Abstract
Purpose
Retinitis pigmentosa (RP) is the most common retinal degeneration causing blindness. Although their clinical problems are amenable for the clinical diagnosis, their day-to-day problems for having to live with the disease are mostly unexplored. This study aims to explore and understand the issues and impact of people with RP on quality of life (QoL).
Methods
A qualitative research methodology to facilitate the understanding of the experiences of people with RP was carried out. Data were collected through audio-recorded semi-structured interviews. Thematic analysis occurred through the process of line-by-line coding, aggregation, and theme development using the NVivo-10 software.
Results
Twenty-three interviews were conducted (mean age=56 years; females, 14). We identified five major QoL themes: (1) struggle to perform important day-to-day tasks; (2) concerns about disease progression, disease outcome and personal safety; (3) facing a lot of emotional and psychological challenges; (4) experiencing a myriad of visual symptoms; and (5) adopting different strategies to cope and manage stressful circumstances. Difficulty in performing important day-to-day tasks was the most prominent QoL issue among these people. Their major concerns were going blind and uncertainties about their future. They face a lot of emotional and psychological challenges to adapt to the physiological stress associated with the progressive vision loss. However, they adopt several coping strategies to manage the stressful circumstances.
Conclusions
People with RP experience a myriad of QoL issues. Despite all the hardship, they remain optimistic and learn to accept their eye condition and move on in life.
Introduction
Retinitis pigmentosa is a group of inherited retinal disorders that affects the photoreceptors and the retinal pigmentary epithelium.1 In some disorders the rods are affected first and the cones later (termed rod-cone dystrophy) or the reverse (cone–rod dystrophy). Rod–cone dystrophy is the most common form of RP, in which the first manifestation is night blindness, followed by decreasing visual fields and eventually leading to blindness after several decades. The prevalence of RP is 1 in 3000 to 1 in 5000.2 Majority of the disorders have a genetic basis3 and involve photoreceptor cell death by apoptosis. Retinitis pigmentosa can be inherited as autosomal dominant (30–40%), autosomal recessive (50–60%), or X-liked recessive (5–15%) manner.3, 4, 5, 6 The role of oral vitamin A and docosahexaenoic acid (DHA) in slowing down the degenerative process in typical RP is not well established.7 However, dietary modification and nutritional supplements may be beneficial for rare syndromic forms of RP.8, 9 Newer therapeutic modalities for RP include gene therapy, cell transplantation, neuroprotection and hyperbaric oxygen.10, 11
Retinitis pigmentosa is a disabling disease that is currently incurable. It typically starts at the early teenage years and progresses to severe visual impairment during the 4th and the 5th decade. The classical symptoms of RP include nyctalopia (night blindness), peripheral visual loss and in advanced cases central visual loss and photopsia (seeing flashes of light). Apart from the classical symptoms, people with RP exhibit difficulty adjusting to changing levels of illumination, difficulty seeing in poor contrast,12 abnormal temporal processing,13, 14 and motion perception anomalies.15 All these difficulties along with the progressive visual loss can have a serious impact on quality of life (QoL) of an individual with RP. Even though these problems are identified clinically, limited research has been conducted to understand the impact on day-to-day life of people with RP from their perspectives. A well-conducted qualitative study is essential to understand the patient's experience of living with RP. Hence, the aim of this study was to explore the issues and impact of people with RP on QoL.
Materials and methods
Twenty-three participants with RP were recruited through a nonprobability, convenience sampling techniques. Participants were recruited from the Royal Society for the Blind (Adelaide) and Retina Australia Society (Queensland, Western Australia, Victoria, New South Wales, and Canberra) through emails and flyers. Participants who responded to the email request and the flyers were sent out a research pack consisting of an invitation letter, participant information sheet, consent form and demographic form in the post. Upon receiving the consent form, participants were contacted through telephone to organise a date and time for an interview. A semi-structured interview guide was developed from existing literature and expert consultation and it was validated by a panel of experts. The interviews were carried out over the telephone. All the interviews occurred between August 2014 and June 2015. All interviews were audio recorded and transcribed. Interviews were carried out till thematic saturation (no additional new information arising) was obtained.
An ethical approval was obtained from the Southern Adelaide Clinical Human Research Ethics Committee and the corresponding ethics committees at health care facilities and the study adheres to the Tenets of Declaration of Helsinki.
Data analysis
We used an inductive approach where the content of the data directed the coding and the theme development (data-driven).16 Nodes (words or phrases) to code text segments were generated after scan reading individual transcripts. The nodes bear meaning of the text segments to be coded by them as close as possible. For this, we carried out an open coding strategy which entailed line-by-line coding approach. Each transcript was coded using the nodes in its entirety. Once the coding was complete, individual nodes were reorganized by assimilating them into different categories (that is, nodes of similar concept were brought under the umbrella of a mother node (potential major theme)). The mother nodes with component child nodes (potential sub-themes) were explored to identify linkage between similar patterns across the transcripts.17 This exercise helped us to identify key threads. These key threads were then re-assessed by the authors to come to a decision whether they qualify to form a theme. Any discrepancies between the authors were resolved by discussion. New or improved themes that emerged from later transcripts were incorporated into the coding hierarchy, and earlier transcripts were updated to reflect the modification. The computer program QSR NVivo 10 (QSR International Pty Ltd) was used to code the transcripts systematically.
Rigor
Several identified strategies were used to enhance the trustworthiness of this study including credibility, transferability, dependability, and confirmability. Credibility was achieved through adoption of systematic, in-depth field work and triangulation of time and space (various times of the day, week, and year were used in the collection of the data and use of multi-sites for participant recruitments). Transferability was achieved through description of the clinical context of the study and description of the demographics of the participants. Dependability was achieved through in-depth description of the methodology and confirmability was achieved through the recognition of shortcomings in study's method and their potential effects.
Results
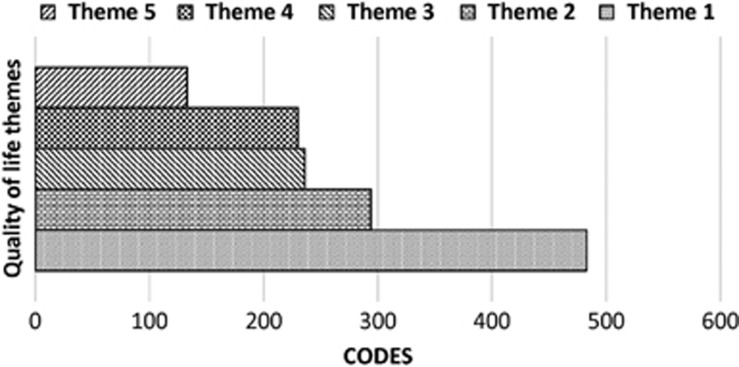
A total of 23 interviews were conducted (mean age=55.6 years (SD=14.3); range=28 to 81 years; females, 14). Two-thirds of the participants were above the age of 50 years and all the participants had bilateral disease (Table 1). The mean age of onset of the disease was 18.8 years (SD=11.8) and the mean duration of the disease was 38.9 years (SD=14.7). We identified five major QoL themes: (1) struggle to perform important day-to-day tasks (activity limitation); (2) concerns about disease progression disease outcome and personal safety (health concerns); (3) facing a lot of emotional and psychological challenges (emotional well-being); (4) experiencing a myriad of visual symptoms (symptoms) and (5) adopting different strategies to manage stressful circumstances (coping; Figure 1)
Table 1. Sociodemographic details of the study sample.
| Variable | n=23 |
|---|---|
| Age (years, n (%)) | |
| ≤55 | 10(43) |
| Range | 28 to 81 |
| Mean age of onset of the disease (years) (SD) | 18.8(11.8) |
| Mean duration of the disease (years) (SD) | 38.9(14.7) |
| Gender, n (%) | |
| Female | 14(61) |
| Country of birth, n (%) | |
| Australia | 18(78) |
| Other | 5(22) |
| Main language spoken, n (%) | |
| English | 22(96) |
| Other | 1(4) |
| Marital status, n (%) | |
| Married | 15(65) |
| De facto/divorced/separated/widowed | 3(13) |
| Never married | 5(22) |
| Education level, n (%) | |
| Secondary or less | 6(26) |
| TAFE/university degree | 17(74) |
| Visual acuity (worse eye, n (%)) | |
| Better than 6/18 | 1(4) |
| 6/18 to 6/60 | 12(52) |
| <6/60 | 10(44) |
| Laterality, n (%) | |
| Bilateral | 23(100) |
| Ocular comorbidity, n (%) | |
| Yes | 8(35) |
| Medical comorbidity, n (%) | |
| Yes | 12(52) |
Figure 1.
Major quality of life (QoL) themes in people with retinitis pigmentosa (RP). X axis: codes=number of times the attribute was discussed across all the transcripts analysed. Y axis: QoL themes. Theme 1, struggle to perform important day-to-day tasks; Theme 2, concerns about disease progression, disease outcome and personal safety; Theme 3, facing a lot of emotional and psychological challenges; Theme 4, experiencing a myriad of visual symptoms; Theme 5, adopting different strategies to manage stressful circumstances.
Struggle to perform important day-to-day tasks (activity limitation)
Participants with RP frequently reported difficulty in performing important day-to-day tasks such as reading, seeing in changing light conditions, shopping, driving, playing sports, taking part in leisure activities and doing household chores (Table 2). They reported difficulty in reading books, menu cards, magazines, and newspapers.
Table 2. Major activity limitation among people with retinitis pigmentosa (RP). Note: codes=number of times the attribute was discussed across all the transcripts analysed.
| Activity limitation | Codes |
|---|---|
| Reading (e.g. books, newspapers, signage, text messages) | 63 |
| Seeing in changing light conditions | 60 |
| Shopping | 48 |
| Driving | 43 |
| Navigation in unfamiliar places | 28 |
| Playing sports | 26 |
| Walking outdoors | 20 |
| Using computers | 19 |
| Engaging in leisure activities (e.g. dancing, singing) | 14 |
'My biggest loss for my own self is reading a novel. I used to love to sit down and read a novel and I can't do that now. I can read still but only for very short periods.'
They often reported missing out the fun of reading and had to rely on low vision assistive devices such as closed circuit television (CCTV), iPhone, kindle, computers and talking books for reading. Poor or too bright lighting conditions are also reported to be a challenge. They eloquently mentioned various situations where they faced difficulties in seeing under different light conditions such as in dark, dim-lights, and bright lights. They were comfortable doing online shopping as they could avoid relying on others for transport. Participants had difficulty in driving both during the day and the night and not being able to drive and associated loss of independence by some has tormented as regret in life. They had difficulty playing sports due to poor hand–eye coordination. Cleaning was the most difficult household chore reported. Other difficulties reported were engaging in leisure activities such as knitting, gardening and playing lawn-bowls and self-grooming.
They experienced difficulties when walking in unfamiliar places, crowded places and using steps. Navigation in unfamiliar places was the most frequent mobility difficulty reported. Being in unfamiliar surrounding caused anxiety and stress. Using a white cane or a guide dog or asking for assistance were some of the methods used by RP people to navigate in such difficult situations. However, they were quite confident walking and navigating in familiar surroundings. They also struggle in confined places and busy places such as shopping malls and airports and generally tried to avoid going to such places. They also expressed dislike for crowds and steps. Going downstairs was reported as a more difficult task than going upstairs.
'I avoid supermarkets or big shops or department stores; I find them very overwhelming and difficult to get around.'
Concerns about disease progression, disease outcome, and personal safety (health concerns)
People with RP expressed lots of concern about their health, disease outcome and personal safety. One of the major health concerns was having frequent accidents such as falls and bumping into things.
'The other fear is that I keep bashing into things and falling over things and hurting myself and getting bruises and scrapes and stuff like that.'
Having to rely on others for reading, shopping, transport, and getting around in darkness was again a major concern. They generally expressed dissatisfaction towards the medical service providers as they felt that the information provided by them was inadequate. The prospect of losing eye sight completely or going blind early was also the biggest concern. The uncertainty of their future as a result of the visual loss, life and career was one of the pressing concerns mentioned. Learning new ways to do everything was challenging for them. They also raised concerns about handling emergency situations such as bushfire, house fire and thunder storms.
'There's fear of being in a place, that if it catches fire or in an accident or something and not being able to get yourself to safety because you can't see, so that's quite frightening.'
Facing a lot of emotional and psychological challenges (emotional well-being)
Participants with RP face a lot of emotional and psychological challenges due to their progressive visual loss. Frustration, worry, shock, anxiety and feel as a burden were the commonly expressed emotions. They frequently expressed frustrations which results from myriad of reasons such as not knowing what to do when being diagnosed with RP, having to learn different ways of doing things, inability to participate in sports and having to depend on people, technology etc.
'It was frustrating because when they give you the diagnosis that you've got this eye condition and you're going to go blind you're in so much shock and you don't really know what to do.'
They worried about their future, their employability, their eye condition, and their coping skills. Unfamiliar surroundings, uncertainties about the progression of the eye condition and inability to identify social cues when in a group caused anxiety. They also go through bouts of depression that is sparked by some kind of life event such as people getting married or people having children that reminded them that life is different to everybody else's. They felt embarrassed and did not want to associate with being a disabled person or being a blind person. Fear of being left on their own, fear of rejection by people or partner and fear of having accidents were often reported.
'Probably being left on my own would be the biggest fear.'
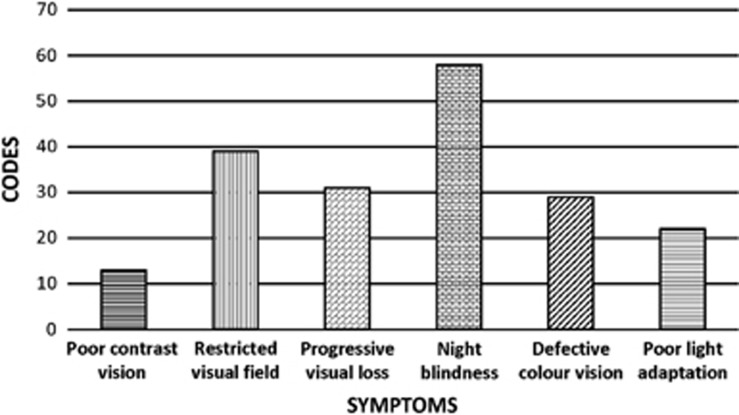
Experiencing a myriad of symptoms (symptoms)
The commonly cited symptoms were night blindness, restricted visual fields, difficulty in discriminating colours, difficulty in adjusting to different light conditions and poor contrast vision (Figure 2). Night blindness was the most common symptom.
Figure 2.
Common visual symptoms reported by people with retinitis pigmentosa (RP). X axis: symptoms. Y axis: codes=number of times the attribute was discussed across all the transcripts analysed.
'I've always had the night blindness but when I was about 15, I suppose, was when it really got to the point where it was difficult to get around.'
Restriction of the peripheral visual field caused depth perception issues resulting in frequent tripping and bumping into things. Limitation of the visual fields was also associated with difficulty in working with computer screens and watching movies. These people had trouble discerning colours that are of a similar spectrum such as yellow and white or blue and green. Adjusting to different lighting condition was also a big issue. People with macular oedema reported worsening of their central vision. They also reported that they have difficulty in seeing things that are of poor contrast.
'My contrast, it depends on the colours. If they're very light colours, no, I don't have any contrast.'
Adopting different strategies to manage stressful circumstances (coping)
Coping strategies were commonly discussed by all the participants. They expressed their resilience in facing the nature of their eye condition. Some of the commonly reported coping strategies were trying to be optimistic, accepting their eye condition/visual loss and learning to live with the eye condition.
'It has taken a lot of work to become more comfortable and accepting of it and I've got a lot less angst now, but I have had to go to counselling and there's been a lot of tears and reliance on people for support.'
Trying to be optimistic and thinking that there are people much worse than them helped them to cope better. Accepting their eye condition and learning to do things in a different ways was also a common coping mechanism among these people. They tried to get away with their frustrations by listening to books, playing sports and travelling to places to meet people. Interacting with people with similar eye condition was also an important way of coping. Thinking that their eye condition was not life threatening helped them to move on. They also learned to enjoy life and appreciate it.
'I work very hard to have a good life despite my vision loss and as long as I can have a good meal a couple of times a week and a couple of glasses of wine that'll do.'
Other QoL issues
People with RP had difficulty interacting with their friends and family members. Difficulty in identifying social cues and inability to participate in social events in the evenings made social life a bit harder for them. Their progressive visual loss was not well understood by their family members and friends that affected their long term relationship with them. Despite these hardships majority of the participants were very independent. Early onset of the disease affected their career development and progress in life. Difficulty in finding suitable jobs and reduced job opportunities were frequently reported. They had to frequently change jobs to suit their abilities due to the progressive worsening of their eye condition and majority of them had to give up work and retrain into something else. Loss of income associated with loss of job caused financial constraints.
'I was earning a very good income and that was cut completely. Well now, as a remedial massage therapist I do have an income but it's still very small at the early stages of my practice but it will grow, I know over time.'
Inconveniences ensued in day-to-day life for having to live with RP and the subsequent vision loss was commonly discussed. Lack of independence and having to rely on others was reported as one of the major inconvenience. Having to plan and organize for the things beforehand was also a major inconvenience. Most of them depended on gadgets for doing most of the things such as reading, shopping, moving around and so on. Having more complicated travel plans because of driving limitations, having to allow a bit of extra leeway when going to unfamiliar places, having to concentrate on things harder, having to be slower and more careful, and having limitations on where you can go were the other inconveniences.
'I still go places I don't know but I do allow – I must admit I do allow either extra time or extra awareness because it's unfamiliar and I know I'm not going to recognise things so I have to allow myself a bit of extra leeway.'
Discussion
This study systematically explored the overall impact of RP on quality of life. The participants of this study described emotional impacts and adaptation to their visual disability that were consistent with previous qualitative research.18, 19 Our study shows that people with RP experience a myriad of QoL issues. We identified five major QoL themes (activity limitation, health concerns, emotional well-being, symptoms, and coping). This information may be used to help inform the eye care providers, who should take such perspectives into consideration when evaluating and managing their patients with RP. Moreover, understanding the extent of the QoL impact of these people can help identify subgroups with relatively poor perceived health and help guide interventions to improve their situations and avert more serious consequences.
Activity limitation was the major QoL issue among people with RP. The greater functional limitations experienced by the people with RP may be due to bilateral involvement, severe visual impairment and the progressive nature of the eye condition. Participants expressed a series of concerns because of uncertainty surrounding their eye condition which is progressive and incurable. Similar health concerns were reported in previous qualitative studies.19, 20 People with RP face a lot of emotional and psychological challenges due to the physiological stress associated with the vision loss. Studies show that vison loss, from any eye disease has been linked with a range of emotional and social issues.21, 22 People with vision loss may experience emotional reactions like fear, anxieties, frustration, depression and embarrassment.23, 24 In fact, the most common psychological comorbidity in vision loss is depression and it has been shown that people with visual impairment have high incidence of depression.25, 26, 27 People with RP also expressed a lot of emotional reactions such as frustration, anxiety, depression, shock, worry, and fear. Social manifestations of vision loss include increased social isolation, family problems, and divorce.23, 28, 29 Similar social issues were reported by people with RP. Progressive loss of the photoreceptors causes a myriad of visual symptoms in RP. The common visual symptoms among our participants were night blindness, progressive visual field loss, and difficulty in light adaptation. In contrast, a previous study has reported a different set of symptoms (day-to-day visual fluctuations, intermittent diplopia, photopsia, high glare, and visual hallucinations).18
Individuals with RP experience different levels of stress. It could be due to uncertainty to their ability to perform different activities, lack of independence, increased fear of falling due to difficulties with mobility and increased mental effort and information processing required to compensate for the limited visual information.30, 31 However, most people with RP are able to cope with their visual loss by adopting several coping strategies. Trying to be optimistic and accepting their eye condition/visual loss were the common coping strategies adopted by our participants. Similar coping strategies were reported in previous studies.18, 19
People with RP have greater functional limitations compared to people with major blinding retinal conditions such as age related macular degeneration (AMD) and diabetic retinopathy (DR), because in these major blinding conditions the visual disability is mostly due to the loss of central vision,24, 32, 33 whereas in RP the visual disability is due to the loss of both the peripheral and the central vision. Retinitis pigmentosa also causes a greater emotional and psychological impact on the individuals than AMD and DR because RP is not treatable, whereas AMD and DR are mostly treatable. The major health concern among people with RP was going blind, whereas the major concern among people with AMD and DR was mostly related to the treatment outcomes.24, 32 Early onset of the eye disease affects the career development and progress in life of people with RP, which is not the case in AMD which typically has a late onset.
There are currently nine RP-specific patient-reported outcome (PRO) instruments.31, 34, 35, 36, 37, 38, 39, 40, 41 The motive behind our endeavor to develop a comprehensive RP-specific PRO is that none of the existing PRO instrument has undergone comprehensive validation in this disease group and their content coverage is limited to measuring only a few QoL domains (predominantly mobility).42, 43, 44 Lack of an appropriate RP-specific PRO measure restricts the understanding of the full impact of RP on QoL. Understanding patients' perspective is also critical as newer treatment modalities such as gene therapy, cell transplantation, retinal prosthesis and neuroprotection are fast emerging. Moreover, the US Food and Drug Administration (FDA) and most funding organisations now insist on using PRO instruments in clinical trials to assess the intervention/treatment outcomes. Hence there is also a need for developing comprehensive and psychometrically sound RP-specific PRO instrument. The findings of this study will guide us to develop the content (items) of a comprehensive RP-specific PRO instrument, which will be technologically advanced in the form of item banking implemented via computer adaptive testing (CAT). An item bank is simply a large collection of items/questions that measure a unidimensional construct such as activity limitation, emotional well-being, social participation, and so on.45A disease-specific item bank will have a series of calibrated item pools covering important domains of QoL.44 The CAT system choses the best and highly informative items from the available item pool that closely match with the participant's ability. As the item administration is based on the participant's response to previous items, the CAT provides an effective, quick and precise measurement of QoL.46, 47 Item banks have been developed and implemented in other fields of health care48, 49 and is currently under construction for eye diseases such as glaucoma, DR and AMD.24, 50, 51
One of the limitations of this study was the small sample size. Unlike a quantitative study where the statistical power of the study depends on an adequate sample size, in a qualitative study the sample size should be adequate enough to assure that most of the perceptions that might be important are uncovered, but at the same time should not be too large to become repetitive. The sample size in the qualitative data should follow the concept of saturation when the collection of new data do not shed any further light on the issue under investigation. Our sample size for this study was based on the information saturation. The other limitation of this study was that our cohort had predominantly people with late stages of RP and we did not have a broad spectrum of people with RP. This is because our cohort was selected from charity organizations. People who suffer more from the disease are more likely to join organizations to seek more information and support. These people are also more likely to take part in research. This could have resulted in selection bias. Ideal would be to have even distribution of people with different disease severity and age distribution in the cohort. However, we had five individuals (22% of participants) who were younger than 40 years and their perspectives were also obtained. The youngest participant we had was of 28 years. Moreover, RP is a heterogeneous disease and our finding may not be generalized to all the people living with RP. The other limitation of this study was that greater number of our participants were females. Retinitis pigmentosa has no racial, ethnic or sexual predilection. However, the X-linked type is more prevalent in males. More number of female participants may be because women are more likely to participate in surveys than men.52, 53
Acknowledgments
We thank all the members of the Royal Society for the Blind and members of the Retina Australia (QLD, VC, WA, NSW, and ACT). We also thank our research assistant Susan Aldhous. This study is funded by National Health and Medical Research Council (grant no. 1031838).
Disclaimer
We report no proprietary or commercial interest in any product mentioned or concept discussed in this article
Footnotes
The authors declare no conflict of interest.
References
- Retinitis pigmentosa. A symposium on terminology and methods of examination. Ophthalmology 1983; 90(2): 126–131. [PubMed] [Google Scholar]
- Boughman JA, Conneally PM, Nance WE. Population genetic studies of retinitis pigmentosa. Am J Hum Genet 1980; 32(2): 223–235. [PMC free article] [PubMed] [Google Scholar]
- Hartong DT, Berson EL, Dryja TP. Retinitis pigmentosa. Lancet 2006; 368(9549): 1795–1809. [DOI] [PubMed] [Google Scholar]
- Bunker CH, Berson EL, Bromley WC, Hayes RP, Roderick TH. Prevalence of retinitis pigmentosa in Maine. Am J Ophthalmol 1984; 97(3): 357–365. [DOI] [PubMed] [Google Scholar]
- Grondahl J. Estimation of prognosis and prevalence of retinitis pigmentosa and Usher syndrome in Norway. Clin Genet 1987; 31(4): 255–264. [DOI] [PubMed] [Google Scholar]
- Ferrari S, Di Iorio E, Barbaro V, Ponzin D, Sorrentino FS, Parmeggiani F. Retinitis pigmentosa: genes and disease mechanisms. Curr Genomics 2011; 12(4): 238–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musarella MA, Macdonald IM. Current concepts in the treatment of retinitis pigmentosa. J Ophthalmol 2011; 2011: 753547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gouras P, Carr RE, Gunkel RD. Retinitis pigmentosa in abetalipoproteinemia: Effects of vitamin A. Invest Ophthalmol 1971; 10(10): 784–793. [PubMed] [Google Scholar]
- Baldwin EJ, Gibberd FB, Harley C, Sidey MC, Feher MD, Wierzbicki AS. The effectiveness of long-term dietary therapy in the treatment of adult Refsum disease. J Neurol Neurosurg Psychiatry 2010; 81(9): 954–957. [DOI] [PubMed] [Google Scholar]
- Shintani K, Shechtman DL, Gurwood AS. Review and update: current treatment trends for patients with retinitis pigmentosa. Optometry 2009; 80(7): 384–401. [DOI] [PubMed] [Google Scholar]
- He Y, Zhang Y, Su G. Recent advances in treatment of retinitis pigmentosa. Curr Stem Cell Res Ther 2015; 10(3): 258–265. [DOI] [PubMed] [Google Scholar]
- Alexander KR, Derlacki DJ, Fishman GA. Contrast thresholds for letter identification in retinitis pigmentosa. Invest Ophthalmol Vis Sci 1992; 33(6): 1846–1852. [PubMed] [Google Scholar]
- Dagnelie G, Massof RW. Foveal cone involvement in retinitis-pigmentosa progression assessed through psychophysical impulse-response parameters. Invest Ophthalmol Vis Sci 1993; 34(1): 243–255. [PubMed] [Google Scholar]
- Tyler CW, Ernst W, Lyness AL. Photopic flicker sensitivity losses in simplex and multiplex retinitis pigmentosa. Invest Ophthalmol Vis Sci 1984; 25(9): 1035–1042. [PubMed] [Google Scholar]
- Turano K, Wang X. Motion thresholds in retinitis pigmentosa. Invest Ophthalmol Vis Sci 1992; 33(8): 2411–2422. [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Sage Publications, Inc, 1998. [Google Scholar]
- Basit T. Manual or electronic? The role of coding in qualitative data analysis. Educ Res 2003; 45(2): 143–154. [Google Scholar]
- Bittner AK, Edwards L, George M. Coping strategies to manage stress related to vision loss and fluctuations in retinitis pigmentosa. Optometry 2010; 81(9): 461–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fourie R. A qualitative self-study of Retinitis Pigmentosa. Br J Vis Impair 2007; 25(3): 217–232. [Google Scholar]
- Combs R, Hall G, Payne K, Lowndes J, Devery S, Downes SM et al. Understanding the expectations of patients with inherited retinal dystrophies. Br J Ophthalmol 2013; 97(8): 1057–1061. [DOI] [PubMed] [Google Scholar]
- Evans JR, Fletcher AE, Wormald RP. Depression and anxiety in visually impaired older people. Ophthalmology 2007; 114(2): 283–288. [DOI] [PubMed] [Google Scholar]
- Horowitz A. The prevalence and consequences of vision impairment in later life. Top Geriatr Rehabil 2004; 20(3): 185–195. [Google Scholar]
- Fenwick E, Rees G, Pesudovs K, Dirani M, Kawasaki R, Wong TY et al. Social and emotional impact of diabetic retinopathy: a review. Clin Exp Ophthalmol 2012; 40(1): 27–38. [DOI] [PubMed] [Google Scholar]
- McCloud C, Khadka J, Gilhotra JS, Pesudovs K. Divergence in the lived experience of people with macular degeneration. Optom Vis Sci 2014; 91(8): 966–974. [DOI] [PubMed] [Google Scholar]
- Brody BL, Gamst AC, Williams RA, Smith AR, Lau PW, Dolnak D et al. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration. Ophthalmology 2001; 108(10): 1893–1900. [DOI] [PubMed] [Google Scholar]
- Shmuely-Dulitzki Y, Rovner BW. Screening for depression in older persons with low vision. Somatic eye symptoms and the Geriatric Depression Scale. Am J Geriatr Psychiatry 1997; 5(3): 216–220. [DOI] [PubMed] [Google Scholar]
- Rovner BW, Ganguli M. Depression and disability associated with impaired vision: the MoVies Project. J Am Geriatr Soc 1998; 46(5): 617–619. [DOI] [PubMed] [Google Scholar]
- Coyne KS, Margolis MK, Kennedy-Martin T, Baker TM, Klein R, Paul MD et al. The impact of diabetic retinopathy: perspectives from patient focus groups. Fam Pract 2004; 21(4): 447–453. [DOI] [PubMed] [Google Scholar]
- Bernbaum M, Albert SG, Duckro PN, Merkel W. Personal and family stress in individuals with diabetes and vision loss. J Clin Psychol 1993; 49(5): 670–677. [DOI] [PubMed] [Google Scholar]
- Turano KA, Geruschat DR, Baker FH, Stahl JW, Shapiro MD. Direction of gaze while walking a simple route: Persons with normal vision and persons with retinitis pigmentosa. Optom Vis Sci 2001; 78(9): 667–675. [DOI] [PubMed] [Google Scholar]
- Turano KA, Geruschat DR, Stahl JW, Massof RW. Perceived visual ability for independent mobility in persons with retinitis pigmentosa. Invest Ophthalmol Vis Sci 1999; 40(5): 865–877. [PubMed] [Google Scholar]
- Fenwick EK, Pesudovs K, Khadka J, Dirani M, Rees G, Wong TY et al. The impact of diabetic retinopathy on quality of life: qualitative findings from an item bank development project. Qual Life Res 2012; 21(10): 1771–1782. [DOI] [PubMed] [Google Scholar]
- Moore LW. Severe visual impairment in older women. West J Nurs Res 2000; 22(5): 571–588. [DOI] [PubMed] [Google Scholar]
- Geruschat DR, Turano KA, Stahl JW. Traditional measures of mobility performance and retinitis pigmentosa. Optom Vis Sci 1998; 75(7): 525–537. [DOI] [PubMed] [Google Scholar]
- Lodha N, Westall CA, Brent M, Abdolell M, Heon E. A modified protocol for the assessment of visual function in patients with retinitis pigmentosa. Adv Exp Med Biol 2003; 533: 49–57. [DOI] [PubMed] [Google Scholar]
- Kennedy WL, Rosten JG, Young LM, Ciuffreda KJ, Levin MI. A field expander for patients with retinitis pigmentosa: a clinical study. Am J Optom Physiol Opt 1977; 54(11): 744–755. [DOI] [PubMed] [Google Scholar]
- Lowe J, Drasdo N. Patients' responses to retinitis pigmentosa. Optom Vis Sci 1992; 69(3): 182–185. [DOI] [PubMed] [Google Scholar]
- Somani S, Brent MH, Markowitz SN. Visual field expansion in patients with retinitis pigmentosa. Can J Ophthalmol 2006; 41(1): 27–33. [DOI] [PubMed] [Google Scholar]
- Szlyk JP, Fishman GA, Grover S, Revelins BI, Derlacki DJ. Difficulty in performing everyday activities in patients with juvenile macular dystrophies: comparison with patients with retinitis pigmentosa. Br J Ophthalmol 1998; 82(12): 1372–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szlyk JP, Seiple W, Fishman GA, Alexander KR, Grover S, Mahler CL. Perceived and actual performance of daily tasks: relationship to visual function tests in individuals with retinitis pigmentosa. Ophthalmology 2001; 108(1): 65–75. [DOI] [PubMed] [Google Scholar]
- Sumi I, Matsumoto S, Okajima O, Shirato S. The relationship between visual disability and visual scores in patients with retinitis pigmentosa. Jpn J Ophthalmol 2000; 44(1): 82–87. [DOI] [PubMed] [Google Scholar]
- Khadka J, McAlinden C, Pesudovs K. Quality assessment of ophthalmic questionnaires: review and recommendations. Optom Vis Sci 2013; 90(8): 720–744. [DOI] [PubMed] [Google Scholar]
- Prem Senthil M, Khadka J, Pesudovs K. Assessment of patient-reported outcomes in retinal diseases: a systematic review. Surv Ophthalmol 2016. Under review. [DOI] [PubMed]
- Khadka J, Fenwick E, Lamoureux E, Pesudovs K. Methods to develop the eye-tem bank to measure ophthalmic quality of life. Optom Vis Sci 2016; 93(12): 1485–1494. [DOI] [PubMed] [Google Scholar]
- Pesudovs K. Item banking: a generational change in patient-reported outcome measurement. Optom Vis Sci 2010; 87(4): 285–293. [DOI] [PubMed] [Google Scholar]
- Wainer H, Neil D, Ronald F, Bert G, Robert M. Computerized Adaptive Testing: a Primer, 2nd edn. Lawerance Erlbaum: NJ, 2000. [Google Scholar]
- Wang YC, Hart DL, Cook KF, Mioduski JE. Translating shoulder computerized adaptive testing generated outcome measures into clinical practice. J Hand Ther 2010; 23(4): 372–382. [DOI] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol 2010; 63(11): 1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna D, Krishnan E, Dewitt EM, Khanna PP, Spiegel B, Hays RD. The future of measuring patient-reported outcomes in rheumatology: Patient-Reported Outcomes Measurement Information System (PROMIS). Arthritis Care Res (Hoboken) 2011; 63(Suppl 11): S486–S490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenwick EK, Pesudovs K, Khadka J, Rees G, Wong TY, Lamoureux EL. Evaluation of item candidates for a diabetic retinopathy quality of life item bank. Qual Life Res 2013; 22(7): 1851–1858. [DOI] [PubMed] [Google Scholar]
- Khadka J, McAlinden C, Craig JE, Fenwick EK, Lamoureux EL, Pesudovs K. Identifying content for the glaucoma-specific item bank to measure quality-of-life parameters. J Glaucoma 2015; 24(1): 12–19. [DOI] [PubMed] [Google Scholar]
- Curtin R, Presser S, Singer E. The effects of response rate changes on the index of consumer sentiment. Public Opin Q 2000; 64(4): 413–428. [DOI] [PubMed] [Google Scholar]
- Singer E, Van Hoewyk J, Maher MP. Experiments with incentives in telephone surveys. Public Opin Q 2000; 64(2): 171–188. [DOI] [PubMed] [Google Scholar]