Abstract
Purpose
Several complications may arise in patients wearing complete prosthetic appliances, including denture-associated infections and mucosal stomatitis due to Candida species. This study evaluated the activity of anti-Candida agents in denture adhesive and the cytotoxicities of these preparations for primary human gingival epithelial (GE) keratinocytes.
Materials and Methods
The anti-Candida activities of antimicrobial peptides, antimicrobial lipids, and antifungal agents against C. albicans ATCC 64124 or HMV4C were assessed in microdilution assays containing water or 1% denture adhesive. The minimal inhibitory concentrations (MIC) and the minimal bactericidal concentrations (MBC) were determined. The cytotoxicities of denture adhesive compounded with these agents were assessed in 1.0 × 105 primary GE keratinocytes in LGM-3 media with resazurin.
Results
Lactoferricin B, SMAP28, sphingosine, dihydrosphingosine, and phytosphingosine in 1% denture adhesive lost antimicrobial activity for C. albicans (p < 0.05). Amphotericin B, chlorhexidine dihydrochloride, chlorhexidine gluconate, fluconazole, and nystatin in 1% denture adhesive or compounded directly into denture adhesive and then diluted to 1% adhesive, did not lose antimicrobial activity. Compounded formulations were not cytotoxic (LD50 > 100.0 μg/ml) against primary human GE keratinocytes.
Conclusions
Antimicrobial peptides and antimicrobial lipids had diminished activities in 1% adhesive, suggesting that components in adhesives may inactivate local innate immune factors in the oral cavity, possibly predisposing denture wearers to Candida species infections. More importantly, antifungal agents retained their anti-C. albicans activities in denture adhesive, strongly suggesting that antifungal agents could be candidates for inclusion in adhesive formulations and used as prescribed topical treatments for individuals with denture stomatitis.
Keywords: Antimicrobial peptides, antimicrobial lipids, antifungal agents, denture prosthesis, denture adhesive, Candida, stomatitis, keratinocyte
Denture stomatitis and lesions are estimated to occur in up to 67% of complete denture wearers, compromising the quality of life of the edentulous patient.1 The result is erythema beneath the denture, most commonly on the palatal mucosa.2 The etiology of denture stomatitis is multifactorial and may be associated with both local and systemic factors.3 The most likely contributors include denture trauma, wearing dentures at night, denture hygiene, Candida species infections, low salivary pH, sugar consumption, and predisposing systemic conditions like aging, malnutrition, immunosuppression, radiation therapy, diabetes mellitus, and antibiotic treatment.1,4
The role of Candida infections in the pathogenesis of denture stomatitis is well known, and multiple strains of Candida species including C. albicans, C. glabrata, and C. tropicalis can populate the denture as well as the oral tissues.5-7 Furthermore, there is a direct relationship between the presence of C. albicans and other oral microorganisms and nocturnal denture use.8,9 One study reported that continuous wearing of dentures resulted in 61% of patients (n= 75) developing denture stomatitis, compared with 18% of those who did not wear their dentures at night.8
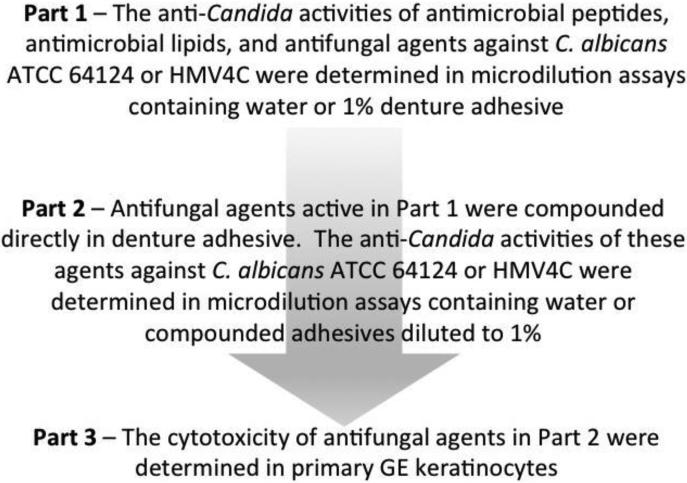
The underlying causes of denture stomatitis have not been well studied, but may be related to the long-term use of adhesives, which may alter the oral microflora or predispose the individual to oral candidiasis. Efficient treatment of denture stomatitis relies not only in the treatment of the tissues, but also the denture. Adding anti-Candida agents to denture adhesives could inhibit the colonization and growth of C. albicans of removable prostheses and reduce the severity and inflammation associated with stomatitis. The purpose of this study was to assess the anti-Candida activity of antimicrobial peptides, antimicrobial lipids, and antifungal agents when assayed in denture adhesive, the activity of these agents when compounded directly into denture adhesive, and cytotoxicity of these compounded formulations against primary human GE keratinocytes (Fig 1).
Figure 1.
Schema showing our approach to assess the anti-Candida activity of the antimicrobial substances for C. albicans ATCC 6412 and HMV4C when assayed in denture adhesive, the activity of antifungal agents when compounded directly into denture adhesive, and the cytotoxicity of compounded formulations against primary human GE keratinocytes.
MATERIALS AND METHODS
Solution and reagents
A commercial denture adhesive (Polygrip, GSK, Philadelphia, PA) that contained polymethylvinylether/maleic acid, sodium-calcium mixed partial salt, petrolatum, cellulose gum and mineral oil was used. Out-of-the-tube adhesive paste and 50% (wt./vol.) and 10% (wt./vol.) adhesive gels prepared using sterile (0.22 μm filtered) deionized water were all too viscous as diluents for broth microdilution assays. Therefore a 2% (wt./vol.) stock solution was used as a diluent for antimicrobial peptides, antimicrobial lipids, and antifungal agents and mixed 1:2 with C. albicans cultures to a final 1% denture adhesive concentration.
To confirm the sterility of the 2% denture adhesive, 100.0 μl was put onto trypticase soy agar and incubated at 37°C for 48 hours. No growth was observed.
C. albicans strains
Two strains of C. albicans were used. ATCC 64124 is the Darlington strain originally isolated from a patient suffering from chronic mucocutaneous candidiasis and treated with ketoconazole.10 HMV4C is a laboratory strain from the Iowa Institute for Oral Health Research (courtesy of Dr. David Drake, College of Dentistry, University of Iowa). Both strains were maintained on trypticase soy agar and cultured weekly. Their identities were confirmed with a Bruker Daltonik MALDI Biotyper (State Hygienic Laboratory, University of Iowa Research Park, Coralville, IA).
Cultures were prepared as described in the M27-A2 document from the Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Approved Standard, Second Edition ISBN 1-56238-469-4.11 C. albicans was cultured in RPMI 1640 media with 0.165 M MOPS, with L-glutamine, and without sodium bicarbonate (Lonza, Walkersville, MD) and incubated at 35°C. After 3 hours, the C. albicans culture turbidity was adjusted to an optical density of 80% transmittance (0.108 optical density) at 530 nm in a spectrophotometer (Spectronic 20D1; Thermo Fisher Scientific, Inc., Waltham, MA). Culture suspensions adjusted to this concentration typically contained 1.2 to 3.7 × 106 CFU/ml. Culture suspensions were diluted 10−3-fold in RPMI 1640 media containing resazurin (Alamar Blue; Invitrogen Corp., Carlsbad, CA).
Antimicrobial substances
The antimicrobial peptides histatin 5, lactoferricin B, and SMAP28 were used. Histatin 5 (AnaSpec, Inc., Fremont, CA) is a small cationic protein with fungicidal activity against C. albicans, C. kefyr, C. krusei, and C. parapsilosis.12 Lactoferricin B (AnaSpec, Inc.) is the active 17 to 41 amino acid residue fragment of lactoferrin. SMAP28 (Multiple Peptide Systems, San Diego, CA) is a sheep myeloid antimicrobial peptide with broad-spectrum antimicrobial activity against a variety of bacteria including oral pathogens.13-16
The antimicrobial long chain bases sphingosine (D-sphingosine), dihydrosphingosine (D-erythro-dihydrosphingosine), and phytosphingosine (Sigma-Aldrich, St. Louis, MO) were used and prepared as previously described.17,18 Long chain bases were dissolved in a chloroform:methanol solution (2:1), dispensed in tared glass tubes, dried under nitrogen, re-weighed, mixed with sterile 0.14 M NaCl to make 1.0 mg/ml stock solutions, and sonicated into solution at 5-minute increments at 37°C.
The antifungal agents amphotericin B, chlorhexidine dihydrochloride, chlorhexidine gluconate, fluconazole, and nystatin were used. Amphotericin B (Lonza) was supplied as a sterile 250 μg/ml solution. Chlorhexidine dihydrochloride (Sigma-Aldrich) was dissolved in methanol to make a 10.0 mg/ml stock solution. Chlorhexidine gluconate (Gum, oral rinse USP; Sunstar Americas, Inc., Schaumberg, IL) was supplied as a sterile 1.2 mg/ml solution (0.12%). Fluconazole (Sigma-Aldrich) was dissolved in N, N-dimethylformamide (Sigma-Aldrich) to make a 10.0 mg/ml stock solution. Nystatin (Sigma-Aldrich) was dissolved in dimethyl sulfoxide (Sigma-Aldrich) to make a 10.0 mg/ml stock solution.
Broth microdilution assay
A broth microdilution assay using resazurin (Alamar Blue) was used as described in the M27-A2, Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Approved Standard, Second Edition.11 In Part 1 (Fig 1), antimicrobial and antifungal substances were diluted 2-fold in 100.0 μl sterile deionized water or in 2% (wt./vol.) sterile denture adhesive in 96-well microtiter plates (Immulon 1 plates; ISC Bioexpress, Kaysville, UT). Next, 100.0 μl sterile deionized water or 2% (wt./vol.) denture adhesive was added to control wells; 100.0 μl RPMI 1640 media with resazurin containing 1.2 to 3.7 × 103 CFU/ml of C. albicans was added to wells containing diluted antimicrobial or antifungal agents in water or 2% (wt./vol.) denture adhesive (positive growth control wells); 100.0 μl sterile RPMI 1640 media with resazurin was added to wells containing water or 2% (wt./vol.) denture adhesive (negative growth control wells). In Part 2 (Fig 1), an antifungal agent-adhesive preparation was compounded by adding 0.1 g of antifungal agent to 10.0 g adhesive; 0.2 g of this preparation was added to 10.0 ml of Dulbecco's phosphate buffered saline (Gibco by Life Technologies, Corp., Grand Island NY) to form a 2.0% (wt/vol) preparation containing 200 μg/ml antifungal agent. The compounded adhesive was diluted 1:2 from 200 to 12.5 μg/ml. Then 100.0 μl RPMI 1640 media with resazurin containing 1.2 to 3.7 × 103 CFU/ml of C. albicans was added to wells containing diluted antifungal agents in water or 2% (wt./vol.) denture adhesive (positive growth control wells); 100.0 μl sterile RPMI 1640 media with resazurin was added to wells containing water or 2% (wt./vol.) denture adhesive (negative growth control wells).
After 48 hours at 35°C, the metabolic reduction of resazurin to resorufin was determined using an excitation wavelength of 544 nm and an emission wavelength of 590 nm (SpectraMax M2e Multi-Mode Microplate Reader; Molecular Devices, LLC, Sunnyvale, CA). The minimal inhibitory concentration (MIC) was defined as the lowest concentration of antimicrobial peptide, antimicrobial lipid, or antifungal agent found to reduce the fluorescence of microbial growth by more than 50% of the positive growth control. Well contents from the preceding three wells with no fluorescence were then spotted onto trypticase soy agar and incubated at 35°C for 48 hours. The minimal bactericidal concentration (MBC) was defined as the lowest concentration of antimicrobial or antifungal agent that produced viable growth from the wells.
Cytotoxicity of antifungal agents compounded in denture adhesives
For Part 3, the cytotoxicity of antifungal agents compounded in denture adhesive was examined using two strains of first passage human gingival epithelial (GE) keratinocyte cell lines, prepared in a previous study.19 GE keratinocytes were counted with a hemocytometer, adjusted to contain 1.0 × 105 viable keratinocytes/ml in LGM-3 media containing 2.5% FBS, added to 96-well plates (Corning, Inc., Corning, NY) at a density of 2.0×104 cells/well, and allowed to attach in a humidified incubator at 37°C in 5% CO2. After 2 hours, the cell culture media and nonadherent cells were removed.
The antifungal-adhesive preparation compounded above was diluted 1:2 from 200 to 12.5 μg/ml in 2% (wt./vol.) denture adhesive. 100 μl of the compounded adhesive was added to the GE keratinocyte cell cultures and 100 μl of LGM-3 media with resazurin was added, resulting in final concentrations of 100.0, 50.0, 25.0, and 12.5 μg antifungal agent/ml in 1% adhesive. LGM-3 media with resazurin and LGM-3 media with resazurin and denture adhesive were added to GE keratinocytes and served as live cell controls (LC). LGM-3 media with resazurin containing 1% sodium azide was added to GE keratinocytes and served as killed cell controls (KC). The plates were incubated at 37°C with 5% CO2. At 16 hours, the metabolic reduction of resazurin to resorufin was determined using an excitation wavelength of 544 nm and an emission wavelength of 590 nm (SpectraMax M2e Multi-Mode Microplate Reader). Cytotoxicity was defined as the (median fluorescence intensity of the test dilution/fluorescence intensity of LC) × 100. The lethal dose 50 (LD50) was determined where the 50% point intercepts the dose response curve to the concentration along the x-axis.
Microscopy
To assess whether denture adhesive induced visible changes in solutions of antimicrobial substances, 900 μl of 2% denture adhesive was mixed with 100 μl of histatin 5, lactoferricin B, SMAP28, sphingosine, dihydrosphingosine, phytosphingosine, amphotericin B, chlorhexidine dihydrochloride, chlorhexidine gluconate, fluconazole, or nystatin in a 24-well microtiter plate. The final concentration of antimicrobial agent was 10.0 μg/ml. Preparations were kept at room temperature. At 16 hours, preparations were examined for precipitates using a tissue culture microscope.
Statistical analysis
Broth microdilution assays containing antimicrobial peptides and antimicrobial lipids were performed twice and contained three replications each time (n = 6). Broth microdilution assays containing antifungal agents were performed twice and contained 6 replications each time (n = 12). One-way fixed-effects ANOVA models were used to the MIC and MBC concentrations. Pairwise group comparisons were conducted using Tukey's Honest Significant Differences (HSD). A 0.05 level was used to determine statistically significant differences. All analyses were conducted using JMP (Version 10.0, SAS, Cary, NC).
When MICs fell outside the range of the assay, we considered the MIC and MBC to be equal to the highest concentration used in the assay. For example, if the MIC was > 300 μg/ml, the MIC was conservatively estimated to be 300 μg/ml for the purpose of statistical analysis.
RESULTS
Activity of the antimicrobial agents when assayed in denture adhesive
Incorporating 1% denture adhesive in the broth microdilution assay did not inhibit the growth of C. albicans ATCC 64124 or HMV4C (data not shown); however, there were some differences in their growth patterns in water versus 1% denture adhesive (data not shown). The median fluorescence intensity (MFI) values of C. albicans ATCC 64124 and HMV4C in water were similar and not significantly different (p > 0.05); however, the MFI values of both C. albicans strains ATCC 64124 and HMV4C in water were higher (p < 0.05) than the MFI values of C. albicans ATCC 64124 in 1% denture adhesive.
In Part 1, the MICs and MBCs of antimicrobial peptides, antimicrobial lipids, and antifungal agents diluted in water or in denture adhesive for C. albicans ATCC 64124 and HMV4C were compared. Histatin 5 from two commercial sources had anti-C. albicans activities outside the range of concentrations used in our assays in water and 1% denture adhesive. MICs and MBCs were > 41.5 μg/ml for histatin 5 (Sigma-Aldrichdata not shown) and > 300.0 μg/ml for histatin 5 (AnaSpec) (Table 1). Lactoferricin B and SMAP28 were active against both C. albicans ATCC 64124 and HMV4C in water, but had anti-C. albicans activities outside the range of concentrations used in our assays in 1% denture adhesive (p < 0.05, Table 1).
Table 1.
MIC and MBC of antimicrobial agents in water or 1% denture adhesive for C. albicans ATCC 6412 and HMV4C. MIC and MBC values in each row with the same letter are not significantly different (p < 0.05).
| Test | ATCC 64124 (1% adhesive) | ATCC 64124 (water) | HMV4C (1% adhesive) | HMV4C (water) |
|---|---|---|---|---|
| Histatin 5 | ||||
| MIC | >300.0 (0.0)a | >300.0 (0.0)a | >300.0 (0.0)a | >300.0 (0.0)a |
| MBC | >300.0 (0.0)a | >300.0 (0.0)a | >300.0 (0.0)a | >300.0 (0.0)a |
| Lactoferricin B | ||||
| MIC | >300.0 (0.0)a | 100.0 (25.0)b | >300.0 (0.0)a | 75.0 (0.0)b |
| MBC | >300.0 (0.0)a | 125.0 (25.0)b | >300.0 (0.0)a | 150.0 (0.0)b |
| SMAP28 | ||||
| MIC | >20.0a | 1.3 (0.0)b | >20.0 (0.0)a | 1.3 (0.0)b |
| MBC | >20.0a | 1.7 (0.4)b | >20.0 (0.0)a | 1.7 (0.4)b |
| Sphingosine | ||||
| MIC | >25.0 (0.0)a | 1.6 (0.0)b | >25.0 (0.0)a | 0.3 (0.1)c |
| MBC | >25.0 (0.0)a | 2.1 (0.5)b | >25.0 (0.0)a | 0.3 (0.1)c |
| Dihydrosphingosine | ||||
| MIC | >25.0 (0.0)a | 0.8 (0.0)b | >25.0 (0.0)a | 0.4 (0.0)c |
| MBC | >25.0 (0.0)a | 20.8 (4.2)a | >25.0 (0.0)a | 0.4 (0.0)b |
| Phytosphingosine | ||||
| MIC | >25.0 (0.0)a | 10.4 (2.1)b | >25.0 (0.0)a | 0.4 (0.0)c |
| MBC | >25.0 (0.0)a | 14.6 (5.5)a | >25.0 (0.0)a | 0.4 (0.0)b |
MIC, minimal inhibitory concentrations
MBC, minimal bactericidal concentrations
Shown are the mean μg/ml (standard error μg/ml) values. n = 6.
Sphingosine, dihydrosphingosine, and phytosphingosine were also active against C. albicans ATCC 64124 and HMV4C in water, but had anti-C. albicans activities outside the range of concentrations used in our assays in 1% denture adhesive (p < 0.05, Table 1). The MBCs of sphingosine for C. albicans ATCC 64124 and the MBCs of sphingosine, dihydrosphingosine, and phytosphingosine for C. albicans HMV4C were all lower in water than that in 1% denture adhesive (p < 0.05, Table 1).
Amphotericin B, chlorhexidine dihydrochloride, chlorhexidine gluconate, fluconazole, and nystatin in water were all active against C. albicans ATCC 64124 and HMV4C (Table 2). The MICs of chlorhexidine dihydrochloride, chlorhexidine gluconate, fluconazole, and nystatin in water were similar to that in 1% denture adhesive (p > 0.05, Table 2). Interestingly, the denture adhesive increased the antimicrobial activity of amphotericin B for C. albicans ATCC 64124 (p < 0.05, Table 2).
Table 2.
MIC and MBC of antifungal agents in water or 1% denture adhesive for C. albicans ATCC 6412 and HMV4C. MIC and MBC values in each row with the same letter are not significantly different (p < 0.05).
| Test | ATCC 64124 (1% adhesive) | ATCC 64124 (water) | HMV4C (1% adhesive) | HMV4C (water) |
|---|---|---|---|---|
| Amphotericin B | ||||
| MIC | 0.05 (0.02)b | 0.2 (0.1)a | 0.1 (0.0)b | 0.2 (0.1)a,b |
| MBC | 0.1 (0.1)a | 0.3 (0.1)a | 0.1 (0.0)a | 0.2 (0.1)a |
| Chlorhexidine dihydrochloride | ||||
| MIC | 2.5 (1.7)a | 1.2 (0.5)a | 2.3 (0.1)a | 2.2 (1.1)a |
| MBC | 1.4 (0.8)a | 1.2 (0.5)a | 1.4 (0.4)a | 1.2 (0.5)a |
| Chlorhexidine gluconate | ||||
| MIC | 0.5 (0.2)a | 0.2 (0.0)a | 0.6 (0.3)a | 0.3 (0.1)a |
| MBC | 0.1 (0.2)a | 0.2 (0.0)a | 0.7 (0.4)a | 0.3 (0.1)a |
| Fluconazole | ||||
| MIC | 62.5 (0.0)a | 50.0 (0.0)a | 0.1 (0.0)b | 0.3 (0.1)b |
| MBC | 2.0 (0.0)b | 50.0 (0.0)a | 0.3 (0.1)b | 0.4 (0.1)b |
| Nystatin | ||||
| MIC | 0.8 (0.0)a | 1.0 (0.4)a | 0.8 (0.0)a | 0.9 (0.4)a |
| MBC | 0.6 (0.1)a | 1.0 (0.4)a | 0.9 (0.3)a | 0.9 (0.4)a |
MIC, minimal inhibitory concentrations
MBC, minimal bactericidal concentrations
Shown are the mean μg/ml (standard error μg/ml) values. n = 12.
Microscopy
Early in the work to assess the activity of anti-Candida agents in denture adhesive, precipitates were noted in some preparations. To assess the extent of these changes, 900 μl of 2% denture adhesive was mixed with 100 μl of histatin 5, lactoferricin B, SMAP28, sphingosine, dihydrosphingosine, phytosphingosine, amphotericin B, chlorhexidine dihydrochloride, chlorhexidine gluconate, fluconazole, or nystatin in a 24-well microtiter plate and examined at 16 hours using a tissue culture microscope. Insoluble precipitates were observed in preparations containing adhesive and histatin 5, lactoferricin B, SMAP28, sphingosine, dihydrosphingosine, phytosphingosine, and chlorhexidine dihydrochloride (Fig 2). Some precipitates were small, dense, and somewhat uniform in size (Figs 2a-c, f, h), whereas others were large and amorphous (Figure 2d, e). Interestingly, anti-Candida agents that precipitated in denture adhesive also had diminished anti-Candida antimicrobial activities.
Figure 2.
Micrographs of denture adhesive containing a) histatin 5, b) lactoferricin B, c) SMAP28, d) sphingosine, e) dihydrosphingosine, f) phytosphingosine, g) amphotericin B, h) chlorhexidine dihydrochloride, i) chlorhexidine gluconate, j) fluconazole, k) nystatin, and l) water. Note the presence of precipitates in preparations containing adhesive and a) histatin 5, b) lactoferricin B, c) SMAP28, d) sphingosine, e) dihydrosphingosine, f) phytosphingosine, h) and chlorhexidine dihydrochloride.
Antifungal agents compounded in denture adhesive
In Part 2, amphotericin B, chlorhexidine dihydrochloride, chlorhexidine gluconate, fluconazole, and nystatin were compounded directly in denture adhesive; diluted to 2.0% adhesive; and added to C. albicans ATCC 64124 and HMV4C in RPMI 1640 media with resazurin. Amphotericin B, chlorhexidine gluconate, fluconazole, and nystatin had high anti-C. albicans activity when compounded directly into denture adhesive and MIC values were ≥ 50 μg/ml for C. albicans ATCC 64124 and HMV4C (Table 3). Chlorhexidine dihydrochloride was active when compounded into denture adhesive, however MIC values were 2 to 3 times the MIC of chlorhexidine dihydrochloride in water (Table 2).
Table 3.
MIC and MBC of antifungal agents compounded into denture adhesive for C. albicans ATCC 6412 and HMV4C. MIC and MBC values in each row with the same letter are not significantly different (p < 0.05).
| Test | ATCC 64124 (1% adhesive) | ATCC 64124 (water) | HMV4C (1% adhesive) | HMV4C (water) |
|---|---|---|---|---|
| Amphotericin B | ||||
| MIC | 50.0 (0.0)a | 3.1 (0.0)b | 50.0 (0.0)a | 1.6 (0.0)c |
| MBC | 50.6 (0.4)a | 2.6 (0.5)b | 50.3 (0.0)a | 2.6 (0.5)b |
| Chlorhexidine dihydrochloride | ||||
| MIC | 3.1 (0.0)a,b | 1.3 (0.3)b | 9.4 (3.1)a | 3.1 (0.0)a,b |
| MBC | 3.1 (0.0)b | 1.3 (0.3)b | 10.4 (2.08)a | 3.1 (0.0)b |
| Chlorhexidine gluconate | ||||
| MIC | > 50.0 (0.0)a | 6.3 (0.0)c | > 50.0 (0.0)a | 12.5 (0.0)b |
| MBC | > 50.0 (0.0)a | 6.3 (0.0)c | > 50.0 (0.0)a | 12.5 (0.0)b |
| Fluconazole | ||||
| MIC | > 50.0 (0.0)a | > 50.0 (0.0)b | 0.1 (0.0)a | 0.1 (0.0)b |
| MBC | > 50.0 (0.0)a | > 50.0 (0.0)a | 0.1 (0.0)b | 0.1 (0.0)b |
| Nystatin | ||||
| MIC | > 50.0 (0.0)a | 3.1 (0.0)b | 50.0 (0.0)a | 2.6 (0.5)b |
| MBC | 0.01 (0.0)c | 3.1 (0.0)b | 50.0 (0.0)a | 3.1 (0.0)b |
MIC, minimal inhibitory concentrations
Shown are the mean μg/ml (standard error) values
Cytotoxicity of antifungal agents compounded in denture adhesives
The cytotoxicities of the five antifungal agents compounded in denture adhesive were examined using two primary GE keratinocyte cell lines. Preparations containing 100.0, 50.0, 25.0, and 12.5 μg/ml antifungal agent in 1% adhesive were not cytotoxic to either of these cell lines (LD50 > 100 μg/ml).
DISCUSSION
The oral cavity produces a diverse array of innate immune molecules, including antimicrobial peptides and proteins,20-22 antimicrobial lipids,18 and chemokines, cytokines, and other biological mediators.23 These molecules serve to control commensal flora as well as to moderate innate immune responses, adaptive immune responses, and inflammation. The results of this study suggest that denture adhesives may inactivate the activity of these innate immune molecules, possibly leading to the growth of C. albicans and the onset of denture-induced stomatitis.
Efficient treatment of denture stomatitis relies not only on the treatment of the tissues, but also the denture. Adding select antimicrobial substances to denture adhesives to inhibit the growth of C. albicans could aid in the treatment and/or prevention of denture stomatitis. Importantly, not all agents were inhibited in the presence of denture adhesive. The results of this study also suggest that chlorhexidine dihydrochloride and fluconazole could be candidates for inclusion in adhesive formulations and used as prescribed topical treatments for individuals with denture stomatitis. Adhesive preparations could be compounded to contain an antifungal that could treat infection and inflammation caused by the presence of C. albicans.
This is among the first studies to assess the MIC and MBC of antimicrobial peptides, antimicrobial lipids, and antifungal agents in a denture adhesive against C. albicans. Our results suggest that some antimicrobial agents known to be effective against fungi and bacteria lose their activity in the presence of 1% denture adhesive. One explanation for the loss of antimicrobial activity may be due to a denaturation of the antimicrobial substance by components in the adhesive (Fig 2). For example, both antimicrobial peptides and antimicrobial lipids formed a precipitate when mixed with denture adhesive. Denture adhesive contains a complex mixture of methyl vinyl ether/maleic acid, mineral oil, petrolatum, and carboxymethyl cellulose. To what extent these components induced the precipitation of the antimicrobial peptides or antimicrobial lipid is not known and will have to be determined in subsequent studies.
Future studies will include additional antimicrobial and antifungal agents and the use of different antimicrobial assays like the radial diffusion assay. Supplemental information suggests that similar trends occur with anti-Candida agents in radial diffusion assays containing 1% denture adhesive.24 Moreover, future studies will include the use of these antifungals in a randomized clinical control trial assessing the antifungal denture adhesive.
CONCLUSIONS
In this study, denture adhesive reduced antimicrobial activity of lactoferricin B, SMAP28, sphingosine, dihydrosphingosine, phytosphingosine, amphotericin B, chlorhexidine gluconate, and nystatin. This decrease in activity was seen in the presence of 1% denture adhesive in conventional broth microdilution assays. Both C. albicans strains were susceptible to chlorhexidine dihydrochloride (ATCC 6412 and HMV4C) and fluconazole (HMV4C). In conclusion, these latter two antifungal agents may be candidates for inclusion in adhesive formulations and used as prescribed topical treatments for individuals with denture stomatitis.
Acknowledgments
The authors thank Ryan T. Jepson, Clinical Laboratory Technical Specialist, State Hygienic Laboratory, University of Iowa Research Park, Coralville, IA for his help in confirming the identity of the C. albicans cultures.
This work was supported by NIH NIDCR grant R01 DE014390.
Footnotes
This study was presented at 2015 John J. Sharry Research Competition, at the American College of Prosthodontists Annual Session, Orlando, FL.
The authors deny any conflicts of interest.
References
- 1.Martori E, Ayuso-Montero R, Martinez-Gomis J, et al. Risk factors for denture-related oral mucosal lesions in a geriatric population. J Prosthet Dent. 2014;111:273–279. doi: 10.1016/j.prosdent.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 2.Arendorf TM, Walker DM. Denture stomatitis: a review. J Oral Rehabil. 1987;14:217–227. doi: 10.1111/j.1365-2842.1987.tb00713.x. [DOI] [PubMed] [Google Scholar]
- 3.Gendreau L, Loewy ZG. Epidemiology and etiology of denture stomatitis. J Prosthodont. 2011;20:251–260. doi: 10.1111/j.1532-849X.2011.00698.x. [DOI] [PubMed] [Google Scholar]
- 4.Zarb G, Bolender C, Eckert S, et al. Complete Dentures and Implant-Supported Prostheses. Mosby; St. Louis: 2004. Prosthodontic Treatment for Edentulous Patients. [Google Scholar]
- 5.Webb BC, Thomas CJ, Willcox MD, et al. Candida-associated denture stomatitis. Aetiology and management: a review. Part 3. Treatment of oral candidosis. Aust Dent J. 1998;43:244–249. doi: 10.1111/j.1834-7819.1998.tb00172.x. [DOI] [PubMed] [Google Scholar]
- 6.Webb BC, Thomas CJ, Willcox MD, et al. Candida-associated denture stomatitis. Aetiology and management: a review. Part 2. Oral diseases caused by Candida species. Aust Dent J. 1998;43:160–166. doi: 10.1111/j.1834-7819.1998.tb00157.x. [DOI] [PubMed] [Google Scholar]
- 7.Webb BC, Thomas CJ, Willcox MD, et al. Candida-associated denture stomatitis. Aetiology and management: a review. Part 1. Factors influencing distribution of Candida species in the oral cavity. Aust Dent J. 1998;43:45–50. doi: 10.1111/j.1834-7819.1998.tb00152.x. [DOI] [PubMed] [Google Scholar]
- 8.Jeganathan S, Payne JA, Thean HP. Denture stomatitis in an elderly edentulous Asian population. J Oral Rehabil. 1997;24:468–472. doi: 10.1046/j.1365-2842.1997.00523.x. [DOI] [PubMed] [Google Scholar]
- 9.Emami E, de Grandmont P, Rompre PH, et al. Favoring trauma as an etiological factor in denture stomatitis. J Dent Res. 2008;87:440–444. doi: 10.1177/154405910808700505. [DOI] [PubMed] [Google Scholar]
- 10.Ryley JF, Wilson RG, Barrett-Bee KJ. Azole resistance in Candida albicans. Sabouraudia. 1984;22:53–63. [PubMed] [Google Scholar]
- 11.Pfaller MA, Chaturvedi V, Espinel-Ingroff A, et al. Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Approved Standard. NCCLS; Wayne, PA, 19087-1898 USA: 2002. [Google Scholar]
- 12.Xu T, Levitz SM, Diamond RD, et al. Anticandidal activity of major human salivary histatins. Infect Immun. 1991;59:2549–2554. doi: 10.1128/iai.59.8.2549-2554.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brogden KA, Nordholm G, Ackermann M. Antimicrobial activity of cathelicidins BMAP28, SMAP28, SMAP29, and PMAP23 against Pasteurella multocida is more broad-spectrum than host species specific. Vet Microbiol. 2007;119:76–81. doi: 10.1016/j.vetmic.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Guthmiller JM, Vargas KG, Srikantha R, et al. Susceptibilities of oral bacteria and yeast to mammalian cathelicidins. Antimicrob Agents Chemother. 2001;45:3216–3219. doi: 10.1128/AAC.45.11.3216-3219.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joly S, Maze C, McCray PB, Jr., et al. Human beta-defensins 2 and 3 demonstrate strain-selective activity against oral microorganisms. J Clin Microbiol. 2004;42:1024–1029. doi: 10.1128/JCM.42.3.1024-1029.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weistroffer PL, Joly S, Srikantha R, et al. SMAP29 congeners demonstrate activity against oral bacteria and reduced toxicity against oral keratinocytes. Oral Microbiol Immunol. 2008;23:89–95. doi: 10.1111/j.1399-302X.2007.00389.x. [DOI] [PubMed] [Google Scholar]
- 17.Fischer CL, Drake DR, Dawson DV, et al. Antibacterial activity of sphingoid bases and fatty acids against Gram-positive and Gram-negative bacteria. Antimicrob Agents Chemother. 2012;56:1157–1161. doi: 10.1128/AAC.05151-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fischer CL, Walters KS, Drake DR, et al. Oral mucosal lipids are antibacterial against Porphyromonas gingivalis, induce ultrastructural damage, and alter bacterial lipid and protein compositions. Int J Oral Sci. 2013;5:130–140. doi: 10.1038/ijos.2013.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joly S, Organ CC, Johnson GK, et al. Correlation between beta-defensin expression and induction profiles in gingival keratinocytes. Mol Immunol. 2005;42:1073–1084. doi: 10.1016/j.molimm.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 20.Gorr SU. Antimicrobial peptides of the oral cavity. Periodontol 2000. 2009;51:152–180. doi: 10.1111/j.1600-0757.2009.00310.x. [DOI] [PubMed] [Google Scholar]
- 21.Gorr SU. Antimicrobial peptides in periodontal innate defense. Front Oral Biol. 2012;15:84–98. doi: 10.1159/000329673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gorr SU, Abdolhosseini M. Antimicrobial peptides and periodontal disease. J Clin Periodontol. 2011;38(Suppl 11):126–141. doi: 10.1111/j.1600-051X.2010.01664.x. [DOI] [PubMed] [Google Scholar]
- 23.Khan A. Detection and quantitation of forty eight cytokines, chemokines, growth factors and nine acute phase proteins in healthy human plasma, saliva and urine. J Proteomics. 2012;75:4802–4819. doi: 10.1016/j.jprot.2012.05.018. [DOI] [PubMed] [Google Scholar]
- 24.Bates AM, Garaicoa JL, Fischer CL, et al. Promise of combining antifungal agents in denture adhesives to fight Candida species infections. Data in Brief. 2016 doi: 10.1111/jopr.12565. manuscript in review. [DOI] [PMC free article] [PubMed] [Google Scholar]