Abstract
Malaria is transmitted by many Anopheles species whose proportionate contributions vary across settings. We re-assessed the roles of Anopheles arabiensis and Anopheles funestus, and examined potential benefits of species-specific interventions in an area in south-eastern Tanzania, where malaria transmission persists, four years after mass distribution of long-lasting insecticide-treated nets (LLINs). Monthly mosquito sampling was done in randomly selected households in three villages using CDC light traps and back-pack aspirators, between January-2015 and January-2016, four years after the last mass distribution of LLINs in 2011. Multiplex polymerase chain reaction (PCR) was used to identify members of An. funestus and Anopheles gambiae complexes. Enzyme-linked immunosorbent assay (ELISA) was used to detect Plasmodium sporozoites in mosquito salivary glands, and to identify sources of mosquito blood meals. WHO susceptibility assays were done on wild caught female An. funestus s.l, and physiological ages approximated by examining mosquito ovaries for parity. A total of 20,135 An. arabiensis and 4,759 An. funestus were collected. The An. funestus group consisted of 76.6% An. funestus s.s, 2.9% An. rivulorum, 7.1% An. leesoni, and 13.4% unamplified samples. Of all mosquitoes positive for Plasmodium, 82.6% were An. funestus s.s, 14.0% were An. arabiensis and 3.4% were An. rivulorum. An. funestus and An. arabiensis contributed 86.21% and 13.79% respectively, of annual entomological inoculation rate (EIR). An. arabiensis fed on humans (73.4%), cattle (22.0%), dogs (3.1%) and chicken (1.5%), but An. funestus fed exclusively on humans. The An. funestus populations were 100% susceptible to organophosphates, pirimiphos methyl and malathion, but resistant to permethrin (10.5% mortality), deltamethrin (18.7%), lambda-cyhalothrin (18.7%) and DDT (26.2%), and had reduced susceptibility to bendiocarb (95%) and propoxur (90.1%). Parity rate was higher in An. funestus (65.8%) than An. arabiensis (44.1%). Though An. arabiensis is still the most abundant vector species here, the remaining malaria transmission is predominantly mediated by An. funestus, possibly due to high insecticide resistance and high survival probabilities. Interventions that effectively target An. funestus mosquitoes could therefore significantly improve control of persistent malaria transmission in south–eastern Tanzania.
Background
Malaria continues to be one of the most significant mosquito-borne parasitic diseases, affecting about 212 million people, causing 429,000 deaths annually [1], and adversely affect socio-economic development in sub-Saharan African countries [2]. The World Health Organization (WHO) estimates that there has been a decline in malaria burden, and that morbidity worldwide reduced by 21% and mortality by 29% between 2010 and 2015, but sub-Saharan Africa still accounts for approximately 92% of all malaria deaths and cases [1]
Tanzania has experienced a decline in malaria transmission following the introduction of insecticide treated nets (ITNs) and the scale-up of long-lasting insecticide treated nets (LLINs) [3]. By 2010, the country had made significant progress, and most areas that were experiencing prevalence above 50% in 2000, now had below 10% prevalence [4]. However, the most recent malaria indicator survey has returned an average prevalence of 14.8% prevalence in children under 5 years in Tanzania [5]. Getting to zero transmission therefore remains a major challenge, mainly because the persistent malaria transmission is mediated by mosquitoes that are not adequately responsive to control by existing indoor insecticidal interventions, such as LLINs and indoor residual spraying (IRS). The Tanzanian National Malaria Control Program is aiming at cutting down malaria transmission to 1% by 2020 [6], thus the need for new complementary approaches is even more urgent.
Despite the high coverage of LLINs, high indoor densities of potentially infectious mosquitoes remain common in some places [7, 8]. Evidence suggests that indoor densities of major malaria vectors such as An. funestus and An. arabiensis depend on house design features, environmental conditions and demographic composition [8, 9]. Previous studies have reported high levels of resistance in An. funestus to pyrethroids in Tanzania [10] and elsewhere in East Africa [11–13]. An. funestus is one of the major malaria vectors in Africa and is widely distributed across the continent [14, 15]. The species is highly anthropophilic and endophilic, with higher vectorial capacity than most other vector species [14, 16]. The An. funestus group includes several sibling species, which are difficult to distinguish morphologically, but can be separated by polymerase chain reaction (PCR) using a cocktail of species-specific primers [17]. Previous studies in Tanzania have reported presence of four member species in the An. funestus group, namely An. funestus s.s, An. rivulorum, An. leesoni and An. parensis [18]. All the four members of the An. funestus group have been found positive for P. falciparum though the infection rates are often higher in the predominantly anthropophagic An. funestus s.s than the rest. The importance of this vector is increasingly associated with the persistent malaria transmission [8, 10], and it has been suggested that it could be responsible for resurgence of malaria transmission in rural Tanzania [10].
In this study, we assessed contributions of residual populations of major malaria vectors, An. arabiensis and An. funestus, in endemic villages in rural south-eastern Tanzania, where the last mass distribution of LLINs prior to our study had been completed in 2011 [19]. The study assessed prevalence of Plasmodium sporozoites in the vector species, survival rates of these vectors, and their resistance status to examine what factors might be mediating the role of these two major species in the ongoing malaria transmission. Inferences are made with regard to what would happen if appropriate species-specific interventions were deployed in this and similar settings. More specifically, interventions that effectively target mosquito species mediating most of the remnant malaria transmission should result in extensive declines in the transmission. Where one vector species dominates the transmission system, approaches against such vectors may offer opportunities to sufficiently disrupt local malaria transmission.
Methods
Study area
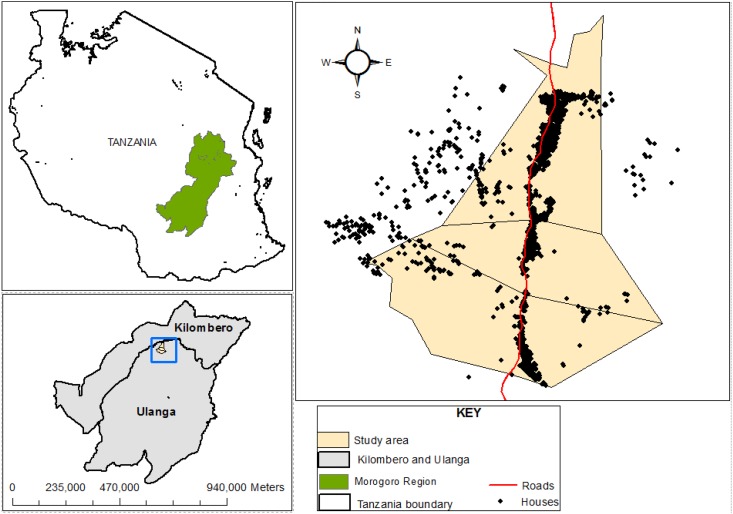
The study was conducted in three villages in the Kilombero floodplains in Ulanga district, south-eastern Tanzania (Fig 1). This area is perennially meso-endemic for malaria and has high mosquito densities throughout the year, peaking between January and May. Annual rainfall and temperatures range from 1200 to 1800 mm and 20°C to 32.6°C respectively. Malaria vector species in the area comprise primarily of the An. gambiae s.l (almost exclusively consisting of An. arabiensis), and An. funestus group. Several other Anopheles mosquitoes such as An. coustani, An. pharoensis, An. squamosus, An. ziemanni and An. wellcomei are also found, as well as several culicine species, mainly Mansonia mosquitoes, Aedes mosquitoes and Culex species. The major vector control intervention in this area is LLINs [19], and the last mass-distribution of nets, prior to this study had been conducted between 2010 and 2011 [19].
Fig 1. Map of the study area, showing the villages and households in Ulanga district where the study was conducted.
Study procedures
This study was part of a high-resolution longitudinal mosquito surveillance program, where we collected host-seeking and indoor-resting mosquitoes between January 2015 and January 2016, in randomly selected households, and also selected sentinel households within the Health and Demographic Surveillance System (HDSS) maintained by Ifakara Health Institute in the study area [20].
Monitoring indoor densities of host-seeking and resting disease-transmitting mosquitoes
Firstly, 1600 households were randomly selected from the HDSS households database in three study villages of Kivukoni, Minepa and Mavimba, and assigned to 16 geographical clusters each consisting of 100 households. The sampling clusters were assigned based on household latitudes so that clusters 1–16 were arranged in a north-south direction in the study area. From each geographical cluster, six households were selected for sampling. These included three households randomly selected on monthly basis, and another three households that were fixed as sentinel households, visited repeatedly every month. This way, 96 households were studied per month, each time consisting of 48 sentinel households across the study area, and 48 new households randomly selected each month. Geo-positions of all the households were recorded using hand held GPS receivers (Magellan eXplorist 110). Each household was visited only once each month, and mosquitoes were sampled from one room with occupant(s) sleeping under mosquito nets, using miniature Centre for Disease Control (CDC) light traps set near occupied bed nets at the foot end, at approximately 1.5 m from the ground [21, 22]. The traps were operated from18:00 to 06:00 each night.
Indoor resting mosquitoes were collected using a backpack aspirator [23] from the walls, bed nets and floors in same households where the CDC light trap catches were conducted. Aspiration of resting mosquitoes was conducted for approximately 15 minutes in each household. Each morning, the collected mosquitoes were killed in a closed container using alcohol. The mosquitoes were identified morphologically and sorted by taxa and sex before they were identified by PCR. The identification was done following the taxonomic key developed by Gillies and Coetzee, i.e. Keys for the Anopheles of Africa, south of Sahara [24].
Identification of sibling species and detection of Plasmodium infection in malaria vectors
All female An. gambiae complex mosquitoes, were examined by multiplex polymerase chain reaction (PCR) technique as described by Scott et al. [18] to distinguish sibling species. Similarly, all samples of An. funestus were examined by PCR, using techniques developed by Koekemoer et al. [25] and Cohuet et al. [26] to distinguish sibling species. All Anopheles mosquitoes caught were segregated by species and examined in pools by enzyme-linked immunosorbent assays (ELISA), to detect Plasmodium sporozoites in their salivary glands [27]. To avoid false positives, the ELISA lysates were boiled for 10 minutes at 100°C, effectively eliminating heat-labile non Plasmodium falciparum protozoan antigens [28]. We assessed all the collected Anopheles gambiae s.l and Anopheles funestus s.l mosquitoes by ELISA, using heads and thoraces. However, only a sub-sample was assessed by PCR for species identification, using legs.
Identification of mosquito blood meals
Blood meal analysis was also done on a sub-sample, working only with the mosquitoes that were blood-fed. Each mosquito abdomen was separated from the thorax and homogenized in phosphate buffer saline (PBS) following the method described by Beier et al. [29]. This way, all the blood-fed mosquitoes were screened for human, bovine, chicken, goat and dog blood using ELISA.
Assessment of insecticide susceptibility and parity rates
The insecticide susceptibility tests were conducted using standard WHO guidelines [30]. Insectary-reared An. gambiae s.s (Ifakara strain) was used as a reference susceptible population. Because of the difficulties in finding An. funestus larvae in the study area, adult female mosquitoes were collected indoors from April to July 2016, by CDC light traps from the same households in three villages. The mosquitoes were transferred into netting cages and maintained on 10% glucose solution. An. funestus mosquitoes were then separated from other mosquito species by gently sucking them from the cages into a small-netting cage using mouth aspirators and all other mosquito species were killed.
Non blood-fed adult An. funestus s.l females were therefore exposed to 0.75% permethrin, 0.05% deltamethrin, 0.05% lambda cyhalothrin, 4% dieldrin, 4% DDT, 0.1% bendiocarb, 0.1% propoxur, 0.25% pirimiphos methyl, and 1% malathion, as recommended by the WHO. Up to 100 adult females of unknown age were exposed to each insecticide during the experiment, including at least four replicates. In each test, mosquitoes collected from the same villages at the same time were exposed to oil impregnated papers, constituting additional controls. The number of knocked-down mosquitoes in each tube was counted and recorded after 10, 15, 20, 30, 40, 50 and 60 minutes. After one hour of exposure, mosquitoes were transferred to the holding tubes and maintained on 10% sugar solution then monitored for survival and mortality after 24 hours. The post exposure observation was conducted after 80 minutes only if the knockdown was less than 80% [30].
Physiological age of the wild-caught female malaria vectors was approximated based on the status of their ovaries, i.e. whether they had previously laid eggs or not [31]. Abdomens of a randomly selected sub-samples of unfed female An. funestus and An. arabiensis collected from the selected households were dissected for parity [32]. Each unfed female mosquito was first anesthetized in a refrigerator. A drop of distilled water was added to a slide and each specimen kept still on the slide, then the seventh and eighth abdominal segment was pulled using a fine needle under a stereo dissecting microscope. The ovarial tracheoles were then observed under a compound microscope at 10X magnification, to determine whether they were parous or nulliparous [31].
Data analysis
Statistical analyses were carried out using R statistical software version 3.3.1 [33]. Mosquito abundance was over-dispersed so we modeled it following a negative binomial distribution using the generalized linear mixed model automatic differentiation model builder (glmmADMB) package [34] with log link function. Here, mosquito abundance (nightly total count) were treated as response variable while locality (villages) were treated as fixed effect.
Plasmodium infection rates and blood meal sources of malaria vectors were estimated as percentages of total mosquitoes assayed. Similarly, observed mean mortality after 24 hours of exposure to each insecticide was calculated as percentage of total mosquitoes exposed in all four exposure replicates [30]. The insecticide susceptibility test findings were interpreted according to WHO guidelines [30].
The EIR was calculated as a function of biting rates and proportion of tested mosquitoes infected with sporozoites. Since we initially calculated these biting rates for each trap night, the EIR was adjusted by multiplying the daily EIR values by 365 nights (Annual EIR = Nightly biting rate x Sporozoite rate x 365). We relied on values comparative trap evaluations done in the same study area, where CDC light traps had been directly compared to human landing catches inside households [35]. Those earlier trials had indicated that CDC light traps consistently caught 0.3 times as many An. gambiae s.l as human landing catches, and 0.68 times as many An. funestus mosquitoes as human landing catches [35]. In this current study, we have therefore adjusted the CDC light trap catches using these coefficients, but also presented the unadjusted results.
Ethical considerations
Meetings with local leaders were held in the study areas and the main aims of the study were explained by the scientists. Permission to conduct studies in the separate villages was obtained from respective leaders of each of the villages; Mr. Ayubu Salila, Mr. Kiluka Mdumba and Mr. Baalesa Ligola for Kivukoni, Minepa and Mavimba villages respectively. I confirm that the field studies did not involve endangered or protected species. A written and signed informed consent was obtained from each household head participating in the study. All information was given in Kiswahili, the local language. All the households were provided and protected by intact LLINs (Olyset®nets) as previously distributed by the universal bednets coverage campaign [36]. Ethical approval for the study was obtained from Ifakara Health Institute Institutional Review Board (IHI/IRB/No: 34–2014), and the Medical Research Coordination Committee of the National Institute of Medical Research (Certificate No.NIMR/HQ/R.8a/Vol.IX1903).
Results
Indoor densities of Anopheles mosquitoes in the area
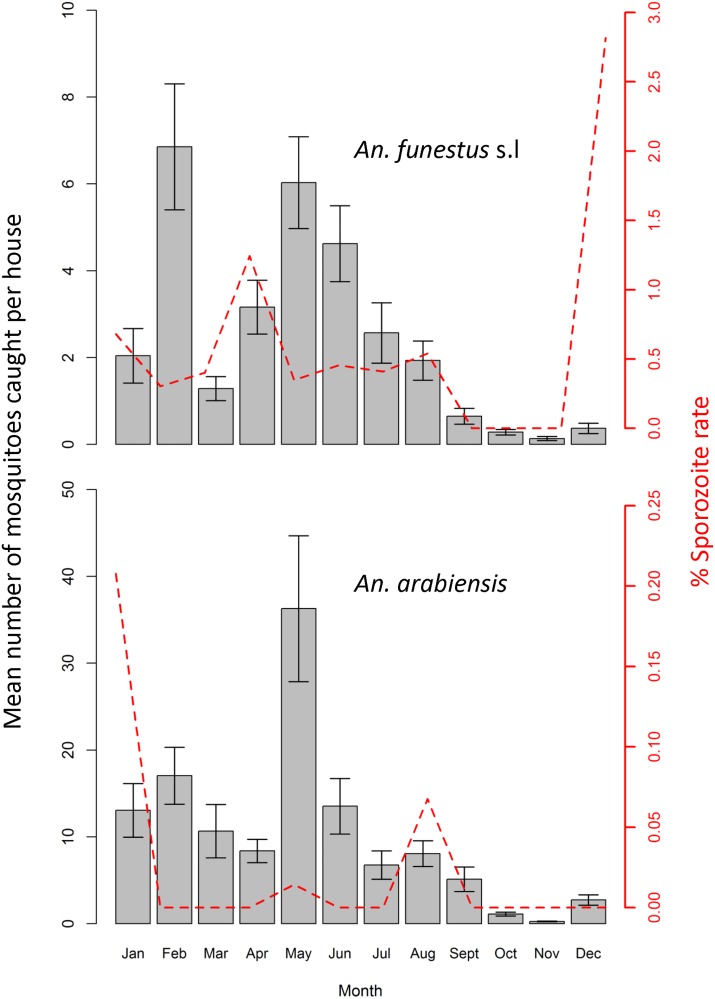
A total of 25670Anopheles mosquitoes were collected by CDC light trap and back pack aspirator, comprising An. funestus s.l (18.7%) and An. gambiae s.l, which in turn comprised of An. arabiensis sibling species (79.0%), An. pharoensis (0.5%), An. squamosus (0.4%), An. ziemanni (0.3%) and An. wellcomei (0.4%). The highest densities, i.e. 54% and 65% of all An. arabiensis and 65% of all An. funestus were observed in the middle of study area, i.e. Minepa village. Densities of An. peaked between May, while the density of An. funestus peaked in February and May.one month after onset of the long rainy season, which is the main malaria transmission season. The lowest vector densities were observed between September and November (Fig 2).
Fig 2. Mean number of Anopheles funestus s.l and Anopheles arabiensis mosquitoes caught per house per night.
Y error bars represent the 2-standard errors of the mean.
Sibling species of malaria vectors and Plasmodium infection rates
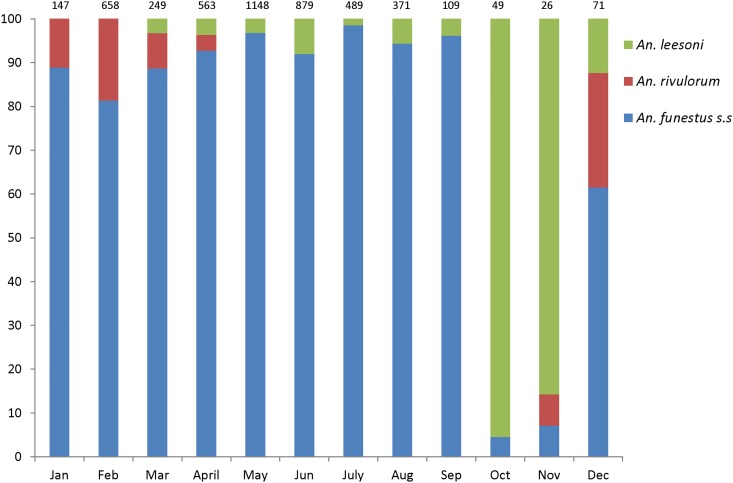
A total of 20,135 An. gambiae s.l and 4,759 An. funestus s.l mosquitoes were assayed in the laboratory by PCR or ELISA or both. All the An. gambiae s.l. mosquitoes tested by PCR were confirmed to be An. arabiensis (100%). On the other hand, the An. funestus group consisted of 76.6% An. funestus s.s, 2.9% An. rivulorum, 7.1% An. leesoni, and 13.4% unamplified samples. Monthly variations of proportions of the An. funestus sibling species is shown in Fig 3.
Fig 3. Monthly variations in the composition of sibling species of Anopheles funestus group in the study area.
The CDC-light trap catches were used to estimate malaria transmission densities as Entomological Inoculation Rates (EIR) as shown in Table 1. Infection rates were higher in An. funestus than An. arabiensis. Using unadjusted estimates, the overall EIR (bites per person per year) was 9.19, of which An. funestus contributed 86.21%, while An. arabiensis contributed 13.79% (Table 1). However, when considering estimates adjusted on the basis of relative efficiencies of CDC light traps compared to Human Landing Catches, the overall EIR (bites per person per year) was 15.87, of which An. funestus contributed 73.39%, while An. arabiensis contributed 26.61% (Table 1). The highest sporozoite rate among An. funestus was in April, when 13.79% towards the transmission. Nightly biting rate among An. funestus was highest in May, i.e. 344 bites/month, while the highest biting rate in An. arabiensis was 2090 bites/month in the same month (Table 2). Of all An. funestus s.l mosquitoes that tested positive for malaria parasites, 96% were An. funestus s.s, the remaining 4% being An. rivulorum. None of the An. leesoni tested positive for Plasmodium sporozoites.
Table 1. Infectious status of malaria vectors and dominant contribution of Anopheles funestus mosquitoes to ongoing malaria transmission, despite their low abundance relative to Anopheles arabiensis.
| Anopheles arabiensis | Anopheles funestus s.l | |
|---|---|---|
| Total number of mosquitoes collected by CDC Light Trap (January 2015 to January 2016) | 20135 | 4759 |
| Total number of trap nights | 1152 | 1152 |
| Biting rate per night | 17.48 | 4.13 |
| Relative efficiency (CDC-LT) relative to HLC (Derived from Okumu et al 2008 [38]) | 0.3 | 0.68 |
| Corrected biting rate | 58.26 | 6.08 |
| Total number of mosquitoes analysed for Plasmodium falciparum circumsporozoite protein (CSP) | 20135 | 4759 |
| Total number of sporozoite positive mosquitoes | 4 | 25 |
| Sporozoite rate | 0.0002 | 0.0053 |
| Annual EIR (Adjusted)** | 4.22 | 11.65 |
| % EIR Contribution (Adjusted)** | 26.61% | 73.39% |
| Annual EIR (not adjusted) | 1.27 | 7.92 |
| % EIR Contribution (not adjusted) | 13.79% | 86.21% |
• Annual EIR (Corrected biting rate x Sporozoite rate x 365)
• Overall EIR (EIR for An. arabiensis+ EIR for An. funestus) = 18.45
• *86.3% of the mosquitoes from the An. funestus group tested were An. funestus s.s, 8.4% were An. leesoni and 5.2% were An. rivulorum. Of all An. funestus s.l mosquitoes that tested positive for malaria parasites, 96% were An. funestus s.s, the remaining 4% being An. rivulorum.
• **Where the estimates are adjusted, these adjustments were done using coefficients computed as the ratio of mosquito catches by CDC-Light Traps to catches Human Landing Catch methods. These coefficients were 0.3 for An. arabiensis and 0.68 for An. funestus as determined by Okumu et al 2008 [35]
Table 2. Monthly sporozoite rates and Entomological Inoculation Rates (EIR) (number of infectious bites per person per month) for Anopheles funestus and Anopheles arabiensis from January to December 2016.
| Anopheles funestus | Anopheles arabiensis | |||||||
|---|---|---|---|---|---|---|---|---|
| Month | Number of Mosquitoes Tested | Monthly biting rates (adjusted**) | Sporozoite Infection Rate | Mean Monthly EIR | Number of Mosquitoes Tested | Monthly biting rates (adjusted **) | Sporozoite Infection Rate | Mean Monthly EIR |
| January | 147 | 44.10 | 0.0219 | 0.97 | 963 | 288.90 | 0.0068 | 1.96 |
| February | 658 | 197.40 | 0.0107 | 2.12 | 1640 | 492.00 | 0.0000 | 0.00 |
| March | 249 | 74.70 | 0.0129 | 0.96 | 2111 | 633.30 | 0.0000 | 0.00 |
| April | 563 | 168.90 | 0.0413 | 6.98 | 1502 | 450.60 | 0.0000 | 0.00 |
| May | 1148 | 344.40 | 0.0113 | 3.89 | 6968 | 2090.40 | 0.0005 | 0.94 |
| June | 879 | 263.70 | 0.0153 | 4.04 | 2576 | 772.80 | 0.0000 | 0.00 |
| July | 489 | 146.70 | 0.0132 | 1.94 | 1283 | 384.90 | 0.0000 | 0.00 |
| August | 371 | 111.30 | 0.0174 | 1.94 | 1478 | 443.40 | 0.0023 | 1.00 |
| September | 109 | 32.70 | 0.0000 | 0.00 | 859 | 257.70 | 0.0000 | 0.00 |
| October | 49 | 14.70 | 0.0000 | 0.00 | 244 | 73.20 | 0.0000 | 0.00 |
| November | 26 | 7.80 | 0.0000 | 0.00 | 51 | 15.30 | 0.0000 | 0.00 |
| December | 71 | 21.30 | 0.0910 | 1.94 | 460 | 138.00 | 0.0000 | 0.00 |
** Values adjusted based on Okumu et al 2008; see Table 1
Indoor densities of Culicine mosquitoes in the area
A total of 103,382 Culicine mosquitoes, comprising of 100,047 Culex (96.7%), 3197 Mansonia (3.1%) and 138 Aedes mosquitoes (0.1%). Of all the Culex mosquitoes collected, males contributed 76.3%, while females contributed 23.7%. For Mansonia, males contributed 58.6% while females contributed 41.4%. Lastly, Aedes males contributed 26.1% while females were 73.9%.
Mosquito blood meal sources
A total of 82 mosquitoes that were identified by PCR also had blood meals in their abdomen, so these were assessed by way of blood-meal ELISA. These included 64 An. arabiensis, 17 An. funestus s.s, and 1 An. leesoni. The study identified a broad spectrum of host blood antigens, mostly humans (79.2%), followed by cattle (17.1%), dogs (2.4%) and chicken (1.2%). The analysis did not detect any mixed blood meals. The results for mosquito blood meals are summarized in Table 3.
Table 3. Host blood antigens detected in blood-meals obtained from Anopheles mosquitoes.
| Blood meal source | Anopheles arabiensis | Anopheles funestus s.s | Anopheles leesoni | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Human | 47 | 73.4 | 17 | 100 | 1 | 100 |
| Bovine | 14 | 22 | 0 | 0 | 0 | 0 |
| Dog | 2 | 3.1 | 0 | 0 | 0 | 0 |
| Chicken | 1 | 1.5 | 0 | 0 | 0 | 0 |
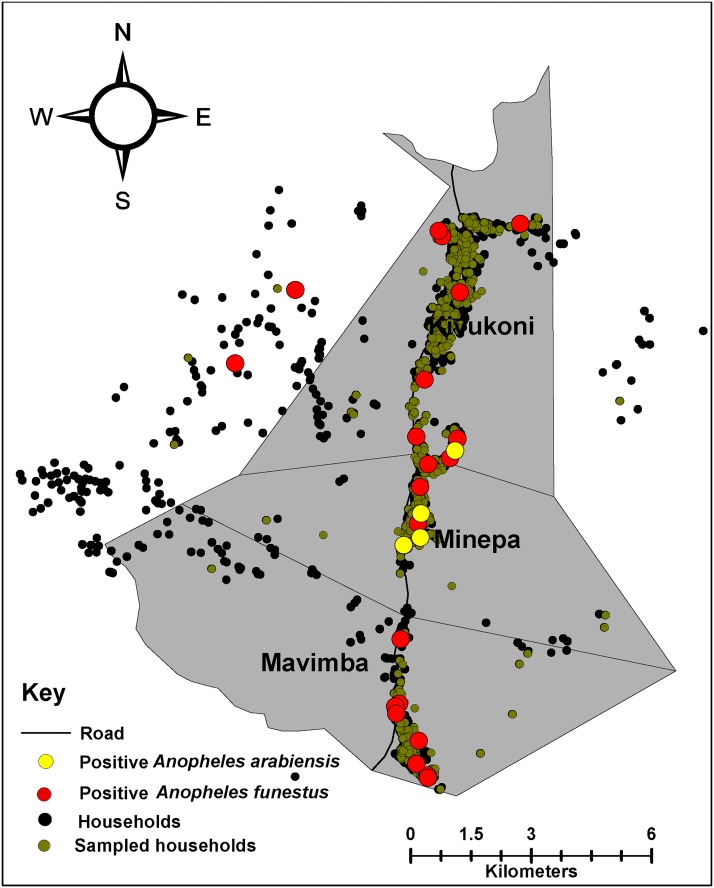
Spatial distribution of sporozoite infected An. funestus and An. Arabiensis
Sporozoite infected An. funestus were widely distributed across all the study villages, it was also observed that An. arabiensis were mostly confined to an area in the middle of the study area (Fig 4). The total number of sporozoite infected mosquitoes during the year was, however, too small to enable detailed analysis of spatial relations.
Fig 4. Distribution of Plasmodium infected An. funestus and An. arabiensis.
Insecticide susceptibility test results
The insecticide susceptibility test results are summarized in Table 3. There was 100% mortality in the susceptible reference An. gambiae s.s colony when exposed to all the candidate insecticides tested. The wild-caught An. funestus were also fully susceptible to pirimiphos methyl (100% mortality), malathion (100%), and dieldrin (100%), but they were resistant to permethrin (10.5% mortality), deltamethrin (18.7%), lambda cyhalothrin (18.7%) and DDT (26.2%). In these tests, the An. funestus also showed reduced susceptibility to bendiocarb (95% mortality) and propoxur (90.1% mortality). The overall mortality of the An. funestus mosquitoes exposed to control papers was 5.4%.
Parity rates of An. funestus relative to An. arabiensis mosquitoes
Of the 302 An. funestus dissected, 65.8% were parous, 28.8% were nulliparous, and 5.2% were pre-gravid. Of the 162 An. arabiensis dissected, 49.3% were parous, 37% were nulliparous and 13.5% were pre-gravid.
Discussion
Malaria prevalence is declining across most of African countries [1], due to improved vector control [1] and case management, but also urbanization, improved health care and better living standards [1]. Long-lasting insecticide treated nets (LLINs) and indoor residual spraying (IRS) contributed 78% of all gains accrued since 2000 [37]. In rural south-eastern Tanzania, where malaria prevalence has reduced by >60% since 2000, low-level transmission still persists despite persistently high LLIN coverage [38]. Our study re-assessed the residual malaria transmission dynamics in rural south-eastern Tanzania, in an area where the last mass distribution of bednets was conducted between 2010 and 2011, four years before our study [19]. This study therefore provides an essential update, of the transmission situation and demonstrates the now dominant role of An. funestus. Like in most residual transmission settings in East Africa, our study confirms that populations of formerly notorious An. gambiae s.s, have significantly diminished, or completely vanished [10, 39]. An. arabiensis now dominates in numbers, but the far more competent vector An. funestus carries most of the residual malaria parasites, despite being highly outnumbered by An. arabiensis. This study clearly provides a clear lead to the hypothesis that interventions targeting An. funestus could dramatically reduce malaria transmission in areas such as the ones where this study was conducted.
This study has also determined that An. funestus vector is resistant to pyrethroids used on LLINs (Table 4), and survives unexpectedly longer than An. arabiensis, thus requiring new control approaches. Given the extensive resistance in the species population against a wide range of insecticides currently approved for public health use, it appears that we now have only a limited set of options, including organophosphates such as pirimiphos methyl. Thus, one of the main control methods that could be used against this species is focal IRS with long-lasting formulations of organophosphates (e.g. Actellic® CS-300), against which An. funestus are still highly susceptible. Other potential interventions may include house improvement and house screening, as well as use of eave baffles treated with organophosphates, which would take far less insecticide, but deliver equal impact on the mosquito populations as IRS (Killeen et al unpublished manuscript). Going forward, it may be desirable to conduct new evidence-based studies in well-characterized areas such as these study sites, to demonstrate possible vector elimination strategies leading to malaria transmission control. Approaches may include combinations of organophosphate-based IRS alongside other interventions like LLINs, improved housing and larval source management, especially where rice growing is commonly practiced.
Table 4. Summary of data on susceptibility of wild-caught adult female Anopheles funestus mosquitoes collected in the study sites.
| Insecticide tested | Total. No. Exposed | Number of mosquitoes knocked- down (KD) | Mortality | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10 min | 15 min | 20 min | 30 min | 40 min | 50 min | 60 min | % KD 60 min | Total No. Dead | % Dead | Status* | ||
| Control | 129 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 5.4 | - |
| 0.75% Permethrin | 95 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1.1 | 10 | 10.5 | RR |
| 0.05% Deltamethrin | 80 | 2 | 2 | 1 | 2 | 3 | 3 | 6 | 7.5 | 15 | 18.7 | RR |
| 0.05% Lambda cyhalothrin | 80 | 0 | 0 | 1 | 1 | 1 | 2 | 4 | 5.0 | 15 | 18.7 | RR |
| 0.1% Bendiocarb | 80 | 0 | 2 | 2 | 6 | 27 | 31 | 35 | 43.7 | 76 | 95.0 | RI |
| 0.1% Propoxur | 81 | 21 | 36 | 46 | 67 | 58 | 75 | 77 | 95.0 | 73 | 90.1 | RI |
| 0.25% Pirimiphos-methyl | 84 | 6 | 3 | 8 | 46 | 63 | 80 | 80 | 95.2 | 84 | 100.0 | SS |
| 5% Malathion | 80 | 7 | 13 | 32 | 55 | 74 | 78 | 79 | 98.7 | 80 | 100.0 | SS |
| 4% DDT | 80 | 0 | 0 | 4 | 7 | 9 | 8 | 13 | 16.2 | 21 | 26.2 | RR |
| 0.4% Dieldrin | 80 | 0 | 0 | 0 | 0 | 2 | 6 | 14 | 17.5 | 80 | 100.0 | SS |
*Susceptibility status:
• SS: Indicates susceptibility
• RR: Confirmation of resistance in the tested mosquito population.
• RI: Suggest the existence of resistance and further investigation is needed.
To achieve malaria elimination, we must identify and target all pockets of transmission, including geographically distinct areas of high transmission and demographically high-risk sub-populations [40, 41]. In this study setting in rural south-eastern Tanzania, low-level transmission persists, despite over 80% LLIN coverage [38]. The persistent residual transmission is most definitely mediated predominantly by An. funestus s.s, suggesting possibly that targeted, high impact, species-specific interventions may improve control and accelerate efforts towards eventual malaria elimination. Our recent findings suggested that the overall distribution of malaria mosquitoes, including An. funestus is strongly influenced by and can be predicted based on numbers and spatial variability of household occupancy [8]. The densities of Anopheles mosquitoes were highest in rainy season even though transmission was evidently sustained at low densities even in dry season, mostly by An. funestus. Since aquatic breeding habitats for An. funestus are not easily identified, it may be necessary to identify other environmental characteristics that affect natural abundance of An. funestus within villages and between households. This approach can be feasible by involving the local community and volunteers. The evidence from Mwangungulu et al show that scientists can rely on community knowledge and experiences to identify areas where mosquitoes are most abundant [42].
The data presented here would be essential in developing control measures that target primarily the most important residual vector species, in this case An. funestus. In these specific study settings in Tanzania, the nucleated settlements, and spatial correlations between human biomass and vector densities [8], indicates this proposed study area renders itself well to spatially-targeted interventions. The study has rigorously demonstrated that An. funestus is now the primary vector of malaria in this area in rural-south eastern Tanzania, despite concurrently high densities of other species such as An. arabiensis. The area historically had very high malaria transmission, averaged 400 infectious bites/person/year (ib/p/y) until early 2000s [43], with prevalence as high as 70% in 1990s [44], but this study indicates that transmission has now dropped around 20 ib/p/y. Moreover, this study has also demonstrated that An. funestus s.s co-exists with An. rivulorum and An. leesoni, but malaria transmission was mainly mediated by An. funestus s.s. It is not possible to determine conclusively if the greater contribution of the An. funestus s.s. to malaria transmission is mostly due to its relatively higher abundance than that of the other sibling species, but it is clear that this species mediates most of the residual transmission.
Of all the An. funestus mosquitoes that tested positive for malaria parasites, An. funestus s.s. comprised 96% of those An. funestus s.l. which were positive for Plasmodium sporozoites., though their overall relative abundance was 76.6%, while An. rivulorum was responsible for 4% of the infections though their relative abundance was only 2.9% of all the An. funestus mosquitoes. Anopheles leesoni, constituted 7.1% of all mosquitoes in this group, but carried no infections at all. Given that the ELISA lysates were all boiled to eliminate any false positives [28], occasionally associated with non-Plasmodium protozoans transmitted by zoophilic mosquitoes [45], we can assume, based on the 4% sporozoites rates, that An. rivulorum is indeed an important vector in this setting, and that its role is limited mostly by its low densities, relative to the other species. Other studies in East Africa have previously demonstrated the importance of the species in residual transmission settings [46], its role increasing after the decline of An. gambiae s.s populations [47, 48] (Table 5). Our study did not however, identify any Plasmodium infections in any of the other Anopheles mosquitoes collected, i.e. An. coustani, An. squamosus, An. ziemanni and An.wellcomei, at any time during the study, thus these species are likely to be of negligible importance in malaria transmission in this setting. Furthermore, this can be attributed to their low relative abundance in this area. Some previous studies have reported sporozoite infections in An. coustani [49], An. squamosus [50] and An. ziemanni [51], but no such evidence was observed in this current study. Table 5 shows some of the other localities where An. funestus mosquitoes significantly contribute to the residual malaria transmission.
Table 5. Examples of other localities where Anopheles funestus mosquitoes have been demonstrated to mediate most of the residual malaria transmission, and where control programs targeting An. funestus with effective interventions, could drastically reduce local transmission.
| SN | Country | Intervention | Dominant Vectors | Other Vectors | Resistance Status | Sporozoite Rates | Implications for malaria transmission control | Reference |
|---|---|---|---|---|---|---|---|---|
| 1 | Kenya | ITNs and LLINs | An. funestus | An. arabiensis, An. gambiae s.s. | Pyrethroid resistance confirmed | An. funestus 4.5%, An. arabiensis 0.9%, An.gambiae s.s 8.6% | Reduced effectiveness of the current interventions | [52] |
| 2 | Burkina Faso | An. gambiae s.l. | An. funestus s.l, An. nili | No pyrethroid detected. An. funestus in was highly resistant to dieldrin | An. funestus (2.6% -9.7%) | An. funestus had higher biting rates and high sporozoite rate compared to An.gambiae complex | [53] | |
| 3 | Tanzania | LLINs | An. gambiae s.l. | An. funestus s.l | Pyrethroid resistance confirmed | An. funestus (0.16% -1.47%) | Resurgence of malaria transmission in Kilombero valley, Tanzania | [10] |
| 4 | Senegal | LLINs | An. funestus | - | - | An. funestus 1.28% | An. funestus changed their host seeking behaviour following the introduction of LLINs, thus compromising effectiveness of LLINS. | [54] |
| 5 | Cameroon | An. funestus s.s | An. gambiae s.s | - | An. funestus 6.8%, An.gambiae s.s 0.6%- 4.1% | An. funestus accounts for 88% of the transmission in this setting. | [55] |
The extremely high proportion of Plasmodium infections currently mediated by An. funestus mosquitoes in this area is compounded by, and is likely also a result of the very high insecticide resistance in this species. This study found that An. funestus mosquitoes were not only carrying most of the residual malaria parasites, but they were also very highly resistant to common pyrethroids used for vector control, i.e. deltamethrin, permethrin, lambda-cyhalothrin, as well as to the organochlorine, DDT. Moreover, there was also reduced susceptibility to insecticides like bendiocarb and propoxur, which would normally be candidates for replacing the pyrethroids. An earlier study by Lwetoijera et a.l in the neighbouring Kilombero district, also found increasing importance of An. funestus in malaria transmission associated with high resistance [10]. Even though the insecticide susceptibility status for An. arabiensis was not evaluated in this study, a separate study from these villages by Matowo et al (unpublished findings) found An. arabiensis to be also highly resistant to pyrethroid chemicals.
While the high human blood index observed in the An. funestus clearly suggests that the species could still be best targeted by household-based interventions that protect humans. Observations of increasing outdoor biting by the different An. funestus sibling species has been reported in this study area [56, 57], which warrants consideration of complementary interventions that also target outdoor-biting vectors. Also, given the high resistance to the common insecticides for vector control, it appears that use of organophosphates, against which the vector is still susceptible, notably pirimiphos methyl, could provide a temporary solution against residual malaria transmission in this area. Long-lasting formulations of pirimiphos methyl already exist [58], which could be used for IRS in this area to complement LLINs, as it has already been implemented in Zanzibar, northern region and lake zones in Tanzania [59].
Other possible high value interventions could be insecticidal eave baffles (Killeen et al. Unpublished), especially in areas where even outdoor-biting populations forage indoors for their adult life [60]. This study did not assess the role of An. funestus on outdoor malaria transmission, but, a separate study conducted in the same villages by Ngowo et al (unpublished findings) yield evidence that some An. funestus collected outdoors were found to be sporozoite positive. Furthermore, tools should be included such as chemicals with new AIs available for IRS that are being evaluated for consideration by the WHO, including non-pyrethroid active ingredients like neonicotinoids as well as bednets that combine synergists with pyrethroids, or those that combine different insecticide classes to tackle insecticide resistance and lower vector survival.
One limitation of this study is that collections for insecticide susceptibility were conducted on wild caught females of variable age, since we could not find adequate larvae for the assays. WHO recommends where possible to use mosquitoes of the same age cohort (F1 progeny). Using wild mosquitoes that are older than the standard 3–5 days may lead to underestimation of resistance depending on the species distribution and the insecticide being tested. Blood meal analyses were carried out on visually blooded mosquitoes and so may have missed those with small amounts of blood in their abdomens, such as those that had interrupted feeding or had partially digested the blood. Another potential limitation is that parity assessments, such as the ones conduced here are greatly impacted by season, this study conducted parity assessment for mosquitoes collected for two months, we suggest that future further studies should be done to assess parity status across seasons. Lastly, there was also a significant non-amplification of mosquito samples during the PCR analysis to determine the sibling species. About 13.4% of all sample analyzed in the laboratory did not amplify. An analysis of the sample handling processes, the analysis process, and the control samples, suggests that the laboratory processes were unlikely to be the reason for the non-amplification. Instead, this situation might have arisen due to sub-optimal storage conditions of some samples, or minor discrepancies in the morphological identification. These specific processes therefore deserve greater attention in future analyses.
Conclusion
This study provides an update on the residual malaria transmission situation in rural south-eastern Tanzania, where LLINs were already widely distributed. Though An. arabiensis is still the most abundant vector species here, ongoing residual transmission is predominantly mediated by An. funestus, possibly due to high resistance and high survival probabilities. Interventions that effectively target An. funestus could therefore significantly improve control of residual malaria transmission in the area.
Supporting information
A file containing supplementary data depicting graphs used in this manuscript.
(CSV)
Acknowledgments
We thank the local communities of Ulanga district for allowing us to work in their houses. We thank Mr. Zeno Lipambila, Mr. Maxeclin Ngakuka and Mr. Hamis Bwanary for their assistance during mosquito collection in the village. We also thank the project team Alex Limwagu, Jose Mgando, Doreen Siria, Felician Meza, Said Abbasi, Dickson Lwetoijera, Deogratius Roman, Elihaika Minja, Mercy Opiyo, Jonhson Kyeba, Robert Sumaye, Mwajabu Hamis, and Sebard Mteteleka. We thank Japhet Kihonda for assistance during mosquito dissection, Neema Nombo and Paulina Kasanga for their help in the susceptibility tests.
Data Availability
The relevant data are within the paper and its Supporting Information file.
Funding Statement
EK was supported by Wellcome Trust and the Association of Physicians of Great Britain and Ireland for funding this research (Grant Number: 100540/Z/12/Z), EK is also supported by the Consortium for Advanced Research Training in Africa (CARTA), which is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Wellcome Trust (UK) (Grant No: 087547/Z/08/Z), the Carnegie Corporation of New York (Grant No--B 8606.R02), Sida (Grant No:54100029)), NSM received financial supports from Wellcome Masters Fellowship, Grant number: WT104029/Z/14/Z. FOO is also supported by a Wellcome Trust Intermediate Research Fellowship (Grant number: WT102350/Z/13/Z) and a grant from World Health Organization, Special Program for Research and Training in Tropical Diseases (Grant No. B40445). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization (2016) World Malaria Report.
- 2.Sicuri E, Vieta A, Lindner L, Constenla D, Sauboin C (2013) The economic costs of malaria in children in three sub-Saharan countries: Ghana, Tanzania and Kenya. Malaria Journal 12(1):307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Malaria Control Program (Tanzania) (2013) An Epidemiological Profile Of Malaria And Its Control In Mainland Tanzania:Report Funded By Roll Back Malaria And Department For International Development
- 4.Killeen G, Tami A, Kihonda J, Okumu F, Kotas M, Grundmann H, et al. (2007) Cost-sharing strategies combining targeted public subsidies with private-sector delivery achieve high bednet coverage and reduced malaria transmission in Kilombero Valley, southern Tanzania. BMC Infectious Diseases 7(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United Republic of Tanzania (2016) Tanzania Demographic and Health Survey and Malaria Indicator Survey 2015–2016
- 6.Mandike R. Tanzanian National Malaria Control Program (NMCP) (2014) Strategy 2014–2020. Presentation
- 7.Lwetoijera DW, Kiware SS, Mageni ZD, Dongus S, Harris C, Devine GJ, et al. (2013) A need for better housing to further reduce indoor malaria transmission in areas with high bed net coverage. Parasites and Vectors 6(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaindoa EW, Mkandawile G, Ligamba G, Kelly-Hope LA, Okumu FO (2016) Correlations between household occupancy and malaria vector biting risk in rural Tanzanian villages: implications for high-resolution spatial targeting of control interventions. Malaria Journal. 15(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kirby MJ, Green C, Milligan PM, Sismanidis C, Jasseh M, Conway DJ, et al. (2008) Risk factors for house-entry by malaria vectors in a rural town and satellite villages in The Gambia. Malaria Journal. 7(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lwetoijera DW, Harris C, Kiware SS, Dongus S, Devine GJ, McCall PJ, et al. (2014) Increasing role of Anopheles funestus and Anopheles arabiensis in malaria transmission in the Kilombero Valley, Tanzania. Malaria Journal. 13(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawada H, Dida GO, Ohashi K, Komagata O, Kasai S, Tomita T, et al. (2011) Multimodal pyrethroid resistance in malaria vectors, Anopheles gambiae ss, Anopheles arabiensis, and Anopheles funestus ss in western Kenya. PLOS One; 6(8):e22574 10.1371/journal.pone.0022574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morgan JC, Irving H, Okedi LM, Steven A, Wondji CS (2010) Pyrethroid resistance in an Anopheles funestus population from Uganda. PLOS One;5(7):e11872 10.1371/journal.pone.0011872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mulamba C, Riveron JM, Ibrahim SS, Irving H, Barnes KG, Mukwaya LG, et al. (2014) Widespread pyrethroid and DDT resistance in the major malaria vector Anopheles funestus in East Africa is driven by metabolic resistance mechanisms. PLOS One; 9(10):e110058 10.1371/journal.pone.0110058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huho B, Briët O, Seyoum A, Sikaala C, Bayoh N, Gimnig J, et al. (2013) Consistently high estimates for the proportion of human exposure to malaria vector populations occurring indoors in rural Africa. International Journal of Epidemiology; 42(1):235–47 10.1093/ije/dys214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coetzee M, Fontenille D (2004) Advances in the study of Anopheles funestus, a major vector of malaria in Africa. Insect Biochemistry and Molecular Biology;34(7):599–605 10.1016/j.ibmb.2004.03.012 [DOI] [PubMed] [Google Scholar]
- 16.Cohuet A, Simard F, Toto J-C, Kengne P, Coetzee M, Fontenille D (2003) Species identification within the Anopheles funestus group of malaria vectors in Cameroon and evidence for a new species. The American Journal of Tropical Medicine and Hygiene; 69(2):200–5 [PubMed] [Google Scholar]
- 17.Koekemoer L, Kamau L, Hunt R, Coetzee M (2002) A cocktail polymerase chain reaction assay to identify members of the Anopheles funestus (Diptera: Culicidae) group. The American Journal of Tropical Medicine and Hygiene; 66(6):804–11 [DOI] [PubMed] [Google Scholar]
- 18.Scott JA, Brogdon WG, Collins FH (1993) Identification of single specimens of the Anopheles gambiae complex by the polymerase chain reaction. The American Journal of Tropical Medicine and Hygiene; 49(4):520–9 [DOI] [PubMed] [Google Scholar]
- 19.Renggli S, Mandike R, Kramer K, Patrick F, Brown NJ, McElroy PD, et al. (2013) Design, implementation and evaluation of a national campaign to deliver 18 million free long-lasting insecticidal nets to uncovered sleeping spaces in Tanzania. Malaria Journal; 12(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Geubbels E, Amri S, Levira F, Schellenberg J, Masanja H, Nathan R (2015) Health & demographic surveillance system profile: the Ifakara rural and urban health and demographic surveillance system (Ifakara HDSS). International journal of Epidemiology; 44(3):848–61 10.1093/ije/dyv068 [DOI] [PubMed] [Google Scholar]
- 21.Mboera L, Kihonda J, Braks M, Knols B. Short report (1998) Influence of centers for disease control light trap position, relative to a human-baited bed net, on catches of Anopheles gambiae and Culex quinquefasciatus in Tanzania. The American Journal of Tropical Medicine and Hygiene; 59(4):595–6 [DOI] [PubMed] [Google Scholar]
- 22.Lines J, Curtis C, Wilkes T, Njunwa K (1991) Monitoring human-biting mosquitoes (Diptera: Culicidae) in Tanzania with light-traps hung beside mosquito nets. Bulletin of Entomological Research;81(01):77–84 [Google Scholar]
- 23.Maia MF, Robinson A, John A, Mgando J, Simfukwe E, Moore SJ (2011) Comparison of the CDC Backpack aspirator and the Prokopack aspirator for sampling indoor-and outdoor-resting mosquitoes in southern Tanzania. Parasite and Vectors;4:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gillies M, Coetzee M (1987) A supplement to the Anophelinae of Africa South of the Sahara (Afrotropical Region)
- 25.Koekemoer LL, Kamau L, Hunt RH, Coetzee M (2002) A cocktail polymerase chain reaction assay to identify members of the Anopheles funestus (Diptera: Culicidae) group. Am J Trop Med Hyg; 66(6):804–11 [DOI] [PubMed] [Google Scholar]
- 26.Cohuet A, Simard F, Toto JC, Kengne P, Coetzee M, Fontenille D (2003) Species identification within the Anopheles funestus group of malaria vectors in Cameroon and evidence for a new species. Am J Trop Med Hyg; 69(2):200–5 [PubMed] [Google Scholar]
- 27.Beier JC, Perkins PV, Koros JK, Onyango FK, Gargan TP, Wirtz RA, et al. (1990) Malaria sporozoite detection by dissection and ELISA to assess infectivity of afrotropical Anopheles (Diptera: Culicidae). Journal of Medical Entomology; 27(3):377–84 [DOI] [PubMed] [Google Scholar]
- 28.Durnez L, Van Bortel W, Denis L, Roelants P, Veracx Al, Trung HD, et al. (2011) False positive circumsporozoite protein ELISA: a challenge for the estimation of the entomological inoculation rate of malaria and for vector incrimination. Malar J 1;10:195 10.1186/1475-2875-10-195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beier JC, Perkins PV, Wirtz RA, Koros J, Diggs D, Gargan TP, et al. (1988) Bloodmeal identification by direct enzyme-linked immunosorbent assay (ELISA), tested on Anopheles (Diptera: Culicidae) in Kenya. Journal of Medical Entomology; 25(1):9–16 [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization (2013). Test procedures for insecticide resistance monitoring in malaria vector mosquitoes. Geneva, World Health Organization [Google Scholar]
- 31.Detinova TS (1962) Age grouping methods in Diptera of medical importance with special reference to some vectors of malaria. Age Grouping Methods in Diptera of Medical Importance with special reference to some Vectors of Malaria. [PubMed]
- 32.World Health Organization (1975) Manual on practical entomology part II method and techniques, pp. 1–186. Geneva, Switzerland.
- 33.Pinheiro J, Bates D, DebRoy S, Sarkar D. R (2013) Development Core Team. nlme: Linear and nonlinear mixed effects models. R package version: 3.1–109. Computer software.
- 34.Skaug H, Fournier D, Nielsen A, Magnusson A, Bolker B (2013) Generalized linear mixed models using AD model builder. R package version 07.
- 35.Oketch F, Kotas M, Kihonda J, Killeen G, Moore S (2008) Comparative evaluation of methods used for sampling malaria vectors in the Kilombero Valley, South Eastern Tanzania. The Open Tropical Medicine Journal;1:51–5 [Google Scholar]
- 36.Bonner K, Mwita A, McElroy PD, Omari S, Mzava A, Lengeler C, et al. (2011) Design, implementation and evaluation of a national campaign to distribute nine million free LLINs to children under five years of age in Tanzania. Malaria Journal;10(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bhatt S, Weiss D, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. (2015) The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature;526(7572):207–11 10.1038/nature15535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tanzania National Malaria Control Program, Ifakara Health Institute, World Health Organization, KEMRI-Wellcome Trust (2013) An epidemiological profile of malaria and its control in mainland Tanzania.
- 39.Bayoh MN, Mathias DK, Odiere MR, Mutuku FM, Kamau L, Gimnig JE, et al. (2010) Anopheles gambiae: historical population decline associated with regional distribution of insecticide-treated bed nets in western Nyanza Province, Kenya. Malaria Journal;9(1):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sturrock HJ, Hsiang MS, Cohen JM, Smith DL, Greenhouse B, Bousema T, et al. (2013) Targeting asymptomatic malaria infections: active surveillance in control and elimination. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bousema T, Griffin JT, Sauerwein RW, Smith DL, Churcher TS, Takken W, et al. (2012) Hitting hotspots: spatial targeting of malaria for control and elimination. PLOS Medicine;9(1):e1001165 10.1371/journal.pmed.1001165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mwangungulu SP, Sumaye RD, Limwagu AJ, Siria DJ, Kaindoa EW, Okumu FO (2016). Crowdsourcing vector surveillance: using community knowledge and experiences to predict densities and distribution of outdoor-biting mosquitoes in rural Tanzania. PLOS One.;11(6):e0156388 10.1371/journal.pone.0156388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Russell TL, Lwetoijera DW, Maliti D, Chipwaza B, Kihonda J, Charlwood JD, et al. (2010) Impact of promoting longer-lasting insecticide treatment of bed nets upon malaria transmission in a rural Tanzanian setting with pre-existing high coverage of untreated nets. Malar J;9(1):187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith T, Charlwood JD, Kihonda J, Mwankusye S, Billingsley P, Meuwissen J, et al. (1993) Absence of seasonal variation in malaria parasitemia in an area of intense seasonal transmission. Acta Tropica;54:55–72 [DOI] [PubMed] [Google Scholar]
- 45.Bashar K, Tuno N, Ahmed Tu, Howlader AJ (2013) False positivity of circumsporozoite protein (CSP)–ELISA in zoophilic anophelines in Bangladesh. Acta tropica;125(2):220–5 10.1016/j.actatropica.2012.10.004 [DOI] [PubMed] [Google Scholar]
- 46.Kawada H, Dida GO, Sonye G, Njenga SM, Mwandawiro C, Minakawa N (2012). Reconsideration of Anopheles rivulorum as a vector of Plasmodium falciparum in Western Kenya: some evidence from biting time, blood preference, sporozoite positive rate, and pyrethroid resistance. Parasites and Vectors;5(1):230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gillies M, Smith A (1960) The effect of a residual house spraying campaign in East Africa on species balance in the Anopheles funestus group: the replacement of Anophelesfunestus by Anopheles rivulorum. Bulletin of Entomological Research;51:243–53 [Google Scholar]
- 48.Wilkes T, Matola Y, Charlwood J (1996) Anopheles rivulorum, a vector of human malaria in Africa. Medical and Veterinary Entomology;10:108–10 [DOI] [PubMed] [Google Scholar]
- 49.Mwangangi JM, Muturi EJ, Muriu SM, Nzovu J, Midega JT, Mbogo C (2013) The role of Anopheles arabiensis and Anopheles coustani in indoor and outdoor malaria transmission in Taveta District, Kenya. Parasites and Vectors;6(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stevenson JC, Simubali L, Mbambara S, Musonda M, Mweetwa S, Mudenda T, et al. (2016) Detection of Plasmodium falciparum Infection in Anopheles squamosus (Diptera: Culicidae) in an Area Targeted for Malaria Elimination, Southern Zambia. Journal of medical entomology:tjw091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maia MF, Abonuusum A, Lorenz LM, Clausen P-H, Bauer B, Garms R, et al. (2012) The effect of deltamethrin-treated net fencing around cattle enclosures on outdoor-biting mosquitoes in Kumasi, Ghana. PLOS One;7(9):e45794 10.1371/journal.pone.0045794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCann RS, Ochomo E, Bayoh MN, Vulule JM, Hamel MJ, Gimnig JE, et al. (2014) Reemergence of Anopheles funestus as a vector of Plasmodium falciparum in western Kenya after long-term implementation of insecticide-treated bed nets. The American Journal of Tropical Medicine and Hygiene;90(4):597–604 10.4269/ajtmh.13-0614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dabire K, Baldet T, Diabate A, Dia I, Costantini C, Cohuet A, et al. (2007) Anopheles funestus (Diptera: Culicidae) in a humid savannah area of western Burkina Faso: bionomics, insecticide resistance status, and role in malaria transmission. Journal of Medical Entomology;44(6):990–7. [DOI] [PubMed] [Google Scholar]
- 54.Sougoufara S, Diédhiou SM, Doucouré S, Diagne N, Sembène PM, Harry M, et al. (2014) Biting by Anopheles funestus in broad daylight after use of long-lasting insecticidal nets: a new challenge to malaria elimination. Malaria Journal;13(1):125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cohuet A, Simard F, Wondji CS, Antonio-Nkondjio C, Awono-Ambene P, Fontenille D (2004) High malaria transmission intensity due to Anopheles funestus (Diptera: Culicidae) in a village of savannah–forest transition area in Cameroon. Journal of Medical Entomology;41(5):901–5 [DOI] [PubMed] [Google Scholar]
- 56.Matowo NS, Moore J, Mapua S, Madumla EP, Moshi IR, Kaindoa EW, et al. (2013) Using a new odour-baited device to explore options for luring and killing outdoor-biting malaria vectors: a report on design and field evaluation of the Mosquito Landing Box. Parasites and vectors; 6(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Matowo NS, Koekemoer LL, Moore SJ, Mmbando AS, Mapua SA, Coetzee M, et al. (2016) Combining Synthetic Human Odours and Low-Cost Electrocuting Grids to Attract and Kill Outdoor-Biting Mosquitoes: Field and Semi-Field Evaluation of an Improved Mosquito Landing Box. PLOS One;11(1):e0145653 10.1371/journal.pone.0145653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Oxborough RM, Kitau J, Jones R, Feston E, Matowo J, Mosha FW, et al. (2014) Long-lasting control of Anopheles arabiensis by a single spray application of micro-encapsulated pirimiphos-methyl (Actellic® 300 CS). Malaria Journal;13(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.National Malaria Control Programme (NMCP) (2015) Tanzania Supplemental environmental assessment for indoor residual spraying for malaria control 2015–2020.
- 60.Killeen GF, Govella NJ, Lwetoijera DW, Okumu FO (2016) Most outdoor malaria transmission by behaviourally-resistant Anopheles arabiensis is mediated by mosquitoes that have previously been inside houses. Malaria Journal;15(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A file containing supplementary data depicting graphs used in this manuscript.
(CSV)
Data Availability Statement
The relevant data are within the paper and its Supporting Information file.