Abstract
AIM
To investigate interferon-γ-inducible protein-10’s (IP-10) potential to anticipate rapid (RVR)- and sustained virological responses (SVR) to chronic hepatitis C (CHC) treatment.
METHODS
We included case series examining RVR or SVR in relation to 24 or 48 wk treatment for CHC, in patients treatment free for at least six months, with genotype 1 or 4, and in relation to 24 wk treatment for genotype 2 and 3, with pegylated interferon in combination with ribavirin. Patients had to have both a baseline IP-10 level as well as a hepatitis C virus (HCV)-RNA determination 4 wk after treatment initiation or 24 wk after end of treatment. Studies including patients with liver diseases other than CHC, human immunodeficiency virus-infection, treatment with immunosuppresents or cytostatica, alcohol dependency or active intravenous drug-use were excluded. We found 81 articles by searching the MEDLINE and EMBASE databases. Eight studies were eligible for inclusion. Their quality were assesed using an 18 point checklist for case series, developed using a modified Delphi technique. Information was extracted from the articles, and no raw data was requisitioned. The review protocol was registered at the International Prospective Register of Systematic Reviews (reg. number: CRD42014008736).
RESULTS
Three studies reported on baseline IP-10 level in association with RVR. A signigficant association was found for HCV genotype 1 infection by two studies. Only two studies reported on HCV genotype 4 infected and genotype 2 and 3 infected patients, respectively. A trend was seen for an association between RVR and baseline IP-10 for genotype 4, while no association was found for genotype 2 and 3. Seven studies provided information regarding baseline IP-10 and SVR. Following the pattern regarding rapid virological response all five studies examining SVR in relation to baseline IP-10 levels for HCV, genotype 1 infected patients showed a significant association. Likewise a significant association was seen for HCV, genotype 4 infected, while no association was found for HCV, genotype 2 and 3 infected. Though only two studies examined the assosiation for HCV genotype 4 infected and HCV genotype 2 and 3 infected respectively.
CONCLUSION
We found indications of a possible association between baseline IP-10 level and virological responses in patients with CHC genotype 1 and 4.
Keywords: Chronic hepatitis C, Inducible protein-10’s, Sustained virological response, Interferon-γ-inducible protein-10, CXCL-10, Chemokine, Genotype, Pegylated interferon, Ribavirin, Rapid virological response
Core tip: This is the first systematic review examining the association between baseline levels of interferon-γ-inducible protein-10 (IP-10) and virological response to treatment with pegylated interferon and ribavirin among patients chronically infected with hepatitis C virus, genotype 1-4. We found a possible correlation for genotype 1 and 4 infected patients, indicating that baseline IP-10 levels could predict which patients, infected with genotype 1 or 4, would have the highest likelihood of benefitting from antiviral treatment with pegylated interferon and ribavirin. These findings can be especially relevant in countries, where treatments with direct acting antivirals are not readily applicable.
INTRODUCTION
Every year 3-4 million individuals are infected with hepatitis C virus (HCV) of whom only 20%-35% clear the infection, meaning that 2.4-3.2 million individuals remain chronically infected, defined as detectable HCV-RNA in two consecutive measurements ≥ six months apart. Globally, the prevalence of chronic hepatitis C (CHC) is estimated to 150 million people, with CHC being the leading cause of chronic liver disease[1]. CHC can lead to formation of connective tissue (fibrosis) in the liver. However, the rate and severity of the inflammation and fibrosis vary[2,3]. Though only 5%-20% of HCV infected patients develop cirrhosis, these patients have an increased risk of developing hepatocellular carcinoma, a condition responsible for more than 300000 deaths annually[1].
Until recently, the standard of care for CHC was lengthy dual therapy with pegylated interferon plus ribavirin (peg-IFN/RBV), either as 180 μg peg-IFN-α-2a weekly or peg-INF-α-2b 1.5 μg/kg per week in combination with ribavirin 15 mg/kg per day (minimum 1000 mg daily and maximum 1400 mg daily), fixed doses of 1000 mg for patients < 75 kg and 1200 mg for patients > 75 kg with genotype 1 or 4 or flat dosing of 800 mg daily for genotypes 2 and 3 - a treatment with modest success rates, severe adverse events and variation in treatment response between genotypes[4]. Therefore, a great effort has been put into identifying biomarkers to predict rapid virological response (RVR), defined as undetectable serum HCV-RNA at week four of antiviral treatment, and sustained virological response (SVR), defined as the undetectable HCV-RNA 24 wk after discontinuing antiviral treatment. One of the most promising chemokine biomarker candidate is interferon-γ inducible protein-10 (IP-10). Both intrahepatic IP-10 mRNA and plasma levels of IP-10 are elevated in individuals with CHC[5,6], strongly indicating that intrahepatic IP-10 is the source of plasma IP-10. Several studies have suggested that pretreatment levels of IP-10 have the capability to predict RVR and SVR[6-9]. In addition, hepatic inflammation and fibrosis have been shown to correlate with IP-10 levels[10-12], and it has been proposed, that plasma levels of IP-10 can predict the risk of fibrosis progression[13]. Later years have seen the forthcoming of the new direct acting antivirals (DAA), and all current treatment recommendations for CHC patients from the European Association for the Study of the Liver contain at least one DAA[14]. The current DAAs are the NS5B polymerase inhibitor, sofosbuvir, the NS3/4A protease inhibitor simeprevir and the NS5A-replication-inhibitors daclatasvir and ledispavir or the so-called 3D regimen containing the dual NS3/4A protease inhibitors Paritaprevir/Ritonavir, the NS5A inhibitor Ombitasvir and the NS5B palm polymerase inhibitor Dasabuvir. This has yielded the possibility for treating CHC patients with interferon free, all-oral regimens, with high SVR-rates and fewer adverse events[14-18]. Despite of these great advantages, the cost of DAAs will without doubt substantially delay their introduction as standard treatment in low and middle-income countries by years to come. Moreover, even in high income countries, treatment with DAA therapy is reserved for patients with advanced liver disease, despite the fact that a majority of patients are expected to benefit from the treatment. Therefore, peg-IFN/RBV treatment still has a role to play in treatment of patients with CHC, and the need for markers that can predict successful treatment outcomes to peg-INF-α/RBV are still needed.
Several studies have independently shown an association between virological response and baseline IP-10 concentrations for CHC patients infected with genotype 1 and 4[19-21]. However, the association seems to be lacking for CHC patients, infected with HCV genotype 2 and 3[21,22]. Despite this being the case, a systematic review to address and clarify the differences in IP-10 properties, in relation to the different HCV genotypes, is missing. The aim of this systematic review was therefore to examine IP-10’s ability to predict RVR and SVR in patients with CHC genotypes 1-4 treated with peg-IFN/RBV. We succeeded in doing so, with data presented in the following.
MATERIALS AND METHODS
On initiation of this review a protocol was made and registred at the International Prospective Register of Systematic Reviews (PROSPERO) - registration number: CRD42014008736. Protocol can be found at https://www.crd.york.ac.uk/PROSPERO/.
Literature search
Using the search profiles listed in the Appendix I in the supporting information, suitable literature was identified in MEDLINE and EMBASE. The first article sorting was performed by rating the article headlines, while the second sorting was performed on abstract level. Papers passing both sorting rounds were considered for the review, and thoroughly scrutinized based on pre-defined inclusion and exclusion criteria as listed below. The initial search provided 81 articles; 34 in MEDLINE and 47 in EMBASE. After the first- and second-sorting, 14 articles remained from MEDLINE and 14 articles from EMBASE of which 10 were duplicates. One article was found by manual searching the references, bringing the total number of articles after the third sorting to 19. During the third sorting, 11 articles were excluded[6,8,22-30]. This left 8 studies for inclusion[7,9,19,21,31-34]. Overveiw of the entire sorting proces is shown in Figure 1.
Figure 1.
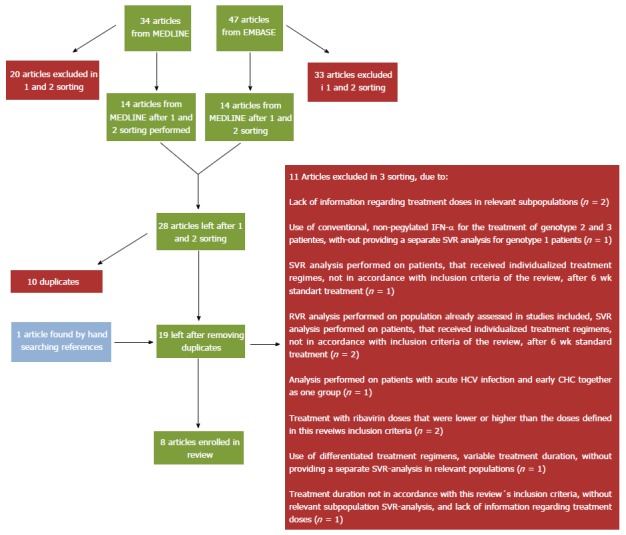
Flow chart depicting the sorting of articles. The chart depicts the number of articles found by searching the MEDLINE and EMBASE databases 04.15.2014, the number of articles excluded during the first and second sorting, the number of duplicates, the number of articles found by manual searching references, and the number of articles excluded in the third sorting, with indication of the reason for exclusion. Articles progressing down the chart from the original search to final inclusion are marked with green boxes, articles found by manual search are marked with blue boxes, and articles excluded are marked with red boxes. SVR: Sustained virological responses; RVR: Rapid virological responses; CHC: Chronic hepatitis C; HCV: Hepatitis C virus.
Inclusion criteria
Case series examining RVR or SVR in relation to 24 or 48 wk treatment with either 180 μg Peg-IFN-α-2a weekly or peg-INF-α-2b 1.5 μg/kg per week in combination with ribavirin 15 mg/kg per day (minimum 1000 mg daily and maximum 1400 mg daily) or fixed doses of 1000 mg for patients < 75 kg and 1200 mg for patients > 75 kg or flat dosing of 800 mg daily, in CHC patients infected with HCV, genotypes 1 or 4, treatment free for at least six months prior to inclusion, with both a baseline IP-10 level- and HCV-RNA determination, as well as a HCV-RNA determination four weeks after treatment initiation to assess RVR and/or 24 wk after end of treatment to assess SVR.
Case series studies examining RVR or SVR, in relation to 24 wk treatment with either 180 μg Peg-IFN-α-2a per week or peg-INF-α-2b 1.5 μg/kg per week in combination with ribavirin 800 mg daily or fixed doses of 1000 mg for patients < 75 kg and 1200 mg for patients > 75 kg, in CHC patients infected with HCV, genotypes 2 or 3, treatment free for at least six months prior to inclusion, with both a baseline IP-10 level- and HCV-RNA determination 4 wk after treatment initiation to assess RVR and/or 24 wk after end of treatment to assess SVR.
Exclusion criteria
Liver diseases other than CHC, Co-infection with human immunodeficiency virus (HIV), co-infection with hepatitis B virus (HBV), alcohol dependency (regular intake of ≥ 75 g/d), active intravenous drug-use, treatment with immunosuppressants or cytostatica and prior treatment for CHC within the last 6 mo.
Quality assessment
The quality of the 8 included articles were appraised using an 18 point checklist for case series, developed using a modified Delphi technique[35]. Each criterion can be answered with “yes”, “no” or “partially reported/unclear”, with the 18 criteria being weighted equally. In line with a pilot study conduted testing the assesment tool, we choose to rate studies with 14 or more “yes responses” as “high-quality studies”, and studies with 13 or less “yes responses” as “low-quality studies”. No studies were excluded on the basis of the criteria scores. The full checklist can be found in the Appendix II in the supporting information. Table 1 shows the sum score of the checklist. The baseline demographics regarded as important for the appraisel of the studies were: Number of patients included, patient ethnicity, patient age, male/female ratio, HCV RNA, liver enzyme level [alanine transaminase (ALT) or aspartate transaminase (AST)], body mass index (BMI), genotype, liver fibrosis stage and distribution on interleukin 28B (IL28B) single nucleotide polymorphism (SNPs).
Table 1.
Overview of the modified Delphi, 18-point quality assessment checklist for studies included in the review
| Ref. | Yes response | No response | Partiel reported/ unclear | Assessment |
| Fattovich et al[21] | 16 | 2 | 0 | High-quality |
| Diago et al[7] | 15 | 2 | 1 | High-quality |
| Apolinario et al[9] | 14 | 2 | 2 | High-quality |
| Darling et al[31] | 14 | 1 | 3 | High-quality |
| Lagging et al[34] | 14 | 3 | 1 | High-quality |
| Al-Ashgar[19] | 13 | 3 | 2 | Low-quality |
| Derbala et al[32] | 13 | 2 | 3 | Low-quality |
| Kurelac et al[33] | 12 | 3 | 3 | Low-quality |
Studies was ranked as high quality if the provided ≥ 14 “yes” answers, or low quality if they provided ≤ 13 “yes” answers.
RESULTS
Patient baseline demographic
All information was extracted from the articles, no raw data was requisitioned. Overall, presentation of baseline demographic data was missing in one study. Instead, this study provided baseline demographics in the following subpopulations: IL28 rs12979860 (CC, CT, TT), rs12980275 (AA, AG, GG), rs8099917 (TT, TG, GG)[34]. Only baseline characteristics for rs12979860 are reported in the review, as these were representative for the study population. All studies provided baseline information on total number of patients included, gender and age. Four studies failed to provide BMI[7,9,19,31], and four studies did not supply exact information regarding patient ethnicity[7,9,19,32]. Information regarding number of patients included, ethnicity, age, male/female ratio, and BMI is reported in Table 2. ALT or AST values were not reported by two studies[33,34], one of these however stated that all patients included had two serum ALT values above the upper limit of normal within 6 mo of treatment initiation[34]. Effect on liver parenchyma and HCV-RNA load are shown in Table 3. Regarding fibrosis stage, four studies used the Ishak score[7,31,33,34], two studies used the Scheuer score[9,32], and two studies used the Metavir staging system[19,21]. Overview of genotype and fibrosis stage is presented in Table 4. Information regarding treatment regimens can be found in Table 5. Four studies provided information on IL28B SNP distribution. An overview of SNPs can be seen in Table 6.
Table 2.
Baseline total patient number, number of male patients, mean age, body mass index and ethnicity for the 8 included studies
| Ref. |
Patients |
Mean age | BMI |
Ethnicity |
|||
| Males | Total (n) | (yr) | (kg/m2) | Caucasian | African American | Asian | |
| Apolinario et al[9] | 40 | 63 | 41 (± 9.3)5 | Information not provided | Information not provided6 | ||
| 1Lagging et al[34] | 169 | 2522 | 2529 | ||||
| IL28B rs12979860 CC | 64 | 93 | 41.6 (± 10.1)5 | 25.1 (± 3.6)5 | |||
| IL28B rs12979860 CT | 77 | 123 | 41.9 (± 9.5)5 | 25.0 (± 3.5)5 | |||
| IL28B rs12979860 TT | 28 | 36 | 41.9 (± 11.4)5 | 25.0 (± 3.5)5 | |||
| Diago et al[7] | 77 | 137 | 42 (± 9.7)5 | Information not provided | Information not provided | ||
| Fattovich et al[21] | 133 | 2263 | 46 (± 11)5 | 24.7 (± 3.8)5 | 226 | ||
| Kurelac et al[33] | 17 | 46 | 41.5 (± 12.4)5 | 23.7 (21.9-25)4 | 46 | ||
| Darling et al[31] | 176 | 272 | 48.4 (± 7.4)5 | Information not provided | 138 | 134 | |
| Darbala et al[32] | 144 | 159 | 46.47 (± 8.83)5 | 30.18 (± 5.05)5 | Information not provided7 | ||
| Al-Ashgar et al[19] | 41 | 64 | 38.7 (± 11.5)5 | Information not provided | Information not provided8 | ||
Study did not provide baseline characteristics for their entire population, but instead provided baseline demographics in accordance with IL-28 genotype (only baseline characteristics for rs12979860 are reported in the review, as these were representative for the study population);
253 was reported to be enrolled, however when adding the males and female patients, it sums to 252;
Only 226 out of 280 patients had serum available for iP-10 testing;
Median (25-75 percentiles);
Mean (SD);
51 patients from clinical trials had Spanish nationality;
Egyptian nationality;
Saudi nationality;
95% of the original DITTO patient population were Caucasian. BMI: Body mass index.
Table 3.
Hepatitis C virus-RNA and patient liver enzyme status for the 8 included studies
| Ref. |
HCV-RNA |
Liver enzyme level |
|||||
|
High viral load |
Low viral load |
All patients | AST | ALT | |||
| n | Limit | n | Limit | ||||
| Apolinario et al[9] | 28 | ≥ 6.3 log IU/mL5 | 35 | < 6.3 log IU/mL5 | 118 IU/L (± 64) $ | ||
| 1Lagging et al[34] | |||||||
| IL28B rs12979860 CC | 6.3 log IU/mL (± 0.8)3 | Information not provided | |||||
| IL28B rs12979860 CT | 6.1 log IU/mL (± 0.7)3 | ||||||
| IL28B rs12979860 TT | 5.9 log IU/mL (± 0.8)3 | ||||||
| Diago et al[7] | 85 | ≥ 5.7 log IU/mL5 | 52 | < 5.7 log IU/mL5 | 117.2 IU/L (± 81.6)3 | ||
| Fattovich et al[21] | 147 | ≥ 5.6 log IU/mL5 | 5.74 log IU/mL (± 0.9)35 | 92 IU/L (± 78)3 | |||
| Kurelac et al[33] | 5.55 log IU/mL (5.52-6.1)25 | Information not provided | |||||
| Darling et al[31] | 6.66 log IU/mL (± 6.76)35 | 90.9 IU/L (72.9)3 | |||||
| Darbala et al[32] | 4.95 log IU/mL (3.6-5.63)45 | 38 IU/L (27-51)4 | 51 IU/L (34-87)4 | ||||
| Al-Ashgar et al[19] | 45 | ≥ 5.78 log IU/mL | 19 | < 5.78 log IU/mL5 | 67.5 IU/L (43.5-106.8)2 | 56.0 IU/L (32.0-86.0)2 | |
Lagging et al provided baseline demographics in accordance with IL-28 genotype (only baseline characteristics for rs12979860 are reported in the review, as these were representative for the study population);
Median (25-75 percentiles);
Mean (SD);
Median (IQR);
Recalculated into log IU/mL. HCV-RNA is shown as number of patients with high or low viral load or as the mean or median for the entire population. Depending of the presentation in the original article, levels of ALT, AST or both are shown. HCV: Hepatitis C virus; ALT: Alanine transaminase; AST: Aspartate transaminase.
Table 4.
Genotype and liver fibrosis stage for the 8 included studies
| Ref. |
Genotype (n) |
Method |
Liver fibrosis stage |
|||||||||
| 1 | 2 | 3 | 4 | 0 | 1 | 2 | 3 | 4 | 5 | 6 | ||
| Apolinario et al[9] | 43 | 20 | Scheuer score | 28 | 35 | |||||||
| Lagging et al[34]4 | 1701 | 231 | 491 | 111 | Ishak score | 11 | 61 | 65 | 30 | 15 | 20 | 14 |
| IL28B rs12979860 CC | 44 | 13 | 33 | 3 | 3 | 18 | 27 | 11 | 5 | 12 | 5 | |
| IL28B rs12979860 CT | 96 | 7 | 15 | 5 | 7 | 35 | 27 | 17 | 7 | 6 | 6 | |
| IL28B rs12979860 TT | 30 | 3 | 1 | 3 | 1 | 8 | 11 | 2 | 3 | 2 | 3 | |
| Diago et al[7] | 103 | 9 | 25 | Ishak score | 106 | 31 | ||||||
| Fattovich et al[21] | 92 | 87 | 47 | Metavir2 | 121 | 21 | ||||||
| Kurelac et al[33] | 46 | Ishak | 34 | 12 | ||||||||
| Darling et al[31] | 272 | Ishak | 220 | 52 | ||||||||
| Darbala et al[32] | 159 | Scheuer score | 109 | 50 | ||||||||
| Ashgar et al[19] | 64 | Metavir | 343 | 10 3 | ||||||||
Baseline information for the sub analysis of IL28 12979860. Two hundred and fifty-two patients are reported to be enrolled, however adding the genotypes yields 253 patients. Likevise biopsies from 228 patients are described, however when adding the Ishak scores only yields 216 patients;
Biopsies only available for 142 patients;
Histology available for 44 patients;
Lagging et al provided baseline demographics in accordance with IL-28 genotype (only baseline characteristics for rs12979860 are reported in the review, as these were representative for the study population). A box stretching over two - or more genotypes or fibrosis stage, indicates that the number refers to the combined group.
Table 5.
Overview of the treatment regimens for pegylated interferon in combination with ribavirin, for the 8 studies included, in relation to dose and duration
| Ref. | Genotype | Duration | Interferon treatment | Ribavirin treatment | |
| Apolinario et al[9] | Multi-centerpatients | 1 | 48 wk | 180 μg peg-INF-α-2a once weekly | 800 mg per day or 1000 mg < 75 kg, 1200 mg > 75 kg |
| Non-1 | 24-48 wk | ||||
| Out patiens | 1 | 48 wk | peg-INF-α2b 1.5 μg/kg per week | 1000-1200 mg per day | |
| Non-1 | 24 wk | ||||
| Lagging et al[34] | 1 | 6 wk1 | 180 μg peg-INF-α-2a once weekly | 1000 mg < 75 kg, 1200 mg > 75 kg per day | |
| Diago et al[7] | 1 | 48 wk | peg-INF-α-2b 1.5 μg/kg per week or 180 μg peg-INF-α-2a/week | 1000 mg < 75 kg, 1200 mg > 75 kg per day | |
| Non-1 | 24 wk | ||||
| Fattovich et al[21] | 1 and 4 | 48 wk | peg-INF-α-2b 1.5 μg/kg per week or 180 μg peg-INF-α-2a/week | 800-1200 mg per day | |
| 2 and 3 | 24 wk | ||||
| Kurelac et al[33] | 1 | 48 wk | peg-INF-α-2b 1.5 μg/kg per week | Weight based ribavirin treatment2 | |
| Darling et al[31] | 1 | 48 wk | 180 μg peg-INF-α-2a once weekly | 1000-1200 mg per day | |
| Derbala et al[32] | 4 | 48 wk | Peg-IFN once weekly3 | 1000 mg < 75 kg, 1200 mg > 75 kg per day | |
| Al-Ashgar[19] | 4 | 48 wk | 180 μg peg-INF-α-2a once weekly | 1000 mg < 75 kg, 1200 mg > 75 kg | |
After 6 wk, patients were randomized to differentiated treatment regimes;
No further information on ribavirin treatment was provided;
No further information on the subtype of peg-IFN was provided. Apolinario et al[9] feature patients from both an outpatient clinic as well as patients from two multicenter trials receiving different treatment regimens, illustrated by the segregation in the genotype column. peg-IFN: Pegylated interferon.
Table 6.
Overview of the marker distribution, in the four studied that supplied information on interleukin 28B single nucleotide polymorphism
| Ref. | Genotype (n) |
rs12979860 |
rs12980275 |
rs8099917 |
rs11881222 |
||||||||
| CC | CT | TT | AA | AG | GG | TT | TG | GG | AA | AG | GG | ||
| Lagging et al[30] | 1 (253) | 93 | 123 | 37 | 101 | 115 | 37 | 153 | 90 | 10 | |||
| Fattovich et al[21] | 1 (92) | 33 | 44 | 15 | 33 | 45 | 14 | 49 | 38 | 5 | |||
| 2 (87) | 34 | 43 | 10 | 34 | 42 | 11 | 47 | 34 | 6 | ||||
| 3 (47) | 25 | 21 | 1 | 25 | 20 | 2 | 34 | 13 | 0 | ||||
| Darling et al[31] | 1 (201) | 63 | 103 | 44 | |||||||||
| Derbala et al[32] | 4 (159) | 57 | 77 | 25 | 96 | 55 | 8 | 64 | 75 | 20 | |||
Genotype column indicates specific genotype, and total number of patients with the specific genotype. Each marker column is divided into allelic distribution for the IL28B SNP genotype. SNP: Single nucleotide polymorphism.
Rapid virological response
An overview is presented in Table 7. Lagging et al[34] (2011) examined IP-10’s ability to predict virological response and treatment outcome in 170 patients with genotype 1, from the DITTO-HCV study group. After six weeks, patients were randomized to individualized treatment, or continued on the standard combination therapy as no sub analysis on SVR for patient receiving therapy, corresponding with the review’s inclusion criteria for the course of 24-48 wk, was provided. Only results regarding RVR are featured in the review. The study found that patients obtaining RVR had significantly lower median baseline IP-10 levels than patients without a RVR. These findings were similar to results reported by Fattovich et al[21] that patients infected with HCV, genotype 1, who achieved RVR, had a significant lower mean baseline IP-10, than those who did not. However, this association was not seen for patients infected with HCV genotype 2 or 3. The study also enrolled genotype 4 infected patients, but due to insufficient numbers (n = 15), these were excluded. Al-Ashgar et al[19], 2013 studied the relationship between IP-10 and virological response in patients infected with genotype 4, and showed a trend towards lower mean baseline IP-10 in patients with RVR, than in those without, though the association was not significant.
Table 7.
Overview of rapid virological response in the 3 studies providing information on baseline inducible protein-10’s, and hepatitis C virus RNA levels at week 4
| Ref. | Patients (n) | IP-10 measurement method | Genotype (n) |
Baseline IP-10 concentration, grouped by rapid virological response (pg/mL) |
Overall RVR (n) |
|||
| RVR | Non-RVR | P-value | RVR | Non-RVR | ||||
| Lagging et al[34] | 170 | ELISA (Quantikine, R and D systems, Minneapolis, MN, United States) | 1 (170) | 222 | 401 | P < 0.01 (median) | 33 | 137 |
| 1Fattovich et al[21] | 226 | ELISA (Quantikine, R and D systems, Minneapolis, MN, United States) | 1 (92) | 2.4 (± 0.28) | 2.6 (± 0.25) | P < 0.01 (log mean ± SD) | 172 | 108 |
| 2 (87) | 2.38 (± 0.31) | 2.3 (± 0.30) | P > 0.05 (log mean ± SD) | |||||
| 3 (47) | 2.45 (± 0.23) | 2.48 (± 0.39) | P > 0.05 (log mean ± SD) | |||||
| Al-Ashgar et al[19] | 64 | ELISA (Quantikine, R and D systems, Minneapolis, MN, United States) | 4 (64) | 483.9 (± 261.6) | 609.9 (±424.3) | P > 0.05 (mean ± SD) | 12 | 52 |
Entire patient population was 280, genotype 4 infected were removed from the analyses, and IP-10 results was available for 226 patients. IP-10: Inducible protein-10; RVR: Rapid virological response.
SVR
An overview is presented in Table 8. Following the pattern regarding RVR, all five studies examining SVR in relation to baseline IP-10 levels for HCV genotype 1 infected patients, showed a significant association.
Table 8.
Overview of sustained viral response in the 8 studies providing information on baseline inducible protein-10’s, and hepatitis C virus-RNA levels 24 wk after end-of- treatment
| Ref. | Patients (n) | IP-10 measurement method | Genotype (n) |
Baseline IP-10 concentration, grouped by sustained virological response (pg/mL) |
Overall SVR |
|||
| SVR | Non-SVR | P-value | SVR | Non-SVR | ||||
| Apolinario et al[9] | 63 | ELISA (OptEIA, Pharmingen, San Diego, CA, United States) | 1 (43) | 245 (± 154) | 381 (± 138) | P < 0.05 (mean ± SD) | 36 | 27 |
| Diago et al[7] | 137 | ELISA (Human immunoassay kit; BioSource Europe SA, Nivelles, Belgium | 1 (103) | 347 (± 197.4) | 500.6 (± 311.2) | P < 0.01 (mean ± SD) | 792 | 582 |
| 1 (103) | 332.4 (± 222.1) | 476.8 (± 305.3) | P < 0.01 (mean ± SD) | |||||
| 2 (9) | ||||||||
| 3 (25) | ||||||||
| 1Fattovich et al[21] | 226 | ELISA (Quantikine, R and D systems, Minneapolis, MN, United States ) | 1 (92) | 2.47 ± 0.23 | 2.65 ± 0.28 | P < 0.001 (log mean ± SD) | 2092 | 712 |
| 2 (87) | 2.37 ± 0.31 | 2.33 ± 0.35 | P > 0.05 (log mean ± SD) | |||||
| 3 (47) | 2.42 ± 0.21 | 2.67 ± 0.46 | P < 0.05a (log mean ± SD) | |||||
| Kurelac et al[33] | 46 | ELISA (Quantikine, R and D systems, Minneapolis, MN, United States ) | 1 (46) | 185 (63-518) | 395.5 (111-926) | P < 0.0001 (median, range) | 26 | 20 |
| Darling et al[31] | 272 | ELISA (Quantikine, R and D systems, Minneapolis, MN, United States ) | 1 (272) | 437 (± 31) | 704 (± 44) | P < 0.001 (mean ± SD) | 157 | 115 |
| Derbala et al[32] | 159 | Luminex, Cytokine multiplex immunoassay kit (Merck Millipore, Billerica, MA, United States) | 4 (159) | Exact data not provided, only graphic presentation | P < 0.001 (median, IQR) | 98 | 61 | |
| Al-Ashgar et al[19] | 64 | ELISA (Quantikine, R andD systems, Minneapolis, MN, United States ) | 4 (64) | 462 (± 282.6) | 840.4 (± 490.6) | P < 0.01 (mean ± SD) | 41 | 23 |
Entire patina population was 280, genotype 4 removed from the analyses, and IP-10 results was available for 226 patients Note that M. Derbala et al did not provide written specification on IP-10 levels for SVR compared to non-SVR, and only supplied a graphic depiction, which could not be interpreted to adequate results;
SVR for the entire population.
P = 0.02. Only the results of statistical tests with a P value < 0.01 were considered of interest, because of the multiple comparisons between subjects with and without SVR. SVR: Sustained viral response; IP-10: Inducible protein-10.
Apolinario et al[9] enrolled 63 Spanish patients from clinical trials and out patient clinics. Forty-three patients had genotype 1, while 20 had a non-1 genotype. Among the 43 HCV genotype 1 infected patients, mean baseline IP-10 levels were significantly lower in patients who reached a SVR compared to those who did not. Because some of the genotype non-1 infected patients received 48 wk of therapy, the results for these are not provided in Table 7. Diago et al[7] also found a significant association between mean baseline IP-10 and SVR for their overall population of Spanish patients. An association that remained significant, when the analysis was restricted to HCV genotype 1 infected patients. The same significant association between lower baseline IP-10 and SVR for HCV genotype 1 infected, were reported for Italian, Croatian and American patients[21,31,33]. An interesting aspect of the study by Kurelac et al[33], 2012 was, that the greatest difference in IP-10, between patients with a SVR vs non-SVR, was seen at treatment week 4, where median IP-10 levels were 185 pg/mL (63-518) and 424 pg/mL (90-815) (P < 0.0001), respectively. Darling et al[31] noted, that the significant association between baseline IP-10 levels and SVR remained when patients were grouped as Caucasian Americans (CA) or African Americans (AA) (447 ± 44 pg/mL vs 677 ± 69 pg/mL, P < 0.001 and 418 pg/mL ± 35 vs 716 pg/mL ± 55, P < 0.001, respectively). Fattovich et al[21] were the only ones that reported on HCV genotype 2 and 3 patients. As with the results regarding RVR, no association was found between SVR and baseline IP-10. Derbala et al[32] and Al-Ashgar et al[19] studied HCV genotype 4 infected Egyptian and Saudi patients, respectively, and showed significantly higher values of baseline IP-10 in non-SVRs than in SVRs. Interestingly, a sub analysis, performed by Al-Ashgar et al[19] on genotype 4a and 4d, showed that this correlation was present for genotype 4d (465.9 pg/mL ± 349.1 vs 904.9 pg/mL ± 532.1, P < 0.001), but not for genotype 4a (564.7 pg/mL ± 288.9 vs 568 pg/mL ± 384.9, P = 0.300). Derbala et al[32] failed to provide information on the exact levels of IP-10, and instead provided a graphic depiction, which could not be interpreted to adequate results.
DISCUSSION
Several studies have independently shown levels of IP-10 to be associated with both RVR and SVR to peg-IFN/RBV treatment for CHC patients infected with HCV, genotype 1 and 4, but not for genotype 2 and 3. We conducted this systematic review to assess variation in IP-10’s predictive ability for RVR and SVR to peg-INF/RBV treatment in patients chronically infected with HCV genotypes 1-4.
Our main findings indicate that a correlation exist between baseline IP-10 and SVR- and in part for RVR - for genotype 1 and possibly for genotype 4, however not for genotype 2 or 3.
Three studies provided information on baseline IP-10 in relation to RVR[19,21,34]. Studies reporting on HCV, genotype 1 infected patients, found significant lower baseline IP-10 values in patients achieving RVR compared to those who did not[21,34]. Only a trend, failing to reach significance, was described between baseline IP-10 and RVR in genotype 4 infected patients[19] and no significant relation was found in relation to genotype 2 or -3[21]. Seven studies provided information on baseline IP-10 in relation to SVR[7,9,19,21,31-33]. All five studies reporting on HCV genotype 1 infected patients[7,9,21,31,33] found significantly lower IP-10 levels of SVR than non-SVR. Diago et al[7] did not provide separate results for the group of genotype non-1 patients included, which was surprising, as three quarters of the patients were infected with HCV, genotype 1, and could very well be the reason for finding a significant association in the overall population, when all genotypes were analyzed together. In line with this, Apolinario et al[9] stated that no associations was found for their genotype non-1 group. However lacking differentiation into sub genotypes, compromise the value of information, especially as no association were found for HCV, genotype 2 or 3 infected[21], and both studies reporting on genotype 4 infected patients[19,32] found significant lower baseline IP-10 level in their populations, when comparing patients achieving SVR vs non-SVR. It should be noted, that while Fattovich et al[21] considered two-sided P-values < 0.05 as statistical significant, only results of statistical tests with a P-value < 0.01 were considered of interest, because of the multiple comparisons between subjects with and without SVR. Therefore IP-10 was not considered to be associated with SVR, for HCV genotype 3 infected individuals, even though the p-value was found to be 0.02.
One study observed that the greatest difference in IP-10 levels was found at week 4. Patients, who at this point had IP-10 levels higher than 250 pg/mL, had a 40-fold risk of not reaching SVR compared to patients with IP-10 levels lower than 250 pg/mL[33]. This might indicate, that IP-10 levels at treatment week 4, could be used to assess if peg-INF/RBV treatment should be discontinued or not in genotype 1 patients - and perhaps could also be used to evaluate the need for adjacent DAA treatment (i.e., using a 4 wk lead in phase with peg-INF/RBV treatment before apprising the need for DAAs). However, the small number of patients participating calls for caution when interpreting these results, and further studies of IP-10 levels at treatment week 4 should be encouraged.
One study[31] showed that the correlation between baseline IP-10 and SVR remained significant even when the population was grouped according to ethnicity (P < 0.001). The latter is interesting as AA ethnicity is otherwise considered an unfavorable prognostic factor for obtaining SVR[36-38], and might imply that IP-10 could help aid the decision as to whom would have the greatest potential benefit from peg-INF/RBV treatment regardless of ethnicity. In this context it is interesting that it has previously been shown that HCV infected AA had higher IP-10 levels than corresponding CA patients, while uninfected AA had IP-10 levels similar to uninfected CA[28]. The effect of race on Interferon Stimulated Genes, once at the stage of CHC, should therefore be examined further.
Findings, regarding SVR for HCV genotype 2 and 3, followed the same pattern as the results for RVR with no association between baseline IP-10 and SVR present for genotype 2 or 3[21]. Supporting our findings, this lacking correlation in patients with HCV genotype 2 and 3, has also been shown when treating patients with standard and low (90 μg once weekly) peg-INF/RBV regimens[22].
As mentioned, a significant correlation between IP-10 and SVR was reported by both studies, including HCV genotype 4 infected patients[19,32]. One of these[19] also performed differentiated analyses on HCV genotype 4 subtypes, 4a and 4d, showing a significant association only for the latter (P = 0.330 and P < 0.001, respectively). It would have been interesting to examine if this was also the case for RVR, as it could be speculated that the association between baseline IP-10 and RVR in HCV genotype 4 infected patients failed to show significance, because both subtype 4a and 4d were analyzed as a whole. Therefore, subsequent studies making RVR and SVR assessments should be encouraged to perform differential analysis on individual viral subtypes, in order to uncover more specific associations. The setup for this study, did not allow us to investigate, what specific mechanisms account for the differences in correlation between baseline IP-10 and HCV genotype 1 and 4 compared with HCV genotype 2 and 3. However it is of great interest that these differences occur, and should be investigated further. Inversely patients infected with HCV genotype 2 or 3 generally has a more favorable response to treatment with PEG-IFN and RBV. Therefore, in a clinical setting the underlying mechanism might not be relevant, as genotype 2 and 3 patients would readily be treated, whereas clinitians might be more reluctant to initiate peg-INF treatment to genotype 1 and 4 - infected individuals and here IP-10 levels might help to show which patients should undergo treatment.
This review focused on the association between pretreatment IP-10 levels and virological responses. However, IL28B SNPs should be addressed when considering IP-10, as they are strongly linked with treatment response to Peg-INF/ RBV[39-45]. Especially are homozygote genotypes at markers rs8099917 (TT), rs12979860 (CC) and rs12980275 (AA) associated with a favorable outcome to treatment. While IL28B polymorphisms were not found to be predictive for treatment response in HCV genotype 2 and 3 infected individuals by Fattovich et al[21], pretreatment IL28B polymorphisms, HCV-RNA- and IP-10 levels independently predict RVR in HCV genotype 1 infected individuals, with RVR in turn being the strongest predictor of SVR. Combining the IL28B polymorphisms and HCV-RNA yielded a specificity of 98% but a low sensitivity of 39%. By including IP-10 values in the equation, the sensitivity and the negative predictive value was raised from 81% to 94%, however lowering the positive predictive value from 87% to 76%. This is consistent with other findings in HCV genotype 1 infected, homozygous carriers of the favorable IL28B SNPs, with low IP-10 level, which also significantly predicted a first phase decline of HCV RNA, which translated into increased rates of RVR and SVR[30]. While the two latter studies was carried out solely on Caucasian patients infected with HCV genotype 1, the additive predictive effect has also been shown for both HCV genotype 1 infected AA and CA patients[31], and HCV genotype 4 infected patients[32], respectively. Although low in numbers, these results could indicate, that both variables should be considered in a clinical context, before initiating treatment with Peg-INF/RBV in patients infected with HCV genotype 1 or 4. Further studies examining the association in HCV genotype 2 and 3 infected patients should be encouraged.
Conducting a systematic review with clear and stringent in- and exclusions criteria, is an obvious strength of this study, ensuring homogeneity between the studies included, hereby allowing an unbiased assessment of the current evidence. Another strength of our study was that we assessed the quality of the studies included, and provided a detailed declaration of the studies aim, method - including treatment regimens and duration, as well as baseline patient demographics for the individual studies - supplying a solid ground for interpreting the results put forth. Although some authors recommend the use of quality assesments, other consider them misleading[46], and there remains uncertainties about the relationship between methodology, validity and the use of sum scores to judge the quality of studies[47]. Therefore we chose not to exclude any articles based on their quality score (e.g., high quality or low quality), but instead presented the ratings of the studies in the review to serve as an objective guide to interpret the review’s results, rather than a tool for selecting studies for the review. As seen by the exclusion criteria, we wished to eliminate the possible uncertainties that could arise by including studies treating HIV/HCV - or HBV/HCV co-infected patients. Therefore, it should be mentioned that even though there was no indication towards inclusion of co-infected patients, three of the included studies, based in the United States, Croatia and Egypt, contained no clear exclusion criteria for HIV- or HBV- infection[31-33].
Only a limited number of articles fulfilled the in- and exclusion criteria to be assessed in this review. Hence, more work is needed to establish a sufficient ground for final conclusions to be made. Further, there was an overweight of studies that addressed the association between SVR and baseline IP-10 in CHC patients infected with HCV genotype 1, whereas there was only a small fraction addressing the association between SVR and baseline IP-10 for genotype 2, 3 and 4, as well as studies examining the relationship between RVR and baseline IP-10 constituting an insufficient base for assessing baseline IP-10’s predictive ability in these regards.
In this systematic review, we found correlations between baseline IP-10 levels and SVR in patients chronically infected with HCV genotype 1 and 4, while no such association was found for patients infected with HCV genotype 2 or 3. Likewise, we found indications of a possible correlation between baseline IP-10 and RVR for HCV genotype 1 infected patients, while no such association were found for HCV genotype 2 or 3 patients, and only a trend was found for HCV genotype 4 infected patients. However, the amount of information regarding baseline RVR for genotypes 1-4, and SVR’s relation with baseline IP-10 for genotypes 2, 3 and 4 were insufficient for final conclusions.
COMMENTS
Background
Until recently, the standard of care for chronic hepatitis C (CHC) patients was lengthy dual therapy with pegylated interferon plus ribavirin (peg-IFN/RBV), a treatment with modest success rates, severe adverse events and variation in treatment response between hepatitis C virus (HCV) genotypes. Therefore, efforts to identifying biomarkers that can predict virological responses to treatment have been made. Interferon-γ inducible protein-10 (IP-10) is one such promising marker, with several studies independently showing an association between virological response and baseline IP-10 concentrations for CHC patients infected with HCV genotype 1 and 4. However, the association seems to be lacking for CHC patients, infected with HCV genotype 2 and 3.
Research frontiers
IP-10 has been shown to be expressed at higher levels in HCV genotype 1 infected CHC patients with moderate to severe fibrosis compered to patients with mild or non fibrosis. Therefore, studies are being made to examine if this correlation is also found in HCV genotype 2 and 3 infected CHC patients. In addition to this, examinations of baseline IP-10 ability to predict fibrosis progression in CHC patients are pending. IP-10 research in relation to CHC is therefore expanding from the possible correlation between virological response to treatment with peg-INF/RBV at baseline, to also include fibrosis score at baseline and fibrosis progress over time.
Innovations and breakthroughs
Despite the work done so far to correlate IP-10 levels to treatment response, this is to our knowledge, the fist systematic review to address and clarify the differences in IP-10 properties, in relation to the different HCV genotypes and virological response. The authors found indications of correlations between baseline IP-10 levels and SVR in CHC patients infected with HCV genotype 1 and 4, but not in patients infected with HCV genotype 2 or 3. Likewise, the authors found indications of a possible correlation between baseline IP-10 and RVR for HCV genotype 1 infected patients, while no such association were found for HCV genotype 2 or 3 patients, and only a trend was found for HCV genotype 4 infected patients.
Applications
Despite of the great advantages with the new treatment options with direct acting antivirals (DAA), the cost of DAAs will without doubt substantially delay their introduction as standard treatment in low and middle-income countries by years to come. In addition, DAA in high-income countries is still reserved for patients with advanced liver disease. Therefore, peg-IFN/RBV treatment still has a role to play in treatment of patients with CHC. Their findings of a possible correlation between baseline IP-10 levels and SVR in CHC patients infected with HCV genotype 1 and 4 but not for genotypes 2 and 3 could be beneficial in a clinical setting. Genotype 2 and 3 patients would readily be treated, as these patients generally have a favorable outcome to peg-IFN/RBV compared to genotype 1 and 4 infected individuals. In such patients, IP-10 levels might help to show which patients would have the best prognosis for a positive outcome to treatment.
Terminology
Interferon-γ inducible protein-10, more commonly denoted IP-10 or CXCL10, is a non-ELR-CXC chemokine, binding to the CXC-receptor-3. It functions as a chemotactic, attracting T lymphocytes and NK cells to the site of inflammation. Within the liver, IP-10 mRNA is produced by hepatocytes in inflammatory areas, and both intrahepatic IP-10 mRNA - and plasma levels of IP-10 are elevated in individuals with CHC, indicating that intrahepatic IP-10 is the source of plasma IP-10. The hypothesis therefore is that IP-10 can function as proxy for the level of liver inflammation, which in turns lead to fibrosis formation.
Peer-review
This is a well written and comprehensive systemic review to explore the association between baseline levels of interferon-γ-inducible protein-10 and virological response to treatment with pegylated interferon and ribavirin among patients chronically infected with hepatitis C virus, genotype 1-4.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Denmark
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: Ruhwald M is registered as inventor on a patent application disclosing IP-10 based liver fibrosis monitoring, using DBS, which could be viewed as a conflict-of-interest. Otherwise all the authors declare that they have no competing interests.
Data sharing statement: The technical appendix, and dataset are available from the corresponding author at nina.weis@regionh.dk.
Peer-review started: October 28, 2016
First decision: December 1, 2016
Article in press: January 18, 2017
P- Reviewer: Balsano C, Bock CT, Chiu KW S- Editor: Ji FF L- Editor: A E- Editor: Li D
References
- 1.WHO. 2014. Fact Sheet number 164, Hepatitis C. Available from: http://www.who.int/mediacentre/factsheets/fs164/en/ [Google Scholar]
- 2.Poynard T, Ratziu V, Charlotte F, Goodman Z, McHutchison J, Albrecht J. Rates and risk factors of liver fibrosis progression in patients with chronic hepatitis c. J Hepatol. 2001;34:730–739. doi: 10.1016/s0168-8278(00)00097-0. [DOI] [PubMed] [Google Scholar]
- 3.Ghany MG, Kleiner DE, Alter H, Doo E, Khokar F, Promrat K, Herion D, Park Y, Liang TJ, Hoofnagle JH. Progression of fibrosis in chronic hepatitis C. Gastroenterology. 2003;124:97–104. doi: 10.1053/gast.2003.50018. [DOI] [PubMed] [Google Scholar]
- 4.Smith DB, Bukh J, Kuiken C, Muerhoff AS, Rice CM, Stapleton JT, Simmonds P. Expanded classification of hepatitis C virus into 7 genotypes and 67 subtypes: updated criteria and genotype assignment web resource. Hepatology. 2014;59:318–327. doi: 10.1002/hep.26744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeremski M, Petrovic LM, Talal AH. The role of chemokines as inflammatory mediators in chronic hepatitis C virus infection. J Viral Hepat. 2007;14:675–687. doi: 10.1111/j.1365-2893.2006.00838.x. [DOI] [PubMed] [Google Scholar]
- 6.Askarieh G, Alsiö A, Pugnale P, Negro F, Ferrari C, Neumann AU, Pawlotsky JM, Schalm SW, Zeuzem S, Norkrans G, et al. Systemic and intrahepatic interferon-gamma-inducible protein 10 kDa predicts the first-phase decline in hepatitis C virus RNA and overall viral response to therapy in chronic hepatitis C. Hepatology. 2010;51:1523–1530. doi: 10.1002/hep.23509. [DOI] [PubMed] [Google Scholar]
- 7.Diago M, Castellano G, García-Samaniego J, Pérez C, Fernández I, Romero M, Iacono OL, García-Monzón C. Association of pretreatment serum interferon gamma inducible protein 10 levels with sustained virological response to peginterferon plus ribavirin therapy in genotype 1 infected patients with chronic hepatitis C. Gut. 2006;55:374–379. doi: 10.1136/gut.2005.074062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romero AI, Lagging M, Westin J, Dhillon AP, Dustin LB, Pawlotsky JM, Neumann AU, Ferrari C, Missale G, Haagmans BL, et al. Interferon (IFN)-gamma-inducible protein-10: association with histological results, viral kinetics, and outcome during treatment with pegylated IFN-alpha 2a and ribavirin for chronic hepatitis C virus infection. J Infect Dis. 2006;194:895–903. doi: 10.1086/507307. [DOI] [PubMed] [Google Scholar]
- 9.Apolinario A, Diago M, Lo Iacono O, Lorente R, Pérez C, Majano PL, Clemente G, García-Monzón C. Increased circulating and intrahepatic T-cell-specific chemokines in chronic hepatitis C: relationship with the type of virological response to peginterferon plus ribavirin combination therapy. Aliment Pharmacol Ther. 2004;19:551–562. doi: 10.1111/j.1365-2036.2004.01872.x. [DOI] [PubMed] [Google Scholar]
- 10.Zeremski M, Dimova R, Brown Q, Jacobson IM, Markatou M, Talal AH. Peripheral CXCR3-associated chemokines as biomarkers of fibrosis in chronic hepatitis C virus infection. J Infect Dis. 2009;200:1774–1780. doi: 10.1086/646614. [DOI] [PubMed] [Google Scholar]
- 11.Harvey CE, Post JJ, Palladinetti P, Freeman AJ, Ffrench RA, Kumar RK, Marinos G, Lloyd AR. Expression of the chemokine IP-10 (CXCL10) by hepatocytes in chronic hepatitis C virus infection correlates with histological severity and lobular inflammation. J Leukoc Biol. 2003;74:360–369. doi: 10.1189/jlb.0303093. [DOI] [PubMed] [Google Scholar]
- 12.You CR, Park SH, Jeong SW, Woo HY, Bae SH, Choi JY, Sung YC, Yoon SK. Serum IP-10 Levels Correlate with the Severity of Liver Histopathology in Patients Infected with Genotype-1 HCV. Gut Liver. 2011;5:506–512. doi: 10.5009/gnl.2011.5.4.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zeremski M, Dimova R, Astemborski J, Thomas DL, Talal AH. CXCL9 and CXCL10 chemokines as predictors of liver fibrosis in a cohort of primarily African-American injection drug users with chronic hepatitis C. J Infect Dis. 2011;204:832–836. doi: 10.1093/infdis/jir424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.EASL Recommendations on Treatment of Hepatitis C 2015. J Hepatol. 2015;63:199–236. doi: 10.1016/j.jhep.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 15.Gane EJ, Stedman CA, Hyland RH, Ding X, Svarovskaia E, Symonds WT, Hindes RG, Berrey MM. Nucleotide polymerase inhibitor sofosbuvir plus ribavirin for hepatitis C. N Engl J Med. 2013;368:34–44. doi: 10.1056/NEJMoa1208953. [DOI] [PubMed] [Google Scholar]
- 16.Lawitz E, Mangia A, Wyles D, Rodriguez-Torres M, Hassanein T, Gordon SC, Schultz M, Davis MN, Kayali Z, Reddy KR, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med. 2013;368:1878–1887. doi: 10.1056/NEJMoa1214853. [DOI] [PubMed] [Google Scholar]
- 17.Osinusi A, Meissner EG, Lee YJ, Bon D, Heytens L, Nelson A, Sneller M, Kohli A, Barrett L, Proschan M, et al. Sofosbuvir and ribavirin for hepatitis C genotype 1 in patients with unfavorable treatment characteristics: a randomized clinical trial. JAMA. 2013;310:804–811. doi: 10.1001/jama.2013.109309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sulkowski MS, Gardiner DF, Rodriguez-Torres M, Reddy KR, Hassanein T, Jacobson I, Lawitz E, Lok AS, Hinestrosa F, Thuluvath PJ, et al. Daclatasvir plus sofosbuvir for previously treated or untreated chronic HCV infection. N Engl J Med. 2014;370:211–221. doi: 10.1056/NEJMoa1306218. [DOI] [PubMed] [Google Scholar]
- 19.Al-Ashgar HI, Khan MQ, Helmy A, Al-Thawadi S, Al-Ahdal MN, Khalaf N, Al-Qahtani A, Sanai FM. Relationship of interferon-γ-inducible protein-10 kDa with viral response in patients with various heterogeneities of hepatitis C virus genotype-4. Eur J Gastroenterol Hepatol. 2013;25:404–410. doi: 10.1097/MEG.0b013e32835bc2cf. [DOI] [PubMed] [Google Scholar]
- 20.Apolinario A, Majano PL, Alvarez-Pérez E, Saez A, Lozano C, Vargas J, García-Monzón C. Increased expression of T cell chemokines and their receptors in chronic hepatitis C: relationship with the histological activity of liver disease. Am J Gastroenterol. 2002;97:2861–2870. doi: 10.1111/j.1572-0241.2002.07054.x. [DOI] [PubMed] [Google Scholar]
- 21.Fattovich G, Covolo L, Bibert S, Askarieh G, Lagging M, Clément S, Malerba G, Pasino M, Guido M, Puoti M, et al. IL28B polymorphisms, IP-10 and viral load predict virological response to therapy in chronic hepatitis C. Aliment Pharmacol Ther. 2011;33:1162–1172. doi: 10.1111/j.1365-2036.2011.04635.x. [DOI] [PubMed] [Google Scholar]
- 22.Rotman Y, Borg BB, Soza A, Feld JJ, Modi AA, Loomba R, Lutchman G, Rivera E, Doo E, Ghany MG, et al. Low- and standard-dose peginterferon alfa-2a for chronic hepatitis C, genotype 2 or 3: efficacy, tolerability, viral kinetics and cytokine response. Aliment Pharmacol Ther. 2010;31:1018–1027. doi: 10.1111/j.1365-2036.2010.04263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yoneda S, Umemura T, Joshita S, Ichijo T, Matsumoto A, Yoshizawa K, Katsuyama Y, Ota M, Tanaka E. Serum chemokine levels are associated with the outcome of pegylated interferon and ribavirin therapy in patients with chronic hepatitis C. Hepatol Res. 2011;41:587–593. doi: 10.1111/j.1872-034X.2011.00802.x. [DOI] [PubMed] [Google Scholar]
- 24.Nikolova NS, Antonov K, Jelev D, Mateva L, Krastev Z. The Cytokine Ip-10 in Chronic Hbv and Hcv Infection. J of IMAB. 2013;19:442–447. [Google Scholar]
- 25.Moura AS, Carmo RA, Teixeira AL, Teixeira MM, Rocha MO. Soluble inflammatory markers as predictors of virological response in patients with chronic hepatitis C virus infection treated with interferon-α plus ribavirin. Mem Inst Oswaldo Cruz. 2011;106:38–43. doi: 10.1590/s0074-02762011000100006. [DOI] [PubMed] [Google Scholar]
- 26.Lee S, Varano J, Flexman JP, Cheng W, Watson MW, Rossi E, Adams LA, Bulsara M, Price P. Decreased IP-10 and elevated TGFbeta1 levels are associated with viral clearance following therapy in patients with hepatitis C virus. Dis Markers. 2010;28:273–280. doi: 10.3233/DMA-2010-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feld JJ, Grebely J, Matthews GV, Applegate T, Hellard M, Sherker A, Cherepanov V, Petoumenos K, Yeung B, Kaldor JM, et al. Plasma interferon-gamma-inducible protein-10 levels are associated with early, but not sustained virological response during treatment of acute or early chronic HCV infection. PLoS One. 2013;8:e80003. doi: 10.1371/journal.pone.0080003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Butera D, Marukian S, Iwamaye AE, Hembrador E, Chambers TJ, Di Bisceglie AM, Charles ED, Talal AH, Jacobson IM, Rice CM, et al. Plasma chemokine levels correlate with the outcome of antiviral therapy in patients with hepatitis C. Blood. 2005;106:1175–1182. doi: 10.1182/blood-2005-01-0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Casrouge A, Decalf J, Ahloulay M, Lababidi C, Mansour H, Vallet-Pichard A, Mallet V, Mottez E, Mapes J, Fontanet A, et al. Evidence for an antagonist form of the chemokine CXCL10 in patients chronically infected with HCV. J Clin Invest. 2011;121:308–317. doi: 10.1172/JCI40594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lagging M, Romero AI, Westin J, Norkrans G, Dhillon AP, Pawlotsky JM, Zeuzem S, von Wagner M, Negro F, Schalm SW, et al. IP-10 predicts viral response and therapeutic outcome in difficult-to-treat patients with HCV genotype 1 infection. Hepatology. 2006;44:1617–1625. doi: 10.1002/hep.21407. [DOI] [PubMed] [Google Scholar]
- 31.Darling JM, Aerssens J, Fanning G, McHutchison JG, Goldstein DB, Thompson AJ, Shianna KV, Afdhal NH, Hudson ML, Howell CD, et al. Quantitation of pretreatment serum interferon-γ-inducible protein-10 improves the predictive value of an IL28B gene polymorphism for hepatitis C treatment response. Hepatology. 2011;53:14–22. doi: 10.1002/hep.24056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Derbala M, Rizk NM, Al-Kaabi S, John A, Sharma M, El-dweik N, Yakoob R, Pasic F, Almohanadi M, Alejji K, et al. The predictive value of IL28B rs12979860, rs11881222 and rs8099917 polymorphisms and IP-10 in the therapeutic response of Egyptian genotype 4 patients. Virology. 2013;444:292–300. doi: 10.1016/j.virol.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 33.Kurelac I, Lepej SZ, Grlgic I, Gorenec L, Papic N, Dusek D, Barsic B, Vince A. Chemokine CXCL10 at week 4 of treatment predicts sustained virological response in patients with chronic hepatitis C. J Interferon Cytokine Res. 2012;32:386–391. doi: 10.1089/jir.2012.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lagging M, Askarieh G, Negro F, Bibert S, Söderholm J, Westin J, Lindh M, Romero A, Missale G, Ferrari C, et al. Response prediction in chronic hepatitis C by assessment of IP-10 and IL28B-related single nucleotide polymorphisms. PLoS One. 2011;6:e17232. doi: 10.1371/journal.pone.0017232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moga C, Guo B, Schopflocher D, Harstall C. 2012. Development of a quality appraisal tool for case series studies using a modified Delphi technique. [Methodology Paper] Available from: http://www.ihe.ca/advanced-search/development-of-a-quality-appraisal-tool-for-case-series-studies-using-a-modified-delphi-technique. [Google Scholar]
- 36.Muir AJ, Bornstein JD, Killenberg PG. Peginterferon alfa-2b and ribavirin for the treatment of chronic hepatitis C in blacks and non-Hispanic whites. N Engl J Med. 2004;350:2265–2271. doi: 10.1056/NEJMoa032502. [DOI] [PubMed] [Google Scholar]
- 37.Jeffers LJ, Cassidy W, Howell CD, Hu S, Reddy KR. Peginterferon alfa-2a (40 kd) and ribavirin for black American patients with chronic HCV genotype 1. Hepatology. 2004;39:1702–1708. doi: 10.1002/hep.20212. [DOI] [PubMed] [Google Scholar]
- 38.De Maria N, Colantoni A, Idilman R, Friedlander L, Harig J, Van Thiel DH. Impaired response to high-dose interferon treatment in African-Americans with chronic hepatitis C. Hepatogastroenterology. 2002;49:788–792. [PubMed] [Google Scholar]
- 39.Ge D, Fellay J, Thompson AJ, Simon JS, Shianna KV, Urban TJ, Heinzen EL, Qiu P, Bertelsen AH, Muir AJ, et al. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature. 2009;461:399–401. doi: 10.1038/nature08309. [DOI] [PubMed] [Google Scholar]
- 40.Mangia A, Thompson AJ, Santoro R, Piazzolla V, Tillmann HL, Patel K, Shianna KV, Mottola L, Petruzzellis D, Bacca D, et al. An IL28B polymorphism determines treatment response of hepatitis C virus genotype 2 or 3 patients who do not achieve a rapid virologic response. Gastroenterology. 2010;139:821–827, 827.e1. doi: 10.1053/j.gastro.2010.05.079. [DOI] [PubMed] [Google Scholar]
- 41.McCarthy JJ, Li JH, Thompson A, Suchindran S, Lao XQ, Patel K, Tillmann HL, Muir AJ, McHutchison JG. Replicated association between an IL28B gene variant and a sustained response to pegylated interferon and ribavirin. Gastroenterology. 2010;138:2307–2314. doi: 10.1053/j.gastro.2010.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rauch A, Kutalik Z, Descombes P, Cai T, Di Iulio J, Mueller T, Bochud M, Battegay M, Bernasconi E, Borovicka J, et al. Genetic variation in IL28B is associated with chronic hepatitis C and treatment failure: a genome-wide association study. Gastroenterology. 2010;138:1338–1345, 1345.e1-7. doi: 10.1053/j.gastro.2009.12.056. [DOI] [PubMed] [Google Scholar]
- 43.Suppiah V, Moldovan M, Ahlenstiel G, Berg T, Weltman M, Abate ML, Bassendine M, Spengler U, Dore GJ, Powell E, et al. IL28B is associated with response to chronic hepatitis C interferon-alpha and ribavirin therapy. Nat Genet. 2009;41:1100–1104. doi: 10.1038/ng.447. [DOI] [PubMed] [Google Scholar]
- 44.Tanaka Y, Nishida N, Sugiyama M, Kurosaki M, Matsuura K, Sakamoto N, Nakagawa M, Korenaga M, Hino K, Hige S, et al. Genome-wide association of IL28B with response to pegylated interferon-alpha and ribavirin therapy for chronic hepatitis C. Nat Genet. 2009;41:1105–1109. doi: 10.1038/ng.449. [DOI] [PubMed] [Google Scholar]
- 45.Thompson AJ, Muir AJ, Sulkowski MS, Ge D, Fellay J, Shianna KV, Urban T, Afdhal NH, Jacobson IM, Esteban R, et al. Interleukin-28B polymorphism improves viral kinetics and is the strongest pretreatment predictor of sustained virologic response in genotype 1 hepatitis C virus. Gastroenterology. 2010;139:120–9.e18. doi: 10.1053/j.gastro.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 46.Stein K, Dalziel K, Garside R, Castelnuovo E, Round A. Association between methodological characteristics and outcome in health technology assessments which included case series. Int J Technol Assess Health Care. 2005;21:277–287. doi: 10.1017/s0266462305050373. [DOI] [PubMed] [Google Scholar]
- 47.Saunders LD, Soomro GM, Buckingham J, Jamtvedt G, Raina P. Assessing the methodological quality of nonrandomized intervention studies. West J Nurs Res. 2003;25:223–237. doi: 10.1177/0193945902250039. [DOI] [PubMed] [Google Scholar]


