Summary
Objective
To report on any adverse effects on health and wellbeing of working as a doctor, as described by senior doctors.
Design
Questionnaires sent in 2014 to all medical graduates of 1974 and 1977.
Participants
3695 UK medical graduates.
Setting
United Kingdom.
Main outcome measures
Statements about adverse effects upon health, wellbeing and career.
Results
The aggregated response rate from contactable doctors was 84.6% (3695/4369). In response to the question ‘Do you feel that working as a doctor has had any adverse effects on your own health or wellbeing?’, 44% of doctors answered ‘yes’. More GPs (47%) than hospital doctors (42%) specified that this was the case. Three-quarters of doctors who answered ‘yes’ cited ‘stress/work–life balance/workload’ as an adverse effect, and 45% mentioned illness.
In response to the statement ‘The NHS of today is a good employer when doctors become ill themselves’, 28% of doctors agreed, 29% neither agreed nor disagreed and 43% disagreed. More women doctors (49%) than men doctors (40%) disagreed with this statement. More general practitioners (49%) disagreed than hospital doctors (37%).
Conclusions
Chronic stress and illness, which these doctors attributed to their work, were widely reported. Although recent changes may have alleviated some of these issues, there are lessons for the present and future if the NHS is to ensure that its medical workforce receives the support which enables current doctors to enjoy a full and satisfying career and to contribute fully to health service provision in the UK. Older doctors, in particular, need support to be able to continue successfully in their careers.
Keywords: Medical careers, non-clinical, workforce, physicians, career choice
Introduction
Stress, burnout and vulnerability to ill health are commonplace among doctors.1–4 These conditions are compounded by an unwillingness to take time off from work when needed, a tendency to self-prescribe and a reluctance to see a General Practitioner (GP).5–8 In the UK, there has been an increase in self-referrals for mental health issues9 and recorded sickness levels are under-reported when compared to self-reported measures.10 Much of the focus has been upon medical students and junior doctors.1,7,11–14 However, studies which have included more senior doctors have also found rising levels of stress and ill health, a perceived lack of cover when ill creating a pressure to stay at work and poor levels of support for doctors with chronic illness.8,15,16
In 2013, the UK’s National Health Service (NHS) outlined a number of pledges to its staff which go beyond an employee’s legal rights.17 Among these, it pledged to ‘provide support and opportunities for staff to maintain their health, wellbeing and safety’ (p. 13). A recent NHS staff survey found that 60% of staff worked unpaid overtime, one-third reported stress and 63% reported working while being unwell.18 A large national initiative to improve the health and wellbeing of NHS staff was recently announced.19
We have surveyed senior UK-trained doctors. The aim of this paper is to report their self-described adverse effects upon health, wellbeing and career. We report whether doctors feel that working as a doctor has had any adverse effects on their own health or wellbeing, and whether doctors believe that the NHS is a good employer when doctors themselves become ill. We compared the replies of men and women, of those working in different specialties and of retired and working doctors.
Methods
The UK Medical Careers Research Group surveyed the UK medical graduates of 1974 and 1977 and asked them about a wide range of issues relating to their professional work. We sent questionnaires by post and email to these senior doctors in 2014. Up to four reminders were sent to non-respondents. Further details of the methodology are available elsewhere.20
As part of a wider range of questions about career plans, views on retirement and training, senior doctors were asked to rate a number of statements (and answer some questions) about their health and wellbeing. The doctors were asked ‘Do you feel that working as a doctor has had any adverse effects on your own health or wellbeing?’ Doctors could choose from ‘Yes’, ‘No’ or ‘Prefer not to answer’. Those doctors who replied ‘Yes’ were asked to provide text comments to ‘describe the adverse effects on your health or wellbeing’. Two researchers read these comments and developed a coding scheme which contained seven themes. Each comment was allocated up to three themes. The researchers coded independently and then discussed any areas of disagreement. The coded comments were then analysed quantitatively using statistic software developed by SPSS.
The doctors were presented with the statement ‘The NHS of today is a good employer when doctors become ill themselves’ and were asked to give the extent to which they agreed with the statement, using a five-point scale covering ‘strongly agree’, ‘agree’, ‘neither agree nor disagree’, ‘disagree’ and ‘strongly disagree’, plus a ‘don’t know’ option). For ease of analysis, we aggregated to a three-point scale (with ‘strongly agree’ and ‘agree’ combined and ‘strongly disagree’ combined with ‘disagree’).
We were interested in variation in agreement or disagreement about health and wellbeing by gender, by retirement status (whether the doctor had retired, retired and ‘returned’ for some medical work, was working full-time in medicine, or part-time in medicine) and by career specialty. Each doctor’s career specialty was assigned using a combination of information provided by the doctor in this priority order: specialist register listing with the General Medical Council in 2014, first consultant specialty appointment, first non-consultant career grade specialty appointment, year first appointed as a GP principal, and examination of job history. Respondents were then grouped for analysis into four groups: hospital medical specialties, surgical specialties, general practice/family medicine (GP), and other hospital-based specialties combined (paediatrics, emergency medicine, obstetrics and gynaecology, anaesthetics, radiology, clinical oncology, pathology, and psychiatry).
The quantitative data were analysed by univariable crosstabulation. To test statistical significance we used χ2 statistics (reporting Yates’s continuity correction where appropriate). We used binary logistic regression to analyse the effect of factors in combination. Variables which were significant as single variables were included in the regression model. Respondents were grouped according to cohort (1974, 1977), gender, specialty (four groups as above), and retirement status (retired and not now working in medicine, retired and ‘returned’ for some medical work, working full-time in medicine, and working part-time in medicine).
Results
Response rates
In 1974 and 1977, respectively, 2347 and 3135 doctors graduated in the UK. Of these 5482 doctors, 4369 were contactable by us in 2014. The aggregated response rate from them, over both surveys, was 84.6% (3695/4369). Of the 3695 survey responses, 98 completed a short version of the questionnaire which did not include any questions about health and wellbeing: these are excluded from the rest of this paper, leaving 3597 full respondents. In all analyses we excluded doctors working outside of medicine and those who did not give details of their employment. This reduced the sample size to 3550 doctors. Appendix 1 contains further information about the cohort and the doctors included in analyses.
Adverse effects on health or wellbeing (univariable analysis)
The doctors were asked ‘Do you feel that working as a doctor has had any adverse effects on your own health or wellbeing?’ 44% of doctors answered ‘yes’ (Table 1). There was no difference between male and female doctors in this respect (χ22 = 1.4, p = 0.24). More GPs (47%) answered yes than doctors from the hospital medical specialties (35%) and surgery (38%) (χ23 = 25.1, p < 0.001). More doctors from the 1977 cohort (48%) said yes than doctors from the 1974 cohort (39%) (χ21 = 26.3, p < 0.001). Doctors who were retired were more likely than other doctors to say yes (χ23 = 14.9, p < 0.01). We examined differences between the specialties that make up the ‘other hospital-based’ specialties and there were no significant differences between them (χ27 = 8.3, p = 0.307).
Table 1.
Predictors of ‘Do you feel that working as a doctor has had any adverse effects on your own health or wellbeing?’ by cohort year, gender, specialty, and retirement status (numbers and percentages of doctors who replied ‘yes’).
| Univariable analysis |
Multivariable analysis |
|||||
|---|---|---|---|---|---|---|
| Group | Agreement (%) (n/N) | df | χ2 | p | OR (95% CI) | p |
| All | 44.4 (1411/3176) | |||||
| Cohort | 1 | 26.3 | <0.001 | |||
| 1977* | 48.3 (895/1854) | 1 | ||||
| 1974 | 39.0 (516/1322) | 0.7 (0.6, 0.8) | <0.001 | |||
| Gender | 1 | 1.4 | 0.236 | |||
| Men† | 43.7 (971/2221) | – | – | |||
| Women† | 46.1 (440/955) | – | – | |||
| Specialty | 3 | 25.1 | <0.001 | |||
| GP* | 46.9 (725/1547) | 1 | ||||
| Hospital medical specialties | 34.9 (137/392) | 0.7 (0.5, 0.8) | <0.001 | |||
| Surgery | 38.2 (125/327) | 0.7 (0.6, 1.0) | 0.020 | |||
| Other hospital | 46.6 (424/910) | 1.0 (0.8, 1.2) | 0.962 | |||
| Retirement status | 3 | 14.9 | <0.01 | |||
| Retired, not now working in medicine* | 46.5 (655/1408) | 1 | ||||
| Retired, and 'returned' for some medical work | 46.6 (399/856) | 1.0 (0.8, 1.2) | 0.947 | |||
| Working full-time in medicine | 38.4 (223/580) | 0.7 (0.6, 0.9) | 0.002 | |||
| Working part-time in medicine | 40.4 (134/332) | 0.7 (0.6, 1.0) | 0.020 | |||
*Reference group for multivariable model.
†Gender was not significant univariably and so was excluded from the model.
Note: ‘Univariable’ denotes single factor χ2 test for each predictor. ‘Multivariable’ denotes binomial logistic regression result for each predictor with all other predictors in the model. A total of 3358 of 3550 doctors (Appendix 1) answered the question. We excluded cases where one or more predictors were missing, or where the dependent variable was missing, which reduced the sample size to 3176.
The odds ratio (OR) indicates whether a (randomly chosen) member of the group in question was more, or less, likely than a member of the reference group to agree with the statement. For example, a doctor who was ‘Working full-time in medicine’ would be 0.7 times as likely as a doctor who was ‘Retired, not now working in medicine’ to agree with the statement.
Adverse effects on health or wellbeing (multivariable analysis)
A binary logistic regression model was fitted with cohort, specialty group, and retirement status as predictors (Table 1). In the multivariable model, all characteristics which were found to be significant in the univariable analysis remained significant. Odds ratios and 95% confidence intervals are shown in Table 1.
Adverse effects on health or wellbeing (text answers)
Of the 1475 doctors who replied that, ‘yes’, they felt that working as a doctor had had adverse effects on their health or wellbeing, 1380 doctors went on to further describe the adverse effects upon their health or wellbeing.
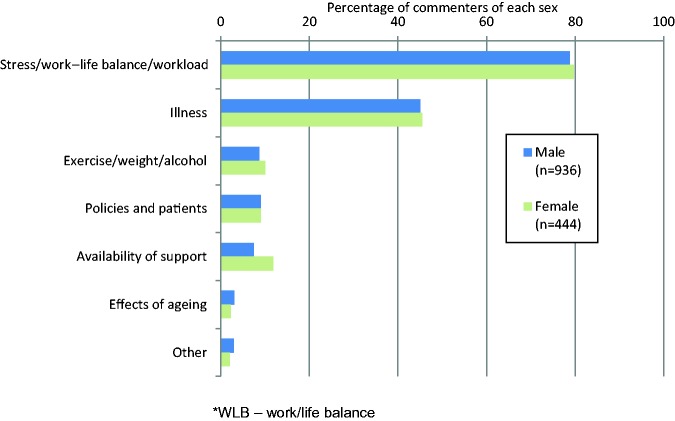
Seven themes, as grouped by us, emerged from the doctors’ comments to this question: ‘Stress/work–life balance/workload’, ‘Illness’, ‘Exercise/weight/alcohol’, ‘Policies/patients’, ‘Availability of support’, ‘Effects of ageing’, and ‘Other’. Stress/work–life balance/workload was raised by 79.1% of commenters, Illness was raised by 45.2%, Exercise/weight/alcohol by 9.2%, Policies/patients by 9.1%, Availability of support by 8.9%, and Effects of ageing by 2.8% (Figure 1).
Figure 1.
Adverse effects on health or wellbeing.
The emphasis in our questionnaire was on the adverse effects of working as a doctor on the doctor’s own health and wellbeing, and not on the consequences, if any, for patient care. However, a small number of doctors added that there had been an adverse effect on their work and on the quality of patient care. Typical comments are shown in Box 1.
Box 1.
Adverse effects of working as a doctor upon patient care: some comments.
| I found the continuing long hours, despite working part time, caused continual tiredness and exhaustion and I was concerned that this would affect my competence (female, General Practice). |
| Trying to do more work than could safely be done in the time available was very stressful. The public and government now expect perfection. The threat of litigation was very wearing (male, General Practice). |
| Towards the end of my career I felt increasingly stressed, the pressures of acute work were partly responsible, but also the increasing burden of management and administrative work which I felt had no direct relation to the standard of the clinical service we were delivering. In fact I can name specific measures taken in my trust to meet particular targets which undoubtedly reduced the quality of clinical care (male, Hospital Medical Specialties). |
| Burnout in last 5 years. I felt unable to provide the service I felt my patients deserved despite lengthening my hours and reducing my income (male, General Practice). |
| I was very unhappy with the changes that occurred during my final years in medicine. In my view, neither staff nor patients were well served by the trust I worked for (female, Psychiatry). |
| The effects of constant stress and pressure of work had an adverse effect on my work (female, Paediatrics). |
| The biggest factor was an increasingly heavy and exacting workload without sufficient time for complex cases. I felt unable to work as safely as I would have liked due to work overload (female, Pathology). |
| Life effectively ruined by severe migraine triggered by cuts in NHS leading to drastic bed closures in psychiatry. Hence unable to provide safe and satisfactory service for patients (female, Psychiatry). |
| Constant battle with the Primary Care Trust who disallow and obstruct patient care (male, General Practice). |
| I feel that my professional performance has been compromised at times by physical and mental fatigue (male, General Practice). |
| Psychiatrists can become ‘ODD’ because of their client group. Compassion burnout a problem in last years, immune to some horrific child abuse issues (female, Psychiatry) |
| Stress and burn out. There is only so much you can give without it affecting standards of care (male, General Practice). |
Stress/work–life balance/workload
Doctors mentioned stress and workload very frequently in their comments: ‘The pressures on junior doctors in the 1970s and 1980s caused immense stress and medium-term damage to my health and well-being’ (female, 1977). Another doctor said ‘I think I have been very overworked & stressed, & been unable to have “me” time or time for my family’ (female, 1977).
Many doctors expressed regret that they had lost so much time with their family, particularly with their children: ‘Long hours – I feel I neglected my children in their teenage years’ (female, 1977). Some doctors believed that working as a doctor had led to relationship problems: ‘Stress has been difficult to deal with throughout my career. Workload led to the collapse of my first marriage’ (male, 1974).
Illness
Episodes of burnout and depression were frequently attributed to the stress and workload doctors faced: ‘Stress and on-call led to depression leading to time off work and long term treatment’ (female, 1977) and ‘Chronic stress has caused burn out & depression’ (male, 1977).
Doctors often believed that physical illnesses such as stroke, heart disease, hypertension, and migraine were caused by, or aggravated by, stress: ‘Developed Ischaemic heart disease at 48. The massive workload of on-call work in the first 10 years contributed to this’ (male, 1974). Some doctors also developed mental illness: ‘Had acute bipolar disorder in mid-fifties as a result of tiredness and stress at work’ (male, 1977).
There were many instances of procedural/job-related illness: ‘Prolapsed intervertebral disc from bending over chairs that are too low and varicose veins from endless ward rounds’ (male, 1977), ‘Repetitive strain injuries doing procedures’ (male, 1974), and ‘I have suffered from surgeon’s neck prolapsed cervical disc, ruptured triangular fibro-cartilage of the wrist and a myocardial infarction – all related to work’ (male, 1977).
Many doctors commented that their health had improved substantially since retirement:
I developed high blood pressure, high cholesterol & migraines. Since retirement I have suffered none of these things & only realise with hindsight that I had accepted chronic ill health - mental & physical as a normal state but in reality these were work related. (female, 1977)
Exercise/weight/alcohol
Many doctors commented on the lack of opportunity for exercise: ‘I did not do enough exercise because I was so busy’ (male, 1977). Or the lack of time to eat properly: ‘Sleep deprivation & inadequate meal breaks meant at times I had poor eating habits & lacked exercise. I am now hypertensive’ (female, 1977) and ‘Irregular hours & meals – Diabetes Type II’ (male, 1974).
Some doctors commented that they drank too much alcohol: ‘OOH [out of hours] work and normal day work a factor in physical and mental exhaustion. No time for regular exercise and use of alcohol to cope’ (female, 1977).
Policies and patients
Many doctors feared or had experienced complaints and litigation: ‘I was the victim of a malicious complaint resulting in GMC “fitness to practice” hearing. I didn’t die, instead I nearly died from acute coronary syndrome, 5 months after the hearing’ (male, 1974).
Patient demand and ‘unrealistic expectations’ were also seen as being difficult: ‘Stress of GP responsibility & political pressure that raised patient expectation beyond what could be delivered led to my mental health deterioration with anxiety & depression’ (female, 1977).
Doctors complained about frequent policy changes and increased bureaucracy adding to the pressures they faced: ‘There were extremely stressful periods involving cuts in 1980s – 3 re-organisations in 1990s when I was a medical manager’ (female, 1974) and ‘Repeated restructuring & reorganisations in the Department of Health & specifically at Regional level caused me significant stress & adversely affected my mental health’ (female, 1974).
Availability of support
Some doctors said that they had received good support when they had needed it: ‘There were times in my career when I felt under great workload pressures and found myself anxious and sleeping badly. The support of my wife and my work partners helped me through’ (male, 1974).
Many doctors, however, did not receive the support they needed from their employer or colleagues: ‘High stress job unsupported by senior management’ (male, 1977) and ‘Pressure on coming back too early when not well’ (female, 1977). A few doctors had experienced bullying: ‘surviving in a unit where bullying was rife caused considerable stress’ (female, 1974).
Effects of ageing
The effects of growing older were mentioned by several doctors:
Surgeons are never going to be able to survive to state retirement age and there needs to be a process of reduction in activity after 60. On-call commitments need to be phased out of consultant job plans after the age of 55. (male, 1977)
and ‘I think that the profession makes little allowance for the effects of growing older’ (male, 1977). A few doctors mentioned how difficult they found their work as they got older: ‘It was very tiring & demanding & your energy levels fall as you get older’ (female, 1977), ‘We simply do not have the stamina in our 50s that we had in our 20s but the expectation on us is the same’ (male, 1977), and ‘At 62 I feel drained by the overwhelming demand we currently face in General Practice’ (male 1977).
One doctor said that she wanted to retire, but couldn’t yet do so: ‘I am exhausted, desperate to retire, but at 63 am still working 12-14 hour days’ (female, 1974). Many doctors talked about retirement as being a positive experience: ‘25 years as an NHS GP completely devastated me. I am so glad it is all over’ (male, 1977).
Other
Several doctors, while agreeing in the previous question that, ‘yes’, they felt that working as a doctor had had adverse effects on their health or wellbeing, went on to play down the negative effects they had experienced: ‘It is difficult to know whether the pressure of work contributed to mental health problems or not’ (male, 1977) and ‘Aware of the horrid things that happen to people so become quite negative and nervous about my health. Not currently medicated but considering review by GP’ (female, 1974).
The NHS of today is a good employer when doctors become ill themselves (univariable analysis)
The doctors were presented with the statement ‘The NHS of today is a good employer when doctors become ill themselves’. There were 49 missing answers to this statement. Of doctors who answered the statement, 713 (21.2%) answered ‘don’t know’: these doctors are excluded from the analysis, giving a total of 2594 responses on the five-point scale. Twenty-eight per cent of doctors agreed or strongly agreed with the statement, 29% answered ‘neither’, and 43% disagreed or strongly disagreed. More women doctors (49%) than men doctors (40%) disagreed with this statement (χ22 = 16.8, p < 0.001). More GPs (49%) than hospital doctors (37%) disagreed with this statement (χ22 = 48.2, p < 0.001). There were significant differences between the replies of doctors in the specialties that make up the ‘other hospital-based’ specialties (χ27 = 25.4, p < 0.001). Psychiatrists disagreed with the statement the most (71% disagreed) and anaesthetists disagreed with it the least (42% disagreed), with the other specialties that made up the group not differing significantly in their responses from the overall average level of disagreement (53%) in the group.
Doctors who were retired and not now working were more likely than other doctors to disagree with the statement (Table 2; χ26 = 24.5, p < 0.001); 47% of retired doctors who were not working disagreed with this statement compared with 36% of doctors still working full-time. No difference was observed between the two cohorts (χ22 = 2.1, p = 0.35).
Table 2.
Predictors of ‘The NHS of today is a good employer when doctors become ill themselves’ by cohort year, gender, specialty, and retirement status.
| Univariable analysis |
Multivariable analysis* |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Group | Disagreement (%) | Neither (%) | Agreement (%) | N | df | χ | p | OR (95% CI) | p |
| All | 42.6 | 29.0 | 28.4 | 2594 | |||||
| Cohort | 2 | 2.1 | 0.345 | ||||||
| 1977† | 41.2 | 30.4 | 28.5 | 1040 | – | – | |||
| 1974† | 43.6 | 28.0 | 28.4 | 1554 | – | – | |||
| Gender | 2 | 16.8 | <0.001 | ||||||
| Women‡ | 48.7 | 26.6 | 24.6 | 759 | 1 | ||||
| Men | 40.1 | 29.9 | 30.0 | 1835 | 1.4 (1.2, 1.8) | <0.001 | |||
| Specialty | 6 | 48.5 | <0.001 | ||||||
| GP‡ | 49.1 | 28.0 | 22.9 | 1226 | 1 | ||||
| Hospital medical specialties | 36.3 | 30.4 | 33.3 | 306 | 1.9 (1.4, 2.6) | <0.001 | |||
| Surgery | 36.2 | 29.4 | 34.4 | 282 | 1.8 (1.3, 2.5) | <0.001 | |||
| Other hospital | 37.3 | 29.7 | 32.9 | 780 | 1.9 (1.5, 2.4) | <0.001 | |||
| Retirement status | 6 | 24.5 | <0.001 | ||||||
| Retired, not now working in medicine‡ | 47.3 | 25.6 | 27.0 | 1132 | 1 | ||||
| Retired, and ‘returned’ for some medical work | 41.3 | 31.1 | 27.6 | 758 | 1.0 (0.8, 1.3) | 0.973 | |||
| Working full-time in medicine | 36.1 | 31.1 | 32.7 | 440 | 1.2 (0.9, 1.6) | 0.139 | |||
| Working part-time in medicine | 37.1 | 33.3 | 29.5 | 264 | 1.4 (1.0, 2.0) | 0.031 | |||
*The multivariable analysis is based on the comparison of the ‘% agreement’ results with the other two response categories combined.
†Cohort was not significant univariably and so was excluded from the model.
‡Reference group for multivariable model.
Note: A total of 2691 of 3550 doctors (Appendix 1) answered the question. ‘Univariable’ denotes single factor χ2 test for each predictor. The univariable analysis excluded doctors falling outside of the four specialty groups in the table above: this reduced the sample size to 2594. ‘Multivariable’ denotes binomial logistic regression result for each predictor with all other predictors in the model. We excluded cases where one or more predictors were missing, where the dependent variable was missing, or where the respondent was undecided: this reduced the sample size for the logistic regression from 2594 to 1843.
The odds ratio (OR) indicates whether a (randomly chosen) member of the group in question was more, or less, likely than a member of the reference group to agree with the statement. For example, a man would be 1.4 times as likely as a woman to agree with the statement.
The NHS of today is a good employer when doctors become ill themselves (multivariable analysis)
A binary logistic regression model was fitted with gender, specialty group, and retirement status as predictors (Table 2). In the multivariable model, gender and specialty group remained significant. Odds ratios and 95% confidence intervals are shown in Table 2.
Discussion
Main findings
Almost half of senior doctors said that working as a doctor had had adverse effects on their own health or wellbeing. More GPs than hospital doctors believed this to be the case. The most frequently mentioned adverse effect in text comments was ‘Stress/work–life balance/workload’ followed by illness.
Almost half of senior doctors did not agree that the NHS is a good employer when doctors become ill themselves. More women than men, and more GPs than hospital doctors disagreed that the NHS is a good employer when doctors become ill themselves.
Strengths and limitations
This was a national study of doctors who graduated from all UK medical schools in 1974 and 1977. These doctors had been surveyed several times over their careers. A response rate of 84.6% is very high for a self-completed survey. However, some non-response bias may have been present, though we have no evidence to suggest that responders are different from non-responders in characteristics relevant to this study. For example, 70.0% of non-responders were male, compared with 69.1% of responders (p = 0.67).
We present both numeric and qualitative summaries of the textual data. A purely numeric approach would have been inappropriate where the representativeness of the sample is not known.
Comparison with existing literature
Almost half of the senior doctors in our study said that working as a doctor had had adverse effects on their own health or wellbeing, particularly in relation to stress, work–life balance, and workload. A national study of senior hospital doctors in the UK found that senior doctors experience ‘unreasonable’ levels of stress most or all of the time, and 74% felt that work stress levels had increased in the last year.16 A national UK study of doctors at different career stages found that ‘exhaustion and fatigue’ is the most frequently raised topic by doctors in comments about working when feeling acutely ill.8 Many doctors in our study believed that working as a doctor had caused them to become ill. Over two-thirds of hospital consultants have reported that their health has been affected by work-related stress.16
In addition to the stress-related illnesses reported in our study, the doctors also reported specific job-related physical illnesses, often as a result of repeating the same manual task over and over again. Surgeons, in particular, have been found to be at greatest risk of musculoskeletal pain.21,22
Almost half of senior doctors in our study did not agree that the NHS is a good employer when doctors become ill themselves. A recent NHS staff survey found that 63% of staff attended work in the last three months despite being ill.18 In this same study, two-thirds of staff felt that their manager took a positive interest in their health. This last finding is different from our own, but the staff survey was not limited to doctors or to senior staff.
Conclusions
These doctors were speaking retrospectively at, or towards, the end of their careers. Their comments reveal a huge burden of ill health which many respondents attributed to aspects of their work, the working environment, or the difficulty of achieving a sustainable balance of work and home commitments. Some of the reported ill health may have arisen due to chronic long-term physical or mental stressors. Many doctors felt that the health service as an employer had, in their own experience, not been good at responding to doctors who became ill or who were subject to difficult and demanding personal circumstances. Although some of the reported comments relate to the past, there are lessons for the present and future if the NHS is to ensure that its medical workforce receives the support which enables current doctors to enjoy a full and satisfying career and to contribute fully to health service provision in the UK.
Doctors may not provide optimal care when they are ill themselves or lack wellbeing. We found instances where doctors ascribed a reduced quality of patient care to their own health and wellbeing issues. Although such comments were small in number, they arose unprompted and are suggestive of an unacknowledged problem, namely that some doctors, over time, acquire problems through the nature of their work which may adversely affect the quality of care they are able to provide. This is worthy of further investigation and planning. In the context in which medical careers are getting longer and retirement ages are increasing, doctors in the latter stages of their careers may have to adapt the make-up of their work to reflect the best use of their skills, experience, and abilities.
Appendix 1: UK doctors who graduated in 1974 and 1977: Response to 2014 survey and career status of respondents
| Year of graduation |
||||||
|---|---|---|---|---|---|---|
| 1974 | 1977 | Total | ||||
| Graduation cohort | 2347 | (100.0%) | 3135 | (100.0%) | 5482 | (100.0%) |
| Known to be deceased | 100 | (4.3%) | 110 | (3.5%) | 210 | (3.8%) |
| Declined to participate | 20 | (0.9%) | 50 | (1.6%) | 70 | (1.3%) |
| Uncontactable | 415 | (17.7%) | 418 | (13.3%) | 833 | (15.2%) |
| Contacted | 1812 | (77.2%) | 2557 | (81.6%) | 4369 | (79.7%) |
| Contactable doctors | 1812 | (100.0%) | 2557 | (100.0%) | 4369 | (100.0%) |
| Did not respond | 267 | (14.7%) | 407 | (15.9%) | 674 | (15.4%) |
| Responded in brief | 47 | (2.6%) | 51 | (2.0%) | 98 | (2.2%) |
| Responded in full | 1498 | (82.7%) | 2099 | (82.1%) | 3597 | (82.3%) |
| Respondents in full - Current employment | 1498 | (100.0%) | 2099 | (100.0%) | 3597 | (100.0%) |
| *Working full-time in medicine | 188 | (12.6%) | 471 | (22.4%) | 659 | (18.3%) |
| *Working part-time in medicine | 141 | (9.4%) | 243 | (11.6%) | 384 | (10.7%) |
| Working full-time outside medicine | 6 | (0.4%) | 10 | (0.5%) | 16 | (0.4%) |
| Working part-time outside medicine | 6 | (0.4%) | 8 | (0.4%) | 14 | (0.4%) |
| *Retired, not now working in medicine | 779 | (52.0%) | 793 | (37.8%) | 1572 | (43.7%) |
| *’Retired and returned’ for some medical work | 370 | (24.7%) | 565 | (26.9%) | 935 | (26.0%) |
| Other/no reply | 8 | (0.5%) | 9 | (0.4%) | 17 | (0.5%) |
Note: In all analyses we excluded doctors working outside of medicine and those who did not give details of employment (focussing upon those groups marked * above). This reduced the sample to 3550 doctors.
Declarations
Competing Interests
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and all authors want to declare: (1) financial support for the submitted work from the policy research programme, Department of Health. All authors also declare: (2) no financial relationships with commercial entities that might have an interest in the submitted work; (3) no spouses, partners, or children with relationships with commercial entities that might have an interest in the submitted work; (4) no non-financial interests that may be relevant to the submitted work.
Funding
This is an independent report commissioned and funded by the Policy Research Programme in the Department of Health (project number 016/0118). The views expressed are not necessarily those of the funding body.
Ethics approval
National Research Ethics Service, following referral to the Brighton and Mid-Sussex Research Ethics Committee in its role as a multi-centre research ethics committee (ref 04/Q1907/48 amendment Am02 March 2015).
Guarantor
All authors are guarantors.
Contributorship
TWL and MJG designed and conducted the surveys. FS performed the analysis and wrote the first draft of the paper. All authors contributed to further drafts and all approved the final version.
Acknowledgements
We thank Janet Justice and Alison Stockford for data entry. We are very grateful to all the doctors who participated in the surveys.
Provenance
Not commissioned; peer-reviewed by Raymond Chadwick.
References
- 1.Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med 2014; 89: 443–451. [DOI] [PubMed] [Google Scholar]
- 2.Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc 2013; 88: 1358–1367. [DOI] [PubMed] [Google Scholar]
- 3.Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R. Chronic stress experience in young physicians: impact of person- and workplace-related factors. Int Arch Occup Environ Health 2010; 83: 373–379. [DOI] [PubMed] [Google Scholar]
- 4.Doran N, Fox F, Rodham K, Taylor G, Harris M. Lost to the NHS: a mixed methods study of why GPs leave practice early in England. Br J Gen Pract 2016; 66: e128–e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tan PC, Robinson G, Jayathissa S, Weatherall M. Coming to work sick: a survey of hospital doctors in New Zealand. N Z Med J 2014; 127: 23–35. [PubMed] [Google Scholar]
- 6.Feeney S, O’Brien K, O’Keeffe N, Iomaire AN, Kelly ME, McCormack J, et al. Practise what you preach: Health behaviours and stress among non-consultant hospital doctors. Clin Med 2016; 16: 12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dyrbye LN, West CP, Satele D, Boone S, Sloan J, Shanafelt TD. A national study of medical students’ attitudes toward self-prescribing and responsibility to report impaired colleagues. Acad Med 2015; 90: 485–493. [DOI] [PubMed] [Google Scholar]
- 8.Smith F, Goldacre MJ, Lambert TW. Working as a doctor when acutely ill: comments made by doctors responding to UK surveys. J R Soc Med Open 2016; 7, DOI: 10.1177/2054270416635035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meerten M, Rost F, Bland J, Garelick AI. Self-referrals to a doctors’ mental health service over 10 years. Occup Med 2014; 64: 172–176. [DOI] [PubMed] [Google Scholar]
- 10.Murphy IJ. Self-reported and employer-recorded sickness absence in doctors. Occup Med 2014; 64: 417–420. [DOI] [PubMed] [Google Scholar]
- 11.Rogers ME, Creed PA, Searle J. Emotional labour, training stress, burnout, and depressive symptoms in junior doctors. J Voc Educ Train 2014; 66: 232–248. [Google Scholar]
- 12.Pereira-Lima K, Loureiro SR. Burnout, anxiety, depression, and social skills in medical residents. Psychol Health Med 2014; 20: 353–362. [DOI] [PubMed] [Google Scholar]
- 13.Morrow G, Burford B, Carter M, Illing J. Have restricted working hours reduced junior doctors’ experience of fatigue? A focus group and telephone interview study. Br Med J Open 2014; 4: e004222–e004222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paice E, Hamilton-Fairley D. Avoiding burnout in new doctors: sleep, supervision and teams. Postgrad Med J 2013; 89: 493–494. [DOI] [PubMed] [Google Scholar]
- 15.Smith F, Goldacre MJ, Lambert TW. Working as a doctor when chronically ill or disabled: comments made by doctors responding to UK surveys. J R Soc Med Open 2016; 7, DOI:10.1177/2054270416649282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hospital Consultants and Specialists Association. Who Cares for the Carers?. The Impact of Workplace Stress on Senior Hospital Doctors, London: Hospital Consultants and Specialists Association, 2015. [Google Scholar]
- 17.Department of Health. The NHS Constitution: The NHS Belongs to Us All, London: Department of Health, 2013. [Google Scholar]
- 18.National Health Service. Staff Survey 2015, London: National Health Service, 2015. [Google Scholar]
- 19.NHS England. Simon Stevens announces major drive to improve health in NHS workplace. See https://www.england.nhs.uk/2015/09/02/nhs-workplace/ (last checked 21 November 2016).
- 20.Lambert T, Goldacre M. Participation in medicine by graduates of medical schools in the United Kingdom up to 25 years post graduation: national cohort surveys. Acad Med 2013; 88: 699–709. [DOI] [PubMed] [Google Scholar]
- 21.Vijendren A, Yung M, Sanchez J. The ill surgeon: a review of common work-related health problems amongst UK surgeons. Langenbeck’s Arch Surg 2014; 399: 967–979. [DOI] [PubMed] [Google Scholar]
- 22.Vijendren A, Yung M, Sanchez J. Occupational health issues amongst UK doctors: a literature review. Occup Med 2015; 65: 519–528. [DOI] [PubMed] [Google Scholar]