Abstract
Background
Although ischemic stroke risk is increased among people living with HIV infection, little is known about the epidemiology of ischemic stroke subtypes in contemporary HIV-infected cohorts. We examined the distribution of ischemic stroke subtypes among predominantly treated HIV-infected individuals to determine if and how the distribution differs from that of the general population.
Methods
We studied 60 HIV-infected and 60 HIV-uninfected adults with a history of first-ever ischemic stroke between 2000 and 2012. Ischemic strokes were classified as one of five subtypes based on established criteria. We used multinomial logistic regression models to compare the relative frequency of ischemic stroke subtypes by HIV status.
Results
Large artery atherosclerosis (23%) and stroke of undetermined etiology (23%) were the most common stroke subtypes among HIV-infected individuals. The most recent plasma HIV viral load before the stroke event differed by subtype, with a median undetectable viral load for individuals with large artery stroke and stroke of undetermined etiology. Using cardioembolic stroke as the reference subtype, HIV-infected individuals were at higher proportional risk of stroke of undetermined etiology compared with uninfected individuals [relative risk ratio (RRR) 8.6, 95% CI 1.2–63.7, p=0.04]. Among HIV-infected individuals with virologically suppressed infection, we observed a trend toward a greater proportion of strokes attributable to large artery atherosclerosis (RRR 6.7, 95% CI 0.8–57.9, p=0.08).
Conclusions
HIV-infected individuals may be at greater proportional risk of stroke of undetermined etiology compared with uninfected individuals. Further investigation is warranted to confirm this finding and determine underlying reasons for this greater risk.
Keywords: HIV infection, cerebrovascular disease, ischemic stroke subtype, cerebral infarction
Introduction
In recent large cohort studies, the risk of stroke is increased for people living with HIV infection compared with uninfected individuals.1–3 While several studies have evaluated the distribution of ischemic and hemorrhagic strokes in HIV infection, less is known about the epidemiology of ischemic stroke subtypes. Understanding the distribution of ischemic stroke subtypes in HIV would aid in focusing future investigations of the pathogenesis of this elevated stroke risk and to develop potential novel interventions to modify stroke risk in HIV infection. Many of the prior studies investigating ischemic stroke subtypes in HIV infection were performed in cohorts from either before the introduction of antiretroviral therapy (ART) or of largely untreated HIV-infected individuals with advanced disease4–7 and are not generalizable to people living with HIV infection in the modern era of widely available and highly effective combination ART.
In this study of a contemporary cohort of people living with HIV infection and HIV-uninfected patients followed in outpatient clinics from an urban safety net hospital, we examined the distribution of ischemic stroke subtypes to determine if and how, among predominantly ART-treated HIV-infected individuals, the distribution differs from that of the general population.
Methods
Study design
We identified all HIV-infected individuals 18 years of age and older with a first-ever ischemic stroke diagnosed between 2000 and 2012, who were seen on at least two occasions by a medical provider in an HIV clinic at an urban safety net hospital in San Francisco. Potential cases were first identified by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for cerebrovascular disease (433, 434, 436, 437, 443.21 or 443.24). The diagnosis of ischemic stroke was then validated by medical record review by a board-certified neurologist (F.C.C.), using criteria adapted from the World Health Organization MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) project and the Multi-Ethnic Study of Atherosclerosis (MESA).8,9 Cases were excluded if the stroke event occurred before the diagnosis of HIV. The majority of HIV-infected stroke cases were included in a previously published case-control study with a different HIV-infected comparator group.10
The HIV-uninfected cohort was frequency-matched in a 1:1 ratio to the HIV-infected cohort based on calendar year of ischemic stroke diagnosis from among individuals followed in a primary care clinic in the same urban hospital with an ICD-9-CM code for cerebrovascular disease but no ICD-9-CM code for HIV Infection. Ischemic stroke diagnoses in the HIV-uninfected cohort were also validated by medical record review.
Covariates
Demographics, stroke risk factors, health-related behaviors, and laboratories were abstracted from medical records. The presence of vascular risk factors was defined based on problem lists in the primary care or HIV clinic documentation and neurology admission notes. All health-related behaviors (e.g., smoking, alcohol and substance use) were categorized as current versus never or prior use. Individuals for whom no information was available regarding health-related behaviors were classified as unknown. The most proximate CD4 count and plasma HIV RNA level prior to the stroke event for the HIV-infected cases were recorded. HIV RNA levels below the limit of detection were coded as 0 log copies/mL.
Ischemic stroke mechanism
The stroke evaluation performed for each case was reviewed in detail by a board-certified neurologist (F.C.C.) following protocols from MESA.9,11 Records reviewed included discharge summaries; follow up neurology, cardiology, and primary care/HIV clinic notes; and all available brain magnetic resonance imaging (MRI) and computed tomography (CT) images. Results of electrocardiograms, echocardiograms, Holter monitoring, carotid ultrasound, and conventional angiography were also examined. Based on available data, ischemic strokes were categorized as large artery atherosclerosis (extra- and intracranial), small vessel occlusion (lacunar), cardioembolism, other known etiology, or undetermined etiology based on MESA and TOAST criteria.12 According to TOAST criteria, individuals for whom a complete ischemic stroke evaluation was not performed were classified as undetermined etiology. To be considered complete, an ischemic stroke evaluation had to include a minimum of brain imaging (CT or MRI), extra- and intracranial vascular imaging, electrocardiogram and echocardiogram.11
Statistical analysis
We compared demographic and clinical characteristics between HIV-infected and uninfected stroke cases using Student’s t- or Chi-squared tests and HIV-related laboratories by stroke subtype using the Kruskal-Wallis test. We used multinomial logistic regression to determine the relative risk of ischemic stroke subtypes by HIV status after first adjusting for demographics (Model 1) and then for demographics plus additional vascular risk factors identified by forward stepwise selection (Model 2). P values were 2-sided with <0.05 considered statistically significant. Statistical analyses were performed using Stata (StataCorp 2012. Stata Statistical Software: Release 12; Stata Corporation, College Station, TX). The institutional review board of the University of California, San Francisco, approved the study.
Results
Clinical and demographic data were collected for 60 HIV-infected and 60 HIV-uninfected stroke cases (Table 1). HIV-infected individuals tended to be younger at the time of stroke, and there were fewer women in the HIV-infected group. The proportions of White and Black HIV-infected stroke cases were greater than among uninfected stroke cases. Median CD4 count for HIV-infected individuals was 276 cells/mm3 [interquartile range (IQR) 122, 419] and median plasma HIV RNA level was 3.24 log copies/mL (IQR 0, 4.35). Sixty-five percent (65%) of HIV-infected individuals were on combination ART at the time of the stroke and 37% were virologically suppressed in the 6 months preceding the event.
Table 1.
Clinical characteristics of HIV-infected and uninfected individuals with a history of ischemic stroke at an urban safety net hospital
| HIV-infected individuals n=60 No. (%)a |
HIV-uninfected individuals n=60 No. (%)a |
P value | |
|---|---|---|---|
|
| |||
| Demographics | |||
|
| |||
| Age (years), mean (SD) | 50 (8) | 60 (12) | <0.001 |
|
| |||
| Women | 12 (20) | 23 (38) | 0.03 |
|
| |||
| Race | |||
| White | 26 (43) | 15 (25) | <0.001 |
| Black/African-American | 28 (47) | 15 (25) | |
| Latino/Hispanic | 1 (2) | 17 (28) | |
| Other/Unknown | 5 (8) | 13 (22) | |
|
| |||
| Stroke risk factors | |||
|
| |||
| Hypertension | 44 (73) | 46 (77) | 0.67 |
|
| |||
| Dyslipidemia | 25 (42) | 32 (53) | 0.20 |
|
| |||
| Diabetes mellitus | 10 (17) | 22 (37) | 0.01 |
|
| |||
| Coronary heart disease | 15 (25) | 16 (27) | 0.84 |
|
| |||
| Heart failure/cardiomyopathy | 10 (17) | 14 (23) | 0.35 |
|
| |||
| Atrial fibrillation/flutter | 4 (7) | 17 (28) | 0.002 |
|
| |||
| Current substance use and health-related behaviors | |||
|
| |||
| Smoker | 36 (60) | 20 (33) | <0.001 |
|
| |||
| Alcohol | 22 (37) | 9 (15) | 0.018 |
|
| |||
| Methamphetamine | 10 (17) | 2 (3) | 0.05 |
|
| |||
| Cocaine | 23 (38) | 4 (7) | <0.001 |
|
| |||
| Heroin | 5 (8) | 1 (2) | 0.21 |
|
| |||
| Ischemic stroke subtype | |||
|
| |||
| Large artery | 14 (23) | 13 (22) | <0.001 |
| Small vessel | 12 (20) | 20 (33) | |
| Cardioembolic | 12 (20) | 24 (40) | |
| Undetermined etiology | 14 (23) | 2 (3) | |
| Other etiology | 8 (13) | 1 (2) | |
Unless otherwise indicated
Large artery atherosclerosis and stroke of undetermined etiology were the most common ischemic stroke subtypes (23% each) among HIV-infected individuals, followed by small vessel occlusion (20%), cardioembolism (20%) and stroke of other determined etiology, which included strokes due to infectious and carcinomatous meningitis and a hypercoagulable state in the setting of HIV-related malignancy (13%, Table 1). Of the strokes of undetermined etiology, six individuals had an incomplete stroke evaluation, four had a complete evaluation without an identifiable etiology, and four had a stroke diagnosed at a different hospital with insufficient records available for review. Among HIV-uninfected individuals, only 3% of strokes were of undetermined etiology, while cardioembolism (40%) and small vessel occlusion (33%) were the most common subtypes, followed by large artery atherosclerosis (22%) and stroke of other determined etiology (2%). Among the 2 HIV-uninfected individuals with a stroke of undetermined etiology, both had a complete evaluation without an identified etiology.
Plasma HIV RNA level prior to the stroke event for HIV-infected cases differed by ischemic stroke subtype (p=0.04, Figure 1). The median HIV RNA level was undetectable for individuals with large artery strokes (IQR 0, 3.28 log copies/mL) and stroke of undetermined etiology (IQR 0, 3.68 log copies/mL). For small vessel strokes, the median HIV RNA was 3.35 (IQR 1.45, 4.87 log copies/mL), for cardioembolism 3.63 (IQR 0, 4.40 log copies/mL), and for strokes of other determined etiology 4.65 (IQR 3.55, 5.39 log copies/mL). We observed a similar inverse trend for most recent CD4 count before the stroke event, with highest CD4 counts among individuals with large artery disease and stroke of undetermined etiology (p=0.07, Figure 1).
Figure 1. Plasma HIV RNA level (A) and CD4 count (B) by ischemic stroke subtype among HIV-infected individuals.
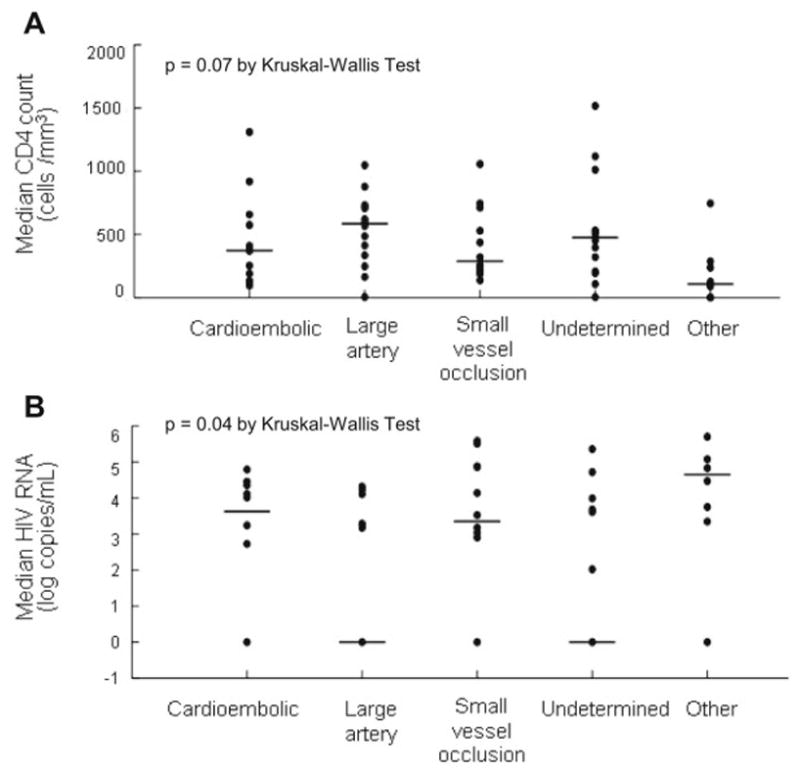
The most recent plasma HIV RNA level and CD4 count before the stroke event differed significantly by ischemic stroke subtype. HIV-infected individuals with stroke of undetermined etiology and large artery atherosclerotic stroke had lowest median viral loads and highest median CD4 counts.
Using cardioembolism as the reference subtype, the relative risk of having a stroke of undetermined etiology was higher for HIV-infected compared with uninfected individuals after adjustment for demographics [relative risk ratio (RRR) 8.9, 95% CI 1.6 to 51.4, p=0.02] and for demographics plus covariates (hypertension, coronary heart disease and atrial fibrillation) chosen by forward stepwise selection (RRR 8.6, 95% CI 1.2 to 63.7, p=0.04). There was a trend toward a greater relative risk of having a stroke of other determined etiology among HIV-infected versus uninfected individuals (RRR 7.2, 95% CI 0.7 to 73.2, p=0.10). In an analysis restricted to ischemic strokes in HIV-infected individuals who were virologically suppressed in the 6 months before the stroke event (n=22) and all HIV-uninfected cases, the increased relative risk of having a stroke of undetermined etiology for HIV-infected individuals remained, while the trend toward a higher relative risk of stroke of other determined etiology was no longer present (Table 2). In the full model adjusting for demographics along with hypertension, coronary heart disease and atrial fibrillation, the relative risk of having a stroke due to large artery atherosclerosis compared with cardioembolism was increased for HIV-infected versus uninfected individuals, but confidence intervals were too wide to rule out no difference in risk (RRR 6.7, 95% CI 0.8 to 57.9, p=0.08, Table 2). Although several health-related behaviors were more common among HIV-infected individuals (Table 1), none remained in the forward stepwise multivariable model.
Table 2.
Adjusted relative risk of ischemic stroke subtype in HIV-infected versus uninfected individuals at a safety net hospital
| Model 1a Relative risk ratio (95% CI) | P value | Model 2b Relative risk ratio (95% CI) | P value | |
|---|---|---|---|---|
| All HIV-infected + uninfected individuals (n=120) | ||||
| Cardioembolic stroke (n=36) | Reference | ---- | Reference | ---- |
| Large artery stroke (n=27) | 2.0 (0.6–6.3) | 0.25 | 1.6 (0.4–5.9) | 0.50 |
| Small vessel occlusion (n=32) | 1.6 (0.5–5.1) | 0.43 | 1.3 (0.4–4.8) | 0.65 |
| Stroke of undetermined etiology (n=16) | 8.9 (1.6–51.4) | 0.01 | 8.6 (1.2–63.7) | 0.04 |
| Stroke of other determined etiology (n=9) | 7.2 (0.7–73.2) | 0.10 | 8.7 (0.7–116.2) | 0.10 |
| Virologically suppressed HIV-infected + all uninfected individuals (n=82) | ||||
| Cardioembolic stroke (n=28) | Reference | ---- | Reference | ---- |
| Large artery stroke (n=21) | 3.0 (0.6–14.2) | 0.17 | 6.7 (0.8–57.9) | 0.08 |
| Small vessel occlusion (n=23) | 1.5 (0.3–8.6) | 0.68 | 3.2 (0.4–29.2) | 0.31 |
| Stroke of undetermined etiology (n=8) | 16.5 (1.8–151.3) | 0.01 | 31.8 (2.2–459.6) | 0.01 |
| Stroke of other determined etiology (n=2) | 3.4 (0.04–284.5) | 0.59 | 7.0 (0.01–3876.7) | 0.55 |
Adjusted for age, sex and race.
Adjusted for age, sex, race, hypertension, coronary heart disease and atrial fibrillation.
Discussion
In this study, the largest ever of a contemporary HIV-infected cohort of which more than half of individuals were on ART, people living with HIV infection were at proportionally higher risk for stroke of undetermined etiology versus cardioembolic stroke compared with HIV-uninfected individuals. Furthermore, the magnitude of the higher relative risk of stroke of undetermined etiology was even more pronounced when we compared the subset of treated, virologically suppressed HIV-infected with uninfected individuals.
Elucidating the distribution of ischemic stroke subtypes in HIV infection may guide research aimed at understanding the pathogenesis of increased stroke risk in HIV infection. In addition, as individual stroke subtypes are associated with different rates of recurrence and prognosis,13 understanding the distribution of stroke subtypes in HIV may be crucial to developing more specific cerebrovascular risk assessments. Most of the large observational studies of HIV and cerebrovascular disease in the current era of ART have relied on billing and administrative codes to identify individuals with a history of ischemic stroke. As a result, information on ischemic stroke subtype is often lacking in these studies, as subtypes cannot be reliably ascertained from ICD codes. Many of the studies that have categorized ischemic stroke subtypes in HIV infection have been in cohorts assessed either before the introduction of effective combination ART or in primarily untreated HIV-infected individuals with advanced disease.4–7 In small but more contemporary studies of ischemic stroke subtypes in HIV-infected individuals with variable ART use and virological suppression,14,15 the distribution of subtypes has varied (Figure 2).
Figure 2. Distribution of ischemic stroke subtypes in more contemporary HIV cohorts.
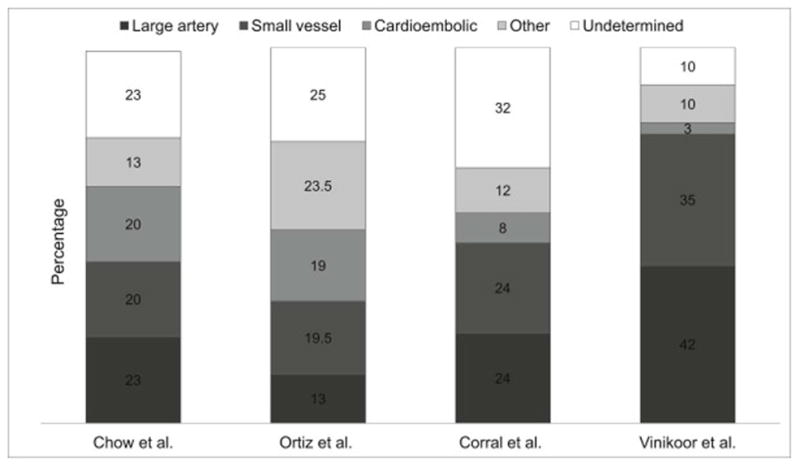
In more recently published studies, although all with less than half of individuals virologically suppressed, the distribution of ischemic stroke subtypes in HIV-infected cohorts has been variable.
| Authors | Ischemic strokes in PLWH, n | Years | % on ART / % virologically suppressed | Mean or median CD4 count (cells/mm3) |
|---|---|---|---|---|
| Chow et al. (current study) | 60 | 2000–2012 | 65 / 37 | 276 |
| Ortiz et al.7 | 77 | 1996–2005 | 37a / NA | 113a |
| Corral et al.14 | 25 | 1996–2008 | 100 / 48 | 355 |
| Vinikoor et al.15 | 31 | 1999–2010 | 94b / 43b | 267b |
We found that the median plasma HIV RNA differed significantly among ischemic stroke subtypes, with a median undetectable HIV RNA among individuals with strokes due to large artery atherosclerosis and undetermined etiologies (Figure 1). This finding prompted us to perform a post-hoc analysis restricted to virologically suppressed HIV-infected stroke cases in light of previously reported differences in cerebrovascular risk between individuals who are viremic and those who are aviremic.1,15,16 Among HIV-infected individuals with well-controlled infection, the trend toward a higher relative risk of stroke of other determined etiology (largely from infectious meningitis and malignancy associated with advanced HIV) among HIV-infected individuals was no longer present, which may have been due to decreased power. However, we still observed a greater proportion of strokes due to an undetermined etiology in the virologically suppressed HIV-infected cohort. The high frequency of strokes of undetermined etiology among HIV-infected individuals in this and prior studies6,7,14,17 raises the question of whether 1) HIV-infected individuals, even with well-controlled infection, may be less likely to receive a complete etiologic evaluation for stroke or 2) novel mechanisms may contribute to the increased risk of stroke in HIV infection, rendering our standard stroke evaluation inadequate to fully characterize stroke risk in HIV-infected individuals. Due to our modest sample size and the fact that the “stroke of undetermined etiology” category, by definition, includes both individuals who have had a complete evaluation with no likely etiology identified and those who have had an incomplete evaluation, we are not able to draw any further conclusions regarding these two possibilities, both of which have implications for stroke risk reduction in HIV infection and merit a more systematic evaluation.
Among individuals with well-controlled HIV, we also observed a trend toward a greater proportion of ischemic strokes attributable to large artery atherosclerosis in the HIV-infected group compared with uninfected individuals after adjusting for demographics and stroke risk factors. The pathogenesis of cardiovascular disease in HIV infection is postulated to be due, in part, to chronic inflammation and immune activation leading to endothelial dysfunction and subclinical atherosclerosis.18 Markers of subclinical large vessel atherosclerosis, such as carotid intima-media thickness and prevalence of new focal carotid plaques, have been shown to be abnormal even in treated, virologically suppressed HIV-infected individuals compared with uninfected controls.19,20 While this was an exploratory analysis, the trend toward a greater proportion of large artery atherosclerotic compared with cardioembolic strokes suggests that these mechanisms may also be critical in the development of elevated cerebrovascular risk in treated HIV infection and underscores the need to understand the mechanisms at play in order to develop targeted interventions.
Our study has limitations that must be considered when interpreting the findings. First, the relatively small sample of stroke cases in both the HIV-infected and uninfected groups may not fully reflect the true population distribution of ischemic stroke subtypes. We observed a high proportion of cardioembolic strokes among uninfected individuals, which may have impacted comparisons of stroke subtype distribution by HIV status. However, while the relative frequency of ischemic stroke subtypes reported in the general population is not uniform, several studies of both predominantly white and black populations have demonstrated that cardioembolic strokes constitute the single largest subtype of ischemic stroke.21–23 Disparities in age, race, and sex certainly affect the relative frequency of stroke subtypes. To account for differences by HIV status, we forced the inclusion of demographic characteristics into all of the multinomial regression models. In addition, we may have missed ischemic strokes that were evaluated outside of our hospital system. However, we chose stroke cases only from individuals followed in either HIV or primary care outpatient clinics at our hospital to minimize differential misclassification or incomplete capture of stroke events by HIV status. Finally, while our study is one of the largest ever in the modern era of treatment with more than half of individuals on ART, due to the still modest sample size, the comparison of stroke subtypes by HIV status is not intended to be definitive but rather to generate novel hypotheses regarding ischemic stroke mechanisms in HIV infection that will inform future investigations.
Summary
Our primary goal was to describe the relative frequency of ischemic stroke subtypes among a contemporary HIV-infected cohort and, secondarily, to compare the distribution to a group of uninfected individuals drawn from the same safety net hospital after adjusting for differences in age, racial distribution, sex and select stroke risk factors. Our findings raise the possibility that people living with HIV infection who are ART-treated and virologically suppressed may be at greater proportional risk of stroke of undetermined etiology and strokes due to large artery atherosclerosis compared with uninfected individuals.
Acknowledgments
Grant support: This work has been supported by the National Center for Advancing Translational Sciences of the NIH under Award Number KL2TR000143. Support for statistical analysis provided through the UCSF Clinical and Translational Science Institute (UL1TR000004).
Footnotes
Work conducted in the Department of Neurology, University of California, San Francisco, Zuckerberg San Francisco General Hospital, San Francisco, CA, USA
Disclosures: All authors report no relevant disclosures.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chow FC, Regan S, Feske S, et al. Comparison of ischemic stroke incidence in HIV-infected and non-HIV-infected patients in a US health care system. J Acquir Immune Defic Syndr. 2012;60:351–358. doi: 10.1097/QAI.0b013e31825c7f24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rasmussen LD, Engsig FN, Christensen H, et al. Risk of cerebrovascular events in persons with and without HIV: a Danish nationwide population-based cohort study. AIDS. 2011;25:1637–1646. doi: 10.1097/QAD.0b013e3283493fb0. [DOI] [PubMed] [Google Scholar]
- 3.Durand M, Sheehy O, Baril JG, et al. Risk of spontaneous intracranial hemorrhage in HIV-infected individuals: a population-based cohort study. J Stroke Cerebrovasc Dis. 2013;22:e34–41. doi: 10.1016/j.jstrokecerebrovasdis.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 4.Qureshi AI, Janssen RS, Karon JM, Weissman JP, Akbar MS, Safdar K, et al. Human immunodeficiency virus infection and stroke in young patients. Arch Neurol. 1997;54:1150–1153. doi: 10.1001/archneur.1997.00550210078016. [DOI] [PubMed] [Google Scholar]
- 5.Mochan A, Modi M, Modi G. Stroke in black South African HIV-positive patients: a prospective analysis. Stroke. 2003;34:10–15. doi: 10.1161/01.str.0000043821.35051.fa. [DOI] [PubMed] [Google Scholar]
- 6.Patel VB, Sacoor Z, Francis P, et al. Ischemic stroke in young HIV-positive patients in Kwazulu-Natal, South Africa. Neurology. 2005;65:759–761. doi: 10.1212/01.wnl.0000174434.00402.b5. [DOI] [PubMed] [Google Scholar]
- 7.Ortiz G, Koch S, Romano JG, et al. Mechanisms of ischemic stroke in HIV-infected patients. Neurology. 2007;68:1257–1261. doi: 10.1212/01.wnl.0000259515.45579.1e. [DOI] [PubMed] [Google Scholar]
- 8.The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol. 1988;41:105–114. doi: 10.1016/0895-4356(88)90084-4. [DOI] [PubMed] [Google Scholar]
- 9.Bild DE. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 10.Chow FC, Bacchetti P, Kim AS, et al. Effect of CD4+ cell count and viral suppression on risk of ischemic stroke in HIV infection. AIDS. 2014;28:2573–2577. doi: 10.1097/QAD.0000000000000452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. [Accessed November 23, 2016];Multi-Ethnic Study of Atherosclerosis Manual of Operations, Section 4 and Appendix B. https://www.mesa-nhlbi.org/PublicDocs/MesaMOO/Appendix11_MESA_ClinicalEvents_MOP.pdf.
- 12.Adams HP, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 13.Redfors P, Jood K, Holmegaard L, et al. Stroke subtype predicts outcome in young and middle-aged stroke sufferers. Acta Neurol Scand. 2012;126:329–335. doi: 10.1111/j.1600-0404.2012.01653.x. [DOI] [PubMed] [Google Scholar]
- 14.Corral I, Quereda C, Moreno A, et al. Cerebrovascular ischemic events in HIV-1-infected patients receiving highly active antiretroviral therapy: incidence and risk factors. Cerebrovasc Dis. 2009;27:559–563. doi: 10.1159/000214219. [DOI] [PubMed] [Google Scholar]
- 15.Vinikoor MJ, Napravnik S, Floris-Moore M, et al. Incidence and clinical features of cerebrovascular disease among HIV-infected adults in the southeastern United States. AIDS Res Hum Retroviruses. 2013;29:1068–1074. doi: 10.1089/aid.2012.0334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sico JJ, Chang C-CH, So-Armah K, et al. HIV status and the risk of ischemic stroke among men. Neurology. 2015;84:1933–1940. doi: 10.1212/WNL.0000000000001560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Evers S, Nabavi D, Rahmann A, et al. Ischaemic cerebrovascular events in HIV infection: a cohort study. Cerebrovasc Dis. 2003;15:199–205. doi: 10.1159/000068828. [DOI] [PubMed] [Google Scholar]
- 18.Hsue PY, Deeks SG, Hunt PW. Immunologic basis of cardiovascular disease in HIV-infected adults. J Infect Dis. 2012;205(suppl 3):S375–382. doi: 10.1093/infdis/jis200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hsue PY, Hunt PW, Schnell A, et al. Role of viral replication, antiretroviral therapy, and immunodeficiency in HIV-associated atherosclerosis. AIDS. 2009;23:1059–1067. doi: 10.1097/QAD.0b013e32832b514b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanna DB, Post WS, Deal JA, et al. HIV infection is associated with progression of subclinical carotid atherosclerosis. Clin Infect Dis. 2015;61:640–650. doi: 10.1093/cid/civ325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Petty GW, Brown RD, Whisnant JP, et al. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke. 1999;30:2513–2516. doi: 10.1161/01.str.30.12.2513. [DOI] [PubMed] [Google Scholar]
- 22.Woo D, Gebel J, Miller R, et al. Incidence rates of first-ever ischemic stroke subtypes among blacks: a population-based study. Stroke. 1999;30:2517–2522. doi: 10.1161/01.str.30.12.2517. [DOI] [PubMed] [Google Scholar]
- 23.Kolominsky-Rabas PL, Weber M, Gefeller O, et al. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke. 2001;32:2735–2740. doi: 10.1161/hs1201.100209. [DOI] [PubMed] [Google Scholar]


