Abstract
Objective
The aim of this systematic review was to identify and summarize the published literature on the use of telemedicine for the diagnosis and management of inflammatory and/or autoimmune rheumatic disease.
Methods
We performed a registered systematic search (CRD42015025382) for studies using the MEDLINE (1946-August 2015), Embase (1974-August 2015), Web of Science (1900-August 2015), and Scopus (1946-August 2015) databases. We included studies which demonstrated the use of telemedicine for diagnosis and/or management of inflammatory/autoimmune rheumatic disease. Following data extraction, we performed a descriptive analysis.
Results
Our literature search identified 1,468 potentially eligible studies. Of these, 20 reports were ultimately included in this review. Studies varied significantly in publication type, quality of evidence, and the reporting of methods. Most demonstrated a high risk of bias. Rheumatoid arthritis was the most commonly studied rheumatic disease (42% of patients). Studies demonstrated conflicting results regarding the effectiveness of telemedicine (18 found it effective, one found it effective but possibly harmful, and one found it ineffective). A limited number of studies included some component of a cost analysis (n=6, 16% of patients); all of these found telemedicine to be cost-effective.
Conclusion
Studies identified by this systematic review generally found telemedicine to be effective for the diagnosis and management of autoimmune/inflammatory rheumatic disease; however, there is limited evidence to support this conclusion. Further studies are needed to determine the best uses of telemedicine for the diagnosis and management of these conditions.
Keywords: Systematic Review, Rheumatology, Telerheumatology, Telemedicine, Telehealth, Remote Consultation/methods, Health Services Accessibility, Diagnosis, Management, Rheumatic Diseases/diagnosis, Rheumatic Diseases/therapy
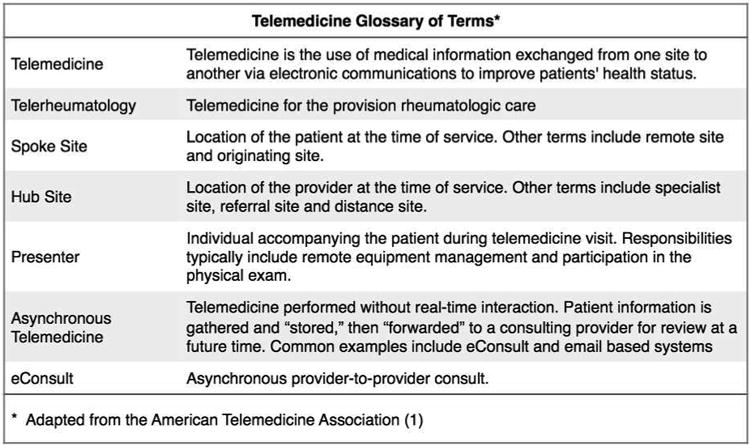
The past 20 years has seen an explosion in the utilization of telemedicine (TM) within both primary and subspecialty care. Loosely defined, TM is the use of communications technology for the provision of healthcare (1) (see Figure 1). Methods in TM vary widely, and may include telephone-based systems such as telephone triage, asynchronous methods such as eConsult and store-and-forward consults (e.g., as used to forward images to remote radiologists, dermatologists, and pathologists), as well as the more familiar video telecommunications (VTC) systems, in which both parties simultaneously see and hear one another.
Figure 1. Telemedicine Glossary.
The growth and increasing sophistication of TM has been made possible in part by the increasing availability of conventional high-speed internet connectivity, although satellite-based systems have played an important role in accessing remote areas for decades (2-7). The increased sophistication of TM's remote virtual examination has also been important. Now widely available, remote high-definition cameras, virtual stethoscopes, fiber optic clinical instruments and remote ultrasound have greatly expanded the range of TM's remote diagnostic capabilities.
The clinical applications of TM are diverse. A variety of clinical specialties now employ TM, including primary care (8-10), psychiatry (11,12), dermatology (6,13,14), infectious disease (15), diabetes management (16,17), neurology (18,19), cardiology (20,21), pain management (9), and others. TM is now commonly available in a variety of settings, including emergency departments (22), inpatient hospital wards (23), intensive care units (24), and even commercial pharmacies (25).
In the first published application of TM to rheumatology, Chase and Lisse described their experiences using TM for a series of 10 rheumatology consults within the Texas State prison system (26). During a 90-day period, a total of 10 new rheumatology consults were chosen at random and evaluated via real-time VTC. A prison physician acted as the “presenter,” or remote-site examiner, for all patient interviews. In addition to regular video, high definition cameras as well as remote-site virtual stethoscopes and other equipment were available. The authors felt their TM consults were “equal to in-site consultation,” and that both prison staff and the rheumatologist reported “satisfaction” with the service.
Despite this early success, several editorialists have questioned the value of telerheumatology. A commonly cited concern is telerheumatology's reliance on a remote physical exam by a non-specialist provider or “presenter” (27-29).
The objective of this study was to perform a systematic review to summarize the existing research in telerheumatology, highlighting salient features of study design, patient population, and TM methods as well as the study authors' conclusions. In this review we focus on TM in the management of inflammatory or autoimmune rheumatic disease, largely because of the greater complexities and risks involved with the TM-based management of these conditions. We hope this research will both summarize the literature to date and help inform future studies of telerheumatology.
Methods
Methods for study inclusion and data analysis were pre-specified in a registered protocol (PROSPERO 2015:CRD42015025382) and were consistent with major guidelines on the reporting of a systematic review (30). A glossary of the terms used in this study is provided in Figure 1.
Data Sources and Searches
A computerized literature search of the following databases was performed: MEDLINE (1946-July 2015), Embase (1974-July 2015), Web of Science (1900-July 2015), and Scopus (1946-July 2015). Additional studies were identified by a manual search of the published reference list of all studies included in this review. Details of the search strategy are available online in the Supplementary Appendix.
Study Selection
A three-step process was performed in parallel by two of the authors (EF and JM) to determine eligibility for inclusion. First, the full list of deduplicated files was reviewed and non-relevant studies excluded. Second, abstracts were obtained for studies deemed relevant by title. Finally, for relevant abstracts, full text studies were obtained and reviewed by two of the authors (EF and JM). Disagreements were arbitrated by a third reviewer when needed (LF).
Inclusion Criteria
To be included, studies must have used one or more methods of TM in an experimental fashion for either the diagnosis and/or management of patients diagnosed with, or referred for evaluation of, an autoimmune or inflammatory rheumatic disease. Only English language studies were considered. No a priori study publication date range restrictions were employed. Studies with patients of all ages were eligible for inclusion. All study types, including full length studies and brief reports, as well as abstracts from scientific meetings, were eligible. We included both observational and randomized studies. When a study did not provide an indication for referral or did not provide the final diagnosis, new patient consults from that study were assumed to have at least the potential for an autoimmune or inflammatory rheumatic diagnosis, and therefore were included in this review.
This study defined “telemedicine” and other TM terms in accordance with those of the American Telemedicine Association, namely as “the use of medical information exchanged from one site to another via electronic communications to improve a patient's clinical health status” (1). All methods of TM, i.e., asynchronous (eConsult, store-and-forward, email based, etc.) and synchronous (real-time telephone, radio or video), were included. Mobile health care services were eligible for inclusion if alerts resulted in real or potential action by a subject's providers. Studies of telephone triage systems as well as applications for remote self-monitoring were included if the trial outcomes evaluated, at least in part, the telephone triage system's effects on physician or provider disease management. Studies employing physicians, advanced practice nurses, physician associates, registered nurses or pharmacists as presenters were included.
Data Classification
Study Characteristics
The hub site (or specialist site) locations were obtained from the publication if listed. If unlisted, the hub site was assumed to be the municipality listed for the corresponding author, or the primary author if a corresponding author was not listed. Publication types were derived from the studies as listed; communications or letters were classified as brief reports. Trial methods lacking randomization were all classified as observational. Phase of care was classified as diagnosis or follow-up. Consult encounters were assumed to be for patients undergoing diagnosis, whereas follow-up encounters were assumed to be for patients previously diagnosed. Studies identifying both diagnosis and follow-up phases of care were extracted as not specified unless the number of patients for each phase was explicitly reported.
Telemedicine Methods and Characteristics
Communications methods were classified as using asynchronous approaches (examples include both store-and-forward and eConsult methods), standard telephone-based methods, smartphone based methods, or two-way real-time VTC. E-mail based systems were coded as asynchronous. Telephone interviews (both two and three-way) and standard telephone-based triage systems were coded as telephone-based. Texting or smartphone application-based methods were coded as smartphone. A study was coded as VTC when a video link between patient and specialist was employed. For VTC-based methods, a TM presenter, along with level of training, was extracted if provided. If a provider or other medical staff member was reported as present during a VTC but not recognized as a presenter in the methods, they were coded as a presenter. For non-VTC based studies, the presenter was listed as not applicable, in keeping with the definitions of presenter as defined elsewhere (1). The specialist (either rheumatologist or rheumatology clinic registered nurse) was noted and further classified by affiliation (academic) or geographic location if possible. If a study reported on TM costs or provided any kind of cost analysis, with or without supportive data, it was coded as positive for cost effectiveness assessment. Remote hardware was summarized if provided by the primary study. For telephone-based methods, remote hardware was listed as not applicable (no solely telephone-based studies included here used additional multi-media support). Network characteristics were classified as conventional internet, standard telephone, satellite-based, or not specified. ISDN (Integrated Services Digital Network) of any bandwidth was extracted as conventional internet. If satellite-based telecommunications were utilized at any point, the network was coded as satellite-based.
Disease Characteristics
Diseases were classified as inflammatory arthritis, connective tissue disease, gout, vasculitis, polymyalgia rheumatic, or primary disease not specified. Inflammatory arthritis was additionally sub-categorized as rheumatoid arthritis (RA) or other inflammatory arthritis, the latter including ankylosing spondylitis, psoriatic arthritis, and unspecified inflammatory arthritides. If no clear disease categorization could be derived, patients were classified as primary disease not specified.
Study Conclusions and Author Comments
A study conclusion (effective or ineffective) was extrapolated from each study, based on the statements of the authors within the text of their conclusion. Additional qualifiers (potentially harmful) were noted, if present.
Data Extraction
Data extraction was performed by one study author [JM], with patient counts, disease attributes, phase of care and details regarding TM methodology validated by a second [EF]. The extracted data and conclusions of the identified studies were then summarized qualitatively in a tabular format to provide a descriptive synthesis of the available literature.
Results
Using our search strategy (see Supplemental Appendix for details) a total of 1,468 non-duplicated abstracts were identified (see Figure 2). Of these, 1,376 were excluded based on title or abstract review alone. For the 92 studies remaining, 66 were excluded following a full text review: four studies were excluded for having fewer than 10 total inflammatory/autoimmune patients (31-34), and the remainder excluded for failing to meet other inclusion criteria. Additionally, three studies were excluded during data extraction for having identical data published in two different sources (4,35,36). One study was added following a manual search of the references of the included studies (37). Thus, a total of 20 studies were ultimately included in this systematic review.
Figure 2. Flow Diagram of Search Results.
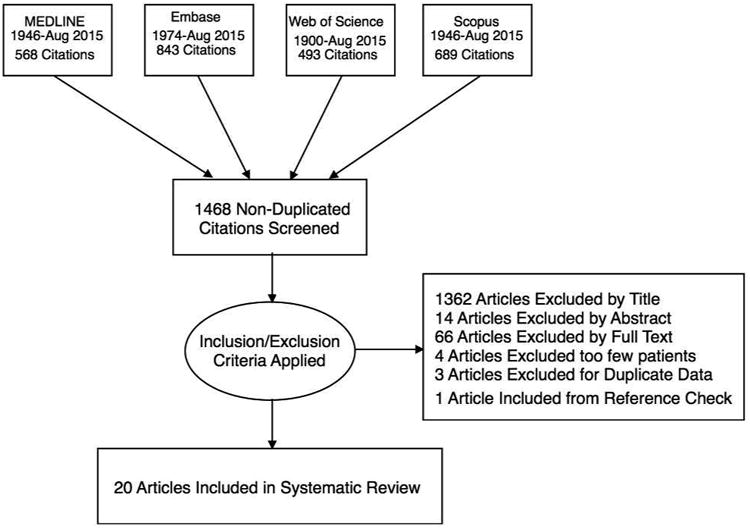
Table 1 summarizes the general characteristics of the studies identified by our search. A total of 1,430 patients with inflammatory or autoimmune rheumatic conditions were included across 20 the studies found. Most studies were published prior to 2010 (n=12). The majority of studies (n=11) and patients (n=986, 69%) were from Europe. With the exception of one randomized trial (38), the risk of bias was high across all studies, due to their observational design (n=19). Half of the included studies (n=10) and their respective patients (n=1,040, 73%) were published in abstract form only. The single randomized trial found in this review included baseline demographics only; no patient outcome data following TM consult were provided (38). Nine studies used telerheumatology exclusively for diagnosis, four used it exclusively for follow-up visits, and three studies used it for both; three studies did not specify the phase of care (data not shown). The number of patients seen for diagnosis (n=481, 34%) was smaller than those seen in follow-up (n=859, 60%); a minority of patients (n=90, 6%) did not have an identified phase of care. One study, a non-randomized prospective trial of VTC, administered a survey to the spoke site primary care physicians (7). They reported a high degree of satisfaction with telerheumatology services among the participating physicians, but did not collect any patient reported outcomes.
Table 1. General characteristics of telerheumatology studies.
| Studies, n | Patients, n | % Total Patients | |
|---|---|---|---|
| Overall Totals | 20 | 1430 | 100% |
| Date of Publication | |||
| 2010-2015 | 8 | 730 | 51% |
| Prior to 2010 | 12 | 700 | 49% |
| Hub Site Location | |||
| North America | 8 | 395 | 28% |
| Europe/Great Britain | 11 | 986 | 69% |
| Australia & New Zeland | 1 | 49 | 3% |
| Publication Type | |||
| Full Length Article | 7 | 258 | 18% |
| Brief Report | 3 | 132 | 9% |
| Abstract | 10 | 1040 | 73% |
| Trial Method | |||
| RCT | 1 | 46 | 3% |
| Observational | 19 | 1384 | 97% |
| Phase of Care * | |||
| Diagnosis/New Consult | 12 | 481 | 34% |
| Follow-up/Maintenance | 7 | 859 | 60% |
| Not specified | 3 | 90 | 6% |
A single trial may have included multiple phases of care
Table 2 describes the specific TM features used. The majority of studies employed VTC (n=12), followed by telephone-based methods (n=6), and asynchronous methods (n=3). One study used a smartphone-based method. (Note: some studies used more than one method.) Of the studies using VTC, TM presenters varied widely in training, and included physicians [studies n=8, patients n=332 (23%)] as well as nurses and physical therapists [studies n=3, patients n=106 (7%)]. Two VTC studies did not specify the use or training of presenters (39,40). Six studies (with 16% of total patients) included a statement of cost-effectiveness or some components of a cost-benefit analysis. No study identified by this systematic review employed rigorous cost-benefit methods.
Table 2. Telemedicine characteristics of included studies.
| Studies n | Patients (n) | % Total Patients | |
|---|---|---|---|
| Communications Method * | |||
| A synchronous | 3 | 210 | 15% |
| Telephone-Based | 6 | 631 | 44% |
| Smartphone | 1 | 137 | 10% |
| VTC | 12 | 484 | 34% |
| VTC Patient Presenter | |||
| Physician | 8 | 332 | 23% |
| RN, PT, Med Tech | 3 | 106 | 7% |
| Not specified | 2 | 68 | 5% |
| Cost Analysis Attempted | |||
| Yes | 6 | 226 | 16% |
Studies/patients may have been counted more than once per trial
Table 3 reviews patient disease characteristics for the studies included in this review. Inflammatory arthritis was the most common rheumatologic diagnosis reported (n=859, 60%), with the majority of these classified as RA (n=598, 42%). Other inflammatory arthritis diagnoses (psoriatic arthritis, ankylosing spondylitis, other spondyloarthropathies) were diagnosed in 261 (18%) patients. Only 62 (4%) of the patients were diagnosed with a connective tissue disease (systemic lupus erythematosus, scleroderma, etc.). Patients with gout (n=11) and vasculitis or polymyalgia rheumatica (n=23) made up 1% and 2% respectively of the total number of patients.The patient final diagnosis was not discernible (i.e., primary disease not specified) in 34% (n=486).
Table 3. Disease characteristics of included studies.
| Patients (n) | % Total Patients | |
|---|---|---|
| Inflammatory Arthritis | 859 | 60% |
| RA | 598 | 42% |
| Other IA | 261 | 18% |
| Connective Tissue Disease | 62 | 4% |
| Gout | 11 | 1% |
| Vasculitis/PMR | 23 | 2% |
| Primary Disease Not Specified | 486 | 34% |
Table 4 summarizes the 20 studies identified by our search, highlighting the study characteristics, patient populations, rheumatic diseases, phase of care, TM methods, and general conclusions. Study duration varied significantly (min=3 months, max=9 years; average=15 months). Six studies did not specify their duration. A total of 17 trials found telerheumatology to be effective. One trial concluded telerheumatology to be effective through improving access to care, yet also possibly harmful, as indicated by a potential delay initiation of DMARD therapy when synovitis goes unrecognized (41). One trial evaluating the use of a low-resolution camera for inpatient telerheumatology consults found this intervention ineffective (42).
Table 4. List of telerheumatology studies.
| Author / Year | Study Characteristics | Diseases | Telemedicine Methods | Author's Conclusion |
|---|---|---|---|---|
| Chalmers A, and Arnold H 2010 (64) | Design: Prospective observational Duration: 4 months Pub Type: Abstract Patients: 28 Hub: Vancouver, Canada |
IA, CTD | Phase of Care: Diagnosis, follow-up Method: Two way VTC Remote Hardware: Remote site high resolution still camera Network: Not specified Specialist: Academic rheumatologist Presenter: Physiotherapist trained in joint assessment |
Effective |
| Chase J, et al. 1995 (26) | Design: Prospective observational Duration: 3 months Pub Type: Abstract Patients: 10 Hub: Galveston, Texas |
Not specified | Phase of Care: Not Specified Method: Two way VTC Remote Hardware: Multiple remote site cameras, stethoscope Network: Not specified Specialist: Academic rheumatologist Presenter: Physician |
Effective |
| Davis P, et al. 2001 (5) | Design: Prospective observational Duration: 6 months Pub Type: Full length article Patients: 27 Hub: Edmonton, Canada |
IA, CTD | Phase of Care: Diagnosis Method: Two way VTC Remote Hardware: High resolution still camera Network: Satellite Specialist: Academic rheumatologist Presenter: Physician |
Effective |
| Graham LE, McGimpsey, et al. 2000 (42) | Design: Prospective observational Duration: 4 months Pub Type: Brief Report Patients: 17 Hub: Belfast, Ireland |
IA, CTD | Phase of Care: Diagnosis Method: Telephone, followed by two way VTC Remote Hardware: Low resolution video with still image freeze Network: Conventional telephone Specialist: Academic rheumatologist Presenter: Physician |
Ineffective |
| Hampson R, et al. 2003 (36) | Design: Prospective observational Duration: 6 months Pub Type: Abstract Patients: 154 Hub: Glasgow, United Kingdom |
IA | Phase of Care: Follow-Up Method: Telephone Remote Hardware: NA Network: Conventional telephone Specialist: NA Presenter: NA |
Effective |
| Jong M, et al. 2004 (7) | Design: Prospective observational Duration: 5 months Pub Type: Full length article Patients: 0 Hub: St. John's, Newfoundland, CA |
Not specified | Phase of Care: Diagnosis Method: Two-way VTC, store-and-forward, visiting clinic Remote Hardware: Not specified Network: Satellite Specialist: Academic rheumatologist Presenter: Physician |
Effective |
| Kulcsar Z, et al. 2014 (41) | Design: Retrospective analysis Duration: 16 months Pub Type: Abstract Patients: 11 Hub: Lebanon, New Hampshire |
IA, gout | Phase of Care: Not Specified Method: Two-way VTC Remote Hardware: Not specified Network: Not specified Specialist: Academic rheumatologist Presenter: RN/PT/MA |
Effective, potentially harmful |
| LeClercq S, et al. 2008 (47) | Design: Prospective observational Duration: 2 years Pub Type: Abstract Patients: 195 Hub: Calgary, Alberta |
IA | Phase of Care: Diagnosis, follow-up Method: Two-way VTC Remote Hardware: Not specified Network: Conventional telephone Specialist: Academic rheumatologist Presenter: Physician |
Effective |
| Leggett P, et al. 2001 (56) | Design: Prospective observational Duration: Not specified Pub Type: Brief Report Patients: 15 Hub: Belfast, Ireland |
Not specified | Phase of Care: Diagnosis Method: Telephone, followed by two-way VTC Remote Hardware: High resolution close-up camera Network: Conventional internet Specialist: Academic rheumatologist Presenter: Physician |
Effective |
| McManus J, et al. 2008 (65) | Design: Retrospective analysis Duration: 3.5 years Pub Type: Full length article Patients: 28 Hub: Multiple |
Not specified | Phase of Care: Diagnosis Method: Store-and-foreward Remote Hardware: Still image capture Network: Not specified Specialist: United States rheumatologists Presenter: NA |
Effective |
| McNamara S, et al. 2011 (39) | Design: Prospective observational Duration: Not specified Pub Type: Abstract Patients: 19 Hub: Galway, Ireland |
Not specified | Phase of Care: Diagnosis Method: Two-way VTC Remote Hardware: Laptop computer Network: Not specified Specialist: Rheumatologist Presenter: Not specified |
Effective |
| Pal B, et al. 1999 (66) | Design: Prospective observational Duration: Not specified Pub Type: Full length article Patients: 86 Hub: Manchester, England |
IA, CTD, gout, PMR/vasculitis | Phase of Care: Diagnosis Method: Store-and-Foreward Remote Hardware: Not specified Network: Not specified Specialist: Academic rheumatologist Presenter: NA |
Effective |
| Pal, B 1998 (37) | Design: Prospective observational Duration: 1 year Pub Type: Brief report Patients: 100 Hub: Manchester, UK |
IA, CTD, gout, PMR/vasculitis | Phase of Care: Follow-Up Method: Telephone Remote Hardware: NA Network: Conventional telephone Specialist: Academic rheumatologist Presenter: NA |
Effective |
| Platford L, et al. 2012 (49) | Design: Prospective observational Duration: 1 year Pub Type: Abstract Patients: 67 Hub: Grampian, Scotland |
Not specified | Phase of Care: Not Specified Method: Two-way VTC Remote Hardware: Not specified Network: Not specified Specialist: Rheumatologist Presenter: RN/PT/MA |
Effective |
| Poulsen KA, et al. 2015 (40) | Design: Prospective observational Duration: 1 year Pub Type: Full length article Patients: 49 Hub: Townsville, Australia |
Not specified | Phase of Care: Diagnosis, follow-up Method: Two-way VTC Remote Hardware: Not specified Network: Not specified Specialist: Rheumatologist Presenter: Not specified |
Effective |
| Puolakka K, et al. 2012 (53) | Design: Retrospective analysis Duration: Not specified Pub Type: Abstract Patients: 137 Hub: Lappeenranta, Finland |
IA | Phase of Care: Follow-Up Method: Smartphone Remote Hardware: Not specified Network: Cellphone Specialist: Academic rheumatologist Presenter: NA |
Effective |
| Saiz M, et al. 2013 (54) | Design: Retrospective analysis Duration: 11 months Pub Type: Abstract Patients: 323 Hub: Valencia, Spain |
IA, CTD, PMR/vasculitis | Phase of Care: Follow-Up Method: Telephone Remote Hardware: NA Network: Conventional telephone Specialist: Rheumatology Clinic RN Presenter: NA |
Effective |
| Scalvini S, et al. 2009 (48) | Design: Prospective observational Duration: 1 year Pub Type: Full length article Patients: 22 Hub: Cremonia, Italy |
Not specified | Phase of Care: Diagnosis, follow-up Method: Telephone Remote Hardware: NA Network: Conventional internet Specialist: Regional rheumatologist Presenter: Physician |
Effective |
| Schmidt T, et al. 2014 (50) | Design: Retrospective analysis Duration: 9 years Pub Type: Abstract Patients: 96 Hub: San Antonio, Texas |
IA, CTD | Phase of Care: Diagnosis Method: eConsult Remote Hardware: Not specified Network: Not specified Specialist: Academic rheumatologist Presenter: NA |
Effective |
| Wallace P, et al. 2002 (38) | Design: Randomized Trial Duration: 6 months Pub Type: Full length article Patients: 46 Hub: London, England |
Not specified | Phase of Care: Diagnosis Method: Two-way VTC Remote Hardware: Not specified Network: Conventional internet Specialist: Rheumatologist Presenter: Physician |
Inconclusive |
Discussion
To the best of our knowledge, we have conducted the first systematic review of TM for the management of inflammatory and autoimmune rheumatic diseases. This study both highlights areas of opportunity and identifies a need for further research. A relatively small number of studies have been published to date. In general, most study authors find telerheumatology to be effective, although data supporting this conclusion remain limited (43).
Interest in TM arose in part as a means to improve access to care in rural populations (2,3,44-46), and improving the accessibility of rheumatology care was a frequently cited goal of the studies included in this review (5,7,26,40,41,47-50). Limited access to care in rheumatology is likely to persist, both due to existing regional workforce shortages (51) as well as to a growing shortage of rheumatology providers (52).
As with TM more generally, an evidence gap exists for the research and implementation of telerheumatology. Research is needed to best determine under which rheumatologic conditions, and at what phase in care, telerheumatology is likely to be most valuable. Our systematic review found RA to be the most common diagnosis studied (n=598, see Table 3), with the majority of patients (538, or 90%) evaluated in follow-up (data not shown). Thirteen studies included here evaluated patients at diagnosis. Although 10 of these found diagnosis by telerheumatology to be effective, one study found that TM may actually delay initiation of disease-modifying therapy (41). Few patients were diagnosed with rheumatic diseases other than inflammatory arthritis, such as connective tissue disease, vasculitis and gout. For example, only 35 patients, or about 7% of the total number of patients seen at diagnosis, were diagnosed with a connective tissue disease (data not shown).
Some of the study authors included in this review (53,54) make an important distinction between telerheumatology used to diagnose new disease versus its use in the management of established conditions. Diagnosis of a new condition may require a higher level of confidence in the physical exam. A common criticism of telerheumatology is its reliance on proxy examination performed by presenters with varying levels of training. Martin-Khan et al. reviewed observer agreement in specialist TM, finding only one study evaluating the diagnostic accuracy of the remote musculoskeletal exam (55). Leggett et al. (56), also included in this review, examined the diagnostic accuracy of 100 patients in a non-randomized study. Patients were initially interviewed by a single rheumatologist: first by telephone, followed by a VTC session and then finally in person. Diagnostic accuracy was poor by telephone only (kappa = 0.62) but improved significantly with VTC (kappa = 0.96). Weakness within the study design, however, limits the utility of these otherwise encouraging results.
Similarly, of the eight studies using physician presenters included in this review, seven concluded that diagnosis by telerheumatology to be effective (5,7,26,38,47,48,56), whereas Graham et al. found a low-resolution bedside video camera ineffective (42). Only two of these studies, however, went on to confirm the accuracy of the diagnosis using a face-to-face “gold standard” office visit (42,56). In contrast to these findings, one study using an untrained presenter found that VTC was not effective in detecting synovitis, leading to an average 11-week delay in initiating disease-modifying therapy (41). These results highlight the need for additional research on the training and use of musculoskeletal VTC presenters in telerheumatology.
Important to the evaluation and implementation of TM, including telerheumatology, is cost. Initial investment in TM equipment and personnel can be significant, and the need for satellite communications or dedicated internet may further increase monthly expenses. An early cost-comparison study of an established outpatient orthopedic and dermatology TM system at the University of Michigan predicted a 21% reduction in per-visit costs, but at a substantial cost to society due to increases in specialty care volume (57). In addition, this same study also found the primary beneficiary of cost savings were both patients (from lower travel costs) and employers (from improved employee productivity), whereas the bulk of the financial risk of telemedicine was carried by the medical providers who invested in TM equipment and infrastructure. More recently, a 2012 systematic review determined there was insufficient evidence to conclude that TM is cost-effective (58). A framework for evaluating the costs and benefits of TM was first published in 1995 (59), although widespread reporting of TM-related costs has yet to occur (60). In our systematic review,none of the articles included used robust methods for cost-effectiveness (61,62). Including cost analysis in future research is an important step toward the rational implementation of telerheumatology.
Precise reporting of telerheumatology methods is generally lacking. While no widely adopted standard for TM methods is currently in use, reporting the TM modality (asynchronous, VTC), phase of care (diagnosis versus follow-up) and basic technical specifications of the study (remote hardware and accessories, network characteristics) may assist with future cost analysis and study replication. Making note of a VTC presenter's level of training (e.g., physician, physical therapist, RN or other), along with any musculoskeletal training (if provided), will help future research clarify the importance of this position vis-à-vis patient outcomes and cost estimates.
Mobile or smartphone-based telemonitoring of rheumatic disease represents an application of TM distinct from patient-specialist VTC or telephone-based TM encounters discussed thus far. The evidence for smartphone-based methods for rheumatic disease self-management was recently reviewed by Azevedo et al. (63), highlighting the current patient-focused use of this technology. For unclear reasons, interoperable smartphone applications - where patient data is passed from phone to a specialist's electronic medical records system - appear to be much less common in the rheumatic diseases. Our review identified only one Smartphone-based RA telemonitoring study where patient data was forwarded/collected for provider review, resulting in changes in management (53).
In summary, our study reviews the existing literature on the use of TM for the diagnosis and management of inflammatory and autoimmune rheumatic disease. Most data relate to the management of inflammatory arthritis during follow-up. Studies to date are at high risk of bias, use predominately VTC telerheumatology, and include physicians as the patient presenter. TM reporting methods varied widely and rigorous cost analyses are lacking. Most studies viewed telerheumatology favorably, with one notably stating a potential for harm. Additional research is needed to clarify the specific contexts in which telerheumatology will improve the delivery of care for patients with known or suspected inflammatory or autoimmune rheumatic disease.
Significance and Innovations.
Randomized trials and cost-effectiveness analysis evaluating telerheumatology are lacking
This study reveals a generally favorable opinion of telerheumatology within a limited body of evidence
The effectiveness of telemedicine in rheumatology may vary by disease, phase of care, and by the telemedicine methods used
Acknowledgments
Financial Support: Financial support for this study was provided in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health, under Award Number AR060231-01 (Fraenkel). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding agreement ensured the authors' independence in designing the study, interpreting the data, writing, and publishing the report.
Footnotes
Conflict of Interest/Disclosures: None
Contributor Information
John A. McDougall, Yale University School of Medicine, Section of Rheumatology.
Elizabeth D Ferucci, Alaska Native Tribal Health Consortium, Community Health Services.
Janis Glover, Yale University Sterling Memorial Library, Medical Library.
Liana Fraenkel, Yale University, Dept. of Internal Medicine, Section of Rheumatology.
References
- 1.Nomenclature. [Accessed February 8, 2016];American Telemedicine Association. Available at: http://www.americantelemed.org/resources/nomenclature#.Vqo3yMdVedU.
- 2.Hudson HE, Parker EB. Medical communication in Alaska by satellite. N Engl J Med. 1973;289:1351–1356. doi: 10.1056/NEJM197312202892506. [DOI] [PubMed] [Google Scholar]
- 3.Foote DR. Satellite communication for rural health care in Alaska. J Commun. 1977;27:173–182. doi: 10.1111/j.1460-2466.1977.tb01874.x. [DOI] [PubMed] [Google Scholar]
- 4.Davis P. An evaluation of telehealth technology in provision of distant and global rheumatology consults. J Rheumatol. 2001;28:75–75. [PubMed] [Google Scholar]
- 5.Davis P, Howard R, Brockway P. An evaluation of telehealth in the provision of rheumatologic consults to a remote area. J Rheumatol. 2001;28:1910–1913. [PubMed] [Google Scholar]
- 6.Kanthraj GR, Srinivas CR. Store and forward teledermatology. Indian J Dermatol Venereol Leprol. 2007;73:5–12. doi: 10.4103/0378-6323.30643. [DOI] [PubMed] [Google Scholar]
- 7.Jong M, Kraishi M. A comparative study on the utility of telehealth in the provision of rheumatology services to rural and northern communities. Int J Circumpolar Health. 2004;63:415–421. doi: 10.3402/ijch.v63i4.17758. Available at: http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=15709316&retmode=ref&cmd=prlinks. [DOI] [PubMed] [Google Scholar]
- 8.Vidrine JI, Shete S, Cao Y, Greisinger A, Harmonson P, Sharp B, et al. Ask-Advise-Connect: a new approach to smoking treatment delivery in health care settings. JAMA Intern Med. 2013;173:458–464. doi: 10.1001/jamainternmed.2013.3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kroenke K, Krebs EE, Wu J, Yu Z, Chumbler NR, Bair MJ. Telecare collaborative management of chronic pain in primary care: a randomized clinical trial. JAMA. 2014;312:240–248. doi: 10.1001/jama.2014.7689. [DOI] [PubMed] [Google Scholar]
- 10.Daniel H, Sulmasy LS. Health and Public Policy Committee of the American College of Physicians. Policy Recommendations to Guide the Use of Telemedicine in Primary Care Settings: An American College of Physicians Position Paper. Ann Intern Med. 2015;163:787–789. doi: 10.7326/M15-0498. [DOI] [PubMed] [Google Scholar]
- 11.Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry. 2013;170:256–262. doi: 10.1176/appi.ajp.2012.12081064. [DOI] [PubMed] [Google Scholar]
- 12.Fortney JC, Pyne JM, Mouden SB, Mittal D, Hudson TJ, Schroeder GW, et al. Practice-based versus telemedicine-based collaborative care for depression in rural federally qualified health centers: a pragmatic randomized comparative effectiveness trial. Am J Psychiatry. 2013;170:414–425. doi: 10.1176/appi.ajp.2012.12050696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Norton SA, Burdick AE, Phillips CM, Berman B. Teledermatology and underserved populations. Arch Dermatol. 1997;133:197–200. [PubMed] [Google Scholar]
- 14.Barbieri JS, Nelson CA, James WD, Margolis DJ, Littman-Quinn R, Kovarik CL, et al. The reliability of teledermatology to triage inpatient dermatology consultations. JAMA Dermatol. 2014;150:419–424. doi: 10.1001/jamadermatol.2013.9517. [DOI] [PubMed] [Google Scholar]
- 15.León A, Cáceres C, Fernández E, Chausa P, Martin M, Codina C, et al. A new multidisciplinary home care telemedicine system to monitor stable chronic human immunodeficiency virus-infected patients: a randomized study. PLoS ONE. 2011;6:e14515. doi: 10.1371/journal.pone.0014515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhai YK, Zhu WJ, Cai YL, Sun DX, Zhao J. Clinical- and cost-effectiveness of telemedicine in type 2 diabetes mellitus: a systematic review and meta-analysis. Medicine (Baltimore) 2014;93:e312. doi: 10.1097/MD.0000000000000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mansberger SL, Sheppler C, Barker G, Gardiner SK, Demirel S, Wooten K, et al. Long-term Comparative Effectiveness of Telemedicine in Providing Diabetic Retinopathy Screening Examinations: A Randomized Clinical Trial. JAMA Ophthalmol. 2015;133:518–525. doi: 10.1001/jamaophthalmol.2015.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Demaerschalk BM, Miley ML, Kiernan TEJ, Bobrow BJ, Corday DA, Wellik KE, et al. Stroke telemedicine. Mayo Clin Proc. 2009;84:53–64. doi: 10.4065/84.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wechsler LR. Advantages and limitations of teleneurology. JAMA Neurol. 2015;72:349–354. doi: 10.1001/jamaneurol.2014.3844. [DOI] [PubMed] [Google Scholar]
- 20.Melnyk SD, Zullig LL, McCant F, Danus S, Oddone E, Bastian L, et al. Telemedicine cardiovascular risk reduction in veterans. American Heart Journal. 2013;165:501–508. doi: 10.1016/j.ahj.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bove AA, Homko CJ, Santamore WP, Kashem M, Kerper M, Elliott DJ. Managing hypertension in urban underserved subjects using telemedicine--a clinical trial. American Heart Journal. 2013;165:615–621. doi: 10.1016/j.ahj.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 22.Telemedicine in Emergency Medicine. American College of Emergency Physicians. 2000:1–13. Available at: http://www.acep.org/workarea/DownloadAsset.aspx?id=8988.
- 23.Sanders RB, Simpson KN, Kazley AS, Giarrizzi DP. New hospital telemedicine services: potential market for a nighttime telehospitalist service. Telemed J E Health. 2014;20:902–908. doi: 10.1089/tmj.2013.0344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kahn JM, Cicero BD, Wallace DJ, Iwashyna TJ. Adoption of ICU telemedicine in the United States. Critical Care Medicine. 2014;42:362–368. doi: 10.1097/CCM.0b013e3182a6419f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CVS Health to Partner with Direct-to-Consumer Telehealth Providers to Increase Access to Physician Care. CVS Health. [Accessed February 8, 2016]; Available at: https://www.cvshealth.com/content/cvs-health-partner-direct-consumer-telehealth-providers-increase-access-physician-care.
- 26.Chase JL, Llsse JR, Brecht RM. Rheumatology in the 21st Century - Telemedicine Leading the Way. Arthritis Rheum. 1995;38:R39–R39. [Google Scholar]
- 27.Sanders PA. Cyberclinic in rheumatology. J R Coll Physicians Lond. 1999;33:400–401. [PMC free article] [PubMed] [Google Scholar]
- 28.Lewtas J. Telemedicine in rheumatology. J Rheumatol. 2001;28:1745–1746. [PubMed] [Google Scholar]
- 29.Rothschild B. Telerheumatology: not ready for prime time. Intern Med J. 2013;43:468–469. doi: 10.1111/imj.12052. [DOI] [PubMed] [Google Scholar]
- 30.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 31.Huston JL, Burton DC. Patient satisfaction with multispecialty interactive teleconsultations. J Telemed Telecare. 1997;3:205–208. doi: 10.1258/1357633971931174. [DOI] [PubMed] [Google Scholar]
- 32.Vassallo DJ, Hoque F, Roberts MF, Patterson V, Swinfen P, Swinfen R. An evaluation of the first year's experience with a low-cost telemedicine link in Bangladesh. J Telemed Telecare. 2001;7:125–138. doi: 10.1258/1357633011936273. [DOI] [PubMed] [Google Scholar]
- 33.Melcer T, Crann B, Hunsaker D, Deniston W, Caola L. A retrospective evaluation of the development of a telemedicine network in a military setting. Mil Med. 2002;167:510–515. [PubMed] [Google Scholar]
- 34.Singh M, Das RR. Utility of telemedicine for children in India. Indian J Pediatr. 2010;77:73–75. doi: 10.1007/s12098-009-0292-x. [DOI] [PubMed] [Google Scholar]
- 35.Pal B. Tele-rheumatology: telephone follow up and cyberclinic. Comput Methods Programs Biomed. 2001;64:189–195. doi: 10.1016/s0169-2607(00)00138-3. [DOI] [PubMed] [Google Scholar]
- 36.Hampson R, Tierney A, Capell HA, Madhok R. Evaluation of an interactive intelligent telephone based monitoring system for patients with rheumatoid arthritis (RA) Arthritis Rheum. 2003;48:S460–S460. [Google Scholar]
- 37.Pal B. Following up outpatients by telephone: pilot study. BMJ. 1998;316:1647. doi: 10.1136/bmj.316.7145.1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wallace P, Haines A, Harrison R, Barber JA, Thompson S, Roberts J, et al. Design and performance of a multi-centre randomised controlled trial and economic evaluation of joint tele-consultations [ISRCTN54264250] BMC Fam Pract. 2002;3:1. doi: 10.1186/1471-2296-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McNamara S, O'Neill L, Carey JJ, Coughlan RJ. Validation of electronic audiovisual media assessments of patients with rheumatic diseases. Irish Journal of Medical Science. 2011;180:S195. [Google Scholar]
- 40.Poulsen KA, Millen CM, Lakshman UI, Buttner PG, Roberts LJ. Satisfaction with rural rheumatology telemedicine service. Int J Rheum Dis. 2015;18:304–314. doi: 10.1111/1756-185X.12491. [DOI] [PubMed] [Google Scholar]
- 41.Kulcsar Z, Albert DA, Merrihew K, Mecchella J. Tele-rheumatology: Despite improved access could there be a potential delay in care without a skilled “presenter”? Arthritis & Rheumatology. 2014;66:S1008–S1009. [Google Scholar]
- 42.Graham LE, McGimpsey S, Wright S, McClean G, Carser J, Stevenson M, et al. Could a low-cost audio-visual link be useful in rheumatology? J Telemed Telecare. 2000;6(1):S35–7. doi: 10.1258/1357633001934078. [DOI] [PubMed] [Google Scholar]
- 43.Askling J, Baecklund E, Granath F, Geborek P, Fored M, Backlin C, et al. Anti-tumour necrosis factor therapy in rheumatoid arthritis and risk of malignant lymphomas: relative risks and time trends in the Swedish Biologics Register. Ann Rheum Dis. 2009;68:648–653. doi: 10.1136/ard.2007.085852. [DOI] [PubMed] [Google Scholar]
- 44.Bashshur RL, Shannon G. History of Telemedicine: Evolution, Context, and Transformation. New Rochelle (NY): Mary Ann Liebert, Inc; 2009. [Google Scholar]
- 45.Dhillon HS, Doermann AC, Walcoff P. Telemedicine and rural primary health care: an analysis of the impact of telecommunications technology. Socioecon Plann Sci. 1978;12:37–48. doi: 10.1016/0038-0121(78)90020-4. [DOI] [PubMed] [Google Scholar]
- 46.Freiburger G, Holcomb M, Piper D. The STARPAHC collection: part of an archive of the history of telemedicine. J Telemed Telecare. 2007;13:221–223. doi: 10.1258/135763307781458949. [DOI] [PubMed] [Google Scholar]
- 47.LeClercq S, Martin L, Connors S. Arthritis consultation utilizing telehealth in southern Alberta; a 2 year pilot project. J Rheumatol. 2008;35:1193–1194. [Google Scholar]
- 48.Scalvini S, Tridico C, Glisenti F, Giordano A, Pirini S, Peduzzi P, et al. The SUMMA Project: a feasibility study on telemedicine in selected Italian areas. Telemed J E Health. 2009;15:261–269. doi: 10.1089/tmj.2008.0109. [DOI] [PubMed] [Google Scholar]
- 49.Platford L, Macdonald A, Kumar P. Rheumatology televideoclinic service in Orkney: survey of patient satisfaction questionnaire. Scottish Medical Journal. 2012;57:115–116. [Google Scholar]
- 50.Schmidt T, Lappan C, Battafarano D. Rheumatology E-consult services: A rheumatology workforce management model. Arthritis & Rheumatology. 2014;66:S44. [Google Scholar]
- 51.American College of Rheumatology Committee on Rheumatology Training and Workforce Issues. FitzGerald JD, Battistone M, Brown CR, Cannella AC, Chakravarty E, et al. Regional distribution of adult rheumatologists. Arthritis Rheum. 2013;65:3017–3025. doi: 10.1002/art.38167. [DOI] [PubMed] [Google Scholar]
- 52.Deal CL, Hooker R, Harrington T, Birnbaum N, Hogan P, Bouchery E, et al. The United States rheumatology workforce: supply and demand, 2005-2025. Arthritis Rheum. 2007;56:722–729. doi: 10.1002/art.22437. [DOI] [PubMed] [Google Scholar]
- 53.Puolakka K, Sokka T, Kautiainen H. Cell phone based automated monitoring of patients with early rheumatoid arthritis. Arthritis Rheum. 2012;64:S163–S164. [Google Scholar]
- 54.Telephonic rheumatologist nurse consulting: 1 year time experience. Ann Rheum Dis. 2013;71 [Google Scholar]
- 55.Martin-Khan M, Wootton R, Whited J, Gray LC. A systematic review of studies concerning observer agreement during medical specialist diagnosis using videoconferencing. J Telemed Telecare. 2011;17:350–357. doi: 10.1258/jtt.2011.101113. [DOI] [PubMed] [Google Scholar]
- 56.Leggett P, Graham L, Steele K, Gilliland A, Stevenson M, O'Reilly D, et al. Telerheumatology--diagnostic accuracy and acceptability to patient, specialist, and general practitioner. Br J Gen Pract. 2001;51:746–748. [PMC free article] [PubMed] [Google Scholar]
- 57.Stensland J, Speedie SM, Ideker M, House J, Thompson T. The relative cost of outpatient telemedicine services. Telemed J. 1999;5:245–256. doi: 10.1089/107830299311998. [DOI] [PubMed] [Google Scholar]
- 58.Mistry H. Systematic review of studies of the cost-effectiveness of telemedicine and telecare. Changes in the economic evidence over twenty years J Telemed Telecare. 2012;18:1–6. doi: 10.1258/jtt.2011.110505. [DOI] [PubMed] [Google Scholar]
- 59.Bashshur RL. Telemedicine effects: cost, quality, and access. J Med Syst. 1995;19:81–91. doi: 10.1007/BF02257059. [DOI] [PubMed] [Google Scholar]
- 60.World Health Organization. Telemedicine: Opportunities and Developments in Member States. Available at: http://www.who.int/goe/publications/goe_telemedicine_2010.pdf.
- 61.Dávalos ME, French MT, Burdick AE, Simmons SC. Economic evaluation of telemedicine: review of the literature and research guidelines for benefit-cost analysis. Telemed J E Health. 2009;15:933–948. doi: 10.1089/tmj.2009.0067. [DOI] [PubMed] [Google Scholar]
- 62.Edejer T. Making choices in health: WHO guide to cost-effectiveness analysis. 2003 [Google Scholar]
- 63.Azevedo ARP, de Sousa HML, Monteiro JAF, Lima ARNP. Future perspectives of Smartphone applications for rheumatic diseases self-management. Rheumatol Int. 2015;35:419–431. doi: 10.1007/s00296-014-3117-9. [DOI] [PubMed] [Google Scholar]
- 64.Chalmers A, Arnold H. The implementation and evaluation of a pilot project in telerheumatology. J Rheumatol. 2010;2:1323. [Google Scholar]
- 65.McManus J, Salinas J, Morton M, Lappan C, Poropatich R. Teleconsultation program for deployed soldiers and healthcare professionals in remote and austere environments. Prehosp Disaster Med. 2008;23:210–6. discussion 217. [PubMed] [Google Scholar]
- 66.Pal B, Laing H, Estrach C. A cyberclinic in rheumatology. J R Coll Physicians Lond. 1999;33:161–162. [PMC free article] [PubMed] [Google Scholar]


