Abstract
Objective
Meniscal tears occur frequently in patients with knee osteoarthritis (OA). The aim of our study was to determine whether meniscal damage identified on magnetic resonance imaging (MRI) is associated with the severity of knee pain or the frequency of meniscal symptoms in patients with knee OA.
Methods
We performed a cross-sectional study using data from the Meniscal Tear in Osteoarthritis Research (MeTeOR) trial. We characterized meniscal damage hierarchically as: root tear; maceration; long and short complex or horizontal tears; and simple tears. Subjects completed the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Pain Scale and a survey of frequency of meniscal symptoms. We used multivariable general linear models to assess the relationships between meniscal damage and a) pain severity; and b) meniscal symptoms, after adjusting for demographic and radiographic features. In further analysis root tear was considered as a binary variable.
Results
Analysis included 227 knees. Root tears were present in 19%, maceration in 14%, long complex or horizontal tears in 22%, short complex or horizontal tears in 30%, and simple tears in 14%. Root tears were associated with higher WOMAC pain scores. The adjusted mean WOMAC Pain score was 45.2 (SE 2.7) for those with root tear and 38.7 (SE 1.2) for subjects without root tear (p=0.03). We did not find statistically significant associations between meniscal morphology and frequency of meniscal symptoms.
Conclusion
Root tears were associated with greater pain than meniscal tears or maceration. We did not find a relationship between meniscal damage and meniscal symptoms.
Introduction
Symptomatic knee OA is estimated to affect over 9 million adults in the United States1. Up to 91% of patients with symptomatic knee OA have concurrent meniscal tears on magnetic resonance imaging (MRI)2. The menisci provide load bearing and stability to the knee; thus, alterations in meniscal positioning and meniscal damage contribute to cartilage loss in OA3. However, the contribution of meniscal damage to pain and functional status in patients with symptomatic OA is unclear, as the few prior studies of these relationships have had contradictory findings2, 4, 5.
MRI is an effective non-invasive mechanism for evaluating intraarticular structures of the knee and the diagnosis of meniscal tears6. Horizontal tears (parallel to the tibial plateau), complex tears (multiple tears in more than one plane) and maceration (loss of meniscal substance) are often associated with advancing age and degeneration7–9. Vertical tears (perpendicular to the tibial plateau and parallel to the circumferential meniscal fibers) and radial tears (perpendicular to the tibial plateau and to the circumferential meniscal fibers) may lead to meniscal displacement and extrusion8, 10. Meniscal root tears are lesions at the attachment of the meniscal root in the posterior horn and are of particular interest due to disruption of biomechanical stability and load bearing7, 11, 12. We shall use the term “meniscal damage” in this paper to refer to tears of the meniscus or meniscal root, and maceration. Figure 1 provides examples of these damage types as identified on MRI.
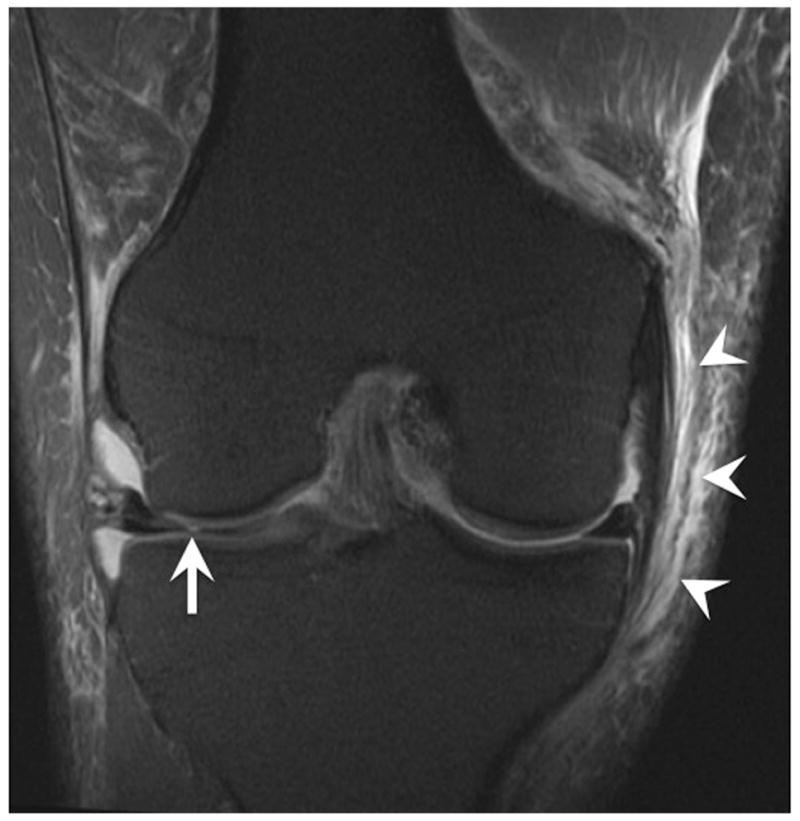
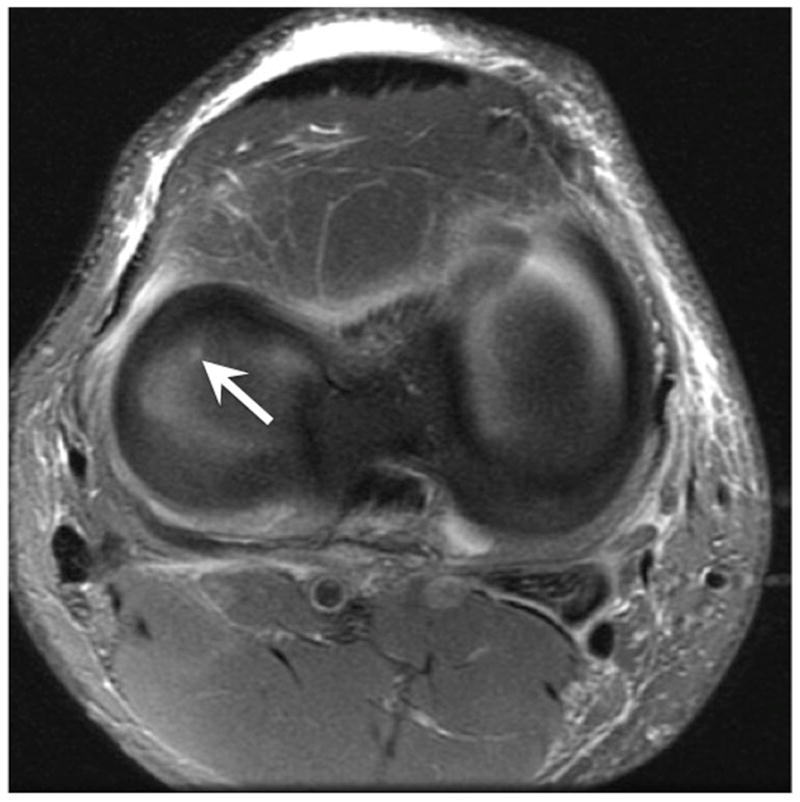
Figure 1. Examples of meniscal damage on MRI with annotation.




a) Vertical tear: Sagittal intermediate-weighted MRI of the knee shows a vertical tear of the posterior horn of the medial meniscus (arrow).
b) Maceration: Coronal intermediate-weighted MRI of the left knee shows diminutive body of the lateral meniscus with partial maceration (arrow) and lateral extrusion. There is also a medial extrusion of medial meniscus (arrowhead). Large lateral and small medial femoral osteophytes are noted. There is a severe cartilage loss with denudation of the lateral tibial plateau which is also remodeled.
c) Radial tear: Coronal fat-suppressed proton density-weighted MRI of the right knee (1) shows a small radial tear of the medial meniscus (arrow) with grade 1 sprain of the medial collateral ligament (arrowheads). Axial fat-suppressed proton density-weighted MRI (2) confirms the radial tear is located at the anterior horn and body junction of the medial meniscus (arrow).
d) Horizontal tear: Sagittal fat-suppressed proton density-weighted MRI shows horizontal oblique tear of the posterior horn of the lateral meniscus (arrow). There is also a moderate Hoffa-synovitis (circle) shown as a hyperintensity signal at the intercondyar region.
e) Root tear: Coronal intermediate-weighted MRI of the left knee shows a complete vertical tear of the posterior root of the medial meniscus (arrow) with medial meniscal subluxation (arrowhead).
Whether meniscal tears and damage contribute to symptoms in OA patients is particularly relevant as an estimated 500,000, or half of all knee arthroscopic surgeries, are undertaken for meniscal tears13. One potential avenue of research for improving outcomes for patients with meniscal damage is to increase our understanding of the symptomatic expression and significance of meniscal abnormalities visualized on imaging studies. Our work builds upon the foundational observations of Roubille et al, who reported that meniscal tear in the lateral compartment and meniscal extrusion associated with a higher likelihood of neuropathic pain5. We continue this inquiry into specific meniscal structural phenotypes by examining distinct meniscal injury morphologies. However, to our knowledge no studies have examined the relationship between the type of meniscal damage documented on MRI and intensity of patient reported symptoms.
We developed hypotheses based on the clinically important effects these tear types have on clinical symptoms and pain as evidenced by prior literature and the insight of senior orthopedic surgeons 4, 14, 15. We hypothesized that simple tears, defined as vertical or radial tears, would be associated with mechanical symptoms (clicking, catching, popping) reflecting the effect of mobile meniscal tissue interfering with smooth joint motion. Further, we hypothesized that complex tears, horizontal tears, and maceration would be associated with higher levels of patient-reported pain due to disrupted load bearing from the damaged meniscus. In particular we hypothesized that root tears would be associated with worse pain because of their marked disruption of knee biomechanics 11, 12. To investigate these hypotheses we evaluated the relationships between the type of meniscal damage documented on MRI and a) knee pain severity; and b) meniscal symptoms.
Methods
Study Population
We used baseline data from subjects enrolled in the Meniscal Tear in Osteoarthritis Research (MeTeOR) trial, a randomized clinical trial of arthroscopic partial meniscectomy (APM) versus physical-therapy for management of meniscal tear16. Three hundred fifty-one subjects were recruited from 7 academic referral centers between June 2008 and August 2011. Recruited males and females were 45 years or older and had an MRI of the knee with evidence of meniscal tear extending to the meniscal surface. Included patients had evidence of OA as determined by osteophyte and joint space narrowing on plain radiograph, or osteophytes or full thickness cartilage defect on MRI. Study participants had to have at least four weeks of knee pain and at least one of the following symptoms: clicking, catching, popping, giving way, pain with pivot or torque, pain that is episodic, and pain that is acute and localized to one joint line. Exclusion criteria included a chronically locked knee, inflammatory arthritis, or prior surgery, including meniscal surgery, on the index knee. Subjects with radiographic Kellgren Lawrence (KL) grade 4 OA (greater than 50% loss of tibiofemoral joint space) were excluded as total knee replacement was felt to be more appropriate than APM in this setting 17. In the MeTeOR study baseline and 18 month MRIs were read in a paired fashion by a central reader; thus, we included the 227 subjects with complete baseline and 18 month MRI data. The remaining 124 subjects without follow up MRIs did not differ from the 227 in regards to age, sex, race or BMI. Each subject contributed one “index knee” to this analysis. Details of MeTeOR have been previously published18. Our study was approved by the Partners HealthCare Human Research Committee. This trial is registered at clinicaltrials.gov (NCT00597012)
Data elements
We used several domains of available data including age, sex, body mass index (BMI), and KL radiographic grade, which was categorized as 0) normal; 1) questionable osteophyte; 2) definite osteophyte; 3) <50% joint space narrowing17.
Evaluation of Meniscal Morphology
The MRIs performed at enrollment were re-read centrally by a single experienced musculoskeletal radiologist and scored according to the MRI OA Knee Score (MOAKS) criteria7. The MOAKS total OA scores for this reader were closely associated to the total OA scores of another highly experienced reader in a sample of 10 subjects, with an interclass correlation of 0.98. MOAKS was chosen as it provides comprehensive meniscal evaluation with graded scores for meniscal tear morphology, extrusion, maceration and hypertrophy, as well as criteria for scoring other areas of pathoanatomy7. We categorized MOAKS meniscal damage data into 5 hierarchical groups: 1) root tear (posterior horn); 2) maceration (partial or complete, in any compartment); 3) long complex or horizontal tears (spanning 2 or 3 regions); 4) short complex or horizontal tears (visualized in only 1 region); and 5) simple tears, comprised of vertical and radial tears. This hierarchical approach permitted us to assign one tear type to each subject. If a subject had both root tear and maceration, he or she was classified as ‘root tear’ because clinically root tear was felt to be higher (worst) in the pain hierarchy. The hierarchy was based on the clinically important effects these tear types have on pain as evidenced by prior literature and the insight of senior orthopedic surgeons 14, 15. We further categorized meniscal damage by creating a binary indicator for root tear. As with the hierarchical grouping, any subject with root tear, regardless presence or absence of other meniscal damage, was classified as having a root tear. We assessed each region (anterior, body, posterior) of both the medial and lateral menisci.
Other MRI-based factors
We assessed MOAKS-based evidence of meniscal extrusion, bone marrow lesions (BMLs, size and number), cartilage damage (size and depth), and Hoffa-synovitis as potential covariates. Extruded menisci were measured according to the MOAKS and categorized as 1) any extrusion <2mm; 2) any extrusion 2–2.9mm; 3) any extrusion ≥ 3mm. MOAKS divides the articular and subspinous region of the knee into 15 subregions to grade BML size and number. The maximum size and number of BML in a given knee will be used for analysis. BML size was graded as 0) no BML; 1) < 33%; 2) 33–66%; 3) >66% of a subregion occupied. The number of subregions with BML (possible range from 0–15) was categorized as 1, 2, 3 or ≥4. We quantified cartilage damage as size of any cartilage loss (% of surface area in region) and depth of cartilage damage (% of full thickness loss in region). All 15 subregions were assessed, the maximum size of cartilage damage and maximum depth of cartilage damage for a given knee was used for analysis. Cartilage damage size was categorized as 0) none; 1) <10%; 2) 10–75%; and 3) >75%. Cartilage damage depth categorized as 0) none; 1) <10%; 2) 10–75% and 3) >75%. Hoffa-synovitis was regarded as 0) normal; 1) mild; 2) moderate; 3) severe as based on MOAKS grading scale 7. Due to the use of non-contrast MRI in this and many OA studies, hyperintense signal of Hoffa’s fat pad as demonstrated on T2/Intermediate weighted or proton density with fat suppressed sequences is used as a proxy for synovitis7.
Assessment of Patient Symptoms
At trial entry subjects enrolled in MeTeOR completed a questionnaire that contained measures of pain and meniscal symptoms. The WOMAC Pain Score was used to assess overall patient-reported knee pain in the last week, and was transformed to a 0–100 scale with 0 being least amount of pain and 100 greatest amount of pain. The meniscal symptom questions evaluated frequency of characteristic meniscal symptoms including clicking, catching, popping, giving way, locking, swelling, and pain with pivoting/twisting. Each symptom was ranked on an ordinal scale assessing symptom frequency in the past week; 1) no symptoms in past week; 2) once in the past week; 3) 2–6 times in the last week; 4) 1–2 times per day; 5) several times per day 16. Clicking, catching and popping had the highest inter-item correlations and the weakest correlations with the WOMAC Pain Score (0.27, 0.32, and 0.25 respectively), suggesting they were measuring a different symptom domain19. Therefore, we used these three characteristics to assess frequency and severity of meniscal symptoms. We summed the responses to these three items, yielding a score with possible range 3–15, with 15 indicating the most frequent meniscal symptoms.
Statistical Analysis
We described characteristics of the baseline study cohort using means and percentages. We used multivariable general linear models to assess the relationships between meniscal damage and a) pain severity; and b) meniscal symptoms. Age, sex, BMI and KL grade were included in the adjusted models due to these variables’ clinical relevance. We additionally considered meniscal extrusion, maximum BML size and number of meniscal subregions affected by BML, cartilage damage size and depth, and Hoffa-synovitis for inclusion in the final model, in order to isolate the independent effects of meniscal damage. In a secondary analysis we examined presence of a root tear as a binary predictor of WOMAC pain as we hypothesized that these tears may incite greater pain. As our cohort included participants who provided both baseline and 18 month MRIs, we re-analyzed the final models using all participants that had available baseline MRIs (n=281). We performed a sensitivity analysis to facilitate comparison of our study to the results from Kamimura4. For this analysis the occurrence of any catching in the past week was regarded as a binary outcome (yes or no). Fisher’s exact test was used to assess for the association between the meniscal tear morphologies and catching. A p value of <0.05 was considered the threshold for significance. In an additional sensitivity analysis we used multivariable linear models to investigate for association between a) meniscal damage (categorical) and b) root tear (binary) and the WOMAC pain score components focusing on weight-bearing activities (climbing stairs, walking, standing).
All analyses were performed using SAS 9.4 statistical software (SAS Institute Inc., Cary, NC).
Results
Baseline Features
The sample consisted of 227 knees (one per person) with complete MRI and survey data. The baseline characteristics for study participants stratified by each damage category are presented in Table 1. The mean age for the entire cohort was 58 years (standard deviation (SD) 7), and was similar across the distinct damage morphologies (range 57–61). There was a slight female predominance of 58% in the entire cohort and most notably in root tears (71% female). The average BMI of the cohort was 30. Subjects with maceration had the lowest average BMI of 29, root tears had the highest BMI at 31, while all other damage variables had an average BMI of 30. In the total cohort subjects were roughly evenly distributed over the four KL grades, with between 50 and 64 subjects in each grade. However, among the meniscal damage types, maceration had the highest percentage of patients with KL grade 2 or 3 (77%). In the total cohort 64% of the subjects had a maximum BML size >0% and ≤66%, and 62% had a maximum number of BML between 1–3. Those with maceration and root tears had larger BMLs and more subregions with BML in comparison to other damage morphologies. The majority of subjects in both the entire cohort and each damage category had mild synovitis. With regard to the hierarchical classification of meniscal damage, root tears were seen in 19% of subjects, maceration in 14%, long complex or horizontal tears in 22%, short complex or horizontal tears in 30%, and simple tears in 14% of subjects.
Table 1.
Baseline characteristics by meniscal damage morphology
| Overall | Meniscal Damage Morphology | |||||
|---|---|---|---|---|---|---|
| Root tear N= 42 | Maceration N=31 | Long complex or horizontal tear N= 50 | Short complex or horizontal tear N= 69 | Simple tear N=32 | ||
| Age years mean (SD) | 59 (7) | 59 (8) | 61 (8) | 60 (8) | 57 (7) | 57 (6) |
| Sex | ||||||
| Male | 95 (42) | 12 (29) | 15 (48) | 19 (38) | 34 (49) | 13 (41) |
| Female | 132 (58) | 30 (71) | 16 (52) | 31 (62) | 35 (51) | 19 (59) |
| BMI kg/m2 mean (SD) | 30 (6) | 31 (6) | 29 (5) | 30 (7) | 30 (6) | 30 (7) |
| Meniscal Extrusion | ||||||
| <2mm | 44 (19) | 1 (2) | 4 (13) | 15 (30) | 16 (23) | 6 (19) |
| 2–2.9mm | 98 (43) | 19 (45) | 9 (29) | 20 (40) | 38 (55) | 11 (34) |
| ≥3mm | 85 (37) | 22 (52) | 18 (58) | 15 (30) | 15 (22) | 15 (47) |
| Kellgren-Lawrence score | ||||||
| 0 | 50 (22) | 10 (24) | 2 (7) | 10 (20) | 18 (26) | 9 (28) |
| 1 | 53 (23) | 9 (21) | 5 (16) | 11 (22) | 20 (29) | 8 (25) |
| 2 | 60 (26) | 10 (24) | 9 (29) | 11 (22) | 20 (29) | 9 (28) |
| 3 | 64 (28) | 13 (31) | 15 (48) | 18 (36) | 11 (16) | 6 (19) |
| Bone marrow lesion size | ||||||
| None | 44 (19) | 6 (14) | 2 (7) | 11 (22) | 14 (20) | 11 (34) |
| <33% | 71 (31) | 9 (21) | 7 (23) | 18 (36) | 27 (39) | 9 (28) |
| 33–66% | 75 (33) | 21 (50) | 12 (39) | 11 (22) | 21 (30) | 9 (28) |
| >66% | 35 (15) | 6 (14) | 10 (32) | 10 (20) | 5 (7) | 3 (9) |
| Bone narrow lesion number | ||||||
| 0 | 44 (19) | 6 (14) | 2 (7) | 11 (22) | 14 (20) | 11 (34) |
| 1 | 58 (26) | 9 (21) | 6 (19) | 18 (36) | 18 (26) | 6 (19) |
| 2 | 47 (21) | 10 (24) | 6 (19) | 8 (16) | 15 (22) | 6 (19) |
| 3 | 35 (15) | 8 (19) | 3 (10) | 6 (12) | 12 (17) | 6 (19) |
| 4 | 41 (18) | 9 (21) | 14 (45) | 7 (14) | 8 (12) | 3 (9) |
| Cartilage damage size | ||||||
| None | 4 (2) | 0 (0) | 0 (0) | 2 (4) | 0 (0) | 2 (6) |
| <10% | 15 (7) | 1 (2) | 0 (0) | 4 (8) | 9 (13) | 1 (3) |
| 10–75% | 120 (54) | 25 (60) | 11 (37) | 23 (46) | 43 (64) | 18 (56) |
| >75% | 85 (38) | 16 (38) | 19 (63) | 21 (42) | 15 (22) | 11 (34) |
| Cartilage Damage thickness | ||||||
| None | 80 (36) | 9 (21) | 4 (13) | 25 (50) | 24 (36) | 16 (50) |
| <10% | 54 (24) | 10 (24) | 5 (17) | 8 (16) | 35 (37) | 6 (19) |
| 10–75% | 75 (33) | 23 (55) | 15 (50) | 14 (28) | 15 (22) | 8 (25) |
| >75% | 15 (7) | 0 (0) | 6 (20) | 3 (6) | 3 (4) | 2 (6) |
| Hoffa-Synovitis | ||||||
| None | 49 (22) | 5 (12) | 6 (19) | 9 (18) | 20 (29) | 7 (22) |
| Mild | 132 (58) | 24 (57) | 21 (68) | 31 (62) | 35 (51) | 20 (63) |
| Moderate | 41 (18) | 10 (24) | 3 (10) | 10 (20) | 13 (19) | 5 (16) |
| Severe | 3 (1) | 3 (7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Meniscal damage: root tears, maceration, long complex or horizontal tear (spanning 2–3 subregions), short complex or horizontal tear (spanning 1 subregion), simple tears (radial and vertical)
All cells provide N (%) except where indicated
BMI; body mass index
Cartilage damage size; maximum percent of surface area in region with any cartilage loss
Cartilage damage depth; percent of cartilage damage that is full thickness loss
Bone marrow lesion size; maximum percent of any meniscal subregion occupied by BML
Bone marrow lesion number; maximum number of BML in any subregion
Meniscal Damage and Symptoms
The average WOMAC pain sore was 40.4 (SD 17.4) and the average meniscal symptom score was 6.8 (SD 3.6) for the entire cohort. In bivariable analyses, the WOMAC pain scores appeared to differ among the damage categories and approached but did not meet statistical significance (p=0.05): WOMAC pain was highest (worst) in the root tear group, with a mean of 46.5 (standard error (SE) 2.7) compared to any of the other damage categories (Table 2). Long degenerative complex tears had the lowest mean WOMAC pain score of 35.7 (SE 2.4). We did not observe any clinically important or statistically significant associations between meniscal damage and frequency of meniscal symptoms as scores for all root tear, maceration and meniscal tear types ranged between 6 and 7 (Table 2).
Table 2.
Associations of meniscal damage morphology with meniscal symptom score and WOMAC pain score
| Crude means (SE) | Adjusted means (SE) | |||
|---|---|---|---|---|
| Meniscal Damage Morphology | Meniscal Symptomsa | WOMAC Painb | Meniscal Symptomsc * | WOMAC Paind * |
| Root tear | 7.3 (0.6) | 46.5 (2.7) | 7.3 (0.6) | 45.1 (2.7) |
| Maceration | 7.1 (0.7) | 40.1 (3.1) | 7.1 (0.7) | 41.5 (3.0) |
| Long complex or horizontal tear | 6.0 (0.5) | 35.7 (2.4) | 6.0 (0.5) | 34.9 (2.3) |
| Short complex or horizontal tear | 7.2 (0.4) | 40.9 (2.1) | 7.1 (0.4) | 40.5 (2.0) |
| Simple tear | 6.6 (0.7) | 40.5 (3.0) | 6.5 (0.7) | 39.8 (2.9) |
WOMAC; Western Ontario & McMaster Universities Osteoarthritis Index Pain Score.
Adjusted for age, sex, body mass index and Kellgren-Lawrence grade
p=0.44
p=0.05
p=0.36
p=0.04
In sensitivity analysis we did not find meaningful or statistically significant associations between meniscal damage and catching (p=0.69). In the total cohort 49% of subjects reported any catching. Subject with root tears were most likely to report catching at 58% and subjects with long degenerative or complex tears were least likely to report catching at 44%.
Multivariable Modeling
Predictors of WOMAC Pain
We did not observe bivariable associations between WOMAC pain score or meniscal symptom score and the BML indicators, cartilage damage indicators, meniscal extrusion, or Hoffa-synovitis and therefore did not include these covariates in the multivariable model. A significant association between meniscal damage and WOMAC pain persisted after adjustment for covariates, with root tears having the highest levels of pain (45.1, SE 2.7) and long complex or horizontal tears the lowest (34.9, SE 2.3) (p=0.04). In multivariable linear regression analyses that considered root tear as a binary predictor, 42 (19%) of participants had root tear. The adjusted mean WOMAC Pain score was 45.2 (SE 2.7) for those with root tear and 38.7 (SE 1.2) in subjects without root tear after adjustment for age, sex, BMI and KL grade (p=0.03). The difference in mean WOMAC pain between those with and without root tears was 6.5 (95% confidence interval (CI) 0.6,12.3). In multivariable models adjusted for age, sex, BMI and KL no statistically significant association was demonstrated between meniscal damage and the weight-bearing components of WOMAC pain (p=0.22). In multivariable models including root tear as a binary predictor we found borderline statistical significant association with the weight-bearing components of WOMAC pain (adjusted mean for root tear; 46 (SE 3) versus those with no root tear; adjusted mean 40 (SE 1), p=0.06)
Predictors of Meniscal Symptoms
The multivariable model adjusted for age, sex BMI and KL grade did not identify an association between meniscal damage and meniscal symptoms as all scores ranged between 6 and 7 (p=0.36; Table 2).
Re-analyzing the models after including all (n=281) participants with baseline MRIs again showed an association between type of meniscal damage and WOMAC pain, but no association between type of meniscal damage and meniscal symptoms. Regarding root tear as a binary exposure in the entire cohort yielded similar results to that of the initial cohort of 227; adjusted mean WOMAC Pain score was 44.2 (SE 2.5) for those with root tear and 39.1 (SE 1.1) in subjects without root tear (p=0.06)
Discussion
In our cross sectional study of patients with OA and meniscal damage we found that there was statistically significant variability among the different types of meniscal damage and patient reported pain, with root tears conferring somewhat higher levels of pain. In secondary analysis comparing root tears to all other types of meniscal damage we found statistically significantly greater severity of knee pain in subjects with root tear than in those without such tears; this difference persisted after adjusting for imaging markers of OA severity including KL grade. The effect size from this analysis was 0.3, a small but likely clinically relevant effect 20. Including only the weight bearing components of WOMAC pain in the analysis of those with and without root tears yielded a similar effect size of 0.2. Our finding of lower pain in subjects with longer complex or horizontal tears is also noteworthy. We hypothesize that these longer tears may represent more chronic tears that have extended over months to years, and that the more chronic lesions are less painful. This hypothesis merits further examination. Our results did not demonstrate an association between type of meniscal damage and mechanical meniscal symptoms. Specifically, contrary to our initial hypothesis, simple tears did not produce a higher frequency of classical meniscal symptoms (clicking, popping and catching). Our study took into account meniscal extrusion, cartilage damage, BML, and Hoffa’s synovitis as contributors to pain, but did not find bivariable associations between these imaging characteristics and pain. However, our sample consisted of patients with both OA and meniscal damage. The relationship between the imaging characteristics and pain could be mediated through meniscal damage, and therefore is less pronounced in our population. Furthermore, our patient population may represent a different spectrum of disease, as all were clinically considered appropriate for surgery. We are cautious with generalization of these associations given the level of symptom severity in our particular cohort. While we did not observe bivariable association between these variables and pain, we cannot exclude that significant association would be demonstrated after adjustment for other factors.
Tears in the posterior root were only first identified around 25 years ago 21. Subsequent reports in both the elderly and general populations estimate a prevalence of root tears varying widely from 1% to 29% in keeping with the 19% prevalence of root tears noted in our study8, 22. There has been less attention paid to the symptomatology of root tears, though previous studies have shown an association between root tears and increased pain, specifically in the posterior aspect of the knee4, 14. Conversely, data from patients undergoing total knee replacement showed no association with medial meniscal root tears and joint line tenderness or pain on VAS, however, this population had predominantly KL grade 4 (severe) OA23. Based on the greater degree of pain observed with root tears even after adjustment for potential confounders it appears that root tears may indeed contribute independently to symptoms. The cross-sectional nature of this study precludes identification of the causal pathway. It could be, for example, that root tears predispose the knee to increased cartilage damage, and attendant pain24. The persistence of the association between root tear and pain after adjustment for KL level makes this argument less likely.
Posterior root tears have been the focus of several investigations over the last decade due to evidence that this morphologic tear type uniquely alters the biomechanics of the knee through loss of hoop tension and increased tibofemoral contact predisposing patients to accelerated cartilage damage and accelerated OA11, 12, 24–27. Prior research using a medial meniscus posterior root avulsion model in cadaver knees found that root avulsions led to meniscal extrusion, while repair of the avulsion led to less extrusion27. As has been shown by Roubille et al meniscal extrusion has been associated with a higher likelihood of neuropathic pain5. Another study of cadaver knees demonstrated increase peak pressure in the medial compartment in knees with medial root tears; furthermore, the peak contact pressures did not differ between knees with root tear and those with a total meniscectomy11. We hypothesize that these features may also ultimately contribute to increased levels of pain seen in root tears. While we did not find an independent relationship between meniscal extrusion or cartilage damage and pain, we cannot exclude that either extrusion or cartilage damage may still be a contributory mechanism. Work from Lee et al are in agreement with our findings, reporting that the majority of root tear patients had pain (66.7 with pain on full flexion, 61.9% with joint line tenderness) while a minority had locking or giving way, 14.3% and 9.5% respectively28. Opinions on how to best manage root tears to mitigate further knee damage and symptomatology are varied and include APM, meniscal repair, and non-surgical management29–33. These observations suggest that further research should focus on whether root tears respond similarly to treatment (operative, non-surgical) as compared with other tear types and whether treatment responses are durable, given the greater risk of OA progression. Further investigation into different types or morphologies of root tears is warranted as within the root tear category some morphologies may be more amenable to surgical intervention than others.
Our results differ from those of Kamimura et al, who found an association between medial meniscal tear type on arthroscopy and clinical symptoms4. Kamimura et al categorized tears into radial tears, root tears, horizontal tears and flap tears. Radial tears did not demonstrate a statistically significant association with catching, a conclusion that is further supported by our data (simple tears in our study were comprised of radial and vertical tears). However, flap tears did cause statistically significantly greater catching sensation in the study of Kamimura et al 4. In our sensitivity analysis we did not find that any of the meniscal damage categories, including simple tears which we hypothesized would cause meniscal symptoms due to mobility, had clinically or statistically significant associations with catching. It is conceivable that the arthroscopist can identify a flap tear that is mobile and interferes with joint motion causing mechanical symptoms, while MRI cannot identify those tears that are truly mobile.
Our study has several limitations. As the design is cross-sectional, associations cannot be interpreted as causal. We included subjects with complete baseline and 18 month MRI data. This may introduce selection bias as those with worse symptoms may have been less likely to return to follow up evaluation and were therefore excluded. Surgeons may have preferentially offered study enrollment based on the level of meniscal symptoms. Patients with more severe meniscal symptoms, such as frequent locking, could have proceeded to surgery and not have been considered for trial enrollment. Therefore, the trial population may not have sufficient variability in meniscal symptoms to demonstrate significant differences based on tear type. Our patient population all had severe symptomatology and were surgical candidates, we advise caution with generalization of our results to a broader population. Further, all of our patients had meniscal damage; therefore, our results cannot assist in clinical decision making for patients with mechanical meniscal symptoms without evidence of meniscal damage on MRI. Meniscal damage was classified in a hierarchical fashion, thus we cannot exclude the possibility that subjects had multiple types of damage morphology. However, additional analysis demonstrated that only 45 of the 227 knees had greater than one type of damage morphology. Due to the limited number of meniscal damage identified in the lateral compartment, we are unable to make compartment specific comparisons. Physical activity may be associated with type of meniscal damage and pain, however, data on activity levels was not collected. While the majority of this trial cohort is white, patients were enrolled from several centers across the United States and males and females were equally represented making this generalizable to the larger population.
In summary, we did not find an association between type of meniscal damage and frequency of mechanical meniscal symptoms. However, root tears were associated with greater levels of pain despite adjustment demographic and radiographic features. As root tears may have unique properties in regards to knee symptoms and biomechanics, further studies examining the outcomes of surgical and conservative management of patients with meniscal damage should take damage morphology into consideration.
Acknowledgments
Role of the Funding Source
Source of funding: P60 AR047782, R01 AR05557, T32 AR055885, K24 AR 057827 Sources of funding had no role or input in study design, collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Footnotes
Contributions:
| LM* | HY | JC | AG | MJ | ET | XL | EL | JK | |
|---|---|---|---|---|---|---|---|---|---|
| Conception and design | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Provision of study materials or patients | ✓ | ✓ | ✓ | ✓ | |||||
| Statistical expertise | ✓ | ✓ | |||||||
| Analysis and interpretation of the data | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Drafting of the article | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Critical revision of the article for important intellectual content | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Final approval of the article | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Obtaining of funding | ✓ | ✓ |
Use of Human Subjects
In the MeTeOR trial the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. All included patients gave informed consent for participation.
Competing Interests
Lindsey A. MacFarlane: No disclosures
Heidi Yang: No disclosures
Jamie E. Collins: No disclosures
Ali Guermazi: Dr. Guermazi is a Consultant to MerckSerono, TissueGene, OrthoTrophix,
AstraZeneca and Genzyme. He is a Shareholder of BICL, LLC.
Morgan H. Jones: Dr. Jones receives support from NIH grant R01 AR05557 09 (Jeff Katz, PI). He also receives support from NIH grant K23 AR066133 02 (Morgan Jones, PI).
Erin Teeple: Dr. Teeple was an external consultant for Tribiologics, LLC. The work was done in 2014 and she does not have an ongoing financial relationship with the company.
Li Xu: No disclosures
Elena Losina: No disclosures
Jeffrey N. Katz: No disclosures
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85-A:4–9. doi: 10.2106/00004623-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54:795–801. doi: 10.1002/art.21724. [DOI] [PubMed] [Google Scholar]
- 4.Kamimura M, Umehara J, Takahashi A, Aizawa T, Itoi E. Medial meniscus tear morphology and related clinical symptoms in patients with medial knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2015;23:158–163. doi: 10.1007/s00167-014-2939-z. [DOI] [PubMed] [Google Scholar]
- 5.Roubille C, Raynauld JP, Abram F, Paiement P, Dorais M, Delorme P, et al. The presence of meniscal lesions is a strong predictor of neuropathic pain in symptomatic knee osteoarthritis: a cross-sectional pilot study. Arthritis Res Ther. 2014;16:507. doi: 10.1186/s13075-014-0507-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oei EH, Nikken JJ, Verstijnen AC, Ginai AZ, Myriam Hunink MG. MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology. 2003;226:837–848. doi: 10.1148/radiol.2263011892. [DOI] [PubMed] [Google Scholar]
- 7.Hunter DJ, Guermazi A, Lo GH, Grainger AJ, Conaghan PG, Boudreau RM, et al. Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score) Osteoarthritis Cartilage. 2011;19:990–1002. doi: 10.1016/j.joca.2011.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359:1108–1115. doi: 10.1056/NEJMoa0800777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Englund M, Guermazi A, Lohmander LS. The meniscus in knee osteoarthritis. Rheum Dis Clin North Am. 2009;35:579–590. doi: 10.1016/j.rdc.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen JC, De Smet AA, Graf BK, Rosas HG. MR imaging-based diagnosis and classification of meniscal tears. Radiographics. 2014;34:981–999. doi: 10.1148/rg.344125202. [DOI] [PubMed] [Google Scholar]
- 11.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 12.Marzo JM, Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37:124–129. doi: 10.1177/0363546508323254. [DOI] [PubMed] [Google Scholar]
- 13.Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93:994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 14.Habata T, Uematsu K, Hattori K, Takakura Y, Fujisawa Y. Clinical features of the posterior horn tear in the medial meniscus. Arch Orthop Trauma Surg. 2004;124:642–645. doi: 10.1007/s00402-004-0659-4. [DOI] [PubMed] [Google Scholar]
- 15.Antony B, Driban JB, Price LL, Lo GH, Ward RJ, Nevitt M, et al. The relationship between meniscal pathology and osteoarthritis depends on the type of meniscal damage visible on magnetic resonance images: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2016 doi: 10.1016/j.joca.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368:1675–1684. doi: 10.1056/NEJMoa1301408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kellgren JLJ. The Epidemiology of Chronic Rheumatism, Atlas of Standard Radiograph. Vol. 2. Oxford: Blackwell Scientific; 1963. [Google Scholar]
- 18.Katz JN, Chaisson CE, Cole B, Guermazi A, Hunter DJ, Jones M, et al. The MeTeOR trial (Meniscal Tear in Osteoarthritis Research): rationale and design features. Contemp Clin Trials. 2012;33:1189–1196. doi: 10.1016/j.cct.2012.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 20.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 21.Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy. 1991;7:297–300. doi: 10.1016/0749-8063(91)90131-g. [DOI] [PubMed] [Google Scholar]
- 22.Choi JY, Chang EY, Cunha GM, Tafur M, Statum S, Chung CB. Posterior medial meniscus root ligament lesions: MRI classification and associated findings. AJR Am J Roentgenol. 2014;203:1286–1292. doi: 10.2214/AJR.14.12559. [DOI] [PubMed] [Google Scholar]
- 23.Choi ES, Park SJ. Clinical Evaluation of the Root Tear of the Posterior Horn of the Medial Meniscus in Total Knee Arthroplasty for Osteoarthritis. Knee Surg Relat Res. 2015;27:90–94. doi: 10.5792/ksrr.2015.27.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guermazi A, Hayashi D, Jarraya M, Roemer FW, Zhang Y, Niu J, et al. Medial posterior meniscal root tears are associated with development or worsening of medial tibiofemoral cartilage damage: the multicenter osteoarthritis study. Radiology. 2013;268:814–821. doi: 10.1148/radiol.13122544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33:569–574. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 26.Takahashi K, Hashimoto S, Nakamura H, Mori A, Sato A, Majima T, et al. Medial meniscal posterior root/horn radial tears correlate with cartilage degeneration detected by T1rho relaxation mapping. Eur J Radiol. 2015;84:1098–1104. doi: 10.1016/j.ejrad.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 27.Hein CN, Deperio JG, Ehrensberger MT, Marzo JM. Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee. 2011;18:189–192. doi: 10.1016/j.knee.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 28.Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25:951–958. doi: 10.1016/j.arthro.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 29.Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16:849–854. doi: 10.1007/s00167-008-0569-z. [DOI] [PubMed] [Google Scholar]
- 30.Bin SI, Kim JM, Shin SJ. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20:373–378. doi: 10.1016/j.arthro.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 31.Kim SB, Ha JK, Lee SW, Kim DW, Shim JC, Kim JG, et al. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27:346–354. doi: 10.1016/j.arthro.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Han SB, Shetty GM, Lee DH, Chae DJ, Seo SS, Wang KH, et al. Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy. 2010;26:1326–1332. doi: 10.1016/j.arthro.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 33.Lim HC, Bae JH, Wang JH, Seok CW, Kim MK. Non-operative treatment of degenerative posterior root tear of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2010;18:535–539. doi: 10.1007/s00167-009-0891-0. [DOI] [PubMed] [Google Scholar]


