Abstract
Introduction
Although pre-exposure prophylaxis (PrEP) greatly reduces risk of HIV infection in HIV-negative individuals, use is not widespread enough to impact HIV incidence. Involvement of primary care physicians (PCPs) in PrEP prescription is essential, but previous research has shown low rates of prescription among PCPs. To identify targets for interventions, the information–motivation–behavioral skills model for PrEP discussion and prescription was tested in a ten-city sample of PCPs.
Methods
PCPs from ZIP codes with high HIV incidence in ten U.S. cities (N=280, 52% male, 56% white) completed a survey online between July 2014 and May 2015. Information items assessed knowledge, motivation items evaluated attitudes, and behavioral skills items measured comfort with behaviors involved in prescribing PrEP. Providers indicated whether they had discussed PrEP with or prescribed PrEP to patients. Data were analyzed in 2015 and 2016.
Results
One third of PCPs had discussed and 17% had prescribed PrEP. A structural equation model with good fit supported the information–motivation–behavioral skills model. Information and motivation predicted behavioral skills (b=0.35, 95% CI=0.13, 0.57 and b=0.31, 95% CI=0.14, 0.47, respectively). Behavioral skills predicted prescription (OR=1.31, 95% CI=1.13, 1.53). Behavioral skills mediated effects of information and motivation on prescription (OR=1.10, 95% CI=1.03, 1.21 and OR=1.09, 95% CI=1.03, 1.17, respectively).
Conclusions
The information–motivation–behavioral skills model can be applied to PCPs’ PrEP discussion and prescription. Its constructs represent potential targets for PCP-directed interventions to increase PrEP use in high-risk populations.
INTRODUCTION
With nearly 50,000 new infections annually in the U.S.,1 HIV remains a critical health challenge. Pre-exposure prophylaxis (PrEP) reduces the risk of HIV infection in HIV-negative individuals by 44%–86%2 in at-risk populations, with even greater reductions among those who are most adherent.3,4 Thus, PrEP could significantly impact the HIV epidemic if it reached at-risk populations.
Although uptake has been growing consistently,5 PrEP use has not become widespread enough to impact HIV incidence.6 It is estimated that 1.2 million U.S. adults would benefit from being on PrEP7; however, only an estimated 49,000 people are currently taking it.8 PrEP must be delivered by healthcare providers, and to attain its full potential, PrEP must be offered to those at highest HIV risk, some of whom may have lower levels of awareness about PrEP (e.g., African American men who have sex with men).9,10 Thus, widespread access to PrEP depends on healthcare providers, especially primary care physicians (PCPs), taking an active role in discussing and prescribing PrEP.
Unfortunately, rates of PrEP prescription among PCPs are low. Although PCPs encounter patients who may benefit from PrEP, they may not be aware of PrEP or comfortable prescribing it. Only a minority of PCPs (28%–45%) currently indicate a willingness to prescribe PrEP,11 and fewer still (0%–17%) have prescribed it.12–15 Notably, relatively few studies have evaluated the PrEP experiences of non-HIV providers.11,12,15–18
Interventions targeting providers may be one way to increase PrEP prescription among PCPs. To design effective interventions, it is necessary to know what theoretic constructs should be targeted to increase discussions and prescriptions of PrEP. The information–motivation–behavioral skills (IMB) model19 is one theoretic model relevant to HIV that may be useful in describing the PrEP behaviors of PCPs. This model, traditionally used to predict HIV-related health and risk behaviors, theorizes that that information about the targeted behavior and motivation to perform the behavior (e.g., positive attitudes or social norms) lead to the development of relevant behavioral skills (individuals’ objective and perceived abilities to perform the target behavior). These behavioral skills then contribute directly to the outcome behavior and also partially mediate associations between information and motivation and behavior itself. This model is well supported by research,20,21 typically explaining 35%–51% of the variance in behavior.21
The IMB model may also be effective in predicting health provider behaviors. Research with different types of providers has shown that theoretic constructs in models of health behavior predict behaviors such as pharmacists’ adjustment of medication regimens,22 nurses’ proper measurement of blood pressure,23 and nurses’ support of breastfeeding mothers.24 Additionally, these constructs are predictive of behavioral precursors such as providers’ intentions and willingness to engage in various behaviors.25,26 Factors predicting provider intentions and behavior that are in line with the IMB model include knowledge,24,27 attitudes,24,25 and perceived control and beliefs about capabilities.22,23,25–27 Overall, a review suggested that constructs from health behavior theories explain an average of 31% of the variance in target behaviors of health providers.27 Regarding PrEP specifically, PrEP knowledge is associated with willingness to prescribe PrEP28 as well as future intention to prescribe and experience prescribing PrEP among HIV and non-HIV providers,15 and PrEP prescription self-efficacy is associated with intentions to prescribe PrEP.11 No studies have tested the IMB model in predicting PrEP behaviors among health providers.
In the current study, to identify theoretic constructs associated with PCPs’ PrEP behaviors, the IMB model was tested in relation to PrEP discussion and prescription in a sample of PCPs from ten U.S. cities. Analyses addressed two research questions:
Are information, motivation, and behavioral skills associated with PrEP discussion and prescription? In line with the IMB model, hypotheses were that information (knowledge about PrEP) and motivation (attitudes toward PrEP) would be associated with behavioral skills (confidence in prescribing PrEP) and, in turn, behavioral skills would be associated with both PrEP discussion with patients and prescribing PrEP to patients.
Do behavioral skills mediate associations between information and motivation and PrEP discussion and prescription? In line with the IMB model, hypotheses were that behavioral skills would mediate associations between information and motivation and discussion and prescription.
METHODS
Study Population
As part of a larger survey, data were collected from PCPs (including physicians, nurse practitioners, and physician assistants) between July 2014 and May 2015. Participants in the larger study, which included both PCPs and HIV providers, were classified as PCPs if they did not provide HIV-related care to patients in their practice.
Potential participants were recruited using databases from three professional organizations. Only providers who practiced in the ten U.S. cities with the largest number of prevalent HIV cases were recruited; recruitment was further restricted to providers whose practices were within ZIP codes where HIV prevalence was at least 0.5%—greater than the U.S. prevalence of 0.3%29—to ensure the relevance of HIV prevention.
For the larger study, potential participants were sent an invitation by postal mail or e-mail, if available. Unique login and password combinations allowed entry into the online survey. Eligibility criteria included:
spending at least 4 hours per week working in an ambulatory setting;
having patients aged 13–64 years in their practice patient population; and
describing their practice as family medicine, internal medicine, internal medicine/pediatrics, obstetrics/gynecology, infectious diseases, or HIV medicine (no PCPs described their practice as HIV medicine).
Up to three reminders were sent to non-responders. Participants completing the survey were eligible to receive a $100 honorarium. An estimated 2,088 potential participants were sent an invitation, and 627 individuals entered the study website, yielding a response rate of approximately 30%. Of these, 525 individuals (280 PCPs and 245 HIV providers) met the study eligibility criteria, provided informed consent, and took the survey. The analytic sample comprised the 280 PCPs.
This study was approved by the IRB at the Medical College of Wisconsin.
Measures
No established measures of study constructs were available; therefore, measures were developed by the second author based on previous work and theoretic considerations. A 15-member expert panel consisting of PCPs, HIV providers, and HIV prevention researchers reviewed all measure items, and measures were revised based on their recommendations. Measures were then pilot tested by 25 providers meeting study eligibility criteria but located outside of the ten targeted cities; minor clarifications to wording resulted from their feedback.
For purposes of structural equation modeling, individual items for each construct were grouped into three parcels of items representing average scores on sets of items; these parcels served as the indicators for latent constructs. Parcels were formed based on the balancing of factor loadings.30
To assess information, participants were asked whether they were aware of the concept of HIV PrEP. Those who were aware of PrEP indicated how familiar they considered themselves with prescribing PrEP. Providers who indicated that they were somewhat or very familiar were asked seven factual multiple-choice questions about PrEP based on the Centers for Disease Control and Prevention guidelines (e.g., How often should individuals be tested for HIV while taking PrEP?; Appendix lists all items). Their answers were scored as correct (1) or incorrect (0). This scale had adequate reliability (α=0.71). Participants who were unaware or unfamiliar with PrEP were assumed to lack knowledge of the details of prescribing PrEP and received zeroes as scores, consistent with other knowledge scales where don’t know responses are considered incorrect.31 Higher construct scores indicated greater knowledge.
To assess motivation, participants rated their level of agreement with eight items assessing attitudes toward PrEP (Table 1) on a 5-point scale from completely disagree to completely agree. This scale had adequate reliability (α=0.80). Higher construct scores indicated more positive attitudes.
Table 1.
Items Assessing Primary Care Physicians’ PrEP Motivation and Behavioral Skills.
| Motivation: PrEP attitudes (1=completely disagree, 5=completely agree) | M (SD) |
Factor loading |
| 1. PrEP can be a cost-effective HIV prevention intervention if used with an appropriate population of patients. |
3.98 (0.86) |
0.57 |
| 2. PrEP is too costly to warrant its use. (R) | 3.31 (0.94) |
0.66 |
| 3. Individuals who are at risk for HIV should be encouraged to use condoms rather than to take PrEP. (R) |
2.92 (1.13) |
0.60 |
| 4. Individuals who take PrEP are likely to increase their sexual risk behaviors and negate the benefits of PrEP. (R) |
3.25 (1.04) |
0.77 |
| 5. Money should not be spent on HIV prevention for men who have sex with men. (R) |
4.45 (0.88) |
0.57 |
| 6. There is insufficient evidence at this time for me to consider PrEP an appropriate preventive treatment option. (R) |
3.66 (1.09) |
0.72 |
| 7. Widespread use of PrEP will likely significantly increase rates of antiretroviral resistance. (R) |
3.02 (0.93) |
0.63 |
| 8. Individuals who are prescribed PrEP are not likely to adhere to their medication. (R) |
3.27 (0.91) |
0.68 |
|
Behavioral skills: Comfort prescribing PrEP (1=completely uncomfortable, 5=completely comfortable) |
||
| Please rate how uncomfortable or comfortable you are with the following: | ||
| 1. Determining whether a patient’s sexual risk behaviors warrant the use of PrEP. |
3.64 (1.11) |
0.82 |
| 2. Determining whether a patient’s IV drug use behaviors warrant the use of PrEP. |
3.75 (1.17) |
0.80 |
| 3. Discussing the efficacy of PrEP with a patient. | 3.58 (1.24) |
0.89 |
| 4. Discussing whether PrEP is a good option for a patient. | 3.57 (1.21) |
0.89 |
| 5. Discussing the potential side effects of the antiretroviral medications used for PrEP (emtricitabine and tenofovir, together called Truvada) with a patient. |
3.21 (1.28) |
0.85 |
| 6. Determining whether a patient has a contraindication to using PrEP. | 3.31 (1.24) |
0.87 |
| 7. Prescribing PrEP to a patient for whom PrEP was appropriate and no contraindications were apparent. |
3.55 (1.26) |
0.86 |
| 8. Following patients on PrEP to monitor for side effects. | 3.46 (1.30) |
0.87 |
| 9. Following patients on PrEP to test them for HIV. | 3.85 (1.19) |
0.84 |
Notes: Item descriptive statistics are reported for primary care physicians from 10 U.S. cities (N=280). All descriptive statistics apply to items following reverse-coding.
PrEP, pre-exposure prophylaxis; R, items reverse-coded for scoring.
To assess behavioral skills, participants indicated their level of comfort with nine behaviors involved in prescribing PrEP (Table 1) on a 5-point scale from completely uncomfortable to completely comfortable. This scale had high reliability (α=0.95). Higher construct scores indicated greater comfort.
Providers indicated whether they had ever discussed PrEP with a patient and whether they had ever prescribed PrEP to a patient.
A number of demographic and practice features were considered as control variables. Participants indicated their sex, age, race/ethnicity, professional position, and specialty area. Location was treated as a clustering variable.
Statistical Analysis
Missing data rates ranged from 1% to 13%, with most missing data occurring on demographic variables. Overall, 5% of data were missing. Multiple imputation, a modern method for dealing with missing data, was used to replace missing values.32 All study variables were included when imputing 100 data sets in Mplus, version 7. Analyses were conducted with all data sets, and parameter estimates were pooled using the imputation algorithms in Mplus.
The primary analyses were conducted using structural equation modeling, allowing for tests of the direct and indirect associations hypothesized by the IMB model. Information, motivation, and behavioral skills were represented as latent constructs with three indicators each (described in Measures section), whereas PrEP discussion and prescription were manifest variables. Latent constructs were identified by fixing variance at 1.
First, a measurement model was tested to assure latent constructs were adequate representations. Next, a structural model including the full IMB model and covariates was constructed. In this model, directional paths led from information and motivation to behavioral skills, discussion, and prescription, and from behavioral skills to discussion and prescription, in line with hypotheses. Additionally, paths led from covariates to all constructs; covariates were maintained in the model if they were associated with outcomes at the p<0.10 level. Information and motivation were allowed to correlate, as were discussion and prescription.
Models were fit with a robust weighted least squares estimator in Mplus. Model fit was assessed using traditional fit indices,33 including the comparative fit index (CFI), the Tucker–Lewis index (TLI), and the root-mean-square error of approximation (RMSEA). Good fit was indicated by CFI and TLI values >0.95 and RMSEA values <0.05. Given the use of multiple imputation, these fit indices were averages over 100 imputations. Standardized factor loadings, correlations, unstandardized coefficients (for continuous outcome variables), ORs (for categorical outcome variables), and 95% CIs are reported.
When testing mediation, 95% CIs were calculated using the distribution-of-the-product method in RMediation. This is recommended given the non-normal distribution of indirect effects.34 For indirect effects, unstandardized coefficients and 95% CIs as well as ORs are reported.
All analyses accounted for clustering by metropolitan area using TYPE=COMPLEX in Mplus, which involves SEs adjusted with a sandwich estimator. Study analyses were conducted in 2015 and 2016.
RESULTS
Demographic, practice, and patient characteristics are summarized in Table 2. The sample included 280 PCPs (52% male; mean age, 50 [SD=8] years; 56% white). Between 6% and 15% came from each of the ten metropolitan areas. Most (62%) specialized in internal medicine, and nearly all (94%) were physicians.
Table 2.
Demographic, Practice, and Patient Characteristics of Study Participants (N=280)
| Demographic characteristics | % | M (SD) |
|---|---|---|
| Male | 52% | |
| Age | 50.4 (8.0) | |
| Race/ethnicity | ||
| White | 56% | |
| Asian/Asian American | 24% | |
| Black/African American | 10% | |
| Other races | 2% | |
| Latino/Latina | 12% | |
| Location | ||
| Atlanta | 11% | |
| Chicago | 12% | |
| Dallas | 11% | |
| Houston | 15% | |
| LA | 11% | |
| NYC | 9% | |
| Miami | 6% | |
| Philadelphia | 10% | |
| San Francisco | 9% | |
| Washington, DC | 7% | |
| Practice characteristics | ||
| Professional position | ||
| Physician | 94% | |
| Nurse practitioner | 6% | |
| Physician assistant | <1% | |
| Specialty area | ||
| Internal medicine | 62% | |
| Family medicine | 38% | |
| Hours per week in ambulatory setting | ||
| More than 24 | 73% | |
| 17–24 | 12% | |
| 4–16 | 15% | |
| Practice setting | ||
| Private – solo practice | 25% | |
| Private – group practice | 33% | |
| Public hospital/hospital-based clinic | 7% | |
| Community health center | 8% | |
| Academic/university-based hospital or clinic | 22% | |
| Veteran’s Administration clinic or hospital | 2% | |
| Other | 3% | |
| Years licensed | 19.7 (8.2) | |
| Patient characteristics | ||
| Majority of patients ages 13–64 | 78% | |
| Est. percentage of patients who are MSM | ||
| 1–25% | 84% | |
| More than 25% | 4% | |
| Don’t know | 12% | |
| Est. percentage of patients with Medicare/Medicaid | 34% (23%) | |
| Est. percentage of patients who are uninsured | 9% (11%) | |
| Est. number of HIV negative patients | 1,374.3 (1397.9) | |
| Est. number of HIV positive patients | 12.4 (16.0) | |
LA, Los Angeles; NYC, New York City; Est., estimated
Descriptive information related to IMB constructs and PrEP behaviors is included in Table 3. PCPs generally indicated low levels of familiarity with and knowledge of PrEP. Although 75% were aware of PrEP, of those with awareness, only 37% indicated they were somewhat or very familiar with PrEP. These providers answered an average of 67% of knowledge items correctly. Attitudes toward PrEP and confidence related to PrEP prescription were both moderate. One third (33%) of PCPs had discussed PrEP with patients, and only 17% had prescribed PrEP.
Table 3.
PrEP Descriptive Statistics for Primary Care Physicians From 10 U.S. Cities (N=280)
| Study construct | % | M (SD) |
|---|---|---|
| Information | ||
| Aware of PrEP | 75% | |
| Somewhat or very familiar with PrEP | 37% | |
| PrEP knowledge (range: 0–7) | 4.7 (1.9) | |
| Motivation | ||
| PrEP attitudes (range: 1–5) | 3.5 (0.6) | |
| Behavioral skills | ||
| Comfort prescribing PrEP (range: 1–5) | 3.5 (1.0) | |
| PrEP discussion (Ever) | 33% | |
| PrEP prescription (Ever) | 17% |
PrEP, pre-exposure prophylaxis
The measurement model was a good fit to the data (χ2[24, N=280] = 41.40, RMSEA=0.05, CFI=0.99, TLI=0.99). All factor loadings were positive and significant (B>0.75, p<0.001 for all). This model showed the expected positive correlations between IMB constructs: information was correlated with both motivation (r=0.38, 95% CI=0.27, 0.49) and behavioral skills (r=0.39, 95% CI=0.28, 0.51), and motivation was correlated with behavioral skills (r=0.34, 95% CI=0.19, 0.50).
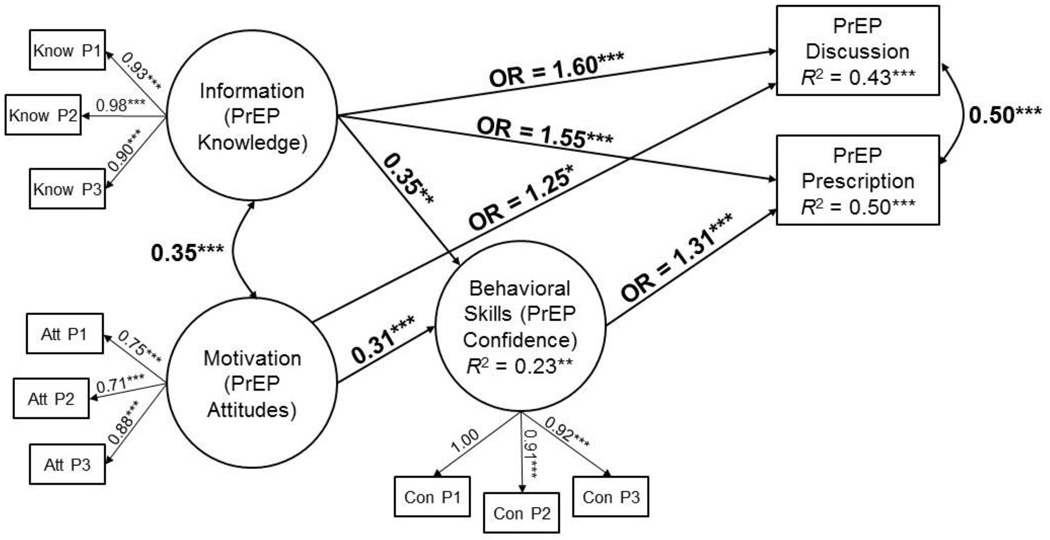
The structural model was a good fit to the data (χ2[66, N=280] = 73.45, RMSEA=0.02, CFI=0.98, TLI=0.97). Results (Figure 1) generally supported the IMB model. In line with hypotheses, both information and motivation were positively associated with behavioral skills (b=0.35, 95% CI=0.13, 0.57 and b=0.31, 95% CI=0.14, 0.47, respectively). In turn, also in line with hypotheses, behavioral skills were positively associated with PrEP prescription (OR=1.31, 95% CI=1.13, 1.53); however, contrary to hypotheses, behavioral skills were not associated with PrEP discussion (OR=1.10, 95% CI=0.94, 1.30). In line with the IMB model, behavioral skills mediated the effects of information and motivation on PrEP prescription, as indicated by a significant indirect effect of information on prescription via behavioral skills (b=0.10, 95% CI=0.03, 0.19, OR=1.10, 95% CI=1.03, 1.21) and a significant indirect effect of motivation on prescription via behavioral skills (b=0.08, 95% CI=0.03, 0.16, OR=1.09, 95% CI=1.03, 1.17).
Figure 1.
Structural equation model showing associations between information, motivation, and behavioral skills and pre-exposure prophylaxis (PrEP) discussion and prescription in a sample of primary care physicians (PCPs) from 10 U.S. cities (N=280).
Notes: Unstandardized coefficients, correlations, and ORs are presented. Indicators of latent variables are parcels representing sets of scale items. The model was a good fit to the data, Χ2(66, N=280)=73.45, root-mean-square error of approximation (RMSEA)=0.02, comparative fit index (CFI)=0.98, Tucker-Lewis index (TLI)=0.97. Demographic control variables were also included in the model (paths not shown); male sex was significantly associated with behavioral skills, b=0.22, 95% CI=0.01, 0.42, and Latino ethnicity was significantly associated with PrEP discussion, OR=0.56, 95% CI=0.32, 0.97. ***p<0.001; **p<0.01; *p<0.05
In addition to paths predicted by the IMB model, information and motivation also had direct, positive associations with PrEP discussion (OR=1.60, 95% CI=1.36, 1.85 and OR=1.25, 95% CI=1.01, 1.55, respectively), whereas information only had a direct, positive association with PrEP prescription (OR=1.55, 95% CI=1.27, 1.89). As expected, information was positively correlated with motivation (r =0.35, 95% CI=0.26, 0.45) and discussion was positively correlated with prescription (r =0.50, 95% CI=0.36, 0.64).
Covariate paths maintained in the model were from male sex to behavioral skills (b=0.22, 95% CI=0.01, 0.42), from Latino ethnicity to discussion (OR=0.56, 95% CI=0.32, 0.97), from age to prescription (OR=0.97, 95% CI=0.93, 1.004), and from Latino ethnicity to prescription (OR=0.57, 95% CI=0.32, 1.00).
This model explained 23% of the variance in behavioral skills, 43% of the variance in discussion, and 50% of the variance in prescription.
DISCUSSION
The current study demonstrated that the IMB model can be applied to PrEP discussion and prescription in a sample of PCPs from ten U.S. cities. Here, the variables of the IMB model explained more than 40% of the variance in both discussion and prescription, with information about PrEP, attitudes toward PrEP, and confidence in PrEP-related skills all playing important roles. These constructs represent potential targets for interventions directed at healthcare providers in order to increase rates of PrEP use in high-risk populations.
In this sample of PCPs recruited from ZIP codes with above-average HIV incidence, one third had discussed PrEP with patients, and only 17% had prescribed PrEP. Few PCPs considered themselves familiar with PrEP; those who were familiar answered approximately two thirds of factual questions relevant to PrEP prescription correctly. Knowledge of PrEP had the strongest associations with both confidence in skills and PrEP-related behaviors and could present an easy target for interventions and trainings directed at PCPs. Notably, the Centers for Disease Control and Prevention issued guidelines for PrEP prescription 2 months before study data collection began (May 2014)36; exposure to these guidelines could increase providers’ knowledge of PrEP. PCPs’ knowledge could also be increased through Continuing Medical Education courses as well as online trainings.
Attitudes toward and confidence in prescribing PrEP were also important correlates of PrEP discussion and PrEP prescription, respectively. Given the initial controversy related to PrEP and the complexities involved with discussing PrEP and determining whether a patient is an appropriate candidate, it is not surprising that motivation and behavioral skills are related to PrEP prescription. Interventions targeting PCPs should include aspects that will increase providers’ motivation to prescribe PrEP and increase their skills to do so rather than focusing solely on raising awareness of PrEP. Educational interventions could improve PCPs’ attitudes toward PrEP by correcting factual inaccuracies (e.g., that there is insufficient evidence of the effectiveness of PrEP or that PrEP results in risk compensation). Attitudes might also become more positive if PCPs were exposed to PrEP “success stories” or heard from respected colleagues who are PrEP prescribers. The skills required to prescribe PrEP, such as discussing sexual behavior with patients, are somewhat specialized and may make providers uncomfortable; providers’ confidence with these behaviors could be targeted through skills trainings and role plays.
Notably, the combination of information, motivation, and behavioral skills explained more than 40% of the variance in discussion and prescription, which compares favorably to other studies using the IMB model21 as well as previous studies using theoretic models of health behavior to predict providers’ intentions and behavior.27 This suggests that an IMB-based intervention targeted to providers would be appropriate; such an intervention should be tested in future RCTs.
Limitations
The current study has several strengths, including the sample recruited from areas with high HIV prevalence in ten cities and the use of structural equation modeling to test the full IMB model. Limitations of this research include the relatively modest sample size and low engagement in PrEP prescription, which prevented consideration of more-nuanced measures of PrEP behaviors, such as the number of prescriptions. Additionally, new measures were used to assess IMB-related constructs, given that no established measures existed. However, these measures were developed and reviewed by experts in the field, pilot tested, and demonstrated acceptable reliability. Providers who indicated no awareness or familiarity with PrEP were considered to lack knowledge of PrEP prescription; future research should test knowledge for all providers. Finally, the current study is cross-sectional, and no conclusions can be drawn regarding causality. It is also possible that unmeasured constructs may confound reported relationships; the mediational model should be confirmed in future research.
CONCLUSIONS
The current study supported the IMB model, showing that PrEP knowledge, attitudes toward PrEP, and confidence in prescribing PrEP are correlates of PCPs’ PrEP discussion and prescription in a U.S. sample recruited from areas with above-average HIV prevalence. Involvement of PCPs in PrEP prescription is essential if PrEP is to have an impact on the HIV epidemic. As interventions and training programs are developed to increase PrEP prescription among PCPs, the constructs of the IMB model present reasonable targets, and interventions may prove more successful if they address all three constructs.
Supplementary Material
Acknowledgments
This research was supported by funding from Gilead Sciences, Inc. and by National Institute of Mental Health grants 5P30-MH052776 and K01-MH099956. This study was approved by the IRB at the Medical College of Wisconsin. JLW devised the research questions, performed data analysis, and wrote the first draft of the article. AEP conceptualized and designed the larger study, coordinated and supervised data collection, and contributed to writing and editing the article. Both authors approved the final article as submitted.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Prejean J, Song R, Hernandez A, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. https://doi.org/10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spinner CD, Boesecke C, Zink A, et al. HIV pre-exposure prophylaxis (PrEP): A review of current knowledge of oral systemic HIV PrEP in humans. Infection. 2016;44(2):151–158. doi: 10.1007/s15010-015-0850-2. https://doi.org/10.1007/s15010-015-0850-2. [DOI] [PubMed] [Google Scholar]
- 3.Anderson PL, Glidden DV, Liu A, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4(151):151ra125. doi: 10.1126/scitranslmed.3004006. https://doi.org/10.1126/scitranslmed.3004006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant RM, Anderson PL, McMahan V, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: A cohort study. Lancet Infect Dis. 2014;14(9):820–829. doi: 10.1016/S1473-3099(14)70847-3. https://doi.org/10.1016/S1473-3099(14)70847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laufer FN, O'Connell DA, Feldman I, Zucker HA. Vital signs: Increased Medicaid prescriptions for preexposure prophylaxis against HIV infection—New York, 2012–2015. MMWR Morb Mortal Wkly Rep. 2015;64(46):1296–1301. doi: 10.15585/mmwr.mm6446a5. https://doi.org/10.15585/mmwr.mm6446a5. [DOI] [PubMed] [Google Scholar]
- 6.Grant R, Liu A, Hecht J, Buchbinder S, Weber S, Crouch P. Scale-up of preesposure prophylaxis in San Francisco to impact HIV incidence; Conference on Retroviruses and Opportunistic Infections; 2015; Seattle, WA. [Google Scholar]
- 7.Smith DK, Van Handel M, Wolitski RJ, et al. Vital Signs: Estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition - United States, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(46):1291–1295. doi: 10.15585/mmwr.mm6446a4. https://doi.org/10.15585/mmwr.mm6446a4. [DOI] [PubMed] [Google Scholar]
- 8.Bush S, Magnuson D, Rawlings M, Hawkins T, McCallister S, Giler RM. Racial characteristics of FTC/TDF for pre-exposure prophylaxis users in the U.S; Paper presented at: ASM Microbe; 2016; Boston, MA. [Google Scholar]
- 9.Kelley CF, Kahle E, Siegler A, et al. Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clin Infect Dis. 2015;61(10):1590–1597. doi: 10.1093/cid/civ664. https://doi.org/10.1093/cid/civ664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eaton LA, Driffin DD, Bauermeister J, Smith H, Conway-Washington C. Minimal awareness and stalled uptake of pre-exposure prophylaxis (PrEP) among at risk, HIV-negative, Black men who have sex with men. AIDS Patient Care STDS. 2015;29(8):423–429. doi: 10.1089/apc.2014.0303. https://doi.org/10.1089/apc.2014.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sachdev DD, Stojanovski K, Liu AY, et al. Intentions to prescribe preexposure prophylaxis are associated with self-efficacy and normative beliefs. Clin Infect Dis. 2014;58(12):1786–1787. doi: 10.1093/cid/ciu229. https://doi.org/10.1093/cid/ciu229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.White JM, Mimiaga MJ, Krakower DS, Mayer KH. Evolution of Massachusetts physician attitudes, knowledge, and experience regarding the use of antiretrovirals for HIV prevention. AIDS Patient Care STDS. 2012;26(7):395–405. doi: 10.1089/apc.2012.0030. https://doi.org/10.1089/apc.2012.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karris MY, Beekmann SE, Mehta SR, Anderson CM, Polgreen PM. Are we prepped for preexposure prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clin Infect Dis. 2014;58(5):704–712. doi: 10.1093/cid/cit796. https://doi.org/10.1093/cid/cit796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petroll A, Bogart L, Horvath K, Mcauliffe T. PrEP knowledge, attitudes, awareness, and experience among a national sample of U.S. primary care and HIV providers; 10th International Conference on HIV Treatment and Prevention Adherence; 2015; Miami, FL. [Google Scholar]
- 15.Blumenthal J, Jain S, Krakower D, et al. Knowledge is power! Increased provider knowledge scores regarding pre-exposure prophylaxis (PrEP) are associated with higher rates of PrEP prescription and future intent to prescribe PrEP. AIDS Behav. 2015;19(5):802–810. doi: 10.1007/s10461-015-0996-z. https://doi.org/10.1007/s10461-015-0996-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mimiaga MJ, White JM, Krakower DS, Biello KB, Mayer KH. Suboptimal awareness and comprehension of published preexposure prophylaxis efficacy results among physicians in Massachusetts. AIDS Care. 2014;26(6):684–693. doi: 10.1080/09540121.2013.845289. https://doi.org/10.1080/09540121.2013.845289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma M, Wilton J, Senn H, Fowler S, Tan DH. Preparing for PrEP: Perceptions and readiness of Canadian physicians for the implementation of HIV pre-exposure prophylaxis. PLoS One. 2014;9(8):e105283. doi: 10.1371/journal.pone.0105283. https://doi.org/10.1371/journal.pone.0105283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krakower DS, Oldenburg CE, Mitty JA, et al. Knowledge, beliefs and practices regarding antiretroviral medications for HIV prevention: Results from a survey of healthcare providers in New England. PLoS One. 2015;10(7):e0132398. doi: 10.1371/journal.pone.0132398. https://doi.org/10.1371/journal.pone.0132398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher JD, Fisher WA. Changing AIDS risk behavior. Psychol Bull. 1992;111(3):455–474. doi: 10.1037/0033-2909.111.3.455. https://doi.org/10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 20.Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006;25(4):462–473. doi: 10.1037/0278-6133.25.4.462. https://doi.org/10.1037/0278-6133.25.4.462. [DOI] [PubMed] [Google Scholar]
- 21.Fisher WA, Fisher JD, Harman J. The Information-Motivation-Behavioral Skills Model: A general social psychological approach to understanding and promoting health behavior. In: Suls J, Wallston K, editors. Social Psychological Foundations of Health and Illness. Malden, MA: Blackwell Publishing Ltd; 2003. pp. 82–106. https://doi.org/10.1002/9780470753552.ch4. [Google Scholar]
- 22.Amin MEK, Chewning B. Predicting pharmacists' adjustment of medication regimens in Ramadan using the Theory of Planned Behavior. Res Social Adm Pharm. 2015;11(1):e1–e15. doi: 10.1016/j.sapharm.2014.04.004. https://doi.org/10.1016/j.sapharm.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 23.Nelson JM, Cook PF, Ingram JC. Utility of the Theory of Planned Behavior to predict nursing staff blood pressure monitoring behaviours. J Clin Nurs. 2014;23(3–4):461–470. doi: 10.1111/jocn.12183. https://doi.org/10.1111/jocn.12183. [DOI] [PubMed] [Google Scholar]
- 24.Bernaix LW. Nurses' attitudes, subjective norms, and behavioral intentions toward support of breastfeeding mothers. J Hum Lact. 2000;16(3):201–209. doi: 10.1177/089033440001600304. https://doi.org/10.1177/089033440001600304. [DOI] [PubMed] [Google Scholar]
- 25.Herbert KE, Urmie JM, Newland Ba, Farris KB. Prediction of pharmacist intention to provide Medicare medication therapy management services using the Theory of Planned Behavior. Res Social Adm Pharm. 2006;2(3):299–314. doi: 10.1016/j.sapharm.2006.02.008. https://doi.org/10.1016/j.sapharm.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 26.Macalino GE, Sachdev DD, Rich JD, et al. A national physician survey on prescribing syringes as an HIV prevention measure. Subst Abuse Treat Prev Policy. 2009;4(13) doi: 10.1186/1747-597X-4-13. https://doi.org/10.1186/1747-597x-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Godin G, Belanger-Gravel A, Eccles M, Grimshaw J. Healthcare professionals' intentions and behaviours: A systematic review of studies based on social cognitive theories. Implement Sci. 2008;3(36):1–12. doi: 10.1186/1748-5908-3-36. https://doi.org/10.1186/1748-5908-3-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tripathi A, Ogbuanu C, Monger M, Gibson JJ, Duffus WA. Preexposure prophylaxis for HIV infection: Healthcare providers' knowledge, perception, and willingness to adopt future implementation in the southern U.S. South Med J. 2012;105(4):199–206. doi: 10.1097/SMJ.0b013e31824f1a1b. https://doi.org/10.1097/SMJ.0b013e31824f1a1b. [DOI] [PubMed] [Google Scholar]
- 29.CDC. HIV Surveillance Report, 2014. Atlanta, GA: CDC; 2015. Nov, [Google Scholar]
- 30.Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: Exploring the question, weighing the merits. Struct Equ Modeling. 2002;9(2):151–173. https://doi.org/10.1207/S15328007SEM0902_1. [Google Scholar]
- 31.Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV Knowledge Questionnaire. AIDS Educ Prev. 2002;14(2):172–182. doi: 10.1521/aeap.14.2.172.23902. https://doi.org/10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schafer JL. Multiple imputation: A primer. Stat Methods Med Res. 1999;8(1):3–15. doi: 10.1177/096228029900800102. https://doi.org/10.1191/096228099671525676. [DOI] [PubMed] [Google Scholar]
- 33.Kline RB. Principles and practice of structural equation modeling. Guilford press; 2011. [Google Scholar]
- 34.Tofighi D, MacKinnon DP. RMediation: An R package for mediation analysis confidence intervals. Behav Res Methods. 2011;43(3):692–700. doi: 10.3758/s13428-011-0076-x. https://doi.org/10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.CDC. Preexposure prophylaxis for the prevention of HIV infection in the United States–2014: A clinical practice guideline. Atlanta, GA: CDC; 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.