Abstract
Celiac disease, also known as “celiac sprue”, is a chronic inflammatory disorder of the small intestine, produced by the ingestion of dietary gluten products in susceptible people. It is a multifactorial disease, including genetic and environmental factors. Environmental trigger is represented by gluten while the genetic predisposition has been identified in the major histocompatibility complex region. Celiac disease is not a rare disorder like previously thought, with a global prevalence around 1%. The reason of its under-recognition is mainly referable to the fact that about half of affected people do not have the classic gastrointestinal symptoms, but they present nonspecific manifestations of nutritional deficiency or have no symptoms at all. Here we review the most recent data concerning epidemiology, pathogenesis, clinical presentation, available diagnostic tests and therapeutic management of celiac disease.
Keywords: Celiac disease, Epidemiology, Diagnosis, Treatment, Pathogenesis
Core tip: Celiac disease is a chronic inflammatory disorder of the small intestine, produced by the ingestion of dietary gluten products in susceptible people. It is a multifactorial disease, including genetic and environmental factors. Thanks to advanced understanding of its pathogenesis, numerous therapeutic strategies have been devised for the treatment of celiac disease. But there is need of further basic research studies and randomized clinical trials to introduce them into usual management of this disease.
INTRODUCTION
Celiac disease defined an autoimmune disorder originating by an aberrant adaptive immune response against gluten-containing grains in susceptible individuals. Celiac disease was first described in 1888 by Samuel Gee, but only in 1953 it became clear the importance of the gluten in the origin of this pathology[1-3]. In celiac subjects the ingestion of gluten leads to an enteropathy with an impairment of the mucosal surface and, consequently, abnormal absorption of nutrients[4-7]. Celiac disease might be considered a syndrome, because of the wide spectrum of clinical manifestations and the involvement of various human systems. Celiac disease shows peculiar features in comparison to others autoimmune disorders, including the complete recovery of the mucosal damage as well as the reversibility of its progression and chronic dynamics, with a total avoidance of gluten. Conversely, it is now ascertained that undiagnosed celiac disease, might have severe consequences in children as well as in adult subjects[8-10]. Besides celiac disease and wheat allergy, a new entity has been included, apparently not driven by an immune response: The non-celiac gluten sensitivity (NCGS). The pathogenesis of NCGS remains largely unknown, although it is now ascertained that it includes a set of factors[3,11]. Here, we review the epidemiology, pathogenesis, clinical presentation, diagnostic tests and therapeutic management of celiac disease.
EPIDEMIOLOGY
In the last decades a high number of epidemiological data have been reported. Nowadays celiac disease is one of the most frequent genetically based disorder in humans, although it was thought that some country, including United States, were exempt from this disease[12]. Europe is historically considered a geographical area at high frequency, with a prevalence of 1%-2%, although it has been recently shown a similar prevalence in United States[13,14]. Despite the advances in diagnosis, the overall prevalence of this disease remains still unclear. A variable frequency has been reported between European countries, although it is still uncertain whether it depends on the different screening tool, sample size or a real variability of celiac disease prevalence[15]. What is known is that many cases remains undiagnosed, as idealized with the “iceberg model” (Figure 1). Typical cases of celiac disease are diagnosed because of suggestive symptoms. The submerged part of the iceberg represents all the undiagnosed cases that usually show atypical, minimal, or even absent symptoms[16]. A multicenter study reported a prevalence of 1 out of 133 (0.75%) in healthy people in the United States, and similar frequency is confirmed by studies on European and Australian populations[12]. The overall prevalence of celiac disease ranges from 4.5% among high-risk subjects to 0.75% in not-at-risk subjects[12]. High-risk subjects include the relatives of patients with celiac disease, children or adults with celiac disease-associated symptoms (i.e., diarrhea, abdominal pain and constipation) and children or adult subjects with celiac disease-associated disorders (i.e., Diabetes Mellitus type-1, Down syndrome, anemia, infertility, osteoporosis)[17]. It has been shown that celiac disease is not exclusive of industrialized countries, but includes North Africa, Middle East and India with an incidence overlapping those of European countries[18-20]. However, given the worldwide distribution of the causal factors this heterogeneous diffusion is not surprising. It has been shown that the Saharawi, an Algerian population has the highest prevalence of celiac disease (nearly, 6%) among all of the worldwide populations[16,21,22].
Figure 1.
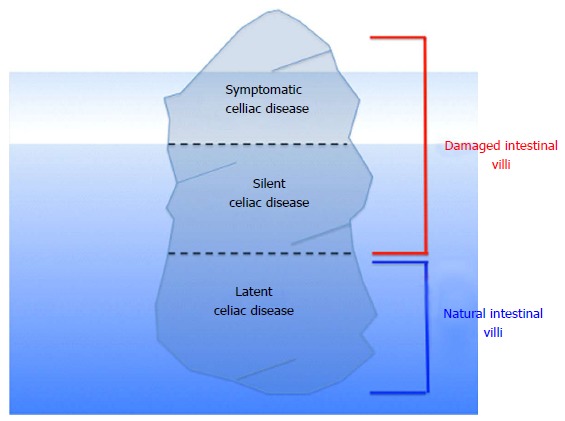
The “iceberg model” idealizing the interplay between celiac disease genetic makeup and exposure to gluten, the environmental trigger of the disease.
GENETIC SUSCEPTIBILITY
The best-characterized genetic risk factor for celiac disease, accounting for 35% of the total genetic risk, is the presence of genes encoding for MHC class II proteins including human leukocyte antigen (HLA) DQ 2 and HLA-DQ8[23-25]. Over 90% of affected subjects express HLA-DQ2 molecules; the remainder express HLA-DQ8. The frequency of celiac disease risk HLA genotypes is about 30%, whereas only 1%-3% develops the disease[26]. It is now accepted that HLA is one of the main but not sufficient factors involved in the onset of celiac disease, but a multitude of genetic factors are responsible in celiac disease susceptibility, as demonstrated by studies on monozygotic twins[27].
Recently, genome-wide association studies have identified 39 non-HLA loci that also predispose to celiac disease[28]. One of these genes may relate to genetic variants on chromosome 19, in the myosin IXB gene (i.e., MYO9B), and may potentially predict responsiveness to a gluten-free diet (GFD)[29,30]. Both HLA-DQ2 and HLA-DQ8 codified for heterodimers located on Antigen-Presenting Cells (APCs)[31]. It has been ascertained that they present gluten peptides to antigen-specific T-lymphocytes in the intestinal mucosa, inducing their proliferation as well as cytokine production. In particular, tTG2 may transform non-charged glutamine into negatively charged glutamic acid[32].
Environmental factors
Feeding patterns in the first year of life and potential viral infections (i.e., rotavirus)[33] might be involved in the development of celiac disease[34]. A prospective study has investigated the role of a specific infectious agent in celiac disease and the authors have found that an increased frequency of rotavirus infection predicts increased risk of celiac disease autoimmunity in children[35]. Gluten, one of the most common ingredients in human nutrition[36], is mainly composed by prolamines and glutenin. The prolamines in wheat are gliadins, in rye secalines and in barley hordeins. Catassi et al[37] proposed that 50 mg gluten/day is the minimum amount able to determine evident alterations to the small-intestinal mucosa in celiac disease subjects. Others pivotal “environmental factors” as the milk-feeding type and the duration of breast-feeding, can also play a role, influencing the intestinal microenvironment[38]. In addition, increased intestinal Gram-negative and reduced Bifidobacteria, has been found in celiac disease subjects[39]. Other debated environmental factors could be represented by heavy metals[40] and bacterial TG present in food stuff[41].
IMMUNE SYSTEM AND THE CELIAC DISEASE
Celiac disease resembles a systemic immune-mediated disorder[34,42-44]. The primary mechanism involved in celiac disease is related to an inappropriate adaptive immune response to gluten-derived peptides. It has been ascertained that prolamines contain critical epitopes presented by either HLA-DQ2 or HLA-DQ8 induce a CD4+ T-lymphocytes response. In celiac disease pathogenesis the role exerted by the intestinal epithelia barrier, physiologically impermeable to macromolecules such as gliadin is actually recognized. In people with a genetic susceptibility to develop celiac disease, gliadin interacts with the intestinal cells to trigger the disassembling of the inter-enterocyte tight junctions (TJs). The impairment of the TJs determines the up-regulation of zonulin, a peptide involved in TJ regulation and responsible for the increased gut permeability. Gliadin peptides pass through the epithelial barrier and activate T-lymphocytes located in the lamina propria. Activated CD4+ T-lymphocytes produce high levels of pro-inflammatory cytokines, inducing either a T-helper 1 pattern dominated by IFN-γ, and a T-helper 2 pattern, which causes a clonal expansion of B-lymphocytes that subsequently differentiate in plasma-cells secreting anti-gliadin and anti-tissue-transglutaminase antibodies[45]. Some gliadin peptides that are not recognized by T-lymphocytes activate both APCs and intestinal epithelial cells; in particular, CD8+ T-lymphocytes may be stimulated by interleukin (IL)-15. An increased density of CD8+ intraepithelial cells is considered as a hallmark of celiac disease[34]. Gliadin-specific T-cell responses have been found to be enhanced by the action of tissue transglutaminase, an enzyme located in the extracellular space of the sub-epithelial region or at the epithelial brush border[46].
HISTOLOGICAL FEATURES OF THE CELIAC DISEASE
Physiologically the height of enterocytes ranges between 29-34 μm. T-cells are usually located in the lamina propria; however, the number of intraepithelial lymphocytes (IELs) is highly variable. A large number of subjects without disease have less than 20 lymphocytes per 100 epithelial cells; based on the experiences of Hayat et al[47] and Veress et al[48], a density of IELs between 25 and 29/100 epithelial cells is considered borderline and pathological over 30/100 epithelial cells.
Tissue samples taken from subjects affected by celiac disease mainly show: (1) Decreased enterocyte height; (2) Crypt hyperplasia; (3) Villous atrophy; (4) Increased intraepithelial T lymphocytes.
Although still debated, recently, Mubarak et al[49] have shown that staining for CD3 has an additional value in the histological detection of celiac disease lesions[49,50]. Immunohistochemical stains for CD3 and CD8 do not improve detection of gluten-sensitive enteropathy in duodenal biopsies. A different grading has been proposed for the evaluation of the gluten free diet in duodenal mucosal healing[51].
Table 1 reports Marsh classification of histologic findings in celiac disease[52]. Modifications to this scoring system have been proposed[53,54]. Oberhuber et al[55] suggested that Marsh III lesions should be included into a, b, and c categories. However, Figure 2 shows two prototypical tissues classified as Marsh II (A) and Marsh IIIA (B).
Table 1.
Marsh classification of histologic findings in celiac disease
| Marsh 0 | Normal mucosal architecture without significant intraepithelial lymphocytic infiltration. |
| Marsh I | Lymphocytic enteritis: Normal mucosal architecture with a marked infiltration of villous epithelium by lymphocytes; arbitrarily defined marked as more than 30 lymphocytes per 100 enterocytes |
| Marsh II | Lymphocytic enteritis with crypt hyperplasia: intraepithelial lymphocytosis and elongation and branching of crypts in which there is an increased proliferation of epithelial cells |
| Marsh III | Intraepithelial lymphocytosis, crypt hyperplasia, and villous atrophy. There are 3 distinct stages of villous atrophy |
| Marsh IIIA | Partial villous atrophy, the villi are blunt and shortened. Arbitrarily, samples are classified as partial villous atrophy if the villus-crypt ratio was less than 1:1 |
| Marsh IIIB | Subtotal villous atrophy, villi are clearly atrophic, but still recognizable |
| Marsh IIIC | Total villous atrophy, villi are rudimentary or absent, and the mucosa resemble colonic mucosa. |
Modifications to this scoring system have been proposed[53,54]. Oberhuber et al[55] suggested that Marsh III lesions should be included into a, b, and c categories. However, Marsh et al[52] examined these subdivisions by means of correlative light and scanning electron microscopy, and demonstrate that Oberhuber’s classification is untenable. In their view, this categorization reflects misinterpretations of the real architectural contours of flat mucosae.
Figure 2.
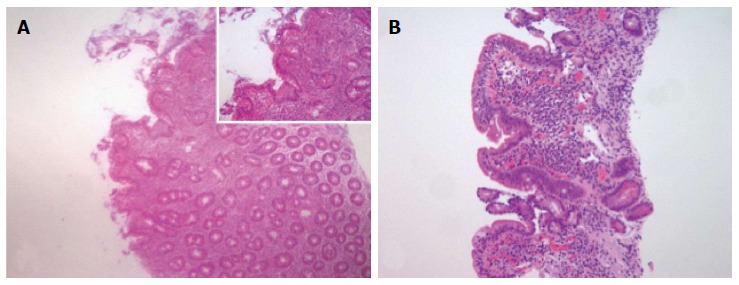
Histological features of celiac disease. A: Example of tissue scored as Marsh 2 characterized by lymphocytic enteritis with crypt hyperplasia: Intraepithelial lymphocytosis and elongation and branching of crypts in which there is an increased proliferation of epithelial cells; B: Example of tissue scored as Marsh 3A characterized by partial villous atrophy, the villi are blunt and shortened. Arbitrarily, samples are classified as partial villous atrophy if the villus-crypt ratio was less than 1:1 (Objective magnification × 4, inset × 10).
CELIAC DISEASE: CLINICAL PRESENTATION
Celiac disease is greatly heterogeneous, at least in part depending on the patient’s age, the duration and extent of disease, and the presence of extra-intestinal comorbidities.
Although celiac disease was originally thought as a pediatric disorder, the diagnosis is increasingly made in adults[16]. Various subtypes of celiac disease have been described[56].
Classical or typical form. It is characterized by common clinical symptoms related to abnormal intestinal absorption. Generally occurs between 6 and 18 mo of age, after the introduction of weaning foods containing prolamines[57]. Histology shows villous atrophy and crypt hyperplasia.
Atypical form
It is characterized by a prevalence of extra-intestinal symptoms with few or no gastrointestinal symptoms. Usually, atypical forms are encountered in older children and adults and the common features of abnormal absorption are absent.
Silent or asymptomatic form
It is characterized by serological and histological abnormalities without evidence of clinical symptoms. This subtype is often observed in subjects with a family history of celiac disease, patients with associated autoimmune (i.e., type 1 diabetes) or genetic disorders (i.e., Down, Turner, or Williams syndrome).
Latent form
It is characteristic of subjects with previous asymptomatic celiac disease, although a gluten-containing diet. Positive serology but no villous atrophy or others tissue abnormalities are recognized. Troncone et al[58] postulated that the presence of elevated endomysial antibodies in these patients might be one of the most important predictor of progression.
Potential form
The term “potential” is used in individuals who have never had diagnosis of celiac disease, but show presence of appropriate genetic background (HLA-DQ2/DQ8), positive serology, with normal or mildly abnormal histology.
Refractory form
It is defined by the presence of malabsorptive symptoms and villous atrophy that persist 1 year after a strict gluten-free diet. Several refractory patients (roughly, 5%-30%) never respond to a gluten-free diet[59], others initially responded but have a recurrence of symptoms and intestinal damage. Two different sub-types of refractory celiac disease have been recognized: “Type 1”, showing a normal intraepithelial lymphocytes count and “type 2” presenting aberrant intraepithelial lymphocytes[29].
Celiac disease can affect individuals from any age, but two peaks can be seen: In the childhood (< 6-year-old) and 4th-5th decade[46]. Classical presentation is more frequent in pediatric and tends to occur early in life (6-24 mo), whereas atypical presentation generally occurs at a later age (> 5-year-old) and in adults[60].
DERMATOLOGICAL CELIAC DISEASE
Dermatitis herpetiformis is an inflammatory cutaneous disease, presenting with diffuse, symmetrical, polymorphic lesions consisting of erythema, urticarial plaques, papules, herpetiform vesiculae and blisters followed by erosions, excoriations and hyperpigmentation. It is characterized by typical histopathological and immunopathological findings. Rarely it is diagnosed in childhood but commonly appears in the third decade.
MAIN CONDITIONS ASSOCIATED TO CELIAC DISEASE
A set of conditions can be associated with celiac disease. The term “associated conditions” refers to states that are found more frequently in patients affected by celiac disease[61]. These conditions include “genetic disorders” such as Down syndrome, Turner syndrome and Williams syndrome, and “autoimmune” or “neurological” disorders.
Type 1-diabetes
One of the most recognized and widely investigated disorders associated with celiac disease is type 1-diabetes[62]. Ludvigsson et al[63] reported that type 1-diabetes constitutes a 5- to 10-fold risk increase for celiac disease in a very large cohort of children. This increasing of risk may partly be explained by shared genetic risk represented by HLA. A percentage approximately of 5%-10% of patients affected by type 1-diabetes presented celiac disease related antibodies with up to 75% having abnormalities on small intestinal biopsy tissue[64]. The prevalence of celiac disease ranges between 1% to 19% in patients with type 1 diabetes mellitus[65]. Prospective studies of high-risk infants for type 1 diabetes and celiac disease have been shown that early introduction of gluten is associated with an increased risk for autoimmunity[66-68]. However, the relationship between the two conditions is still debated[69].
Autoimmune thyroid disorders
In patients affected by celiac disease it has been reported an increased prevalence (nearly, 2%-5%) of thyroid disorders (i.e., hyperthyroidism-Graves’s disease or hypothyroidism-Hashimoto’s thyroiditis), diagnosed either before than after the diagnosis of gluten-enteropathy[65]. These two conditions share genetic risk factors represented by HLA-DQ2 and DQ8. HLA-DQ2 and DQ8 haplotypes have been association with Hashimoto’s thyroiditis, while HLA-DQ2 association is less clear in Graves’ disease. This difference between hyper- and hypothyroidism is reflected also by the greater risk of celiac disease in patients with Hashimoto’s disorder than patients with Graves[70]. In addition to HLA, it has been reported an association with the gene encoding cytotoxic T-lymphocyte-associated antigen-4[65]. Another mechanism related to the association between these two conditions is represented by abnormal absorption with consequent selenium deficiency induced by celiac disease. Stazi et al[70] highlighted that the abnormal selenium absorption in celiac disease could be the factor directly leading to thyroid and intestinal damage, since thyroid is particularly sensitive to selenium deficiency. In the setting of autoimmune thyroid disease it should be useful to pay attention to celiac disease marker and to monitor growth and pubertal status. In patients with celiac disease, a screening for thyroid abnormalities has been also suggested in some cases[61].
Autoimmune hepatitis and other forms of liver involvement
The involvement of liver is common among patients affected by celiac disease[71]. Hypertransaminasemia has been reported in about 40% of adults and in 54% of children with a classical presentation of celiac disease at the time of diagnosis[72]. Conversely, celiac disease is present in about 9% of patients with chronic unexplained hypertransaminasemia[73,74]. It has been postulated that the mechanism leading to hepatic damage is related to entry of toxins, inflammatory molecules and antigens in the portal circulation. Volta et al[75] pointed up about the need of a serological screening for celiac disease in all patients with persistent hypertransaminasemia of unknown cause. Moreover, exclusion of a gluten-related liver damage is necessary for all patients affected by autoimmune liver disorders or by those forms of severe liver disease, whose etiology remains unknown, and for patients enrolled for liver transplant. A prolonged exposition to gluten in a patient with an overlooked celiac disease, in fact, can causes chronic hepatitis and liver cirrhosis[75,76].
Neurological disorders
It has been reported a potential link between celiac disease and different neurological disorders[77]. Data concerning the association between neurological conditions and celiac disease remain poor. Although ataxia is a neurological disorder indicated in some patients with celiac disease[78], the most frequent neurologic condition in celiac disease subjects is epilepsy, showing a prevalence between 1.2% and 5%[79]. Its clinical spectrum in association with celiac disease varies from focal to generalize with variable outcome and response to gluten avoidance. In 1985 it has been described a more specific and rare syndrome characterized by the co-presence of celiac disease, epilepsy, and occipital calcifications (CEC). Gobbi suggested that the HLA genotype predisposing to CEC is the same to that predispose to celiac disease[79].
COMPLICATIONS ASSOCIATED WITH UNTREATED CELIAC DISEASE
Evidences that celiac disease in adults, especially if diagnosed late is burdened by complications have been reported. Among them: (1) Osteoporosis: It represents the most common complication resulting from abnormal calcium absorption secondary to defective calcium transport by the diseased small intestine, but also due to vitamin D deficiency. With an early gluten free diet in children it is possible to prevent the bone disease in adult life; (2) Enteropathy-associated intestinal T cells lymphoma: It represents one of the most important complication; (3) Collagenous sprue: Patients do not react to diet and histology shows extra-cellular matrix components in the intestinal wall at the level of the superficial sub-epithelial layer. This morphological pattern is very similar to the condition of collagenous colitis described in the colon, where the thickness of the connective band best highlighted with Masson’s trichrome is more than 15 nanometers, although this is a very rare event described in the literature; (4) Refractory sprue: This condition is depicted as collagenous sprue although can be identified by immunohistochemical staining, demonstrating that T lymphocytes, which in normal conditions express CD3 and CD8, in this case present only the expression of CD3 and not of CD8; (5) Ulcerative jejunoileitis: Extensive ulceration of the intestinal mucosa, and involving ileum and jejunum. It presents around 50 years old with chronic diarrhea, steatorrhoea and complications of intestinal ulceration (perforation, haemorrhage or obstruction)[59]; (6) Non-Hodgkin lymphoma: Recent data suggests an association between celiac disease and Non-Hodgkin lymphoma[80]; (7) Small bowel adenocarcinoma: Even rare, a connection between carcinoma of the small bowel and celiac disease is known since 1958[81]. The etiologic factors predisposing to malignancy in celiac disease are uncertain. Possibilities include immunologic disturbance associated with mucosal lymphocyte infiltration, premalignant changes in the damaged surface epithelial cells, increased permeability to oncogenic factors and abnormal absorption of protective substances such as vitamins A and E; and (8) Reproductive disorders: Celiac disease might be associated with decreased fertility in both males and females[82].
DIAGNOSTIC TESTS OF CELIAC DISEASE
Serological tests
Anti-tissue transglutaminase antibodies: the best strategy for serological diagnosis is the blood detection of IgA anti-tissue transglutaminase antibodies (tTGA) by enzyme-linked immunosorbent assay (ELISA). These antibodies show a sensitivity up to 97%, a specificity around 96%, and an accuracy of 98%, whereas IgA anti-endomysial (IgA EMA) antibodies are employed as a confirmatory test in tTGA positive cases due to their higher specificity (about 100% vs 91% of tTGA). In concomitance of IgA deficiency and celiac disease, found in around 2%-10% of the patients, it is recommended to detect celiac disease testing tTG-IgG. “False negative” occurs, as previously reported, in case of IgA deficiency. The IgA EMA represents the most specific test (approximately 100%), with a sensitivity around 94% and a diagnostic accuracy of 97%[83]. However, EMA are routinely detected by indirect subjective immunofluorescence[84]. These antibodies can also result falsely negative in case of IgA deficiency and in children aged > 2 years.
Anti-gliadin antibodies: The antigliadin (AGA) antibodies (IgG and IgA) are today no longer recommended because of their low sensitivity and specificity and inferior accuracy, except in younger children[85].
Deamidated gliadin peptides: Actually detection of antigliadin antibodies have been replaced by the more recently developed immunoassays employing antibodies to deamidated gliadin peptides, IgA and IgG. To increase the diagnostic accuracy, in the last years the clinicians tend to prescribe serial testing.
Histology
The gold standard to diagnose celiac disease in adulthood is the intestinal biopsy sampled by endoscopy[54,86]. Histology of celiac disease consists of an integrated assessment of different entities: villous atrophy, crypt hyperplasia, decreased enterocyte height, inflammatory infiltrates in small-bowel mucosal biopsies. Based on one or more of these elementary lesions the histopathology of celiac disease is subdivided into different diagnostic categories according to the Marsh classification[86] (Table 1).
The open question remains the early lesions, i.e., normal villi with a pathologic increase in intraepithelial T-lymphocytes, that it is possible to find in many others conditions[87]. Villanacci et al[86] pointed out that three conditions deserve specific mention: (1) “Autoimmune enteritis”; (2) Damage by drugs: especially non-steroidal anti-inflammatory drugs (NSAID) that cause morphological modifications likely to those of celiac disease; and (3) The co-infection with Helicobacter pylori in the stomach[86].
Recently, have been introduced methods to quantify pathologic features of the small intestinal mucosa in celiac patients[88].
Genetic analyses
HLA testing should not be routinely performed in all celiac disease cases, but it is indicated only when diagnosis is controversial. Large multicenter studies have shown that only 0.4% of celiac disease patients are both DQ2 and DQ8 negative[89]. In the absence of HLADQ2/8, it is consented to rule out predisposition to celiac disease in family members of celiac patients[86]. HLA test represents a helpful tool particularly for potential celiac disease, to suggest (if positive) or reject (if negative) the diagnosis. Furthermore, HLA negativity in patients with villous atrophy and negative serology should direct towards other possible causes of these histological alterations. Many disorders, such as lactose intolerance, bacterial overgrowth, Crohn’s disease, infectious diseases (i.e., Giardia lamblia, Cryptosporidium, Microsporidium, Cytomegalovirus, Herpes virus, Whipple’s disease), characterized by malabsorption share the same histological findings as celiac disease.
In vitro gluten challenge test
Currently, several studies have proposed that gluten-sensitive immunological activation in celiac disease can be reproduced by in vitro gluten challenge test using culture cells from the duodenal mucosa[90].
CURRENT TREATMENTS OF CELIAC DISEASE
Life-long gluten-free diet
The current available treatment for celiac disease is life-long gluten-free diet[91-93]. Generally clinical improvement is achieved within a few weeks and the mucosal damage recovers in 1-2 years[16]. As patients with celiac disease may have accompanying brush border lactase deficiency secondary to damage to surface epithelial cells, milk and dairy products should be avoided in the first period of treatment too. As vitamin B deficiency is common after an extended period on a GFD, all patients are advised to take a gluten-free multivitamin[84]. Early diagnosis and treatment are fundamental in pediatric celiac disease particularly, as some of the complications may be irreversible: Growth retardation, abnormal dentition, osteoporosis[29]. Several observational studies suggest that prolonging breast-feeding and delaying and gradually introducing gluten in the first year of life may reduce the risk of celiac disease development during childhood[60]. As described above, even products specifically targeted to dietary treatment of celiac disease may contain tiny amounts of gluten proteins[16]. Another cause of uncertainty is represented by the differences in the labeling rules for food products existing among countries. Specific considerations about gluten free diet and refractory celiac disease should be taken. Even with respect of dietary restriction, actually, in the minority of patients affected by refractory celiac disease (RCD), GFD is ineffective. It has showed a higher mortality compared with RCD type 1, explainable by the more severe malnutrition combined with the higher risk of developing overt lymphoma[94]. These forms of the disease can require corticosteroids and other immunosuppressant, like azathioprine or cyclosporin, which can improve transiently clinical symptoms in most patients. But till date, it has not yet been possible to design effective treatments for the both form of RCD[94]. Furthermore, it is important remember that these drugs may enhance the risk of progression into an overt T-cell lymphoma, so they require caution particularly in RCD type 2 patients, at risk of developing this complication. Recently, have been used with some success chemotherapy agents such as the anti-T cell nucleoside analogues Cladribine and Pentostatine, and it has been proposed also as a therapeutic option the stem cell transplantation[95,96].
Other drug-based therapies are in under investigations although patients indicate GFD as a good and well-tolerated therapy[97,98].
Gluten-degrading enzymes
Enzyme supplement therapy with bacterial prolyl-endopeptidasis expressed by various microorganism has been proposed to accelerate gluten digestion in the gastrointestinal tract and thus to destroy T cell epitopes[99]. Prolyl-endopeptidasis are proline-specific enzymes capable to cleave gluten peptides. Actually, there are introduced into clinical trials two drug candidates, ALV003 and AN-PEP (Aspergillus niger prolyl-endoprotease). Recent data on results of two phase 1 clinical trials have revealed that pre-treating gluten with ALV003 eliminates the peripheral blood T cell response in celiac disease patients, suggesting the potential therapeutic utility of gluten-specific enzymes to treat celiac disease[100]. Currently is undergoing clinical phase IIa testing showing a significantly reduce gluten-related T-cell responses compared with placebo but without a significantly reduction of symptoms typically induced by the gluten[101].
AN-PEP is an enzyme that degrades gluten peptides efficiently in a pH compatible with that found in the stomach. Therefore this enzyme might be suitable for oral supplementation but further studies are necessary[102].
Modified grains
Can be developed either through selective breeding of early wheat species or using small interfering RNA (siRNA) technology to mutate or silence immunostimulatory sequence[103].
Blocking gluten entry across the intestinal epithelium
Zonulin inhibitor larazotide (AT-1001) corrects intestinal barrier defects. It has been explored in an animal model[99]. AT-1001 is currently the best-studied pharmacologic agent to treat patients with celiac disease, actually undergone in phase II clinical trials[104]. It has been shown that patients treated with AT-1001 had an improved symptom score, a less pronounced autoantibody response and pro-inflammatory production, and lower urinary nitrate excretion when compared with the placebo controls[105].
Rho/Rho kinase inhibition
It has been clarified that the increase in intestinal permeability is dependent on Rho kinase (ROCK) activity[106]. In addition to regulating tight junction structure and function, ROCK is known to regulate axon growth[107,108]. The drug could be used to establish whether ROCK inhibition can reverse gluten-dependent increase in intestinal permeability in these patients[104].
Immunotherapy
The first observation of the occurrence of celiac disease following allogenic bone marrow transplantation performed in a patient with acute leukemia, made evident the involvement of T-lymphocyte in pathogenesis of this condition[109]. Since then, a lot of acknowledgments have been acquired such that many efforts are being made to develop immunologic therapeutic tools. Cytokine therapies based either on amplification of regulatory cytokines or on blockage of inflammatory cytokines expression are largely diffused for management of the severe autoimmune disorders. Also for celiac disease resistant to dietary approach and especially for refractory celiac disease, the use of immunomodulators is developing. IL-15 blocking antibodies have shown the capability to induce intra-epithelial lymphocytes apoptosis in the intestinal epithelium of human IL-15 transgenic mouse models[110]. These antibodies have been only investigated on patients with rheumatoid arthritis and a human study for celiac disease is still awaited. Only human recombinant IL-10 was tried and it showed suppression of gluten-dependent T-cell activation in celiac disease cultured intestinal mucosa[111]. But later, a pilot study conducted on patients affected by refractory celiac disease did not show any pharmacological efficacy of this monoclonal antibody[110]. Anti-IFN-γ antibodies demonstrated a good tolerance among patients with inflammatory bowel disease, but the use in patients with celiac disease needs of more investigations. Equal considerations can be assumed also for the use of antibodies anti-TNF-α, commonly recognized for the treatment of inflammatory bowel disease but described only in few case reports of patients with refractory celiac disease[112,113]. Another possible target of immunotherapy is represented by chemokines and their receptors, which play a significant role in the pathogenesis of celiac disease through the recruitment of lymphocytes in the gut. T-lymphocytes that home to the small intestine express CCR9, which binds to the CCL25 secreted by intestinal epithelial cells, and integrin α4β7, which binds to mucosal vascular addressin cell 1 (MAdCAM-1). Therefore both molecules are necessary for migration of T-cells to the intestinal mucosa and could represent potential therapeutic targets. Furthermore, a monoclonal antibody anti-integrin α4 (Natalizumab) has revealed effectiveness in Crohn’s disease suggesting a possible effectiveness also in celiac disease[114] as well as a CCR9 inhibitor (CCX282-B) and integrin α4β7 blocking antibody (LDP-02), both already studied in patients affected by Crohn’s disease but still under investigation for celiac disease[115]. Some concern could be raised about the benefit of blocking lymphocyte homing to the intestine, and potential long-term adverse consequences, also because beneficial immunosuppressive regulatory T cells are equally inhibited. Since its demonstration, the possibility to develop tolerance to gluten in certain patients affected by celiac disease has gained more attractiveness as another potential immunomodulatory approach[116,117]. An alternative method studied for induction of tolerance to gluten is oral administration of a genetically modified Lactococus lactis bacterium, capable of secreting deamidated DQ8-restricted gliadin epitope. This experiment was conducted on previously sensitized transgenic mice and demonstrated the induction of Foxp3+ regulatory T-lymphocytes and a significant suppression of local and systemic T-cell responses to the corresponding gliadin peptide[104,118]. Also this approach still needs of human trials, although others clinical trials for non-specific immunomodulation have been carried out to test the role of parasitic infection in inhibition of immune response to gluten[119]. In fact, the disappearance of intestinal parasites from humans in developed countries has created a predisposition to develop autoimmune disease, a phase I clinical trial using larvae from the hookworm Necator Americanus has been initiated with the purpose of establishing a potential shift of T-cells response toward a suppressive T-regulatory response, however to date, any significant effect was revealed by this infection on gluten-induced enteropathy[120].
Vaccines
Clinical trials have been started with a prototypical vaccine based on a set of gluten peptides that are recognized by HLA-DQ2 in an immunodominant manner[104], and phase I has been recently completed. A great interest is focused on vaccination, especially for raising the compliance of many patients which could beneficiate with a single-dose administration rather than a daily intake of other treatment options[110]. The risk of immune system activation related to the vaccine therapy and its side effects represent a still open question that need of further investigations. There is still need of more studies also for the most part of the previously mentioned alternative treatment options, with large long-term clinical trials that could answer to the unresolved questions relating to their real clinical effectiveness, their safety, and their affordability.
CONCLUSION
It is indubitable that celiac disease remains a still controversial and complex human disorder. There is need of further research studies and randomized clinical trials to introduce them into usual management of this disease. A number of unanswered questions remain to clarify including the real associations of celiac disease with other conditions, and the impact of some environmental factor in its pathogenesis. There are still controversial opinion about the effective role of the breast feeding in celiac disease, what is to be elucidated if it could offer a permanent protection or if only delays the appearance of the disease. In addition, an improvement in non-invasive diagnostic tests could allow avoidance of endoscopy, especially in pediatric patients, and a more defined efficacy of the new therapeutic tools could improve quality of life either in term of reduction of complications and physical health either in term of social life.
Footnotes
Conflict-of-interest statement: The authors declare that they have no competing interests.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: April 25, 2016
First decision: June 6, 2016
Article in press: March 24, 2017
P- Reviewer: Krupa-Kozak U, Vasudevan A S- Editor: Song XX L- Editor: A E- Editor: Wu HL
References
- 1.Losowsky MS. A history of coeliac disease. Dig Dis. 2008;26:112–120. doi: 10.1159/000116768. [DOI] [PubMed] [Google Scholar]
- 2.Dicke WK, Weijers HA, Van de kamer JH. Coeliac disease. II. The presence in wheat of a factor having a deleterious effect in cases of coeliac disease. Acta Paediatr. 1953;42:34–42. doi: 10.1111/j.1651-2227.1953.tb05563.x. [DOI] [PubMed] [Google Scholar]
- 3.Elli L, Branchi F, Tomba C, Villalta D, Norsa L, Ferretti F, Roncoroni L, Bardella MT. Diagnosis of gluten related disorders: Celiac disease, wheat allergy and non-celiac gluten sensitivity. World J Gastroenterol. 2015;21:7110–7119. doi: 10.3748/wjg.v21.i23.7110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fasano A, Catassi C. Current approaches to diagnosis and treatment of celiac disease: an evolving spectrum. Gastroenterology. 2001;120:636–651. doi: 10.1053/gast.2001.22123. [DOI] [PubMed] [Google Scholar]
- 5.Green PH, Lebwohl B, Greywoode R. Celiac disease. J Allergy Clin Immunol. 2015;135:1099–1106; quiz 1107. doi: 10.1016/j.jaci.2015.01.044. [DOI] [PubMed] [Google Scholar]
- 6.Assimakopoulos SF, Papageorgiou I, Charonis A. Enterocytes’ tight junctions: From molecules to diseases. World J Gastrointest Pathophysiol. 2011;2:123–137. doi: 10.4291/wjgp.v2.i6.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeon MK, Klaus C, Kaemmerer E, Gassler N. Intestinal barrier: Molecular pathways and modifiers. World J Gastrointest Pathophysiol. 2013;4:94–99. doi: 10.4291/wjgp.v4.i4.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rubio-Tapia A, Kyle RA, Kaplan EL, Johnson DR, Page W, Erdtmann F, Brantner TL, Kim WR, Phelps TK, Lahr BD, et al. Increased prevalence and mortality in undiagnosed celiac disease. Gastroenterology. 2009;137:88–93. doi: 10.1053/j.gastro.2009.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holmes S. Coeliac disease: symptoms, complications and patient support. Nurs Stand. 2010;24:505–506: quiz 508. doi: 10.7748/ns2010.05.24.35.50.c7752. [DOI] [PubMed] [Google Scholar]
- 10.Norström F, Lindholm L, Sandström O, Nordyke K, Ivarsson A. Delay to celiac disease diagnosis and its implications for health-related quality of life. BMC Gastroenterol. 2011;11:118. doi: 10.1186/1471-230X-11-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elli L, Roncoroni L, Bardella MT. Non-celiac gluten sensitivity: Time for sifting the grain. World J Gastroenterol. 2015;21:8221–8226. doi: 10.3748/wjg.v21.i27.8221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fasano A, Berti I, Gerarduzzi T, Not T, Colletti RB, Drago S, Elitsur Y, Green PH, Guandalini S, Hill ID, et al. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med. 2003;163:286–292. doi: 10.1001/archinte.163.3.286. [DOI] [PubMed] [Google Scholar]
- 13.Rewers M. Epidemiology of celiac disease: what are the prevalence, incidence, and progression of celiac disease? Gastroenterology. 2005;128:S47–S51. doi: 10.1053/j.gastro.2005.02.030. [DOI] [PubMed] [Google Scholar]
- 14.Fasano A. Where have all the American celiacs gone? Acta Paediatr Suppl. 1996;412:20–24. doi: 10.1111/j.1651-2227.1996.tb14242.x. [DOI] [PubMed] [Google Scholar]
- 15.Mustalahti K, Catassi C, Reunanen A, Fabiani E, Heier M, McMillan S, Murray L, Metzger MH, Gasparin M, Bravi E, et al. The prevalence of celiac disease in Europe: results of a centralized, international mass screening project. Ann Med. 2010;42:587–595. doi: 10.3109/07853890.2010.505931. [DOI] [PubMed] [Google Scholar]
- 16.Lionetti E, Catassi C. New clues in celiac disease epidemiology, pathogenesis, clinical manifestations, and treatment. Int Rev Immunol. 2011;30:219–231. doi: 10.3109/08830185.2011.602443. [DOI] [PubMed] [Google Scholar]
- 17.Vriezinga SL, Schweizer JJ, Koning F, Mearin ML. Coeliac disease and gluten-related disorders in childhood. Nat Rev Gastroenterol Hepatol. 2015;12:527–536. doi: 10.1038/nrgastro.2015.98. [DOI] [PubMed] [Google Scholar]
- 18.Cataldo F, Montalto G. Celiac disease in the developing countries: a new and challenging public health problem. World J Gastroenterol. 2007;13:2153–2159. doi: 10.3748/wjg.v13.i15.2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barada K, Bitar A, Mokadem MA, Hashash JG, Green P. Celiac disease in Middle Eastern and North African countries: a new burden? World J Gastroenterol. 2010;16:1449–1457. doi: 10.3748/wjg.v16.i12.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malekzadeh R, Sachdev A, Fahid Ali A. Coeliac disease in developing countries: Middle East, India and North Africa. Best Pract Res Clin Gastroenterol. 2005;19:351–358. doi: 10.1016/j.bpg.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 21.Catassi C, Doloretta Macis M, Rätsch IM, De Virgiliis S, Cucca F. The distribution of DQ genes in the Saharawi population provides only a partial explanation for the high celiac disease prevalence. Tissue Antigens. 2001;58:402–406. doi: 10.1034/j.1399-0039.2001.580609.x. [DOI] [PubMed] [Google Scholar]
- 22.Catassi C, Rätsch IM, Gandolfi L, Pratesi R, Fabiani E, El Asmar R, Frijia M, Bearzi I, Vizzoni L. Why is coeliac disease endemic in the people of the Sahara? Lancet. 1999;354:647–648. doi: 10.1016/s0140-6736(99)02609-4. [DOI] [PubMed] [Google Scholar]
- 23.Trynka G, Wijmenga C, van Heel DA. A genetic perspective on coeliac disease. Trends Mol Med. 2010;16:537–550. doi: 10.1016/j.molmed.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 24.Romanos J, van Diemen CC, Nolte IM, Trynka G, Zhernakova A, Fu J, Bardella MT, Barisani D, McManus R, van Heel DA, et al. Analysis of HLA and non-HLA alleles can identify individuals at high risk for celiac disease. Gastroenterology. 2009;137:834–840, 840.e1-3. doi: 10.1053/j.gastro.2009.05.040. [DOI] [PubMed] [Google Scholar]
- 25.Dieli-Crimi R, Cénit MC, Núñez C. The genetics of celiac disease: A comprehensive review of clinical implications. J Autoimmun. 2015;64:26–41. doi: 10.1016/j.jaut.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 26.Sollid LM, Markussen G, Ek J, Gjerde H, Vartdal F, Thorsby E. Evidence for a primary association of celiac disease to a particular HLA-DQ alpha/beta heterodimer. J Exp Med. 1989;169:345–350. doi: 10.1084/jem.169.1.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuja-Halkola R, Lebwohl B, Halfvarson J, Wijmenga C, Magnusson PK, Ludvigsson JF. Heritability of non-HLA genetics in coeliac disease: a population-based study in 107 000 twins. Gut. 2016;65:1793–1798. doi: 10.1136/gutjnl-2016-311713. [DOI] [PubMed] [Google Scholar]
- 28.Dubois PC, Trynka G, Franke L, Hunt KA, Romanos J, Curtotti A, Zhernakova A, Heap GA, Adány R, Aromaa A, et al. Multiple common variants for celiac disease influencing immune gene expression. Nat Genet. 2010;42:295–302. doi: 10.1038/ng.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Freeman HJ, Chopra A, Clandinin MT, Thomson AB. Recent advances in celiac disease. World J Gastroenterol. 2011;17:2259–2272. doi: 10.3748/wjg.v17.i18.2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wolters VM, Verbeek WH, Zhernakova A, Onland-Moret C, Schreurs MW, Monsuur AJ, Verduijn W, Wijmenga C, Mulder CJ. The MYO9B gene is a strong risk factor for developing refractory celiac disease. Clin Gastroenterol Hepatol. 2007;5:1399–1405, 1405.e1-2. doi: 10.1016/j.cgh.2007.08.018. [DOI] [PubMed] [Google Scholar]
- 31.Qiao SW, Sollid LM, Blumberg RS. Antigen presentation in celiac disease. Curr Opin Immunol. 2009;21:111–117. doi: 10.1016/j.coi.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ráki M, Schjetne KW, Stamnaes J, Molberg Ø, Jahnsen FL, Issekutz TB, Bogen B, Sollid LM. Surface expression of transglutaminase 2 by dendritic cells and its potential role for uptake and presentation of gluten peptides to T cells. Scand J Immunol. 2007;65:213–220. doi: 10.1111/j.1365-3083.2006.01881.x. [DOI] [PubMed] [Google Scholar]
- 33.Troncone R, Auricchio S. Rotavirus and celiac disease: clues to the pathogenesis and perspectives on prevention. J Pediatr Gastroenterol Nutr. 2007;44:527–528. doi: 10.1097/MPG.0b013e31804ca0ec. [DOI] [PubMed] [Google Scholar]
- 34.Troncone R, Jabri B. Coeliac disease and gluten sensitivity. J Intern Med. 2011;269:582–590. doi: 10.1111/j.1365-2796.2011.02385.x. [DOI] [PubMed] [Google Scholar]
- 35.Stene LC, Honeyman MC, Hoffenberg EJ, Haas JE, Sokol RJ, Emery L, Taki I, Norris JM, Erlich HA, Eisenbarth GS, et al. Rotavirus infection frequency and risk of celiac disease autoimmunity in early childhood: a longitudinal study. Am J Gastroenterol. 2006;101:2333–2340. doi: 10.1111/j.1572-0241.2006.00741.x. [DOI] [PubMed] [Google Scholar]
- 36.Pinier M, Fuhrmann G, Verdu EF, Leroux JC. Prevention measures and exploratory pharmacological treatments of celiac disease. Am J Gastroenterol. 2010;105:2551–2561; quiz 2562. doi: 10.1038/ajg.2010.372. [DOI] [PubMed] [Google Scholar]
- 37.Catassi C, Fabiani E, Iacono G, D’Agate C, Francavilla R, Biagi F, Volta U, Accomando S, Picarelli A, De Vitis I, et al. A prospective, double-blind, placebo-controlled trial to establish a safe gluten threshold for patients with celiac disease. Am J Clin Nutr. 2007;85:160–166. doi: 10.1093/ajcn/85.1.160. [DOI] [PubMed] [Google Scholar]
- 38.Silano M, Agostoni C, Guandalini S. Effect of the timing of gluten introduction on the development of celiac disease. World J Gastroenterol. 2010;16:1939–1942. doi: 10.3748/wjg.v16.i16.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sanz Y, De Pama G, Laparra M. Unraveling the ties between celiac disease and intestinal microbiota. Int Rev Immunol. 2011;30:207–218. doi: 10.3109/08830185.2011.599084. [DOI] [PubMed] [Google Scholar]
- 40.Elli L, Rossi V, Conte D, Ronchi A, Tomba C, Passoni M, Bardella MT, Roncoroni L, Guzzi G. Increased Mercury Levels in Patients with Celiac Disease following a Gluten-Free Regimen. Gastroenterol Res Pract. 2015;2015:953042. doi: 10.1155/2015/953042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lerner A, Matthias T. Possible association between celiac disease and bacterial transglutaminase in food processing: a hypothesis. Nutr Rev. 2015;73:544–552. doi: 10.1093/nutrit/nuv011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.du Pré MF, Sollid LM. T-cell and B-cell immunity in celiac disease. Best Pract Res Clin Gastroenterol. 2015;29:413–423. doi: 10.1016/j.bpg.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 43.Kim SM, Mayassi T, Jabri B. Innate immunity: actuating the gears of celiac disease pathogenesis. Best Pract Res Clin Gastroenterol. 2015;29:425–435. doi: 10.1016/j.bpg.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mazzarella G. Effector and suppressor T cells in celiac disease. World J Gastroenterol. 2015;21:7349–7356. doi: 10.3748/wjg.v21.i24.7349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Björck S, Lindehammer SR, Fex M, Agardh D. Serum cytokine pattern in young children with screening detected coeliac disease. Clin Exp Immunol. 2015;179:230–235. doi: 10.1111/cei.12454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Matthias T, Neidhöfer S, Pfeiffer S, Prager K, Reuter S, Gershwin ME. Novel trends in celiac disease. Cell Mol Immunol. 2011;8:121–125. doi: 10.1038/cmi.2010.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hayat M, Cairns A, Dixon MF, O’Mahony S. Quantitation of intraepithelial lymphocytes in human duodenum: what is normal? J Clin Pathol. 2002;55:393–394. doi: 10.1136/jcp.55.5.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Veress B, Franzén L, Bodin L, Borch K. Duodenal intraepithelial lymphocyte-count revisited. Scand J Gastroenterol. 2004;39:138–144. doi: 10.1080/00365520310007675. [DOI] [PubMed] [Google Scholar]
- 49.Mubarak A, Wolters VM, Houwen RH, ten Kate FJ. Immunohistochemical CD3 staining detects additional patients with celiac disease. World J Gastroenterol. 2015;21:7553–7557. doi: 10.3748/wjg.v21.i24.7553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hudacko R, Kathy Zhou X, Yantiss RK. Immunohistochemical stains for CD3 and CD8 do not improve detection of gluten-sensitive enteropathy in duodenal biopsies. Mod Pathol. 2013;26:1241–1245. doi: 10.1038/modpathol.2013.57. [DOI] [PubMed] [Google Scholar]
- 51.Elli L, Zini E, Tomba C, Bardella MT, Bosari S, Conte D, Runza L, Roncoroni L, Ferrero S. Histological evaluation of duodenal biopsies from coeliac patients: the need for different grading criteria during follow-up. BMC Gastroenterol. 2015;15:133. doi: 10.1186/s12876-015-0361-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marsh MN. Gluten, major histocompatibility complex, and the small intestine. A molecular and immunobiologic approach to the spectrum of gluten sensitivity (‘celiac sprue’) Gastroenterology. 1992;102:330–354. [PubMed] [Google Scholar]
- 53.Oberhuber G. Histopathology of celiac disease. Biomed Pharmacother. 2000;54:368–372. doi: 10.1016/S0753-3322(01)80003-2. [DOI] [PubMed] [Google Scholar]
- 54.Mills JR, Murray JA. Contemporary celiac disease diagnosis: is a biopsy avoidable? Curr Opin Gastroenterol. 2016;32:80–85. doi: 10.1097/MOG.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 55.Oberhuber G, Granditsch G, Vogelsang H. The histopathology of coeliac disease: time for a standardized report scheme for pathologists. Eur J Gastroenterol Hepatol. 1999;11:1185–1194. doi: 10.1097/00042737-199910000-00019. [DOI] [PubMed] [Google Scholar]
- 56.Ludvigsson JF, Leffler DA, Bai JC, Biagi F, Fasano A, Green PH, Hadjivassiliou M, Kaukinen K, Kelly CP, Leonard JN, et al. The Oslo definitions for coeliac disease and related terms. Gut. 2013;62:43–52. doi: 10.1136/gutjnl-2011-301346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tully MA. Pediatric celiac disease. Gastroenterol Nurs. 2008;31:132–140; quiz 141-142. doi: 10.1097/01.SGA.0000316532.69484.44. [DOI] [PubMed] [Google Scholar]
- 58.Troncone R, Greco L, Mayer M, Paparo F, Caputo N, Micillo M, Mugione P, Auricchio S. Latent and potential coeliac disease. Acta Paediatr Suppl. 1996;412:10–14. doi: 10.1111/j.1651-2227.1996.tb14240.x. [DOI] [PubMed] [Google Scholar]
- 59.Ho-Yen C, Chang F, van der Walt J, Mitchell T, Ciclitira P. Recent advances in refractory coeliac disease: a review. Histopathology. 2009;54:783–795. doi: 10.1111/j.1365-2559.2008.03112.x. [DOI] [PubMed] [Google Scholar]
- 60.Rodrigo-Sáez L, Fuentes-Álvarez D, Pérez-Martínez I, Alvarez-Mieres N, Niño-García P, de-Francisco-García R, Riestra-Menéndez S, Bousoño-García C, Alonso-Arias R, López-Vázquez A. Differences between pediatric and adult celiac disease. Rev Esp Enferm Dig. 2011;103:238–244. [PubMed] [Google Scholar]
- 61.Barker JM, Liu E. Celiac disease: pathophysiology, clinical manifestations, and associated autoimmune conditions. Adv Pediatr. 2008;55:349–365. doi: 10.1016/j.yapd.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Akirov A, Pinhas-Hamiel O. Co-occurrence of type 1 diabetes mellitus and celiac disease. World J Diabetes. 2015;6:707–714. doi: 10.4239/wjd.v6.i5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ludvigsson JF, Ludvigsson J, Ekbom A, Montgomery SM. Celiac disease and risk of subsequent type 1 diabetes: a general population cohort study of children and adolescents. Diabetes Care. 2006;29:2483–2488. doi: 10.2337/dc06-0794. [DOI] [PubMed] [Google Scholar]
- 64.Bao F, Yu L, Babu S, Wang T, Hoffenberg EJ, Rewers M, Eisenbarth GS. One third of HLA DQ2 homozygous patients with type 1 diabetes express celiac disease-associated transglutaminase autoantibodies. J Autoimmun. 1999;13:143–148. doi: 10.1006/jaut.1999.0303. [DOI] [PubMed] [Google Scholar]
- 65.Ch’ng CL, Jones MK, Kingham JG. Celiac disease and autoimmune thyroid disease. Clin Med Res. 2007;5:184–192. doi: 10.3121/cmr.2007.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Norris JM, Barriga K, Klingensmith G, Hoffman M, Eisenbarth GS, Erlich HA, Rewers M. Timing of initial cereal exposure in infancy and risk of islet autoimmunity. JAMA. 2003;290:1713–1720. doi: 10.1001/jama.290.13.1713. [DOI] [PubMed] [Google Scholar]
- 67.Norris JM, Barriga K, Hoffenberg EJ, Taki I, Miao D, Haas JE, Emery LM, Sokol RJ, Erlich HA, Eisenbarth GS, et al. Risk of celiac disease autoimmunity and timing of gluten introduction in the diet of infants at increased risk of disease. JAMA. 2005;293:2343–2351. doi: 10.1001/jama.293.19.2343. [DOI] [PubMed] [Google Scholar]
- 68.Ziegler AG, Schmid S, Huber D, Hummel M, Bonifacio E. Early infant feeding and risk of developing type 1 diabetes-associated autoantibodies. JAMA. 2003;290:1721–1728. doi: 10.1001/jama.290.13.1721. [DOI] [PubMed] [Google Scholar]
- 69.Hummel M, Bonifacio E, Naserke HE, Ziegler AG. Elimination of dietary gluten does not reduce titers of type 1 diabetes-associated autoantibodies in high-risk subjects. Diabetes Care. 2002;25:1111–1116. doi: 10.2337/diacare.25.7.1111. [DOI] [PubMed] [Google Scholar]
- 70.Stazi AV, Trinti B. Selenium status and over-expression of interleukin-15 in celiac disease and autoimmune thyroid diseases. Ann Ist Super Sanita. 2010;46:389–399. doi: 10.4415/ANN_10_04_06. [DOI] [PubMed] [Google Scholar]
- 71.Anania C, De Luca E, De Castro G, Chiesa C, Pacifico L. Liver involvement in pediatric celiac disease. World J Gastroenterol. 2015;21:5813–5822. doi: 10.3748/wjg.v21.i19.5813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bardella MT, Vecchi M, Conte D, Del Ninno E, Fraquelli M, Pacchetti S, Minola E, Landoni M, Cesana BM, De Franchis R. Chronic unexplained hypertransaminasemia may be caused by occult celiac disease. Hepatology. 1999;29:654–657. doi: 10.1002/hep.510290318. [DOI] [PubMed] [Google Scholar]
- 73.Rubio-Tapia A, Murray JA. The liver in celiac disease. Hepatology. 2007;46:1650–1658. doi: 10.1002/hep.21949. [DOI] [PubMed] [Google Scholar]
- 74.González-Abraldes J, Sánchez-Fueyo A, Bessa X, Moitinho E, Feu F, Mas A, Escorsell A, Bruguera M. Persistent hypertransaminasemia as the presenting feature of celiac disease. Am J Gastroenterol. 1999;94:1095–1097. doi: 10.1111/j.1572-0241.1999.01021.x. [DOI] [PubMed] [Google Scholar]
- 75.Volta U. Pathogenesis and clinical significance of liver injury in celiac disease. Clin Rev Allergy Immunol. 2009;36:62–70. doi: 10.1007/s12016-008-8086-x. [DOI] [PubMed] [Google Scholar]
- 76.Zali MR, Rostami Nejad M, Rostami K, Alavian SM. Liver complications in celiac disease. Hepat Mon. 2011;11:333–341. [PMC free article] [PubMed] [Google Scholar]
- 77.Bushara KO. Neurologic presentation of celiac disease. Gastroenterology. 2005;128:S92–S97. doi: 10.1053/j.gastro.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 78.Grossman G. Neurological complications of coeliac disease: what is the evidence? Pract Neurol. 2008;8:77–89. doi: 10.1136/jnnp.2007.139717. [DOI] [PubMed] [Google Scholar]
- 79.Gobbi G. Coeliac disease, epilepsy and cerebral calcifications. Brain Dev. 2005;27:189–200. doi: 10.1016/j.braindev.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 80.Smedby KE, Akerman M, Hildebrand H, Glimelius B, Ekbom A, Askling J. Malignant lymphomas in coeliac disease: evidence of increased risks for lymphoma types other than enteropathy-type T cell lymphoma. Gut. 2005;54:54–59. doi: 10.1136/gut.2003.032094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Richir M, Songun I, Wientjes C, Snel P, Dwars B. Small Bowel Adenocarcinoma in a Patient with Coeliac Disease: Case Report and Review of the Literature. Case Rep Gastroenterol. 2010;4:416–420. doi: 10.1159/000313547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ozgör B, Selimoğlu MA. Coeliac disease and reproductive disorders. Scand J Gastroenterol. 2010;45:395–402. doi: 10.3109/00365520903508902. [DOI] [PubMed] [Google Scholar]
- 83.Volta U, Villanacci V. Celiac disease: diagnostic criteria in progress. Cell Mol Immunol. 2011;8:96–102. doi: 10.1038/cmi.2010.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ludvigsson JF, Green PH. Clinical management of coeliac disease. J Intern Med. 2011;269:560–571. doi: 10.1111/j.1365-2796.2011.02379.x. [DOI] [PubMed] [Google Scholar]
- 85.Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol. 2013;108:656–676; quiz 677. doi: 10.1038/ajg.2013.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Villanacci V, Ceppa P, Tavani E, Vindigni C, Volta U. Coeliac disease: the histology report. Dig Liver Dis. 2011;43 Suppl 4:S385–S395. doi: 10.1016/S1590-8658(11)60594-X. [DOI] [PubMed] [Google Scholar]
- 87.Lerner A, Matthias T. Rheumatoid arthritis-celiac disease relationship: joints get that gut feeling. Autoimmun Rev. 2015;14:1038–1047. doi: 10.1016/j.autrev.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 88.Ciaccio EJ, Bhagat G, Lewis SK, Green PH. Quantitative image analysis of celiac disease. World J Gastroenterol. 2015;21:2577–2581. doi: 10.3748/wjg.v21.i9.2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Catassi C, Fasano A. Celiac disease diagnosis: simple rules are better than complicated algorithms. Am J Med. 2010;123:691–693. doi: 10.1016/j.amjmed.2010.02.019. [DOI] [PubMed] [Google Scholar]
- 90.Khalesi M, Jafari SA, Kiani M, Picarelli A, Borghini R, Sadeghi R, Eghtedar A, Ayatollahi H, Kianifar HR. In Vitro Gluten Challenge Test for Celiac Disease Diagnosis. J Pediatr Gastroenterol Nutr. 2016;62:276–283. doi: 10.1097/MPG.0000000000000917. [DOI] [PubMed] [Google Scholar]
- 91.Hassan K, A-Kader H. Celiac disease: the search for adjunctive or alternative therapies. Expert Rev Gastroenterol Hepatol. 2014;8:313–321. doi: 10.1586/17474124.2014.882769. [DOI] [PubMed] [Google Scholar]
- 92.Makharia GK. Current and emerging therapy for celiac disease. Front Med (Lausanne) 2014;1:6. doi: 10.3389/fmed.2014.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Plugis NM, Khosla C. Therapeutic approaches for celiac disease. Best Pract Res Clin Gastroenterol. 2015;29:503–521. doi: 10.1016/j.bpg.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Malamut G, Cellier C. Is refractory celiac disease more severe in old Europe? Am J Gastroenterol. 2011;106:929–932. doi: 10.1038/ajg.2011.105. [DOI] [PubMed] [Google Scholar]
- 95.Dray X, Joly F, Lavergne-Slove A, Treton X, Bouhnik Y, Messing B. A severe but reversible refractory sprue. Gut. 2006;55:1210–1211. doi: 10.1136/gut.2005.089987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Al-Toma A, Verbeek WH, Mulder CJ. Update on the management of refractory coeliac disease. J Gastrointestin Liver Dis. 2007;16:57–63. [PubMed] [Google Scholar]
- 97.Norsa L, Tomba C, Agostoni C, Branchi F, Bardella MT, Roncoroni L, Conte D, Elli L. Gluten-free diet or alternative therapy: a survey on what parents of celiac children want. Int J Food Sci Nutr. 2015;66:590–594. doi: 10.3109/09637486.2015.1064872. [DOI] [PubMed] [Google Scholar]
- 98.Tomal J, McKiernan D, Guandalini S, Semrad CE, Kupfer S. Celiac patients’ attitudes regarding novel therapies. Minerva Gastroenterol Dietol. 2016;62:275–280. [PubMed] [Google Scholar]
- 99.Fasano A, Araya M, Bhatnagar S, Cameron D, Catassi C, Dirks M, Mearin ML, Ortigosa L, Phillips A. Federation of International Societies of Pediatric Gastroenterology, Hepatology, and Nutrition consensus report on celiac disease. J Pediatr Gastroenterol Nutr. 2008;47:214–219. doi: 10.1097/MPG.0b013e318181afed. [DOI] [PubMed] [Google Scholar]
- 100.Siegel M, Garber ME, Spencer AG, Botwick W, Kumar P, Williams RN, Kozuka K, Shreeniwas R, Pratha V, Adelman DC. Safety, tolerability, and activity of ALV003: results from two phase 1 single, escalating-dose clinical trials. Dig Dis Sci. 2012;57:440–450. doi: 10.1007/s10620-011-1906-5. [DOI] [PubMed] [Google Scholar]
- 101.Tye-Din JA, Anderson RP, Ffrench RA, Brown GJ, Hodsman P, Siegel M, Botwick W, Shreeniwas R. The effects of ALV003 pre-digestion of gluten on immune response and symptoms in celiac disease in vivo. Clin Immunol. 2010;134:289–295. doi: 10.1016/j.clim.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 102.Mitea C, Havenaar R, Drijfhout JW, Edens L, Dekking L, Koning F. Efficient degradation of gluten by a prolyl endoprotease in a gastrointestinal model: implications for coeliac disease. Gut. 2008;57:25–32. doi: 10.1136/gut.2006.111609. [DOI] [PubMed] [Google Scholar]
- 103.Setty M, Hormaza L, Guandalini S. Celiac disease: risk assessment, diagnosis, and monitoring. Mol Diagn Ther. 2008;12:289–298. doi: 10.1007/BF03256294. [DOI] [PubMed] [Google Scholar]
- 104.Sollid LM, Khosla C. Novel therapies for coeliac disease. J Intern Med. 2011;269:604–613. doi: 10.1111/j.1365-2796.2011.02376.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Schuppan D, Junker Y, Barisani D. Celiac disease: from pathogenesis to novel therapies. Gastroenterology. 2009;137:1912–1933. doi: 10.1053/j.gastro.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 106.Utech M, Ivanov AI, Samarin SN, Bruewer M, Turner JR, Mrsny RJ, Parkos CA, Nusrat A. Mechanism of IFN-gamma-induced endocytosis of tight junction proteins: myosin II-dependent vacuolarization of the apical plasma membrane. Mol Biol Cell. 2005;16:5040–5052. doi: 10.1091/mbc.E05-03-0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.McKerracher L, Higuchi H. Targeting Rho to stimulate repair after spinal cord injury. J Neurotrauma. 2006;23:309–317. doi: 10.1089/neu.2006.23.309. [DOI] [PubMed] [Google Scholar]
- 108.González-Mariscal L, Lechuga S, Garay E. Role of tight junctions in cell proliferation and cancer. Prog Histochem Cytochem. 2007;42:1–57. doi: 10.1016/j.proghi.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 109.Bargetzi MJ, Schönenberger A, Tichelli A, Fried R, Cathomas G, Signer E, Speck B, Gratwohl A. Celiac disease transmitted by allogeneic non-T cell-depleted bone marrow transplantation. Bone Marrow Transplant. 1997;20:607–609. doi: 10.1038/sj.bmt.1700926. [DOI] [PubMed] [Google Scholar]
- 110.Rashtak S, Murray JA. Review article: coeliac disease, new approaches to therapy. Aliment Pharmacol Ther. 2012;35:768–781. doi: 10.1111/j.1365-2036.2012.05013.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Salvati VM, Mazzarella G, Gianfrani C, Levings MK, Stefanile R, De Giulio B, Iaquinto G, Giardullo N, Auricchio S, Roncarolo MG, et al. Recombinant human interleukin 10 suppresses gliadin dependent T cell activation in ex vivo cultured coeliac intestinal mucosa. Gut. 2005;54:46–53. doi: 10.1136/gut.2003.023150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gillett HR, Arnott ID, McIntyre M, Campbell S, Dahele A, Priest M, Jackson R, Ghosh S. Successful infliximab treatment for steroid-refractory celiac disease: a case report. Gastroenterology. 2002;122:800–805. doi: 10.1053/gast.2002.31874. [DOI] [PubMed] [Google Scholar]
- 113.Costantino G, della Torre A, Lo Presti MA, Caruso R, Mazzon E, Fries W. Treatment of life-threatening type I refractory coeliac disease with long-term infliximab. Dig Liver Dis. 2008;40:74–77. doi: 10.1016/j.dld.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 114.Ghosh S, Goldin E, Gordon FH, Malchow HA, Rask-Madsen J, Rutgeerts P, Vyhnálek P, Zádorová Z, Palmer T, Donoghue S. Natalizumab for active Crohn’s disease. N Engl J Med. 2003;348:24–32. doi: 10.1056/NEJMoa020732. [DOI] [PubMed] [Google Scholar]
- 115.Crespo Pérez L, Castillejo de Villasante G, Cano Ruiz A, León F. Non-dietary therapeutic clinical trials in coeliac disease. Eur J Intern Med. 2012;23:9–14. doi: 10.1016/j.ejim.2011.08.030. [DOI] [PubMed] [Google Scholar]
- 116.Hopman EG, von Blomberg ME, Batstra MR, Morreau H, Dekker FW, Koning F, Lamers CB, Mearin ML. Gluten tolerance in adult patients with celiac disease 20 years after diagnosis? Eur J Gastroenterol Hepatol. 2008;20:423–429. doi: 10.1097/MEG.0b013e3282f4de6e. [DOI] [PubMed] [Google Scholar]
- 117.Bardella MT, Fredella C, Trovato C, Ermacora E, Cavalli R, Saladino V, Prampolini L. Long-term remission in patients with dermatitis herpetiformis on a normal diet. Br J Dermatol. 2003;149:968–971. doi: 10.1111/j.1365-2133.2003.05579.x. [DOI] [PubMed] [Google Scholar]
- 118.Huibregtse IL, Marietta EV, Rashtak S, Koning F, Rottiers P, David CS, van Deventer SJ, Murray JA. Induction of antigen-specific tolerance by oral administration of Lactococcus lactis delivered immunodominant DQ8-restricted gliadin peptide in sensitized nonobese diabetic Abo Dq8 transgenic mice. J Immunol. 2009;183:2390–2396. doi: 10.4049/jimmunol.0802891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Daveson AJ, Jones DM, Gaze S, McSorley H, Clouston A, Pascoe A, Cooke S, Speare R, Macdonald GA, Anderson R, et al. Effect of hookworm infection on wheat challenge in celiac disease--a randomised double-blinded placebo controlled trial. PLoS One. 2011;6:e17366. doi: 10.1371/journal.pone.0017366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Scanlon SA, Murray JA. Update on celiac disease - etiology, differential diagnosis, drug targets, and management advances. Clin Exp Gastroenterol. 2011;4:297–311. doi: 10.2147/CEG.S8315. [DOI] [PMC free article] [PubMed] [Google Scholar]


