Abstract
Objective: This multisite study compared the perceptions of three stakeholder groups regarding information technologies as barriers to and facilitators of clinical practice guidelines (CPGs).
Design: The study settings were 18 U.S. Veterans Affairs Medical Centers. A purposive sample of 322 individuals participated in 50 focus groups segmented by profession and included administrators, physicians, and nurses. Focus group participants were selected based on their knowledge of practice guidelines and involvement in facility-wide guideline implementation.
Measurements: Descriptive content analysis of 1,500 pages of focus group transcripts.
Results: Eighteen themes clustered into four domains. Stakeholders were similar in discussing themes in the computer function domain most frequently but divergent in other domains, with workplace factors more often discussed by administrators, system design issues discussed most by nurses, and personal concerns discussed by physicians and nurses. Physicians and nurses most often discussed barriers, whereas administrators focused most often on facilitation. Facilitators included guideline maintenance and charting formats. Barriers included resources, attitudes, time and workload, computer glitches, computer complaints, data retrieval, and order entry. Themes with dual designations included documentation, patient records, decision support, performance evaluation, CPG implementation, computer literacy, essential data, and computer accessibility.
Conclusion: Stakeholders share many concerns regarding the relationships between information technologies and clinical guideline use. However, administrators, physicians, and nurses hold different opinions about specific facilitators and barriers. Health professionals' disparate perceptions could undermine guideline initiatives. Implementation plans should specifically incorporate actions to address these barriers and enhance the facilitative aspects of information technologies in clinical practice guideline use.
For more than a decade, the Institute of Medicine and federal agencies such as the Agency for Healthcare Research and Quality have recommended clinical practice guidelines (CPGs) as a means of improving patient care outcomes in acute care settings.1,2,3,4,5 In response, researchers, professional organizations, and health facilities are developing and implementing practice guidelines with increasing frequency in a variety of health care arenas as a means to lessen wide practice variations, improve quality of care, and control escalating medical costs.6,7,8,9 A major concern that health professionals and organizations share is developing methods for integrating the vast amount of clinical data and scientific support required for providing evidence-based health care. Policymakers have long recommended computers as a means for bridging this gap between research and practice. Essential components of a health information infrastructure include decision support systems, point-of-contact documentation, Internet access to guidelines, order entry features, and easy communication between settings.1,2,3,4,5,6,7,8,9,10
Most studies on the use of computers in health care have focused on a single professional perspective.11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30 Physicians11,12,13,14,15,16,17,18 and nurses19,20,21,22,23,24,25 are those most frequently surveyed about their computer knowledge, attitudes, and skills. Only a few studies have elicited the perceptions of pharmacists, diabetes educators, occupational therapists, and mental health workers.26,27,28,29,30 Using this disciplinary approach, researchers find that many health professionals view the incorporation of information technology into clinical practice favorably.11,12,13,22 Inconclusive or dissenting opinions about health care information technologies are offered from groups whose work-related tasks are not adequately addressed by their organization's computer systems.14,15,18,19,20,30
Unfortunately, this single-provider focus does not well represent clinical reality as experienced by interdisciplinary teams composed of physicians, nurses, social workers, pharmacists, therapists, dieticians, ancillary personnel, and health administrators. While each professional has unique informational and technological needs related to clinical guidelines, the organizational supports for interdisciplinary teams using guidelines remain largely unexplored. Few exceptions to the single profession perspective trend exist, and these suggest important discrepancies in perceptions about computer technologies between occupational groups working together in the same setting.31,32,33,34,35 The views of physicians and nurses on order entry systems reveal cross-disciplinary agreement regarding the speed of order execution and patient care quality. Physicians reported that computers decreased their patient contact time, whereas nurses noted the opposite effect.32,33 In another example, pharmacists highly endorsed computer technologies as a benefit to clinical practice, whereas physicians and nurses were skeptical of pharmaceutical information obtained through computerized drug references.34 A multimethod approach to evaluating computer acceptance in two pediatric offices attributes users' reactions to differences in organizational culture, beliefs about the benefits of computers, and supportive versus strained relationships between informaticists and clinic staff.35
What are the concerns of key stakeholders regarding the use of computers to support CPGs? In this study, three stakeholder groups (administrators, physicians, and nurses) from 18 Veterans Affairs Medical Centers (VAMCs) participated in 50 focus groups designed to identify barriers and facilitators to the implementation and maintenance of clinical practice guidelines initiatives in acute care facilities.
Background
The Veterans Health Administration (VHA) has fostered efforts to adapt and implement evidence-based CPGs. In 1996, the VHA began implementing CPGs as part of their quality performance program. Many of these guidelines are those recommended by the U.S. Preventive Services Task Force (immunizations, cancer screening, obesity, and alcohol and tobacco use), agencies such as the Agency for Health Care Policy and Research (smoking cessation), or developed by the VHA (diabetes, hypertension, and ischemic heart disease). The VHA annually rolls out two to four new or revised CPGs. Correspondingly, the VHA evaluates facility performance through the External Peer Review Program (EPRP). The EPRP is a contracted on-site review of clinical records. Data are abstracted quarterly from a sample of patient health records at each VAMC facility by trained abstractors. Thus, the VHA offers a natural field setting to study organizational factors across a single system implementing specified CPGs.
As part of the VHA's Quality Enhancement Research Initiative (QUERI), we designed a multicomponent study to examine factors associated with effective CPG implementation within VAMC hospitals. In one phase of this study, participants' insights about the organizational structure and process features that assist and deter guideline use were elicited through focus group methodology. Our early data analysis revealed four major facilitators and four major barriers in overall CPG implementation, maintenance, and adherence. Facilitators were information technology (particularly computerized patient records and decision support), work reorganization, audit/feedback, and administrative support. Barriers were time, workload, informatics deficits, and guideline credibility/compatibility. Because information technology was identified as both a major barrier and facilitator and, as stakeholders highlighted different aspects, we wished to further examine this specific domain. The purpose of this paper then is to compare the perceptions of administrators, physicians, and nurses regarding information technologies as barriers and facilitators of CPGs implementation and use.
Methods
Study Settings
The sampling unit was the VAMC and the population all VAMCs providing acute ambulatory care services. VAMC facility performance across a series of chronic illness quality of care indicators was benchmarked using chart audit data.36 Site sampling was purposive using the maximize variation method37 to capture facilities with characteristics associated with either high or low EPRP performance such as organizational structure (university affiliation, bed size), patient demographics (ethnic diversity, average age), and geographic region [Veterans Integrated Service Networks (VISN)]. Oversampling of facilities with high EPRP scores was performed on the premise that these facilities had been more successful in implementing the CPGs, may have used a more diverse set of implementation strategies than lower scoring facilities, and also may have greater insight into their successes. Eighteen VAMCs from 11 VISNs participated in this study. We enrolled 13 facilities with high EPRP performance scores and five sites with lower ratings. Eight of the sites were affiliated with university hospitals. Hospital size averaged 314 beds (range, 63–800+ beds). Three VAMCs had fewer than 100 beds, ten had between 100 and 400 beds, four had 401 to 800 beds, and one VAMC had more than 800 beds. Patient demographics varied widely among the research sites. The average patient age ranged from 61 to 69 years by site. The percentage of minority patients by facility ranged from 0% to 44%.
Research Participants
Institutional review board and VA Research Committee approval was obtained before participant recruitment. Focus groups were conducted with VAMC employees who had either administrative responsibility or clinical leadership roles for guideline implementation initiatives in their facilities. Study participants were placed into one of three groups according to their current professional role. Administrator focus groups were conducted with managers who supervised unit-level guideline use and included medical chiefs of staff, directors of nursing, and clinic directors. Physician focus groups were held with all types of primary care providers, including physicians, nurse practitioners, and physician assistants responsible for prescribing CPG-based treatments. Nurse focus groups included people responsible for providing and documenting guideline-based patient care. This group was primarily composed of nurses but also included dieticians, pharmacists, and social workers. The clinicians, as guideline team members and change champions, were both implementers and users of CPGs. In total, we interviewed 322 individuals in 17 administrator, 16 physician, and 17 nurse focus groups. Each study participant completed a brief demographic survey. ▶ depicts the participants' demographic characteristics.
Table 1.
Participant Demographic Characteristics
| Participant Demographics (N = 322) | Administrator Focus Groups* (n = 102) | Physician Focus Groups† (n = 103) | Nurse Focus Groups‡ (n = 117) |
|---|---|---|---|
| Mean age (y) | 47.8 | 46.3 | 44.4 |
| % Female | 63% | 43% | 86% |
| Mean years career | 22.9 | 18.7 | 19.9 |
| Mean years VA system | 17.1 | 7.7 | 13.4 |
Administrators include medical chiefs of staff, directors of nursing, and clinic directors.
Physicians include physicians, nurse practitioners, and physician assistants.
Nurses include nurses, dieticians, pharmacists, and social workers.
Data Collection Analysis
Focus group methodology38 was used to obtain the interview data. A discussion guide based on a comprehensive review of the CPG literature and the objectives of the study structured the interviews. The focus group guide elicited participants' understandings of CPGs, reviewed facility history with guideline use and current implementation strategies, identified facilitators and barriers to CPG adoption and maintenance, and gathered suggestions for improvements in ongoing guideline initiatives. In all, 50 focus groups were completed over a 14-month period from 1999 to 2001. Individuals with graduate preparation and previous experience in leading focus groups conducted the sessions. Groups were formed around a conference-style setup to facilitate discussion among members. The focus groups lasted approximately 90 minutes each. A brief survey began the sessions, and, after an introductory set of remarks from the leader about process and procedures, discussion followed the focus group guide. Sessions were recorded on audio tapes using two separate taping systems to ensure data collection in the event of machine failure. This procedure also aided accurate transcription by having voice recordings from two different locations. All tapes were transcribed verbatim, and the transcriptions were checked for accuracy by team members.
The focus group sessions resulted in nearly 1,500 pages of transcripts that were examined using a descriptive content analysis. Descriptive content analysis is a structured document analysis technique by which a researcher examines textual data using a mutually exclusive and comprehensive categorical coding plan and numerical counts of themes.39 The frequency with which a theme is mentioned is considered an indicator of its importance within a stakeholder group as well as a gauge of consensus among groups. A coding template was created from the parent study's conceptual framework and its more than 300 first level codes and then extended with topics from the theoretical and research literature on CPGs, organizational change, and health informatics.40,41
Computer-assisted text analysis software (NUD*IST Vivo [NVivo], Scolari Software) was used for coding and sorting transcribed data and compiling and comparing themes across groups. To prepare the first-level codes for the in-depth analysis reported here, we conducted an NVivo code search for all text coded with the terms computer, electronic medical record, electronic patient record, and technology, as well as a text search for passages surrounding the text words of computer, electronic, and technology. These passages were combined into a unified text data set and recoded for the more discrete (second-level) themes related to the use of information technologies in CPG initiatives. These second-level codes were then additionally coded as a facilitator, barrier, or neutral statement about computers and practice guidelines. The frequency with which each of the themes appeared was recorded and the percentage of occurrence within a domain and as a facilitator/barrier statement calculated. Finally, the themes were clustered into domains, assembled into a data matrix arrayed by stakeholder group, and analyzed to determine points of thematic agreement and divergence among participants.
Results
Introduction to Major Themes and Domains
Eighteen themes related to the use of information technologies for clinical guideline use were identified and clustered into four domains (▶). Overall, administrators, physicians, and nurses discussed the themes in the computer tasks domain most frequently (33% of all comments). Administrators discussed the workplace factors themes (43%) more frequently than the other stakeholder groups. Nurses and other clinicians emphasized the topics in the system designs (38%) domain more than the other stakeholders. Nurses (46%) and physicians (34%) identified themes in the personal concerns domain more often than did the administrators (20%).
Table 2.
Distribution of Themes by Participant Group and Domain Percentage
| Domain (n = 4) Themes (n = 18) |
Administrators 337 (34%) |
Physicians 297 (30%) |
Nurses 358 (36%) |
All Comments 992 (100%) |
|---|---|---|---|---|
| No. (% Domain) | No. (% Domain) | No. (% Domain) | No. (% of Total) | |
| Computer tasks | 115 (34%) | 109 (33%) | 108 (33%) | 332 (33%) |
| Documentation | ||||
| Decision support | ||||
| Performance evaluation | ||||
| Data retrieval | ||||
| Order entry | ||||
| Workplace factors | 120 (43%) | 69 (25%) | 91 (32%) | 280 (28%) |
| Patient records | ||||
| Guideline implementation | ||||
| Guideline maintenance | ||||
| Computer literacy | ||||
| Resources | ||||
| System designs | 69 (32%) | 63 (29%) | 82 (38%) | 214 (22%) |
| Accessibility | ||||
| Essential data | ||||
| Charting formats | ||||
| Computer glitches | ||||
| Personal concerns | 33 (20%) | 56 (34%) | 77 (46%) | 166 (17%) |
| Time | ||||
| Workload | ||||
| Attitudes | ||||
| Computer complaints |
▶ displays the frequency of themes coded as facilitators or barriers for CPG use. Participants largely discussed computer-related barriers (64%) to clinical guidelines more often than their facilitative aspects (36%). The tendency to identify computers as barriers was more common within the physician (78%) and the nurse (68%) focus groups. In contrast, the administrator focus groups modestly (51%) highlighted computers as guideline facilitators.
Table 3.
Facilitator and Barrier Statements by Stakeholder Group
| Stakeholder Group | Facilitators n = 353 (36%) | Barriers n = 639 (64%) | Total Statements (N = 992) |
|---|---|---|---|
| Administrators | 171 (51%) | 166 (49%) | 337 |
| Physicians | 66 (22%) | 231 (78%) | 297 |
| Nurses | 116 (32%) | 242 (68%) | 358 |
▶ (facilitators) and ▶ (barriers) use Venn diagrams to depict relationships within the data. Each circle represents a stakeholder group: administrators (large dash), nurses (dots), and physicians (small dash). Areas of overlap between the circles represent thematic agreement between the corresponding groups with the center indicating concurrence among the three stakeholder groups. Overall, few themes clearly emerged as a facilitator or a barrier to guideline implementation. Administrators alone identified the usefulness of computers for guideline maintenance and for developing charting formats. Computer-related barriers included resources, computer complaints, computer glitches, time, workload, attitudes, data retrieval, and order entry. Participants identified many themes as both a barrier and a facilitator. Themes with dual designations included patient records, documentation, decision support, performance evaluation, guideline implementation, computer literacy, essential data, and accessibility. An in-depth discussion of these themes and domains follows.
Figure 1.
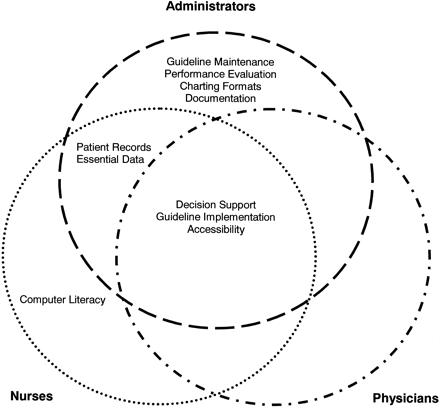
Computers as facilitators of clinical practice guidelines.
Figure 2.
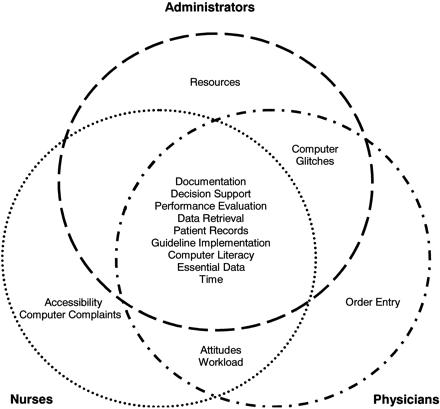
Computers as barriers to clinical practice guidelines.
Discussion of Major Domains and Themes
Computer Tasks Domain
The computer function domain outlines five activities that participants perform with computers: documentation, decision support, performance evaluation, data retrieval, and order entry. Administrators were evenly divided in their views of these computer tasks as facilitators or barriers of guideline use. However, physicians and nurses largely considered these computer-augmented tasks as barriers to providing health services. A small number of stakeholders in each group viewed inefficient data retrieval as an obstacle to guideline use. Physicians alone were frustrated when order entry tasks were added to their already full workdays, especially when only limited instruction was given on their use. Documentation, decision support, and performance evaluation, viewed as both a barrier and a facilitator depending on the stakeholder group, are discussed in more detail below.
Documentation
Documentation of patient care was problematic for all stakeholders. Nearly three fourths of the participants' comments about documentation mentioned barriers. Although administrators agreed that quality documentation would enhance guideline-based patient care, the burdens of documenting care activities using the computer as currently programmed outweighed any potential benefits for most participants. Documentation of patient care data took considerable time, added to clinicians' workload, interfered with workflow patterns, required frequent updates, and was difficult for people with underdeveloped keyboarding skills.
Decision support
Decision support refers to tasks that assist health professionals with clinical decision making through the integration of patient information and evidence-based scientific recommendations. Stakeholders from the three groups mentioned the positive features of several electronic decision support features including automated clinical reminders, alerts, prompts, and templates. However, physicians and nurses referenced the benefits of paper-based tools such as cue cards, flowsheets, and checklists as frequently as they mentioned computerized decision support. Participants were generally supportive of computerized decision support features although an important area of tension was noted. Administrators believed that decision support functions saved time, relieved workloads, and eased charting requirements. In contrast, physicians and nurses stated that these features lengthened the time needed for patient care and increased their workload by adding new documentation tasks.
Performance evaluation
Administrators used performance evaluation programs to monitor patient outcomes and assess physician adherence to CPGs. Administrators considered performance evaluation as a useful tool for improving organizational and clinical outcomes. However, members of all stakeholder groups voiced concern that these electronic surveillance features would allow unfavorable and unfair judgments about professionals' clinical practices.
Workplace Factors Domain
This domain categorized five themes related to computer use within the larger institutional context: patient records, guideline implementation, guideline maintenance, computer literacy, and resources. Administrators viewed many workplace factor themes as guideline facilitators, whereas physicians and nurses felt that they hampered clinical practice.
Patient records
The major theme of this domain was patient records. Administrators and nurses agreed that comprehensive patient records were fundamental to providing quality health care services. However, most participants contended that current methods of maintaining health records were barriers to efficient patient care. Stakeholders were divided as to whether electronic records were facilitators of or barriers to using clinical guidelines. Although a recognized barrier to efficiency, nurses and physicians who felt “computer illiterate” and those who considered themselves too busy to access or learn computer guidelines preferred paper-based records to electronic versions. Many physicians suggested support for dictation and transcription services.
Guideline implementation
Stakeholders in all three groups preferred consistent, facility-wide guideline implementation efforts. However, some facilities allowed users to choose how they would implement a new guideline or computer system. This practice caused considerable tension between those who were required to use an innovation and those who might choose to use it. Stakeholders spoke often about user-friendly programs that enabled clinical use of the guidelines. In addition, administrators noted that computers promoted local adaptation of national protocols and allowed guideline sharing between geographically distant facilities.
Guideline maintenance
Administrators alone stated that computers facilitated the long-term use of CPGs within a facility. The primary mechanism by which this process occurred was by assuring health professionals' adherence to evidence-based protocols. Administrators additionally suggested that updating patient care data frequently and providing “custom fit” information for a clinic or health provider aided guideline maintenance efforts.
Computer literacy
Participants in all stakeholder groups believed that low computer literacy or the degree of comfort and capability with information technology was a barrier to guideline use. People with weak computer skills were frustrated when new documentation tasks were added to their clinical responsibilities. Physicians and administrators acknowledged that staff needed considerable education on evidence-based guidelines and informatics. Nevertheless, physicians were concerned about the lack of compensated computer in-service opportunities. Nurses were the only group to report that their strong computer skills aided guideline efforts.
Resources
Administrators viewed organizational resources as barriers to effective guideline use. Insufficient budgets to purchase computers and an inadequate supply of human and technological capital to bolster guideline program efforts were commonly cited concerns.
System Designs Domain
This domain delineated four factors related to computer hardware, software/programming, and system capabilities: accessibility, essential data, charting formats, and computer glitches. Again, the administrator focus groups discussed the facilitative aspects of system designs themes more often than physician or nurse focus groups.
Accessibility
Accessibility is the freedom and opportunity to log onto computers and employ guideline-related features such as charting formats, decision support tools or Web-based references. All stakeholder groups agreed that access to such basic features promoted guideline use. However, nurses felt their limited access impeded guideline use. Many nurses were denied entry to basic computer features, such as the Internet, e-mail, or charting screens. In contrast to administrators and physicians who accessed personal desktop computers, nurses shared computer terminals in a central location. Nurses stated that completing their extensive documentation in a timely manner was challenging as the computers to which they did have access had less than optimal processing speeds and were not located at the point of contact with patients. These situations resulted in poor clinical workflow and caused delays in patient care.
Essential data
All stakeholder groups were concerned about the type, amount, and accuracy of the clinical information being documented. Participants wanted to collect high-quality data that are both accurate and complete but with only the minimal amount of data required for clinical decision making. Finding this data balance point was not easy, as illustrated by a common concern: the documentation of services received outside the VA system. Nurses and physicians hesitated to document self-reported patient data such as a vaccination received at a community flu clinic, even though medical errors might occur without this information.
Charting formats
Administrators were uniquely positive among all stakeholders in regard to the facilitative role of standardized charting formats for promoting guideline initiatives. In their discussions, the goal of administrators was to embed evidence-based documentation templates within the computer to structure the recording and presentation of patient health data.
Computer glitches
Computer glitches, or situations in which the computer responded in a way that the user did not anticipate, were barriers to guideline use. Physicians complained that previously collected patient data were not incorporated into the current problem lists making treatment decisions difficult. Other common problems were charting formats that did not mimic the clinical encounter, recognize valid data, or include adequate free text space. Administrators also were concerned about the implications of such glitches for guideline use.
Personal Concerns Domain
The personal concerns domain related to participants' idiosyncratic issues with information technologies. Four themes including time, workload, attitudes, and computer complaints comprised this domain. Eighty-five percent of stakeholders' comments about their relationships with computers were barrier statements. Nurses (46%) and physicians (34%) expressed numerous personal concerns, whereas administrators (20%) tended to downplay the effects of these themes on guideline implementation and use.
Time and workload
Administrators, physicians, and nurses agreed that implementing clinical guidelines took time. However, only physicians and nurses recognized that guideline responsibilities and computerized documentation added to their workload, and the computer, rather than freeing up time for patient care, pulled professionals away from interactions with patients. For physicians, typing orders and notes instead of dictating impinged on the number of patients that they could visit during clinic. Nurses, however, attributed their additional workload to environmental designs that caused inefficient workflow. Computer workstations located far from patient rooms made point-of-contact charting impossible. In addition, insufficient numbers of computers caused charting backups during shift changes and other peak times of the day.
Attitudes
Physicians and nurses agreed that their attitudes toward computers were important barriers to guideline use. Physicians recounted their lack of motivation to learn the computer, implement computerized guidelines, or change their current behaviors to keep in step with constantly changing scientific evidence. Nurses and other clinicians discussed their general misgivings about using computers to deliver patient care, citing the intrusive nature of computer technology that provided an unwanted barrier between themselves and their patients.
Computer complaints
Nurses and other clinicians articulated many computer features that make them ill-fitting tools for human bodies and minds. Health-related computer complaints included eyestrain, carpal tunnel syndrome, and other repetitive stress injuries. Other concerns were related to work style preferences. Examples included frustration while waiting for slow computers to catch up with one's thoughts, being forced to type rather than write progress notes and orders, and the lack of voice-activated equipment for dictating patient care activities.
Discussion
In this paper, we describe areas of congruence and variation in health professionals' views of the role of information technology in CPG implementation. Understanding the areas that stakeholders agree on informs organizations of specific strengths and weaknesses of their CPG implementation processes. For example, physicians, nurses, and administrators agree that widespread accessibility to computers and online guideline features will facilitate long-term guideline initiatives. Similarly, examining divergence in stakeholders' beliefs about computerized guidelines is also important as this signals miscommunication between key user groups. For instance, physicians and nurses expressed similar concerns regarding the additional workload clinical guidelines bring to their busy schedules. However, administrators failed to acknowledge that the extra documentation tasks that accompany guideline implementation projects are barriers to guideline use. Health care organizations must address the concerns of the clinical staff to ensure guideline success.
Consideration of the subtle patterns in participants' perceptions can reveal where points of conflict affecting guideline implementation efforts exist. In our study, administrators, nurses, and physicians recognized that access to basic computer features (charting templates, e-mail, and the Internet) is essential to successful guideline implementation. However, only physicians and administrators enjoyed unlimited access to these crucial programs. Nurses and other clinicians reported that limited access to computers and evidence-based guidelines not only hindered their own ability to deliver quality health care but also impeded physician workflow. Paradoxically, the stakeholder group with the least access to computers—the nursing staff—was the only group that considered their own computer literacy skills as a facilitator of guideline initiatives.
What does the clinical and administrative staff desire from the information systems that support clinical guideline projects? Foremost is an overall improvement in the function of many computer features. Clearly, administrators, physicians, and nurses are less than satisfied with the methods by which documentation of current guideline initiatives occurs. Focusing charting tasks on the collection of essential data is a start. Expanding data input and data retrieval options to include voice-based recording in addition to keyboarding was strongly encouraged. Practitioners with prescriptive authority also desired improvements in order entry systems.
Next, a rearrangement of the physical and virtual spaces of the hospital is needed to make guideline use effortless. Administrators mentioned standardized charting formats embedded into the computer as one method to accomplish this task. However, without access to such templates, the considerable amounts of patient care data gathered by nurses and other clinicians will not be available to the decision support features that the three stakeholder groups agree will facilitate guideline use. Further, unless there are adequate numbers of computer stations located in areas where physicians, nurses, and other clinicians do their work, much of the information needed for decision making will not be incorporated into the electronic patient record in the first place.
Finally, health care organizations must provide basic and ongoing training in clinical guidelines and information technologies to ensure quality patient care. Writing a computer program is one thing; changing the human mind that is interacting with that computer program is an entirely different proposition. The majority of the participants in this study were educated before the advent of clinical guidelines or information technologies as a part of clinical practice. Without a theoretical understanding of the intent of a guideline and a technical competence with the computers used to support it, physicians, nurses, and administrators will be limited in their ability to positively influence patient care outcomes through evidence-based practice.
Limitations
Our primary research aim was to identify key organizational factors associated with effective guideline use in VAMCs among three stakeholder groups: administrators, physicians, and nurses. Our focus group discussion guide did not specifically elicit information about the roles of information technologies in guideline implementation. Nevertheless, participants employed in both administrative and clinical positions, working at different hospitals with varying levels of competence in evidence-based health care and geographically distributed across a wide area frequently and spontaneously mentioned computer technology as facilitators or barriers to the guideline implementation process. The themes identified in this study thus provide a basis for further research on health workers' attitudes toward the computerization of clinical guidelines. We also recommend that future work on this topic include information technology specialists as key stakeholders who might provide different perspectives regarding facility-wide adoption of information systems and practice guidelines.
The purpose of the parent study was to examine factors associated with effective CPG implementation within VAMC hospitals. In our initial analysis, information technology emerged as a major domain for both the facilitators of and barriers to guideline implementation efforts. Further analysis of the perceptions that interdisciplinary teams of guideline users hold toward computers was warranted. However, because information technology was not the focus of the parent study and we had not made the a priori assumption of the importance of information technology factors, we did not collect data on all organizational characteristics that may have been of interest. For example, many themes that were identified in our analysis, such as physician dictation, inconsistent implementation of CPGs within hospitals and across health systems, the type and distribution of computers within facilities, participants' level of access to basic features of the computer or online clinical guidelines, and the computer literacy levels of participants were not collected. Subsequent research incorporating pertinent organizational data should prove fruitful.
Finally, our study focused on guideline initiatives in acute care VAMC hospitals. The VHA, the national health care system in which this study took place, is notable for use of an advanced electronic patient record, regular system-wide implementation of CPGs, and audit and feedback of performance measures. In settings where these innovations are not supported at the institutional level, professionals may express different opinions about the role of computers in guideline implementation and maintenance.
Conclusion
In this study, we identified many issues that health care professionals hold regarding the role of information technologies in CPG implementation, maintenance, and adherence. Administrators, physicians, and nurses recognize that computer accessibility and consistent guideline implementation of protocols and informatics systems facilitate the successful implementation of practice guidelines in acute care settings. These stakeholder groups also described many barriers to computerized guideline use. Factors related to computer tasks and glitches, poor-quality data, computer illiteracy, time and workload issues, and haphazard guideline implementation undermine organizational pushes to improve health care quality and patient outcomes. Further, two highly promoted innovations, decision support systems and electronic patient records, received mixed reviews from all three participant groups.
Health care information technologies hold considerable promise for CPGs use. However, a number of potential barriers to effective guideline use will require systematic approaches to overcome. Although administrators, physicians, and nurses share many concerns about the barriers to adopting guidelines into practice, our results also delineate differences in stakeholders' opinions about implementation initiatives. The key difference is that administrators are convinced that computers are facilitators of CPGs, whereas physicians and nurses remain skeptical of their utility. The particular strengths and concerns of various stakeholders merit attention as each makes essential contributions to patient outcomes. The perceptions discussed by the key stakeholders in this study suggest important opportunities for training, resource allocation, workplace design, and adaptation of present information systems to maximize facilitators and overcome barriers associated with computer technology in delivering evidence-based patient care.
Portions of this paper were presented at the Midwest Nursing Research Society Annual Research Conference, April 4–7, 2003, Grand Rapids, MI.
Supported by the Department of Veterans Affairs, Veterans Health Administrations, Health Services Research and Development Service, Quality Enhancement Research Initiative (QUERI), Investigator Initiated Research Grants #CPI 99-126 and #CPI 01-141, awarded to Dr. Doebbeling. Ms. Lyons's work was supported by an institutional training grant from the National Institutes of Health, National Institute of Nursing Research (NINR), Research Training in Gerontological Nursing, Grant #T32 NR07058, awarded to Dr. Tripp-Reimer and by an Individual NRSA Fellowship Grant #F31 NR008081 from NINR.
The authors thank Nancy Goldsmith, BA, Program Associate, Office for Nursing Research, University of Iowa College of Nursing, for her insightful contributions. The participation of health care professionals and administrators in the data collection, the support of the Network Directors and Quality Managers, and the opportunity to work with The Department of Veterans Affairs Office of Quality and Performance, the Office of Information Technology, Health Services Research and Development QUERI Program, and National Clinical Practice Guideline Council are greatly appreciated.
References
- 1.Clancy C, Scully T. A call to excellence: how the federal government's health agencies are responding to the call for improved patient safety and accountability in medicine. Health Affairs. 2003;22:113–5. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine. The Computer-based Patient Record: An Essential Technology for Health Care. Washington, DC: National Academy Press, 1991.
- 3.Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press, 2000.
- 4.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press, 2001. [PubMed]
- 5.Agency for Healthcare Quality and Research. Making Health Care Safe: A Critical Analysis of Patient Safety Practices. Rockville, MD: AHRQ, 2001.
- 6.American Nurses Association. Position Paper on Computer-based Patient Record Standards. Washington, DC: American Nurses Association, 1995.
- 7.Eagle KA, Garson AJ, Beller GA, Sennett C. Closing the gap between science and practice: the need for professional leadership. Health Affairs. 2003;22:196–201. [DOI] [PubMed] [Google Scholar]
- 8.Joint Commission on Accreditation of Healthcare Organizations. New safety and error reduction standards for hospitals. Joint Commission Perspectives. 2001;21:1–3. [PubMed]
- 9.Mello MM, Studdert DM, Brennan TA. The Leapfrog standards: ready to jump from marketplace to courtroom? Health Affairs. 2003;22:46–59. [DOI] [PubMed] [Google Scholar]
- 10.Bakken S. An informatics infrastructure is essential for evidence-based practice. J Am Med Inform Assoc. 2001;8:199–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flanagan JR, Doebbeling BN, Dawson JD, Beekmann SE. Randomized study of on-line vaccine reminders in adult primary care. Proc AMIA Symp. 1999:755–9. [PMC free article] [PubMed]
- 12.Overhage JM, Perkins S, Tierney WM, McDonald CJ. Controlled trial of direct physician order entry: effects on physicians' time utilization in ambulatory primary care internal medicine practices. J Am Med Inform Assoc. 2001;8:361–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schriger DL, Baraff LJ, Rogers WH, Cretin S. Implementation of clinical guidelines using a computer charting system. Effect on the initial care of health care workers exposed to body fluids. JAMA. 1997;278:1585–90. [PubMed] [Google Scholar]
- 14.Schriger DL, Baraff LJ, Buller K, et al. Implementation of clinical guidelines via a computer charting system: effect on the care of febrile children less than three years of age. J Am Med Inform Assoc. 2000;7:186–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berner ES, Maisiak RS. Influence of case and physician characteristics on perceptions of decision support systems. J Am Med Inform Assoc. 1999;6:428–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown SH, Coney RD. Changes in physicians' computer anxiety and attitudes related to clinical information system use. J Am Med Inform Assoc. 1994;1:381–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cork RD, Detmer WM, Friedman CP. Development and initial validation of an instrument to measure physicians' use of, knowledge about, and attitudes toward computers. J Am Med Inform Assoc. 1998;5:164–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murff HJ, Kannry J. Physician satisfaction with two order entry systems. J Am Med Inform Assoc. 2001;8:499–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pabst MK, Scherubel JC, Minnick AF. The impact of computerized documentation on nurses' use of time. Comput Nurs. 1996;14:25–30. [PubMed] [Google Scholar]
- 20.Miller A, Jeffcote R. Practice nurses and computing: some evidence on utilization, training, and attitudes to computer use. Health Inform J. 1997;3:10–6. [Google Scholar]
- 21.Murphy CA, Maynard M, Morgan G. Pretest and post-test attitudes of nursing personnel toward a patient care information system. Comput Nurs. 1994;12:239–44. [PubMed] [Google Scholar]
- 22.Axford RL, Carter BE. Impact of clinical information systems on nursing practice. Nurses' perspectives. Comput Nurs. 1996;14:156–63. [PubMed] [Google Scholar]
- 23.Bongartz C. Computer-oriented patient care: a comparison of nurses' attitudes and perceptions. Comput Nurs. 1988;6:204–10. [PubMed] [Google Scholar]
- 24.Dumas JA, Dietz EO, Connolly PM. Nurse practitioner use of computer technologies in practice. Comput Nurs. 2001;19:34–40. [PubMed] [Google Scholar]
- 25.Getty M, Ryan AA, Ekins MLC. A comparative study of the attitudes of users and non-users towards computerized care planning. J Clin Nurs. 1999;8:431–9. [DOI] [PubMed] [Google Scholar]
- 26.Murray MD, Loos B, Tu W, Eckert GJ, Zhou XH, Tierney WM. Effects of computer-based prescribing on pharmacist work patterns. J Am Med Inform Assoc. 1998;5:546–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anderson RM, Donnelly MB, Hess GE. An assessment of computer use, knowledge, and attitudes of diabetes educators. Diabetes Educ. 1992;18:40–6. [DOI] [PubMed] [Google Scholar]
- 28.Lewis D. Current computer use by diabetes educators. Diabetes Educ. 2001;27:239–44. [DOI] [PubMed] [Google Scholar]
- 29.Unsworth CA, Townsend MC. Occupational therapists' skills and attitudes regarding use of computers and assistive technology. Occup Ther Int. 1997;4:52–65. [Google Scholar]
- 30.Walter G, Cleary M, Rey JM. Patterns of use, attitudes and expectations of mental health staff regarding computers. J Qual Clin Pract. 2000;20:20–3. [DOI] [PubMed] [Google Scholar]
- 31.Henderson RD, Deane FP. User expectations and perceptions of a patient management information system. Comput Nurs. 1996;14:188–93. [PubMed] [Google Scholar]
- 32.Weiner M, Gress T, Thiemann DR, et al. Contrasting views of physicians and nurses about an inpatient computer-based provider order-entry system. J Am Med Inform Assoc. 1999:234–44. [DOI] [PMC free article] [PubMed]
- 33.Lee F, Teich JM, Spurr CD, Bates DW. Implementation of physician order entry: user satisfaction and self-reported usage patterns. J Am Med Inform Assoc. 1996;3:42–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shumway JM, Jacknowitz AI, Abate MA. Analysis of physicians', pharmacists', and nurses' attitudes toward the use of computers to access drug information. Methods Inf Med. 1990;29:99–103. [PubMed] [Google Scholar]
- 35.Travers D, Downs S. Comparing user acceptance of a computer system in two pediatric offices: a qualitative study. Proc AMIA Annu Symp. 2000:853–7. [PMC free article] [PubMed]
- 36.Doebbeling B, Vaughn T, Woolson R, et al. Benchmarking Veterans Affairs Medical Centers in the delivery of preventive health services: comparison of methods. Med Care. 2002;40:540–54. [DOI] [PubMed] [Google Scholar]
- 37.Patton MQ. Qualitative Research & Evaluation Methods. , 2nd ed. Newbury Park, CA: Sage, 1990.
- 38.Morgan DL. Focus Groups as Qualitative Research. , 2nd ed. Newbury Park, CA: Sage, 1996.
- 39.Bailey KD. Methods of Social Research. , 4th ed. New York: Free Press, 1994.
- 40.Crabtree BF, Miller ML. Using codes and code manuals: A template organizing style of interpretation. In: Crabtree BF, Miller WL (eds). Doing Qualitative Research, 2nd ed. Thousand Oaks, CA: Sage, 1999.
- 41.Miles MB, Huberman M. Qualitative Data Analysis: An Expanded Sourcebook. , 2nd ed. Thousand Oaks, CA: Sage, 1994.


