Abstract
Introduction
Both excessive weight gain and weight loss are important risk factors in the older population. Neighborhood environment may play an important role in weight change, but neighborhood effects on weight gain and weight loss have not been studied separately. This study examined the associations between neighborhood socioeconomic deprivation and excessive weight gain and weight loss.
Methods
This analysis included 153,690 men and 105,179 women (aged 51–70 years). Baseline addresses were geocoded into geographic coordinates and linked to the 2000 U.S. Census at the Census tract level. Census variables were used to generate a socioeconomic deprivation index by principle component analysis. Excessive weight gain and loss were defined as gaining or losing >10% of baseline (1995–1996) body weight at follow-up (2004–2006). The analysis was performed in 2015.
Results
More severe neighborhood socioeconomic deprivation was associated with higher risks of both excessive weight gain and weight loss after adjusting for individual indicators of SES, disease conditions, and lifestyle factors (Quintile 5 vs Quintile 1: weight gain, OR=1.36, 95% CI=1.28, 1.45 for men and OR=1.20, 95% CI=1.13, 1.27 for women; weight loss, OR=1.09, 9%% CI=1.02, 1.17 for men and OR=1.23, 95% CI=1.14, 1.32 for women). The findings were fairly consistent across subpopulations with different demographics and lifestyle factors.
Conclusions
Neighborhood socioeconomic deprivation predicts higher risk of excessive weight gain and weight loss.
Introduction
Maintaining a healthy body weight is critical to managing one's health. In adults, substantial changes in body weight have been associated with higher disease risk and increased mortality.1 On one hand, excessive weight gain and obesity are established risk factors for numerous chronic conditions and contribute to higher death risk among the older population.2,3 On the other hand, weight loss is also a strong predictor of higher mortality, particularly among older adults,4 and a study of older Americans estimated that losing >10% of body weight after age 50 years was associated with an approximate 60% increase in mortality.5
Body weight is influenced by behaviors such as physical activity, diet, and sleep, as well as disease status and psychological states, all of which are sensitive to societal and contextual factors and are shaped by the environment in which one lives. A growing body of literature examined the relationship between neighborhood characteristics and weight status. Several cross-sectional studies reported a relationship between neighborhood socioeconomic deprivation and higher BMI.6–9 However, results from longitudinal investigations on this relationship are mixed: Some studies reported higher weight gain and elevated risk of obesity among residents of more-deprived neighborhoods,10–12 whereas others found no association.9,13
A major limitation in the current literature is that all of the previous studies focused on average weight change and did not distinguish between those who experienced weight loss and those with weight gain. Examining average weight change not only conceals the full picture of weight trajectory, but also prevents further investigation into the exact health consequences of neighborhood deprivation, as weight gain and weight loss are often products of different biological processes. Whereas excessive weight gain is caused by an altered energy balance with excessive dietary intake and inadequate physical activity, excessive weight loss is commonly a result of diseases, including cancer, and decline associated with aging.14,15 Neighborhood socioeconomic conditions may influence both health behaviors and disease risks that may lead to either weight gain or weight loss. Therefore, there is a need for studies that examine neighborhood socioeconomic deprivation in relation to weight gain and weight loss separately.
The NIH-AARP Diet and Health study, a large cohort of middle- to older-aged men and women, offers a unique opportunity to study the health effects of neighborhood characteristics, and previous research in this population has linked neighborhood socioeconomic deprivation with a large range of disease outcomes, including cancer and mortality, as well as health behaviors such as diet.16–21 The primary goal of the current study was to prospectively examine neighborhood socioeconomic deprivation in relation to both excessive weight gain and weight loss. A secondary goal was to examine whether the relationship between neighborhood deprivation and weight change is modified by individual factors, including individual-level SES, health behaviors, and disease conditions.
Methods
Study Population
Details of the NIH-AARP Diet and Health Study were reported previously.22 Briefly, the study recruited 566,399 AARP members (aged 50–71 years) residing in one of six U.S. states (California, Florida, Louisiana, New Jersey, North Carolina, and Pennsylvania) and two metropolitan areas (Atlanta, Georgia and Detroit, Michigan). The analytic cohort consisted of 153,690 men and 105,179 women (details on exclusions in Appendix). The study was approved by the National Cancer Institute Special Studies IRB.
Measures
The participants reported residential address at baseline. The addresses were geocoded into geographic coordinates and linked to the 2000 U.S. Census at the Census tract level. The method developed by Messer et al.23 was applied to generate an empirical neighborhood socioeconomic deprivation index18 using principle component analysis (details presented in Appendix).
Participants reported height (in inches and feet) at baseline and current weight (in pounds) at baseline (1995–1996) and follow-up (2004–2006). Excessive weight gain and loss were defined as gaining or losing >10% of baseline body weight, as previous reports have associated these two conditions with higher mortality in middle- to older-aged populations.5,24 At each time point, BMI (kg/m2) was calculated and obesity was defined as BMI ≥30 kg/m2.
Statistical Analysis
The authors used SAS, version 9.3 to conduct multiple logistic regression (proc surveylogistic) to calculate the OR and 95% CI for each condition, comparing participants living in more-deprived neighborhood (second through fifth quintile) at baseline with the reference group (first quintile). For the main analysis, a series of multiple regression models were considered. The base model was adjusted for age and baseline BMI. A second model, considered the main model, was additionally adjusted for potential confounders, including indicators of individual-level SES (race and education) and medical conditions at baseline. Finally, a third model was additionally adjusted for lifestyle factors, including smoking, physical activity, TV viewing, sleep duration, alcohol consumption, and diet. Details about covariates are presented in table footnotes and figure legends. In all models, robust variance estimation was used for SE estimation to account for clustering across Census tracts.25
Results
Baseline study characteristics across quintiles of neighborhood deprivation index are presented in Table 1 (Appendix Tables 2 and 3 list sex-specific distributions). When compared with those from the least deprived neighborhood, participants from more-deprived neighborhoods were more likely to be women and black, and were less likely to be married or have a college education. Overall, residents of more-deprived neighborhoods had a less healthy life style with more current smoking, less physical activity, more TV viewing, and a lower Healthy Eating Index score. They also had higher prevalence of heart disease, stroke, and diabetes at baseline. Cross-sectional analysis showed that more severe deprivation was strongly associated with higher BMI and higher obesity at baseline (Appendix Table 4). Compared with the reference group, men and women in the most deprived neighborhood were 33% and 56% more likely to be obese, respectively.
Table 1. Baseline Study Characteristics According to Quintiles of Deprivation Index Among 258,875 Participants.
| Neighborhood deprivation | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Characteristics | Overal l | Q1 (high SES) | Q2 | Q3 | Q4 | Q5 (low SES) |
| Age at baseline, mean (SD) | 61.9 (5.3) | 61.6 (5.4) | 61.7 (5.4) | 62.0 (5.3) | 62.2 (5.3) | 62.0 (5.3) |
| BMI, kg/m2, mean (SD) | 26.9 (4.5) | 26.2 (4.1) | 26.7 (4.3) | 27.0 (4.5) | 27.2 (4.6) | 27.6 (4.9) |
| BMI, kg/m2, % | ||||||
| 15-<18.5 | 0.7 | 0.8 | 0.7 | 0.7 | 0.7 | 0.7 |
| 18.5-<25 | 35.5 | 41.2 | 37.3 | 35.1 | 32.9 | 31.2 |
| 25-<30 | 42.9 | 42.9 | 43.2 | 43.0 | 43.4 | 42.0 |
| 30-<35 | 15.3 | 11.8 | 14.2 | 15.6 | 16.7 | 18.0 |
| 35-50 | 5.6 | 3.4 | 4.6 | 5.7 | 6.3 | 8.0 |
| Female, % | 40.6 | 34.6 | 37.8 | 40.3 | 42.7 | 47.7 |
| White, non-Hispanic, % | 92.7 | 95.5 | 95.1 | 95.2 | 94.2 | 83.4 |
| College and post-college, % | 43.2 | 65.1 | 49.8 | 39.7 | 32.8 | 28.5 |
| Married, % | 70.4 | 77.3 | 72.9 | 71.0 | 69.2 | 61.6 |
| Smoking, % | ||||||
| Never | 38.3 | 40.5 | 38.3 | 37.4 | 37.4 | 37.8 |
| Former | 49.0 | 49.7 | 50.2 | 50.1 | 49.0 | 46.3 |
| Current | 9.4 | 6.6 | 8.3 | 9.5 | 10.4 | 12.3 |
| Vigorous physical activity, % | ||||||
| Never/rarely | 15.2 | 11.5 | 13.8 | 15.6 | 16.3 | 19.6 |
| <3 times/month | 13.5 | 12.7 | 13.6 | 13.6 | 13.6 | 14.2 |
| 1-2 times/week | 22.1 | 22.5 | 22.6 | 22.4 | 22.0 | 21.3 |
| 3-4 times/week | 28.1 | 30.8 | 28.9 | 28.0 | 27.4 | 25.2 |
| ≥5 times/week | 20.1 | 22.0 | 20.5 | 19.7 | 19.9 | 18.6 |
| TV viewing, % | ||||||
| ≤2 hours/day | 36.5 | 47.1 | 40.0 | 35.5 | 32.6 | 31.3 |
| 3-4 hours/day | 43.7 | 40.3 | 43.5 | 44.9 | 45.5 | 43.9 |
| 5-6 hours/day | 14.3 | 10.0 | 12.7 | 15.0 | 16.4 | 17.6 |
| ≥7 hours/day | 4.3 | 2.3 | 3.5 | 3.1 | 5.0 | 6.6 |
| Nighttime sleep, % | ||||||
| ≤5 hours | 2.4 | 1.4 | 2.1 | 2.4 | 2.7 | 3.6 |
| 6-7 hours | 30.9 | 28.2 | 29.9 | 30.4 | 31.3 | 34.7 |
| 7-8 hours | 63.1 | 66.9 | 64.7 | 63.6 | 62.4 | 57.8 |
| ≥9 hours | 3.3 | 3.3 | 3.0 | 3.3 | 3.4 | 3.4 |
| Alcohol consumption, g/d, mean (SD) | 12.7 (34.2) | 14.3 (29.9) | 13.4 (32.5) | 13.0 (35.5) | 12.2 (36.0) | 10.9 (36.8) |
| Fruits and vegetables, servings/1,000 kcal, mean (SD) | 4.0 (1.8) | 4.1 (1.8) | 4.0 (1.8) | 4.0 (1.8) | 3.9 (1.8) | 3.9 (1.9) |
| Whole grains, servings per 1,000 kcal, mean (SD) | 0.69 (0.46) | 0.71 (0.44) | 0.69 (0.45) | 0.69 (0.46) | 0.69 (0.46) | 0.68 (0.48) |
| Total fat, % of energy, mean (SD) | 0.30 (0.08) | 0.29 (0.07) | 0.30 (0.07) | 0.30 (0.08) | 0.30 (0.07) | 0.31(0.0 8) |
| Red meat, g/1,000 kcal, mean (SD) | 33.8 (21.0) | 31.6 (20.5) | 33.3 (20.6) | 34.6 (21.1) | 35.1 (21.1) | 34.6 (21.5) |
| Total energy, kcal/d, mean (SD) | 1,846 (886) | 1,795 (749) | 1,825 (813) | 1,848 (869) | 1,857 (914) | 1,907 (1051) |
| HEI-2005 total score | 67.4 (11.1) | 68.6 (10.5) | 67.8 (10.9) | 67.2 (11.1) | 66.9 (11.3) | 66.4 (11.5) |
| Self-reported health, excellent, % | 18.9 | 26.0 | 20.9 | 17.9 | 15.8 | 13.8 |
| Chronic conditions | ||||||
| Heart disease | 11.9 | 10.8 | 11.5 | 12.1 | 12.8 | 12.6 |
| Stroke | 1.5 | 1.1 | 1.2 | 1.4 | 1.7 | 2.0 |
| Cancer | 12.1 | 12.8 | 12.0 | 12.1 | 12.1 | 11.6 |
| Diabetes | 7.2 | 5.1 | 6.2 | 7.2 | 8.1 | 9.6 |
HEI, health eating index
Over 10 years of follow-up, on average, men gained 0.17 (SD=7.44) kg and women gained 0.96 (SD=7.67) kg. Neighborhood deprivation was positively associated with average weight change over follow-up after adjusting for individual-level factors. Men and women in the most deprived neighborhood gained 0.36 kg and 0.15 kg more weight than the reference group (Appendix Table 4).
The main focus of the study was to examine neighborhood deprivation in relation to excessive weight gain and weight loss separately (Table 2, Figure 1). During the follow up, 8.7% of men and 16.1% of women gained ≥10% of baseline weight and 7.6% of men and 9.5% of women lost ≥10% of baseline weight. In both men and women, neighborhood deprivation was associated with higher risks of both excessive weight gain and loss. The association remained after adjusting for individual indicators of SES, disease conditions, and lifestyle factors (results from Models 2 and 3 in Table 2). There was also a clear dose effect with graded increase in risks with more severe deprivation. Interestingly, there appeared to be a sex difference in the association for both excessive weight gain and weight loss. The neighborhood effect on excessive weight gain was stronger in men, whereas the effect on excessive weight loss was stronger in women (Quintile 5 vs Quintile 1: weight gain, OR=1.36, 95% CI=1.28, 1.45 in men and OR=1.20, 95% CI=1.13, 1.27 in women; weight loss, OR=1.09, 95% CI=1.02, 1.17 in men and OR=1.23, 95% CI=1.14, 1.32 in women). Restricting analysis to participants who lived in the same neighborhood at baseline and follow-up had a minimal impact on the results (Appendix Table 5). Moreover, results from multinomial regressions with a trichotomous outcome (excessive weight gain, excessive weight loss, and no excessive weight gain or loss) were largely similar (Appendix Table 6). Additionally, the association of excessive weight change with individual neighborhood characteristics was examined (Appendix Figure 1). There was a consistent positive association between most of the individual deprivation variables and risk of excessive weight gain and loss.
Table 2. Association Between Neighborhood Socioeconomic Deprivation and Excessive Weight Gain and Loss From 1995-1996 to 2004-2006.
| Neighborhood deprivation | |||||
|---|---|---|---|---|---|
|
|
|||||
| Weight change | Q1 (high SES) | Q2 | Q3 | Q4 | Q5 (low SES) |
| Men (N=153,690) | |||||
| Weight gain, ≥10% | |||||
| No. (%) | 2,242 (6.6) | 2,667 (8.3) | 2,712 (8.8) | 2,821 (9.5) | 2,847 (10.5) |
| OR (95% CI) | |||||
| Model 1 | ref | 1.29 (1.21, 1.37) | 1.40 (1.32, 1.48) | 1.56 (1.47, 1.65) | 1.71 (1.62, 1.82) |
| Model 2 | ref | 1.22 (1.15, 1.29) | 1.27 (1.19, 1.34) | 1.36 (1.28, 1.45) | 1.45 (1.37, 1.55) |
| Model 3 | ref | 1.19 (1.12, 1.26) | 1.22 (1.15, 1.30) | 1.31 (1.23, 1.39) | 1.36 (1.28, 1.45) |
| Weight loss, ≥10% | |||||
| No. (%) | 2,178 (6.4) | 2,261 (7.0) | 2,376 (7.7) | 2,432 (8.2) | 2,332 (8.6) |
| OR (95% CI) | |||||
| Model 1 | ref | 1.02 (0.96, 1.09) | 1.07 (1.00, 1.14) | 1.10 (1.04, 1.17) | 1.14 (1.07, 1.22) |
| Model 2 | ref | 1.02 (0.95, 1.08) | 1.05 (0.99, 1.12) | 1.08 (1.01, 1.15) | 1.12 (1.05, 1.20) |
| Model 3 | ref | 1.01 (0.95, 1.08) | 1.04 (0.98, 1.11) | 1.07 (1.00, 1.14) | 1.09 (1.02, 1.17) |
| Women (N=105,179) | |||||
| Weight gain, ≥10% | |||||
| No. (%) | 2,538 (14.2) | 3,168 (16.2) | 3,349 (16.1) | 3,771 (17.0) | 4,211 (17.1) |
| OR (95% CI) | |||||
| Model 1 | ref | 1.21 (1.14, 1.28) | 1.24 (1.17, 1.31) | 1.37 (1.29, 1.45) | 1.37 (1.30, 1.45) |
| Model 2 | ref | 1.16 (1.10, 1.23) | 1.17 (1.10, 1.24) | 1.26 (1.19, 1.34) | 1.26 (1.19, 1.33) |
| Model 3 | ref | 1.14 (1.07, 1.21) | 1.13 (1.06, 1.19) | 1.22 (1.15, 1.29) | 1.20 (1.13, 1.27) |
| Weight loss, ≥10% | |||||
| No. (%) | 1,260 (7.6) | 1,690 (8.6) | 1,996 (9.6) | 2,309 (10.4) | 2,784 (11.3) |
| OR (95% CI) | |||||
| Model 1 | ref | 1.07 (0.99, 1.15) | 1.10 (1.02, 1.19) | 1.16 (1.08, 1.24) | 1.18 (1.10, 1.27) |
| Model 2 | ref | 1.08 (1.00, 1.17) | 1.13 (1.05, 1.22) | 1.18 (1.10, 1.27) | 1.26 (1.17, 1.35) |
| Model 3 | ref | 1.07 (0.99, 1.16) | 1.11 (1.03, 1.20) | 1.17 (1.09, 1.26) | 1.23 (1.14, 1.32) |
Notes: Model 1: adjusted for age (continuous) and baseline BMI (continuous); Model 2: adjusted for age, baseline BMI, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian or Pacific Islander or American Indian/Alaskan Native, other), education (<12 years, 12 years, post high school, some college, college/post graduate, unknown), and baseline history of heart disease (yes, no), stroke (yes, no), cancer (yes, no) and diabetes (yes, no); Model 3: adjusted for variables in mode 2 and smoking status (never, former, current, unknown), smoking dose (0, 1-10, 11-20, 21-30, 31-40, 41-50, 51-60, >60 cigarettes per day, unknown), year since quitting (never quit, >10, 5-9, 1-4, <1, unknown), vigorous physical activity (never/rarely, <3 times/month, 1-2, 3-4, >5 times/week, unknown), TV viewing (≤2, 3-4, 5-6, 7+ hours, unknown), sleep duration (<5, 5-6, 7-8, 9+ hours, unknown), alcohol drinking (continuous), total caloric intake (continuous), and intake of fruits and vegetables, whole grain, and dietary fat (all continuous and adjusted for total energy intake by dividing intake amount by total calories).
Figure 1.
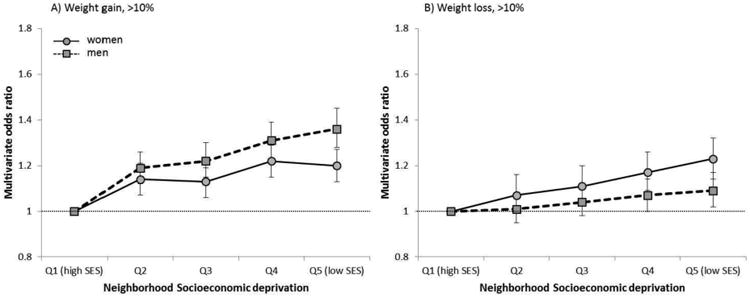
Multivariable OR and 95% CI for excessive weight gain and weight loss during follow-up for quintiles of baseline neighborhood socioeconomic deprivation index.
Notes: Multivariable models adjusted for age (continuous), baseline BMI (continuous), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian or Pacific Islander or American Indian/Alaskan Native, other), education (<12 years, 12 years, post high school, some college, college/post graduate, unknown), baseline history of heart disease (yes, no), stroke (yes, no), cancer (yes, no), and diabetes (yes, no), smoking status (never, former, current, unknown), smoking dose (0, 1-10, 11-20, 21-30, 31-40, 41-50, 51-60, >60 cigarettes per day, unknown), year since quitting (never quit, >10, 5-9, 1-4, <1, unknown), vigorous physical activity (never/rarely, <3 times/month, 1-2, 3-4, >5 times/week, unknown), TV viewing (≤2, 3-4, 5-6, 7+ hours, unknown), sleep duration (<5, 5-6, 7-8, 9+ hours, unknown), alcohol drinking (continuous), total caloric intake (continuous), and intake of fruits and vegetables, whole grain, and dietary fat (all continuous and adjusted for total energy intake by dividing intake amount by total calories). P-for-interaction for sex: <0.0001 for excessive weight gain and 0.57 for excessive weight loss.
Stratified analysis was performed to examine whether the associations between neighborhood deprivation and excessive weight gain and loss differed across subpopulations with different age, education, race, smoking, baseline BMI, physical activity, and chronic conditions (Figure 2). Overall, there was a higher risk of excessive weight gain and loss in more-deprived neighborhoods in most of the subpopulations. However, baseline BMI appeared to be a strong effect modifier for neighborhood effects on excessive weight loss in men (p for interaction, 0.0002) and both excessive weight gain (p<0.0001) and weight loss (p=0.0002) in women, with the associations more pronounced among people with normal BMI (<25 kg/m2) at baseline. The association for excessive weight gain among men was not modified by baseline BMI, but was by smoking, with the strongest effect observed among never smokers (p=0.0006). Another notable finding was that the effects of neighborhood deprivation appeared to be weak or null among blacks and women reporting <12 years of education. However, the authors did not detect a statistically significant interaction with race and education, probably due to the small sample size of blacks and people with <12 years of education.
Figure 2.
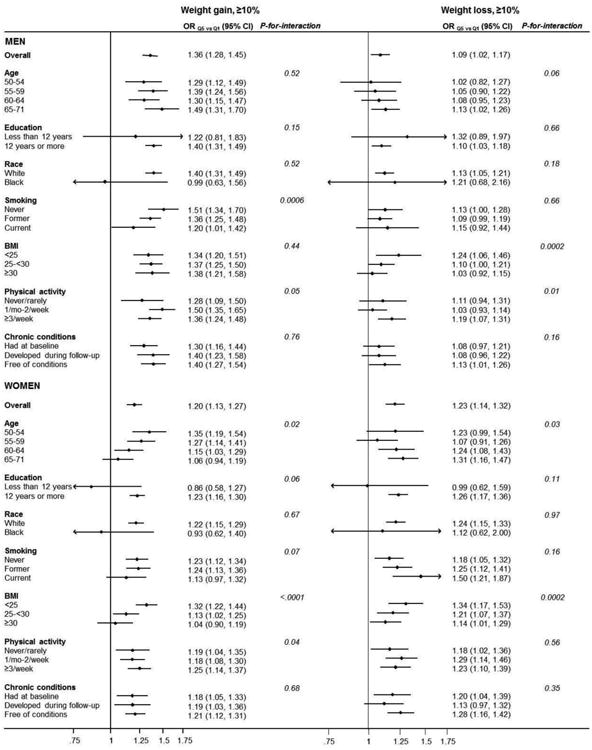
Prospective association between baseline neighborhood socioeconomic deprivation index and excessive weight gain and weight loss from 1995-1996 to 2004-2006, by sex and across subgroups with different age, education, race, smoking, BMI, physical activity, and chronic conditions.a
Notes: The ORs and 95% CIs were calculated comparing the 5th quintile(most deprived) of neighborhood socioeconomic deprivation index with the 1st quintile(least deprived), adjusted for age (continuous), baseline BMI (continuous), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian or Pacific Islander or American Indian/Alaskan Native, other), education (<12 years, 12 years, post high school, some college, college/post graduate, unknown), baseline history of heart disease (yes, no), stroke (yes, no), cancer (yes, no) and diabetes (yes, no), smoking status (never, former, current, unknown), smoking dose (0, 1-10, 11-20, 21-30, 31-40, 41-50, 51-60, >60 cigarettes per day, unknown), year since quitting (never quit, >10, 5-9, 1-4, <1, unknown), vigorous physical activity (never/rarely, <3 times/month, 1-2, 3-4, >5 times/week, unknown), TV viewing (≤2, 3-4, 5-6, 7+ hours, unknown), sleep duration (<5, 5-6, 7-8, 9+ hours, unknown), alcohol drinking (continuous), total caloric intake (continuous), and intake of fruits and vegetables, whole grain, and dietary fat (all continuous and adjusted for total energy intake by dividing intake amount by total calories). Covariate that was stratified by was not adjusted in the respective analysis. P-for-interaction refers to the p-value for the cross-product term of neighborhood SES and stratifying variables.
aRefers to any of the following conditions: diabetes, cancer, cardiovascular diseases, emphysema, and renal disease.
Finally, a higher risk of developing obesity was observed among participants living in more-deprived neighborhoods (Appendix Figure 2). Compared with the reference group, men and women in the most deprived neighborhood had a 17%–20% increased risk of developing obesity (Quintile 5 vs Quintile 1: OR=1.20, 95% CI=1.11, 1.30 for men and OR=1.17, 95% CI=1.06, 1.29 for women).
Discussion
In a large cohort of American men and women aged 50–71 years at baseline, those who lived in neighborhoods with greater socioeconomic deprivation exhibited a higher risk of gaining or losing >10% of baseline weight over 10 years of follow up. Given that both excessive weight gain and weight loss are established risk factors for poor health and high mortality in the older adults,1 these results highlight the adverse health effects of neighborhood deprivation, even after adjusting for individual-level health behaviors.
Previous prospective studies on neighborhood deprivation and weight change reported mixed results. In the Atherosclerosis Risk in Communities Study9 and women in the American's Changing Lives survey,13 researchers found that low neighborhood SES was associated with higher BMI at baseline, but not with the longitudinal trend in BMI. However, three other studies in the Black Women's Health Study,10 the Whitehall II Study,11 and the Dallas Heart Study12 all reported a positive association between more severe neighborhood deprivation and weight gain. The heterogeneity in study populations in earlier studies may partially account for the inconsistency among their findings. As the results from subgroup analysis of the current study show, the neighborhood effects on weight could differ by a number of factors, such as gender, smoking, and baseline BMI. More importantly, the mixed results from earlier studies may be due to the fact that all studies focused on average weight change without investigating weight gain and weight loss separately. This is especially problematic for studies of the older population, as weight loss becomes more prevalent.15 Because both weight loss and weight gain were associated with neighborhood deprivation, their combined effects could reduce associations between average weight change and such deprivation. This did occur in this study, and is reflected in the small aggregate difference in weight change (<0.4 kg) between the most and least deprived neighborhoods. Average weight change does not accurately reflect the different weight trajectories of individuals, and future studies on neighborhood environment and weight status should examine weight gain and weight loss separately.
More severe neighborhood deprivation was associated with higher risk of excessive weight gain and developing obesity in both men and women. The finding is consistent with that from the Black Women's Health Study, which reported a 32% increase in risk of obesity comparing the highest quintile of neighborhood deprivation with the lowest.10 A leading hypothesis postulates that lower SES neighborhoods are less walkable, have fewer recreational options, and lack of access to healthy food choices, which lead to a sedentary lifestyle, unhealthy diet, and ultimately obesity.26 However, adjusting for baseline lifestyle factors such as physical activity, TV viewing, and diet only had a small impact on the present results (<10% change in effect size), suggesting that other mechanisms may also be in play. One important mechanism may be through stress response. In disadvantaged neighborhoods, street violence, material deprivation, and an impaired social support network create a stressful environment.27 Living in such an environment leads to chronic activation of the hypothalamic-pituitary-adrenal axis and elevated levels of cortisol, which promotes fat accumulation, especially in the visceral fat tissue.14
Interestingly, this study found that in men, the association between neighborhood deprivation and weight gain was stronger and higher in magnitude than in women. This difference appeared to be explained primarily by difference in associations between the older men and women. Though the effects of neighborhood deprivation decreased substantially with age among women, the associations between neighborhood SES and excessive weight gain remained strong among older men. Moreover, although the modest sample size for blacks (<4%) and people with <12 years of education (<6%) in this study population makes it difficult to draw a definite conclusion and the results were not statistically significant, neighborhood deprivation seemed to have a weaker effect on blacks and on women who had low education. Similarly, in the Black Women's Health Study, researchers also found no association between weight gain and neighborhood SES among women with ≤12 years of education.10 Future studies are needed to examine whether the same neighborhood environments may have different psychological and physical impact on people with different demographic characteristics and individual-level SES.
Weight loss in the older population can be caused by chronic diseases such as cancer.14,15 In the current study, the association between neighborhood deprivation and weight loss was maintained among participants who were free of cancer, heart disease, stroke, and diabetes throughout follow-up, suggesting that these conditions were not responsible for the observed association.
However, the authors could not exclude the possible impact of other or undiagnosed conditions. For example, gastrointestinal disease and psychiatric conditions such as depression and dementia are among the most common medical causes of weight loss,15,28 and previous studies have linked neighborhood deprivation with gastrointestinal conditions and depression.29,30 In addition, research has suggested that social isolation and poverty, which are prevalent in poor neighborhoods, can also contribute to weight loss through poor diet and malnutrition.14 General recommendations for treating weight loss in the older population typically focus on appetite enhancement, dietary modification, and nutritional supplements.14,15 However, both health service and dietary choices are often limited for the residents of poor neighborhoods, making the diagnosis and management of weight loss especially difficult. With research increasingly focusing on obesogenic characteristics of poor neighborhood in recent years, weight loss is often overlooked in this population. The authors suggest that the medical and public health community pay more attention to weight loss among the older residents of disadvantaged neighborhoods, and further studies are needed to investigate the scale of the weight loss burden among this population.
Limitations
This study has some limitations. One major limitation is that the baseline neighborhood addresses were reported in 1995–1996, whereas data from the 2000 Census were used to characterize neighborhood conditions. Therefore, two factors could introduce bias and error in exposure measurement: (1) people might have moved out of their neighborhood between the two time periods; and (2) neighborhood conditions might have changed between the mid-90s and 2000. The results changed little when the analysis was restricted to those reporting living in the same neighborhood in 1995–1996 and 2004-–006, suggesting that movers had only a minimal influence on these results. However, the authors could not assess the impact of changing neighborhood conditions as they did not have information about neighborhood deprivation at follow-up. The outcome was measured by self-reported information on weight, which is subject to reporting error and the validity of self-reported weight was influenced by factors like sex, age, race, and education. Although a study found that such biases tend to be stable over time and therefore bias in weight change may be smaller than that in actual weight,31 the authors cannot rule out some bias associated with our self-reported measures. Another limitation is that weight was only assessed at two time points and therefore could not examine a more complete longitudinal weight trajectory in relation to neighborhood deprivation. For example, weight fluctuation could not be assessed within the follow-up period, which is also an important risk factor for higher mortality.32 Also, the study could not distinguish between unintentional and intentional weight loss. However, the association between neighborhood deprivation and weight loss was most pronounced among participants with a normal BMI at baseline. As those who were not overweight or obese would be less likely to undergo intentional weight loss, this finding suggested that the observed effects of neighborhood deprivation on excessive weight loss could not be driven by intentional weight loss alone. Additionally, the authors only had baseline information for most of the covariates, and were not able to evaluate potential changes in those covariate and their impact on the results. Moreover, logistic regression yields an OR that approximates relative risk when the incidence of outcome is <10%. In this study, the incidence of excessive weight gain in was 16.1%, and therefore the actual relative risk for this outcome would be somewhat lower than the OR.
A major strength of the current study is its large sample size. This has allowed the authors to not only investigate the relatively small number of excessive weight gain and loss as the main outcomes, but also perform stratified analysis to examine the potential modifying effect of individual factors. Another strength is its prospective design, which has allowed the authors to focus on weight change, which has important health implication in the older population, independent of baseline weight status.
Conclusions
This study shows that neighborhood deprivation predicts a higher risk for both substantial weight gain and weight loss in the middle- to older-aged population. The findings reinforce the emerging evidence that both weight gain and weight loss are important for health and health disparities. Future studies of neighborhood deprivation and energy balance should address disparities in the underlying causes of unhealthy weight loss as well as disparities in the causes of weight gain.
Supplementary Material
Acknowledgments
The work was supported by the Intramural Research Program of NIH, National Cancer Institute, NIH, DHHS.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Andres R, Muller DC, Sorkin JD. Long-term effects of change in body weight on all-cause mortality. A review. Ann Intern Med. 1993;119(7 Pt 2):737–743. doi: 10.7326/0003-4819-119-7_part_2-199310011-00022. https://doi.org/10.7326/0003-4819-119-7_Part_2-199310011-00022. [DOI] [PubMed] [Google Scholar]
- 2.Zamboni M, Mazzali G, Zoico E, et al. Health consequences of obesity in the elderly: a review of four unresolved questions. Int J Obes (Lond) 2005;29(9):1011–1029. doi: 10.1038/sj.ijo.0803005. https://doi.org/10.1038/sj.ijo.0803005. [DOI] [PubMed] [Google Scholar]
- 3.Han TS, Tajar A, Lean ME. Obesity and weight management in the elderly. Br Med Bull. 2011;97:169–196. doi: 10.1093/bmb/ldr002. https://doi.org/10.1093/bmb/ldr002. [DOI] [PubMed] [Google Scholar]
- 4.Miller SL, Wolfe RR. The danger of weight loss in the elderly. J Nutr Health Aging. 2008;12(7):487–491. doi: 10.1007/BF02982710. https://doi.org/10.1007/BF02982710. [DOI] [PubMed] [Google Scholar]
- 5.Losonczy KG, Harris TB, Cornoni-Huntley J, et al. Does weight loss from middle age to old age explain the inverse weight mortality relation in old age? Am J Epidemiol. 1995;141(4):312–321. doi: 10.1093/aje/141.4.312. https://doi.org/10.1093/aje/141.4.312. [DOI] [PubMed] [Google Scholar]
- 6.Corsi DJ, Finlay JE, Subramanian SV. Weight of communities: a multilevel analysis of body mass index in 32,814 neighborhoods in 57 low- to middle-income countries (LMICs) Soc Sci Med. 2012;75(2):311–322. doi: 10.1016/j.socscimed.2012.02.014. https://doi.org/10.1016/j.socscimed.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 7.Black JL, Macinko J. The changing distribution and determinants of obesity in the neighborhoods of New York City, 2003-2007. Am J Epidemiol. 2010;171(7):765–775. doi: 10.1093/aje/kwp458. https://doi.org/10.1093/aje/kwp458. [DOI] [PubMed] [Google Scholar]
- 8.Laraia BA, Karter AJ, Warton EM, Schillinger D, Moffet HH, Adler N. Place matters: neighborhood deprivation and cardiometabolic risk factors in the Diabetes Study of Northern California (DISTANCE) Soc Sci Med. 2012;74(7):1082–1090. doi: 10.1016/j.socscimed.2011.11.036. https://doi.org/10.1016/j.socscimed.2011.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mujahid MS, Diez Roux AV, Borrell LN, Nieto FJ. Cross-sectional and longitudinal associations of BMI with socioeconomic characteristics. Obes Res. 2005;13(8):1412–1421. doi: 10.1038/oby.2005.171. https://doi.org/10.1038/oby.2005.171. [DOI] [PubMed] [Google Scholar]
- 10.Coogan PF, Cozier YC, Krishnan S, et al. Neighborhood socioeconomic status in relation to 10-year weight gain in the Black Women's Health Study. Obesity (Silver Spring) 2010;18(10):2064–2065. doi: 10.1038/oby.2010.69. https://doi.org/10.1038/oby.2010.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stafford M, Brunner EJ, Head J, Ross NA. Deprivation and the development of obesity a multilevel, longitudinal study in England. Am J Prev Med. 2010;39(2):130–139. doi: 10.1016/j.amepre.2010.03.021. https://doi.org/10.1016/j.amepre.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 12.Powell-Wiley TM, Ayers C, Agyemang P, et al. Neighborhood-level socioeconomic deprivation predicts weight gain in a multi-ethnic population: longitudinal data from the Dallas Heart Study. Prev Med. 2014;66:22–27. doi: 10.1016/j.ypmed.2014.05.011. https://doi.org/10.1016/j.ypmed.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruel E, Reither EN, Robert SA, Lantz PM. Neighborhood effects on BMI trends: examining BMI trajectories for Black and White women. Health Place. 2010;16(2):191–198. doi: 10.1016/j.healthplace.2009.09.009. https://doi.org/10.1016/j.healthplace.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McMinn J, Steel C, Bowman A. Investigation and management of unintentional weight loss in older adults. BMJ. 2011;342:d1732. doi: 10.1136/bmj.d1732. https://doi.org/10.1136/bmj.d1732. [DOI] [PubMed] [Google Scholar]
- 15.Gaddey HL, Holder K. Unintentional weight loss in older adults. Am Fam Physician. 2014;89(9):718–722. [PubMed] [Google Scholar]
- 16.Doubeni CA, Laiyemo AO, Major JM, et al. Socioeconomic status and the risk of colorectal cancer: an analysis of more than a half million adults in the National Institutes of Health-AARP Diet and Health Study. Cancer. 2012;118(14):3636–3644. doi: 10.1002/cncr.26677. https://doi.org/10.1002/cncr.26677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doubeni CA, Major JM, Laiyemo AO, et al. Contribution of behavioral risk factors and obesity to socioeconomic differences in colorectal cancer incidence. J Natl Cancer Inst. 2012;104(18):1353–1362. doi: 10.1093/jnci/djs346. https://doi.org/10.1093/jnci/djs346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doubeni CA, Schootman M, Major JM, et al. Health status, neighborhood socioeconomic context, and premature mortality in the United States: The National Institutes of Health-AARP Diet and Health Study. Am J Public Health. 2012;102(4):680–688. doi: 10.2105/AJPH.2011.300158. https://doi.org/10.2105/AJPH.2011.300158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lian M, Schootman M, Doubeni CA, et al. Geographic variation in colorectal cancer survival and the role of small-area socioeconomic deprivation: a multilevel survival analysis of the NIH-AARP Diet and Health Study Cohort. Am J Epidemiol. 2011;174(7):828–838. doi: 10.1093/aje/kwr162. https://doi.org/10.1093/aje/kwr162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Major JM, Cross AJ, Doubeni CA, et al. Socioeconomic deprivation impact on meat intake and mortality: NIH-AARP Diet and Health Study. Cancer Causes Control. 2011;22(12):1699–1707. doi: 10.1007/s10552-011-9846-0. https://doi.org/10.1007/s10552-011-9846-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Major JM, Doubeni CA, Freedman ND, et al. Neighborhood socioeconomic deprivation and mortality: NIH-AARP diet and health study. PLoS One. 2010;5(11):e15538. doi: 10.1371/journal.pone.0015538. https://doi.org/10.1371/journal.pone.0015538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schatzkin A, Subar AF, Thompson FE, et al. Design and serendipity in establishing a large cohort with wide dietary intake distributions : the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol. 2001;154(12):1119–1125. doi: 10.1093/aje/154.12.1119. https://doi.org/10.1093/aje/154.12.1119. [DOI] [PubMed] [Google Scholar]
- 23.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83(6):1041–1062. doi: 10.1007/s11524-006-9094-x. https://doi.org/10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wannamethee SG, Shaper AG, Walker M. Weight change, body weight and mortality: the impact of smoking and ill health. Int J Epidemiol. 2001;30(4):777–786. doi: 10.1093/ije/30.4.777. https://doi.org/10.1093/ije/30.4.777. [DOI] [PubMed] [Google Scholar]
- 25.Hosmer DW, L S, Cook ED. Applied Logistic Regression. 2nd. Wiley-Interscience; 2001. [Google Scholar]
- 26.Sallis JF, Floyd MF, Rodriguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729–737. doi: 10.1161/CIRCULATIONAHA.110.969022. https://doi.org/10.1161/CIRCULATIONAHA.110.969022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen E, Miller GE. Socioeconomic status and health: mediating and moderating factors. Annu Rev Clin Psychol. 2013;9:723–749. doi: 10.1146/annurev-clinpsy-050212-185634. https://doi.org/10.1146/annurev-clinpsy-050212-185634. [DOI] [PubMed] [Google Scholar]
- 28.Stajkovic S, Aitken EM, Holroyd-Leduc J. Unintentional weight loss in older adults. CMAJ. 2011;183(4):443–449. doi: 10.1503/cmaj.101471. https://doi.org/10.1503/cmaj.101471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ritchie CS, Locher JL, Roth DL, McVie T, Sawyer P, Allman R. Unintentional weight loss predicts decline in activities of daily living function and life-space mobility over 4 years among community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2008;63(1):67–75. doi: 10.1093/gerona/63.1.67. https://doi.org/10.1093/gerona/63.1.67. [DOI] [PubMed] [Google Scholar]
- 30.Alibhai SM, Greenwood C, Payette H. An approach to the management of unintentional weight loss in elderly people. CMAJ. 2005;172(6):773–780. doi: 10.1503/cmaj.1031527. https://doi.org/10.1503/cmaj.1031527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hattori A, Sturm R. The obesity epidemic and changes in self-report biases in BMI. Obesity (Silver Spring) 2013;21(4):856–860. doi: 10.1002/oby.20313. https://doi.org/10.1002/oby.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Muls E, Kempen K, Vansant G, Saris W. Is weight cycling detrimental to health? A review of the literature in humans. Int J Obes Relat Metab Disord. 1995;19(Suppl 3):S46–50. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


