Abstract
Mutations in the vacuolar protein sorting 35 ortholog (VPS35) gene encoding a core component of the retromer complex, have recently emerged as a new cause of late-onset, autosomal dominant familial Parkinson’s disease (PD). A single missense mutation, AspD620Asn (D620N), has so far been unambiguously identified to cause PD in multiple individuals and families worldwide. The exact molecular mechanism(s) by which VPS35 mutations induce progressive neurodegeneration in PD are not yet known. Understanding these mechanisms, as well as the perturbed cellular pathways downstream of mutant VPS35, is important for the development of appropriate therapeutic strategies. In this review, we focus on the current knowledge surrounding VPS35 and its role in PD. We provide a critical discussion of the emerging data regarding the mechanisms underlying mutant VPS35-mediated neurodegeneration gleaned from genetic cell and animal models and highlight recent advances that may provide insight into the interplay between VPS35 and several other PD-linked gene products (i.e. α-synuclein, LRRK2 and parkin) in PD. Present data support a role for perturbed VPS35 and retromer function in the pathogenesis of PD.
Keywords: VPS35, retromer, Parkinson’s disease (PD), endosomal sorting, mitochondria, autophagy, lysosome, α-synuclein, LRRK2, parkin
INTRODUCTION
Parkinson’s disease (PD), a common progressive neurodegenerative movement disorder, belongs to the family of synucleinopathies that are characterized by the accumulation of aggregated α-synuclein protein. PD affects approximately 1.8% of individuals over the age of 65 years, increasing to ∼5% over 85 years [1, 2]. PD is predominantly an idiopathic disease with the largest risk factor simply being age, however, up to 10% of cases occur in a familial manner with both autosomal dominant and recessive transmission [3]. PD is clinically characterized by the development of the cardinal motor symptoms, bradykinesia, resting tremor, rigidity and postural instability, owing to the relatively selective degeneration of nigrostriatal pathway dopaminergic neurons [1, 2]. Neuropathologically, PD is typically characterized by dopaminergic neuronal loss in the substantia nigra pars compacta (resulting in reduced dopamine levels in the caudate-putamen) accompanied by reactive gliosis, and by the presence of intracytoplasmic, eosinophilic inclusions termed Lewy bodies in surviving brainstem neurons, a major component of which is fibrillar forms of α-synuclein [1, 2].
The etiology of PD remains obscure. In the past two decades, our understanding of the mechanisms underlying the pathogenesis of PD has undergone a remarkable transformation, mainly due to the identification of distinct genetic loci at which mutations are linked to disease [3]. Familial PD is caused by mutations that are inherited in an autosomal dominant (SNCA, LRRK2 [5, 6], VPS35 [7, 8], RAB39B [9], TMEM230 [10]) or autosomal recessive (Parkin [11], PINK1 [12], DJ-1 [13], ATP13A2 [14], PLA2G6 [15], FBX07 [16], DNAJC6 [17], SYNJ1 [18, 19]) manner. In addition to being implicated in the development of inherited PD, common genetic variation at the SNCA and LRRK2 loci confer risk for developing idiopathic PD [3, 20]. Furthermore, mutations in the lysosomal gene product, glucocerebrosidase (GBA), represent a major risk factor for PD [3]. These gene products and their disease-associated mutations have been shown to regulate several cellular pathways, including mitochondrial turnover, synaptic vesicle exocytosis/endocytosis, endosomal sorting, autophagy and lysosomal function [21–23]. Accordingly, a common theme has emerged that involves perturbations in organelle/vesicle trafficking, recycling and turnover that may be central to the pathophysiology of PD.
IDENTIFICATION OF VPS35 MUTATIONS IN PD
In 2008, Wider and colleagues initially reported a Swiss family with late-onset, autosomal dominant PD with a mean age of disease onset of 51 years. The clinical phenotype was slowly progressive, tremor-predominant and levodopa-responsive parkinsonism [24]. In 2011, Vilariño-Güell and coworkers applied next-generation sequencing technology to this Swiss PD family. Utilizing exome sequencing an aspartic acid to asparagine mutation at residue 620 (D620N) (p.Asp620Asn, c.1858G>A) was identified in the vacuolar protein sorting 35 ortholog (VPS35, PARK17, OMIM 614203) gene in all six affected family members who were available for genetic testing [7]. The D620N mutation was also identified in PD families from the United States, Tunisia and Israel (Yemenite Jews) and in one idiopathic PD subject of Yemenite Jewish origin [7]. An independent study identified three Austrian families harboring the D620N mutation in VPS35 that presented with levodopa-responsive PD occasionally accompanied by action tremor [8].
Following the initial reports of VPS35 mutations, other groups have been able to identify the D620N mutation in a number of individuals and families with PD worldwide (Table 1) [25–31]. At this time, only the VPS35 D620N mutation has been confirmed as pathogenic. The VPS35 D620N mutation has been identified predominantly in families of Caucasian descent with autosomal dominant PD. In contrast, VPS35 mutations are rare in Asian populations with the exception of Japanese populations [32]. The frequency of the VPS35 D620N mutation in patients with familial PD is estimated to be 0.1 to 1% [25].
Table 1.
Summary of the distribution and frequency of VPS35 variants linked to Parkinson’s disease
| Mutation | Region where mutation was present | Frequency in PD cohorts | Found in controls? | References |
| D620N | Switzerland | 24/14126 | No | [7, 8, 26–28, 86] |
| Austria | ||||
| United States | ||||
| Tunisia | ||||
| Yemenite Jews | ||||
| United Kingdom | ||||
| France | ||||
| Japan | ||||
| Germany | ||||
| Others | ||||
| P316S | United States | 2/106 | Yes (1/3309) | [7] |
| R524W | Austria | 1/860 | No | [8] |
| L774M | Austria | 8/9730 | Yes (3/7527) | [8, 27] |
| Germany | ||||
| R32S | Spain | 1/134 | Unknown | [31] |
| I560T | Belgium | 1/592 | No | [29] |
| H599R | Belgium | 1/592 | No | [29] |
| M607V | Belgium | 1/592 | No | [29] |
| G51S | Korea | 5/9495 | Yes (2/6513) | [27, 30] |
| Norway | ||||
| Others |
Analyses of the entire VPS35 gene sequence has also revealed a proline to serine substitution at amino acid 316 (P316S) in two affected siblings with PD from a US family (Table 1) [7]. However, the pathogenicity of the P316S variant is uncertain since it was also found in an unaffected sibling in the same family. Additional human genetic and functional studies are therefore warranted to establish whether the P316S variant represents a pathogenic mutation, a risk variant or a rare benign polymorphism. Several additional rare variants have also been identified (i.e. R32S, R524W, I560T, H599R and M607V) in individual PD subjects however their pathogenicity remains inconclusive (Table 1) [25]. Therefore, the D620N mutation represents the only confirmed pathogenic VPS35 variant identified to date.
The clinical symptoms and neuroimaging (i.e. DAT SPECT or Fluorodopa PET) of VPS35-linked PD subjects suggests a classical disease spectrum similar to idiopathic PD [7, 8, 24, 25]. PD subjects harboring VPS35 mutations present clinically with at least 3 of 4 cardinal motor symptoms. Subjects occasionally exhibit action tremor and mild cognitive impairment. All of the reported subjects have responded to levodopa therapy [25, 33]. Given that VPS35-linked PD is clinically and neurochemically indistinguishable from idiopathic PD [3, 33], it would be important to evaluate the neuropathology of PD subjects with VPS35 mutations to confirm whether nigral neurodegeneration and Lewy body pathology similarly form part of the disease spectrum. The neuropathological features of VPS35-linked PD are not yet known since only a single D620N mutation carrier with PD has been assessed at autopsy [24]. The incomplete neuropathological examination of only parts of the cortex and basal ganglia (excluding the brainstem) in this subject did not reveal any signs of Lewy body disease or α-synuclein immunoreactivity in these areas [24]. Therefore, it remains to be determined whether VPS35 mutations lead to PD with classical brainstem Lewy body pathology.
VPS35 AND THE RETROMER
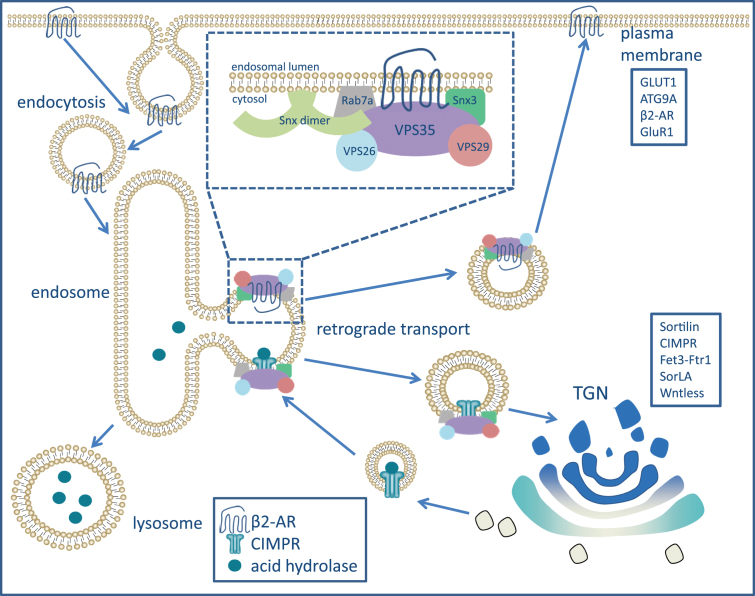
The VPS35 protein functions as a core subunit of a heteropentameric complex referred to as the retromer (Fig. 1) [34]. Originally identified in yeast, the retromer is a protein complex that associates with the endosome to facilitate both endosome-to-Golgi complex and endosome-to-plasma membrane transport and recycling of transmembrane protein cargo [35–37]. In the seminal studies that identified and characterized the retromer, sorting of the VPS10 receptor between the endosome and trans-Golgi network (TGN) by the retromer was shown to be important for the delivery of acid hydrolases to the endosome for their eventual delivery to the lysosome [36, 37]. The retromer is conserved from yeast to mammals in addition to being involved in discrete cellular pathways that may play a role in disease [34].
Fig.1.
Retromer-regulated retrograde transport of endosomal-associated protein cargo. The retromer, along with retromer-associated proteins that assist in membrane binding (Snx3 and Rab7a), is responsible for the retrograde transport of several cargo proteins from the endosomal network to either the trans-Golgi network (TGN) or the plasma membrane. VPS35, along with VPS26 and VPS29, sit at the endosomal membrane and recognize cargo (transmembrane proteins) to be sorted. Two canonical cargo proteins that the retromer is responsible for transporting are the mannose-6-phosphate receptor (CI-MPR) and the β2-adrenergic receptor (β2-AR). These two examples demonstrate the two major routes of transport that are facilitated by the retromer [34]. CI-MPR is responsible for delivering acid hydrolases (cathepsin D, for example) to the endosome for eventual delivery to the lysosome. While other mechanisms are responsible for delivering CI-MPR with its ligand to the endosome, the retromer facilitates the retrieval of CI-MPR to the TGN to bind more ligand, which will eventually make its way to the endosome once again [85]. On the other hand, β2-AR is recycled from the endosome to the plasma membrane where it will stay until activated. Although the retromer is not responsible for the initial endocytosis of β2-AR at the plasma membrane, its role in recycling the receptor back to the plasma membrane prevents it from lysosomal degradation [48].
The retromer is commonly divided into two subcomplexes: a cargo-selective complex trimer (CSC) and a sorting nexin (SNX) dimer (Fig. 1). The CSC is composed of VPS26, VPS29 and VPS35 and is responsible for binding to and sorting protein cargo [34, 38]. Of the CSC proteins, VPS35 is the largest, being composed of 796 amino acids. Structural studies of VPS35 reveal a highly flexible protein that forms an α-solenoid fold that extends throughout the entire length of the protein. The α-solenoid fold is important in the binding of VPS29, whose structure includes a metallophosphoesterase fold that binds to the C-terminal end of VPS35 [39]. The N-terminal portion of VPS35 is responsible for binding to VPS26 through a PRLYL motif [40]. The CSC associates with a SNX dimer that canonically consists of SNX1 or SNX2 and SNX5 or SNX6 in mammalian cells (SNX5 and SNX17 in yeast). These SNX proteins are members of the SNX-BAR family which consist of both a Bin-Amphiphysin-Rvs (BAR) and phox homology (PX) domain that aid in retromer association with the endosomal membrane [34, 39]. Specifically, the BAR domain aids in sensing membrane curvature and possibly in membrane remodeling [35]. The PX domain binds to phosphatidylinositol 3-phosphate (PI3P) on the membrane. PI3P production occurs through the activity of the class III phosphoinositide 3-kinase (PI3K) VPS34, which is regulated by Beclin1 (or VPS30 in yeast) and RAB5 [41, 42]. Once activated, VPS34 phosphorylates phosphatidylinositol resulting in the production of PI3P in the endosomal membrane, which can recruit downstream targets including RAB7A and SNX proteins [41]. Structurally, the CSC cannot sustain a sufficiently strong interaction with the SNX dimer to establish association with the endosome, so RAB7A serves as an additional anchor for retromer association with the endosomal membrane (Fig. 1) [34].
In addition to its major association with a SNX dimer and RAB7A, a small proportion of the CSC can interact with other proteins that demonstrate the importance of the retromer in discrete endosomal sorting pathways. For example, the retromer can associate with the Wiskott-Aldrich syndrome and SCAR homolog (WASH) complex, which is composed of WASH1, strumpellin, FAM21, CCDC53 and KIAA1033/SWIP, and adaptor proteins such as SNX27, to facilitate both the endosome-to-TGN and endosome-to-plasma membrane transport of cargo [43–45]. The WASH complex functions to facilitate the formation of actin patches on the endosomal membrane that generate distinct domains to which cargo are partitioned for transport to the TGN or plasma membrane. The WASH complex associates with the retromer via an interaction between the unstructured tail of FAM21 and the C-terminus of VPS35, and this interaction mediates the endosome-to-TGN retrieval of select cargo such as the cation-independent mannose 6-phosphate receptor (CI-MPR) [44]. Alternatively, the WASH complex can associate with the retromer and SNX27 to facilitate the endosome-to-plasma membrane retrieval of specific cargo including the β2-adrenergic receptor (β2AR), the glucose transporter 1 (GLUT1) and several metal ion transporters [35, 45]. All of the interactions with the retromer reported thus far are dependent on the association of the SNX-BAR dimer with the CSC, however, SNX3 which lacks a BAR domain, can bind to the CSC and facilitate endosome-to-TGN retrieval primarily of the Wntless protein independent of the SNX-dimer [46, 47]. Therefore, the interactions with and within the retromer are multiple and diverse with different subcomplexes most likely serving to mediate the retrieval of specific cargo to distinct vesicular compartments.
Retromer function is clearly important for the transport and recycling of numerous transmembrane cargo from the endosome to the TGN or plasma membrane in a diverse number of cells and tissues, however, the distinct role of the retromer in cells of the central nervous system (CNS) is incompletely understood. Choy et al. [48] identified the retromer as an important mechanism for membrane protein transport to the dendritic processes of neurons. Choy and colleagues demonstrated that the retromer was responsible for the distribution of membrane proteins to the post-synaptic compartment (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid [AMPA] and N-methyl-D-aspartate [NMDA] receptors) and to extra-synaptic locations (β2AR) along the dendrite [48]. Whether the dendritic sorting of receptors is altered in neurodegenerative disease, specifically in PD, remains unclear. However, over the last few years, several studies have suggested a specific role for the retromer in PD.
FUNCTIONAL INSIGHT INTO PD-ASSOCIATED VPS35 MUTATIONS
Evidence for VPS35-induced pathogenicity
While the identification of disease-associated missense mutations in VPS35 suggests dysfunction of the retromer complex as a contributor to PD, our understanding of the molecular and cellular mechanisms of VPS35-dependent neurodegeneration is still rather limited. The absence of truncation, rearrangement or deletion mutations in the VPS35 gene and the dominant inheritance pattern of mutations in PD, suggest that heterozygous VPS35 mutations could potentially act via either i) a toxic gain-of-function mechanism, ii) a dominant-negative mechanism (with a partial or full loss-of-function effect) or iii) via a haploinsufficient mechanism (creating a partial loss-of-function). Distinguishing between these possibilities for the pathogenic effects of disease-causing mutations is rarely simple and is often rather complicated especially when more than one mechanism may be involved. Experimental studies using cell-based and in vivo models (i.e. mice, rats, worms and flies; Table 2) of mutant VPS35-induced neuronal damage have so far provided important clues to the potential function(s) of VPS35, the cellular pathways that are potentially perturbed in PD, and have identified functional interactions with known PD-linked gene products.
Table 2.
Summary of pathological features of animal models of VPS35-linked PD
| Model | Construct | Motor phenotype | Neuropathology | Cellular pathology | Reference |
| mouse KO (germline) | VPS35+/– | ↓ performance in open field test (12 and 18 months) | ∼20% DA neuron loss by12 months | ↓ LAMP2a resulting in ↑ α-syn in DA neurons | [60] |
| ↑ α-syn levels in VM | |||||
| mouse cKO | VPS35–/–/DAT-Cre | ↓ performance in open field test | ↓ DA neurons by 2–3 months | ↓ levels of MFN2 resulting in impaired mitochondrial fusion | [56] |
| Weak/unsteady gait | ↑ α-syn levels in VM | ||||
| ↓ hindlimb stepping | |||||
| mouse KI (D620N) | VPS35D620N/D620N | None (∼5 months) | None (∼5 months) | ↓ evoked striatal dopamine release | [62] |
| mouse viral-mediated gene transfer | Lentiviral vector expressing human VPS35D620N | Unknown | ↓ in DA neurons compared to contralateral side | ↑ mitochondrial fragmentation | [57] |
| rat viral-mediated gene transfer | AAV2/6-VPS35D620N (human) | None | ∼30% DA neuron loss (12 weeks post-injection) | Neurite degeneration (Gallyas silver) | [54] |
| C. elegans deletion mutant | KN555 vps-35 (hu68) II | Unknown | impaired DA9 formation in the presence of A53T α-syn expression | genetic interaction of VPS35 and α-syn | [80] |
| Drosophila transgenic | ddc-Gal4 or GMR-Gal4/UAS-VPS35 | Unknown | Unknown | Rescues mutant LRRK2 eye and locomotor phenotypes, protects against rotenone toxicity | [76] |
| Drosophila transgenic | ddc-Gal4/UAS-huVPS35D620N | ↓ climbing ability | ↓ in DA neurons at 60 days in PPL cluster | ↑ sensitivity to rotenone toxicity | [58] |
| da-Gal4 or hedgehog-Gal4/UAS- huVPS35D620N | Slight ↓ in lifespan | Rescues parkin KO phenotypes | [83] | ||
| Drosophila KO | vps35MH20/vps35E42 | Larval locomotion defects | Defects in NMJ development | Mild eye disorganization in α-syn transgenic flies | [49, 83] |
| RNAi-mediated VPS35 silencing | larval stage lethality | Exacerbates α-syn transgenic fly locomotor impairment | |||
| melanotic masses |
Abbreviations: KO, knockout; cKO, conditional knockout; KI, knockin; DA, dopaminergic; TH, tyrosine hydroxylase; VM, ventral midbrain; NMJ, neuromuscular junction; α-syn, α-synuclein
VPS35 and the retromer are essential for normal cellular function and viability, however, several studies have demonstrated that both silencing and overexpression of VPS35 is detrimental to cellular health. For example, Drosophila overexpressing both human α-synuclein and RNAi directed against VPS35 demonstrated that depletion of VPS35 resulted in defective α-synuclein lysosomal degradation, mainly due to the impaired recycling of the retromer cargo CI-MPR and the reduced delivery of its ligand cathepsin D to lysosomes [49]. This sorting defect resulted in the enhanced accumulation of insoluble α-synuclein and exacerbated α-synuclein-induced locomotor deficits and compound eye disorganization in flies [49]. These data suggest that reduced retromer levels may disrupt the normal lysosomal degradation of α-synuclein leading to its inappropriate accumulation. Such a mechanism is of particular interest to PD as it may offer one explanation for the accumulation of aggregated α-synuclein in Lewy bodies. Similarly, the endosomal sorting of CI-MPR was reported to be disrupted by the D620N VPS35 mutation in mammalian cells [50–52], although alterations in CI-MPR trafficking have not been consistently reported by all studies including in cultured primary neurons [53–55]. The impact of the D620N VPS35 mutation on the sorting of other retromer cargo has not been extensively studied, with reports suggesting no alterations in the sorting of sortilin-1 and SorLA in primary cortical neurons or patient-derived fibroblasts [53, 54]. In mouse cortical neurons and human iPSC-derived dopaminergic neurons, D620N VPS35 has been reported to alter the localization of the AMPA glutamate receptor, GluR1, to dendritic spines suggesting a role for the retromer in post-synaptic receptor trafficking [53]. Consistent among most studies is the observation that the D620N mutation does not alter the subcellular localization of VPS35, the assembly of the CSC or the stability of retromer components in different cellular models [51, 53–55]. Therefore, the D620N mutation is unlikely to influence all retromer functions but rather may have discrete effects involving select cargo and/or subcellular compartments. Whether or not the altered sorting of CI-MPR, GluR1 or other retromer cargo by D620N VPS35 is required or relevant for neurodegeneration remains to be formally established.
To understand the mechanism through which PD-associated mutations in VPS35 contribute to disease pathogenesis, one study demonstrated that the viral-mediated overexpression of human wild-type (WT) or D620N VPS35 in primary cortical neurons equivalently led to neuronal cell death and impaired neurite outgrowth [54]. WT and D620N VPS35 overexpression also markedly increased neuronal vulnerability to PD-relevant cellular stressors, including the mitochondrial Complex-I inhibitors MPP+ and rotenone [54]. Therefore, both WT and D620N VPS35 expression induce equivalent levels of neuronal damage, and are therefore similarly functional in this model, supporting either a gain-of-function mechanism for the D620N mutation or potentially a dominant-negative mechanism whereby VPS35 overexpression interferes with the endogenous retromer. These effects are further substantiated by in vivo confirmation of the pathogenicity of the D620N mutation by the adeno-associated virus (AAV)-mediated overexpression of human WT and D620N VPS35 in the rat substantia nigra. D620N VPS35 induced marked degeneration of substantia nigra dopaminergic neurons in addition to neurite degeneration compared to a control virus over a 12 week period, with an intermediate effect of WT VPS35 [54]. Recent studies using viral-mediated D620N VPS35 expression confirmed nigral dopaminergic neurodegeneration in rodents, lending further support for a toxic gain-of-function or dominant-negative mechanism for the D620N mutation [56, 57]. In agreement with these rodent studies, the overexpression of human D620N or P316S VPS35 in the Drosophila brain induces modest age-dependent dopaminergic neuronal loss, locomotor deficits and reduced survival compared to control flies with an intermediate effect of WT VPS35 [58]. Additionally, the D620N and P316S mutations exacerbate rotenone-induced dopaminergic neurodegeneration in this fly model compared to WT VPS35 [58]. Therefore, the overexpression of mutant VPS35 in rodent or fly models serves to recapitulate some of the hallmark features of PD. However, it is not yet clear whether the pathogenic effects of the D620N mutation in vivo result from a toxic gain-of-function or a dominant-negative mechanism.
While these in vivo overexpression studies suggest that VPS35 mutations may act through a toxic gain-of-function or a dominant-negative mechanism to induce neurotoxicity, some inconsistencies with this notion have been observed in other models. For example, WT VPS35 overexpression was shown to protect against MPP+-induced toxicity in cultured dopaminergic neurons whereas the D620N mutation partially impairs this protective effect [59]. This observation may suggest that PD-associated VPS35 mutations act via a partial loss-of-function mechanism. While the homozygous deletion of VPS35 in mice results in embryonic lethality, heterozygous knockout (KO) mice exhibit progressive PD-related neurodegenerative phenotypes including nigral dopaminergic neuronal loss, decreased striatal dopamine levels, the accumulation of α-synuclein and motor deficits [60]. Although these KO mice lend some support to a loss-of-function mechanism for VPS35 mutations in PD, KO mice may not accurately model the specific pathogenic effects of PD-linked dominant VPS35 mutations (i.e. D620N) which have not been demonstrated to result in a full loss-of-function effect in the majority of models and assays employed so far. Indeed, many of the normal functions of the retromer remain intact in the D620N VPS35 variant compared to the WT protein [53–55]. Furthermore, whether nigrostriatal pathway dopaminergic neurons are selectively vulnerable compared to other neuronal populations in these VPS35 KO mice is not yet clear but would be important to clarify, especially since the heterozygous deletion of VPS35 also enhances Alzheimer’s disease-like phenotypes of APP-sw transgenic mice (Tg2576) that largely occur in the hippocampus and cortex [61]. Therefore, hippocampal and cortical neurons also appear vulnerable in these heterozygous VPS35 KO mice. While VPS35 mutations are clearly able to induce neurodegeneration in vivo in PD models, the exact molecular mechanism through which they act is not yet known and the cellular pathways and protein interactions that are important for neurodegeneration remain unclear.
Recently, a new D620N VPS35 knockin mouse model was reported that suggested a role for the D620N mutation in impaired striatal dopamine release [62]. Using CRISPR/Cas9 gene-editing, a homozygous knockin mouse line was generated that expressed murine D620N VPS35 at similar levels to the WT protein. The endogenous expression of D620N VPS35 did not alter the stability of VPS35, VPS26 or VPS29 proteins or retromer assembly in brain tissue [62], as supported by several prior studies [53–55]. No evidence was found for altered levels of autophagy markers (LC3-II), cathepsin D species, endolysosomal pathway proteins (GM130, EEA1, LAMP1), mitochondria-associated proteins (VDAC1, Drp1, parkin, Mfn2, MUL1, Tom20) or α-synuclein in the brains of D620N VPS35 knockin mice at ∼5 months of age [62]. Degeneration of the nigrostriatal dopaminergic pathway was not observed at 5 months whereas the level of striatal dopamine and its metabolites where also normal at this early age. However, in vivo microdialysis revealed that evoked striatal dopamine release was modestly impaired in the D620N knockin mice at this age [62]. This study suggests that the D620N mutation may act as a partial loss-of-function by causing an early deficit in dopamine release perhaps prior to the onset of neurodegeneration or neuropathology [62]. While this is an interesting new mouse model, a note of caution is warranted as these studies used extremely small group sizes, a single early time point and did not quantify dopaminergic neuronal number or evaluate neuropathology. Therefore, confirmation of these phenotypes and additional phenotypic analysis of this knockin mouse model with advancing age will be important in future studies.
MECHANISMS OF VPS35-INDUCED NEURODEGENERATION
To date, three potential cellular mechanisms have been proposed to underlie mutant VPS35-induced neurodegeneration: i) impaired binding to the WASH complex resulting in defects in macroautophagy, ii) disrupted AMPA receptor trafficking to dendritic spines, and iii) altered mitochondrial dynamics and turnover. While it remains unclear if these mechanisms are relevant for neurodegeneration or causally related to each other, these studies have provided important insight into cellular pathways that are perturbed by the D620N mutation in VPS35 in neurons.
Impaired WASH complex binding and autophagy defects
Two independent studies have identified impaired binding of the WASH complex to VPS35 in human cell lines caused by the D620N mutation [51, 55]. The D620N mutation confers a decreased affinity of VPS35 for binding to FAM21, an important component of the WASH complex, resulting in the reduced endosomal recruitment of the WASH complex. In one study, the endosomal sorting of CI-MPR and GLUT1 was disrupted by the decreased binding of D620N VPS35 to FAM21 [51]. In the other study, decreased WASH complex binding to D620N VPS35 impaired macroautophagy in cells in part via the abnormal sorting of the autophagy protein ATG9A which decreased autophagosome formation [55]. ATG9A is known to regulate early autophagosome formation although its distinct role in this process remains unclear [55]. Since these studies were conducted in non-neuronal cell lines, it is not yet clear whether defective ATG9A sorting and impaired macroautophagy are required for neuronal damage induced by PD-linked VPS35 mutations or whether impaired WASH complex binding to VPS35 is relevant in cell types of the mammalian brain. Although not directly shown to relate to impaired WASH binding, VPS35 deficiency has also been observed to cause autophagy defects. Tang and colleagues observed that VPS35 deficiency in heterozygous KO mice caused a reduction in LAMP2a, a receptor for chaperone-mediated autophagy (CMA), resulting from its increased lysosomal degradation due to impaired recycling to the TGN [60]. CMA has been shown to regulate the lysosomal degradation of α-synuclein [63]. Reduced LAMP2a levels and presumably impaired CMA resulted in the accumulation of α-synuclein in the brains of heterozygous VPS35 KO mice [60]. Overexpression of human D620N VPS35 in dopaminergic neurons of mice similarly reduced LAMP2a levels and induced the accumulation of α-synuclein [60]. In contrast, studies in rats with the AAV-mediated overexpression of human VPS35 variants failed to observe alterations in α-synuclein levels, phosphorylation or pathology in substantia nigra dopaminergic neurons [54]. Whether CMA defects and the subsequent abnormal accumulation of α-synuclein are responsible for dopaminergic neurodegeneration in the VPS35 KO mice has not been determined but would provide an important validation of this putative mechanism.
Disrupted AMPA receptor trafficking
Retromer is localized throughout the neuron, including within the cell soma, axon and dendrites [48, 53, 60, 64]. VPS35 and the retromer are reported to localize to dendritic spines where they are responsible for binding to and trafficking the AMPA receptor GluR1 [53]. Overexpressed D620N VPS35 does not localize as readily to dendritic spines compared to the WT protein, and induces defective trafficking of GluR1 resulting in altered synaptic transmission [53]. These effects are suggested to support a loss-of-function effect for the D620N mutation, however, other aspects of VPS35 function such as retromer subunit interactions (i.e. with VPS26 and VPS29) and endosomal sorting of several retromer cargo are not affected by the D620N mutation in several studies [54, 55], including this one [53]. These observations might instead suggest a dominant-negative mechanism (i.e. partial loss-of-function) for the actions of the D620N mutation [53–55]. D620N VPS35 overexpression causes GluR1 to mislocalize to the cell surface instead of to dendritic spines [53], which could also be interpreted as a gain-of-function effect.
A recent study also implicates abnormal AMPA receptor trafficking as a consequence of VPS35 loss-of-function similar to the actions of the D620N mutation. Tian and coworkers initially demonstrated impaired dendritic spine maturation in heterozygous VPS35 KO mice [65]. VPS35-depleted neurons exhibit decreased synaptic transmission that may result from abnormal trafficking of both GluR1 and GluR2. Abnormal spine maturation could be rescued by the overexpression of GluR2 but not GluR1, suggesting that abnormal GluR2 trafficking is mainly responsible for this phenotype [65]. WT and mutant VPS35 overexpression in primary cortical neurons has similarly been shown to result in the loss of dendritic spines and synaptic boutons, with more severe effects induced by D620N VPS35 relative to the WT and R524W proteins [57]. Collectively, these studies suggest that the D620N mutation alters the retromer-mediated sorting of GluR1/R2 to dendritic spines and perturbs synaptic transmission and morphology but whether these post-synaptic effects serve to elicit neurodegeneration in vivo is unclear.
Impaired mitochondrial dynamics and function
Mitochondrial dysfunction has been consistently implicated in the pathogenesis of both familial and idiopathic PD. Several mitochondrial processes, including defective mitophagy, mitochondrial DNA mutations, altered mitochondrial dynamics (i.e. fission and fusion), impaired mitochondrial biogenesis or defective calcium homeostasis, are altered by a number of genetic mutations in different PD models [66–68]. VPS35 has recently been implicated in mitochondrial function through its reported role in mediating vesicle transport from mitochondria to peroxisomes or lysosomes by regulating the formation of mitochondrial-derived vesicles (MDVs) [69, 70]. It is not yet known whether the generation and trafficking of MDVs is directly altered by PD-linked VPS35 mutations. A recent study demonstrates that the overexpression of human VPS35 variants induces mitochondrial fragmentation and neuronal loss both in cultured cells (rat cortical neurons, M17 cells and human fibroblasts) and in vivo in mouse substantia nigra neurons, with more pronounced effects induced by D620N relative to WT or R524W VPS35 [57]. These effects could be rescued by inhibition of the mitochondrial fission protein dynamin-like protein 1 (DLP1) with the DLP1 inhibitor mdivi-1 [57], suggesting that VPS35 mutations may cause neurodegeneration by disrupting mitochondrial dynamics and function. VPS35 mutations also induced mitochondrial dysfunction, including increased ROS production, decreased ATP levels, decreased mitochondrial membrane potential and impaired bioenergetics, in different cellular models [57]. The D620N mutation enhances the interaction of VPS35 with DLP1 resulting in its inappropriate recycling, mediated by the enhanced turnover of mitochondrial DLP1 complexes via their MDV-dependent transport to lysosomes for degradation, which most likely results in mitochondrial fragmentation and neuronal loss [57]. Collectively, VPS35 mutations potentially induce neurodegeneration by enhancing DLP1-dependent mitochondrial fission.
VPS35 mutations have also been linked to impaired mitochondrial fusion through their interaction with the mitochondrial E3 ubiquitin ligase 1 (MUL1) [56]. Tang and colleagues, using a conditional KO mouse model with the selective deletion of VPS35 in dopaminergic neurons, observe a reduction of the mitochondrial fusion protein, mitofusin 2 (MFN2), in the ventral midbrain of these mice [56]. Neurons lacking VPS35, both in vitro and in vivo, display increased mitochondrial fragmentation consistent with impaired MFN2-dependent mitochondrial fusion that could be rescued by expression of WT VPS35 but not the D620N mutant [56]. Reduced MFN2 levels were due to its increased ubiquitination and proteasomal degradation resulting from increased MUL1 levels, a known regulator of MFN2 turnover [56]. Silencing MUL1 expression in the brain of VPS35-deficient mice restored MFN2 levels and suppressed dopaminergic neuronal degeneration [56]. Notably, the overexpression of PD-linked VPS35 mutants (D620N, P316S or R524W) and VPS35 deficiency were similarly able to increase MUL1 levels and subsequently reduce MFN2 levels [56]. The mechanism by which VPS35 mutations or loss leads to an increase in mitochondrial MUL1 levels is not known. However, it remains unclear whether mutations in VPS35 cause neurodegeneration in PD through this mechanism, especially since the P316S and R524W mutations have not yet been definitively linked to PD [25]. Additionally, this study suggests that VPS35 mutations act purely through a loss-of-function mechanism, although several of the known functions of the retromer are not compromised by these mutations [51, 53–55]. Although the conditional KO of VPS35 in dopaminergic neurons successfully recapitulates PD-like pathology, this may or may not be relevant to VPS35-linked PD because disease-linked mutations do not globally impair retromer function but rather tend to have discrete effects [51, 53–55]. It is also not yet clear in these VPS35 KO models whether nigrostriatal pathway dopaminergic neurons are selectively vulnerable to VPS35 loss-of-function or whether neurons in general critically require VPS35 for their normal function, maintenance and viability. This selective neuronal vulnerability would be important to clarify, particularly for understanding the specific role of VPS35 in PD, and especially given that germline VPS35 KO mice exhibit early embryonic lethality thus highlighting a critical role for VPS35 in normal physiology [60, 61].
PD-LINKED GENE PRODUCTS THAT INTERACT WITH VPS35
It is conceivable that multiple pathogenic events arising from different genetic mutations in PD could converge on one or more common cellular pathways central to the maintenance or viability of dopaminergic neurons, leading to the manifestation of parkinsonism. Recent studies have demonstrated that VPS35 and other PD-linked gene products may operate together in a common pathway where they may interplay to precipitate neurodegeneration in PD. Establishing the nature and hierarchy of their functional interactions and identifying converging pathogenic cellular pathways would expedite the development of pathway-targeted therapeutic interventions for PD.
LRRK2
Mutations in the leucine-rich repeat kinase 2 (LRRK2) gene cause late-onset, autosomal dominant PD that clinically and neurochemically resembles idiopathic PD [71]. To date, LRRK2 mutations account for the most cases of familial PD compared to other PD-linked genes [71, 72]. At least seven mutations in LRRK2 are proven to be pathogenic based upon segregation with disease in PD families, including N1437H, R1441C/G/H, Y1699C, G2019S and I2020T, with G2019S being the most frequent variant [71, 72]. While the normal function of LRRK2 is not yet clear, it has been suggested to influence several cellular processes, including microtubule/cytoskeletal dynamics, protein translation, macroautophagy and CMA, mitochondrial function, endolysosomal sorting pathways and synaptic vesicle recycling [73, 74]. Furthermore, LRRK2 can endogenously phosphorylate and regulate a subset of RAB GTPases that are known to play roles in multiple vesicular trafficking events throughout the cell [75].
Of particular interest is the putative role of LRRK2 in endolysosomal sorting pathways. A recent study used a transcriptome approach to connect common genetic risk variants for idiopathic PD to gene expression changes [50]. Interestingly, common variants at the LRRK2 and PARK16 loci that confer PD risk had similar effects on the brain transcriptome. RAB7L1 was nominated as the gene responsible at the PARK16 locus for the genetic interaction with LRRK2. Functional analyses of LRRK2 and RAB7L1 revealed that both proteins interact and that RAB7L1 overexpression protects against neurotoxic phenotypes induced by G2019S LRRK2 in primary culture and Drosophila models [50]. Reducing RAB7L1 levels in these models correspondingly induced neuronal toxicity which may be similar to the effects of common variants at the PARK16 locus that confer PD risk i.e. by reducing RAB7L1 expression [20, 50]. Both G2019S LRRK2 expression and RAB7L1 gene silencing modulate the sorting of CI-MPR, in a similar manner to D620N VPS35 or VPS35 gene silencing, whereas WT VPS35 overexpression is able to rescue the sorting defects induced by G2019S LRRK2 [50]. WT VPS35 overexpression can also rescue the neurotoxic phenotypes induced by G2019S LRRK2 in neuronal or Drosophila models [50]. Therefore, these data suggest that G2019S LRRK2 and RAB7L1 silencing may commonly induce neuronal toxicity by converging on the retromer complex to manifest its deficiency or dysfunction. However, while the overexpression of mutant LRRK2 in mammalian cell lines or brains of BAC transgenic mice has been shown to reduce the levels of retromer subunits including VPS35 [50], VPS35 protein levels are not altered in brain tissue from G2019S LRRK2 or idiopathic PD cases [54]. A second study has provided further support for a LRRK2/VPS35 functional interaction whereby the overexpression of VPS35 can rescue mutant LRRK2 (I2020T and Y1699C)-induced phenotypes in Drosophila [76]. Although LRRK2 and VPS35 seem to interact and converge on endosomal sorting pathways, the molecular mechanism by which PD-linked LRRK2 mutants decrease VPS35 levels or retromer function is not known and whether this reduction occurs in PD-relevant brain regions or neurons of G2019S LRRK2 rodent models and human PD cases requires additional evaluation. LRRK2 could potentially influence retromer-dependent sorting via the phosphorylation of certain RAB GTPases (i.e. RAB7L1 or RAB7A) although this mechanism has not been explored [75]. It remains to be determined whether the interaction with LRRK2 is relevant to the mechanism by which PD-linked VPS35 mutations precipitate neurodegeneration or whether VPS35 simply lies downstream of LRRK2 in a common pathway.
SNCA/α-synuclein
Lewy bodies, one of the pathological hallmarks of PD, contain aggregated α-synuclein, a protein encoded by the SNCA gene [77]. Mutations or multiplications of SNCA cause early-onset autosomal dominant PD [3, 78]. The normal function of α-synuclein is not yet clear although it is highly expressed in the brain at pre-synaptic compartments where it may play a role as a chaperone for the assembly of SNARE complexes involved in synaptic vesicle recycling [79].
What causes α-synuclein aggregation and Lewy body formation in PD is still not known, however, VPS35 deficiency has been suggested to increase α-synuclein accumulation in the brain via impaired lysosomal function. In Drosophila, VPS35 depletion results in the inappropriate trafficking of CI-MPR and indirectly its ligand cathepsin D [49]. Cathepsin D is a lysosomal protease that aids in the degradation of lysosomal cargo, including α-synuclein [63]. Impaired lysosomal degradation due to cathepsin D missorting potentially promotes α-synuclein accumulation in the Drosophila brain. Additionally, VPS35 depletion in a transgenic fly model expressing human WT α-synuclein exacerbated α-synuclein-induced phenotypes including locomotor impairment and eye disorganization [49]. These observations are consistent with another study suggesting that VPS35 loss-of-function increases the toxicity induced by human α-synuclein variants in transgenic yeast and worm models [80]. Furthermore, the viral-mediated overexpression of WT VPS35, but not the P316S mutant or VPS35 silencing, was shown to rescue hippocampal neuronal loss and pathology that occurs in transgenic mice expressing human WT α-synuclein [80]. This and other observations potentially suggest that α-synuclein, similar to LRRK2, may induce neurotoxicity by manifesting VPS35 or retromer deficiency and that simply restoring VPS35 is potentially neuroprotective in these models. It should be noted, however, that VPS35 deletion in KO mice is also sufficient to induce α-synuclein accumulation in the brain but whether α-synuclein is required for mediating VPS35-dependent neurodegeneration has not been established [56, 60]. These studies collectively raise the tantalizing possibility that VPS35 and α-synuclein may converge in a common pathologic pathway to influence neurodegeneration in PD. At this juncture, however, the exact nature of this neurodegenerative interaction requires additional investigation to clarify whether α-synuclein-induced neurotoxicity is mediated by inducing VPS35 deficiency or dysfunction and/or whether α-synuclein accumulation contributes to the neurotoxicity induced by VPS35 deletion or PD-linked mutations in rodent models. A functional interaction between VPS35 and α-synuclein would have major implications for understanding the pathophysiological mechanisms underlying VPS35-dependent neurodegeneration and PD.
Parkin
Mutations in the PARK2 gene encoding parkin cause early-onset, autosomal-recessive PD and so far over 100 deletions, truncations or point mutations have been identified that confer a parkin loss-of-function [3, 81]. Parkin is an E3 ubiquitin ligase that belongs to the RING-between-RING (RBR) family of ubiquitin ligases [82]. Parkin normally functions in a neuroprotective manner potentially by targeting abnormal substrates for ubiquitination and proteasomal degradation, by promoting the degradation of defective mitochondria through mitophagy in concert with PINK1, and/or by participating in signaling or trafficking pathways involving non-degradative ubiquitination of substrates [66, 81, 82].
Parkin was first linked to the retromer by genetic interaction studies in Drosophila. Flies deficient in VPS35 were crossed with transgenic flies expressing human VPS35 variants (WT, D620N R524W or L774M) to determine if these disease-linked variants are able to rescue VPS35-deficient phenotypes including larval stage lethality, climbing deficits, melanotic masses and defects in the formation of neuromuscular junctions [83]. WT VPS35 expression could rescue these null phenotypes but pathogenic variants could rescue some phenotypes but not others. It was hypothesized that VPS35 might interact with parkin and/or PINK1 due to their shared role in the formation of MDVs [69, 70, 84]. Accordingly, VPS35 was shown to genetically interact with parkin but not with PINK1. Flies with a heterozygous deletion of either VPS35 or parkin displayed no phenotype alone yet combining these deletions in VPS35/parkin double heterozygotes decreased climbing ability, increased sensitivity to the oxidative stressor paraquat and induced mild dopaminergic neuronal loss [83], suggesting that these two gene products may function in a common pathway. Importantly, the overexpression of WT or PD-linked VPS35 variants were equally capable of rescuing parkin null phenotypes suggesting that VPS35 may lie downstream of parkin and that PD-linked mutations in VPS35 are at least partly functional [83]. Although this study supports a genetic interaction of VPS35 and parkin, with parkin most likely acting upstream of VPS35, it does not determine a role for parkin in mediating the pathogenic effects of VPS35 mutations in precipitating neurodegeneration. It remains unclear how parkin specifically contributes to the function of VPS35 or retromer-mediated sorting, although both proteins have been linked to MDV formation [69, 84], raising the possibility that these proteins might converge on this pathway.
CONCLUSIONS AND FUTURE PERSPECTIVES
The discovery of VPS35 mutations linked to autosomal dominant forms of PD has highlighted a role for retromer-mediated endosomal sorting in the pathogenesis of PD. So far only a single mutation (D620N) is known to be truly pathogenic based upon segregation with disease in large multigenerational families with PD. Numerous cellular and in vivo models have now been developed to explore the mechanisms of the D620N mutation in VPS35 and what has emerged so far is evidence that this dominant mutation most likely acts either via a toxic gain-of-function or a dominant-negative mechanism, or potentially via a combination of these mechanisms. VPS35 KO mice also develop PD-like pathology but they are also likely to develop additional severe phenotypes and susceptibilities unrelated to PD that may complicate the identification of specific disease mechanisms [56, 60]. This is perhaps best exemplified by the observation that the homozygous deletion of VPS35 in dopaminergic neurons of mice leads to their marked and early degeneration within 2–3 months of age [56], whereas homozygous D620N knockin mice do not exhibit dopaminergic neurodegeneration within a similar age range [62]. What is also clear is that the overexpression of human VPS35 variants can induce PD-like phenotypes in rodents [54, 57], suggesting that a simple loss-of-function effect caused by PD-linked mutations is highly unlikely. The molecular mechanisms underlying neurodegeneration induced by D620N VPS35 are also not yet understood with suggestions of abnormal sorting of different retromer cargo (i.e. CI-MPR/cathepsin D, GluR1/R2, GLUT1, ATG9A) and/or that the primary defect may lie at the level of WASH complex recruitment to the endosome [49–53, 55, 65]. Downstream of these initial pathogenic events, a number of cellular perturbations have been identified including impaired mitochondrial fusion [56], enhanced mitochondrial fission [57], defects in macroautophagy and CMA [55, 60], altered dendritic sorting of receptors [53, 65] and intriguing connections to other PD-linked gene products (i.e. LRRK2, α-synuclein and parkin) [49, 50, 76, 80, 83]. Many of these putative pathogenic effects still require additional validation in disease-relevant animal models and confirmation of their importance for neurodegeneration mediated by D620N mutant VPS35. Many key questions remain to be asked and answered but for now the pathogenic role of VPS35 in PD has thrust endosomal sorting and related pathways firmly into the limelight as a central mechanism underlying disease pathophysiology.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
The authors are grateful for funding support from the National Institutes of Health (R01 NS091719), Michael J. Fox Foundation for Parkinson’s Research, American Parkinson Disease Association and the Van Andel Research Institute.
REFERENCES
- [1]. Lang AE, & Lozano AM (1998) Parkinson’s disease. Second of two parts. N Engl J Med, 339, 1130–1143. [DOI] [PubMed] [Google Scholar]
- [2]. Lang AE, & Lozano AM (1998) Parkinson’s disease. First of two parts. N Engl J Med, 339, 1044–1053. [DOI] [PubMed] [Google Scholar]
- [3]. Hernandez DG, Reed X, & Singleton AB (2016) Genetics in Parkinson disease: Mendelian versus non-Mendelian inheritance. J Neurochem, 139(Suppl 1), 59–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Polymeropoulos MH, Lavedan C, Leroy E, Ide SE, Dehejia A, Dutra A, Pike B, Root H, Rubenstein J, Boyer R, Stenroos ES, Chandrasekharappa S, Athanassiadou A, Papapetropoulos T, Johnson WG, Lazzarini AM, Duvoisin RC, Di Iorio G, Golbe LI, & Nussbaum RL (1997) Mutation in the alpha-synuclein gene identified in families with Parkinson’s disease. Science, 276, 2045–2047. [DOI] [PubMed] [Google Scholar]
- [5]. Zimprich A, Biskup S, Leitner P, Lichtner P, Farrer M, Lincoln S, Kachergus J, Hulihan M, Uitti RJ, Calne DB, Stoessl AJ, Pfeiffer RF, Patenge N, Carbajal IC, Vieregge P, Asmus F, Muller-Myhsok B, Dickson DW, Meitinger T, Strom TM, Wszolek ZK, & Gasser T (2004) Mutations in LRRK2 cause autosomal-dominant parkinsonism with pleomorphic pathology. Neuron, 44, 601–607. [DOI] [PubMed] [Google Scholar]
- [6]. Paisan-Ruiz C, Jain S, Evans EW, Gilks WP, Simon J, van der Brug M, Lopez de Munain A, Aparicio S, Gil AM, Khan N, Johnson J, Martinez JR, Nicholl D, Carrera IM, Pena AS, de Silva R, Lees A, Marti-Masso JF, Perez-Tur J, Wood NW, & Singleton AB (2004) Cloning of the gene containing mutations that cause PARK8-linked Parkinson’s disease. Neuron, 44, 595–600. [DOI] [PubMed] [Google Scholar]
- [7]. Vilarino-Guell C, Wider C, Ross O, Dachsel J, Kachergus J, Lincoln S, Soto-Ortolaza A, Cobb S, Wilhoite G, & Bacon J (2011) VPS35 mutations in Parkinson disease. Am J Hum Genet, 89, 162–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8]. Zimprich A, Benet-Pages A, Struhal W, Graf E, Eck S, Offman M, Haubenberger D, Spielberger S, Schulte E, & Lichtner P (2011) A mutation in VPS35, encoding a subunit of the retromer complex, causes late-onset Parkinson disease. Am J Hum Genet, 89, 168–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Wilson GR, Sim JC, McLean C, Giannandrea M, Galea CA, Riseley JR, Stephenson SE, Fitzpatrick E, Haas SA, Pope K, Hogan KJ, Gregg RG, Bromhead CJ, Wargowski DS, Lawrence CH, James PA, Churchyard A, Gao Y, Phelan DG, Gillies G, Salce N, Stanford L, Marsh AP, Mignogna ML, Hayflick SJ, Leventer RJ, Delatycki MB, Mellick GD, Kalscheuer VM, D’Adamo P, Bahlo M, Amor DJ, & Lockhart PJ (2014) Mutations in RAB39B cause X-linked intellectual disability and early-onset Parkinson disease with alpha-synuclein pathology. Am J Hum Genet, 95, 729–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10]. Deng HX, Shi Y, Yang Y, Ahmeti KB, Miller N, Huang C, Cheng L, Zhai H, Deng S, Nuytemans K, Corbett NJ, Kim MJ, Deng H, Tang B, Yang Z, Xu Y, Chan P, Huang B, Gao XP, Song Z, Liu Z, Fecto F, Siddique N, Foroud T, Jankovic J, Ghetti B, Nicholson DA, Krainc D, Melen O, Vance JM, Pericak-Vance MA, Ma YC, Rajput AH, & Siddique T (2016) Identification of TMEM230 mutations in familial Parkinson’s disease. Nat Genet, 48, 733–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Kitada T, Asakawa S, Hattori N, Matsumine H, Yamamura Y, Minoshima S, Yokochi M, Mizuno Y, & Shimizu N (1998) Mutations in the parkin gene cause autosomal recessive juvenile parkinsonism. Nature, 392, 605–608. [DOI] [PubMed] [Google Scholar]
- [12]. Valente EM, Abou-Sleiman PM, Caputo V, Muqit MM, Harvey K, Gispert S, Ali Z, Del Turco D, Bentivoglio AR, Healy DG, Albanese A, Nussbaum R, Gonzalez-Maldonado R, Deller T, Salvi S, Cortelli P, Gilks WP, Latchman DS, Harvey RJ, Dallapiccola B, Auburger G, & Wood NW (2004) Hereditary early-onset Parkinson’s disease caused by mutations in PINK1. Science, 304, 1158–1160. [DOI] [PubMed] [Google Scholar]
- [13]. Bonifati V, Rizzu P, van Baren MJ, Schaap O, Breedveld GJ, Krieger E, Dekker MC, Squitieri F, Ibanez P, Joosse M, van Dongen JW, Vanacore N, van Swieten JC, Brice A, Meco G, van Duijn CM, Oostra BA, & Heutink P (2003) Mutations in the DJ-1 gene associated with autosomal recessive early-onset parkinsonism. Science, 299, 256–259. [DOI] [PubMed] [Google Scholar]
- [14]. Ramirez A, Heimbach A, Grundemann J, Stiller B, Hampshire D, Cid LP, Goebel I, Mubaidin AF, Wriekat AL, Roeper J, Al-Din A, Hillmer AM, Karsak M, Liss B, Woods CG, Behrens MI, & Kubisch C (2006) Hereditary parkinsonism with dementia is caused by mutations in ATP13A2, encoding a lysosomal type 5 P-type ATPase. Nat Genet, 38, 1184–1191. [DOI] [PubMed] [Google Scholar]
- [15]. Paisan-Ruiz C, Bhatia KP, Li A, Hernandez D, Davis M, Wood NW, Hardy J, Houlden H, Singleton A, & Schneider SA (2009) Characterization of PLA2G6 as a locus for dystonia-parkinsonism. Ann Neurol, 65, 19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16]. Shojaee S, Sina F, Banihosseini SS, Kazemi MH, Kalhor R, Shahidi GA, Fakhrai-Rad H, Ronaghi M, & Elahi E (2008) Genome-wide linkage analysis of a Parkinsonian-pyramidal syndrome pedigree by 500 K SNP arrays. Am J Hum Genet, 82, 1375–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17]. Edvardson S, Cinnamon Y, Ta-Shma A, Shaag A, Yim YI, Zenvirt S, Jalas C, Lesage S, Brice A, Taraboulos A, Kaestner KH, Greene LE, & Elpeleg O (2012) A deleterious mutation in DNAJC6 encoding the neuronal-specific clathrin-uncoating co-chaperone auxilin, is associated with juvenile parkinsonism. PLoS One, 7, e36458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. Krebs CE, Karkheiran S, Powell JC, Cao M, Makarov V, Darvish H, Di Paolo G, Walker RH, Shahidi GA, Buxbaum JD, De Camilli P, Yue Z, & Paisan-Ruiz C (2013) The Sac1 domain of SYNJ1 identified mutated in a family with early-onset progressive Parkinsonism with generalized seizures. Hum Mutat, 34, 1200–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19]. Quadri M, Fang M, Picillo M, Olgiati S, Breedveld GJ, Graafland J, Wu B, Xu F, Erro R, Amboni M, Pappatá S, Quarantelli M, Annesi G, Quattrone A, Chien HF, Barbosa ER, International Parkinsonism Genetics Network, Oostra BA, Barone P, Wang J, & Bonifati V (2013) Mutation in the SYNJ1 gene associated with autosomal recessive, early-onset Parkinsonism. Hum Mutat, 34, 1208–1215. [DOI] [PubMed] [Google Scholar]
- [20]. Nalls MA, Pankratz N, Lill CM, Do CB, Hernandez DG, Saad M, DeStefano AL, Kara E, Bras J, Sharma M, Schulte C, Keller MF, Arepalli S, Letson C, Edsall C, Stefansson H, Liu X, Pliner H, Lee JH, Cheng R, International Parkinson’s Disease Genomics Consortium (IPDGC), Parkinson’s Study Group (PSG) Parkinson’s Research: The Organized GENetics Initiative (PROGENI), 23andMe, GenePD, NeuroGenetics Research Consortium (NGRC), Hussman Institute of Human Genomics (HIHG), Ashkenazi Jewish Dataset Investigator, Cohorts for Health, Aging Research in Genetic Epidemiology (CHARGE), North American Brain Expression Consortium (NABEC), United Kingdom Brain Expression Consortium (UKBEC), Greek Parkinson’s Disease Consortium, Alzheimer Genetic Analysis Group, Ikram MA, Ioannidis JP, Hadjigeorgiou GM, Bis JC, Martinez M, Perlmutter JS, Goate A, Marder K, Fiske B, Sutherland M, Xiromerisiou G, Myers RH, Clark LN, Stefansson K, Hardy JA, Heutink P, Chen H, Wood NW, Houlden H, Payami H, Brice A, Scott WK, Gasser T, Bertram L, Eriksson N, Foroud T, & Singleton AB (2014) Large-scale meta-analysis of genome-wide association data identifies six new risk loci for Parkinson’s disease. Nat Genet, 46, 989–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. Martin I, Dawson VL, & Dawson TM (2011) Recent advances in the genetics of Parkinson’s disease. Annu Rev Genomics Hum Genet, 12, 301–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22]. Kumaran R, & Cookson MR (2015) Pathways to Parkinsonism redux: Convergent pathobiological mechanisms in genetics of Parkinson’s disease. Hum Mol Genet, 24, R32–R44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23]. Abeliovich A, & Gitler AD (2016) Defects in trafficking bridge Parkinson’s disease pathology and genetics. Nature, 539, 207–216. [DOI] [PubMed] [Google Scholar]
- [24]. Wider C, Skipper L, Solida A, Brown L, Farrer M, Dickson D, Wszolek ZK, & Vingerhoets FJG (2008) Autosomal dominant dopa-responsive parkinsonism in a multigenerational Swiss family. Parkinsonism Relat Disord, 14, 465–470. [DOI] [PubMed] [Google Scholar]
- [25]. Deng H, Gao K, & Jankovic J (2013) The VPS35 gene and Parkinson’s disease. Mov Disord, 28, 569–575. [DOI] [PubMed] [Google Scholar]
- [26]. Kumar KR, Weissbach A, Heldmann M, Kasten M, Tunc S, Sue CM, Svetel M, Kostic VS, Segura-Aguilar J, Ramirez A, Simon DK, Vieregge P, Munte TF, Hagenah J, Klein C, & Lohmann K (2012) Frequency of the D620N mutation in VPS35 in Parkinson disease. Arch Neurol, 69, 1360–1364. [DOI] [PubMed] [Google Scholar]
- [27]. Sharma M, Ioannidis JP, Aasly JO, Annesi G, Brice A, Bertram L, Bozi M, Barcikowska M, Crosiers D, Clarke CE, Facheris MF, Farrer M, Garraux G, Gispert S, Auburger G, Vilariño-Güell C, Hadjigeorgiou GM, Hicks AA, Hattori N, Jeon BS, Jamrozik Z, Krygowska-Wajs A, Lesage S, Lill CM, Lin JJ, Lynch T, Lichtner P, Lang AE, Libioulle C, Murata M, Mok V, Jasinska-Myga B, Mellick GD, Morrison KE, Meitnger T, Zimprich A, Opala G, Pramstaller PP, Pichler I, Park SS, Quattrone A, Rogaeva E, Ross OA, Stefanis L, Stockton JD, Satake W, Silburn PA, Strom TM, Theuns J, Tan EK, Toda T, Tomiyama H, Uitti RJ, Van Broeckhoven C, Wirdefeldt K, Wszolek Z, Xiromerisiou G, Yomono HS, Yueh KC, Zhao Y, Gasser T, Maraganore D, Krüger R, GEOPD, & consortium (2012) A multi-centre clinico-genetic analysis of the VPS35 gene in Parkinson disease indicates reduced penetrance for disease-associated variants. J Med Genet, 49, 721–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28]. Sheerin UM, Charlesworth G, Bras J, Guerreiro R, Bhatia K, Foltynie T, Limousin P, Silveira-Moriyama L, Lees A, & Wood N (2012) Screening for VPS35 mutations in Parkinson’s disease. Neurobiol Aging, 33, 838 e831–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29]. Verstraeten A, Wauters E, Crosiers D, Meeus B, Corsmit E, Elinck E, Mattheijssens M, Peeters K, Cras P, Pickut B, Vandenberghe R, Engelborghs S, De Deyn PP, Van Broeckhoven C, & Theuns J (2012) Contribution of VPS35 genetic variability to LBD in the Flanders-Belgian population. Neurobiol Aging, 33, 1844 e1811–1843. [DOI] [PubMed] [Google Scholar]
- [30]. Gustavsson EK, Guella I, Trinh J, Szu-Tu C, Rajput A, Rajput AH, Steele JC, McKeown M, Jeon BS, Aasly JO, & Farrer MJ (2015) Genetic variability of the retromer cargo recognition complex in parkinsonism. Mov Disord, 30, 580–584. [DOI] [PubMed] [Google Scholar]
- [31]. Bandres-Ciga S, Mencacci NE, Duran R, Barrero FJ, Escamilla-Sevilla F, Morgan S, Hehir J, Vives F, Hardy J, & Pittman AM (2016) Analysis of the genetic variability in Parkinson’s disease from Southern Spain. Neurobiol Aging, 37, 210 e211–215. [DOI] [PubMed] [Google Scholar]
- [32]. Ando M, Funayama M, Li Y, Kashihara K, Murakami Y, Ishizu N, Toyoda C, Noguchi K, Hashimoto T, Nakano N, Sasaki R, Kokubo Y, Kuzuhara S, Ogaki K, Yamashita C, Yoshino H, Hatano T, Tomiyama H, & Hattori N (2012) VPS35 mutation in Japanese patients with typical Parkinson’s disease. Mov Disord, 27, 1413–1417. [DOI] [PubMed] [Google Scholar]
- [33]. Struhal W, Presslauer S, Spielberger S, Zimprich A, Auff E, Bruecke T, Poewe W, Ransmayr G, & Austrian VPS-35 Investigators Team (2014) VPS35 Parkinson’s disease phenotype resembles the sporadic disease. J Neural Transm, 121, 755–759. [DOI] [PubMed] [Google Scholar]
- [34]. Seaman MN (2012) The retromer complex - endosomal protein recycling and beyond. J Cell Sci, 125, 4693–4702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35]. Cullen PJ, & Korswagen HC (2012) Sorting nexins provide diversity for retromer-dependent trafficking events. Nat Cell Biol, 14, 29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36]. Seaman MN, Marcusson EG, Cereghino JL, & Emr SD (1997) Endosome to Golgi retrieval of the vacuolar protein sorting receptor, Vps10p, requires the function of the VPS29, VPS30, and VPS35 gene products. J Cell Biol, 137, 79–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37]. Seaman MN, McCaffery JM, & Emr SD (1998) A membrane coat complex essential for endosome-to-Golgi retrograde transport in yeast. J Cell Biol, 142, 665–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38]. Hierro A, Rojas AL, Rojas R, Murthy N, Effantin G, Kajava AV, Steven AC, Bonifacino JS, & Hurley JH (2007) Functional architecture of the retromer cargo-recognition complex. Nature, 449, 1063–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39]. Bonifacino JS, & Hurley JH (2008) Retromer. Curr Opin Cell Biol, 20, 427–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40]. Gokool S, Tattersall D, Reddy JV, & Seaman MN (2007) Identification of a conserved motif required for Vps35p/Vps26p interaction and assembly of the retromer complex. Biochem J, 408, 287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41]. Rojas R, van Vlijmen T, Mardones GA, Prabhu Y, Rojas AL, Mohammed S, Heck AJ, Raposo G, van der Sluijs P, & Bonifacino JS (2008) Regulation of retromer recruitment to endosomes by sequential action of Rab5 and Rab7. J Cell Biol, 183, 513–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42]. Ruck A, Attonito J, Garces KT, Nunez L, Palmisano NJ, Rubel Z, Bai Z, Nguyen KC, Sun L, Grant BD, Hall DH, & Melendez A (2011) The Atg6/Vps30/Beclin 1 ortholog BEC-1 mediates endocytic retrograde transport in addition to autophagy in C. elegans. Autophagy, 7, 386–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43]. Gomez TS, & Billadeau DD (2009) A FAM21-containing WASH complex regulates retromer-dependent sorting. Dev Cell, 17, 699–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44]. Seaman MN, Gautreau A, & Billadeau DD (2013) Retromer-mediated endosomal protein sorting: All WASHed up!. Trends Cell Biol, 23, 522–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45]. Steinberg F, Gallon M, Winfield M, Thomas EC, Bell AJ, Heesom KJ, Tavare JM, & Cullen PJ (2013) A global analysis of SNX27-retromer assembly and cargo specificity reveals a function in glucose and metal ion transport. Nat Cell Biol, 15, 461–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46]. Harterink M, Port F, Lorenowicz MJ, McGough IJ, Silhankova M, Betist MC, van Weering JR, van Heesbeen RG, Middelkoop TC, Basler K, Cullen PJ, & Korswagen HC (2011) A SNX3-dependent retromer pathway mediates retrograde transport of the Wnt sorting receptor Wntless and is required for Wnt secretion. Nat Cell Biol, 13, 914–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47]. Xu Y, Hortsman H, Seet L, Wong SH, & Hong W (2001) SNX3 regulates endosomal function through its PX-domain-mediated interaction with PtdIns(3)P. Nat Cell Biol, 3, 658–666. [DOI] [PubMed] [Google Scholar]
- [48]. Choy RW, Park M, Temkin P, Herring BE, Marley A, Nicoll RA, & von Zastrow M (2014) Retromer mediates a discrete route of local membrane delivery to dendrites. Neuron, 82, 55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49]. Miura E, Hasegawa T, Konno M, Suzuki M, Sugeno N, Fujikake N, Geisler S, Tabuchi M, Oshima R, Kikuchi A, Baba T, Wada K, Nagai Y, Takeda A, & Aoki M (2014) VPS35 dysfunction impairs lysosomal degradation of alpha-synuclein and exacerbates neurotoxicity in a Drosophila model of Parkinson’s disease. Neurobiol Dis, 71, 1–13. [DOI] [PubMed] [Google Scholar]
- [50]. MacLeod DA, Rhinn H, Kuwahara T, Zolin A, Di Paolo G, McCabe BD, Marder KS, Honig LS, Clark LN, Small SA, & Abeliovich A (2013) RAB7L1 interacts with LRRK2 to modify intraneuronal protein sorting and Parkinson’s disease risk. Neuron, 77, 425–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51]. McGough IJ, Steinberg F, Jia D, Barbuti PA, McMillan KJ, Heesom KJ, Whone AL, Caldwell MA, Billadeau DD, Rosen MK, & Cullen PJ (2014) Retromer binding to FAM21 and the WASH complex is perturbed by the Parkinson disease-linked VPS35(D620N) mutation. Curr Biol, 24, 1670–1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52]. Follett J, Norwood SJ, Hamilton NA, Mohan M, Kovtun O, Tay S, Zhe Y, Wood SA, Mellick GD, Silburn PA, Collins BM, Bugarcic A, & Teasdale RD (2014) The Vps35 D620N mutation linked to Parkinson’s disease disrupts the cargo sorting function of retromer. Traffic, 15, 230–244. [DOI] [PubMed] [Google Scholar]
- [53]. Munsie LN, Milnerwood AJ, Seibler P, Beccano-Kelly DA, Tatarnikov I, Khinda J, Volta M, Kadgien C, Cao LP, Tapia L, Klein C, & Farrer MJ (2015) Retromer-dependent neurotransmitter receptor trafficking to synapses is altered by the Parkinson’s Disease VPS35 mutation p. D620N. Hum Mol Genet, 24, 1691–1703. [DOI] [PubMed] [Google Scholar]
- [54]. Tsika E, Glauser L, Moser R, Fiser A, Daniel G, Sheerin UM, Lees A, Troncoso JC, Lewis PA, Bandopadhyay R, Schneider BL, & Moore DJ (2014) Parkinson’s disease-linked mutations in VPS35 induce dopaminergic neurodegeneration. Hum Mol Genet, 23, 4621–4638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55]. Zavodszky E, Seaman MN, Moreau K, Jimenez-Sanchez M, Breusegem SY, Harbour ME, & Rubinsztein DC (2014) Mutation in VPS35 associated with Parkinson’s disease impairs WASH complex association and inhibits autophagy. Nat Commun, 5, 3828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56]. Tang FL, Liu W, Hu JX, Erion JR, Ye J, Mei L, & Xiong WC (2015) VPS35 deficiency or mutation causes dopaminergic neuronal loss by impairing mitochondrial fusion and function. Cell Rep, 12, 1631–1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57]. Wang W, Wang X, Fujioka H, Hoppel C, Whone AL, Caldwell MA, Cullen PJ, Liu J, & Zhu X (2016) Parkinson’s disease-associated mutant VPS35 causes mitochondrial dysfunction by recycling DLP1 complexes. Nat Med, 22, 54–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58]. Wang HS, Toh J, Ho P, Tio M, Zhao Y, & Tan EK (2014) In vivo evidence of pathogenicity of VPS35 mutations in the Drosophila. Mol Brai, 7, 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59]. Bi F, Li F, Huang C, & Zhou H (2013) Pathogenic mutation in VPS35 impairs its protection against MPP(+) cytotoxicity. Int J Biol Sci, 9, 149–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60]. Tang FL, Erion JR, Tian Y, Liu W, Yin DM, Ye J, Tang B, Mei L, & Xiong WC (2015) VPS35 in dopamine neurons is required for endosome-to-Golgi retrieval of Lamp2a, a receptor of chaperone-mediated autophagy that is critical for alpha-synuclein degradation and prevention of pathogenesis of Parkinson’s disease. J Neurosci, 35, 10613–10628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61]. Wen L, Tang FL, Hong Y, Luo SW, Wang CL, He W, Shen C, Jung JU, Xiong F, Lee DH, Zhang QG, Brann D, Kim TW, Yan R, Mei L, & Xiong WC (2011) VPS35 haploinsufficiency increases Alzheimer’s disease neuropathology. J Cell Biol, 195, 765–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62]. Ishizu N, Yui D, Hebisawa A, Aizawa H, Cui W, Fujita Y, Hashimoto K, Ajioka I, Mizusawa H, Yokota T, & Watase K (2016) Impaired striatal dopamine release in homozygous Vps35 D620N knock-in mice. Hum Mol Genet, in press, doi: 10.1093/hmg/ddw279. [DOI] [PubMed] [Google Scholar]
- [63]. Xilouri M, Brekk OR, & Stefanis L (2013) alpha-Synuclein and protein degradation systems: A reciprocal relationship. Mol Neurobiol, 47, 537–551. [DOI] [PubMed] [Google Scholar]
- [64]. Bhalla A, Vetanovetz CP, Morel E, Chamoun Z, Di Paolo G, & Small SA (2012) The location and trafficking routes of the neuronal retromer and its role in amyloid precursor protein transport. Neurobiol Dis, 47, 126–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65]. Tian Y, Tang FL, Sun X, Wen L, Mei L, Tang BS, & Xiong WC (2015) VPS35-deficiency results in an impaired AMPA receptor trafficking and decreased dendritic spine maturation. Mol Brain, 8, 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66]. Winklhofer KF (2014) Parkin and mitochondrial quality control: Toward assembling the puzzle. Trends Cell Biol, 24, 332–341. [DOI] [PubMed] [Google Scholar]
- [67]. Winklhofer KF, & Haass C (2010) Mitochondrial dysfunction in Parkinson’s disease. Biochim Biophys Acta, 1802, 29–44. [DOI] [PubMed] [Google Scholar]
- [68]. Trancikova A, Tsika E, & Moore DJ (2012) Mitochondrial dysfunction in genetic animal models of Parkinson’s disease. Antioxid Redox Signal, 16, 896–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69]. Braschi E, Goyon V, Zunino R, Mohanty A, Xu L, & McBride HM (2010) Vps35 mediates vesicle transport between the mitochondria and peroxisomes. Curr Biol, 20, 1310–1315. [DOI] [PubMed] [Google Scholar]
- [70]. Sugiura A, McLelland GL, Fon EA, & McBride HM (2014) A new pathway for mitochondrial quality control: Mitochondrial-derived vesicles. EMBO J, 33, 2142–2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71]. Paisan-Ruiz C, Lewis PA, & Singleton AB (2013) LRRK2: Cause, risk, and mechanism. J Parkinsons Dis, 3, 85–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72]. Healy DG, Falchi M, O’Sullivan SS, Bonifati V, Durr A, Bressman S, Brice A, Aasly J, Zabetian CP, Goldwurm S, Ferreira JJ, Tolosa E, Kay DM, Klein C, Williams DR, Marras C, Lang AE, Wszolek ZK, Berciano J, Schapira AH, Lynch T, Bhatia KP, Gasser T, Lees AJ, Wood NW, & International LRRK2 Consortium (2008) Phenotype, genotype, and worldwide genetic penetrance of LRRK2-associated Parkinson’s disease: A case-control study. Lancet Neurol, 7, 583–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73]. Tsika E, & Moore DJ (2012) Mechanisms of LRRK2-mediated neurodegeneration. Curr Neurol Neurosci Rep, 12, 251–260. [DOI] [PubMed] [Google Scholar]
- [74]. Daniel G, & Moore DJ (2015) Modeling LRRK2 pathobiology in Parkinson’s disease: From yeast to rodents. Curr Top Behav Neurosci, 22, 331–368. [DOI] [PubMed] [Google Scholar]
- [75]. Steger M, Tonelli F, Ito G, Davies P, Trost M, Vetter M, Wachter S, Lorentzen E, Duddy G, Wilson S, Baptista MA, Fiske BK, Fell MJ, Morrow JA, Reith AD, Alessi DR, & Mann M (2016) Phosphoproteomics reveals that Parkinson’s disease kinase LRRK2 regulates a subset of Rab GTPases. Elife, 5, pii: e12813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76]. Linhart R, Wong SA, Cao J, Tran M, Huynh A, Ardrey C, Park JM, Hsu C, Taha S, Peterson R, Shea S, Kurian J, & Venderova K (2014) Vacuolar protein sorting 35 (Vps35) rescues locomotor deficits and shortened lifespan in Drosophila expressing a Parkinson’s disease mutant of Leucine-Rich Repeat Kinase 2 (LRRK2). Mol Neurodegener, 9, 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77]. Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, & Goedert M (1997) Alpha-synuclein in Lewy bodies. Nature, 388, 839–840. [DOI] [PubMed] [Google Scholar]
- [78]. Stefanis L (2012) α-Synuclein in Parkinson’s disease. Cold Spring Harb Perspect Med, 2, a009399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79]. Burre J (2015) The synaptic function of alpha-synuclein. J Parkinsons Dis, 5, 699–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80]. Dhungel N, Eleuteri S, Li LB, Kramer NJ, Chartron JW, Spencer B, Kosberg K, Fields JA, Stafa K, Adame A, Lashuel H, Frydman J, Shen K, Masliah E, & Gitler AD (2015) Parkinson’s disease genes VPS35 and EIF4G1 interact genetically and converge on alpha-synuclein. Neuron, 85, 76–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81]. Dawson TM, & Dawson VL (2010) The role of parkin in familial and sporadic Parkinson’s disease. Mov Disord, 25(Suppl 1), S32–S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82]. Seirafi M, Kozlov G, & Gehring K (2015) Parkin structure and function. FEBS J, 282, 2076–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83]. Malik BR, Godena VK, & Whitworth AJ (2015) VPS35 pathogenic mutations confer no dominant toxicity but partial loss of function in Drosophila and genetically interact with parkin. Hum Mol Genet, 24, 6106–6117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84]. McLelland GL, Soubannier V, Chen CX, McBride HM, & Fon EA (2014) Parkin and PINK1 function in a vesicular trafficking pathway regulating mitochondrial quality control. EMBO J, 33, 282–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85]. Seaman MN (2004) Cargo-selective endosomal sorting for retrieval to the Golgi requires retromer. J Cell Biol, 165, 111–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86]. Lesage S, & Brice A (2012) Role of mendelian genes in “sporadic” Parkinson’s disease. Parkinsonism Relat Disord, 18(Suppl 1), S66–S70. [DOI] [PubMed] [Google Scholar]