Summary
Background
The scale-up of tobacco control, especially after the adoption of the Framework Convention for Tobacco Control, is a major public health success story. Nonetheless, smoking remains a leading risk for early death and disability worldwide, and therefore continues to require sustained political commitment. The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) offers a robust platform through which global, regional, and national progress toward achieving smoking-related targets can be assessed.
Methods
We synthesised 2818 data sources with spatiotemporal Gaussian process regression and produced estimates of daily smoking prevalence by sex, age group, and year for 195 countries and territories from 1990 to 2015. We analysed 38 risk-outcome pairs to generate estimates of smoking-attributable mortality and disease burden, as measured by disability-adjusted life-years (DALYs). We then performed a cohort analysis of smoking prevalence by birth-year cohort to better understand temporal age patterns in smoking. We also did a decomposition analysis, in which we parsed out changes in all-cause smoking-attributable DALYs due to changes in population growth, population ageing, smoking prevalence, and risk-deleted DALY rates. Finally, we explored results by level of development using the Socio-demographic Index (SDI).
Findings
Worldwide, the age-standardised prevalence of daily smoking was 25·0% (95% uncertainty interval [UI] 24·2–25·7) for men and 5·4% (5·1–5·7) for women, representing 28·4% (25·8–31·1) and 34·4% (29·4–38·6) reductions, respectively, since 1990. A greater percentage of countries and territories achieved significant annualised rates of decline in smoking prevalence from 1990 to 2005 than in between 2005 and 2015; however, only four countries had significant annualised increases in smoking prevalence between 2005 and 2015 (Congo [Brazzaville] and Azerbaijan for men and Kuwait and Timor-Leste for women). In 2015, 11·5% of global deaths (6·4 million [95% UI 5·7–7·0 million]) were attributable to smoking worldwide, of which 52·2% took place in four countries (China, India, the USA, and Russia). Smoking was ranked among the five leading risk factors by DALYs in 109 countries and territories in 2015, rising from 88 geographies in 1990. In terms of birth cohorts, male smoking prevalence followed similar age patterns across levels of SDI, whereas much more heterogeneity was found in age patterns for female smokers by level of development. While smoking prevalence and risk-deleted DALY rates mostly decreased by sex and SDI quintile, population growth, population ageing, or a combination of both, drove rises in overall smoking-attributable DALYs in low-SDI to middle-SDI geographies between 2005 and 2015.
Interpretation
The pace of progress in reducing smoking prevalence has been heterogeneous across geographies, development status, and sex, and as highlighted by more recent trends, maintaining past rates of decline should not be taken for granted, especially in women and in low-SDI to middle-SDI countries. Beyond the effect of the tobacco industry and societal mores, a crucial challenge facing tobacco control initiatives is that demographic forces are poised to heighten smoking's global toll, unless progress in preventing initiation and promoting cessation can be substantially accelerated. Greater success in tobacco control is possible but requires effective, comprehensive, and adequately implemented and enforced policies, which might in turn require global and national levels of political commitment beyond what has been achieved during the past 25 years.
Funding
Bill & Melinda Gates Foundation and Bloomberg Philanthropies.
Introduction
Smoking was the second leading risk factor for early death and disability worldwide in 2015.1 It has claimed more than 5 million lives every year since 1990,1 and its contribution to overall disease burden is growing, especially in lower income countries. The negative effects of smoking extend well beyond individual and population health2 as billions of dollars in lost productivity and health-care expenditure are related to smoking every year.3 Successfully combatting the tobacco industry's pursuit of new smokers has been further complicated by the substantive—and sometimes rapid—social, demographic, and economic shifts occurring worldwide.4, 5, 6 As the tobacco industry moves to target previously untapped markets,6, 7, 8 strong tobacco control policies and timely monitoring of smoking patterns are imperative.
Research in context.
Evidence before this study
Smoking is a widely recognised risk factor for premature morbidity and mortality, but adequate monitoring of smoking levels and trends throughout the world has been challenging. Increasing investments in multi-country survey series has improved the availability of data for smoking behaviours, especially in lower income countries, but such surveys are quite infrequent and differences in survey questions and definitions can hinder appropriate comparisons between countries and across time. Through the Global Burden of Diseases, Injuries, and Risk Factors 2013 Study (GBD 2013), researchers collated diverse data sources and synthesised them to produce comprehensive, comparable estimates of daily smoking prevalence, by sex and age group, for 188 countries from 1990 to 2013. Additional analyses, including those by Bilano and colleagues in 2015, have applied similar methods to project trends in tobacco use through 2025 in 173 countries for men and 178 countries for women.
Added value of this study
With the 2015 update to the GBD, the number of data sources included was substantially increased and the estimation process for both smoking prevalence and attributable disease burden, as measured by disability-adjusted life-years (DALYs), has been improved. Two novel analyses are also provided through the GBD 2015 study: a birth cohort analysis of smoking patterns over time and a decomposition analysis to parse out changes in total DALYs attributable to smoking to changes in population growth, population ageing, smoking prevalence, and risk-deleted DALY rates. The latter assessment can assist with identifying what factors are contributing to changes in disease burden due to smoking–demographic trends, efforts to address smoking, or some combination of these factors. Further, we used the Socio-demographic Index (SDI), a new summary measure of overall development from GBD 2015, to assess levels and trends in smoking prevalence and attributable burden across the development spectrum.
Implications of all the available evidence
Amid gains in tobacco control worldwide, smoking remains a leading risk factor for early death and disability. Although there have been some success stories, for many countries and territories, faster annualised rates of decline in smoking prevalence occurred between 1990 and 2005 than between 2005 and 2015. Although smoking prevalence and risk-deleted DALY rates fell across SDI quintiles, population growth and ageing ultimately offset these gains and contributed to overall increases in smoking-attributable disease burden in low to middle SDI geographies. Intensified tobacco control and strengthened monitoring are required to further reduce smoking prevalence and attributable burden, especially in view of the fact that demographic factors like population ageing are not easily amenable to intervention.
The past decade has brought a substantial expansion and strengthening of tobacco control initiatives, harnessing a wide range of effective interventions and policy instruments for addressing the tobacco epidemic.9, 10, 11, 12, 13, 14, 15, 16 Successful strategies include taxation of tobacco products,9 bans on smoking in public places and instituting smoke-free zones,10, 11 restrictions on the marketing and promotion of cigarettes, including plain packaging laws,12 community-wide and nation-wide smoking cessation interventions,13, 14 and enforcement of both text and pictorial warning labels on tobacco products.15, 16 Efforts to implement comprehensive tobacco control policies culminated in the adoption of the WHO Framework Convention on Tobacco Control (FCTC) in 2003.17 The FCTC, the world's first public health treaty, is viewed as a key driver of recent progress in reducing tobacco consumption and smoking prevalence in many regions of the world.18 As of 2016, 180 parties have ratified the FCTC,19 and many use WHO's MPOWER measures,20 established in 2008, to guide national and local FCTC compliance.21 More recently, WHO introduced the 25×25 non-communicable disease (NCD) targets, which include decreasing tobacco use by 30% between 2010 and 2025.22 Several countries have committed to an even stronger anti-smoking goal, setting national targets to become tobacco-free.23 Additionally, strengthening FCTC implementation was explicitly included in the United Nations' Sustainable Development Goals (SDGs).24 With tobacco control's increasing prioritisation on the global stage, accurately monitoring patterns in smoking and associated health outcomes is critical for identifying optimal intervention strategies across geographies, demographic groups, and the development spectrum.
Previous analyses of smoking prevalence and attributable disease burden often were hindered by poor data availability, methodological limitations, or both.25, 26, 27 Investments in survey series focused on tobacco, such as the Global Adult Tobacco Surveys (GATS) and the Global Youth Tobacco Surveys (GYTS), have supported more in-depth assessments of national tobacco use.28 Nonetheless, remaining data gaps across countries and time, as well as differences in smoking-related questions and definitions among available data sources, necessitated large analytical improvements to produce a systematic and consistent understanding of smoking patterns. As part of the Global Burden of Diseases, Injuries, and Risk Factors 2013 Study (GBD 2013), Ng and colleagues generated the first comprehensive, comparable estimates of smoking prevalence and tobacco consumption for 188 countries from 1980 to 2013.29 Since then, other studies have used similar data synthesis approaches to project smoking trends from 2010 to 2025 in 173 countries for men and 178 countries for women.30 Previous GBD studies31, 32 have assessed the contribution of smoking to overall disease burden through the comparative risk assessment framework developed by Murray and Lopez.33 Recent studies have quantified the global effects of tobacco on achieving NCD mortality targets34 and life expectancy,35 while several assessed smoking-attributable mortality and non-fatal health outcomes for specific locations.36, 37
In this analysis, we assess smoking prevalence and smoking-attributable disease burden, based on deaths and disability-adjusted life-years (DALYs), by sex and age group for 195 countries and territories from 1990 to 2015. We also investigate differences in smoking prevalence and attributable burden according to the Socio-demographic Index (SDI), a summary measure of income per capita, educational attainment, and total fertility rate.38 Additionally, we assess age and sex patterns by birth cohort across levels of development. Finally, we perform a decomposition analysis of potential drivers of smoking-attributable disease burden over time.
Methods
This study follows the overall GBD 2015 comparative risk assessment framework, details of which have been previously published.1 Here we summarise the main steps in the estimation process; the appendix provides more details about data inputs and modelling strategies (pp 5–9). This study fully adheres to the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER).39
Estimating smoking exposure
Improving upon methods used by Ng and colleagues,29 we calculated two exposure measures: prevalence of daily smoking of tobacco and the smoking impact ratio. We defined a daily smoker as an individual using any type of smoked tobacco product on a daily basis.40, 41 We used 2818 data sources, covering 2928 geography-years of data, identified through the Global Health Data Exchange (GHDx), WHO InfoBase Database, and International Smoking Statistics Database; the appendix provides additional details on data sources (pp 5, 6). For any data that did not match our exposure definition we adjusted for frequency of use or type of tobacco consumed to avoid potential biases. We adjusted for smoking frequency and type simultaneously, which allowed us to account for their mutual correlations with each other (appendix pp 7, 8). Second-hand smoke exposure is estimated separately in GBD and is not included in this analysis.
We generated estimates of smoking prevalence by sex and 5-year age groups starting at age 10 years. Any data that spanned multiple age groups or were reported for both sexes combined were split based on the age-sex patterns recorded from data sources with multiple age-sex groupings.29 We then used spatiotemporal Gaussian process regression (ST-GPR), a data synthesis method widely used in GBD,1 which allowed us to draw strength across geography, time, and age, incorporate both data and model uncertainty, and produce a full time-series of estimates for all 195 geographies. The appendix provides full details on the modelling strategy (pp 5–9).
The second exposure measure, the smoking impact ratio, was first described by Peto and Lopez42 as part of a method to estimate smoking-attributable burden in the absence of information about smoking patterns. The smoking impact ratio is defined as the population lung cancer mortality rate in excess of the background lung cancer mortality rate recorded in non-smokers in the population, relative to the excess lung cancer mortality rate recorded in a reference group of smokers. We computed the smoking impact ratio for each analytic unit using the geography-specific, year-specific, age-specific, and sex-specific population lung cancer mortality rates from GBD 2015,20 and reference group lung cancer mortality rates from prospective cohort studies (appendix p 9).
Defining risk-outcome pairs
We assessed all available evidence that supported causal associations between smoking and 38 health outcomes using a systematic approach adapted from Hill's criteria for causation43 and the World Cancer Research Fund evidence grading schema (appendix p 9).44 We added seven new outcomes to those used in GBD 2013:31 larynx cancer, peptic ulcer disease, rheumatoid arthritis, cataract, macular degeneration, hip fracture, and non-hip fracture.
Estimating attributable burden
We used 5-year lagged smoking prevalence in estimating smoking attributable burden for cardiovascular diseases, tuberculosis, diabetes, lower respiratory infections, asthma, cataracts, macular degeneration, fractures, rheumatoid arthritis, and peptic ulcer disease. We chose a 5-year lag based on findings showing that most risk-reduction occurs within 5 years of quitting smoking.45 We used the smoking impact ratio in estimating smoking- attributable burden for cancers, chronic obstructive pulmonary disease (COPD), interstitial lung disease, other chronic respiratory diseases, and pneumoconiosis. The appendix provides a complete list of outcomes and their associated exposure metric (pp 31, 32).
For each outcome included in this analysis we used relative risk estimates derived from prospective cohort studies comparing smokers to never smokers (appendix p 9). Population attributable fractions were calculated based on estimates of exposure, relative risks, and the theoretical minimum risk exposure level for smoking (zero smoking). Following population attributable fraction calculation, we multiplied estimates of deaths and DALYs by outcome-specific population attributable fractions, and then summed them across all 38 outcomes to compute overall disease burden attributable to smoking (appendix p 9).
Uncertainty analysis
We captured and propagated uncertainty through all steps of the analysis, including sampling uncertainty from data extraction, uncertainty from models used to adjust data reported in non-standard frequency-type combinations, uncertainty in the ST-GPR model, and uncertainty in deaths and DALYs for the 38 included outcomes. Ultimately, we produced 1000 draws of exposure and attributable burden estimates, for each geography, year, age, and sex, from which 95% uncertainty intervals (UIs) were taken using the 2·5 percentile and 97·5 percentile of the distribution.
Decomposing changes in DALYs
To parse out the drivers of changes in smoking-attributable DALYs from 2005 to 2015, we assessed the relative contribution of four factors: population growth, population age structure, risk-deleted DALY rates, and smoking exposure. Risk-deleted rates are defined as the DALY rates that would have been recorded had we removed smoking as a risk factor. We estimated risk-deleted DALY rates by multiplying the observed cause-specific DALY rates by one minus the cause-specific population attributable fractions. For the decomposition analysis, we used the methods developed by Das Gupta (appendix p 10).46
Smoking and its association with SDI
We present results aggregated by level of SDI, a composite indicator of development estimated for each geography based on lag-distributed income per capita, average educational attainment among individuals over age 15 years, and total fertility rate. SDI values were scaled to a range from 0 to 1.38 The appendix provides SDI values for each geography (pp 21–25).
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Global, regional, and national levels and trends of daily smoking
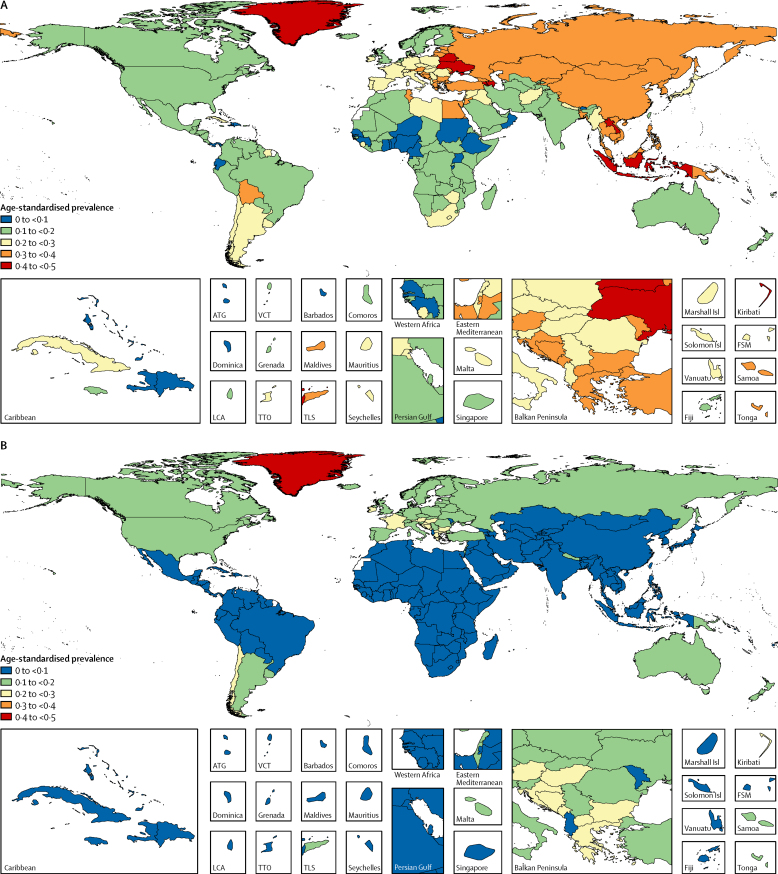
Worldwide in 2015, the age-standardised prevalence of daily smoking was 25·0% (95% uncertainty interval [UI] 24·2–25·7) in men and 5·4% (5·1–5·7) in women (table 1). 51 countries and territories had significantly higher prevalence of smoking than the global average for men, and these countries were located mainly in central and eastern Europe and southeast Asia (figure 1). For women, 70 countries, mainly in western and central Europe, significantly exceeded the global average. Among men, prevalence of daily smoking was highest in middle SDI countries, whereas for women high SDI countries had the highest prevalence of daily smokers (figure 2). Compared with other SDI levels, low SDI geographies generally had the lowest prevalence of daily smoking for both sexes.
Table 1.
Age-standardised prevalence of daily smoking in 2015 and annualised rate of change in age-standardised prevalence from 1990–2015, 1990–2005, and 2005–2015 for men and women
| SDI level | 2015 female age-standardised prevalence | 2015 male age-standardised prevalence | Annualised rate of change, female 1990–2015 | Annualised rate of change, male 1990–2015 | Annualised rate of change, female 1990–2005 | Annualised rate of change, male 1990–2005 | Annualised rate of change, female 2005–2015 | Annualised rate of change, male 2005–2015 | |
|---|---|---|---|---|---|---|---|---|---|
| Global | 5·4 (5·1 to 5·7) | 25·0 (24·2 to 25·7) | −1·7 (−2·0 to −1·4) | −1·3 (−1·5 to −1·2) | −1·6 (−2·0 to −1·2) | −1·2 (−1·4 to −1·0) | −1·8 (−2·4 to −1·1) | −1·5 (−1·9 to −1·1) | |
| Afghanistan | Low SDI | 7·0 (4·6 to 9·7) | 21·4 (18·4 to 24·7) | 0·1 (−2·0 to 2·3) | 0·5 (−0·4 to 1·3) | −0·1 (−3·5 to 3·1) | 0·6 (−0·8 to 2·0) | 0·4 (−4·2 to 4·6) | 0·2 (−1·7 to 2·1) |
| Albania | High-middle SDI | 2·3 (1·8 to 2·9) | 29·0 (26·2 to 31·8) | 0·0 (−1·3 to 1·2) | −0·5 (−1·0 to 0·0) | −0·8 (−2·6 to 1·1) | −1·0 (−1·7 to −0·3) | 1·2 (−1·3 to 3·6) | 0·2 (−0·8 to 1·2) |
| Algeria | Middle SDI | 2·2 (1·5 to 3·2) | 17·5 (14·9 to 20·4) | −5·3 (−7·4 to −3·3) | −1·2 (−2·1 to −0·3) | −5·4 (−8·6 to −2·5) | −1·7 (−3·0 to −0·4) | −5·1 (−9·6 to −0·7) | −0·4 (−2·1 to 1·5) |
| American Samoa | High-middle SDI | 12·8 (10·3 to 15·4) | 27·2 (23·7 to 31·1) | −0·1 (−1·3 to 1·0) | −0·4 (−1·2 to 0·3) | 0·4 (−1·2 to 2·0) | −0·4 (−1·4 to 0·7) | −0·9 (−3·0 to 1·2) | −0·4 (−1·9 to 1·0) |
| Andorra | High SDI | 18·4 (15·9 to 21·0) | 24·9 (21·9 to 27·6) | −0·5 (−1·4 to 0·2) | −1·0 (−1·6 to −0·3) | −0·3 (−1·5 to 0·9) | −0·8 (−1·7 to 0·1) | −0·9 (−2·5 to 0·7) | −1·1 (−2·4 to 0·1) |
| Angola | Low-middle SDI | 1·6 (0·9 to 2·6) | 14·2 (12·5 to 16·1) | −0·7 (−3·5 to 2·2) | 0·5 (−0·2 to 1·3) | −1·2 (−5·7 to 3·3) | 0·4 (−0·8 to 1·5) | 0·0 (−6·0 to 5·7) | 0·8 (−0·8 to 2·3) |
| Antigua and Barbuda | High SDI | 2·2 (1·6 to 3·0) | 4·4 (3·4 to 5·7) | 1·4 (−0·4 to 3·3) | 0·6 (−0·9 to 2·0) | 1·8 (−1·1 to 4·7) | 1·8 (−0·9 to 4·1) | 0·9 (−2·7 to 4·9) | −1·2 (−4·1 to 2·0) |
| Argentina | High-middle SDI | 14·6 (12·7 to 16·6) | 21·1 (18·6 to 23·6) | −1·1 (−1·9 to −0·4) | −1·0 (−1·7 to −0·3) | −1·0 (−2·2 to 0·2) | −1·0 (−2·0 to 0·1) | −1·2 (−3·0 to 0·4) | −1·1 (−2·6 to 0·4) |
| Armenia | High-middle SDI | 1·5 (1·1 to 2·1) | 43·5 (40·0 to 46·9) | 0·3 (−1·5 to 2·2) | 0·0 (−0·4 to 0·5) | 1·1 (−1·7 to 4·0) | 0·6 (−0·1 to 1·3) | −0·8 (−4·5 to 3·1) | −0·7 (−1·7 to 0·1) |
| Australia | High SDI | 13·3 (12·4 to 14·3) | 15·6 (14·5 to 16·6) | −2·1 (−2·4 to −1·8) | −1·9 (−2·2 to −1·6) | −2·3 (−2·7 to −1·9) | −1·7 (−2·1 to −1·4) | −1·9 (−2·7 to −1·1) | −2·2 (−3·0 to −1·4) |
| Austria | High SDI | 22·7 (20·2 to 25·5) | 30·0 (27·4 to 32·6) | 0·3 (−0·3 to 1·0) | −0·3 (−0·7 to 0·2) | 1·1 (0·2 to 1·9) | −0·3 (−0·9 to 0·3) | −0·8 (−2·1 to 0·5) | −0·2 (−1·3 to 0·8) |
| Azerbaijan | High-middle SDI | 1·6 (1·1 to 2·1) | 40·2 (36·5 to 43·7) | 1·1 (−0·7 to 2·7) | 0·9 (0·3 to 1·5) | 0·9 (−2·0 to 3·7) | 0·6 (−0·3 to 1·5) | 1·3 (−2·7 to 5·2) | 1·3 (0·1 to 2·4) |
| Bahrain | High-middle SDI | 6·2 (4·4 to 8·9) | 12·1 (10·1 to 14·3) | −0·2 (−2·2 to 1·7) | −1·3 (−2·3 to −0·4) | −0·5 (−3·6 to 2·5) | −1·9 (−3·3 to −0·5) | 0·2 (−3·7 to 4·5) | −0·3 (−2·4 to 1·7) |
| Bangladesh | Low-middle SDI | 1·8 (1·1 to 2·6) | 38·0 (34·1 to 42·6) | −2·9 (−5·2 to −0·4) | 0·3 (−0·4 to 1·0) | −1·9 (−5·2 to 1·7) | 0·4 (−0·5 to 1·4) | −4·3 (−9·7 to 0·6) | 0·0 (−1·2 to 1·3) |
| Barbados | High-middle SDI | 2·1 (1·5 to 3·0) | 6·9 (5·4 to 8·9) | 1·3 (−0·6 to 3·3) | 0·3 (−1·1 to 1·7) | 1·5 (−1·5 to 4·6) | 1·0 (−1·0 to 3·2) | 1·1 (−3·2 to 5·5) | −0·7 (−3·8 to 2·2) |
| Belarus | High SDI | 13·5 (11·4 to 15·9) | 42·4 (39·7 to 45·1) | 0·7 (−0·3 to 1·8) | −0·8 (−1·2 to −0·5) | 0·3 (−1·6 to 2·1) | −1·5 (−2·0 to −0·9) | 1·3 (−1·0 to 3·8) | 0·1 (−0·7 to 1·0) |
| Belgium | High SDI | 16·7 (15·0 to 18·4) | 21·2 (19·4 to 23·2) | −1·1 (−1·6 to −0·6) | −1·6 (−2·0 to −1·2) | −1·0 (−1·8 to −0·2) | −1·5 (−2·1 to −0·9) | −1·3 (−2·7 to 0·1) | −1·7 (−2·8 to −0·5) |
| Belize | Middle SDI | 2·1 (1·6 to 2·9) | 13·3 (10·7 to 16·0) | −0·9 (−2·5 to 0·9) | −1·0 (−2·2 to 0·1) | −1·2 (−3·9 to 1·6) | −1·4 (−3·0 to 0·4) | −0·4 (−4·1 to 3·5) | −0·6 (−3·0 to 1·7) |
| Benin | Low SDI | 1·0 (0·7 to 1·5) | 8·6 (7·3 to 10·2) | −3·8 (−6·2 to −1·6) | −0·8 (−1·8 to 0·2) | −4·4 (−7·9 to −1·0) | −0·5 (−1·9 to 0·9) | −3·0 (−7·7 to 1·6) | −1·3 (−3·4 to 0·8) |
| Bermuda | High SDI | 4·7 (3·5 to 6·3) | 13·3 (10·8 to 16·1) | −1·1 (−2·8 to 0·5) | −1·0 (−2·2 to 0·2) | −1·5 (−4·1 to 1·3) | −1·0 (−2·8 to 1·0) | −0·6 (−4·2 to 3·0) | −0·9 (−3·6 to 1·6) |
| Bhutan | Low-middle SDI | 3·8 (2·9 to 4·8) | 8·5 (7·2 to 9·9) | 0·3 (−1·8 to 2·4) | −0·5 (−1·6 to 0·7) | −0·2 (−3·9 to 3·6) | −1·1 (−3·0 to 1·1) | 1·0 (−3·3 to 5·5) | 0·4 (−2·1 to 3·0) |
| Bolivia | Middle SDI | 8·8 (7·1 to 10·7) | 32·1 (27·5 to 37·1) | −1·1 (−2·3 to 0·0) | −0·3 (−1·1 to 0·5) | −0·4 (−2·0 to 1·3) | 0·8 (−0·1 to 1·9) | −2·2 (−4·5 to 0·1) | −1·9 (−3·5 to −0·4) |
| Bosnia and Herzegovina | High-middle SDI | 21·1 (18·0 to 24·5) | 36·0 (33·3 to 38·7) | 0·5 (−0·4 to 1·5) | 0·2 (−0·2 to 0·7) | 0·5 (−0·8 to 1·9) | 0·6 (0·0 to 1·3) | 0·5 (−1·2 to 2·1) | −0·3 (−1·1 to 0·5) |
| Botswana | Middle SDI | 4·3 (3·2 to 5·5) | 18·3 (16·3 to 20·5) | −1·0 (−2·4 to 0·5) | −0·4 (−1·1 to 0·2) | −1·1 (−3·4 to 1·2) | −0·6 (−1·5 to 0·3) | −0·8 (−4·1 to 2·3) | −0·2 (−1·5 to 1·1) |
| Brazil | Middle SDI | 8·2 (7·5 to 9·0) | 12·6 (11·8 to 13·5) | −3·3 (−3·9 to −2·7) | −3·3 (−3·8 to −2·9) | −3·4 (−4·3 to −2·6) | −3·8 (−4·4 to −3·2) | −3·0 (−4·1 to −1·9) | −2·6 (−3·5 to −1·8) |
| Brunei | High SDI | 3·7 (3·1 to 4·4) | 19·8 (18·0 to 21·8) | −0·3 (−1·2 to 0·6) | −0·7 (−1·3 to −0·2) | −0·4 (−1·8 to 1·1) | −0·8 (−1·7 to −0·1) | −0·3 (−2·3 to 1·7) | −0·6 (−1·7 to 0·5) |
| Bulgaria | High-middle SDI | 28·3 (24·5 to 32·0) | 35·2 (32·4 to 38·0) | 0·6 (−0·3 to 1·5) | −0·6 (−1·0 to −0·1) | 1·3 (0·1 to 2·8) | 0·0 (−0·6 to 0·6) | −0·5 (−2·1 to 1·1) | −1·4 (−2·4 to −0·5) |
| Burkina Faso | Low SDI | 4·2 (2·8 to 6·3) | 12·5 (10·7 to 14·9) | −1·0 (−3·4 to 1·2) | −0·6 (−1·5 to 0·4) | −1·0 (−4·3 to 2·4) | −0·6 (−2·2 to 1·0) | −1·0 (−5·3 to 3·5) | −0·5 (−2·6 to 1·7) |
| Burundi | Low SDI | 0·9 (0·7 to 1·2) | 9·7 (7·9 to 11·7) | −1·1 (−2·4 to 0·2) | −0·9 (−2·0 to 0·2) | −1·5 (−3·4 to 0·5) | −1·3 (−3·1 to 0·3) | −0·6 (−3·2 to 2·1) | −0·3 (−2·8 to 2·3) |
| Cambodia | Low-middle SDI | 3·8 (2·8 to 5·1) | 34·2 (31·8 to 36·6) | −1·8 (−3·7 to 0·2) | −1·0 (−1·4 to −0·6) | −2·1 (−4·5 to 0·5) | −0·5 (−1·0 to 0·1) | −1·3 (−4·8 to 1·9) | −1·8 (−2·6 to −1·0) |
| Cameroon | Low-middle SDI | 1·6 (1·2 to 2·1) | 8·3 (7·1 to 9·6) | −1·5 (−3·6 to 0·6) | −1·1 (−2·0 to −0·2) | −2·0 (−5·7 to 1·7) | −0·9 (−2·4 to 0·8) | −0·7 (−4·8 to 3·8) | −1·6 (−3·7 to 0·6) |
| Canada | High SDI | 12·4 (10·8 to 14·2) | 14·5 (12·6 to 16·7) | −2·8 (−3·3 to −2·2) | −2·5 (−3·0 to −1·9) | −3·7 (−4·4 to −3·1) | −3·0 (−3·6 to −2·4) | −1·4 (−2·8 to 0·0) | −1·6 (−3·1 to 0·0) |
| Cape Verde | Low-middle SDI | 2·5 (1·7 to 3·6) | 9·8 (8·0 to 11·7) | −0·9 (−3·1 to 1·3) | −0·6 (−1·6 to 0·6) | −1·1 (−4·3 to 2·4) | −0·7 (−2·2 to 0·8) | −0·6 (−5·2 to 4·0) | −0·3 (−2·5 to 1·8) |
| Central African Republic | Low SDI | 1·4 (0·8 to 2·2) | 11·6 (10·1 to 13·4) | −0·8 (−3·6 to 1·9) | 0·3 (−0·4 to 1·1) | −1·2 (−6·1 to 3·0) | 0·2 (−1·0 to 1·3) | −0·2 (−6·5 to 6·1) | 0·6 (−1·0 to 2·2) |
| Chad | Low SDI | 1·9 (1·3 to 2·8) | 11·5 (9·6 to 13·8) | −0·8 (−3·0 to 1·4) | −0·2 (−1·2 to 0·8) | −0·8 (−4·1 to 2·5) | −0·2 (−1·5 to 1·3) | −0·7 (−5·2 to 3·8) | −0·2 (−2·2 to 1·5) |
| Chile | High-middle SDI | 22·7 (20·1 to 25·3) | 27·7 (24·8 to 30·8) | 0·9 (0·2 to 1·6) | 0·3 (−0·3 to 1) | 1·9 (1·0 to 2·9) | 1·2 (0·4 to 2·0) | −0·6 (−2·0 to 0·7) | −1·0 (−2·3 to 0·3) |
| China | Middle SDI | 2·2 (2·1 to 2·4) | 37·5 (36·9 to 38·0) | −2·6 (−3·2 to −2·1) | −1·0 (−1·1 to −0·9) | −3·3 (−4·1 to −2·5) | −1·0 (−1·2 to −0·9) | −1·6 (−2·7 to −0·4) | −1·0 (−1·2 to −0·8) |
| Colombia | High-middle SDI | 6·0 (4·4 to 7·8) | 14·4 (11·6 to 17·5) | −2·2 (−3·7 to −0·6) | −1·8 (−2·9 to −0·7) | −1·8 (−4·1 to 0·4) | −1·4 (−3·0 to 0·2) | −2·8 (−6·4 to 0·9) | −2·3 (−4·6 to 0·1) |
| Comoros | Low SDI | 1·2 (1·0 to 1·5) | 14·0 (11·9 to 16·2) | −0·8 (−1·9 to 0·5) | −0·2 (−1·2 to 0·9) | −1·0 (−2·8 to 1·0) | −0·1 (−1·7 to 1·7) | −0·5 (−3·1 to 2·0) | −0·4 (−2·8 to 1·9) |
| Congo (Brazzaville) | Low-middle SDI | 1·2 (0·7 to 1·9) | 11·0 (9·5 to 12·7) | 0·5 (−2·3 to 3·5) | 0·9 (0·1 to 1·7) | 0·1 (−4·3 to 4·7) | 0·5 (−0·6 to 1·7) | 1·1 (−5·1 to 7·1) | 1·6 (0·1 to 3·3) |
| Costa Rica | High-middle SDI | 4·8 (3·5 to 6·3) | 10·4 (8·3 to 12·7) | −1·1 (−2·8 to 0·7) | −1·8 (−2·9 to −0·7) | −1·1 (−3·7 to 1·4) | −2·0 (−3·4 to −0·5) | −1·1 (−4·4 to 2·5) | −1·5 (−3·9 to 0·7) |
| Côte d'Ivoire | Low SDI | 1·4 (0·9 to 2·0) | 14·2 (12·0 to 16·5) | −2·4 (−4·7 to −0·1) | 0·8 (−0·2 to 1·8) | −2·1 (−5·8 to 1·5) | 0·4 (−1·1 to 2·0) | −3·0 (−7·8 to 1·5) | 1·3 (−0·7 to 3·3) |
| Croatia | High-middle SDI | 25·9 (22·3 to 29·7) | 30·4 (27·7 to 33·3) | 0·0 (−0·9 to 0·8) | −0·9 (−1·4 to −0·4) | −0·8 (−2·0 to 0·4) | −1·3 (−1·9 to −0·6) | 1·2 (−0·6 to 2·9) | −0·4 (−1·4 to 0·7) |
| Cuba | High-middle SDI | 9·4 (7·2 to 11·9) | 20·9 (17·4 to 24·8) | −2·3 (−3·7 to −0·9) | −2·0 (−3·0 to −1·1) | −1·5 (−3·7 to 0·6) | −1·5 (−2·8 to −0·1) | −3·6 (−6·6 to −0·8) | −2·9 (−4·8 to −0·9) |
| Cyprus | High SDI | 14·5 (12·5 to 16·5) | 37·5 (34·6 to 40·5) | 0·5 (−0·4 to 1·4) | 0·5 (0·0 to 1·0) | 1·1 (−0·2 to 2·5) | 1·1 (0·4 to 1·8) | −0·4 (−2·2 to 1·3) | −0·5 (−1·5 to 0·4) |
| Czech Republic | High SDI | 19·4 (16·6 to 22·3) | 28·7 (26·0 to 31·1) | −0·5 (−1·3 to 0·3) | −0·6 (−1·1 to −0·1) | −0·8 (−1·8 to 0·4) | −1·0 (−1·7 to −0·3) | −0·2 (−1·9 to 1·5) | 0·0 (−1·0 to 1·0) |
| Democratic Republic of the Congo | Low SDI | 0·9 (0·5 to 1·4) | 14·1 (12·6 to 15·6) | −1·0 (−3·9 to 1·8) | −0·1 (−0·7 to 0·6) | −1·1 (−5·9 to 3·6) | −0·3 (−1·4 to 0·9) | −1·0 (−7·7 to 5·1) | 0·2 (−1·3 to 1·7) |
| Denmark | High SDI | 16·2 (14·7 to 17·6) | 17·5 (16·1 to 19·1) | −3·0 (−3·4 to −2·6) | −3·0 (−3·4 to −2·6) | −3·5 (−3·9 to −3·1) | −2·4 (−2·8 to −2·0) | −2·3 (−3·3 to −1·3) | −3·8 (−4·8 to −2·8) |
| Djibouti | Low-middle SDI | 2·8 (2·2 to 3·4) | 21·6 (18·2 to 25·0) | 0·0 (−1·2 to 1·3) | −0·5 (−1·5 to 0·5) | 0·1 (−2·0– to 1·9) | −0·5 (−1·8 to 1·0) | 0·0 (−2·4 to 2·6) | −0·6 (−2·5 to 1·2) |
| Dominica | High-middle SDI | 1·2 (0·9 to 1·7) | 6·5 (5·0 to 8·3) | −0·9 (−2·8 to 1·0) | −0·7 (−2·2 to 0·7) | −0·7 (−3·7 to 2·2) | −0·6 (−2·7 to 1·7) | −1·2 (−5·3 to 2·8) | −0·9 (−3·9 to 2·0) |
| Dominican Republic | High-middle SDI | 5·2 (3·9 to 7·0) | 8·7 (7·1 to 10·6) | −2·7 (−4·2 to −1·2) | −2·4 (−3·6 to −1·2) | −2·5 (−4·6 to −0·5) | −2·3 (−3·9 to −0·7) | −3·1 (−6·1 to −0·1) | −2·5 (−4·6 to −0·3) |
| Ecuador | High-middle SDI | 1·9 (1·5 to 2·3) | 8·9 (7·5 to 10·6) | −1·8 (−2·9 to −0·6) | −2·3 (−3·3 to −1·3) | −0·4 (−2·3 to 1·5) | −2·9 (−4·5 to −1·3) | −3·8 (−6·2 to −1·4) | −1·4 (−3·4 to 0·7) |
| Egypt | Middle SDI | 0·6 (0·4 to 0·8) | 31·7 (28·8 to 35·0) | −0·9 (−2·9 to 1·4) | 0·2 (−0·4 to 0·9) | −1·1 (−4·4 to 2·5) | 0·0 (−0·9 to 0·9) | −0·6 (−5·2 to 3·6) | 0·6 (−0·7 to 1·9) |
| El Salvador | Middle SDI | 3·3 (2·4 to 4·5) | 10·0 (7·8 to 12·4) | −1·0 (−3·0 to 0·8) | −0·3 (−1·6 to 1·0) | −1·0 (−3·8 to 1·6) | −0·3 (−2·5 to 1·7) | −1·0 (−4·7 to 2·6) | −0·2 (−3·1 to 2·7) |
| Equatorial Guinea | Middle SDI | 1·2 (0·7 to 1·9) | 8·6 (7·5 to 9·9) | −0·4 (−3·3 to 2·5) | 0·0 (−0·7 to 0·9) | −0·6 (−5·3 to 3·9) | 0·0 (−1·2 to 1·2) | 0·0 (−6·2 to 6·2) | 0·1 (−1·7 to 1·8) |
| Eritrea | Low SDI | 0·6 (0·5 to 0·8) | 10·2 (8·3 to 12·4) | −1·7 (−2·9 to −0·5) | −0·9 (−2·1 to 0·2) | −1·6 (−3·5 to 0·2) | −0·9 (−2·4 to 0·5) | −1·7 (−4·2 to 0·7) | −1·0 (−3·2 to 1·1) |
| Estonia | High SDI | 14·8 (12·8 to 16·9) | 30·2 (28·0 to 32·3) | −0·7 (−1·4 to 0·0) | −0·9 (−1·3 to −0·6) | −0·3 (−1·1 to 0·5) | −0·3 (−0·7 to 0·1) | −1·4 (−3 to 0·2) | −1·9 (−2·8 to −1·1) |
| Ethiopia | Low SDI | 0·8 (0·7 to 1·0) | 7·1 (5·6 to 8·7) | −1·5 (−2·8 to −0·3) | −0·4 (−1·7 to 0·8) | −1·4 (−3·2 to 0·4) | −0·9 (−2·7 to 1·0) | −1·8 (−4·3 to 0·6) | 0·3 (−2·1 to 2·6) |
| Federated States of Micronesia | Middle SDI | 6·5 (5·1 to 8·1) | 20·8 (17·7 to 24·2) | −0·2 (−1·5 to 1·1) | −0·5 (−1·3 to 0·3) | −0·2 (−2·1 to 1·7) | −0·5 (−1·8 to 0·8) | −0·2 (−2·9 to 2·6) | −0·4 (−2·2 to 1·4) |
| Fiji | High-middle SDI | 4·2 (3·4 to 5·2) | 17·5 (15·3 to 19·9) | −0·2 (−1·3 to 1·0) | −0·5 (−1·3 to 0·3) | −0·5 (−2·3 to 1·4) | −0·4 (−1·8 to 0·9) | 0·4 (−2·1 to 2·8) | −0·5 (−2·2 to 1·1) |
| Finland | High SDI | 15·5 (13·8 to 17·4) | 19·3 (17·4 to 21·1) | −0·4 (−0·9 to 0·2) | −1·4 (−1·9 to −1·0) | −0·4 (−1·0 to 0·1) | −1·5 (−1·8 to −1·2) | −0·4 (−1·7 to 0·9) | −1·3 (−2·4 to −0·4) |
| France | High SDI | 21·5 (19·2 to 23·9) | 25·3 (22·9 to 27·6) | −0·6 (−1·2 to −0·1) | −1·5 (−2·0 to −1·1) | −0·4 (−1·2 to 0·3) | −1·5 (−2·1 to −0·9) | −1·0 (−2·3 to 0·4) | −1·6 (−2·7 to −0·4) |
| Gabon | Middle SDI | 2·2 (1·3 to 3·6) | 14·7 (13·1 to 16·4) | −0·2 (−2·9 to 2·6) | 0·4 (−0·2 to 1·2) | 0·0 (−4·4 to 4·2) | 0·6 (−0·5 to 1·8) | −0·3 (−6·1 to 5·4) | 0·1 (−1·4 to 1·6) |
| Georgia | High-middle SDI | 3·8 (2·9 to 4·8) | 38·9 (35·5 to 42·2) | −0·1 (−1·7 to 1·5) | 0·5 (−0·1 to 1·0) | −0·3 (−2·8 to 2·3) | 0·8 (0·0 to 1·6) | 0·1 (−3·1 to 3·4) | −0·1 (−1·2 to 1·0) |
| Germany | High SDI | 19·4 (17·3 to 21·7) | 25·2 (22·8 to 27·4) | −0·3 (−0·9 to 0·2) | −0·9 (−1·4 to −0·5) | −0·2 (−0·8 to 0·4) | −1·1 (−1·6 to −0·6) | −0·5 (−1·9 to 0·7) | −0·6 (−1·7 to 0·4) |
| Ghana | Low-middle SDI | 0·9 (0·6 to 1·3) | 5·8 (4·8 to 6·9) | −0·8 (−2·9 to 1·4) | −1·1 (−2·1 to 0·0) | −0·8 (−3·9 to 2·4) | −0·9 (−2·4 to 0·7) | −0·9 (−5·4 to 3·6) | −1·4 (−3·4 to 0·5) |
| Greece | High-middle SDI | 27·2 (24·6 to 29·6) | 36·6 (34·0 to 39·0) | 0·5 (−0·1 to 0·9) | −0·8 (−1·1 to −0·5) | 1·2 (0·5 to 1·9) | −0·8 (−1·3 to −0·4) | −0·6 (−1·7 to 0·5) | −0·7 (−1·5 to 0·1) |
| Greenland | High-middle SDI | 44·3 (41·1 to 47·6) | 42·7 (39·4 to 45·9) | −0·8 (−1·1 to −0·4) | −1·0 (−1·4 to −0·6) | −0·8 (−1·3 to −0·2) | −1·1 (−1·6 to −0·5) | −0·7 (−1·6 to 0·1) | −0·8 (−1·7 to 0·1) |
| Grenada | High-middle SDI | 2·5 (1·8 to 3·4) | 10·5 (8·3 to 13·1) | −0·6 (−2·5 to 1·2) | 0·3 (−1·0 to 1·6) | −0·3 (−3·1 to 2·5) | 1·0 (−1·1 to 3·0) | −1·1 (−4·9 to 2·7) | −0·7 (−3·4 to 2·0) |
| Guam | High SDI | 14·5 (12·1 to 17·1) | 22·1 (19·4 to 24·8) | −1·0 (−2·1 to 0·0) | −0·9 (−1·6 to −0·1) | −0·5 (−2·1 to 1·1) | −0·7 (−1·8 to 0·4) | −1·7 (−4·0 to 0·6) | −1·2 (−2·8 to 0·4) |
| Guatemala | Low-middle SDI | 2·5 (1·8 to 3·4) | 13·4 (10·8 to 16·4) | −1·0 (−2·7 to 0·8) | 0·3 (−0·9 to 1·6) | −1·7 (−4·4 to 1·0) | 0·0 (−1·8 to 1·8) | 0·2 (−3·5 to 3·8) | 0·9 (−1·7 to 3·4) |
| Guinea | Low SDI | 1·4 (0·9 to 2·1) | 6·9 (5·6 to 8·4) | −1·0 (−3·5 to 1·3) | −0·6 (−1·7 to 0·5) | −1·4 (−5·0 to 2·3) | −0·8 (−2·5 to 1·0) | −0·6 (−5·7 to 4·1) | −0·4 (−2·9 to 2·0) |
| Guinea-Bissau | Low SDI | 1·0 (0·6 to 1·5) | 11·4 (9·4 to 13·5) | −0·9 (−3·4 to 1·6) | −0·3 (−1·4 to 0·8) | −1·2 (−5·2 to 2·6) | −0·5 (−2·1 to 1·1) | −0·4 (−5·4 to 4·7) | 0·1 (−2·2 to 2·2) |
| Guyana | Middle SDI | 2·0 (1·4 to 2·8) | 15·8 (13·0 to 18·9) | −0·9 (−2·7 to 0·9) | 0·8 (−0·3 to 1·9) | −0·1 (−3·0 to 2·7) | 2·3 (0·6 to 4·1) | −2·2 (−6·1 to 1·7) | −1·5 (−3·9 to 0·8) |
| Haiti | Low-middle SDI | 3·2 (2·3 to 4·3) | 8·2 (6·6 to 10·1) | −1·5 (−3·3 to 0·2) | −2·6 (−3·8 to −1·4) | −2·1 (−4·7 to 0·7) | −2·8 (−4·7 to −0·8) | −0·6 (−4·2 to 3·0) | −2·4 (−5·0 to 0·1) |
| Honduras | Middle SDI | 1·8 (1·2 to 2·4) | 16·4 (13·8 to 19·2) | −3·2 (−5·1 to −1·4) | −1·0 (−2·0 to 0·0) | −3·9 (−6·7 to −1·0) | −0·8 (−2·4 to 0·9) | −2·2 (−6·3 to 1·9) | −1·3 (−3·5 to 0·9) |
| Hungary | High SDI | 22·8 (19·5 to 26·1) | 27·5 (25·0 to 29·9) | −0·1 (−1·0 to 0·8) | −1·1 (−1·7 to −0·7) | 0·4 (−0·8 to 1·7) | −0·8 (−1·5 to −0·1) | −0·9 (−2·8 to 0·9) | −1·7 (−2·7 to −0·6) |
| Iceland | High SDI | 14·4 (12·5 to 16·4) | 14·5 (13·0 to 16·3) | −2·8 (−3·4 to −2·2) | −2·8 (−3·4 to −2·3) | −3·2 (−3·9 to −2·5) | −2·9 (−3·5 to −2·2) | −2·2 (−3·7 to −0·7) | −2·8 (−4·2 to −1·4) |
| India | Low-middle SDI | 2·8 (2·6 to 3·2) | 17·4 (16·8 to 18·2) | −0·3 (−1·0 to 0·3) | −2·1 (−2·3 to −1·8) | 1·0 (−0·3 to 2·2) | −1·4 (−1·8 to −1·0) | −2·2 (−3·7 to −0·7) | −3·1 (−3·7 to −2·4) |
| Indonesia | Middle SDI | 3·8 (2·7 to 5·1) | 46·7 (43·9 to 49·5) | 1·8 (0·0 to 3·7) | 0·2 (−0·1 to 0·6) | 5·3 (2·7 to 8·1) | 0·3 (−0·2 to 0·9) | −3·4 (−7·1 to 0·2) | 0·1 (−0·7 to 0·9) |
| Iran | High-middle SDI | 2·1 (1·4 to 3·0) | 17·9 (15·3 to 20·6) | −0·8 (−3·0 to 1·4) | 0·1 (−0·8 to 1·0) | −1·6 (−4·6 to 1·4) | 0·3 (−0·9 to 1·5) | 0·3 (−3·7 to 4·6) | −0·2 (−1·9 to 1·5) |
| Iraq | Middle SDI | 3·0 (2·0 to 4·3) | 23·8 (20·4 to 27·6) | 0·1 (−2·1 to 2·3) | −0·4 (−1·2 to 0·4) | 0·5 (−2·7 to 4·0) | −0·4 (−1·4 to 0·7) | −0·6 (−4·7 to 3·5) | −0·5 (−2·2 to 1·0) |
| Ireland | High SDI | 21·9 (19·5 to 24·5) | 20·6 (18·4 to 22·9) | −0·5 (−1·1 to 0·0) | −1·4 (−1·9 to −0·9) | −0·7 (−1·5 to 0·1) | −1·4 (−2·0 to −0·7) | −0·3 (−1·6 to 1·1) | −1·4 (−2·7 to −0·2) |
| Israel | High SDI | 13·0 (11·4 to 14·9) | 23·4 (21·0 to 26·0) | −1·6 (−2·3 to −0·8) | −1·2 (−1·8 to −0·6) | −2·6 (−3·7 to −1·6) | −1·8 (−2·6 to −0·9) | 0·0 (−1·6 to 1·6) | −0·4 (−1·7 to 0·8) |
| Italy | High SDI | 17·1 (15·3 to 19·0) | 23·2 (21·2 to 25·5) | −0·9 (−1·5 to −0·3) | −1·1 (−1·5 to −0·6) | −0·8 (−1·5 to −0·2) | −1·2 (−1·6 to −0·7) | −1·0 (−2·2 to 0·2) | −0·9 (−1·9 to 0·2) |
| Jamaica | High-middle SDI | 6·3 (4·8 to 8·1) | 12·7 (10·1 to 15·7) | 0·2 (−1·4 to 1·8) | −1·4 (−2·6 to −0·2) | 0·8 (−1·5 to 3·2) | −0·4 (−2·0 to 1·4) | −0·7 (−3·8 to 2·3) | −2·9 (−5·3 to −0·5) |
| Japan | High SDI | 9·3 (8·9 to 9·6) | 26·6 (26·1 to 27·1) | −0·7 (−0·9 to −0·5) | −2·4 (−2·5 to −2·3) | 0·7 (0·4 to 1·0) | −1·7 (−1·8 to −1·6) | −2·8 (−3·2 to −2·3) | −3·4 (−3·6 to −3·2) |
| Jordan | High-middle SDI | 6·8 (5·1 to 8·8) | 30·7 (26·9 to 34·6) | −0·4 (−2·2 to 1·4) | −0·1 (−0·8 to 0·6) | −0·7 (−3·3 to 2·0) | 0·6 (−0·3 to 1·7) | 0·0 (−3·5 to 3·3) | −1·2 (−2·5 to 0·2) |
| Kazakhstan | High-middle SDI | 4·1 (3·2 to 5·1) | 37·0 (34·4 to 39·5) | 0·4 (−1·2 to 2·0) | −0·1 (−0·6 to 0·4) | 1·8 (−0·8 to 4·5) | −0·1 (−0·9 to 0·7) | −1·7 (−4·9 to 1·6) | −0·1 (−1·2 to 0·9) |
| Kenya | Low SDI | 1·0 (1·0 to 1·1) | 14·9 (14·4 to 15·4) | −1·7 (−2·0 to −1·5) | −0·8 (−1·0 to −0·6) | −1·3 (−1·7 to −1·0) | −0·5 (−0·8 to −0·2) | −2·4 (−2·8 to −1·9) | −1·4 (−1·8 to −0·9) |
| Kiribati | Low-middle SDI | 24·7 (21·3 to 28·4) | 47·8 (43·8 to 51·5) | −0·6 (−1·4 to 0·1) | −0·3 (−0·7 to 0·2) | 0·1 (−0·9 to 1·2) | 0·1 (−0·5 to 0·8) | −1·8 (−3·4 to −0·2) | −0·8 (−1·8 to 0·1) |
| Kuwait | High SDI | 5·2 (4·1 to 6·5) | 23·2 (20·9 to 25·6) | 3·6 (1·7 to 5·4) | −0·6 (−1·2 to 0·1) | 1·7 (−1·1 to 4·8) | −0·6 (−1·7 to 0·4) | 6·4 (3·1 to 9·8) | −0·6 (−1·9 to 0·7) |
| Kyrgyzstan | Middle SDI | 2·8 (2·1 to 3·8) | 32·9 (30·1 to 35·8) | 2·9 (1·2 to 4·7) | 0·2 (−0·3 to 0·7) | 3·0 (0·4 to 5·6) | 0·3 (−0·5 to 1·1) | 2·7 (−0·8 to 6·5) | 0·0 (−1·0 to 1·2) |
| Laos | Low-middle SDI | 9·7 (6·9 to 13·3) | 46·5 (42·6 to 50·3) | −0·1 (−2·0 to 1·7) | −0·3 (−0·8 to 0·1) | 0·5 (−1·7 to 3) | −0·1 (−0·7 to 0·5) | −1·0 (−4·5 to 2·4) | −0·6 (−1·5 to 0·2) |
| Latvia | High SDI | 16·1 (13·8 to 18·6) | 38·3 (35·9 to 40·6) | 0·2 (−0·7 to 1·2) | 0·1 (−0·3 to 0·5) | 0·7 (−0·6 to 2·1) | 0·6 (0 to 1·2) | −0·4 (−2·1 to 1·2) | −0·6 (−1·3 to 0·1) |
| Lebanon | High-middle SDI | 17·9 (13·8 to 22·8) | 28·0 (24·5 to 31·8) | −0·2 (−1·6 to 1·3) | −1·7 (−2·4 to −1·1) | −0·2 (−2·2 to 1·9) | −2·1 (−2·9 to −1·2) | −0·2 (−3·2 to 2·6) | −1·2 (−2·7 to 0·2) |
| Lesotho | Low-middle SDI | 0·9 (0·7 to 1·1) | 28·0 (25·7 to 30·5) | −1·9 (−3·6 to −0·3) | −0·4 (−0·9 to 0·1) | −2·5 (−5·1 to 0·2) | −0·4 (−1·1 to 0·3) | −1·0 (−4·7 to 2·6) | −0·4 (−1·5 to 0·6) |
| Liberia | Low SDI | 0·9 (0·6 to 1·4) | 10·4 (9·0 to 12·0) | −2·5 (−4·9 to −0·2) | −0·6 (−1·5 to 0·3) | −2·8 (−6·5 to 0·8) | −0·2 (−1·7 to 1·2) | −2·0 (−7·5 to 3·4) | −1·2 (−3·4 to 0·7) |
| Libya | Middle SDI | 0·4 (0·2 to 0·6) | 24·8 (21·8 to 28·1) | −0·3 (−2·8 to 2·3) | 0·2 (−0·6 to 0·9) | −0·7 (−4·4 to 3·2) | 0·4 (−0·6 to 1·5) | 0·3 (−4·9 to 5·5) | −0·1 (−1·7 to 1·5) |
| Lithuania | High SDI | 14·0 (12·0 to 16·5) | 32·8 (30·4 to 35·2) | 0·2 (−0·7 to 1·2) | −0·4 (−0·8 to 0·0) | 0·1 (−1·2 to 1·4) | −0·4 (−0·9 to 0·2) | 0·4 (−1·5 to 2·1) | −0·4 (−1·4 to 0·4) |
| Luxembourg | High SDI | 18·5 (16·0 to 21·3) | 23·8 (21·0 to 26·5) | −0·7 (−1·5 to −0·1) | −0·9 (−1·5 to −0·4) | −0·5 (−1·6 to 0·4) | −0·7 (−1·4 to 0·1) | −1·1 (−2·6 to 0·6) | −1·3 (−2·6 to −0·1) |
| Macedonia | High-middle SDI | 23·2 (20·1 to 26·6) | 36·1 (33·4 to 38·9) | 1·0 (−0·1 to 1·9) | 0·4 (−0·1 to 0·9) | 1·2 (−0·3 to 2·7) | 0·7 (0·0 to 1·4) | 0·7 (−1·3 to 2·8) | 0·0 (−1·0 to 1·0) |
| Madagascar | Low SDI | 1·5 (1·2 to 1·9) | 19·0 (15·9 to 22·2) | −3·8 (−5·0 to −2·6) | −1·6 (−2·5 to −0·6) | −3·8 (−5·5 to −1·9) | −1·2 (−2·4 to 0·1) | −3·9 (−6·3 to −1·1) | −2·2 (−4·2 to −0·3) |
| Malawi | Low SDI | 1·4 (1·1 to 1·8) | 15·3 (13·0 to 17·7) | −1·7 (−3·1 to −0·4) | −1·2 (−2·2 to −0·3) | −1·5 (−3·5 to 0·5) | −0·9 (−2·3 to 0·5) | −2·2 (−4·9 to 0·8) | −1·8 (−3·8 to 0·0) |
| Malaysia | High-middle SDI | 1·7 (1·2 to 2·3) | 31·9 (28·8 to 35·1) | −1·7 (−3·7 to 0·4) | −0·7 (−1·2 to −0·1) | −1·9 (−5·0 to 1·4) | −0·6 (−1·4 to 0·2) | −1·3 (−5·4 to 2·6) | −0·7 (−2·0 to 0·4) |
| Maldives | Middle SDI | 6·8 (5·1 to 8·7) | 30·8 (27·7 to 33·9) | −1·2 (−2·9 to 0·6) | 0·7 (0·1 to 1·4) | −0·7 (−3·3 to 2·2) | 0·4 (−0·7 to 1·5) | −1·9 (−5·6 to 1·7) | 1·2 (−0·2 to 2·6) |
| Mali | Low SDI | 0·7 (0·5 to 1·1) | 10·8 (9·1 to 12·7) | −4·6 (−6·8 to −2·3) | 0·2 (−0·9 to 1·1) | −3·7 (−7·4 to −0·2) | 0·1 (−1·4 to 1·8) | −5·9 (−10·8 to −1·0) | 0·2 (−1·9 to 2·4) |
| Malta | High-middle SDI | 15·1 (13·1 to 17·1) | 23·4 (20·8 to 25·9) | −1·4 (−2·2 to −0·6) | −1·9 (−2·5 to −1·3) | −1·9 (−3·0 to −0·8) | −2·4 (−3·2 to −1·7) | −0·6 (−2·3 to 0·9) | −1·1 (−2·4 to 0·2) |
| Marshall Islands | Middle SDI | 4·2 (3·4 to 5·2) | 22·8 (19·4 to 26·5) | −0·5 (−1·8 to 0·9) | −0·7 (−1·6 to 0·1) | −0·7 (−2·6 to 1·2) | −0·6 (−1·8 to 0·6) | −0·3 (−2·8 to 2·4) | −0·8 (−2·5 to 0·6) |
| Mauritania | Low SDI | 2·4 (1·5 to 3·6) | 14·9 (12·4 to 17·8) | −0·7 (−3·3 to 1·6) | −0·2 (−1·2 to 0·7) | −0·8 (−4·2 to 2·7) | 0·2 (−1·2 to 1·7) | −0·6 (−5·5 to 3·5) | −0·9 (−2·9 to 1·1) |
| Mauritius | High-middle SDI | 2·7 (1·8 to 3·9) | 28·3 (24·9 to 31·7) | −0·8 (−3·0 to 1·4) | −1·0 (−1·6 to −0·4) | −2·5 (−6·0 to 0·9) | −1·8 (−2·6 to −1·0) | 1·8 (−2·9 to 6·0) | 0·3 (−1·2 to 1·5) |
| Mexico | Middle SDI | 4·8 (4·5 to 5·2) | 15·0 (14·4 to 15·7) | −3·2 (−3·6 to −2·7) | −2·5 (−2·7 to −2·3) | −5·5 (−6·1 to −4·8) | −4·2 (−4·5 to −3·8) | 0·3 (−0·6 to 1·2) | 0·0 (−0·5 to 0·5) |
| Moldova | High-middle SDI | 5·1 (4·2 to 6·1) | 32·5 (30·6 to 34·6) | 0·4 (−0·9 to 1·6) | −0·9 (−1·3 to −0·5) | 0·3 (−1·8 to 2·3) | −1·0 (−1·6 to −0·4) | 0·5 (−2·3 to 3·2) | −0·7 (−1·6 to 0·2) |
| Mongolia | High-middle SDI | 5·1 (3·9 to 6·4) | 37·0 (33·4 to 40·5) | 0·4 (−1·1 to 2·0) | −0·3 (−0·8 to 0·2) | 0·3 (−1·7 to 2·4) | 0·1 (−0·5 to 0·8) | 0·5 (−2·7 to 3·4) | −0·8 (−1·9 to 0·2) |
| Montenegro | High-middle SDI | 26·4 (23·4 to 29·5) | 33·0 (30·6 to 35·5) | 1·7 (0·9 to 2·6) | 0·9 (0·4 to 1·3) | 2·2 (0·6 to 3·7) | 1·5 (0·7 to 2·4) | 1·0 (−0·8 to 2·8) | −0·2 (−1·2 to 0·8) |
| Morocco | Low-middle SDI | 0·9 (0·6 to 1·3) | 16·0 (13·4 to 18·9) | −2·5 (−4·8 to −0·2) | −1·3 (−2·2 to −0·3) | −4·3 (−8·0 to −0·7) | −1·1 (−2·4 to 0·2) | 0·2 (−4·4 to 4·8) | −1·6 (−3·4 to 0·3) |
| Mozambique | Low SDI | 3·1 (2·5 to 3·8) | 17·2 (14·5 to 20·1) | −1·5 (−2·7 to −0·2) | −0·5 (−1·5 to 0·5) | −0·5 (−2·3 to 1·2) | 0·6 (−0·7 to 1·9) | −2·9 (−5·2 to −0·7) | −2·1 (−3·9 to −0·5) |
| Myanmar | Low-middle SDI | 6·5 (5·0 to 8·4) | 25·8 (23·5 to 28·4) | −1·3 (−2·9 to 0·4) | −1·6 (−2·1 to −1·0) | −0·3 (−2·6 to 2·3) | −1·7 (−2·5 to −1·0) | −2·7 (−5·7 to 0·3) | −1·3 (−2·4 to −0·2) |
| Namibia | Middle SDI | 6·8 (5·3 to 8·6) | 18·3 (16·5 to 20·1) | −1·8 (−3·0 to −0·5) | −1·1 (−1·7 to −0·6) | −1·2 (−3·1 to 0·8) | −1·0 (−1·8 to −0·1) | −2·8 (−5·4 to −0·3) | −1·4 (−2·6 to −0·3) |
| Nepal | Low-middle SDI | 12·7 (9·6 to 16·0) | 27·4 (23·9 to 31·4) | −2·5 (−3·9 to −0·9) | −1·7 (−2·4 to −1·0) | −0·9 (−2·7 to 1·3) | −1·1 (−1·9 to −0·2) | −4·8 (−7·7 to −2·2) | −2·6 (−4·0 to −1·1) |
| Netherlands | High SDI | 16·6 (15·0 to 18·4) | 19·0 (17·1 to 20·8) | −1·7 (−2·2 to −1·3) | −1·8 (−2·2 to −1·4) | −1·4 (−1·9 to −0·9) | −1·2 (−1·6 to −0·8) | −2·2 (−3·3 to −1·1) | −2·7 (−3·8 to −1·7) |
| New Zealand | High SDI | 14·9 (14·0 to 15·9) | 16·3 (15·3 to 17·2) | −1·8 (−2·1 to −1·5) | −1·5 (−1·8 to −1·3) | −1·3 (−1·7 to −0·9) | −1·2 (−1·5 to −0·8) | −2·5 (−3·2 to −1·7) | −2·1 (−2·8 to −1·5) |
| Nicaragua | Middle SDI | 5·4 (3·9 to 7·2) | 12·6 (10·0 to 15·7) | −0·6 (−2·4 to 1·1) | −0·9 (−2·1 to 0·4) | −1·0 (−3·6 to 1·6) | −1·3 (−3·1 to 0·6) | −0·2 (−3·9 to 3·4) | −0·3 (−2·8 to 2·5) |
| Niger | Low SDI | 0·7 (0·4 to 1·0) | 8·0 (6·6 to 9·5) | −1·9 (−4·4 to 0·6) | 0·7 (−0·5 to 1·7) | −1·8 (−5·5 to 1·8) | 0·2 (−1·3 to 2·0) | −1·9 (−6·5 to 2·9) | 1·3 (−1·0 to 3·6) |
| Nigeria | Low-middle SDI | 1·3 (0·9 to 1·9) | 5·5 (4·6 to 6·7) | −4·4 (−6·3 to −2·4) | −3·2 (−4·1 to −2·4) | −7·1 (−10·2 to −3·9) | −3·9 (−5·2 to −2·7) | −0·3 (−4·9 to 4·4) | −2·1 (−4·3 to 0·1) |
| North Korea | Middle SDI | 0·9 (0·6 to 1·4) | 36·7 (33·6 to 39·8) | −0·8 (−3·4 to 1·9) | −0·7 (−1·2 to −0·3) | −0·6 (−4·9 to 3·9) | −0·5 (−1·1 to 0·1) | −1·0 (−7·0 to 5·1) | −1·1 (−2·1 to −0·1) |
| Northern Mariana Islands | High SDI | 25·1 (21·1 to 29·6) | 45·9 (41·7 to 50·1) | −0·2 (−1·1 to 0·7) | −0·3 (−0·7 to 0·2) | −0·1 (−1·6 to 1·3) | −0·2 (−0·9 to 0·5) | −0·3 (−2·1 to 1·5) | −0·4 (−1·4 to 0·7) |
| Norway | High SDI | 14·8 (13·1 to 16·7) | 15·0 (13·3 to 16·7) | −2·6 (−3·2 to −2·0) | −2·8 (−3·3 to −2·2) | −2·7 (−3·7 to −1·9) | −2·5 (−3·4 to −1·7) | −2·4 (−3·9 to −0·8) | −3·1 (−4·5 to −1·8) |
| Oman | High-middle SDI | 1·5 (1·0 to 2·1) | 9·5 (8·0 to 11·4) | 0·6 (−1·6 to 2·9) | −1·4 (−2·4 to −0·5) | 1·6 (−1·4 to 4·6) | −2·2 (−3·5 to −0·9) | −0·9 (−5·3 to 3·5) | −0·2 (−2·2 to 1·8) |
| Pakistan | Low-middle SDI | 4·3 (3·4 to 5·5) | 16·9 (14·9 to 19·2) | −0·4 (−2·3 to 1·6) | −2·0 (−2·8 to −1·1) | −0·7 (−3·9 to 2·9) | −1·1 (−2·3 to 0·3) | 0·1 (−3·4 to 3·8) | −3·3 (−5·0 to −1·7) |
| Palestine | Middle SDI | 2·5 (1·7 to 3·5) | 30·4 (27·2 to 34·0) | −0·8 (−2·9 to 1·2) | −0·4 (−1·0 to 0·2) | −1·0 (−4·2 to 2·2) | −0·2 (−0·9 to 0·6) | −0·6 (−5·5 to 3·8) | −0·7 (−1·9 to 0·5) |
| Panama | High-middle SDI | 2·4 (1·9 to 3·0) | 4·6 (3·8 to 5·5) | −2·1 (−3·5 to −0·6) | −4·1 (−5·3 to −2·9) | −1·1 (−3·7 to 1·5) | −2·6 (−4·5 to −0·6) | −3·7 (−7·1 to −0·1) | −6·3 (−8·9 to −3·6) |
| Papua New Guinea | Low-middle SDI | 15·0 (12·6 to 17·7) | 37·6 (33·8 to 41·5) | −0·2 (−1·2 to 0·9) | −0·5 (−1·0 to 0·1) | 1·2 (−0·2 to 2·6) | 0·1 (−0·7 to 0·9) | −2·2 (−4·2 to −0·2) | −1·2 (−2·4 to −0·1) |
| Paraguay | Middle SDI | 7·7 (5·8 to 10·2) | 12·5 (10·1 to 15·5) | −0·4 (−2·3 to 1·3) | −2·1 (−3·3 to −1·0) | −1·3 (−3·9 to 1·6) | −1·6 (−3·2 to 0·2) | 0·9 (−2·7 to 4·4) | −2·9 (−5·6 to −0·5) |
| Peru | High-middle SDI | 4·2 (3·5 to 5·0) | 11·9 (9·5 to 14·6) | −0·5 (−1·7 to 0·7) | −1·3 (−2·4 to −0·1) | −0·2 (−1·8 to 1·6) | −0·9 (−2·9 to 1·0) | −1·0 (−3·2 to 1·4) | −1·8 (−4·4 to 0·5) |
| Philippines | Middle SDI | 7·4 (5·6 to 9·7) | 34·5 (31·1 to 38·0) | −0·8 (−2·5 to 0·9) | −0·4 (−1·0 to 0·2) | −1·0 (−3·4 to 1·5) | −0·2 (−0·9 to 0·6) | −0·6 (−3·7 to 2·6) | −0·8 (−2·0 to 0·3) |
| Poland | High SDI | 19·3 (16·7 to 22·1) | 26·7 (24·6 to 28·8) | −0·9 (−1·6 to −0·3) | −1·7 (−2·1 to −1·3) | −0·9 (−1·7 to 0·0) | −1·8 (−2·3 to −1·3) | −0·9 (−2·7 to 0·9) | −1·5 (−2·5 to −0·4) |
| Portugal | High-middle SDI | 12·7 (11·0 to 14·8) | 24·9 (22·7 to 27·2) | 1·3 (0·4 to 2·1) | −1·0 (−1·4 to −0·6) | 2·1 (0·9 to 3·3) | −1·2 (−1·8 to −0·6) | 0·0 (−1·8 to 1·8) | −0·7 (−1·7 to 0·3) |
| Puerto Rico | High SDI | 5·7 (4·4 to 7·4) | 12·1 (10·1 to 14·5) | −0·3 (−1·8 to 1·2) | −0·4 (−1·5 to 0·8) | −0·1 (−2·6 to 2·7) | −0·2 (−2·0 to 1·6) | −0·7 (−4·3 to 2·9) | −0·5 (−3·1 to 2·0) |
| Qatar | High-middle SDI | 2·3 (1·7 to 3·1) | 12·2 (10·4 to 14·0) | −3·2 (−5·2 to −1·4) | −0·1 (−1·1 to 0·8) | −6·0 (−9·8 to −2·6) | −1·6 (−3·1 to 0·1) | 1·0 (−3·7 to 5·8) | 2·0 (−0·2 to 4·2) |
| Romania | High-middle SDI | 15·7 (13·3 to 18·4) | 29·3 (26·9 to 31·9) | 0·0 (−0·9 to 1·1) | −0·1 (−0·5 to 0·5) | 0·8 (−0·4 to 2·1) | 0·9 (0·3 to 1·7) | −1·1 (−3·1 to 1·1) | −1·6 (−2·6 to −0·6) |
| Russia | High SDI | 12·3 (10·6 to 14·2) | 38·2 (36·0 to 40·3) | 1·8 (0·9 to 2·7) | −0·5 (−0·8 to −0·2) | 3·2 (2·0 to 4·4) | 0·2 (−0·2 to 0·6) | −0·3 (−2·0 to 1·5) | −1·5 (−2·1 to −0·9) |
| Rwanda | Low SDI | 3·8 (3·2 to 4·6) | 12·4 (10·6 to 14·3) | 0·1 (−1·0 to 1·3) | −1·2 (−2·2 to −0·3) | −0·3 (−2·2 to 1·5) | −1·3 (−2·8 to 0·2) | 0·6 (−1·8 to 3·0) | −1·1 (−3·1 to 0·9) |
| Saint Lucia | High-middle SDI | 1·8 (1·3 to 2·4) | 14·3 (11·5 to 17·7) | 0·0 (−2·0 to 1·8) | 0·6 (−0·6 to 1·9) | 0·4 (−2·6 to 3·2) | 1·5 (−0·5 to 3·5) | −0·7 (−4·8 to 3·2) | −0·7 (−3·4 to 1·8) |
| Saint Vincent and the Grenadines | High-middle SDI | 1·8 (1·3 to 2·5) | 10·8 (8·6 to 13·3) | −0·8 (−2·5 to 0·9) | −1·6 (−2·8 to −0·5) | −0·7 (−3·6 to 2·2) | −2·1 (−4·2 to −0·2) | −1·0 (−5·0 to 3·0) | −0·9 (−3·6 to 1·8) |
| Samoa | Middle SDI | 11·9 (9·7 to 14·4) | 34·8 (30·8 to 38·9) | −0·6 (−1·7 to 0·5) | −1·0 (−1·6 to −0·4) | −0·5 (−2·1 to 1·2) | −1·1 (−1·8 to −0·3) | −0·8 (−3·1 to 1·4) | −0·9 (−2·2 to 0·3) |
| São Tomé and Príncipe | Low-middle SDI | 1·0 (0·7 to 1·5) | 6·2 (5·0 to 7·3) | −1·0 (−3·2 to 1·3) | −0·2 (−1·3 to 0·9) | −1·4 (−5·0 to 2·1) | −0·5 (−2·2 to 1·1) | −0·2 (−5·0 to 4·6) | 0·2 (−2·1 to 2·5) |
| Saudi Arabia | High-middle SDI | 1·7 (1·4 to 2·0) | 19·5 (18·5 to 20·6) | −2·9 (−4·0 to −1·9) | 2·4 (2·1 to 2·8) | −4·9 (−6·5 to −3·2) | 3·6 (2·9 to 4·2) | 0·0 (−2·2 to 2·2) | 0·7 (0·0 to 1·6) |
| Senegal | Low SDI | 1·5 (1·1 to 1·9) | 8·3 (7·2 to 9·6) | 1·1 (−0·8 to 3·0) | −3·0 (−3·9 to −2·1) | −0·9 (−4·3 to 2·7) | −2·4 (−3·8 to −0·9) | 4·1 (−0·1 to 8·3) | −3·9 (−5·8 to −2·0) |
| Serbia | High-middle SDI | 18·9 (15·6 to 22·4) | 28·7 (25·9 to 31·6) | 0·2 (−0·8 to 1·2) | 0·1 (−0·5 to 0·7) | 1·3 (−0·1 to 2·8) | 1·1 (0·4 to 1·8) | −1·5 (−3·5 to 0·3) | −1·5 (−2·6 to −0·5) |
| Seychelles | High-middle SDI | 4·2 (2·8 to 5·9) | 23·7 (20·7 to 26·7) | 0·6 (−1·7 to 2·7) | −0·2 (−1·0 to 0·5) | 0·0 (−3·3 to 3·3) | −0·3 (−1·4 to 0·9) | 1·4 (−3·2 to 5·6) | −0·2 (−1·6 to 1·2) |
| Sierra Leone | Low SDI | 3·8 (2·7 to 5·2) | 21·7 (19·4 to 24·3) | −0·9 (−3·0 to 1·2) | −0·5 (−1·3 to 0·2) | −0·4 (−3·5 to 2·7) | 0·0 (−1·1 to 1·2) | −1·7 (−5·9 to 2·8) | −1·3 (−2·8 to 0·3) |
| Singapore | High SDI | 6·3 (5·3 to 7·4) | 17·9 (16·2 to 19·4) | 0·3 (−0·6 to 1·2) | −0·9 (−1·4 to −0·4) | −0·4 (−1·7 to 0·9) | −1·6 (−2·3 to −0·9) | 1·3 (−0·5 to 3·0) | 0·2 (−0·8 to 1·1) |
| Slovakia | High SDI | 15·1 (12·5 to 18·0) | 25·6 (23·1 to 28·1) | −0·2 (−1·3 to 1·0) | −1·4 (−2·0 to −0·9) | −0·5 (−2·2 to 1·4) | −2·0 (−2·8 to −1·1) | 0·3 (−2·1 to 2·5) | −0·5 (−1·7 to 0·6) |
| Slovenia | High SDI | 18·5 (15·8 to 21·6) | 23·1 (20·8 to 25·5) | −0·4 (−1·4 to 0·6) | −1·7 (−2·3 to −1·2) | −0·7 (−2·2 to 0·8) | −2·7 (−3·4 to −2·0) | 0·0 (−1·8 to 1·9) | −0·3 (−1·6 to 0·9) |
| Solomon Islands | Low-middle SDI | 9·7 (7·9 to 11·8) | 28·5 (24·8 to 32·3) | −0·5 (−1·7 to 0·6) | −0·4 (−1·1 to 0·4) | −0·2 (−1·9 to 1·6) | −0·2 (−1·3 to 0·9) | −1·0 (−3·3 to 1·4) | −0·6 (−2·0 to 0·8) |
| Somalia | Low SDI | 1·6 (1·3 to 2·0) | 13·1 (10·7 to 16·0) | −2·1 (−3·3 to −0·9) | −1·1 (−2·2 to 0·0) | −2·6 (−4·5 to −0·6) | −1·2 (−2·9 to 0·5) | −1·3 (−3·9 to 1·2) | −0·9 (−3·2 to 1·6) |
| South Africa | Middle SDI | 7·5 (7·0 to 8·1) | 21·9 (21·2 to 22·7) | −2·9 (−3·4 to −2·4) | −1·9 (−2·1 to −1·7) | −4·1 (−4·9 to −3·3) | −2·8 (−3·1 to −2·5) | −1·0 (−2·1 to 0·1) | −0·6 (−1·0 to −0·1) |
| South Korea | High SDI | 8·8 (7·6 to 10·1) | 33·5 (31·6 to 35·5) | 2·4 (1·5 to 3·2) | −2·3 (−2·6 to −2·1) | 3·6 (2·3 to 4·8) | −2·8 (−3·1 to −2·4) | 0·6 (−1·3 to 2·3) | −1·6 (−2·4 to −1·0) |
| South Sudan | Low SDI | 1·7 (1·3 to 2·0) | 13·3 (10·9 to 16·0) | −2·1 (−3·2 to −0·9) | −1·0 (−2·1 to 0·0) | −2·5 (−4·4 to −0·7) | −1·1 (−2·7 to 0·6) | −1·4 (−3·6 to 1·0) | −1·0 (−3·4 to 1·4) |
| Spain | High-middle SDI | 18·6 (16·4 to 20·7) | 25·6 (23·3 to 27·8) | −1·1 (−1·6 to −0·6) | −1·7 (−2·1 to −1·3) | −0·6 (−1·2 to 0·2) | −1·5 (−1·9 to −1·0) | −1·9 (−3·3 to −0·6) | −2·0 (−3·1 to −1·0) |
| Sri Lanka | High-middle SDI | 1·2 (0·8 to 1·7) | 19·2 (16·8 to 21·5) | −3·6 (−5·8 to −1·5) | −0·6 (−1·4 to 0·1) | −5·9 (−9·1 to −2·7) | −1·0 (−1·9 to 0·1) | −0·2 (−4·3 to 4·1) | −0·1 (−1·6 to 1·2) |
| Sudan | Low-middle SDI | 0·4 (0·2 to 0·6) | 1·3 (1·0 to 1·7) | 1·0 (−2·0 to 4·4) | −0·5 (−2·1 to 1·0) | 0·4 (−4·7 to 5·7) | −1·1 (−3·4 to 1·3) | 1·9 (−4·8 to 8·8) | 0·3 (−2·7 to 3·6) |
| Suriname | High-middle SDI | 7·5 (5·5 to 9·9) | 27·3 (24·5 to 30·2) | 0·4 (−1·2 to 2·1) | 1·2 (0·3 to 2·2) | 0·7 (−1·9 to 3·0) | 0·8 (−0·7 to 2·5) | −0·1 (−3·7 to 3·6) | 1·8 (−0·1 to 3·8) |
| Swaziland | Middle SDI | 1·3 (1·0 to 1·7) | 10·2 (9·0 to 11·4) | −3·1 (−4·6 to −1·6) | −2·2 (−2·9 to −1·5) | −2·7 (−5·2 to −0·6) | −3·3 (−4·4 to −2·4) | −3·7 (−7·0 to −0·5) | −0·6 (−1·9 to 0·9) |
| Sweden | High SDI | 11·4 (10·6 to 12·1) | 10·3 (9·7 to 11·0) | −2·7 (−3·2 to −2·2) | −3·2 (−3·6 to −2·8) | −2·5 (−3·1 to −1·8) | −4·4 (−5·0 to −3·8) | −3·1 (−3·9 to −2·3) | −1·4 (−2·1 to −0·6) |
| Switzerland | High SDI | 16·5 (14·6 to 18·7) | 21·9 (19·6 to 24·1) | −1·4 (−2·0 to −0·9) | −1·3 (−1·8 to −0·9) | −1·2 (−1·9 to −0·5) | −1·0 (−1·7 to −0·5) | −1·8 (−3·3 to −0·4) | −1·6 (−2·9 to −0·4) |
| Syria | Middle SDI | 8·5 (5·9 to 11·6) | 21·0 (18·0 to 24·2) | −1·2 (−3·1 to 0·6) | −0·8 (−1·6 to 0·1) | −1·1 (−4·0 to 1·9) | −0·6 (−1·9 to 0·7) | −1·4 (−5·5 to 2·5) | −1·0 (−2·6 to 0·6) |
| Taiwan | High SDI | 3·4 (2·2 to 5·2) | 19·0 (16·8 to 21·0) | −1·1 (−3·5 to 1·3) | −3·0 (−3·5 to −2·4) | −1·4 (−5·1 to 2·5) | −2·0 (−2·8 to −1·3) | −0·7 (−5·6 to 3·8) | −4·3 (−5·7 to −3·2) |
| Tajikistan | Middle SDI | 0·4 (0·3 to 0·6) | 19·6 (16·8 to 22·7) | −2·9 (−4·7 to −1·0) | −2·8 (−3·6 to −2·2) | −4·1 (−7·0 to −1·3) | −4·2 (−5·2 to −3·1) | −1·0 (−4·9 to 2·9) | −0·9 (−2·6 to 0·9) |
| Tanzania | Low-middle SDI | 1·4 (1·2 to 1·8) | 16·0 (13·9 to 18·4) | −0·7 (−1·9 to 0·5) | −0·5 (−1·4 to 0·4) | −1·0 (−3·0 to 1·0) | −0·3 (−1·6 to 1·3) | −0·4 (−3·0 to 2·4) | −0·9 (−2·7 to 0·9) |
| Thailand | High-middle SDI | 3·3 (2·3 to 4·6) | 30·9 (28·0 to 34·1) | −1·6 (−3·6 to 0·4) | −1·3 (−1·7 to −0·9) | −2·7 (−5·6 to 0·3) | −1·9 (−2·4 to −1·3) | −0·1 (−4·3 to 3·9) | −0·5 (−1·6 to 0·6) |
| The Bahamas | High SDI | 3·7 (2·7 to 5·1) | 8·0 (6·3 to 10·1) | 3·0 (1·2 to 4·8) | 2·0 (0·5 to 3·3) | 2·7 (−0·1 to 5·6) | 1·4 (−1·0 to 3·7) | 3·3 (−0·6 to 7·1) | 2·8 (−0·1 to 5·6) |
| The Gambia | Low SDI | 0·8 (0·5 to 1·2) | 19·3 (16·7 to 21·9) | −1·6 (−3·8 to 0·6) | −0·8 (−1·5 to 0·1) | −2·0 (−5·6 to 1·5) | −0·7 (−2·0 to 0·6) | −1·0 (−5·8 to 3·9) | −0·8 (−2·7 to 1·1) |
| Timor-Leste | Low-middle SDI | 12·4 (9·8 to 15·1) | 39·8 (37·2 to 42·5) | 4·5 (2·8 to 6·3) | −0·1 (−0·5 to 0·4) | 3·7 (0·3 to 7·0) | 0·2 (−0·5 to 0·9) | 5·8 (2·3 to 9·5) | −0·4 (−1·2 to 0·6) |
| Togo | Low SDI | 1·1 (0·7 to 1·6) | 9·2 (7·9 to 10·7) | −2·3 (−4·5 to 0·0) | −0·2 (−1·1 to 0·7) | −2·3 (−5·8 to 1·0) | 0·0 (−1·6 to 1·5) | −2·4 (−7·2 to 2·9) | −0·5 (−2·6 to 1·7) |
| Tonga | Middle SDI | 11·0 (9·2 to 12·9) | 38·3 (35·2 to 41·8) | −1·2 (−2·2 to −0·3) | 0·1 (−0·4 to 0·6) | −2·1 (−3·5 to −0·9) | 0·2 (−0·4 to 0·9) | 0·1 (−1·7 to 2·0) | −0·2 (−1·2 to 0·8) |
| Trinidad and Tobago | High SDI | 5·1 (3·8 to 6·5) | 22·3 (19·0 to 25·8) | 1·3 (−0·4 to 3·1) | −0·5 (−1·4 to 0·4) | 1·4 (−1·7 to 4·5) | −0·8 (−2·2 to 0·7) | 1·2 (−2·7 to 4·9) | −0·1 (−2·1 to 1·8) |
| Tunisia | Middle SDI | 3·0 (2·0 to 4·2) | 36·1 (32·0 to 40·4) | −2·4 (−4·5 to −0·4) | −0·5 (−1·1 to 0·1) | −3·9 (−6·7 to −1·0) | −0·2 (−1·1 to 0·6) | −0·1 (−4·1 to 3·8) | −0·9 (−2·1 to 0·4) |
| Turkey | High-middle SDI | 13·7 (11·0 to 16·7) | 31·2 (28·6 to 33·9) | 0·1 (−1·0 to 1·5) | −1·9 (−2·3 to −1·4) | 0·3 (−1·4 to 2·3) | −1·4 (−2·0 to −0·8) | −0·3 (−2·6 to 2·1) | −2·6 (−3·6 to −1·6) |
| Turkmenistan | High-middle SDI | 0·9 (0·7 to 1·3) | 13·3 (11·4 to 15·5) | −0·6 (−2·4 to 1·3) | −1·2 (−2·1 to −0·3) | −0·8 (−3·8 to 2·0) | −1·5 (−3·0 to −0·1) | −0·2 (−4·0 to 3·9) | −0·8 (−2·8 to 1·0) |
| Uganda | Low SDI | 2·6 (2·2 to 3·1) | 9·3 (8·0 to 10·8) | −0·1 (−1·2 to 1·1) | −2·2 (−3·2 to −1·1) | −0·9 (−2·8 to 0·9) | −1·5 (−3·2 to 0·2) | 1·2 (−1·3 to 3·7) | −3·2 (−5·5 to −1·1) |
| Ukraine | High-middle SDI | 11·5 (9·4 to 13·7) | 40·6 (37·8 to 43·4) | 0·2 (−1·0 to 1·3) | −0·8 (−1·2 to −0·5) | 0·7 (−1·0 to 2·4) | −0·2 (−0·6 to 0·3) | −0·7 (−2·8 to 1·4) | −1·8 (−2·5 to −1·1) |
| United Arab Emirates | High SDI | 1·8 (1·2 to 2·6) | 11·3 (9·3 to 13·4) | −2·3 (−4·5 to −0·2) | −0·8 (−1·8 to 0·2) | −4·0 (−7·3 to −0·6) | −0·3 (−1·8 to 1·1) | 0·1 (−4·5 to 4·8) | −1·6 (−3·7 to 0·5) |
| UK | High SDI | 18·1 (16·4 to 20·0) | 19·9 (18·1 to 21·7) | −1·4 (−2·0 to −0·8) | −1·4 (−1·9 to −1·0) | −1·6 (−2·3 to −0·8) | −1·8 (−2·4 to −1·1) | −1·2 (−2·3 to −0·1) | −0·9 (−2·0 to 0·1) |
| USA | High SDI | 11·7 (11·5 to 12·0) | 14·4 (14·0 to 14·7) | −2·2 (−2·3 to −2·1) | −2·0 (−2·1 to −1·8) | −2·4 (−2·5 to −2·3) | −1·7 (−1·8 to −1·6) | −2·0 (−2·2 to −1·8) | −2·4 (−2·6 to −2·1) |
| Uruguay | High-middle SDI | 17·0 (14·8 to 19·3) | 21·3 (18·8 to 24·0) | −1·0 (−1·7 to −0·3) | −2·0 (−2·6 to −1·4) | −0·4 (−1·4 to 0·6) | −1·9 (−2·6 to −1·1) | −1·8 (−3·4 to −0·3) | −2·3 (−3·6 to −1·0) |
| Uzbekistan | High-middle SDI | 3·3 (2·5 to 4·2) | 14·1 (12·4 to 16·0) | 2·4 (0·9 to 4·1) | −0·6 (−1·4 to 0·3) | 3·6 (1·0 to 6·2) | 0·3 (−1·0 to 1·6) | 0·6 (−2·5 to 3·8) | −1·9 (−3·6 to −0·2) |
| Vanuatu | Low-middle SDI | 2·8 (2·2 to 3·4) | 28·5 (25·5 to 31·7) | −1·8 (−3·0 to −0·5) | −0·7 (−1·3 to −0·1) | −2·9 (−4·8 to −1·0) | −2·1 (−3·2 to −1·1) | −0·2 (−3·0 to 2·5) | 1·4 (0·0 to 2·9) |
| Venezuela | High-middle SDI | 9·9 (7·5 to 12·7) | 16·7 (13·8 to 20·0) | −0·6 (−2·1 to 0·9) | −0·7 (−1·7 to 0·4) | −0·2 (−2·7 to 2·2) | −0·5 (−2·2 to 1·2) | −1·1 (−4·5 to 2·1) | −0·9 (−3·2 to 1·5) |
| Vietnam | Middle SDI | 1·4 (1·0 to 1·9) | 35·4 (32·1 to 38·7) | −4·4 (−6·1 to −2·7) | −1·5 (−1·9 to −1·0) | −7·5 (−9·6 to −5·2) | −1·8 (−2·3 to −1·2) | 0·3 (−3·7 to 4·2) | −1·0 (−2·1 to 0·0) |
| Virgin Islands, USA | High SDI | 2·8 (2·1 to 3·8) | 4·4 (3·4 to 5·6) | −1·2 (−2·9 to 0·6) | −1·2 (−2·7 to 0·2) | −1·0 (−3·9 to 1·8) | −1·0 (−3·2 to 1·2) | −1·4 (−5·0 to 2·1) | −1·5 (−4·7 to 1·5) |
| Yemen | Low-middle SDI | 6·3 (4·3 to 8·8) | 18·8 (16·1 to 21·8) | −0·9 (−3·1 to 1·1) | −0·7 (−1·6 to 0·2) | −1·0 (−3·7 to 2·0) | −0·3 (−1·4 to 0·9) | −0·8 (−4·8 to 3·2) | −1·4 (−3·0 to 0·2) |
| Zambia | Low-middle SDI | 3·1 (2·5 to 3·8) | 15·2 (12·3 to 18·1) | −0·5 (−1·7 to 0·7) | −0·7 (−1·8 to 0·2) | −0·4 (−2·1 to 1·5) | −0·7 (−2·1 to 0·7) | −0·8 (−3·3 to 1·8) | −0·8 (−2·8 to 1·1) |
| Zimbabwe | Low-middle SDI | 1·4 (1·0 to 1·9) | 20·8 (18·9 to 22·7) | −2·8 (−4·6 to −1·1) | −0·3 (−0·8 to 0·3) | −1·5 (−4·1 to 1·0) | −0·5 (−1·4 to 0·3) | −4·9 (−8·3 to −1·6) | 0·1 (−0·9 to 1·2) |
Data in parentheses are 95% uncertainty intervals. SDI=Socio-demographic Index.
Figure 1.
Age-standardised prevalence of daily smoking for men (A) and women (B), in 2015
ATG=Antigua and Barbuda. VCT=Saint Vincent and the Grenadines. LCA=Saint Lucia. TTO=Trinidad and Tobago. TLS=Timor-Leste. FSM=Federated States of Micronesia.
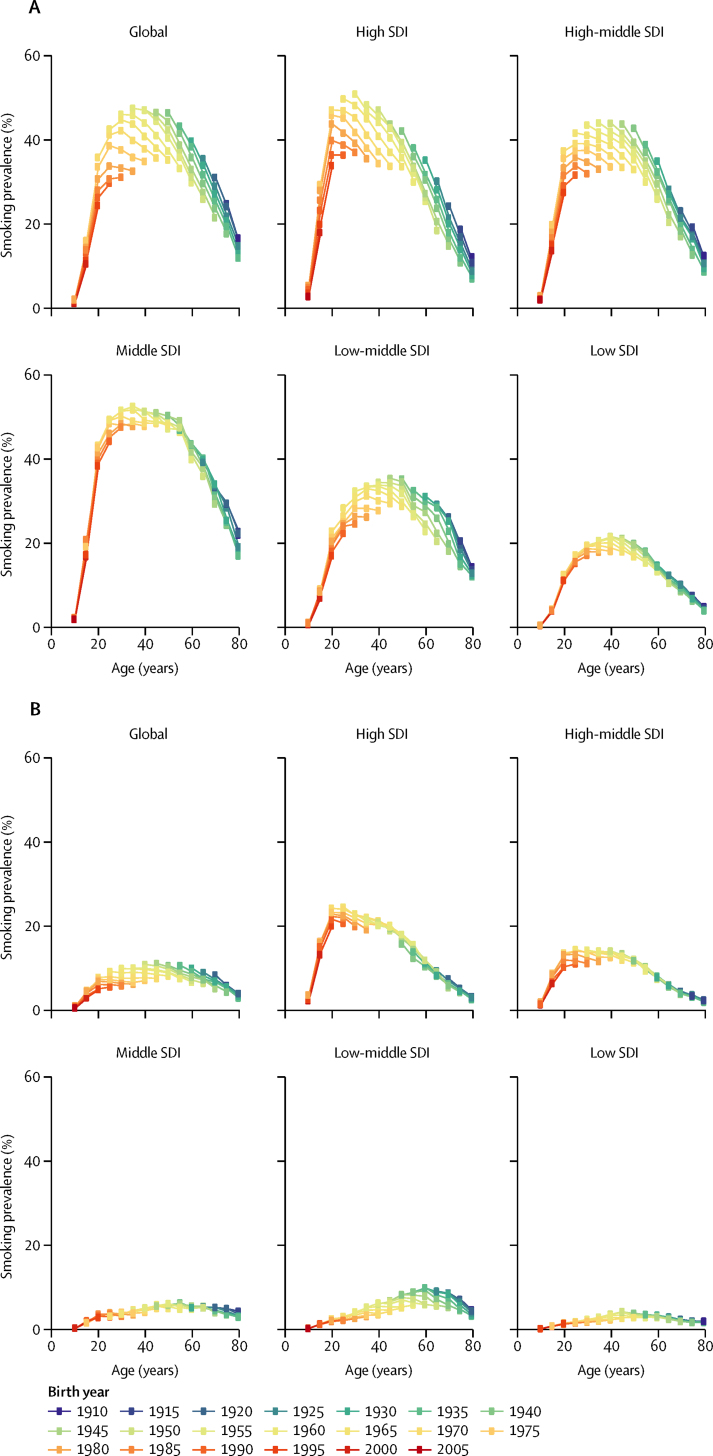
Figure 2.
Prevalence of daily smoking across birth cohorts over time, at the global level and by SDI quintile, for men (A) and women (B)
Birth cohorts are colour-coded by 5-year intervals, with the most recent birth cohort in red (2005) to the least recent birth cohort in dark blue (1910). Every dot represents the prevalence of daily smoking for a given birth cohort and age group. SDI=Socio-demographic Index.
Between 1990 and 2015, the global age-standardised prevalence of daily smoking fell significantly for both sexes, decreasing by 28·4% (95% UI 25·8–31·1) for men and 34·4% (29·4–38·6) for women (table 2). 13 countries (Australia, Brazil, China, Denmark, Dominican Republic, Iceland, Kenya, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the USA) recorded significant annualised rates of decline both between 1990 and 2005 and 2005 and 2015, suggesting sustained progress in tobacco control (table 1). 18 countries showed a faster annualised rate of reduction in daily smoking in the most recent decade compared with between 1990 and 2005. Focusing on the most recent decade, since 2005, 53 (27%) of 195 countries and territories recorded significant decreases in age-standardised prevalence of male daily smoking, whereas only 32 (16%) recorded significant reductions for women.
Table 2.
Size of the smoking population, prevalence, and 1990–2015 percent change in prevalence, by sex, for the ten countries with the largest smoking populations and worldwide
| Overall rank | Ages 15–19 rank | 2015 female smoking population (millions) | 2015 male smoking population (millions) | 2015 female age-standardised prevalence | 2015 male age-standardised prevalence | 2015 female prevalence ages 15–19 | 2015 male prevalence ages 15–19 | Female age-standardised percent change 1990–2015 | Male age-standardised percent change 1990–2015 | Female ages 15–19 percent change 1990–2015 | Male ages 15–19 percent change 1990–2015 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| China | 1 | 1 | 14·4 (10·5 to 19·5) | 253·9 (241·2 to 266·6) | 2·2 (2·1 to 2·4) | 37·5 (36·9 to 38·0) | 1·0 (0·7 to 1·4) | 17·9 (16·4 to 19·6) | −48·4 (−55·1 to −41·2) | −22·4 (−24·0 to −20·7) | −9·7 (−47·0 to 49·6) | −3·6 (−15·4 to 10·1) |
| India | 2 | 2 | 13·5 (9·4 to 19·7) | 90·8 (78·9 to 104·3) | 2·9 (2·6 to 3·2) | 17·5 (16·8 to 18·2) | 1·4 (1·0 to 2·0) | 6·0 (5·1 to 7·0) | −7·1 (−22·3 to 9·1) | −40·6 (−44·3 to −36·6) | 56·1 (−9·8 to 175·7) | −17·1 (−35·2 to 8·0) |
| Indonesia | 3 | 3 | 3·9 (1·1 to 9·8) | 49·8 (38·9 to 60·5) | 3·8 (2·7 to 5·1) | 46·7 (43·9 to 49·5) | 2·3 (0·6 to 6·1) | 27·7 (18·4 to 38·3) | 57·7 (0·8 to 154·2) | 6·3 (−3·4 to 17·0) | 139·6 (−51·4 to 1468·0) | 9·1 (−36·1 to 85·0) |
| USA | 4 | 4 | 17·2 (16·0 to 18·4) | 20·4 (18·9 to 22·0) | 11·7 (11·5 to 12·0) | 14·4 (14·0 to 14·7) | 7·0 (6·4 to 7·6) | 7·7 (7·1 to 8·4) | −43·0 (−44·3 to −41·6) | −38·6 (−40·3 to −37·0) | −62·7 (−66·1 to −58·6) | −59·7 (−63·8 to −55·1) |
| Russia | 5 | 9 | 8·3 (5·0 to 12·6) | 24·9 (20·3 to 29·6) | 12·3 (10·6 to 14·2) | 38·2 (36·0 to 40·3) | 11·8 (6·6 to 19·5) | 22·4 (16·4 to 30·0) | 56·2 (25·1 to 96·3) | −11·2 (−17·3 to −4·8) | 38·0 (−40·3 to 224·9) | −30·6 (−51·7 to −3·6) |
| Bangladesh | 6 | 6 | 1·0 (0·2 to 3·0) | 24·1 (15·3 to 33·6) | 1·8 (1·1 to 2·6) | 38·0 (34·1 to 42·6) | 0·9 (0·1 to 2·7) | 14·9 (7·1 to 26·2) | −51·4 (−72·6 to −10·6) | 6·8 (−9·9 to 27·4) | −37·9 (−91·1 to 390·2) | −7·6 (−63·6 to 148·3) |
| Japan | 7 | 16 | 4·9 (4·4 to 5·6) | 15·3 (14·4 to 16·3) | 9·3 (8·9 to 9·6) | 26·7 (26·1 to 27·1) | 6·7 (5·9 to 7·5) | 11·5 (10·7 to 12·4) | −16·0 (−20·2 to −11·6) | −44·8 (−46·0 to −43·5) | −15·1 (−27·8 to 1·3) | −62·0 (−65·4 to −58·0) |
| Brazil | 8 | 8 | 7·7 (5·7 to 10·2) | 11·1 (8·9 to 13·9) | 8·2 (7·5 to 9·0) | 12·6 (11·8 to 13·5) | 4·8 (3·3 to 7·0) | 7·4 (5·6 to 9·6) | −55·8 (−61·9 to −48·7) | −56·5 (−61·1 to −51·9) | −67·3 (−81·4 to −42·8) | −60·8 (−74·0 to −40·4) |
| Germany | 9 | 13 | 7·1 (4·8 to 9·9) | 9·2 (6·6 to 12·1) | 19·4 (17·3 to 21·7) | 25·2 (22·8 to 27·4) | 15·9 (10·1 to 23·4) | 18·8 (12·6 to 26·6) | −7·8 (−19·2 to 6·2) | −20·6 (−28·9 to −12·2) | −22·6 (−54·6 to 27·6) | −23·7 (−51·5 to 16·7) |
| Philippines | 10 | 10 | 2·6 (0·9 to 5·8) | 13·2 (9·1 to 17·7) | 7·4 (5·6 to 9·7) | 34·5 (31·1 to 38·0) | 2·5 (0·7 to 6·4) | 16·0 (9·1 to 25·5) | −18·2 (−46·6 to 24·1) | −10·1 (−22·0 to 5·0) | −11·3 (−83·9 to 387·4) | −3·2 (−55·0 to 112·4) |
| Global | 165·0 (141·2 to 202·1) | 768·1 (690·1 to 852·2) | 5·4 (5·2 to 5·7) | 25·0 (24·2 to 25·7) | 3·0 (2·6 to 3·7) | 10·6 (9·3 to 12·1) | −34·4 (−38·6 to −29·4) | −28·4 (−31·1 to −25·8) | −36·8 (−49·7 to −20·7) | −34·3 (−45·3 to −21·1) |
Age-standardised estimates and estimates for the 15–19 age group are reported. 95% uncertainty intervals are reported in parentheses. Overall rank is calculated based on the size of the smoking population, both sexes and all ages (10 years and older) combined. Ages 15–19 years rank is calculated based on the size of the smoking population aged 15–19 years, both sexes combined.
Countries with large smoking populations
In 2015, there were 933·1 million (95% UI 831·3–1054·3) daily smokers in the world, 82·3% of whom were men (768·1 million [690·1–852·2]). The ten countries with the largest number of smokers together accounted for 63·6% of the world's daily smokers. China, India, and Indonesia, the three leading countries in total number of male smokers, accounted for 51·4% of the world's male smokers in 2015. On the other hand, the USA, China, and India, which were the leading three countries in total number of female smokers, accounted for only 27·3% of the world's female smokers. Together, these results suggest that the tobacco epidemic is less geographically concentrated for women than for men.
Among the ten countries with the largest number of total smokers in 2015, seven recorded significant decreases in male smoking prevalence and five had significant decreases in female smoking prevalence since 1990 (table 2). Of these countries, Brazil recorded the largest overall reduction in prevalence for both male and female daily smoking, which dropped by 56·5% (51·9–61·1) and 55·8% (48·7–61·9), respectively, between 1990 and 2015. Indonesia, Bangladesh, and the Philippines did not have significant reductions in male prevalence of daily smoking since 1990, and the Philippines, Germany, and India had no significant decreases in smoking among women. All of the three countries with female age-standardised smoking prevalence less than 3·0% (China, India, and Bangladesh) succeeded in keeping smoking prevalence low in women. Notably, female prevalence of daily smoking significantly increased in Russia and Indonesia since 1990 (table 2).
Adolescents
Delving into the smoking patterns of adolescents can shed light on trends in smoking initiation.47 Between 1990 and 2015, the global prevalence of daily smoking for this age group significantly decreased for each sex, falling from 16·1% (95% UI 14·4–18·0) to 10·6% (9·3–12·1) for men and from 4·8% (4·3–5·6) to 3·0% (2·6–3·7) for women (table 2). Despite global decreases, several countries still had a high prevalence of smoking among individuals aged between 15 and 19 years. In 2015, there were 22 countries with female smoking prevalence in this age group higher than 15·0%, 18 of which were located in western or central Europe. Countries with high male smoking prevalence were much more dispersed. Of the 24 countries with male smoking prevalence higher than 20·0%, six were in eastern Europe, and the remainder were spread across ten other regions (appendix pp 13, 14). The rank of countries with the largest smoking populations for the 15–19 years age group was mostly consistent with the rank for all-age smoking populations (table 2).
Although no country had a significant increase for men or women in this age group since 2005, only three countries saw smoking prevalence in 15 to 19 year-olds significantly drop for both men and women since 2005 (New Zealand, Iceland, and the USA). Iceland had the largest significant decrease among men, decreasing from 14·8% (95% UI 11·7–18·5) in 2005 to 9·0% (5·6–13·3) in 2015. New Zealand had the largest significant decline among women, decreasing from 20·8% (18·1–23·8) in 2005 to 12·5% (10·1–15·5) in 2015 (available to view through GHDx).
Shifts in patterns of smoking across cohorts
Parsing out daily smoking prevalence by age group and birth cohort allows for a more fine-grained examination of smoking prevalence, age patterns, and temporal trends by level of development (figure 2). Male age patterns of smoking were fairly consistent across levels of SDI, with prevalence generally peaking between the ages of 25 and 35 years. For women, however, age patterns varied more by SDI; female smoking prevalence typically peaked around age 25 years for high and high-middle SDI countries, while prevalence generally increased until age 60 years in low to middle SDI countries. Across birth cohorts, smoking prevalence decreased by age group, sex, and SDI level. The most notable decreases were recorded in high and high-middle SDI countries for men, where sizeable reductions in smoking prevalence in 15 to 24 year-olds occurred across birth cohorts. Middle SDI countries, which have the highest levels of daily smoking among men, had minimal changes in prevalence across birth cohorts, suggesting far less progress in curbing smoking initiation or promoting cessation. For women, prevalence is consistently lower than in men; nevertheless, reductions in smoking prevalence across birth cohorts generally were smaller than those recorded for men.
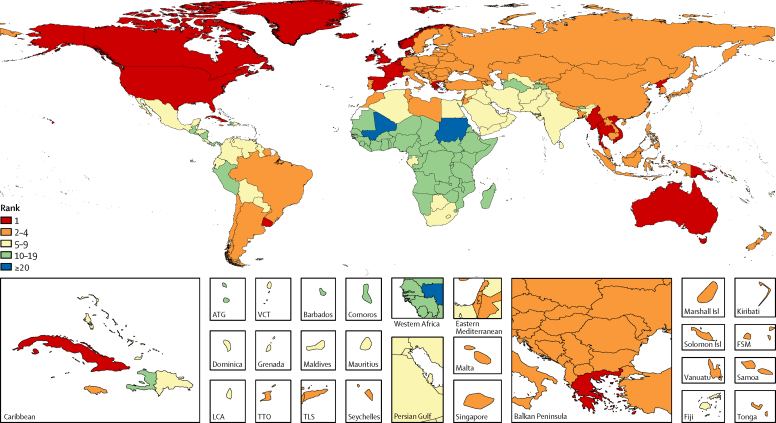
Deaths and disease burden attributable to smoking
In 2015, 6·4 million deaths (95% UI 5·7–7·0) were attributable to smoking worldwide, representing a 4·7% (1·2–8·5) increase in smoking-attributable deaths since 2005. More than 75% of these deaths were in men, and 52·2% took place in four countries (China, India, the USA, and Russia). Smoking was the second-leading risk factor for attributable mortality among both sexes in both 2005 and 2015, following high-systolic blood pressure.1 The relative ranking of smoking-attributable disease burden, as measured in DALYs, increased from third to second between 2005 and 2015. In 2015, there were 148·6 million (95% UI 134·2–163·1) smoking-attributable DALYs worldwide, and smoking was the leading risk factor for attributable disease burden in 24 countries, an increase from 16 countries in 1990 (figure 3). Further, smoking was ranked among the leading five risk factors for 109 countries in 2015. Between 2005 and 2015, only Egypt recorded a significant increase in the age-standardised smoking-attributable mortality rate among both sexes, increasing by 11·4% (95% UI 0·3–24·7) over that time period. On the other hand, 82 countries had significant decreases in their age-standardised smoking-attributable mortality rates since 2005.
Figure 3.
Rankings of smoking as a risk factor for all-cause, all-age attributable DALYs for both sexes combined in 2015
DALYs=disability-adjusted life-years. ATG=Antigua and Barbuda. VCT=Saint Vincent and the Grenadines. LCA=Saint Lucia. TTO=Trinidad and Tobago. TLS=Timor-Leste. FSM=Federated States of Micronesia.
Overall, in 2015, cardiovascular diseases (41·2%), cancers (27·6%), and chronic respiratory diseases (20·5%) were the three leading causes of smoking-attributable age-standardised DALYs for both sexes. Of all risk factors, smoking was the leading risk factor for cancers and chronic respiratory diseases, but only the ninth leading risk factor for cardiovascular diseases.1 The appendix shows the 30 leading causes of DALYs attributable to smoking, including changes over time (pp 19, 20). For women, the leading cause of smoking-attributable DALYs was COPD, whereas the leading cause for men was ischaemic heart disease.
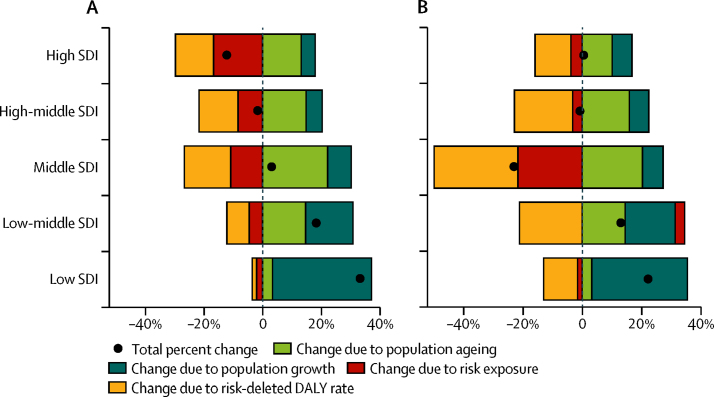
Decomposing changes in attributable burden due to smoking
Relative to changes in smoking exposure, the main drivers of overall changes in attributable burden due to smoking varied by both sex and SDI level (figure 4). Since 2005, all-cause DALYs attributable to smoking for men decreased by 11·8% (95% UI 10·0–13·9) in high-SDI countries, the only SDI level with a significant decrease in attributable burden for men. For women, only middle-SDI countries had a significant reduction in all-cause DALYs attributable to smoking (a 22·6% decrease [9·0–32·8]) between 2005 and 2015. In both instances, a combination of reduced smoking exposure and reduced risk-deleted DALY rates contributed to overall reductions. Conversely, all-cause burden due to smoking significantly increased in low SDI and low-middle SDI countries since 2005 for men. This rise in attributable DALYs was driven mainly by a combination of population growth and population ageing for both sexes. In women, while rising exposure to smoking has resulted in increased DALYs due to smoking for low-middle SDI countries, this increase was not significant. Generally, population growth was the leading factor for increasing attributable burden due to smoking among the low SDI countries between 2005 and 2015. For countries of middle to high SDI, more pronounced sex differences emerged. For instance, decreases in male smoking prevalence propelled an overall reduction in attributable burden for high SDI countries, whereas changes in smoking exposure had minimal effects on overall burden for women at similarly high levels of SDI.
Figure 4.
Decomposition of changes in all-cause DALYs attributable to smoking from 2005 to 2015, by SDI, for men (A) and women (B)
Changes due to population growth, population ageing, risk exposure (smoking prevalence), and the risk-deleted DALY rate are shown. Locations are reported in order of the number of attributable DALYs for both sexes in 2015. DALYs=disability-adjusted life-years. SDI=Socio-demographic Index.
A complete dataset of all results by geography, year, sex, and age group can be downloaded through GHDx, and an interactive data visualisation of smoking prevalence results can be found online.
Discussion
Despite more than half a century of unequivocal evidence of the harmful effects of tobacco on health,48, 49 in 2015, one in every four men in the world was a daily smoker. Prevalence has been, and remains, significantly lower in women—roughly one in every 20 women smoked daily in 2015. Nonetheless, much progress has been accomplished in the past 25 years. Specifically, the age-standardised global prevalence of daily smoking fell to 15·3% (95% UI 14·8–15·9), a 29·4% (27·1–31·8) reduction from 1990, with smoking rates decreasing from 34·9% (34·1–35·7) to 25·0% (24·2–25·7) in men and from 8·2% (7·9–8·6) to 5·4% (5·1–5·7) in women. These reductions were especially pronounced in high SDI countries and Latin America, probably reflecting concerted efforts to implement strong tobacco control policies and programmes in Brazil and Panama, among others.
Yet amid these gains, many countries with persistently high levels of daily smoking recorded marginal progress since 2005, and smoking remained among the leading risk factors for early death and disability in more than 100 countries in 2015, accounting for 11·5% of global deaths (95% UI 10·3–12·6) and 6·0% (5·3–6·8) of global DALYs. Smoking patterns diverged by geography, level of development, sex, and birth cohort, emphasising the need for tailored approaches to change smoking behaviours. Although male smoking prevalence still far exceeded that of female smokers in 2015, the most pronounced reductions in smoking prevalence since 1990 were generally found for men—and more places saw minimal changes or increases in smoking among women. These trends highlight how the tobacco epidemic, and corresponding industry forces, has expanded beyond a male-centred health challenge.
Low to middle SDI countries saw increased disease burden attributable to smoking since 2005, a trend that that occurred despite variable decreases in smoking prevalence and risk-deleted DALY rates. Population growth or ageing, or a combination of both, ultimately contributed to increased disease burden attributable to smoking in these countries. In higher SDI countries, population growth and ageing offset the potential for larger gains in places where notable declines in smoking prevalence and risk-deleted DALY rates occurred. This finding points to a crucial challenge ahead for tobacco control: unless progress in reducing current smoking and preventing initiation can be substantially accelerated, demographic forces, which are far less amenable to immediate intervention, are poised to heighten the disease burden associated with smoking's global toll.
Since 2005, the year when the FCTC entered into force, it has redefined global, regional, and national approaches to tobacco control and policy.50, 51 Case studies point to the successful uptake and enforcement of FCTC components in many countries with especially prominent reductions in smoking prevalence. Pakistan, Panama, and India stand out as three countries that have implemented a large number of tobacco control policies over the past decade and have had marked declines in the prevalence of daily smoking since 2005, compared with decreases recorded between 1990 and 2005.52, 53, 54 At the same time, many countries, including Australia, Brazil, Canada, South Korea, and the USA, among others, achieved sizeable declines in smoking prevalence well before FCTC adoption.15, 56, 57, 58 Altogether, 18 countries recorded a faster annualised rate of decline from 1990 to 2005 than from 2005 to 2015.
Brazil, which has achieved the third largest significant decline in age-standardised smoking prevalence since 1990, is a noteworthy success story. Brazil accomplished this reduction through a combination of tobacco control policies that began with advertising restrictions and smoking bans in some public places starting in 1996 and culminated with Brazil achieving the highest level of achievement in all MPOWER measures except for monitoring by 2011. Policies were comprehensive and were supplemented with fiscal interventions that included raising taxes and establishing minimum prices for tobacco products. Finally, Brazil has achieved high levels of compliance through enforcement.20, 59, 60, 61, 62
Critics of the FCTC argue that the treaty's effectiveness may be limited in various settings, especially since compliance has lagged in many countries.63, 64, 65 The FCTC, while necessary and vital for creating the policy environment for more effective tobacco control worldwide, is not sufficient to fully address each country's tobacco control needs. Rather, countries will need to both implement FCTC-stipulated measures and supplement such policies and programmes with strong enforcement and high rates of compliance. For example, India, where 11·2% of the world's smokers live, supplemented the Cigarettes and Other Tobacco Products Act (COTPA) with the creation of a National Tobacco Control Programme (NTCP) in 2007. NTCP was created to strengthen implementation and enforcement of the various provisions of COTPA at the state and district level. It has been rolled out in phases and currently covers about 40% of all districts in India.66
Despite concerted efforts to control tobacco around the world, there remain a number of countries where current levels and recent trends raise concern. For example, Indonesia, a country with very high levels of smoking, particularly among men, has not yet ratified the FCTC and scores very poorly on the MPOWER indicators.18 Also, in Russia, prevalence among women has been increasing, and, until recently, there were very few laws related to tobacco control.67 Russia passed a comprehensive tobacco control policy in 2014 and has the potential to achieve progress on tobacco control.68 As a region, eastern Europe has seen a statistically significant increase in smoking prevalence among women since 1990. Increases among women, along with a sustained high prevalence of male smokers, can be linked to tobacco industry targeting during the 1990s.6 The tobacco industry is now turning its focus toward emerging markets in sub-Saharan Africa, seeking to exploit the continent's patchwork tobacco control regulations and limited resources to combat industry marketing advances.69, 70 Given the large effects of population growth and ageing on smoking-attributable disease burden—and Africa's rapidly changing demographic profile—a renewed dedication to strong, proactive tobacco policies and monitoring will be vital for the continent.71
The 2030 agenda features tobacco control as a key component to sustainable development, with SDG Target 3.a calling for stronger FCTC implementation.24 Nonetheless, the utility and potential impact of the SDGs on tobacco control may be hindered by the vagueness of Target 3.a (“Strengthen the implementation of the WHO FCTC in all countries, as appropriate”) and absence of defined targets for reducing smoking prevalence by 2030. Ultimately, to move all countries toward stronger tobacco control by 2030, improvements in policy formulation, enforcement and compliance, and the routine monitoring of smoking behaviour are urgently needed. Without valid and reliable data, these efforts risk being more aspirational than grounded in evidence-informed action. Multi-country survey series have substantially improved data availability on smoking prevalence, yet the disadvantages associated with such surveys—high cost, time lags, inconsistent questions across survey series, sample restrictions for young populations, and a reliance on self-reported smoking behaviour—necessitate the development of robust, locally focused, timely, objective, and low-cost methods of tracking smoking trends. Supplementing surveys with biomarker collection is essential because self-reported smoking prevalence is believed to be severely underestimating true smoking prevalence,72, 73, 74, 75 especially in population subgroups or places where tobacco use may not be culturally acceptable.
Our findings should be interpreted taking into consideration the study's limitations. First, our exposure estimation focused on smoked tobacco and did not include smokeless tobacco products and e-cigarettes. Second, our definition of smoking exposure pertained to current daily smokers, and did not include occasional or former smokers, which might underestimate the attributable disease burden to smoking, especially in populations who tend to be less likely to smoke every day, such as women, children and young adults, and individuals with less disposable income. Third, we did not account for the intensity or duration of smoking. Fourth, the study relied on self-reported data, and it is possible that reporting biases varied across countries and over time. Fifth, for long-term effects of smoking on cancers and chronic respiratory diseases, we used the smoking impact ratio method, which estimates the lifetime cumulative effect of cigarette smoking using the proxy of recorded lung cancer mortality rates. This method provides robust estimates of the burden of cancers and chronic respiratory diseases related to tobacco but is not fully consistent with the GBD approach of estimating exposure independently of the outcomes affected by exposure. Also, the smoking impact ratio method is based on the cumulative effect of cigarette smoking rather than all types of tobacco smoking, and might be less robust for geographies in which non-smoker lung cancer might be significantly affected by air pollution or other factors. Sixth, our estimates of DALYs are probably underestimates because relative risk values used for estimating population attributable fractions might not fully represent all possible risk-outcome pairs experienced by sex, age group, and over time.76 Also, burden estimates did not account for the effect of both indoor and outdoor air pollution potentiating risks. Finally, minimal risk-outcome data were available for populations younger than 30 years, and therefore burden attribution was limited to age groups 30 years and older.
Discussion
Despite more than 50 years of anti-tobacco efforts, smoking remains a leading global risk factor. Its toll will remain substantial without more concerted policy initiatives, policy compliance and enforcement, and sustained political will to offset commercial interests. Despite progress in some settings, the war against tobacco is far from won, especially in countries with the highest numbers of smokers. The staggering toll of smoking on health echoes well beyond the individual, especially as tobacco threatens to exact long-term financial and operational burdens on already resource-constrained health systems. To significantly and permanently bend the global tobacco epidemic's trajectory, a renewed and sustained focus is needed on comprehensive tobacco control policies around the world. Success is possible, but requires effective and aggressively enforced policies and laws. Intensified efforts are also greatly needed to keep smoking prevalence rates low in populations which have not experienced a devastating epidemic yet, and to prevent children, adolescents, and young adults from starting to smoke.
Correspondence to: Dr Emmanuela Gakidou, Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA 98121 gakidou@uw.edu
GBD 2015 Tobacco Collaborators
Marissa B Reitsma, Nancy Fullman, Marie Ng, Joseph S Salama, Amanuel Abajobir*, Kalkidan Hassen Abate*, Cristiana Abbafati*, Semaw Ferede Abera*, Biju Abraham*, Gebre Yitayih Abyu*, Akindele Olupelumi Adebiyi*, Ziyad Al-Aly*, Alicia V Aleman*, Raghib Ali*, Ala'a Al Alkerwi*, Peter Allebeck*, Rajaa Mohammad Al-Raddadi*, Azmeraw T Amare*, Alemayehu Amberbir*, Walid Ammar*, Stephen Marc Amrock*, Carl Abelardo T Antonio*, Hamid Asayesh*, Niguse Tadela Atnafu*, Peter Azzopardi*, Amitava Banerjee*, Aleksandra Barac*, Tonatiuh Barrientos-Gutierrez*, Ana Cristina Basto-Abreu*, Shahrzad Bazargan-Hejazi*, Neeraj Bedi*, Brent Bell*, Aminu K Bello*, Isabela M Bensenor*, Addisu Shunu Beyene*, Neeraj Bhala*, Stan Biryukov*, Kaylin Bolt*, Hermann Brenner*, Zahid Butt*, Fiorella Cavalleri*, Kelly Cercy*, Honglei Chen*, Devasahayam Jesudas Christopher*, Liliana G Ciobanu*, Valentina Colistro*, Mercedes Colomar*, Leslie Cornaby*, Xiaochen Dai*, Solomon Abrha Damtew*, Lalit Dandona*, Rakhi Dandona*, Emily Dansereau*, Kairat Davletov*, Anand Dayama*, Tizta Tilahun Degfie*, Amare Deribew*, Samath D Dharmaratne*, Balem Demtsu Dimtsu*, Kerrie E Doyle*, Aman Yesuf Endries*, Sergey Petrovich Ermakov*, Kara Estep*, Emerito Jose Aquino Faraon*, Farshad Farzadfar*, Valery L Feigin*, Andrea B Feigl*, Florian Fischer*, Joseph Friedman*, Tsegaye Tewelde G/hiwot*, Seana L Gall*, Wayne Gao*, Richard F Gillum*, Audra L Gold*, Sameer Vali Gopalani*, Carolyn C Gotay*, Rahul Gupta*, Rajeev Gupta*, Vipin Gupta*, Randah Ribhi Hamadeh*, Graeme Hankey*, Hilda L Harb*, Simon I Hay*, Masako Horino*, Nobuyuki Horita*, H Dean Hosgood*, Abdullatif Husseini*, Bogdan Vasile Ileanu*, Farhad Islami*, Guohong Jiang*, Ying Jiang*, Jost B Jonas*, Zubair Kabir*, Ritul Kamal*, Amir Kasaeian*, Chandrasekharan Nair Kesavachandran*, Yousef S Khader*, Ibrahim Khalil*, Young-Ho Khang*, Sahil Khera*, Jagdish Khubchandani*, Daniel Kim*, Yun Jin Kim*, Ruth W Kimokoti*, Yohannes Kinfu*, Luke D Knibbs*, Yoshihiro Kokubo*, Dhaval Kolte*, Jacek Kopec*, Soewarta Kosen*, Georgios A Kotsakis*, Parvaiz A Koul*, Ai Koyanagi*, Kristopher J Krohn*, Hans Krueger*, Barthelemy Kuate Defo*, Burcu Kucuk Bicer*, Chanda Kulkarni*, G Anil Kumar*, Janet L Leasher*, Alexander Lee*, Mall Leinsalu*, Tong Li*, Shai Linn*, Patrick Liu*, Shiwei Liu*, Loon-Tzian Lo*, Alan D Lopez*, Stefan Ma*, Hassan Magdy Abd El Razek*, Azeem Majeed*, Reza Malekzadeh*, Deborah Carvalho Malta*, Wondimu Ayele Manamo*, Jose Martinez-Raga*, Alemayehu Berhane Mekonnen*, Walter Mendoza*, Ted R Miller*, Karzan Abdulmuhsin Mohammad*, Lidia Morawska*, Kamarul Imran Musa*, Gabriele Nagel*, Sudan Prasad Neupane*, Quyen Nguyen*, Grant Nguyen*, In-Hwan Oh*, Abayomi Samuel Oyekale*, Mahesh PA*, Adrian Pana*, Eun-Kee Park*, Snehal T Patil*, George C Patton*, Joao Pedro*, Mostafa Qorbani*, Anwar Rafay*, Mahfuzar Rahman*, Rajesh Kumar Rai*, Usha Ram*, Chhabi Lal Ranabhat*, Amany H Refaat*, Nickolas Reinig*, Hirbo Shore Roba*, Alina Rodriguez*, Yesenia Roman*, Gregory Roth*, Ambuj Roy*, Rajesh Sagar*, Joshua Salomon*, Juan Sanabria*, Itamar de Souza Santos*, Benn Sartorius*, Maheswar Satpathy*, Monika Sawhney*, Susan Sawyer*, Mete Saylan*, Michael P Schaub*, Neil Schluger*, Aletta Elisabeth Schutte*, Sadaf G Sepanlou*, Berrin Serdar*, Masood Ali Shaikh*, Jun She*, Min-Jeong Shin*, Rahman Shiri*, Kawkab Shishani*, Ivy Shiue*, Inga Dora Sigfusdottir*, Jonathan I Silverberg*, Jasvinder Singh*, Virendra Singh*, Erica Leigh Slepak*, Samir Soneji*, Joan B Soriano*, Sergey Soshnikov*, Chandrashekhar T Sreeramareddy *, Dan J Stein*, Saverio Stranges*, Michelle L Subart*, Soumya Swaminathan*, Cassandra E I Szoeke*, Worku Mekonnen Tefera*, Roman Topor-Madry*, Bach Tran*, Nikolaos Tsilimparis*, Hayley Tymeson*, Kingsley Nnanna Ukwaja*, Rachel Updike*, Olalekan A Uthman*, Francesco Saverio Violante*, Sergey K Vladimirov*, Vasiliy Vlassov*, Stein Emil Vollset*, Theo Vos*, Elisabete Weiderpass*, Chi-Pan Wen*, Andrea Werdecker*, Shelley Wilson*, Mamo Wubshet*, Lin Xiao*, Bereket Yakob*, Yuichiro Yano*, Penpeng Ye*, Naohiro Yonemoto*, Seok-Jun Yoon*, Mustafa Z Younis*, Chuanhua Yu*, Zoubida Zaidi*, Maysaa El Sayed Zaki*, Anthony Lin Zhang*, Ben Zipkin*, Christopher J L Murray†, Mohammad H Forouzanfar†, Emmanuela Gakidou†‡
*Authors listed alphabetically. †Joint senior authors. ‡Corresponding author.
Affiliations
Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA, USA (M B Reitsma BS, N Fullman MPH, M Ng PhD, J S Salama MSc, B Bell MLIS, S Biryukov BS, K Bolt MPH, K Cercy BS, L Cornaby BS, X Dai MSc, Prof L Dandona MD, R Dandona PhD, E Dansereau MPH, K Estep MPA, J Friedman BA, A L Gold MSc, Prof S I Hay DSc, I Khalil MD, G A Kotsakis DDS, K J Krohn BA, P Liu BA, A Lee BA, G Nguyen BA, N Reinig BS, Y Roman MLIS, G Roth MD, E L Slepak MLIS, M L Subart BA, H Tymeson BA, R Updike AB, Prof S E Vollset DrPH, Prof T Vos PhD, S Wilson BA, B Zipkin BS, Prof C J L Murray DPhil, M H Forouzanfar PhD, Prof E Gakidou PhD), University of Queensland, Brisbane, QLD, Australia (A Abajobir MPH, L D Knibbs PhD); Jimma University, Jimma, Ethiopia (K H Abate MS, T T G/hiwot MPH); La Sapienza, University of Rome, Rome, Italy (C Abbafati PhD); University of Hohenheim, Stuttgard, Germany (S F Abera MSc); NMSM Governement College Kalpetta, Kerala, India (Prof B Abraham MPhil); Mekelle University, Mekelle, Ethiopia (Prof G Y Abyu MS, B D Dimtsu MS, S F Ferede Abera MSc); University of Ibadan, Ibadan, Nigeria (A O Adebiyi MD); Washington University in Saint Louis, St Louis, MO, USA (Z Al-Aly MD); University of the Republic, Montevideo, Uruguay (A V Aleman MD, F Cavalleri BS, V Colistro MSc); University of Oxford, Oxford, UK (R Ali FRCP, A Deribew PhD, Prof S I Hay DSc); Luxembourg Institute of Health (LIH), Strassen, Luxembourg (A A Alkerwi PhD); Karolinska Institutet, Stockholm, Sweden (P Allebeck PhD, E Weiderpass PhD); Ministry of Health, Jeddah, Saudi Arabia (R M Al-Raddadi PhD); Marshall University, Huntington, WV, USA (A T Amare MPH); Dignitas International, Zomba, Malawi (A Amberbir PhD, S D Dharmaratne MD); Ministry of Public Health, Beirut, Lebanon (W Ammar PhD, H L Harb MPH); Oregon Health & Science University, Portland, OR, USA (S M Amrock PhD); University of the Philippines Manila, Manila, Philippines (C A T Antonio MD, E J A Faraon MD); Qom University of Medical Sciences, Qom, Iran (H Asayesh PhD); Mizan Tepi University, Mizan Teferi, Ethiopia (N T Atnafu MS); PMA 2020, Addis Ababa, Ethiopia (N T Atnafu MS); The University of Melbourne, Melbourne, VIC, Australia (P Azzopardi MEpi); Murdoch Childrens Research Institute, South Australian Health and Medical Research Institute, Adelaide, SA, Australia (P Azzopardi MEpi); Bucharest University of Economic Studies, Bucharest, Romania (A Banerjee DPhil, J Pedro MS); University of Belgrade, Belgrade, Serbia (A Barac PhD); University of Adelaide, Adelaide, SA, Australia (T Barrientos-Gutierrez PhD, W M Tefera MPH); University of Montreal, Montreal, QC, Canada (A C Basto-Abreu MPH); Charles R. Drew University of Medicine and Science, Los Angeles, CA, USA (Prof S Bazargan-Hejazi PhD); College of Public Health and Tropical Medicine, Jazan, Saudi Arabia (N Bedi MD); University of Alberta, Edmonton, AB, Canada (A K Bello PhD); University of São Paulo, Sao Paulo, Brazil (I M Bensenor PhD); Haramaya University, Harar, Ethiopia (A S Beyene MPH, H S Roba MPH); Queen Elizabeth Hospital Birmingham, Birmingham, UK (N Bhala DPhil); University of Otago Medical School, Otago, New Zealand (N Bhala DPhil); German Cancer Research Center, Heidelberg, Germany (Prof H Brenner MD); Al Shifa Trust Eye Hospital, Rawalpindi, Pakistan (Z Butt PhD); Michigan State University, Lansing, MI, USA (H Chen PhD); Christian Medical College, Vellore, India (Prof D J Christopher MD); New York Medical College, Valhalla, NY, USA (L G Ciobanu MS); Ministerio de Salud Publica, Montevideo, Uruguay (V Colistro MSc); UNICEM, Montevideo, Uruguay (M Colomar MSc); Wolaita Sodo University, Wolaita Sodo, Ethiopia (S A Damtew MPH); Addis Ababa University, Addis Ababa, Ethiopia (S A Damtew MPH, Prof D Kim DrPH, W A Manamo MS); Public Health Foundation of India, New Delhi, India (Prof L Dandona MD, R Dandona PhD); Republican Institute of Cardiology and Internal Diseases, Almaty, Kazakhstan (K Davletov PhD); Kazakh National Medical University, Almaty, Kazakhstan (K Davletov PhD); All India Institute of Medical Sciences, New Delhi, India (Prof A Dayama PhD, A Roy MD, R Sagar MD, M Satpathy PhD); African Population and Health Research Center, Nairobi, Kenya (T T Degfie PhD); RMIT University, Bundoora, VIC, Australia (Prof K Doyle PhD, A L Zhang PhD); Australian National University, Canberra, ACT, Australia (Prof K Doyle PhD); University of Peradeniya, Peradeniya, Sri Lanka (A Y Endries MPH); Russian Academy of Sciences, Moscow, Russia (Prof S P Ermakov DSc); Ministry of Health of the Russian Federation, Moscow, Russia (Prof S P Ermakov DSc, S Soshnikov PhD); Department of Health, Manila, Philippines (E J A Faraon MD); Tehran University of Medical Sciences, Tehran, Iran (F Farzadfar DSc, A Kasaeian PhD, Prof R Malekzadeh MD, S G Sepanlou PhD); Auckland University of Technology, Auckland, New Zealand (V L Feigin PhD); Harvard University, Boston, MA, USA (A B Feigl ScD, J Salomon PhD); Bielefeld University, Bielefeld, Germany (F Fischer MPH); University of Tasmania, Hobart, TAS, Australia (S L Gall PhD); Taipei Medical University, Taipei, Taiwan (W Gao PhD); Howard University, Washington, DC, USA (R F Gillum MD); Government of the Federated States of Micronesia, Palikir, Federated States of Micronesia (S V Gopalani MPH); University of British Columbia, Vancouver, BC, Canada (C C Gotay PhD, J Kopec PhD, H Krueger PhD); West Virginia Department of Health & Human Resources, Bureau for Public Health, Charleston, WV, USA (Rah Gupta MD); Eternal Heart Care Centre and Research Institute, Jaipur, India (Raj Gupta PhD); University of Delhi, Delhi, India (V Gupta PhD); Arabian Gulf University, Manama, Bahrain (Prof R R Hamadeh DPhil); University of Western Australia, Perth, WA, Australia (Prof G Hankey MD); Harry Perkins Institute of Medical Research, Nedlands, WA, Australia (Prof G Hankey MD); Nevada Division of Public and Behavioral Health, Carson City, NV, USA (M Horino MPH); Yokohama City University Graduate School of Medicine, Yokohama, Japan (N Horita PhD); Albert Einstein College of Medicine, Bronx, NY, USA (Prof H D Hosgood PhD); Birzeit University, Birzeit, Palestine (A Husseini PhD); National Institute of Public Health, Cuernavaca, Mexico (B V Ileanu PhD); American Cancer Society, Atlanta, GA, USA (F Islami PhD); Tianjin Centers for Disease Control and Prevention, Tianjin, China (G Jiang MD); Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Japan (Y Jiang PhD); Ruprecht-Karls-University Heidelberg, Mannheim, Germany (Prof J B Jonas MD); University College Cork, Cork, Ireland (Z Kabir PhD); CSIR-Indian Institute of Toxicology Research, Lucknow, India (R Kamal MSc, C N Kesavachandran PhD); Jordan University of Science and Technology, Irbid, Jordan (Prof Y S Khader ScD); Seoul National University, Seoul, South Korea (Prof Y Khang PhD); Northeastern University, Boston, MA, USA (S Khera MD); Ball State University, Muncie, IN, USA (J Khubchandani PhD); Southern University College, Skudai, Malaysia (Y J Kim PhD); Simmons College, Boston, MA, USA (R W Kimokoti MD); University of Canberra, Canberra, ACT, Australia (Y Kinfu PhD); National Cerebral and Cardiovascular Center, Suita, Japan (Y Kokubo PhD, M Sawhney PhD); Brown University, Providence, RI, USA (D Kolte PhD); Health Policy and Humanities, NIHRD, Jakarta, Indonesia (S Kosen MD); Sher-i-Kashmir Institute of Medical Sciences, Srinagar, India (Prof P A Koul MD); Parc Sanitari Sant Joan de Deu (CIBERSAM), Barcelona, Spain (A Koyanagi PhD); BRAC, Dhaka, Bangladesh (Prof B Kuate Defo PhD); Hacettepe University, Ankara, Turkey (B Kucuk Bicer PhD); Rajrajeswari Medical College & Hospital, Bangalore, India (Prof C Kulkarni PhD); Public Health Foundation of India, Guragon, India (G A Kumar PhD); Nova Southeastern University, Fort Lauderdale, FL, USA (J L Leasher OD); National Institute for Health Development, Tallinn, Estonia (M Leinsalu PhD); Södertörn University, Huddinge, Sweden (M Leinsalu PhD); National Center for Chronic and Noncommunicable Disease Control and Prevention (T Li MPH, P Ye MPH), Chinese Center for Disease Control and Prevention, Beijing, China (S Liu PhD); University of Haifa, Haifa, Israel (Prof S Linn PhD); UnionHealth Associates, LLC, St Louis, MO, USA (L Lopez MD); Alton Mental Health Center, Alton, IL, USA (L Lopez MD); University of Melbourne, Melbourne, VIC, Australia (Prof A D Lopez PhD, G C Patton MD, Prof S Sawyer MD, Prof C E I Szoeke PhD); Ministry of Health Singapore, Singapore, Singapore (S Ma PhD); National University of Singapore, Singapore, Singapore (S Ma PhD); Mansoura Faculty of Medicine, Mansoura, Egypt (H Magdy Abd El Razek MBBCH); Imperial College London, London, UK (Prof A Majeed MD, Prof A Rodriguez PhD); Universidade Federal de Minas Gerais, Belo Horizonte, Brazil (Prof D C Malta PhD); Hospital Universitario Doctor Peset, Valencia, Spain (J Martinez-Raga PhD); CEU Cardinal Herrera University, Valencia, Spain (J Martinez-Raga PhD); University of Gondar, Gondar, Ethiopia (A B Mekonnen MS); University of Sydney, Sydney, NSW, Australia (A B Mekonnen MS); United Nations Population Fund, Lima, Peru (W Mendoza MD); Pacific Institute for Research & Evaluation, Calverton, MD, USA (T R Miller PhD); Curtin University, Bentley, WA, Australia (T R Miller PhD); University of Salahaddin, Erbil, Iraw (K A Mohammad PhD); Queensland University of Technology, Brisbane, QLD, Australia (L Morawska PhD); University of Science Malaysia, Kubang Kerian, Malaysia (K I Musa MD); Ulm University, Ulm, Germany (Prof G Nagel PhD); University of Oslo, Oslo, Norway (S P Neupane PhD); Duy Tan University, Da Nang, Vietnam (Q Nguyen MD); Kyung Hee University, Seoul, South Korea (Prof I Oh PhD); North-West University, Mafikeng, South Africa (Prof A S Oyekale PhD); JSS University, Mysore, India (Prof M PA DNB); National Institute of Public Health, Mexico City, Mexico (A Pana MD); Kosin University, Busan, South Korea (E Park PhD); School of Dental Sciences, Karad, India (S T Patil MDS); Alborz University of Medical Sciences, Karaj, Iran (M Qorbani PhD); Contech International Health Consultants, Lahore, Pakistan (A Rafay MS); Contect School of Public Health, Lahore, Pakistan (A Rafay MS); St Paul's Hospital Millenium Medical College, Addis Ababa, Ethiopia (M Rahman PhD); Addis Continental Institute of Public Health, Addis Ababa, Ethiopia (M Rahman PhD); Society for Health and Demographic Surveillance, Suri, India (R K Rai MPhil); International Institute for Population Sciences, Mumbai, India (Prof U Ram PhD); Yonsei University, Wonju, South Korea (C L Ranabhat PhD); Walden University, Minneapolis, MN, USA (Prof A H Refaat PhD); Suez Canal University, Ismailia, Egypt (Prof A H Refaat PhD); University of Lincoln, Lincoln, UK (Prof A Rodriguez PhD); Harborview Medical Center, Seattle, WA, USA (G Roth MD); Marshall Univeristy, Huntington, WV, USA (J Sanabria MD); Case Western Reserve University, Cleveland, OH, USA (J Sanabria MD); University of Sao Paulo, Sao Paulo, Brazil (Prof I D Santos PhD); University of KwaZulu-Natal, Durban, South Africa (Prof B Sartorius PhD, B Yakob PhD); Bayer Turkey, Istanbul, Turkey (M Saylan PhD); University of Zurich, Zurich, Switzerland (M P Schaub PhD); World Lung Association, New York, NY, USA (N Schluger MD); North-West University, Potchefstroom, South Africa (Prof A E Schutte PhD); South African Medical Research Council, Tygerberg, South Africa (Prof A E Schutte PhD); University of Colorado, Aurora, CO, USA (B Serdar PhD); Independent Consultant, Karachi, Pakistan (M A Shaikh MD); Fudan University, Shanghai, China (J She PhD); Korea University, Seoul, South Korea (Prof M Shin PhD, S Yoon PhD); University of Helsinki, Helsinki, Finland (R Shiri PhD); Washington State University, Spokane, WA, USA (K Shishani PhD); Northumbria University, Newcastle upon Tyne, UK (I Shiue PhD); University of Edinburgh, Edinburgh, UK (I Shiue PhD); Reykjavik University, Reykjavik, Iceland (I D Sigfusdottir PhD); Northwestern University, Chicago, IL, USA (J I Silverberg PhD, Y Yano PhD); University of Alabama at Birmingham, Birmingham, AL, USA (J Singh MD); Asthma Bhawan, Jaipur, India (V Singh MD); Dartmouth University, Hanover, NH, USA (S Soneji PhD); Universidad Autonoma de Madrid, Madrid, Spain (Prof J B Soriano PhD); International Medical University, Kuala Lumpur, Malaysia (C T Sreeramareddy MD); University of Cape Town, Cape Town, South Africa (Prof D J Stein PhD); South African Medical Research Council Unit on Anxiety & Stress Disorders, Tygerberg, South Africa (Prof D J Stein PhD); University of Warwick, Coventry, UK (S Stranges PhD, O A Uthman PhD); Indian Council of Medical Research, Chennai, India (S Swaminathan MD); Bahir Dar University, Bahir Dar, Ethiopia (W M Tefera MPH); Jagiellonian University Medical College, Krakow, Poland (R Topor-Madry PhD); Johns Hopkins University, Baltimore, MD, USA (B X Tran PhD); Hanoi Medical University, Hanoi, Vietnam (B X Tran PhD); University Heart Center of Hamburg, Hamburg, Germany (N Tsilimparis PhD); University College London, London, UK (K N Ukwaja MD); University of Bologna, Bologna, Italy (Prof F S Violante MD); Federal Research Institute for Health Organization and Informatics, Moscow, Russia (S K Vladimirov PhD); National Research University Higher School of Economics, Moscow, Russia (Prof V Vlassov MD); Norwegian Institute of Public Health, Bergen, Norway (Prof S E Vollset DrPH); University of Bergen, Bergen, Norway (Prof S E Vollset DrPH); National Health Research Institutes, Taipei, Taiwan (C Wen PhD); Federal Institute for Population Research, Wiesbaden, Germany (A Werdecker PhD); College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia (Prof M Wubshet PhD); Emory University, Atlanta, GA, USA (Q Xiao MPH); Kyoto University, Kyoto, Japan (N Yonemoto MPH); Jackson State University, Jackson, MS, USA (Prof M Z Younis DrPH); Wuhan University, Wuhan, China (Prof C Yu PhD); University Hospital, Setif, Algeria (Prof Z Zaidi PhD); and Mansoura University, Mansoura, Egypt (Prof M E Zaki PhD).
Contributors
Marissa B Reitsma, Nancy Fullman, Joseph S Salama, and Emmanuela Gakidou drafted the report. Marissa B Reitsma, Emmanuela Gakidou, Marie Ng, Mohammad H Forouzanfar, and Christopher J L Murray conceived of the study, developed the analytical framework, and provided overall guidance. Marissa B Reitsma performed the analysis and produced the estimates. Kara Estep and Joseph S Salama managed the project. All authors contributed to at least one of the following: provided data, developed models, reviewed results, interpreted results, initiated modelling infrastructure, or reviewed and contributed to the final report.
Declaration of interests
Dan J Stein reports personal fees from Lundbeck, personal fees from Novartis, personal fees from AMBRF, grants from NRGF, grants from Servier, grants from Biocodex, grants from MRC, personal fees from CIPLA, personal fees from SUN, outside the submitted work; Jasvinder Singh reports personal fees from Savient, personal fees from Takeda, personal fees from Regeneron, personal fees from Iroko, personal fees from Merz, personal fees from Bioiberica, personal fees from Crealta, personal fees from Allergan, personal fees from UBM LLC, personal fees from WebMD, personal fees from The American College of Rheuamtology, institutional grants from Takeda, and institutional grants for Savient, outside the submitted work; Marie Ng reports personal fees from IBM Watson Health, outside the submitted work; Itamar De Souza Santos reports grants from FAPESP (Brazilian public agency), outside the submitted work. All other authors declare no competing interests.
Contributor Information
GBD 2015 Tobacco Collaborators:
Marissa B Reitsma, Nancy Fullman, Marie Ng, Joseph S Salama, Amanuel Abajobir, Kalkidan Hassen Abate, Cristiana Abbafati, Semaw Ferede Abera, Biju Abraham, Gebre Yitayih Abyu, Akindele Olupelumi Adebiyi, Ziyad Al-Aly, Alicia V Aleman, Raghib Ali, Ala'a Al Alkerwi, Peter Allebeck, Rajaa Mohammad Al-Raddadi, Azmeraw T Amare, Alemayehu Amberbir, Walid Ammar, Stephen Marc Amrock, Carl Abelardo T Antonio, Hamid Asayesh, Niguse Tadela Atnafu, Peter Azzopardi, Amitava Banerjee, Aleksandra Barac, Tonatiuh Barrientos-Gutierrez, Ana Cristina Basto-Abreu, Shahrzad Bazargan-Hejazi, Neeraj Bedi, Brent Bell, Aminu K Bello, Isabela M Bensenor, Addisu Shunu Beyene, Neeraj Bhala, Stan Biryukov, Kaylin Bolt, Hermann Brenner, Zahid Butt, Fiorella Cavalleri, Kelly Cercy, Honglei Chen, Devasahayam Jesudas Christopher, Liliana G Ciobanu, Valentina Colistro, Mercedes Colomar, Leslie Cornaby, Xiaochen Dai, Solomon Abrha Damtew, Lalit Dandona, Rakhi Dandona, Emily Dansereau, Kairat Davletov, Anand Dayama, Tizta Tilahun Degfie, Amare Deribew, Samath D Dharmaratne, Balem Demtsu Dimtsu, Kerrie E Doyle, Aman Yesuf Endries, Sergey Petrovich Ermakov, Kara Estep, Emerito Jose Aquino Faraon, Farshad Farzadfar, Valery L Feigin, Andrea B Feigl, Florian Fischer, Joseph Friedman, Tsegaye Tewelde G/hiwot, Seana L Gall, Wayne Gao, Richard F Gillum, Audra L Gold, Sameer Vali Gopalani, Carolyn C Gotay, Rahul Gupta, Rajeev Gupta, Vipin Gupta, Randah Ribhi Hamadeh, Graeme Hankey, Hilda L Harb, Simon I Hay, Masako Horino, Nobuyuki Horita, H Dean Hosgood, Abdullatif Husseini, Bogdan Vasile Ileanu, Farhad Islami, Guohong Jiang, Ying Jiang, Jost B Jonas, Zubair Kabir, Ritul Kamal, Amir Kasaeian, Chandrasekharan Nair Kesavachandran, Yousef S Khader, Ibrahim Khalil, Young-Ho Khang, Sahil Khera, Jagdish Khubchandani, Daniel Kim, Yun Jin Kim, Ruth W Kimokoti, Yohannes Kinfu, Luke D Knibbs, Yoshihiro Kokubo, Dhaval Kolte, Jacek Kopec, Soewarta Kosen, Georgios A Kotsakis, Parvaiz A Koul, Ai Koyanagi, Kristopher J Krohn, Hans Krueger, Barthelemy Kuate Defo, Burcu Kucuk Bicer, Chanda Kulkarni, G Anil Kumar, Janet L Leasher, Alexander Lee, Mall Leinsalu, Tong Li, Shai Linn, Patrick Liu, Shiwei Liu, Loon-Tzian Lo, Alan D Lopez, Stefan Ma, Hassan Magdy Abd El Razek, Azeem Majeed, Reza Malekzadeh, Deborah Carvalho Malta, Wondimu Ayele Manamo, Jose Martinez-Raga, Alemayehu Berhane Mekonnen, Walter Mendoza, Ted R Miller, Karzan Abdulmuhsin Mohammad, Lidia Morawska, Kamarul Imran Musa, Gabriele Nagel, Sudan Prasad Neupane, Quyen Nguyen, Grant Nguyen, In-Hwan Oh, Abayomi Samuel Oyekale, Mahesh PA, Adrian Pana, Eun-Kee Park, Snehal T Patil, George C Patton, Joao Pedro, Mostafa Qorbani, Anwar Rafay, Mahfuzar Rahman, Rajesh Kumar Rai, Usha Ram, Chhabi Lal Ranabhat, Amany H Refaat, Nickolas Reinig, Hirbo Shore Roba, Alina Rodriguez, Yesenia Roman, Gregory Roth, Ambuj Roy, Rajesh Sagar, Joshua Salomon, Juan Sanabria, Itamar de Souza Santos, Benn Sartorius, Maheswar Satpathy, Monika Sawhney, Susan Sawyer, Mete Saylan, Michael P Schaub, Neil Schluger, Aletta Elisabeth Schutte, Sadaf G Sepanlou, Berrin Serdar, Masood Ali Shaikh, Jun She, Min-Jeong Shin, Rahman Shiri, Kawkab Shishani, Ivy Shiue, Inga Dora Sigfusdottir, Jonathan I Silverberg, Jasvinder Singh, Virendra Singh, Erica Leigh Slepak, Samir Soneji, Joan B Soriano, Sergey Soshnikov, Chandrashekhar T Sreeramareddy, Dan J Stein, Saverio Stranges, Michelle L Subart, Soumya Swaminathan, Cassandra E I Szoeke, Worku Mekonnen Tefera, Roman Topor-Madry, Bach Tran, Nikolaos Tsilimparis, Hayley Tymeson, Kingsley Nnanna Ukwaja, Rachel Updike, Olalekan A Uthman, Francesco Saverio Violante, Sergey K Vladimirov, Vasiliy Vlassov, Stein Emil Vollset, Theo Vos, Elisabete Weiderpass, Chi-Pan Wen, Andrea Werdecker, Shelley Wilson, Mamo Wubshet, Lin Xiao, Bereket Yakob, Yuichiro Yano, Penpeng Ye, Naohiro Yonemoto, Seok-Jun Yoon, Mustafa Z Younis, Chuanhua Yu, Zoubida Zaidi, Maysaa El Sayed Zaki, Anthony Lin Zhang, Ben Zipkin, Christopher J L Murray, Mohammad H Forouzanfar, and Emmanuela Gakidou
Supplementary Material
References
- 1.Forouzanfar MH, Afshin A, Alexander LT. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jha P, Peto R. Global effects of smoking, of quitting, and of taxing tobacco. N Engl J Med. 2014;370:60–68. doi: 10.1056/NEJMra1308383. [DOI] [PubMed] [Google Scholar]
- 3.Ekpu VU, Brown AK. The economic impact of smoking and of reducing smoking prevalence: review of evidence. Tob Use Insights. 2015;8:1–35. doi: 10.4137/TUI.S15628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jha P. Deaths and taxes: stronger global tobacco control by 2025. Lancet. 2015;385:918–920. doi: 10.1016/S0140-6736(15)60464-0. [DOI] [PubMed] [Google Scholar]
- 5.Lancet T. What will it take to create a tobacco-free world? Lancet. 2015;385:915. doi: 10.1016/S0140-6736(15)60512-8. [DOI] [PubMed] [Google Scholar]
- 6.Gilmore AB, McKee M. Moving East: how the transnational tobacco industry gained entry to the emerging markets of the former Soviet Union—part I: establishing cigarette imports. Tob Control. 2004;13:143–150. doi: 10.1136/tc.2003.005108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blecher E, Ross H. Tobacco use in Africa: tobacco control through prevention. American Cancer Society; Atlanta, GA, USA: 2013. [Google Scholar]
- 8.Amos A, Greaves L, Nichter M, Bloch M. Women and tobacco: a call for including gender in tobacco control research, policy and practice. Tob Control. 2012;21:236–243. doi: 10.1136/tobaccocontrol-2011-050280. [DOI] [PubMed] [Google Scholar]
- 9.Chaloupka FJ, Yurekli A, Fong GT. Tobacco taxes as a tobacco control strategy. Tob Control. 2012;21:172–180. doi: 10.1136/tobaccocontrol-2011-050417. [DOI] [PubMed] [Google Scholar]
- 10.International Agency for Research on Cancer (IARC) Evaluating the effectiveness of smoke-free policies. In: Evaluating the effectiveness of smoke-free policies. IARC; Lyon, France: 2009. pp. 59–74. [Google Scholar]
- 11.Hopkins DP, Razi S, Leeks KD, Priya Kalra G, Chattopadhyay SK, Soler RE. Smokefree policies to reduce tobacco use. Am J Prev Med. 2010;38:S275–S289. doi: 10.1016/j.amepre.2009.10.029. [DOI] [PubMed] [Google Scholar]
- 12.Henriksen L. Comprehensive tobacco marketing restrictions: promotion, packaging, price and place. Tob Control. 2012;21:147–153. doi: 10.1136/tobaccocontrol-2011-050416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldberg DN, Krantz AJ, Semal S, Zhang H, Trick WE. Outcomes for a public hospital tobacco cessation program: the cook county health and hospitals system experience. J Community Health. 2016;41:1130–1139. doi: 10.1007/s10900-016-0215-5. [DOI] [PubMed] [Google Scholar]
- 14.Çelik İ, Yüce D, Hayran M. Nationwide smoking cessation treatment support program–Turkey project. Health Policy Amst Neth. 2015;119:50–56. doi: 10.1016/j.healthpol.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 15.Hammond D, Fong GT, McNeill A, Borland R, Cummings KM. Effectiveness of cigarette warning labels in informing smokers about the risks of smoking: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15:iii19–iii25. doi: 10.1136/tc.2005.012294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fong GT, Hammond D, Hitchman SC. The impact of pictures on the effectiveness of tobacco warnings. Bull World Health Organ. 2009;87:640–643. doi: 10.2471/BLT.09.069575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO . WHO Framework Convention on Tobacco Control. World Health Organization; Geneva, Switzerland: 2003. [Google Scholar]
- 18.WHO . WHO report on the global tobacco epidemic. World Health Organization; 2015. http://www.who.int/tobacco/global_report/2015/en/ (accessed Nov 8, 2016) [Google Scholar]
- 19.WHO Parties to the WHO Framework Convention on Tobacco Control. World Health Organization. http://www.who.int/fctc/signatories_parties/en/ (accessed Nov 8, 2016).
- 20.WHO . MPOWER: a policy package to reverse the tobacco epidemic. World Health Organization; Geneva, Switzerland: 2008. [Google Scholar]
- 21.Mattioli B, Quaranta MG, Vella S. Review on the evidence on public health impact of existing policies. Foresight and Modelling for European Health Policy and Regulation; Brussels, Belgium: 2016. [Google Scholar]
- 22.WHO NCD Global Monitoring Framework. World Health Organization. http://www.who.int/nmh/global_monitoring_framework/en/ (accessed Nov 8, 2016).
- 23.Beaglehole R, Bonita R, Yach D, Mackay J, Reddy KS. A tobacco-free world: a call to action to phase out the sale of tobacco products by 2040. Lancet. 2015;385:1011–1018. doi: 10.1016/S0140-6736(15)60133-7. [DOI] [PubMed] [Google Scholar]
- 24.United Nations (UN) Transforming our world: the 2030 Agenda for Sustainable Development. UN; New York, NY, USA: 2015. [Google Scholar]
- 25.Lopez AD, Collishaw NE, Piha T. A descriptive model of the cigarette epidemic in developed countries. Tob Control. 1994;3:242–247. [Google Scholar]
- 26.Jha P, Ranson MK, Nguyen SN, Yach D. Estimates of global and regional smoking prevalence in 1995, by age and sex. Am J Public Health. 2002;92:1002–1006. doi: 10.2105/ajph.92.6.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ezzati M, Lopez AD. Estimates of global mortality attributable to smoking in 2000. Lancet. 2003;362:847–852. doi: 10.1016/S0140-6736(03)14338-3. [DOI] [PubMed] [Google Scholar]
- 28.Giovino GA, Mirza SA, Samet JM. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet. 2012;380:668–679. doi: 10.1016/S0140-6736(12)61085-X. [DOI] [PubMed] [Google Scholar]
- 29.Ng M, Freeman MK, Fleming TD. Smoking prevalence and cigarette consumption in 187 countries, 1980-2012. JAMA. 2014;311:183–192. doi: 10.1001/jama.2013.284692. [DOI] [PubMed] [Google Scholar]
- 30.Bilano V, Gilmour S, Moffiet T. Global trends and projections for tobacco use, 1990–2025: an analysis of smoking indicators from the WHO Comprehensive Information Systems for Tobacco Control. Lancet. 2015;385:966–976. doi: 10.1016/S0140-6736(15)60264-1. [DOI] [PubMed] [Google Scholar]
- 31.Forouzanfar MH, Alexander L, Anderson HR. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–2323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lim SS, Vos T, Flaxman AD. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murray CJ, Lopez AD. On the comparable quantification of health risks: lessons from the Global Burden of Disease Study. Epidemiol Camb Mass. 1999;10:594–605. [PubMed] [Google Scholar]
- 34.Kontis V, Mathers CD, Rehm J. Contribution of six risk factors to achieving the 25×25 non-communicable disease mortality reduction target: a modelling study. Lancet. 2014;384:427–437. doi: 10.1016/S0140-6736(14)60616-4. [DOI] [PubMed] [Google Scholar]
- 35.Rentería E, Jha P, Forman D, Soerjomataram I. The impact of cigarette smoking on life expectancy between 1980 and 2010: a global perspective. Tob Control. 2016;25:551–557. doi: 10.1136/tobaccocontrol-2015-052265. [DOI] [PubMed] [Google Scholar]
- 36.Bilano VLF, Borja MP, Cruz EL, Tan AG, Mortera LL, Reganit PFM. Smoking-attributable burden of lung cancer in the Philippines. Tob Control. 2015;24:263–268. doi: 10.1136/tobaccocontrol-2013-051082. [DOI] [PubMed] [Google Scholar]
- 37.Wen CP, Tsai SP, Chen C-J, Cheng TY, Tsai M-C, Levy DT. Smoking attributable mortality for Taiwan and its projection to 2020 under different smoking scenarios. Tob Control. 2005;14:i76–i80. doi: 10.1136/tc.2004.007955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang H, Naghavi M, Allen C. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stevens GA, Alkema L, Black RE. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. The Lancet. 2016;388:e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 40.Bjartveit K, Tverdal A. Health consequences of smoking 1–4 cigarettes per day. Tob Control. 2005;14:315–320. doi: 10.1136/tc.2005.011932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pirie K, Peto R, Reeves GK, Green J, Beral V. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet. 2013;381:133–141. doi: 10.1016/S0140-6736(12)61720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peto R, Lopez AD, Boreham J, Thun M, Heath C. Mortality from tobacco in developed countries: indirect estimation from national vital statistics. Lancet. 1992;339:1268–1278. doi: 10.1016/0140-6736(92)91600-d. [DOI] [PubMed] [Google Scholar]
- 43.Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- 44.World Cancer Research Fund . American Institute for Cancer Research (AICR) Food, nutrition, and physical activity, and the prevention of cancer: a global perspective. AICR; Washington DC: 2007. [Google Scholar]
- 45.Unal B, Critchley J, Capewell S. Impact of smoking reduction on coronary heart disease mortality trends during 1981–2000 in England and Wales. Tob Induc Dis. 2003;1:17. doi: 10.1186/1617-9625-1-3-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Das Gupta P. Standardization and decomposition of rates: a user's manual. US Bureau of the Census; Washington DC: 1993. [Google Scholar]
- 47.GATS Atlas. Online http://www.gatsatlas.org/pdf/#p=42 (accessed Dec 28, 2016).
- 48.Department of Health and Human Services . The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General, 2014. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease and Health Promotion, Office on Smoking and Health; Atlanta, GA, USA: 2014. [Google Scholar]
- 49.Schroeder SA, Koh HK. Tobacco control 50 years after the 1964 surgeon general's report. JAMA. 2014;311:141–143. doi: 10.1001/jama.2013.285243. [DOI] [PubMed] [Google Scholar]
- 50.WHO . WHO Framework Convention on Tobacco Control: Guidelines for Implementation. 2013 edition. World Health Organization; Geneva, Switzerland: 2013. [Google Scholar]
- 51.Hiilamo H, Glantz S. FCTC followed by accelerated implementation of tobacco advertising bans. Tob Control. 2016 doi: 10.1136/tobaccocontrol-2016-053007. published online July 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.WHO Tobacco control in Pakistan. World Health Organization. http://www.who.int/tobacco/about/partners/bloomberg/pak/en/ (accessed Dec 28, 2016).
- 53.WHO . Panama's ban on tobacco advertising protects people's health. WHO; 2016. http://www.who.int/features/2013/panama_ban_tobacco/en/ (accessed Dec 28, 2016) [Google Scholar]
- 54.Mishra GA, Pimple SA, Shastri SS. An overview of the tobacco problem in India. Indian J Med Paediatr Oncol. 2012;33:139–145. doi: 10.4103/0971-5851.103139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Institute of Medicine (IOM) Ending the tobacco problem: a blueprint for the nation. IOM; Washington DC: 2007. [Google Scholar]
- 57.Park EJ, Koh HK, Kwon JW, Suh MK, Kim H, Cho SI. Secular trends in adult male smoking from 1992 to 2006 in South Korea: Age-specific changes with evolving tobacco-control policies. Public Health. 2009;123:657–664. doi: 10.1016/j.puhe.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 58.Stephens T, Pederson LL, Koval JJ, Macnab J. Comprehensive tobacco control policies and the smoking behaviour of Canadian adults. Tob Control. 2001;10:317–322. doi: 10.1136/tc.10.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Malta DC, Vieira ML, Szwarcwald CL. Smoking trends among Brazilian population. National Household Survey, 2008 and the National Health Survey, 2013. Rev Bras Epidemiol. 2015;18:45–56. doi: 10.1590/1980-5497201500060005. [DOI] [PubMed] [Google Scholar]
- 60.Monteiro CA, Cavalcante TM, Moura EC, Claro RM, Szwarcwald CL. Population-based evidence of a strong decline in the prevalence of smokers in Brazil (1989–2003) Bull World Health Organ. 2007;85:527–534. doi: 10.2471/BLT.06.039073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Iglesias R, Jha P, Pinto M, da Costa e Silva VL, Godinho J. Tobacco Control in Brazil. World Bank; Washington DC: 2007. [Google Scholar]
- 62.Mirra AP, Pereira IMTB, Stewien GT de M. Smoking control at the School of Public Health, Universidade de São Paulo. Rev Assoc Médica Bras. 2016;62:48–53. doi: 10.1590/1806-9282.62.01.48. [DOI] [PubMed] [Google Scholar]
- 63.Nagler RH, Viswanath K. Implementation and research priorities for FCTC Articles 13 and 16: tobacco advertising, promotion, and sponsorship and sales to and by minors. Nicotine Tob Res. 2013;15:832–846. doi: 10.1093/ntr/nts331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Owusu-Dabo E, McNeill A, Lewis S, Gilmore A, Britton J. Status of implementation of Framework Convention on Tobacco Control (FCTC) in Ghana: a qualitative study. BMC Public Health. 2010;10:1. doi: 10.1186/1471-2458-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tumwine J. Implementation of the Framework Convention on Tobacco Control in Africa: current status of legislation. Int J Environ Res Public Health. 2011;8:4312–4331. doi: 10.3390/ijerph8114312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Negi S. About National Tobacco Control Cell (NTCC) http://mohfw.nic.in/WriteReadData/l892s/About%20NTCC.pdf (accessed Nov 8, 2016).
- 67.Lunze K, Migliorini L. Tobacco control in the Russian Federation- a policy analysis. BMC Public Health. 2013;13:64. doi: 10.1186/1471-2458-13-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.WHO Russian Federation: President signs comprehensive tobacco control law. WHO. http://www.who.int/fctc/implementation/news/news_russia/en/ (accessed Dec 28, 2016).
- 69.Doku D. The tobacco industry tactics: a challenge for tobacco control in low and middle income countries. Afr Health Sci. 2010;10:201–203. [PMC free article] [PubMed] [Google Scholar]
- 70.Savell E, Gilmore AB, Fooks G. How does the tobacco industry attempt to influence marketing regulations? A systematic review. PLoS One. 2014;9 doi: 10.1371/journal.pone.0087389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Savell E, Gilmore AB, Sims M. The environmental profile of a community's health: a cross-sectional study on tobacco marketing in 16 countries. Bull World Health Organ. 2015;93:851–861. doi: 10.2471/BLT.15.155846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Connor Gorber S, Schofield-Hurwitz S, Hardt J, Levasseur G, Tremblay M. The accuracy of self-reported smoking: a systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine Tob Res. 2009;11:12–24. doi: 10.1093/ntr/ntn010. [DOI] [PubMed] [Google Scholar]
- 73.Jung-Choi K-H, Khang Y-H, Cho H-J. Hidden female smokers in Asia: a comparison of self-reported with cotinine-verified smoking prevalence rates in representative national data from an Asian population. Tob Control. 2011;21:536–542. doi: 10.1136/tobaccocontrol-2011-050012. [DOI] [PubMed] [Google Scholar]
- 74.Malcon MC, Menezes AMB, Assunção MCF, Neutzling MB, Hallal PC. Agreement between self-reported smoking and cotinine concentration in adolescents: a validation study in Brazil. J Adolesc Health Off Publ Soc Adolesc Med. 2008;43:226–230. doi: 10.1016/j.jadohealth.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 75.Stelmach R, Fernandes FLA, Carvalho-Pinto RM. Comparison between objective measures of smoking and self-reported smoking status in patients with asthma or COPD: are our patients telling us the truth? J Bras Pneumol. 2015;41:124–132. doi: 10.1590/S1806-37132015000004526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Carter BD, Abnet CC, Feskanich D. Smoking and mortality: beyond established causes. N Engl J Med. 2015;372:631–640. doi: 10.1056/NEJMsa1407211. [DOI] [PubMed] [Google Scholar]
Uncited Reference
- 55.Wakefield MA, Durkin S, Spittal MJ. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health. 2008;98:1443–1450. doi: 10.2105/AJPH.2007.128991. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.