant impact on the prevalence of HF in the future because of the aging US population.3 In addition to the high and increasing prevalence, the prognosis of patients with HF is poor, with more than half of all patients with HF dying within 5 years of diagnosis.1,4 Consequently, care for patients with HF imposes a significant economic burden on the healthcare sector.3
Despite significant therapeutic advancements, patients with HF require frequent hospitalization for cardiovascular (CV) conditions such as uncontrolled hypertension, ischemia, arrhythmias, congestion, and hypervolemia, as well as non-CV comorbidities.5,6 Results from real-world observational studies have indicated that the majority of patients diagnosed with HF will be hospitalized at least once, and more than half will be hospitalized three or more times within 4–5 years of diagnosis.6 These hospitalizations are particularly resource-intensive; inpatient care has been estimated to cost $83,980 over the lifetime of each patient with HF.7 One study reported that almost 80% of the total lifetime costs associated with HF are accumulated during hospital stays.7
The economic burden of HF is further compounded by a particularly high readmission rate; almost 25% of patients with HF are readmitted within 30 days.8 The rate of readmission for conditions such as HF was of such concern that a requirement for the development of a readmission reduction program was included in the Affordable Care Act of 2010. Consequently, in 2012, the Hospital Readmission Reduction Program (HRRP) was introduced, which penalizes hospitals for excessive rates of readmission for HF, acute myocardial infarction (AMI), pneumonia, chronic obstructive pulmonary disease (COPD), coronary artery bypass graft (CABG) surgery, and hip or knee arthroplasty.9 Of these conditions, HF poses the highest risk for rehospitalization, with 2011–2014 data indicating a 30-day readmission rate of 22% for HF, compared with 30-day readmission rates of 17% for AMI, 16.9% for pneumonia, 4.8% for hip or knee arthroplasty (unplanned), 20.2% for COPD, and 14.9% for CABG surgery.10
Currently available information on the frequency and cost of hospitalization among Medicare beneficiaries varies significantly depending on the data source, the diagnostic criteria, and the specific parameters investigated. In addition, there has been limited published literature regarding the rate of HF-associated hospitalization among Medicare beneficiaries within the past 5 years. In this study, we used data from the national 5% sample of Medicare beneficiaries to investigate the rate of hospitalization, the average per-patient cost associated with each hospitalization, the 30-, 60-, and 90-day readmission rates, and the average length of stay per hospitalization among Medicare beneficiaries with HF.
Methods
Study design
This was a retrospective, observational study carried out using data from the national 5% sample of Medicare beneficiaries. The data were obtained from the Chronic Conditions Warehouse (www.ccwdata.org), which serves as the national repository for Center for Medicare and Medicaid Services (CMS) data. The study design was chosen for its feasibility and the large, nationally representative sample of HF hospitalizations.
Inpatient admission data for patients aged ≥65 years with at least one HF-related hospitalization between the dates of July 1, 2005, and December 31, 2011, were included in the analysis. The data were gathered from annual files containing eligibility, enrollment, demographic, and vital status information, and claims for all Medicare-covered services. These files included Medicare Part A files (inpatient, Skilled Nursing Facility [SNF]), Part B files (outpatient, home health, and noninstitutional), and Part D files (prescription drugs). The date of the patient’s first observed HF-associated hospitalization was identified as the index date; the data pertaining to the 6 months prior to this date (the pre-index period) and the data until the date of death, the end of continuous enrollment, or the end of the study period (whichever occurred first) were retained for analysis. This study was approved by the University of Alabama at Birmingham Institutional Review Board for Human Use and by the CMS Privacy Board. A waiver of consent was obtained; the investigators had no information on the identity of individuals whose data were provided by CMS.
Eligibility criteria
Patients were required to have at least one inpatient claim with HF (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] diagnosis code: 428.xx or 398.91) as the primary diagnosis between July 1, 2005, and December 31, 2010. Thus, for this study, the definition of HF included left ventricular, right ventricular, combined, and unspecified HF.
For the cost of hospitalization and the rate and length of stay analyses, patients had to have a minimum of 6 months of continuous enrollment in Medicare Parts A and B prior to the index date (to ensure the index admission was the incident event) and 36 months of continuous enrollment following the index month (unless the reason for having shorter follow-up was due to death). Individuals in Medicare Advantage (Part C) plans were excluded, because their claims tend to be missing or incomplete. For the readmission analysis, patients were required to have a minimum of 6 months of continuous enrollment in Medicare Parts A and B prior to the index date and 182 days of continuous enrollment following the index month (excluding decedents). Patients aged <65 years on the index date and any patients with evidence of HF (per the above-mentioned ICD-9-CM code) in the pre-index period were excluded. Individuals covered by Medicare who are aged <65 years are typically disabled or have end-stage renal disease and are not representative to the general population. Patients enrolled in Medicare Part C (Medicare Advantage) were also excluded because of incomplete claims data. We did not require Part D eligibility as inpatient drug costs are captured in the inpatient claims.
End points
The primary end point for this study was the average per-patient cost of HF-related, CV-related, and all-cause hospitalizations over the observation period for Medicare beneficiaries with HF. Secondary end points included the rate of HF-related, CV-related, and all-cause hospitalizations per year; the average length of hospital stay for HF-related, CV-related, and all-cause hospitalizations; and the cumulative 30-, 60-, and 90-day readmission rates following HF-related (ICD-9 diagnosis codes beginning 428 or 398.91), CV-related (ICD-9 codes beginning 390 through 459, excluding HF), and all-cause hospitalizations. CV-related conditions included all conditions listed as Diseases of the Circulatory System in ICD-9. These included rheumatic heart disease, hypertension, cardiac ischemia, other forms of heart disease, cerebrovascular disease, and diseases of the arterial and venous systems. All-cause hospitalizations included hospitalizations in an acute care facility for any disease or injury.
The results presented include costs for all end points unadjusted for hospital characteristics, patient demographics, comorbidities, or other factors. Distributions for beneficiary characteristics were calculated and reported for descriptive purposes.
All costs were inflated to $2,015 based on the medical care component of the Consumer Price Index, and the total cost of admission was estimated based on the expenditures paid for claims, including CMS reimbursements and health and patient’s co-insurance, co-payments, and deductibles. The estimation of costs from an all-payer perspective comes the closest, we believe, to capturing the economic costs of hospitalizations.
Results
Patient characteristics
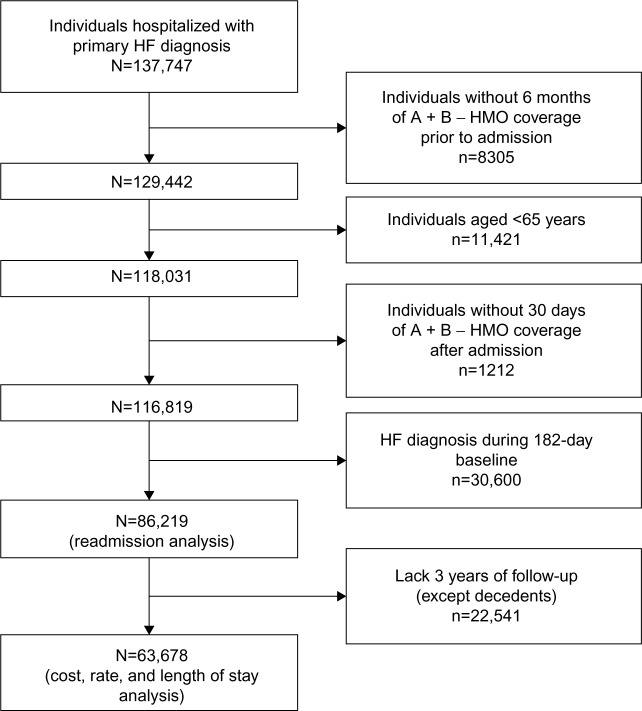
The demographic data and baseline characteristics of the 63,678 patients included in the study are summarized in Table 1. Patient selection is summarized in Figure 1. The majority of patients were female, white, and living in an urban area. The mean age was 81.8 (±8.1 SD) years. Data regarding comorbidities and medication usage in the pre-index period were available for approximately half of the population (35,788) because of their enrollment in Medicare Part D. For those patients without Part D coverage, accurate ascertainment of some comorbidities is problematic. Within this patient group, 64.6% had preexisting hypertension, 29.0% had diabetes, 21.6% had atrial fibrillation, and 2.2% had suffered a previous myocardial infarction. The majority of patients were receiving diuretics (62.3%) and/or β-blockers (58.8%), and 34.2% were receiving angiotensin-converting enzyme inhibitors. These drugs are routinely prescribed to patients with known HF and for those with risk factors for HF, such as hypertension.11
Table 1.
Demographics and baseline characteristics
| ll patients, N=63,678 | n (%) |
|---|---|
| Age cohort, years | |
| 65–69 | 5,424 (8.5) |
| 70–74 | 7,688 (12.1) |
| 75–79 | 10,731 (16.9) |
| 80–84 | 14,212 (22.3) |
| ≥85 | 25,623 (40.2) |
| Sex | |
| Female | 39,008 (61.3) |
| Male | 24,670 (38.7) |
| Race/ethnicity | |
| White | 55,962 (87.9) |
| Black | 5,422 (8.5) |
| Hispanic | 999 (1.6) |
| Other | 1,295 (2.1) |
| Population density | |
| Urban | 45,453 (71.4) |
| Rural | 18,042 (28.3) |
| Unknown | 183 (0.3) |
| US geographic region | |
| Northeast | 13,437 (21.1) |
| Midwest | 16,522 (25.9) |
| South | 25,395 (39.9) |
| West | 8,168 (12.8) |
| Patients enrolled in Medicare Part D (n=35,788) | |
| Comorbidities | |
| Diabetes | 10,391 (29.0) |
| Hypertension | 23,111 (64.6) |
| Stroke | 346 (1.0) |
| Atrial fibrillation | 7,737 (21.6) |
| Myocardial infarction | 790 (2.2) |
| Drug exposurea | |
| β-Blockers | 21,036 (58.8) |
| HF-specific β-blockers | 16,335 (45.6) |
| ACEIs | 12,254 (34.2) |
| ARBs | 6,356 (17.8) |
| Diuretics | 22,295 (62.3) |
| Aldosterone antagonists | 2,344 (6.6) |
| Digitalis/inotropes | 5,130 (14.3) |
Note:
Rate per 100 person-years.
Abbreviations: HF, heart failure; ACEIs, angiotensin converting enzyme inhibitors; ARBs angiotensin receptor blockers.
Figure 1.
Patient selection.
Abbreviations: HF, heart failure, HMO, Health Maintenance Organization.
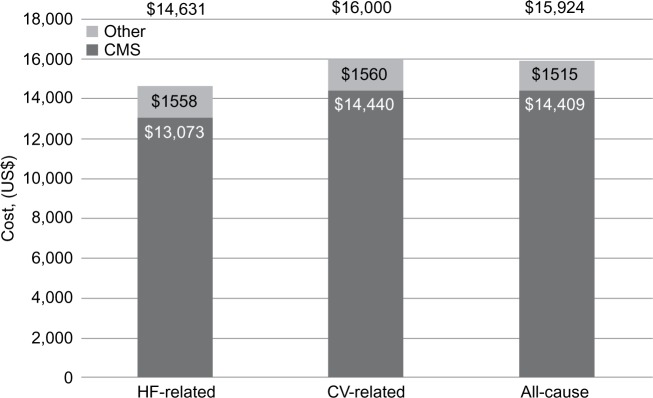
Costs of hospitalization
The total mean per-patient cost of a single HF-related hospitalization was calculated at $14,631, with $13,073 covered by CMS and $1,558 covered by other payers (Figure 2). The total per-patient mean costs associated with a single CV hospitalization and a single all-cause hospitalization were slightly higher, at $16,000 and $15,924, respectively.
Figure 2.
Hospitalization costs by type (mean).
Notes: Other, other insurance, deductibles, and copayments.
Abbreviations: CMS, Centers for Medicare and Medicaid Services; CV, cardiovascular; HF, heart failure.
Rates of hospitalization and length of stay
Over the study period, a total of 217,051 all-cause hospitalizations, including the index admission, were recorded. This correlates to a cumulative rate of hospitalization of 218.8 admissions per 100 person-years, indicating that, on average, each patient was hospitalized more than twice each year during the follow-up period. More than half of these hospitalizations were CV-associated, and 101,031 were attributable to HF (Table 2).
Table 2.
Cumulative hospitalization rate by type (including index admission) and average length of stay by type of hospitalization (days)
| Type of hospitalization | n | Cumulative ratea | LCL | UCL |
|---|---|---|---|---|
| HF | 101,031 | 101.8 | 101.2 | 102.5 |
| CV | 129,701 | 130.7 | 130.0 | 131.4 |
| All-cause | 217,051 | 218.8 | 217.8 | 219.7 |
|
| ||||
| Event | n | Mean (SD) | Median | |
|
| ||||
| HF | 101,031 | 7.07 (7.60) | 5 | |
| CV | 129,701 | 7.25 (8.18) | 5 | |
| All-cause | 217,051 | 7.53 (8.35) | 5 | |
Note:
Rate per 100 person-years.
Abbreviations: CV, cardiovascular; HF, heart failure; LCL, lower control limit; SD, standard deviation; UCL, upper control limit.
The mean length of stay for HF-related hospitalization was 7.07 days, which was slightly shorter than the mean CV-related and all-cause hospitalization length of stay of 7.25 and 7.53 days, respectively (Table 2). The median length of stay for all three hospitalization types was 5 days. For the 30-, 60-, and 90-day readmissions, the mean length of stay for any type of hospitalization remained consistent, ranging from 7.4 to 7.9 days.
Readmission rates
Readmission rates were calculated for 86,219 beneficiaries and encompassed any hospitalization occurring within 3 months of the index event. The cause of readmission was identified using ICD-9 diagnosis codes (ICD-9 codes beginning 428 or 398.91 were considered HF-related; ICD-9 codes beginning 390 through 459, excluding HF, were considered CV-related). The results indicated that 22.3% of patients were readmitted within 30 days, 33.3% were readmitted within 60 days, and 40.2% were readmitted within 90 days, for any cause (Table 3). Although more than half of these readmissions were CV-related, only approximately one-third of all readmissions were directly related to HF, with 30-, 60-, and 90-day readmission rates of 8.4%, 13.4%, and 16.7%, respectively (Table 3). When the 30- and 60-day readmission rates were analyzed by year, there was no evidence of a change in readmission rate over the study period investigated (Figure 3).
Table 3.
The 30-, 60-, and 90-day readmissions following hospitalization for HF
| Event | 30-day readmission | 60-day readmission | 90-day readmission |
|---|---|---|---|
| HF | |||
| Readmissions, n (%) | 11,296 (8.4) | 17,996 (13.4) | 22,382 (16.7) |
| Median days to readmission | 14 | 26 | 36 |
| Mean days to readmission (95% CI) | 14.9 (14.7–15.0) | 27.6 (27.3–27.8) | 39.2 (38.9–39.5) |
| Event rate, n (95% CI) | 1,225 (1,204–1,247) | 1,122 (1,107–1,137) | 1,035 (1,023–1,047) |
| CV | |||
| Readmissions, n (%) | 16,872 (12.6) | 26,408 (19.7) | 32,670 (24.3) |
| Median days to readmission | 14 | 26 | 36 |
| Mean days to readmission (95% CI) | 14.7 (14.6–14.8) | 27.4 (27.2–27.6) | 39.2 (38.9–39.4) |
| Event rate, n (95% CI) | 1,885 (1,858–1,913) | 1,734 (1,714–1,753) | 1,608 (1,592–1,623) |
| All-cause | |||
| Readmissions, n (%) | 29,998 (22.3) | 44,720 (33.3) | 54,000 (40.2) |
| Median days to readmission | 14 | 26 | 37 |
| Mean days to readmission (95% CI) | 14.6 (14.6–14.7) | 27.4 (27.3–27.6) | 39.6 (39.5–39.8) |
| Event rate, n (95% CI) | 3,642 (3,604–3,681) | 3,343 (3,316–3,370) | 3,082 (3,060–3,103) |
Abbreviations: CI, confidence interval; CV, cardiovascular; HF, heart failure.
Figure 3.
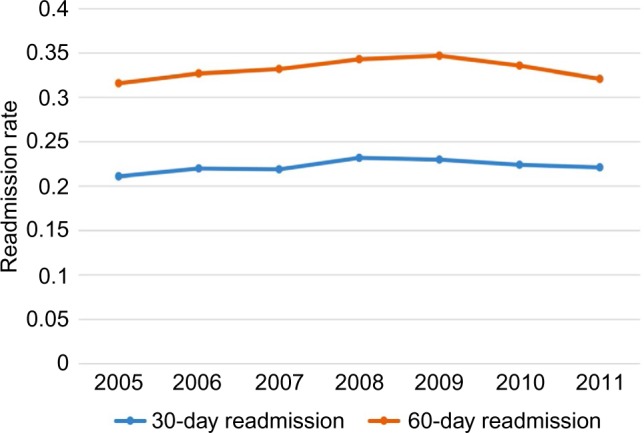
All-cause 30- and 60-day readmission rates by year.
Within the first 30 days, the mean and median number of days to readmission were similar regardless of hospitalization type, at between 14 and 15 days. Approximately 50% of readmissions occurred within 2 weeks of discharge. When the 60- and 90-day readmission results are considered, the relatively low median number of days to readmission (26 and 37, respectively) indicates that patients were more likely to be readmitted at an earlier stage. This is further supported by the decreasing numbers of patients readmitted within each subsequent 30-day period (29,998 readmitted within the first 30 days, 14,722 readmitted between days 31 and 60, and 9,280 readmitted between days 61 and 90).
Discussion
Our findings provide information on the costs associated with potentially avoidable HF hospitalizations, and thus the value of interventions that reduce hospitalization rates. We also examine rehospitalizations, providing information that can eventually be used to access the effects of Medicare’s Hospital Readmission Reductions Program, which specifically targets HF. The data also present more contemporaneous and generalizable cost data than do previous studies.6,12,13
In this study, data from the national 5% sample of Medicare beneficiaries were used to identify patients with a HF-related hospitalization. This allowed for an analysis of how costly hospitalizations following an HF diagnosis are, and how frequently patients are hospitalized following an initial event. The results indicated that the mean cost for HF-related hospitalization was $14,631, with slightly higher mean costs identified for CV-related and all-cause hospitalizations. These results suggest that patients with HF accrue significant hospitalization costs, not only for HF-related causes but also for other CV- and non-CV-related conditions. This is likely due to the high comorbidity load of patients with HF, with conditions such as COPD, renal disease, rheumatologic disease, and dementia known to be particularly costly.12
When the number of hospitalizations was analyzed within this study, a cumulative all-cause hospitalization rate of 218.8 per 100 person-years was identified, indicating that patients were admitted more than twice per year on average. This rate is substantially higher than that identified in 2009 by Dunlay et al – a hospitalization rate of 86.6 per 100 person-years following an HF diagnosis.6
However, it is difficult to compare results between studies because of differences in populations. For example, within this investigation, the data collected were from the National 5% Sample of Medicare Beneficiaries, the patients were predominantly female, the average age was 81.8 years, and patients were identified based on an initial hospitalization for HF. In contrast, the population included in the study published by Dunlay et al were only from Olmsted County, MN, were not necessarily Medicare patients, included an approximately equal number of males and females, had an average age of 76.8 years, and were identified based on medical records rather than by hospitalization.6 Additionally, in our study, the rate of hospitalizations included the index event, whereas the rate of hospitalization in the Olmsted County study excluded the initial hospitalization if the patient was first diagnosed during this hospitalization. This study was also based on more recent data than that used by Dunlay et al (2005–2011 vs 1987–2007)6 and, therefore, it is possible that the increasing rate of hospitalization identified reflects a genuine change. However, this seems unlikely, considering the stability of recent hospitalization trends.1
When these results are considered within the context of the cost of hospitalization identified within this study, patients with HF are likely to accrue a minimum of $34,000 in hospitalization costs per year. This result is substantially higher than that seen in a 2012 study by Greiner et al, in which the total medical costs accrued by Medicare beneficiaries within the year following an index admission for HF were identified as $22,124.13 As with the comparison of hospitalization rates, this difference may in part be due to differing populations or to the rising cost of medical care within the USA, as that study utilized data from 2003 to 2007.13
Within this study, all-cause 30-, 60-, and 90-day readmission rates following the index event were calculated as 22.3%, 33.3%, and 40.2%, respectively. These results are in accordance with previous studies identifying a 30-day readmission rate of up to 23.3%8,13 and a 90-day readmission rate of 39.2%.13 The low median number of days to readmission within each category and the declining number of patients readmitted over time suggest that patients were more likely to be readmitted soon after the initial hospitalization. Despite all patients having initially been hospitalized for HF, only just over half of these readmissions were CV-related, a result that can be explained by the high rate of comorbidities found in patients diagnosed with HF.14
The high rate of readmissions identified in patients with HF is a topic of increasing interest within the health care sector, as it represents an important target for lowering costs and improving outcomes in a patient population that requires a disproportionate amount of funding.15,16 The introduction of the HRRP in 2012 resulted in a substantial decline in readmission rates, as hospitals implemented readmission reduction strategies to avoid penalties.17 Although this falls outside of the period investigated in this study, the 30- and 60-day readmission rates were analyzed by year to ensure that the readmission results were not affected by the 2010 Affordable Care Act’s earlier stipulation that a readmission reduction program be developed. The lack of a discernible change in the 30- and 60-day readmission rates between 2009 and 2011 indicated that there was no early implementation of strategies involving the delay of readmission until after the 30-day period. Although patients with HF will always require frequent hospitalization because of the constant deterioration and high number of comorbidities associated with the condition, the adequate management of patients when they are initially hospitalized has the potential to vastly decrease readmission rates and, therefore, the costs associated with these hospitalizations. In addition to the economic burden, other studies have found substantial deleterious effects of HF on daily living and quality of life among persons living with HF. It is important not to lose track of the patient perspective when assessing the burden of disease.
Several limitations were associated with the use of the national 5% sample of Medicare beneficiaries claims database. 1) When we reviewed the claims, we were unable to differentiate reliably between systolic and diastolic HF. This is because the largest group of patients was classified as “Congestive heart failure, unspecified”. 2) Although a 6-month pre-index period was deemed necessary to ensure that the index admission was the incident event, the requirement for continuous enrollment during this period may have resulted in selection bias. 3) The readmission data excluded those who died during the identified follow-up period, with the remaining patients representing a slightly healthier population than the general HF population. An additional limitation was the exclusion of ~20% of patients who were enrolled in Medicare Advantage plans. These patients tend to be younger and have a lower severity of disease than those in the mainstream fee-for-service plans,18 indicating that the included patients may represent a population with poorer health than would be expected of the entire Medicare population. Similarly, the inclusion of ~50% of patients enrolled in Medicare Part D may have affected results, as these patients tend to receive different medications19 and may also represent a slightly different population.
Conclusion
In summary, we have identified that the costs associated with hospitalization in patients with HF are high. In addition, once patients are hospitalized for HF, they frequently require rehospitalization in the form of 30-, 60-, or 90-day readmissions following the initial HF-related hospitalization. The adequate management of Medicare beneficiaries prior to or during their initial hospitalization for HF has the potential to prevent costly hospital admissions, thereby resulting in significant cost savings and additional benefits to persons living with HF.
Acknowledgments
Writing and editorial support was provided by ApotheCom (San Francisco, CA, USA), which was funded by Amgen, Inc. (Thousand Oaks, CA, USA).
Footnotes
Author contributions
MK was responsible for conception and design of the study, data acquisition, and analysis and interpretation of data. PS performed data acquisition, analysis, and interpretation of data. AK, JM, and HKP were responsible for conception and design of the study and interpretation of data. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
MK and PS have previously received grants/research support from Amgen, Inc. HKP, AK, and JM are employees of Amgen, Inc. The authors report no other conflicts of interest in this work.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Juenger J, Schellberg D, Kraemer S, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart. 2002;87(3):235–241. doi: 10.1136/heart.87.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gheorghiade M, De Luca L, Fonarow GC, Filippatos G, Metra M, Francis GS. Pathophysiologic targets in the early phase of acute heart failure syndromes. Am J Cardiol. 2005;96(6A):11G–17G. doi: 10.1016/j.amjcard.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 5.Gheorghiade M, Zannad F, Sopko G, et al. Acute heart failure syndromes: current state and framework for future research. Circulation. 2005;112(25):3958–3968. doi: 10.1161/CIRCULATIONAHA.105.590091. [DOI] [PubMed] [Google Scholar]
- 6.Dunlay SM, Redfield MM, Weston SA, et al. Hospitalizations after heart failure diagnosis a community perspective. J Am Coll Cardiol. 2009;54(18):1695–1702. doi: 10.1016/j.jacc.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunlay SM, Shah ND, Shi Q, et al. Lifetime costs of medical care after heart failure diagnosis. Circ Cardiovasc Qual Outcomes. 2011;4(1):68–75. doi: 10.1161/CIRCOUTCOMES.110.957225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McHugh MD, Ma C. Hospital nursing and 30-day readmissions among Medicare patients with heart failure, acute myocardial infarction, and pneumonia. Med Care. 2013;51(1):52–59. doi: 10.1097/MLR.0b013e3182763284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Medicare & Medicaid Services Readmissions Reduction Program (HRRP) [Accessed May 16, 2016]. Available from: https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html.
- 10. Medicare.gov Readmissions and deaths-national. 2016. [Accessed May 16, 2016]. Available from: https://data.medicare.gov/Hospital-Compare/Readmissions-and-Deaths-National/qqw3-t4ie#.
- 11.World Health Organization Prevention of cardiovascular disease: guidelines for assessment and management of cardiovascular risk. [Accessed May 16, 2016]. Available from: http://www.who.int/cardiovascular_diseases/publications/Prevention_of_Cardiovascular_Disease/en/. Published August 2007.
- 12.Lang CC, Mancini DM. Non-cardiac comorbidities in chronic heart failure. Heart. 2007;93(6):665–671. doi: 10.1136/hrt.2005.068296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greiner MA, Hammill BG, Fonarow GC, et al. Predicting costs among Medicare beneficiaries with heart failure. Am J Cardiol. 2012;109(5):705–711. doi: 10.1016/j.amjcard.2011.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Deursen VM, Urso R, Laroche C, et al. Co-morbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail. 2014;16(1):103–111. doi: 10.1002/ejhf.30. [DOI] [PubMed] [Google Scholar]
- 15.Linden A, Adler-Milstein J. Medicare disease management in policy context. Health Care Financ Rev. 2008;29(3):1–11. [PMC free article] [PubMed] [Google Scholar]
- 16.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes. 2011;4(1):53–59. doi: 10.1161/CIRCOUTCOMES.110.950964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services Geographic variation public use file. [Accessed May 16, 2016]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Geographic-Variation/GV_PUF.html.
- 18.Friedman B, Jiang HJ, Russo CA. Medicare hospital stays: comparisons between the fee-for-service plan and alternative plans, 2006: Statistical Brief #66. [Accessed May 16, 2016]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK54559/ [PubMed]
- 19.Polinski JM, Donohue JM, Kilabuk E, Shrank WH. Medicare Part D’s effect on the under- and overuse of medications: a systematic review. J Am Geriatr Soc. 2011;59(10):1922–1933. doi: 10.1111/j.1532-5415.2011.03537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]