Abstract
Background
The Alberta Project Promoting active Living and healthy Eating in Schools (APPLE Schools) has been recognized as a “best practice” in preventing childhood obesity. To inform decision making on the economic implications of APPLE Schools and to justify investment, we evaluated the project’s cost-effectiveness following a life-course approach.
Methods
We developed a state transition model for the lifetime progression of body weight status comparing elementary school students attending APPLE Schools and control schools. This model quantified the lifetime impact of APPLE Schools in terms of prevention of excess body weight, chronic disease and improved quality-adjusted life years (QALY), from a school system’s cost perspective. Both costs and health outcomes were discounted to their present value using 3% discount rate.
Results
The incremental cost-effectiveness ratio(ICER) of APPLE schools was CA$33,421 per QALY gained, and CA$1,555, CA$1,709 and CA$14,218 per prevented person years of excess weight, obesity and chronic disease, respectively. These estimates show that APPLE Schools is cost effective at a threshold of ICER < CA$50,000.
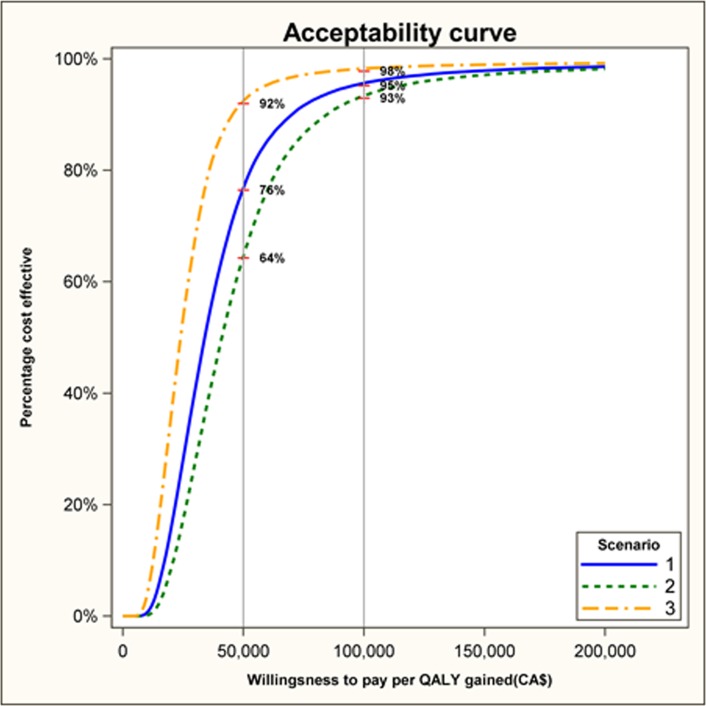
In probabilistic sensitivity analysis, APPLE Schools was cost effective more than 64% of the time per QALY gained, when using a threshold of ICER<CA$50,000, and more than 93% of the time when using a threshold of ICER<CA$100,000.
Conclusion
School-based health promotion, such as APPLE Schools is a cost-effective intervention for obesity prevention and reduction of chronic disease risk over the lifetime. Expanding the coverage and allocating resources towards school-based programs like the APPLE Schools program, is likely to reduce the public health burden of obesity and chronic diseases.
Introduction
Childhood obesity has become a public health priority in Canada and other developed countries [1]. Childhood obesity negatively affects children’s development and quality of life [2], and increases childhood health care costs[3]. It also increases the risk of obesity, chronic diseases and health care costs in adulthood [4]. Societal cost[5] estimates for obesity in Canada range from 1.27 to 11.08 billion Canadian dollars annually[6]. An estimated 2.2% to 12.0% of Canada’s total health care expenditures are consequences of excess body weight [6].
Inadequate physical activity and poor nutrition are underlying causes of obesity [7]. Promotion of active living and healthy eating is considered more effective when targeting children, and schools have been suggested as an ideal setting for health promotion as this is the place to reach nearly all children [8–12]. In 2005, we reported on a successful school-based project that achieved a reduction in the prevalence of excess bodyweight among children in Nova Scotia, Canada [13, 14]. The successful project was recognized as a “best practice” in Canada and inspired the development of the Alberta Project Promoting active Living and healthy Eating (APPLE) Schools in another Canadian jurisdiction [8]. APPLE Schools project was also successful in improving diets and physical activity levels, and in reducing obesity rates [8, 15]. Despite the recognition as ‘best practice’, public health decision makers have been hesitant to invest in large scale applications. They desire evidence on the long-term benefits such as prevention of obesity throughout adulthood and reduction in chronic diseases. Public health decision makers are particularly interested in program costs and potential cost savings resulting from avoided health care costs.
In a recent systematic review of economic evaluations of health promotion programs for children and adolescents, Korber[16] identified twelve economic evaluations of school-based programs in developed countries. However, none of these studies had been conducted in Canada, yet ‘local’ evidence is key to public health decision makers because countries differ with respect to both educational and health care sytems [6]. To better inform public health decision makers, we conducted an incremental cost-effectiveness analysis of the APPLE school program comparing the lifetime health outcomes to the program costs compared to an alternative where no program exists.
Methods
We developed a Markov model to estimate the incremental cost-effectiveness ratio (ICER) for two strategies: APPLE Schools (the intervention program) compared to general schools (No intervention). The ICER was calculated by dividing the incremental cost of the school program by the incremental outcomes throughout the lifetime up to 80 years among male and 84 years among female (i.e ICER = [program cost-0]/[outcome with intervention program–outcome with No intervention program]). The outcomes considered were excess body weight (i.e., overweight and obesity), obesity, chronic disease and quality-adjusted life years (QALY). The QALY outcome combines the changes in both mortality (life years) and the health related quality of life due to morbidity. The $50,000 per QALY willingness-to-pay threshold has been an arbitrary decision rule since 1992 and is still used by many to determine if an intervention is cost-effective[17]. Based on the study of Shiroiwa et al. (2010)[18], $100,000 per QALY was chosen as a threshold for weak evidence of cost-effectiveness.
The intervention program
Details of the intervention program are presented elsewhere [8, 19, 20]. In briefly, the APPLE Schools intervention involved having a full-time School Health Facilitator in each school for two years to implement healthy eating and active living policies, practices and strategies while engaging students, parents, school staff and other stakeholders. With the objective of changing the “school culture” to make the healthy choice the easy choice, the SHF facilitator contributed to the schools' health curriculum, both during instructional and non-instructional school time, developed cross curriculum links, and facilitated professional development days for teachers and school staff. Examples of activities include nutrition programs such as cooking clubs and healthy breakfast, lunch and snack programs, after school physical activity programs, walk-to-school days, community gardens, weekend events, school newsletters and daily health announcements. While the intervention was school wide, the evaluation focused on grade five students (about 10 years of age) [8]. The same surveys and measurements, including height and weight, were conducted in a sample of 148 randomly selected schools in Alberta allowing for a comparison of changes in APPLE Schools with average changes in control schools, as described in detail elsewhere [8].
Conceptual framework and modeling approach
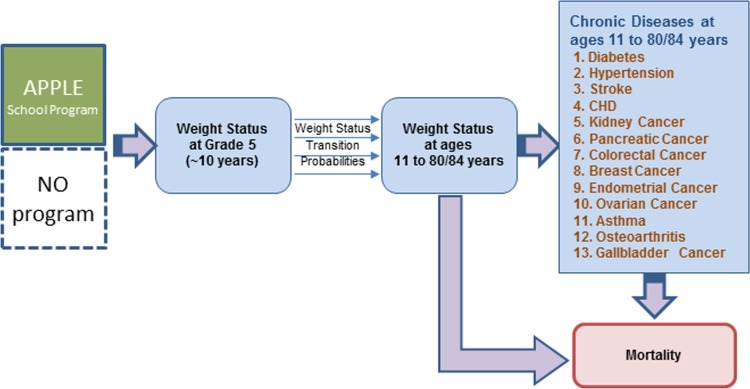
The conceptual framework for evaluating lifetime benefits of students attending APPLE Schools was based on evidence that body weight status at young age determines body weight in adulthood which in turn determines the risk of chronic conditions and health related quality of life [21–25]. Therefore, the effect of APPLE Schools, which was expressed in changes in weight status distribution of grade 5 students attending APPLE Schools relative to those attending control schools, was expected to affect lifetime weight status trajectories and risk of chronic diseases (Fig 1).
Fig 1. Model conceptual framework.
Note: 80 and 84 are the life-expectancies at birth in British Columbia (the highest of all Canadian provinces) for men and women, respectively [26].
We assumed that the ‘school culture’ and lifestyle developed in the two intervention years would continue for another eight years. The model is therefore, based on 10 cohorts of students who pass through grade 5 over a 10-year period.
The model included 43 states based on 3 weight status categories (normal weight, overweight, and obesity), 13 chronic diseases with established links to weight status (i.e Diabetes, Hypertension, Asthma, Osteoarthritis, Stroke, Coronary Heart Disease (CHD), Kidney cancer, Pancreatic cancer, Colorectal cancer, Breast cancer, Endometrial cancer, Ovarian cancer, and Gallbladder cancer) [27], no-chronic disease state and the dead state.
Because school based programs in Canada are mainly funded by the education system, the modeling was carried out from the school system’s cost perspective and was implemented in TreeAge Pro 2016 software [28].
Model inputs
Weight status transition probabilities
We obtained estimates of these probabilities from analysis of longitudinal data from two Canadian cohorts: 1) the National Population Health Survey(NPHS) that follows participants 12 years of age or older, and 2) the National Longitudinal Survey of Children and Youth (NLSCY) that follows children under 12 years of age. In both cohorts, data were collected from participants every 2 years. A multinomial logistic regression model (which allows for more than two levels of the outcome variable) was fitted to data from the two cohorts. The independent variables/covariates in this model were; sex, weight status and age at a given time point, and the outcome was weight status in the next assessment (2 years later). Parameter estimates of the fitted multinomial logistic regression model (S1 Table) were then used in the Markov model to obtain sex and age specific weight status transition probabilities.
Conditional probability of dying given weight status and chronic disease status
We estimated these probabilities based on general Canadian population mortality hazards by sex and age extracted from the Canadian Life table [26] and the effects of weight status (S2 Table) [29] and chronic diseases (S3 Table) [30–35] on all-cause mortality. Because the effects of weights status and chronic diseases on all-cause mortality were not estimated relative to the general population, the weight status distribution (S4 Table)[36] and prevalence of the various chronic diseases(S5 Table)[37–39], were also considered in the estimation.
At each cycle (age), the sex, age and weight status specific mortality hazard was estimated using the equation:
Where
hw,s,a – Conditional probability of dying in 1 year given weight status(w), sex(s) and age(a)
RRw,s,a—Relative risk of dying for weight status w, given sex and age ((Normal weight being the reference status)
Pw,s,a—Proportion of individuals who are in weight status w, given sex and age.
Hs,a – Mortality hazard given sex and age, obtained from the Canadian life table
This estimation approach was used for all relative risks/rate ratios for which the reference category was not the general population, including in the estimation of the conditional probability of dying given chronic disease status (using S3 and S5 Tables) and conditional probability of developing a chronic disease given weight status(using S4, S6 and S7 Tables).
For each given combination of weight status and chronic disease state, we used the higher of the two estimated probabilities of dying, because we did not have estimates of the interaction effects between weight status and chronic diseases.
Probabilities of developing chronic diseases
We estimated these probabilities from published data on incidence rates of chronic diseases (S6 Table) [31, 40–45], the effects of weight status on incidence of these chronic diseases from a meta-analysis by Guh et al (S7 Table) [27] and weight status distribution (S4 Table)[36]. We considered only chronic diseases for which the meta-analysis found a significant effect including Diabetes, Hypertension, Stroke, Coronary artery disease, Asthma, Osteoarthritis and 7 cancers (Kidney, Pancreatic, Colorectal, Breast, Endometrial, Ovarian and Gallbladder) (S7 Table) [27].
Effect of APPLE schools on weight status of grade 5 students
We estimated the effect of the APPLE schools from analysis of weight status data obtained from grade 5 students attending APPLE and Non-APPLE Schools in the years 2008 and 2010. Based on a multinomial logistic regression model, APPLE Schools were estimated to reduce the odds of obesity over normal weight by 0.723 times per year (OR = 0.723, 95%CI: 0.553–0.946) in the two years of program implementation.
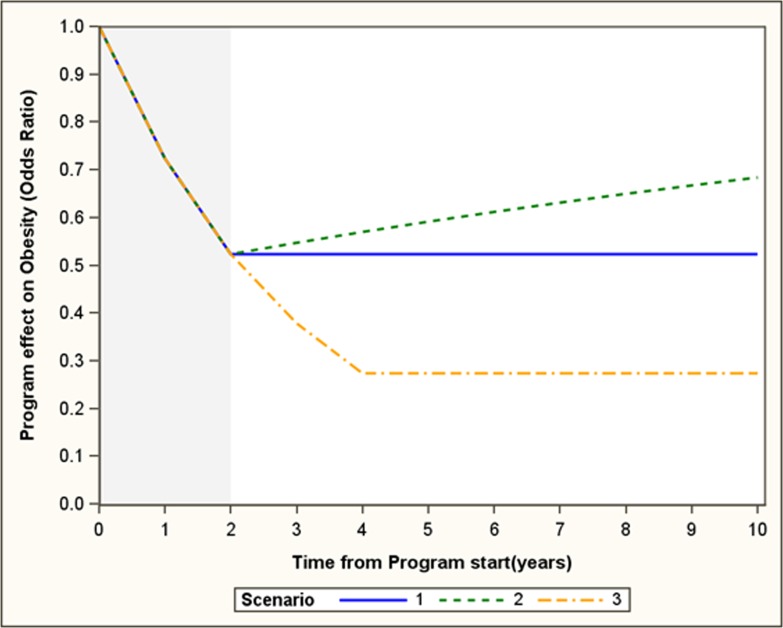
Because the effect of the program was expected to continue for another 8 years, we considered three scenarios for the sustainability of the program effect after the two intervention years (Fig 2):
Fig 2. APPLE schools effects sustainability scenarios.
Scenarios: 1-The annual decline in obesity is maintained for the 2 intervention years then remains at the level reached in 2 years for another 8 years 2- After the two intervention years, the effect starts waning by 5% per year 3- The annual decline in obesity is maintained for 4 years then remains at the level reached in 4 years for another 6 years.
The annual decline in obesity is maintained for the 2 intervention years then remains at the level reached in 2 years for another 8 years(base scenario)
After the two intervention years, the effect wanes by 5% per year
The annual decline in obesity is maintained for 4 years then remains at the level reached in 4 years for another 6 years
Program costs
Using program accounts, we estimated the cost of APPLE Schools in the two year period (2008–2010) to be CA$284 per student per year in 2008 Canadian dollars (S9 Table). This estimate included all salaries of School Health Facilitators and managers, costs of professional development, programming, travel, and research costs.
The ICERs are reported in 2008 Canadian dollars. However for comparison with other published estimates, a conversation to 2011 US dollars was also carried out using estimates of National Consumer Price Indices (CPI) and Purchasing Power Parities (PPP) published by Organisation for Economic Co-operation and Development (OECD) [46, 47].
Outcomes
We estimated the four outcome measures that were included in the model as person years of excess body weight (i.e., overweight and obesity), person years of obesity, person years with chronic diseases and QALY. For every year lived with excess weight, obesity or chronic disease we assigned a decrement in health utility scores producing QALYs lived with the condition. The estimated decrements in health utility score were obtained from previously published estimates from Schultz et al [48] and Jia et al [49] (S8 Table). Though the decrements estimated by Jia et al were based on participants who were 18 years of age or older, we applied the same decrements for children under 18 years as well. For each given combination of weight status and chronic disease Markov state, we used the higher of the two QALY decrement estimates (weight status or chronic disease).
Discounting
All future costs (10 years) and health outcomes (up to 84 years) were discounted to their present values using annual discount rate of 3%[50].
Sensitivity analyses
We conducted a number of sensitivity analyses to examine the robustness of the Markov model. In two-way sensitivity analysis, we varied the program effect scenario and discounting rate (0% and 5%).
We also performed probabilistic sensitivity analysis (PSA) to incorporate uncertainties in all model parameters simultaneously [51, 52]. In PSA, Relative risks and Odds ratios were assumed to follow log-normal distributions and parameters of the multinomial logistic regression model for weight status transitions were assumed to follow a normal distribution. Program costs were assumed to follow a gamma distribution and to have a coefficient of variation of 10%. In PSA, each model parameter was assigned a value drawn randomly from its distribution. We carried out 50,000 simulations of the model for each combination of scenario and outcome.
Ethical consideration
This study has been reviewed and approved by the Health Research Ethics Board of the University of Alberta, Edmonton, Alberta, Canada (Protocol numbers: Pro0003799 and Pro00003800). Parents of the students who participated in the study had provided written informed consent and the students assented to the surveys and assessments of weight and height.
Results
The estimated ICERs of APPLE Schools are presented in Table 1. In scenario 1 and assuming a discount rate of 3%, the model estimated that for every 10 children, 1.26 person years of excess weight (including 1.15 person years of obesity) and 0.14 person years of chronic disease would be prevented in their lifetime. This would correspond to a gain of 0.06 QALYs. In this scenario the ICER was estimated to be CA$1,555 per person year of excess weight prevented, CA$1,709 per person year of obesity prevented and CA$33,421 per QALY gained. Scenario 2 that assumed 5% annual reduction in the achieved effect after two years, the outcomes were slightly smaller leading to ICER of CA$40,396 per QALY gained. Contrary, scenario 3 that assumed 4 years of obesity decline the outcomes were higher resulting in an ICER of CA$23,216 per QALY gained.
Table 1. Cost-effectiveness of APPLE schools.
| YEARS WITH EXCESS WEIGHT | YEARS WITH OBESITY | YEARS WITH CHRONIC DISEASE | QALYs | ||||||
|---|---|---|---|---|---|---|---|---|---|
| SCENARIO | Incremental Cost* | Incremental Effect* | ICER | Incremental Effect* | ICER | Incremental Effect* | ICER | Incremental Effect* | ICER |
| Discount = 3%—Base results | |||||||||
| 1 | 1963.2 | -1.26 | 1,555 | -1.15 | 1,709 | -0.14 | 14,218 | 0.06 | 33,421 |
| 2 | 1963.2 | -1.04 | 1,880 | -0.95 | 2,065 | -0.11 | 17,185 | 0.05 | 40,396 |
| 3 | 1963.2 | -1.82 | 1,081 | -1.65 | 1,187 | -0.20 | 9,878 | 0.08 | 23,216 |
| Discount = 0% | |||||||||
| 1 | 1988.0 | -1.52 | 1,312 | -1.36 | 1,464 | -0.26 | 7,599 | 0.07 | 28,530 |
| 2 | 1988.0 | -1.25 | 1,586 | -1.12 | 1,770 | -0.22 | 9,185 | 0.06 | 34,485 |
| 3 | 1988.0 | -2.18 | 911 | -1.95 | 1,017 | -0.38 | 5,279 | 0.10 | 19,819 |
| Discount = 1% | |||||||||
| 1 | 1979.6 | -1.42 | 1,398 | -1.28 | 1,552 | -0.21 | 9,534 | 0.07 | 30,102 |
| 2 | 1979.6 | -1.17 | 1,689 | -1.06 | 1,876 | -0.17 | 11,524 | 0.05 | 36,386 |
| 3 | 1979.6 | -2.04 | 971 | -1.84 | 1,078 | -0.30 | 6,624 | 0.09 | 20,911 |
| Discount = 2% | |||||||||
| 1 | 1971.3 | -1.33 | 1,479 | -1.21 | 1,633 | -0.17 | 11,742 | 0.06 | 31,761 |
| 2 | 1971.3 | -1.10 | 1,787 | -1.00 | 1,974 | -0.14 | 14,192 | 0.05 | 38,390 |
| 3 | 1971.3 | -1.92 | 1,027 | -1.74 | 1,135 | -0.24 | 8,158 | 0.09 | 22,063 |
| Discount = 4% | |||||||||
| 1 | 1955.2 | -1.20 | 1,629 | -1.10 | 1,779 | -0.12 | 16,954 | 0.06 | 35,037 |
| 2 | 1955.2 | -0.99 | 1,968 | -0.91 | 2,150 | -0.10 | 20,492 | 0.05 | 42,350 |
| 3 | 1955.2 | -1.73 | 1,131 | -1.58 | 1,236 | -0.17 | 11,779 | 0.08 | 24,339 |
| Discount = 5% | |||||||||
| 1 | 1947.4 | -1.15 | 1,698 | -1.06 | 1,844 | -0.10 | 19,938 | 0.05 | 36,590 |
| 2 | 1947.4 | -0.95 | 2,053 | -0.87 | 2,229 | -0.08 | 24,099 | 0.04 | 44,227 |
| 3 | 1947.4 | -1.65 | 1,180 | -1.52 | 1,281 | -0.14 | 13,852 | 0.08 | 25,417 |
*per 10 children (1 from each of the 10 grade 5 cohorts).
Scenarios: 1-The annual decline in obesity is maintained for the 2 intervention years then remains at the level reached in 2 years for another 8 years; 2- After the two intervention years, the effect starts waning by 5% per year; 3- The annual decline in obesity is maintained for 4 years then remains at the level reached in 4 years for another 6 years
Results of probabilistic sensitivity analysis (Fig 3), showed that this program has a high probability of being cost-effective based on the CA$50,000/QALY threshold, 76%, 64% and 92% in scenarios 1, 2, and 3, respectively. When using the CA$100,000 threshold, the corresponding estimates were, 95%, 93% and 98% of the time for scenario 1, 2 and 3, respectively (Fig 3).
Fig 3. Probabilistic sensitivity analysis.
Scenarios: 1-The annual decline in obesity is maintained for the 2 intervention years then remains at the level reached in 2 years for another 8 years 2- After the two intervention years, the effect starts waning by 5% per year 3- The annual decline in obesity is maintained for 4 years then remains at the level reached in 4 years for another 6 years.
Discussion
We took a life course approach to evaluate the cost-effectiveness of APPLE Schools and showed that this program would generally be considered cost-effective at commonly cited threshold levels. In our base scenario, the ICER of APPLE Schools was estimated to be CA$1,555 per person year of excess weight prevented, CA$1,709 per person year of obesity prevented and CA$33,421 per QALY gained. Sensitivity analyses, showed that the APPLE schools program was cost effective (ICER ≤CA$100,000), 95% of the time per QALY gained in the first scenario and that the two alternative scenarios produced estimates that were not substantially different.
To the best of our knowledge, this is the first study to show cost effectiveness of a school-based health promotion in Canada. As countries and jurisdictions vary in their educational and health care systems, the present findings are particularly relevant to public health decision makers in Canada.
Our findings are consistent with previous economic evaluations of school-based programs for the prevention of obesity in other countries. In a recent systematic review, Korber estimated cost-effectiveness ratios for various school-based programs from a societal perspective, ranging from US$1,073 to US$669,1380 per QALY/DALY gained (in 2011 US dollars) [16]. The cost-effectiveness ratios were generally higher for evaluations based on longer time-horizons compared to those based on shorter time horizons. In programs evaluated on a lifetime, as we did, the cost effectiveness ratios ranged from US$15,478 to US$669,138 per QALY/DALY gained. At a threshhold of US$100,000 per QALY gained, three of these programs (Moodie et al 2013 = US$15,478; Rush et al 2014 = US$16,571 and Moodie et al 2010 = US$72,197) would be considered cost effective and two would not be cost-effective (Moodie et al 2011 = US$103,012 and Moodie et al 2009 = US$669,138) [16]. In comparison, our estimated cost-effective ratio for APPLE schools in 2011 US dollars, would be about US$28,302 per QALY gained, which is cost-effective at a threshold of US$100,000 per QALY gained.
In contrast, programs that were evaluated in a shorter time-horizon (10 to 25 years), had estimated cost effectiveness ratios (in 2011 US dollars) ranging from US$1,073 to US$6,179 per QALY gained (Brown et al 2007 = US$1,073; Wang et al 2011 = US$3,061 and Wang et al 2003 = US$6,179).
We showed APPLE Schools to be cost effective despite our evaluation being based on only its effect through changes in BMI without considering other positive outcomes of the program. For example, we miss the effects of reduction in salt on hypertension. We also did not consider cost savings associated with avoided health care services. Their consideration would have resulted in even stronger estimates for cost-effectiveness.
Furthermore, we also miss the health benefits that may arise from improvements in knowledge of health, attitudes, self-efficacy and leadership that are also targeted by the APPLE Schools [53–55]. Therefore, our estimates for the cost effectiveness ratio per QALY gained may be conservative. In addition, we also missed the benefit received by students who were in grade 6 when the APPLE schools started, because we only evaluated student cohorts at grade 5. Furthermore, our evaluation was based on only chronic diseases for which a published meta-analysis had shown significant relationships with weight status [27].
The study also has other limitations to be acknowledged. Whereas heights and weights of students attending APPLE Schools and general schools were measured, heights and weights from the surveys that were used to model the life course weight status transitions were self-reported. In addition, the quantification of effectiveness in this study was based on ecological change in the distribution of weight status of grade 5 students. We did not examine the effect of the program at individual level, because we did not follow the same students over time.
As with most analytical models, economic evaluation models are a simplification of reality with a number of assumptions and model inputs obtained from various sources[56]. Though we used probabilistic sensitivity analysis to address uncertainty in model input parameters, it cannot take into account all the possible sources of uncertainty [52].
In conclusion, based on our modeling approach, APPLE Schools appears to be a cost-effective intervention for obesity prevention and reduction of chronic disease risk over the lifetime of children attending APPLE Schools. Expanding the coverage and allocating resources towards school-based programs like the APPLE schools program, is likely to reduce the public health burden of obesity and chronic diseases.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We thank all of the grade five students, parents and schools for their participation in the REAL Kids Alberta evaluation and the APPLE Schools program, and the evaluation assistants, health promotion coordinators and school health facilitators for their contributions in data collection. We also thank Ms. Irene Wong of Statistics Canada for providing assistance and access to data from the NPHS and the NLSCY surveys.
Data Availability
The approval for REAL kids Alberta schools evaluation was granted by the Health Research Ethics Board at the University of Alberta on the basis that all data would be kept confidential and would be stored and used in adherence to the guidelines established by the University. For these reasons, REAL kids Alberta data used to estimate the effect of the APPLE Schools are available upon request and requests can be made by contacting the Primary Investigator of the study, Dr. Paul Veugelers. The Health Research Ethics Board at the University of Alberta can be contacted at: Research Ethics Office; 308 Campus Tower; 8625 – 112 Street; Edmonton, AB T6G 1K8; Phone: 1.780.492.0459; Email: reoffice@ualberta.ca. The Research Ethics Office assigned Pro00003799 (REAL Kids Alberta) and Pro00003800 (APPLE Schools) as protocol numbers of the studies that collected data that were used in the present study. Data from the National Population Health Survey (NPHS) and the National Longitudinal Survey of Children and Youth (NLSCY) are owned by Statistics Canada and are available from Statistics Canada Research Data Centers for researchers who meet the criteria for access to confidential data. Statistics Canada has an established protocol for researchers to access their data: Researchers have to submit an application and if the application is approved, the applicants have to undergo security screening. After getting security clearance, researchers get to access data in a secure Statistics Canada Research Data Center (RDC). All analyses have to be done at the RDC and only results are allowed to be taken out after vetting by the RDC. Raw data cannot be taken out of the RDC. Further details on the process of accessing Statistics Canada data are available at the following link: http://www.statcan.gc.ca/eng/rdc/programresearchacademic. To access the NPHS and NLSCY data we had to go through the following process: (1) We wrote a proposal for a program of research; (2) We completed the online application form through the Social Sciences and Humanities Research Council (SSHRC) website: https://webapps.nserc.ca/SSHRC/faces/logon.jsp?lang=en_CA; (3) After getting approval for the research program, we had to complete a security screening process. After which we signed a microdata research contract with Statistics Canada; (4) We were then given permission to access data at the Statistics Canada Research Data Centre (RDC) at the University of Alberta. We carried out all the analyses at the RDC and were allowed to take out results after being vetted by the RDC. All other model inputs that were obtained from published literature are provided in accompanying Supporting Information tables.
Funding Statement
The present study was funded through the Collaborative Research and Innovation Opportunities (CRIO) Team program from Alberta Innovates Health Solutions awarded to Paul J. Veugelers (PJV) and Arto Ohinmaa (AO). J. A. Johnson is a Centennial Professor with the School of Public Health. The REAL kids Alberta evaluation was funded through a contract with Alberta Health. APPLE Schools was funded through a philanthropic donation to the School of Public Health at the University of Alberta. The research was funded by an operating grant by the Canadian Institutes for Health Research, Heart and Stroke Foundation of Canada and Canadian Population Health Initiative and a Canada Research Chair in Population Health and AIHS Health Scholarship to Dr. Paul J. Veugelers. All interpretations and opinions in the present study are those of the authors.
References
- 1.Malecka-Tendera E, Mazur A. Childhood obesity: a pandemic of the twenty-first century. Int J Obes (Lond). 2006;30 Suppl 2:S1–3. Epub 2006/05/30. [DOI] [PubMed] [Google Scholar]
- 2.WHO/TB/97.224. WHO report on the tuberculosis epidemic 1997. Use DOTS more widely. 1997;Geneva.
- 3.Kuhle S, Kirk S, Ohinmaa A, Yasui Y, Allen AC, Veugelers PJ. Use and cost of health services among overweight and obese Canadian children. Int J Pediatr Obes. 2011;6(2):142–8. doi: 10.3109/17477166.2010.486834 [DOI] [PubMed] [Google Scholar]
- 4.Anis AH, Zhang W, Bansback N, Guh DP, Amarsi Z, Birmingham CL. Obesity and overweight in Canada: an updated cost-of-illness study. Obes Rev. 2009;11(1):31–40. Epub 2009/05/06. doi: 10.1111/j.1467-789X.2009.00579.x [DOI] [PubMed] [Google Scholar]
- 5.Birmingham CL, Muller JL, Palepu A, Spinelli JJ, Anis AH. The cost of obesity in Canada. CMAJ. 1999;160(4):483–8. PubMed Central PMCID: PMC1230073. [PMC free article] [PubMed] [Google Scholar]
- 6.Tran BX, Nair AV, Kuhle S, Ohinmaa A, Veugelers PJ. Cost analyses of obesity in Canada: scope, quality, and implications. Cost effectiveness and resource allocation: C/E. 2013;11(1):3 Epub 2013/02/12. doi: 10.1186/1478-7547-11-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naukkarinen J, Rissanen A, Kaprio J, Pietilainen KH. Causes and consequences of obesity: the contribution of recent twin studies. Int J Obes (Lond). 2012;36(8):1017–24. Epub 2011/10/12. [DOI] [PubMed] [Google Scholar]
- 8.Fung C, Kuhle S, Lu C, Purcell M, Schwartz M, Storey K, et al. From "best practice" to "next practice": the effectiveness of school-based health promotion in improving healthy eating and physical activity and preventing childhood obesity. Int J Behav Nutr Phys Act. 2012;9:27 PubMed Central PMCID: PMC3414762. doi: 10.1186/1479-5868-9-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McAuley KA, Taylor RW, Farmer VL, Hansen P, Williams SM, Booker CS, et al. Economic evaluation of a community-based obesity prevention program in children: the APPLE project. Obesity (Silver Spring). 2010;18(1):131–6. Epub 2009/05/16. [DOI] [PubMed] [Google Scholar]
- 10.Moodie M, Haby M, Galvin L, Swinburn B, Carter R. Cost-effectiveness of active transport for primary school children—Walking School Bus program. Int J Behav Nutr Phys Act. 2009;6:63 Epub 2009/09/15. PubMed Central PMCID: PMC2758827. doi: 10.1186/1479-5868-6-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang LY, Gutin B, Barbeau P, Moore JB, Hanes J Jr., Johnson MH, et al. Cost-effectiveness of a school-based obesity prevention program. The Journal of school health. 2008;78(12):619–24. Epub 2008/11/13. doi: 10.1111/j.1746-1561.2008.00357.x [DOI] [PubMed] [Google Scholar]
- 12.Wang LY, Yang Q, Lowry R, Wechsler H. Economic analysis of a school-based obesity prevention program. Obes Res. 2003;11(11):1313–24. doi: 10.1038/oby.2003.178 [DOI] [PubMed] [Google Scholar]
- 13.Veugelers PJ, Fitzgerald AL. Prevalence of and risk factors for childhood overweight and obesity. CMAJ. 2005;173(6):607–13. Epub 2005/09/15. PubMed Central PMCID: PMC1197160. doi: 10.1503/cmaj.050445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Veugelers PJ, Fitzgerald AL. Effectiveness of school programs in preventing childhood obesity: a multilevel comparison. American journal of public health. 2005;95(3):432–5. Epub 2005/02/25. PubMed Central PMCID: PMC1449197. doi: 10.2105/AJPH.2004.045898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vander Ploeg KA, McGavock J, Maximova K, Veugelers PJ. School-based health promotion and physical activity during and after school hours. Pediatrics. 2014;133(2):e371–8. doi: 10.1542/peds.2013-2383 [DOI] [PubMed] [Google Scholar]
- 16.Korber K. Quality assessment of economic evaluations of health promotion programs for children and adolescents-a systematic review using the example of physical activity. Health Econ Rev. 2015;5(1):35 PubMed Central PMCID: PMCPMC4658341. doi: 10.1186/s13561-015-0071-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grosse SD. Assessing cost-effectiveness in healthcare: history of the $50,000 per QALY threshold. Expert Rev Pharmacoecon Outcomes Res. 2008;8(2):165–78. doi: 10.1586/14737167.8.2.165 [DOI] [PubMed] [Google Scholar]
- 18.Shiroiwa T, Sung YK, Fukuda T, Lang HC, Bae SC, Tsutani K. International survey on willingness-to-pay (WTP) for one additional QALY gained: what is the threshold of cost effectiveness? Health economics. 2010;19(4):422–37. Epub 2009/04/22. doi: 10.1002/hec.1481 [DOI] [PubMed] [Google Scholar]
- 19.Tran BX, Ohinmaa A, Kuhle S, Johnson JA, Veugelers PJ. Life course impact of school-based promotion of healthy eating and active living to prevent childhood obesity. PLoS One. 2014;9(7):e102242 PubMed Central PMCID: PMC4099303. doi: 10.1371/journal.pone.0102242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tran B, Ohinmaa A, Kuhle S, Johnson JA, Veugelers P. Cost-Effectiveness of School-Based Health Promotion in Canada: A Life-Course Modeling Approach. Value in Health. 16(7):A391. [Google Scholar]
- 21.Venn AJ, Thomson RJ, Schmidt MD, Cleland VJ, Curry BA, Gennat HC, et al. Overweight and obesity from childhood to adulthood: a follow-up of participants in the 1985 Australian Schools Health and Fitness Survey. The Medical journal of Australia. 2007;186(9):458–60. Epub 2007/05/09. [DOI] [PubMed] [Google Scholar]
- 22.Starc G, Strel J. Tracking excess weight and obesity from childhood to young adulthood: a 12-year prospective cohort study in Slovenia. Public Health Nutr. 2011;14(1):49–55. Epub 2010/04/16. doi: 10.1017/S1368980010000741 [DOI] [PubMed] [Google Scholar]
- 23.Park MH, Falconer C, Viner RM, Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev. 2012;13(11):985–1000. Epub 2012/06/27. doi: 10.1111/j.1467-789X.2012.01015.x [DOI] [PubMed] [Google Scholar]
- 24.Lhachimi SK, Nusselder WJ, Lobstein TJ, Smit HA, Baili P, Bennett K, et al. Modelling obesity outcomes: reducing obesity risk in adulthood may have greater impact than reducing obesity prevalence in childhood. Obes Rev. 2013. Epub 2013/04/23. [DOI] [PubMed] [Google Scholar]
- 25.Lehnert T, Sonntag D, Konnopka A, Riedel-Heller S, Konig HH. The long-term cost-effectiveness of obesity prevention interventions: systematic literature review. Obes Rev. 2012;13(6):537–53. Epub 2012/01/19. doi: 10.1111/j.1467-789X.2011.00980.x [DOI] [PubMed] [Google Scholar]
- 26.Statistics Canada. Table 053–0003—Elements of the life table, Canada, provinces and territories, annual (2009/20011), CANSIM (database) October 9, 2015. Available from: http://www5.statcan.gc.ca/cansim/a26?lang=eng&retrLang=eng&id=0530003&&pattern=&stByVal=1&p1=1&p2=1&tabMode=dataTable&csid=.
- 27.Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88 PubMed Central PMCID: PMC2667420. doi: 10.1186/1471-2458-9-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.TreeAge Software. TreeAge Pro 2016, R2.1. Williamstown, MA. Available from: https://www.treeage.com.
- 29.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. PubMed Central PMCID: PMCPMC4855514. doi: 10.1001/jama.2012.113905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Preis SR, Hwang SJ, Coady S, Pencina MJ, D'Agostino RB Sr., Savage PJ, et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation. 2009;119(13):1728–35. PubMed Central PMCID: PMCPMC2789419. doi: 10.1161/CIRCULATIONAHA.108.829176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robitaille C, Dai S, Waters C, Loukine L, Bancej C, Quach S, et al. Diagnosed hypertension in Canada: incidence, prevalence and associated mortality. CMAJ. 2012;184(1):E49–56. PubMed Central PMCID: PMCPMC3255225. doi: 10.1503/cmaj.101863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bronnum-Hansen H, Davidsen M, Thorvaldsen P, Danish MSG. Long-term survival and causes of death after stroke. Stroke. 2001;32(9):2131–6. [DOI] [PubMed] [Google Scholar]
- 33.Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian Cancer Statistics 2015. Toronto, ON: Canadian Cancer Society; 2015.
- 34.Vandentorren S, Baldi I, Annesi Maesano I, Charpin D, Neukirch F, Filleul L, et al. Long-term mortality among adults with or without asthma in the PAARC study. Eur Respir J. 2003;21(3):462–7. [DOI] [PubMed] [Google Scholar]
- 35.Nuesch E, Dieppe P, Reichenbach S, Williams S, Iff S, Juni P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ. 2011;342:d1165 PubMed Central PMCID: PMCPMC3050438. doi: 10.1136/bmj.d1165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Statistics Canada. Canadian Health Measures Survey: Cycle 1 Data Tables: Ottawa, Ont: Statistics Canada; 2010. Available from: http://www.statcan.gc.ca/pub/82-623-x/82-623-x2010001-eng.pdf.
- 37.Statistics Canada. Table 105–0501—Health indicator profile, annual estimates, by age group and sex, Canada, provinces, territories, health regions (2013 boundaries) and peer groups, occasional, CANSIM (database)July 17, 2015. Available from: http://www5.statcan.gc.ca/cansim/a26?lang=eng&id=1050501.
- 38.Statistics Canada. Canadian Community Health Survey—Annual Component (CCHS). Detailed information for 2007 (Cycle 4.1) [cited 2016 March 1]. Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226.
- 39.Ellison LF, Wilkins K. Canadian trends in cancer prevalence. Health Rep. 2012;23(1):7–16. [PubMed] [Google Scholar]
- 40.Pelletier C, Dai S, Roberts KC, Bienek A, Onysko J, Pelletier L. Report summary. Diabetes in Canada: facts and figures from a public health perspective. Chronic Dis Inj Can. 2012;33(1):53–4. [PubMed] [Google Scholar]
- 41.Johansen HL, Wielgosz AT, Nguyen K, Fry RN. Incidence, comorbidity, case fatality and readmission of hospitalized stroke patients in Canada. Can J Cardiol. 2006;22(1):65–71. PubMed Central PMCID: PMCPMC2538981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152 [DOI] [PubMed] [Google Scholar]
- 43.Statistics Canada. Table 103–0550—New cases of primary cancer (based on the August 2015 CCR tabulation file), by cancer type, age group and sex, Canada, provinces and territories, annual, CANSIM (database)July 17, 2015. Available from: http://www5.statcan.gc.ca/cansim/a26?lang=eng&id=1030550.
- 44.Gershon AS, Guan J, Wang C, To T. Trends in asthma prevalence and incidence in Ontario, Canada, 1996–2005: a population study. Am J Epidemiol. 2010;172(6):728–36. doi: 10.1093/aje/kwq189 [DOI] [PubMed] [Google Scholar]
- 45.Kopec JA, Rahman MM, Berthelot JM, Le Petit C, Aghajanian J, Sayre EC, et al. Descriptive epidemiology of osteoarthritis in British Columbia, Canada. J Rheumatol. 2007;34(2):386–93. [PubMed] [Google Scholar]
- 46.OECD. Purchasing Power Parities for GDP and related indicators [cited September, 2016]. Available from: https://stats.oecd.org/Index.aspx?DataSetCode=PPPGDP.
- 47.OECD. Consumer Prices Indices [cited September, 2016]. Available from: http://stats.oecd.org/Index.aspx?DatasetCode=MEI_PRICES.
- 48.Schultz SE, Kopec JA. Impact of chronic conditions. Health Rep. 2003;14(4):41–53. [PubMed] [Google Scholar]
- 49.Jia H, Lubetkin EI. The impact of obesity on health-related quality-of-life in the general adult US population. J Public Health (Oxf). 2005;27(2):156–64. [DOI] [PubMed] [Google Scholar]
- 50.Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the Panel on Cost-effectiveness in Health and Medicine. JAMA. 1996;276(15):1253–8. [PubMed] [Google Scholar]
- 51.Doubilet P, Begg CB, Weinstein MC, Braun P, McNeil BJ. Probabilistic sensitivity analysis using Monte Carlo simulation. A practical approach. Med Decis Making. 1985;5(2):157–77. Epub 1985/01/01. doi: 10.1177/0272989X8500500205 [DOI] [PubMed] [Google Scholar]
- 52.Briggs A, Sculpher M, Buxton M. Uncertainty in the economic evaluation of health care technologies: the role of sensitivity analysis. Health economics. 1994;3(2):95–104. [DOI] [PubMed] [Google Scholar]
- 53.Vander Ploeg KA, Kuhle S, Maximova K, McGavock J, Wu B, Veugelers PJ. The importance of parental beliefs and support for pedometer-measured physical activity on school days and weekend days among Canadian children. BMC Public Health. 2013;13:1132 PubMed Central PMCID: PMCPMC4234294. doi: 10.1186/1471-2458-13-1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Faught E, Vander Ploeg K, Chu YL, Storey K, Veugelers PJ. The influence of parental encouragement and caring about healthy eating on children's diet quality and body weights. Public Health Nutr. 2016;19(5):822–9. doi: 10.1017/S1368980015002049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ferland A, Chu YL, Gleddie D, Storey K, Veugelers P. Leadership skills are associated with health behaviours among Canadian children. Health Promot Int. 2015;30(1):106–13. doi: 10.1093/heapro/dau095 [DOI] [PubMed] [Google Scholar]
- 56.Rittenhouse B. Uses of Models in Economic Evaluations of Medicines and Other Health Technologies. London: Office of Health Economics; 1996. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
The approval for REAL kids Alberta schools evaluation was granted by the Health Research Ethics Board at the University of Alberta on the basis that all data would be kept confidential and would be stored and used in adherence to the guidelines established by the University. For these reasons, REAL kids Alberta data used to estimate the effect of the APPLE Schools are available upon request and requests can be made by contacting the Primary Investigator of the study, Dr. Paul Veugelers. The Health Research Ethics Board at the University of Alberta can be contacted at: Research Ethics Office; 308 Campus Tower; 8625 – 112 Street; Edmonton, AB T6G 1K8; Phone: 1.780.492.0459; Email: reoffice@ualberta.ca. The Research Ethics Office assigned Pro00003799 (REAL Kids Alberta) and Pro00003800 (APPLE Schools) as protocol numbers of the studies that collected data that were used in the present study. Data from the National Population Health Survey (NPHS) and the National Longitudinal Survey of Children and Youth (NLSCY) are owned by Statistics Canada and are available from Statistics Canada Research Data Centers for researchers who meet the criteria for access to confidential data. Statistics Canada has an established protocol for researchers to access their data: Researchers have to submit an application and if the application is approved, the applicants have to undergo security screening. After getting security clearance, researchers get to access data in a secure Statistics Canada Research Data Center (RDC). All analyses have to be done at the RDC and only results are allowed to be taken out after vetting by the RDC. Raw data cannot be taken out of the RDC. Further details on the process of accessing Statistics Canada data are available at the following link: http://www.statcan.gc.ca/eng/rdc/programresearchacademic. To access the NPHS and NLSCY data we had to go through the following process: (1) We wrote a proposal for a program of research; (2) We completed the online application form through the Social Sciences and Humanities Research Council (SSHRC) website: https://webapps.nserc.ca/SSHRC/faces/logon.jsp?lang=en_CA; (3) After getting approval for the research program, we had to complete a security screening process. After which we signed a microdata research contract with Statistics Canada; (4) We were then given permission to access data at the Statistics Canada Research Data Centre (RDC) at the University of Alberta. We carried out all the analyses at the RDC and were allowed to take out results after being vetted by the RDC. All other model inputs that were obtained from published literature are provided in accompanying Supporting Information tables.