Abstract
Objective The aim of this study was to estimate the costs of implementing computerized physician order entry (CPOE) systems in hospitals in a rural state and to evaluate the financial implications of statewide CPOE implementation.
Methods A simulation model was constructed using estimates of initial and ongoing CPOE costs mapped onto all general hospitals in Iowa by bed quantity and current clinical information system (CIS) status. CPOE cost estimates were obtained from a leading CPOE vendor. Current CIS status was determined through mail survey of Iowa hospitals. Patient care revenue and operating cost data published by the Iowa Hospital Association were used to simulate the financial impact of CPOE adoption on hospitals.
Results CPOE implementation would dramatically increase operating costs for rural and critical access hospitals in the absence of substantial costs savings associated with improved efficiency or improved patient safety. For urban and rural referral hospitals, the cost impact is less dramatic but still substantial. However, relatively modest benefits in the form of patient care cost savings or revenue enhancement would be sufficient to offset CPOE costs for these larger hospitals.
Conclusion Implementation of CPOE in rural or critical access hospitals may depend on net increase in operating costs. Adoption of CPOE may be financially infeasible for these small hospitals in the absence of increases in hospital payments or ongoing subsidies from third parties.
Two recent Institute of Medicine (IOM) reports, To Err Is Human1 and Crossing the Quality Chasm,2 raise very serious and troubling questions related to the safety and quality of health care services provided to the American public. These studies conclude that many Americans are injured each year as a result of adverse events during hospitalization. For a rural state like Iowa, extrapolating the IOM's estimated adverse event rate of 2.9% to 3.7% during hospitalization to Iowa's 361,493 acute care hospital admissions in 2000 suggests there were about 10,483 to 13,375 patients admitted who experienced adverse events. If, as the IOM estimates, 8.8% to 13.6% of adverse events result in death,1 there would have been an estimated 923 to 1,819 adverse event–related deaths in Iowa hospitals during 2000. The IOM estimates that as much as 75% of adverse event–related deaths are preventable.
Many of these adverse events relate to medication errors or other errors in the transcription or execution of physician orders during hospitalizations.1,2 A system utilizing computerized physician order entry (CPOE) may prevent some of these errors.3 Misinterpretation of written physician medication orders that result in the administration of an inappropriate drug or drug dose to a patient may be prevented through CPOE systems. CPOE systems also incorporate some elements of artificial intelligence to alert the physician to potential errors in medication orders before the physician's orders are accepted.4 CPOE also may improve the process of care by reducing redundant activities or by reducing staff time required to complete common activities.5 The promise of CPOE is that these features will prevent many serious medication errors and improve efficiency.
The apparent benefits of CPOE prompted the Leapfrog Group for Patient Safety, an organization founded by the Business Roundtable with support from the Robert Wood Johnson Foundation, to adopt CPOE as part of its initial Safety Standards.3 To comply with the Leapfrog Group's CPOE standards, hospitals must (1) require physicians to enter medication orders through administrative systems linked to error prevention software, (2) show that the system leads to the avoidance of at least 50% of potential medication errors, and (3) ensure that physicians are notified of medication order overrides.
There have been a substantial number of studies examining the use and potential benefits of CPOE systems.1,2,4,5,6,7,8,9,10,11,12 Many of these studies suggest significant benefits of CPOE in preventing errors or serious delays in the execution of physician orders. Despite these apparent benefits, relatively few hospitals have implemented CPOE systems, with implementation in small or rural hospitals being especially rare. The most often cited barrier to CPOE implementation is the up-front costs of these systems. Birkmeyer et al.13 estimate that first-year costs could vary from $500,000 to $4.1 million for a 200-bed hospital depending on the nature of the hospital's existing clinical information systems. Subsequent annual maintenance costs were estimated to range from $174,000 to $470,000. Given low or negative operating margins among many hospitals, these costs can represent a significant barrier to adoption of CPOE systems. In addition, hospitals operating in competitive environments may find it difficult to justify large capital expenditures because the return on investment in CPOE systems is not well understood.
The objective of this report is to employ a simulation model to estimate the costs of implementing CPOE in Iowa hospitals and to evaluate the financial implications of statewide CPOE implementation.
Methods
CPOE systems encompass software to enhance existing clinical information systems and entail adaptations of processes of care to utilize CPOE to its full potential. These systems require an information technology (IT) system infrastructure (i.e., hardware and communications) and organizational support (i.e., personnel, accountability and control, education, system maintenance). Because CPOE implementation costs depend critically on the nature of existing information systems and processes, the first step in the feasibility assessment requires a determination of the current IT infrastructure within Iowa hospitals.
To accomplish this task, a published survey instrument designed to measure hospital IT sophistication was employed.14 The instrument was augmented with several questions suggested by a leading vendor of CPOE systems. The resulting survey instrument was mailed to the CEO and CIO (or IT department head) of 114 general medical/surgical hospitals in Iowa during the fall of 2002. If no response was received, a second survey was mailed after a follow-up telephone call to the CEO's office. A total of 74 completed surveys were obtained, for an overall response rate of 64%.
Given the current IT infrastructure of Iowa hospitals, the next task in the evaluation was to estimate the costs of CPOE implementation. The same CPOE vendor that assisted in the development of the IT survey agreed to provide a range of estimates of initial and ongoing CPOE costs. As noted in Appendix 1, these estimates incorporate both the costs of the software and services provided by the vendor and costs of other resources required for CPOE, including enhancements in general IT systems, training, and additional personnel (both employee and contract). Cost estimates were provided for 200-, 400-, and 600-bed hospitals by the nature of the hospital's current clinical information system (CIS). Most CPOE implementation has occurred in hospitals with 200 or more beds. In instances in which CPOE has been implemented in smaller hospitals, the implementation was part of a multihospital system implementation, with some degree of system-level cross subsidization. As such, the vendor provided estimates for 100-bed hospital categories under the proviso that the estimates assumed smaller hospitals would work together as a purchasing cooperative to reduce costs.
The vendor's cost estimates were differentiated by the presence or absence of an existing CIS in the hospital. An existing CIS was defined as a fully integrated system or an integrated system with independent modules that include full internal integration with pharmacy. Based on the Iowa hospitals responding to the IT survey, an existing CIS was present in 67% (10 of 15) of urban hospitals, 50% (2 of 4) of rural referral hospitals, 31% (9 of 29) rural hospitals, and 19% (5 of 27) critical access hospitals. Approximately one third of hospitals in each category did not respond to the survey or to the items used to define an existing CIS. In the model simulations, nonresponding urban hospitals are assumed to have an existing CIS, but all other nonresponding hospitals are assumed to not have an existing CIS.
Cost estimates for new and existing CIS categories are mapped onto bed quantity using a simple quadratic form in bed quantity to interpolate and extrapolate from the vendor supplied cost estimates (▶). An estimate of CPOE cost is assigned to each Iowa hospital based on the hospital's bed size and CIS category. Model simulations on the scenarios use the vendor's lower cost estimates (“low” cost) or their higher cost estimates (“high” cost). To assess the sensitivity of simulation results to these estimated cost bounds, two additional cost scenarios are examined: (1) fixed cost 50% lower and incremental costs 25% lower than the vendor's “low” cost estimate (labeled “lower fixed/marginal cost”) and (2) fixed costs 50% higher and incremental cost 25% higher than the vendor's “high” cost estimate (labeled “higher fixed/marginal cost”). All four of these cost scenarios are illustrated in ▶.
Table 1.
Quadratic Interpolation Models for CPOE Costs by Bed Size
| “Low” Cost Estimates ($1000s) |
“High” Cost Estimates ($1000s) |
|||
|---|---|---|---|---|
| New CIS | Existing CIS | New CIS | Existing CIS | |
| Initial Costs (Model R2) | 0.989 | 0.989 | 0.989 | 0.989 |
| Intercept | 1170.0 | 777.9 | 1766.1 | 1956.8 |
| Beds coefficient | 6.211 | 2.615 | 8.785 | 8.785 |
| Beds squared coefficient | 3.37E-03 | 1.96E-03 | 3.72E-03 | 4.38E-03 |
| Ongoing Costs (Model R2) | 0.997 | 0.997 | 0.997 | 0.996 |
| Intercept | 218.0 | 123.3 | 452.4 | 347.5 |
| Beds coefficient | 0.892 | 0.594 | 1.331 | 1.769 |
| Beds squared coefficient | 6.83E-04 | 3.56E-04 | 1.69E-03 | 9.88E-04 |
Estimated cost = Intercept + (Bed coefficient * #Beds) + (Beds squared coefficient * #Beds * #Beds).
Figure 1.
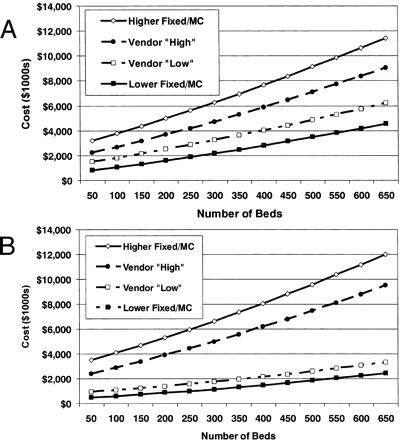
(A) Estimated initial CPOE costs, new clinical information system. (B) Estimated initial CPOE costs, existing clinical information system.
Still another set of alternative CPOE cost estimates were obtained from Birkmeyer et al.,13 who provide cost estimates for hospitals with 200 or 1,000 beds under three sets of assumptions about what they label CPOE “readiness.” They reported “best” case and “worst” case estimates for each readiness scenario and bed quantity. However, it is difficult to map Iowa hospitals onto the CPOE readiness categories utilized by Birkmeyer et al. To develop these alternative CPOE cost estimates for Iowa hospitals, these published cost estimates were extrapolated to Iowa hospitals under the following “worst” and “best” case scenarios.
The worst-case scenario uses the highest of the “worst case” cost estimates under the least CPOE-ready category for all but urban hospitals. For urban hospitals, the worst-case cost estimates for the intermediate readiness category are used.
The best-case scenario uses the lowest of the “best case” cost estimates under either of the two least CPOE-ready categories for all but urban hospitals. For urban hospitals, the best-case cost estimates for the highest readiness category are used. Further, first-year implementation costs are set to zero for urban hospitals that reported a current operational CPOE system.
Since only two bed-quantity estimates were reported, in all cases a simple linear interpolation in bed quantity was used to extrapolate implementation and subsequent operational costs.
Finally, CPOE cost estimates were combined with data for hospital revenues and costs from the Iowa Hospital Association15 to assess the financial impact of CPOE implementation. Simulations focus on the average hospital within four categories: urban, rural-referral, rural, and critical access hospitals. The simulation model uses the following assumptions for costs and revenues as a reference case:
All first-year CPOE implementation costs are treated as capital expenditures.
This CPOE capital is depreciated over five years using straight-line depreciation.
One hundred percent of the initial funds required are financed over a five-year period at an interest rate of 5%.
All subsequent operational costs are financed out of current operations.
CPOE is neutral with respect to non-CPOE costs (i.e., does not reduce or increase other operating costs).
CPOE is neutral with respect to operating revenue, with the exception of critical access hospitals, where CPOE-related changes in the cost base are assumed to affect their cost-based Medicare payments.
It should be emphasized that neutrality of CPOE for non-CPOE costs and revenues is assumed to simplify the simulation model to focus on the cost impact of CPOE per se. With this estimate, the extent of savings in non-CPOE costs or enhancements in revenue needed to make a business case for CPOE can be inferred.
Several alternative scenarios are examined in the financial impact simulation. One set of scenarios focuses on the impact of changes in assumptions about depreciation or interest expense. Another focuses on the potential impact of partial third-party payment for CPOE implementation costs. The simulation model also is used to identify the extent of revenue enhancements or cost savings associated with errors avoided or other process improvements through CPOE over a five- or ten-year period necessary to make CPOE a financially attractive investment for hospitals.
Results
The size distribution of Iowa hospitals is illustrated in ▶. Rural and critical access hospitals tend to have fewer beds than most hospitals that have implemented CPOE, as indicated by the Leapfrog Group. Even urban and rural referral hospitals in Iowa tend to be smaller on average than those in more urban states. This would suggest that implementation of CPOE systems in Iowa hospitals may be more difficult than implementation in more urban states.
Table 2.
Distribution of Iowa Hospital Size (Measured by Beds) by Location, 2000
| Urban (n = 20) | Rural Referral (n = 7) | Rural (n = 44) | Critical Access (n = 45) | |
|---|---|---|---|---|
| Mean | 282 | 212 | 62 | 45 |
| Maximum | 679 | 367 | 156 | 164 |
| 75th percentile | 379 | 280 | 84 | 60 |
| 50th percentile | 238 | 206 | 52 | 29 |
| 25th percentile | 151 | 131 | 40 | 25 |
| Minimum | 62 | 87 | 24 | 13 |
IT Survey
The IT infrastructure survey results are reported in several tables. As shown in ▶, few respondents report that a CPOE system currently is in place. However, the majority of respondents indicated that they are planning to implement a CPOE system. In both cases, it is unclear whether the CPOE systems currently in place or envisioned for the future entail all of the functions of CPOE as defined by the Leapfrog Group.
Table 3.
Survey Responses About Current and Planned CPOE Systems
| Urban (n = 13) | Rural Referral (n = 5) | Rural (n = 28) | Critical Access (n = 21) | |
|---|---|---|---|---|
| CPOE currently in place | 2 (15%) | 0 (0%) | 2 (7%) | 1 (5%) |
| Planning CPOE system | 11 (100%) | 3 (60%) | 17 (61%) | 13 (62%) |
Responses to specific items in the IT infrastructure survey related to patient management activities, physician services, nursing services, emergency department services, surgical (OR) services, and laboratory, radiology, and pharmacy services. Space constraints do not permit these item responses to be reported in detail here, but a consistent pattern is observed across most survey items. The availability of computerized processes tends to be greatest in urban hospitals, followed by rural-referral, rural, and critical access hospitals. However, some types of computerized processes are available in almost all hospitals, such as those related to basic patient management functions (e.g., inpatient or outpatient admissions). Others, such as computerized processes designed to manage staff scheduling and related care planning activities, are relatively uncommon at all Iowa hospitals in the survey sample. A similar, though less consistent, pattern is observed for responses to items related to the availability of technical activities.
The extent of integration across clinical functions and facilities is an important element of CPOE readiness. Mean survey responses related to system integration on a seven-point Likert scale (higher numbers indicating more integration) indicate that urban hospitals tend to have systems that are integrated to the greatest degree among the four hospital categories, whereas critical access hospitals tend to have the lowest degree of reported integration.
Costs of CPOE Implementation
The vendor-supplied CPOE cost estimates are the primary cost estimates used in all the reported analyses here. Estimates for the “best case” and “worst case” cost estimates are reported in ▶. Under the “low” cost scenario, costs for CPOE implementation are on average about $1.3 million for critical access and rural hospitals, $2.0 million for rural referral, and $1.9 million for urban hospitals. Under the “high” cost scenario, costs for CPOE implementation are on average about $2.1 million for critical access and rural hospitals, $3.2 million for rural referral, and $4.4 million for urban hospitals.
Table 4.
Estimated Initial and Ongoing CPOE Costs for Iowa Hospitals
| Mean Estimated CPOE Cost in $1000s (% of 2001 Total Costs) |
||||
|---|---|---|---|---|
| “Low” Cost Estimates |
“High” Cost Estimates |
|||
| Hospital Type | Initial | Ongoing | Initial | Ongoing |
| Urban (n = 20) | $1,866 (1.4%) | $343 (0.3%) | $4,429 (3.3%) | $889 (0.7%) |
| Rural referral (n = 7) | 1,963 (2.2) | 334 (0.4) | 3,218 (3.7) | 673 (0.8) |
| Rural (n = 44) | 1,279 (8.5) | 228 (1.5) | 2,120 (14.1) | 486 (3.2) |
| Critical access (n = 45) | 1,327 (19.2) | 238 (3.4) | 2,097 (30.3) | 492 (7.1) |
For rural and critical access hospitals, these CPOE implementation costs would represent a substantial expansion in total costs. For critical access hospitals, estimated implementation costs represent about 19% of current operating costs on average under the low cost scenario and about 30% of current costs under the high cost scenario. Subsequent year costs for critical access hospitals also represent a significant increase in costs (about 3.4% in the low and 7.1% in the high cost scenario). The cost impact is less pronounced but still substantial for rural hospitals, with estimated implementation costs representing about 9% of current operating costs on average under the low cost scenario and about 14% of current costs under the high cost scenario. Subsequent year costs are estimated to be about 1.5% in the low- and 3.2% in the high-cost scenario.
Financial Impact of CPOE Implementation
Presuming all Iowa hospitals have ready access to capital markets, the substantial implementation costs of CPOE could be spread over several years. The reference case financial simulations use a 5-year borrowing horizon with a 5% interest rate. Likewise, the value of the CPOE capital asset could be depreciated over time (5 years in the reference case).
Current operating margins and the projected impact of CPOE on margins for the first- and second-year post-CPOE are reported in ▶ and ▶. Recall these simulations assume no net financial benefit of CPOE as a simplifying assumption. In the reference case for the low cost scenario (▶), first year margins for urban hospitals on average decrease from 3.7% to 3.3%, and decrease from 5.0% to 4.4% for rural referral hospitals. In the second year after CPOE implementation, margins fall to 3.1% for urban hospitals and 4.0% for rural referral hospitals. The financial impact is more dramatic for rural and critical access hospitals. In the year of implementation, rural hospital margins decrease from 2.4% to 0.3%, with second-year margins decreasing into the negative range at −1.1%. For critical access hospitals, despite the assumed CPOE-induced increase in Medicare payments coupled with an average 66% Medicare share, first-year margins are estimated to decrease from −0.1% to −1.5%, with second-year margins falling to −2.4%.
Table 5.
Estimated Impact of CPOE on Hospital Operating Margins, “Low” CPOE Cost Estimates
| Urban | Rural Referral | Rural | Critical Access | |
|---|---|---|---|---|
| Operating margin (%, 2001) | 3.7% | 5.0% | 2.4% | −0.1% |
| Post-CPOE margin (Y1/Y2) | ||||
| Reference case* | 3.3/3.1 | 4.4/4.0 | 0.3/−1.1 | −1.5/−2.4 |
| Lower fixed/marginal cost | 3.5/3.3 | 4.6/4.4 | 1.3/0.5 | −0.9/−1.4 |
| Interest rate | ||||
| 3.0% | 3.4/3.1 | 4.4/4.0 | 0.5/−1.1 | −1.4/−2.4 |
| 7.0% | 3.3/3.1 | 4.3/4.0 | 0.2/−1.2 | −1.6/−2.5 |
| Depreciation | ||||
| 3 years | 3.2/2.9 | 4.0/3.7 | −0.8/−2.1 | −2.3/−3.1 |
| 7 years | 3.4/3.2 | 4.5/4.1 | 0.8/−0.6 | −1.2/−2.1 |
| Third-party reimbursement | ||||
| 25% | 3.4/3.2 | 4.5/4.2 | 0.8/−0.2 | −1.2/−1.9 |
| 50% | 3.5/3.4 | 4.6/4.4 | 1.3/0.6 | −0.8/−1.3 |
| 75% | 3.6/3.5 | 4.8/4.7 | 1.8/1.4 | −0.5/−0.7 |
5% interest, 5-year depreciation period, no third-party CPOE cost reimbursement (except Medicare for critical access).
Table 6.
Estimated Impact of CPOE on Hospital Operating Margins, “High” CPOE Cost Estimates
| Urban | Rural Referral | Rural | Critical Access | |
|---|---|---|---|---|
| Operating margin (%, 2001) | 3.7% | 5.0% | 2.4% | −0.1% |
| Post-CPOE margin (Y1/Y2) | ||||
| Reference case* | 2.9/2.2 | 4.0/3.2 | −1.0/−3.9 | −2.3/−4.0 |
| Higher fixed/marginal cost | 2.6/1.7 | 3.6/2.6 | −2.5/−6.5 | −3.2/−5.6 |
| Interest rate | ||||
| 3.0% | 2.9/2.3 | 4.1/3.3 | −0.8/−3.7 | −2.1/−4.0 |
| 7.0% | 2.8/2.2 | 3.9/3.2 | −1.2/−4.0 | −2.4/−4.1 |
| Depreciation | ||||
| 3 years | 2.4/1.8 | 3.5/2.7 | −2.7/−5.5 | −3.4/−5.0 |
| 7 years | 3.1/2.4 | 4.2/3.4 | −0.2/−3.1 | −1.8/−3.6 |
| Third-party reimbursement | ||||
| 25% | 3.1/2.6 | 4.2/3.6 | −0.2/−2.3 | −1.7/−3.1 |
| 50% | 3.3/2.9 | 4.5/4.0 | 0.7/−0.8 | −1.2/−2.1 |
| 75% | 3.5/3.3 | 4.7/4.5 | 1.5/0.7 | −0.7/−1.1 |
5% interest, 5-year depreciation period, no third-party CPOE cost reimbursement (except Medicare for critical access).
The financial impact of CPOE is substantially greater for all hospital types in the high CPOE cost scenario (▶). In the reference case, first-year margins for urban hospitals on average decrease from 3.7% to 2.9%, with second-year margins decreasing to 2.2%. For rural referral hospitals, first-year margins decrease from 5.0% to 4.0%, with second-year margins decreasing to 3.2%. Both rural and critical access hospitals would sustain substantial ongoing operating deficits as a result of CPOE implementation in the reference case.
Sensitivity Analyses
Several reference case assumptions are altered to provide a set of one-way sensitivity analyses, as shown in ▶ and ▶. If initial and ongoing CPOE costs are substantially lower than the vendor's “low” cost estimate (▶, “lower fixed/marginal cost”), operating margins for rural and critical access hospitals would be reduced significantly in the absence of cost offsets or revenue enhancements attributable to CPOE (other than the cost pass-through for Medicare in critical access hospitals, which is accounted for in the model). In contrast, if initial and ongoing CPOE costs are substantially higher than the vendor's “high” cost estimate (▶, “higher fixed/marginal cost”), operating margins for rural and critical access hospitals would be reduced to significantly below zero, again assuming revenue and other cost neutrality.
As one would expect, lower interest rates reduce the financial impact of CPOE implementation and vice versa. A shorter depreciation period increases the cost impact in the initial years postimplementation but reduces the cost impact in distal years. A longer depreciation period has the opposite impact. However, the negative financial impact of CPOE implementation remains substantial for rural and critical access hospitals under these alternative scenarios, assuming revenue and other cost neutrality.
The reference case assumes none of the additional costs associated with CPOE can be passed through to third-party payers in the form of higher reimbursement rates for services (with the exception of Medicare for critical access hospitals). The financial impact of CPOE is diminished in alternative scenarios where some portion of CPOE costs is passed through to third-party payers. For urban hospitals in the low-cost scenario, first-year margins decrease from 3.7% to 3.4% (low costs) or 3.1% (high costs) if on average 25% of CPOE costs are passed through to payers. First-year margins improve to 3.6% (low) or 3.5% (high) if 75% of CPOE costs are passed through. A similar pattern emerges for rural-referral hospitals. However, for critical access hospitals, even with 75% cost pass-through for non-Medicare payers (and 100% for Medicare), first-year operating margins decrease from −0.1% to −0.5% (low) or −0.7% (high), with second-year margins decreasing to −0.7% (low) or −1.1% (high).
Third-party Payers
The estimated impact of statewide CPOE implementation in Iowa on third-party payers is reported in ▶. In the reference case (100% cost pass-through for Medicare in critical access hospitals) using the low CPOE cost estimates, aggregate third-party payments to hospitals would increase by $9.8 million in the year of implementation and by $16.7 million in the second year. Using the high CPOE cost estimates, payments by third parties would increase by $15.5 million in the first year and $29.9 million in year two.
Table 7.
Estimated Third-Party Payments for CPOE Costs for Iowa Hospitals
| “Low” Costs |
“High” Costs |
|||
|---|---|---|---|---|
| Third Party Payment ($millions) | Year 1 | Year 2 | Year 1 | Year 2 |
| Medicare (critical access only) | $9.8 | $16.7 | $15.5 | $29.9 |
| 25% CPOE cost pass-through | 17.4 | 29.6 | 29.5 | 56.1 |
| 50% CPOE cost pass-through | 24.9 | 42.5 | 43.6 | 82.3 |
| 75% CPOE cost pass-through | 32.5 | 55.4 | 57.6 | 108.5 |
If all hospitals are able to pass 25% of CPOE costs on average to payers (non-Medicare payers for critical access hospitals), payments from third parties during the year of implementation would increase by $17.4 million (low costs) or $29.5 million (high costs). If hospitals are able to pass 75% of CPOE costs on average to payers (non-Medicare payers for critical access hospitals), payments from third parties during the year of implementation would increase by $32.5 million (low costs) or $57.6 million (high costs). Second-year payments would increase by $55.4 million (low) or $108 million (worst case). In the model, additional payments would decrease by about $1.3 million per year (low) or $2.3 million per year (high) from year three to year five due to declining interest expense and decline by about half in year six (due to the end of depreciation expenses).
To put these estimates into context, based on total net revenues of $4.2 billion for Iowa hospitals in 2001, 75% third-party payment for high CPOE costs would increase hospital payments overall by about 1.4% in year one and 2.3% in year two.
Cost Savings from Improved Safety and Efficiency
One promise of CPOE is that improving safety by reducing medication errors, and by avoiding delays and other inefficiencies in the delivery of hospital care, the cost of inpatient care can be reduced. To what extent would costs have to be reduced for the implementation and maintenance of a CPOE system to be hospital “budget neutral” over a ten-year period?
The reference case model assumes no impact of CPOE on revenues (except Medicare for critical access hospitals) and no impact on other costs. As reported in ▶, using high CPOE cost estimates, critical access hospitals would have to trim annual operating costs by about 3.1% to offset the costs of CPOE over 10 years. For rural hospitals, the required cost offset is about 4.5% of costs. The required offset is about 1.1% per year for rural-referral hospitals and 1.0% per year for urban hospitals. Using the low CPOE cost estimates, annual cost offsets would have to total 1.7% for critical access hospitals, 2.3% for rural hospitals, 0.6% for rural referral hospitals, and 0.4% for urban hospitals.
Table 8.
Estimated Annual Cost Savings from CPOE-Related Efficiency/Safety Improvement Needed for Hospital “Budget Neutrality” Over a Ten-Year Period
| Hospital Type | “Low” Costs | “High” Costs |
|---|---|---|
| Urban (n = 20) | 0.4% | 1.0% |
| Rural referral (n = 7) | 0.6 | 1.1 |
| Rural (n = 44) | 2.3 | 4.5 |
| Critical access (n = 45) | 1.7 | 3.1 |
Discussion
The main impetus behind the Leapfrog Group's support for CPOE systems is the promise that these systems will improve safety by reducing medication errors and other inadequacies in the delivery of hospital care. Several studies offer support for this proposition.4,6,8,10,11,12 However, most of the hospitals that have implemented CPOE are large urban hospitals; few small rural hospitals have attempted to do so. As a result, all existing studies of the effects of CPOE have taken place in large urban hospitals.9,16 It is unclear how well results for studies of large complex urban hospitals apply to small rural hospitals with fewer complex care delivery systems.
Some of the costs of CPOE may be offset if improvements in patient safety or efficiency translate into reductions in patient care costs. However, only a few studies have attempted to assess the impact of CPOE on total patient care costs. Most of these conclude that improvements in the efficiency of the process of care offer the most direct path for cost offsets rather than safety improvements. For example, Mekhjian et al.5 conclude that the introduction of CPOE (coupled with an electronic medication administration record) reduced the time used by hospital staff to complete order execution for pharmacy, radiology, and laboratory services. Acuity-adjusted patient length-of-stay decreased modestly, but there was no effect on costs per admission. Thus, the few studies that have attempted to quantify the impact of CPOE on total operating costs have not identified substantial cost savings.
CPOE also may enhance patient care revenues. First, improved clinical information systems may provide a more complete capture of resources used or a more accurate diagnosis-related group assignment, which could improve reimbursement. Second, if quality-based payment systems expand, CPOE may assist in attaining quality benchmarks that trigger quality premium payments. However, the impact of CPOE on patient care revenues, especially in small rural hospitals, is unknown.
In the absence of cost offsets or revenue enhancements, model results imply that the implementation and ongoing costs of CPOE would represent a substantial percentage increase in operating costs for rural and critical access hospitals. For urban and rural referral hospitals, the cost impact is less dramatic but still substantial. It seems reasonable to speculate that annual cost savings and/or revenue enhancements of 0.5% to 1.0% of total operating costs would not be implausible, given the apparent improvements in production efficiency and reductions in serious medication errors attributed to CPOE. If so, then CPOE implementation should be financially feasible for most urban and rural referral hospitals in Iowa. Indeed, several of these hospitals already have or are currently implementing CPOE systems. However, more substantial (and implausible) cost savings would be required for CPOE to reduce costs enough to make implementation financially feasible for rural or critical access hospitals, especially in “high” cost model scenarios. Thus, it is likely that subsidies for initial and ongoing CPOE costs in these hospitals would be required to make CPOE financially feasible.
Obviously, these conclusions are based on very crude CPOE cost estimates. Often, CPOE implementation has been part of an extensive process of updating and re-engineering entire hospital information systems and processes. If these related costs are taken into account, even the “high” scenario may understate implementation costs. Better estimates of the financial impact of CPOE in smaller hospitals are needed to more fully assess financial feasibility.
Finally, even if CPOE does not “pay for itself” through cost offsets or revenue enhancements, this should not be interpreted as suggesting CPOE is inappropriate for smaller hospitals. An improvement in the quality of care has societal value, so the policy question is whether the extent of quality improvement is sufficient to justify the societal cost of achieving improved quality. The experience in larger hospitals suggests that CPOE is likely to improve outcomes of care in small rural hospitals. Assessing the extent of quality improvement attributable to CPOE in small rural hospitals is hampered by the “small numbers” problem inherent with low patient volumes. Nonetheless, such an assessment is essential for an evaluation of the cost effectiveness of CPOE in small hospitals and should be a priority for future research.
Appendix 1. Estimated CPOE Costs by Type of Expense
| Bed Number | Hardware and Network Software Upgrades | CPOE-Related Software and Support | Selection Process | Testing, Training, and Other |
|---|---|---|---|---|
| “Low” estimates: initial costs | ||||
| Existing CIS | ||||
| 100 Beds | $ 78,300 | $ 250,000 | $ 65,000 | $ 592,400 |
| 200 Beds | 156,700 | 500,000 | 65,000 | 790,000 |
| 400 Beds | 235,000 | 750,000 | 81,300 | 987,400 |
| 600 Beds | 352,500 | 1,125,000 | 121,900 | 1,481,100 |
| No existing CIS | ||||
| 100 Beds | 428,300 | 395,000 | 27,500 | $ 822,000 |
| 200 Beds | 865,700 | 790,000 | 27,500 | 1,096,000 |
| 400 Beds | 1,285,000 | 1,185,000 | 34,400 | 1,370,000 |
| 600 Beds | 1,927,500 | 1,777,500 | 51,600 | 2,055,000 |
| “High” estimates: initial costs | ||||
| Existing CIS | ||||
| 100 Beds | $ 614,200 | $ 540,000 | $ 130,000 | $ 1,383,000 |
| 200 Beds | 1,228,400 | 1,080,000 | 130,000 | 1,844,000 |
| 400 Beds | 1,842,500 | 1,620,000 | 162,500 | 2,305,000 |
| 600 Beds | 2,763,800 | 2,430,000 | 243,800 | 3,457,400 |
| No existing CIS | ||||
| 100 Beds | 614,200 | $ 540,000 | $ 55,000 | 1,267,100 |
| 200 Beds | 1,228,400 | 1,080,000 | 55,000 | 1,689,400 |
| 400 Beds | 1,842,500 | 1,620,000 | 68,800 | 2,111,800 |
| 600 Beds | 2,763,800 | 2,430,000 | 103,100 | 3,167,700 |
| “Low” estimates: ongoing costs | ||||
| Existing CIS | ||||
| 100 Beds | $ 11,100 | $ 40,500 | $ 126,500 | |
| 200 Beds | 22,100 | 81,000 | 168,600 | |
| 400 Beds | 33,200 | 121,500 | 252,900 | |
| 600 Beds | 49,800 | 182,300 | 379,500 | |
| No existing CIS | ||||
| 100 Beds | 5,300 | 66,600 | $ 230,400 | |
| 200 Beds | 5,300 | 133,200 | 307,100 | |
| 400 Beds | 8,000 | 199,800 | 460,700 | |
| 600 Beds | 12,000 | 299,700 | 691,100 | |
| “High” estimates: ongoing costs | ||||
| Existing CIS | ||||
| 100 Beds | $ 76,500 | $ 88,200 | $ 344,300 | |
| 200 Beds | 152,900 | 176,400 | 459,000 | |
| 400 Beds | 229,400 | 264,600 | 688,500 | |
| 600 Beds | 344,000 | 396,900 | 1,032,800 | |
| No existing CIS | ||||
| 100 Beds | 8,900 | $ 88,200 | 483,200 | |
| 200 Beds | 8,900 | 176,400 | 644,300 | |
| 400 Beds | 13,400 | 264,600 | 966,500 | |
| 600 Beds | 20,000 | 396,900 | 1,449,700 |
Supported by the Iowa Department of Public Health.
References
- 1.Kohn LT, Corrigan J, Donaldson MS (eds). To Err Is Human: Building a Safer Health System. National Academy Press, 2000. [PubMed]
- 2.Institute of Medicine (ed). Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press, 2001. [PubMed]
- 3.Leapfrog Group. Fact Sheet: Computer Physician Order Entry. Washington DC: The Leapfrog Group, 2000.
- 4.Bates DW, Teich JM, Lee J, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6:313–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mekhjian HS, Kumar RR, Kuehn L. Immediate benefits realized following implementation of physician order entry at an academic medical center. J Am Med Inform Assoc. 2002;9:529–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bates DW, Leape L, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280:1311–6. [DOI] [PubMed] [Google Scholar]
- 7.Bates DW, Spell N, Cullen DJ, et al. The costs of adverse drug events in hospitalized patients. JAMA. 1997;277:307–11. [PubMed] [Google Scholar]
- 8.Bates DW, Teich JM, Merchia PR, et al. Effects of computerized physician order entry on prescribing practices. Arch Intern Med. 2000;160:2741–7. [DOI] [PubMed] [Google Scholar]
- 9.Oren E, Shaffer ER, Guglielmo BJ. Impact of emerging technologies on medication errors and adverse drug events. American J Health Syst Pharm. 2003;60:1447–58. [DOI] [PubMed] [Google Scholar]
- 10.Evans RS, Pestotnik SL, Classen DC, et al. A computer-assisted management program for antibiotics and other antiinfective agents. N Engl J Med. 1998;338:232–8. [DOI] [PubMed] [Google Scholar]
- 11.Classen DC, Pestotnik SL, Evans RS, et al. Adverse drug events in hospitalized patients: excess length of stay, extra costs, and attributable mortality. JAMA. 1997;277:301–6. [PubMed] [Google Scholar]
- 12.Leape LL, Bates DW, Cullen DJ. Systems analysis of adverse drug events. JAMA. 1995;274:35–43. [PubMed] [Google Scholar]
- 13.Birkmeyer JD, Birkmeyer CM, Skinner JS. Economic Implications of the Leapfrog Safety Standards. Washington, DC: The Leapfrog Group, 2001.
- 14.Peré G, Sicotte C. Information technology sophistication in health care: an instrument validation study among Canadian hospitals. Int J Med Inf. 2001;63:205–23. [DOI] [PubMed] [Google Scholar]
- 15.Iowa Hospital Association. Profiles. August 2001.
- 16.Kuperman GJ, Gibson RF. Computer physician order entry: benefits, costs and issues. Ann Intern Med. 2003;139:31–9. [DOI] [PubMed] [Google Scholar]


