Abstract
Background:
We aimed to explore whether maternal asymptomatic hepatitis B (HB) infection effects on pre-term rupture of membranous (PROM), stillbirth, preeclampsia, eclampsia, gestational hypertension, or antepartum hemorrhage.
Methods:
We searched the PubMed, Scopus, and ISI web of science from 1990 to Feb 2015. In addition, electronic literature searches supplemented by searching the gray literature (e.g., conference abstracts thesis and the result of technical reports) and scanning the reference lists of included studies and relevant systematic reviews. We explored statistical heterogeneity using the, I2 and tau-squared (Tau2) statistical tests.
Results:
Eighteen studies were included. Preterm rupture of membranous (PROM), stillbirth, preeclampsia, eclampsia, gestational hypertension and antepartum hemorrhage were considerable outcomes in this survey. The results showed no significant association between inactive HB and these complications in pregnancy. The small amounts of P-value and chi-square and large amount of I2 suggested the probable heterogeneity in this part, which we tried to modify with statistical methods such as subgroup analysis.
Conclusion:
Inactive HB infection did not increase the risk of adversely mentioned outcomes in this study. Further, well-designed studies should be performed to confirm the results.
Keywords: Inactive hepatitis B, Pregnancy outcome, Pregnancy adverse effect
Introduction
Today, viral hepatitis has a heavy burden on health systems (1). The hepatitis B virus (HBV) as a type of hepatitis viruses can lead to morbidity and mortality on the world (2). The inactive HBV is 100 times (100×) more contagious and more robust than HIV, and it often goes undetected (3). Approximately 25% of sexual contacts of HB infected persons maybe contagious for HBV. HBV is most commonly spread by an infected mother to her infant at birth (4), making it an important issue in the area of pregnancy and childbearing, as it can lead to chronic disease or hepatocellular carcinoma in adults who acquired the virus at birth. “Despite the hepatitis B immunization, HBV infection still is a threatened medical and financial issue and affects young adults in the world. Virus transmission and the fetus health are both the important concerns of women in the world” (5, 6).
As with many diseases in pregnancy, little is known about HBV infection and it was generally accepted that inactive hepatitis B (IHB) infection did not affect gestation or pregnancy outcome (7, 8). However, although conflicting, challenge this belief (9) as some studies have explored the impact of this infection on pregnancy outcomes such as preterm birth, prepartum hemorrhage, gestational diabetes mellitus (GDM, fetal macro-somia or poor the other pregnancy outcomes) (10–30).
Since, awareness of HB effects on pregnancy outcomes is important for both patients and healthcare providers and the study results are controversial we have done this research to partly clarify the effects.
Methods
Search Strategy and selection criteria
We used a specific methodology to do this study based on our previous research (17). We searched PubMed, Scopus, and ISI web of science from 1990 to Feb 2015. After the initial assessment of the electronic sources, references identified as potentially relevant examined to identify the three key journals. In addition, electronic literature searches supplemented by searching the gray literature (e.g., conference abstracts thesis and the result of technical reports) and scanning the reference lists of included studies and relevant systematic reviews. We applied a free keywords or MESH words search with the following terms: inactive hepatitis B, “Hepatitis B surface antigen”, Hbs Ag, hepatitis B carrier, pregnancy outcome, prenatal outcome, obstetric outcomes, pregnancy adverse effect, preterm rupture of membranous (PROM), stillbirth, preeclampsia, eclampsia, gestational hypertension, and antepartum hemorrhage.
We included any cohort, case-control, and cross-sectional studies if they had a healthy control group and reported one or more considered maternal or prinatal outcomes. Patients meeting the following criteria were included:
Pregnant women previously diagnosed as IHB carriers or diagnosed in routine antenatal blood test in pregnancy;
Pregnant women with normal singleton pregnancy with no history of disease or medication consumption.
Studies were excluded if (a) there was no control group of natural conception, (b) obstetric and perinatal outcomes were not reported, (c) the study subjects of primary articles did not have normal singleton pregnancy, or being addicted, or (d) subjects indicated superinfection with hepatitis A, C, D or E virus.
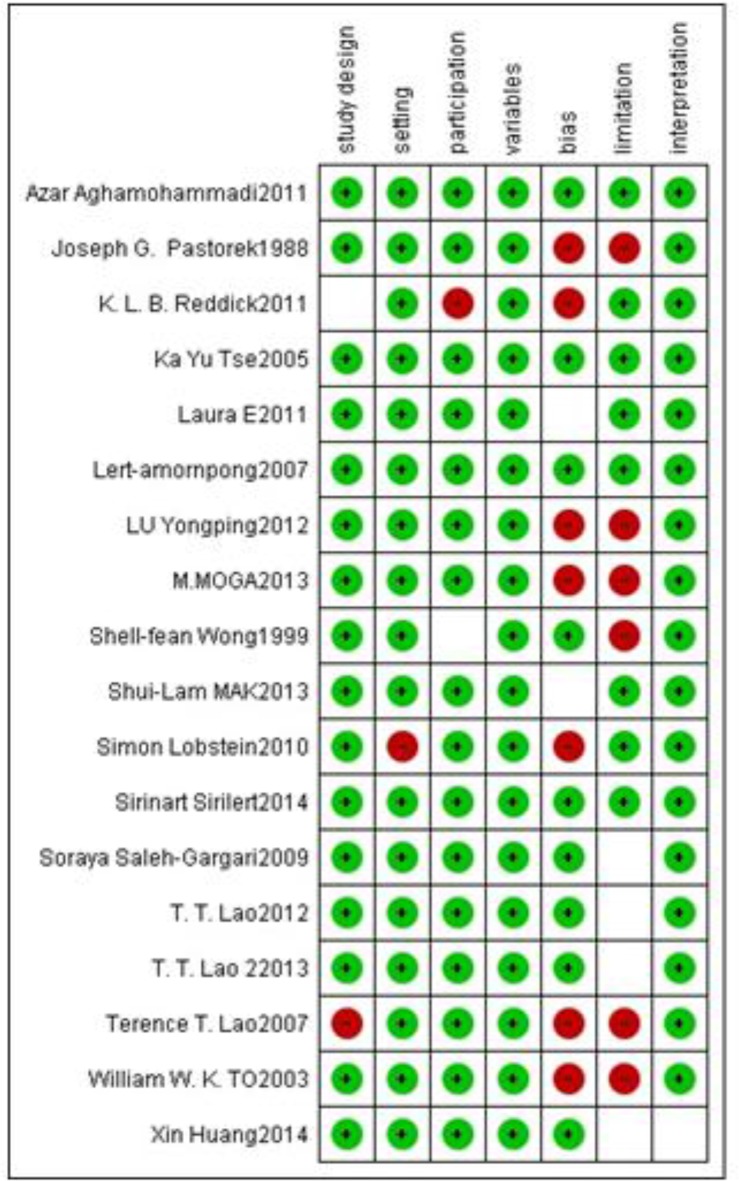
For quality assessment, we used the modified version of STROBE that includes seven items of STROBE checklist (setting, participation, variables, bias, limitation, and interpretation). There were five low-risk studies and nine high-risk studies among the included studies (Fig. 1). For publication bias assessment, we used the Begg and the Egger tests.
Fig. 1:
Risk of bias summary: review authors’ judgments about each risk
Results
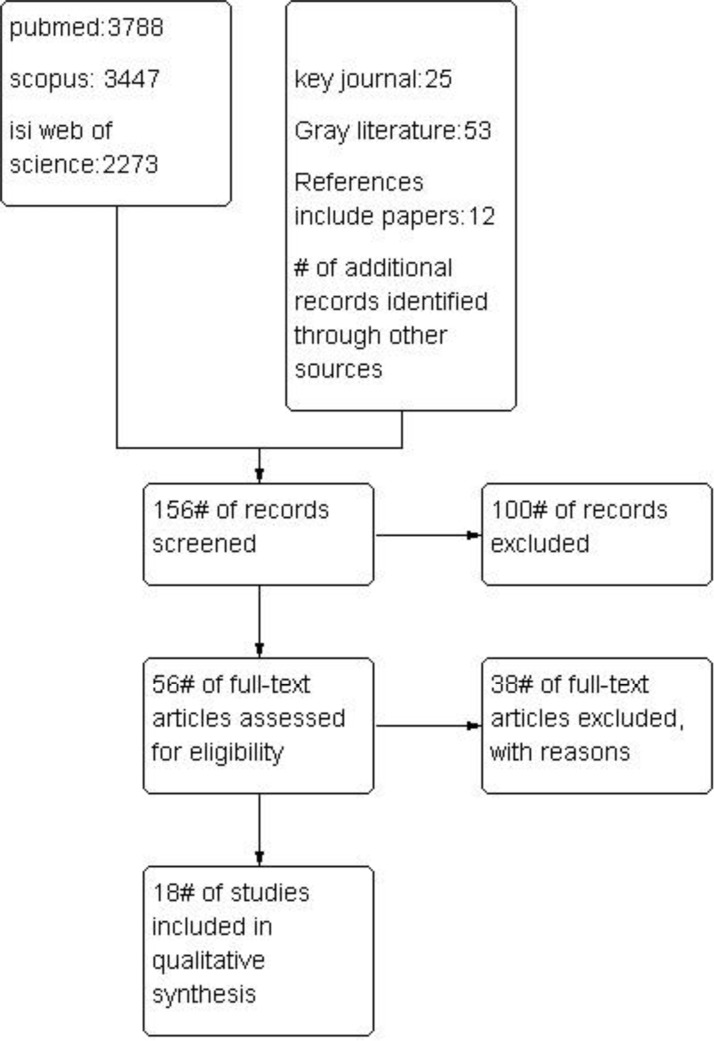
The results of the literature search are summarized in Fig. 2.
Fig. 2:
Flow diagram of the progress through the phases of meta-analysis
Overall, 156 studies were identified and reviewed by two reviewers. Fifty-six studies were selected for a detailed review, and finally, eighteen studies could include in the meta-analysis. Among the included studies, the outcomes were as follows: Eight studies in preterm rupture of membranous (PROM), six in stillbirth, fourteen in preeclampsia, six in eclampsia, eight in gestational hypertension, and nine in antepartum hemorrhage.
Meta-analysis of preterm rupture of membranous (prom) and inactive Hepatitis B
Eight of the eighteen studies compared the PROM between the IHB carrier and healthy pregnant women groups (8, 15, 20, 22, 23, 29, 30).
The P-value was 0.009 and the corresponding I2 statistic was 63%, suggesting moderate variability among the studies. The pooled OR of having preterm rupture of membranous among inactive HB carrier women versus non-infected women was 1.33 (95% CI, 0.94–1.89). These findings suggest no significant association between inactive HB carrier infection and PROM. Subgroup analysis based on study design (case-control and cohort) could not decrease I2, but subgroup analysis based on quality of papers (high vs. low) could decrease I2 only in low-quality group of study.
Meta-analysis of stillbirth and inactive Hepatitis B
Six of the eighteen studies compared the stillbirth between the IHB and healthy pregnant women groups (8, 14, 15, 24, 31, 32).
The P-value was 0.08 and the corresponding I2 statistic was 50%, suggesting low variability among the studies. The combined OR was 0.9. (95% CI: 0.52–1.55). This effect size measure means that the difference between the two groups (infected vs. non-infected) was not statistically significant.
Meta-analysis of preeclampsia and inactive Hepatitis B
Fourteen of the eighteen studies compared the preeclampsia between the IHB carrier and healthy pregnant women groups (7, 8, 12–15, 20–22, 24, 29, 31–33). The P-value was 1.01 and the corresponding I2 statistic was 71%, suggesting severe variability among the studies. The risk of preeclampsia was similar between the two groups (OR=1.03, 95% CI: 0.78–1.35;. For heterogeneity, we conducted two subgroup analyses based on study design and quality that two analyses could decrease I2 only in cohort study group and low-quality study group, respectively
Meta-analysis of eclampsia and inactive hepatitis B
Six of the eighteen studies compared eclampsia between the IHB and healthy pregnant women groups (8, 20–22, 24, 31). The P-value was 0.9 and the corresponding I2 statistic was 0%, suggesting no variability among the studies. The rate of eclampsia was similar between the two groups (OR = 1.33, 95% CI: 0.49–3.63).
Meta-analysis of gestational hypertension and inactive hepatitis B
Eight of the eighteen studies compared gestational hypertension between the IHB and healthy pregnant women groups (8, 14, 20–22, 31, 30). The P-value was 0.1 and the corresponding I2 statistic was 40%, suggesting low variability among the studies. The rate of gestational hypertension was similar between the two groups (OR=0.9, 95% CI: 0.74–1.08,
Meta-analysis of antepartum hemorrhage and inactive hepatitis B
Nine of the eighteen studies compared the antepartum hemorrhage between the IHB and healthy pregnant women groups (8, 12–15, 21, 23, 31, 29). The P-value was 0.0002 and the corresponding I2 statistic was 74%, suggesting moderate variability among the studies. The two groups have a similar chance for antepartum hemorrhage (OR=1.13, 95% CI: 0.84–1.51). Subgroup analysis based on study quality could decrease I2 in both subgroups.
Discussion
IHB was not associated with higher rate of adverse pregnancy outcomes such as PROM, stillbirth, preeclampsia, eclampsia, gestational hypertension, ante partum hemorrhage. However, we must pay attention to the amounts of statistical tests of heterogeneity in our interpretation. If we have a meta-analysis with low sample size, the Chi2 test can detect the small amount of heterogeneity that may be clinically unimportant, as was the case in our review. The other parts of heterogeneity can be related to remarkable differences between the study’s results. Moreover, in our study despite the observed heterogeneity, the amount of Tau2 statistic was small and equal to 0.15. This paradox happens when the variance between studies is low and within studies variance is high (34, 35).
Despite the reasons discussed above, where the amount of I2 test was high, we examined the source of heterogeneity with the special methods. In the section related to PROM, heterogeneity was moderate (I2=63%). Subgroup analysis based on quality of studies could decrease the amount of I2 in low-quality studies. A closer look at the effect size estimated by studies in high-quality group showed that low sample size studies had the larger effect size.
In examining the relationship between stillbirth and IHB, analysis results showed IHB infection is not equal to a significant increase in the risk of stillbirth in patients.
A positive effect of IHB on stillbirth may occur because of a higher probability of these pregnancies being accompanied by premature labor, high blood pressure, gestational diabetes, or premature rupture of membranes (15, 24). However, other studies denied this effect and stated, “so that the risk of transplacental infection is low, the fetal risk should not increase”. (8, 14, 31, 32).
Besides, in this part, the amount of I2 indicated that low heterogeneity was observed among the studies. The forest plot showed that the high heterogeneity (15, 24), which had an OR of almost four to nine times that of the other studies. These two studies had lower sample sizes than the other studies in this section.
In the sections related to hypertensive disorder in pregnancy, including preeclampsia, eclampsia and gestational hypertension, IHB did not have a significant effect on these disturbances in pregnancy. Studies that verified the probable effects of IHB on hypertensive disorder in pregnant women said that the systemic inflammation caused by the IHB is responsible for these effects (15, 24, 30). However, some other non-effect studies believed this effect could only be observed in some Asian studies that did not pay attention to the compounding factors such as higher virus loads in the investigated cohort or lack of gynecological and neonatal management in affected pregnant women in these areas (7, 8, 12, 13). The conclusion did not end here in this part because the amount of heterogeneity was different in each part. The study results regarding preeclampsia and hepatitis proposed substantial heterogeneity (I2=70%), therefore, we conducted two subgroup analyses based on quality and study design. Quality subgroup analysis modified the amount of I2 only in the low-quality study group (I2=30%), but the other analysis did not have any effect. The high heterogeneity was indicated visual inspection of forest plot (15) that had an OR almost five times of those in the other studies. In this group, most of the studies were conducted in Hong Kong, and one in Iran, so the racial difference may have a role in this heterogeneity.
The last part of this study is allocated to postpartum hemorrhage and its possible association with inactive hepatitis B. The results of individual studies do not confirm this relationship. Three primary studies that found this result related this effect to increases in both the incidence of placenta previa and placental abruption in these pregnancies (29). Heterogeneity between study results was high, and subgroup analyses based on quality modified it in both groups.
Strength of evidence
This study was one of the few studies that attempted to evaluate the adverse effects of IHB on the outcome of pregnancy.
Limitations
The first limitation was importing low-quality studies. The reason for this limitation was the small number of studies done in this area. The second limitation was related to the nature of inactive hepatitis. IHB is endemic in some countries, such as China, so there are many studies conducted in this country that did not have an English abstract and use of them needs to be searched in native languages. The other limitation was about the original articles on meta-analysis performed. Some of these articles have reported the association between IHB viral load and considered outcomes in pregnancy.
Conclusion
IHB carrier status did not increase the risk of adverse effects such as preterm rupture of membranous (PROM), stillbirth, preeclampsia, eclampsia, gestational hypertension, and antepartum hemorrhage during pregnancy. Women who are IHBcarriers can be managed as any other low-risk pregnancies if they do not have other antenatal complications or associated risk factors such as additional diseases in pregnancy. However, these results should be assessed with further well-designed studies.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
Shahroud University of Medical Sciences supports this article. This article is a part of the PhD thesis. We would like to thank Vic-Chancellor of Education as well as Vic-chancellor of Research and Technology of Shahroud University of Medical Sciences for financial support of this study. The authors declare that they have no conflicts of interest.
References
- 1.Alavian SM, Ebrahimi E, Abedini M. (2016). Necessity for HBs Ag screening in pregnant women in Iran, needed now. Iran Red Crescent Med J, (In Press):e40844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lavanchy D. (2004). Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat, 11(2):97–107. [DOI] [PubMed] [Google Scholar]
- 3.Karimi-Sari H, Tajik M, Bayatpoor ME, Alavian SM. (2017). Increasing the Awareness of the General Population: An Important Step in Elimination Programs of Viral Hepatitis. Am J Gastroenterol, 112 (2): 393–395. [DOI] [PubMed] [Google Scholar]
- 4.Alavian SM, Nikfar S, Kebriaeezadeh A, Lotfi F, Sanati E, Rezaei Hemami M, Keshavarz K. (2016). A Cost-Utility Analysis of Different Antiviral Medicine Regimens in Patients with Chronic Hepatitis C Virus Genotype 1 Infection. Iran Red Crescent Med J, 18(11): e37094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mirmomen S, Alavian SM, Hajarizadeh B, Yektaparast B, Zahedi MJ, Zand V, Azami AA, Hosseini MM, Faridi AR, Davari K, Hajibeigi B. (2006). Epidemiology of Hepatitis B, Hepatitis C, and Human Immunodeficiency Virus Infecions in Patients with Beta-Thalassemia in Iran: A Multicenter Study. Arch Iran Med, 9 (4): 319 – 323. [PubMed] [Google Scholar]
- 6.Alavian SM. (2007). Decreasing the hepatitis B burden in Tunisia need more attention to adults for vaccination. Epidemiol Infect, 145(7):1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pastorek JG, Miller JM, Summers PR. (1988). The effect of hepatitis B antigenemia on pregnancy outcome. Am J Obstet Gynecol, 158 (3 Pt 1): 486–9. [DOI] [PubMed] [Google Scholar]
- 8.Wong S, Chan LY, Yu V, Ho L. (1999). Hepatitis B carrier and perinatal outcome in singleton pregnancy. Am J Perinatol, 16 (9): 485–8. [DOI] [PubMed] [Google Scholar]
- 9.DegliEsposti S, Shah D. (2011). Hepatitis B in Pregnancy: Challenges and Treatment. Gastroenterol Clin North Am, 40 (2): 355–72. [DOI] [PubMed] [Google Scholar]
- 10.Lao TT, Sahota DS, Suen SS, Lau TK, Leung TY. (2010). Chronic hepatitis B virus infection and rubella susceptibility in pregnant women. J Viral Hepat, 17 (10): 737–41. [DOI] [PubMed] [Google Scholar]
- 11.Elefsiniotis I, Tsoumakas K, Vezali E, Glynou I, Drakoulis N, Saroglou G. (2010). Spontaneous preterm birth in women with Hepatitis B virus infection. Int J Gynaecol Obstet, 110 (3): 241–4. [DOI] [PubMed] [Google Scholar]
- 12.Reddick KL, Jhaveri R, Gandhi M, James AH, Swamy GK. (2011). Pregnancy outcomes associated with viral hepatitis. J Viral Hepat, 18 (7): e394–8. [DOI] [PubMed] [Google Scholar]
- 13.Lao TT, Chan BC, Leung WC, Ho LF, Tse KY. (2007). Maternal Hepatitis B infection and gestational diabetes mellitus. J Hepatol, 47 (1): 46–50. [DOI] [PubMed] [Google Scholar]
- 14.Lao TT, Sahota DS, Suen SS, Law LW, Leung TY. (2012). Maternal HBs Ag status and infant size–a Faustian bargain?. J Viral Hepat, 19 (7): 519–24. [DOI] [PubMed] [Google Scholar]
- 15.Saleh-Gargari S, Hantoushzadeh S, Zendehdel N, Jamal A, Aghdam H. (2009). The Association of Maternal HBs Ag Carrier Status and Perinatal Outcome. Hepat Mon, 9 (3): 180–4. [Google Scholar]
- 16.Safir A, Levy A, Sikuler E, Sikuler E, Sheiner E. (2010). Maternal Hepatitis B virus or hepatitis C virus carrier status as an independent risk factor for adverse perinatal outcome. Liver Int, 30 (5): 765–70. [DOI] [PubMed] [Google Scholar]
- 17.Ebrahimi E, Keramat A, Yunesian M, Alavian SM, Khosravi A, Montazeri A, Abedini M. (2016). Maternal inactive hepatitis B Status and Birth-Outcomes: A Systematic Review and Meta-Analysis. Iran Red Crescent Med J, 18 (11): e 31820. [Google Scholar]
- 18.Lao TT, Sahota DS, Cheng YK, Law LW, Leung TY. (2013). Maternal Hepatitis B surface antigen status and incidence of pre eclampsia. J Viral Hepat, 20 (5): 343–9. [DOI] [PubMed] [Google Scholar]
- 19.Vandenbroucke JP, Elm Ev, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M. (2007). Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology, 18(6):805–35. [DOI] [PubMed] [Google Scholar]
- 20.Connell LE , Salihu HM , Salemi JL , August EM, Weldeselasse H, Mbah AK. (2011). Maternal Hepatitis B and hepatitis C carrier status and perinatal outcomes. Liver Int, 31 (8): 1163–70. [DOI] [PubMed] [Google Scholar]
- 21.MAK SL, leung KY. (2013). Hepatitis B Carriers in Hong Kong, Prevalence and Pregnancy Outcomes. HKJGOM, 13 (1):67–73. [Google Scholar]
- 22.LU Y, Chen YP, Xiao X, Liang X, Li J, Huang S, Chen X, Hocher B. (2012). Impact of maternal Hepatitis B surface antigen carrier status on preterm delivery in southern China. Nan Fang Yi Ke Da Xue Xue Bao, 32 (9): 1369–72. [PubMed] [Google Scholar]
- 23.Moga M, Anastasiu C, bagiu N. (2012). Is maternal HBs Ag carrier status associated with adverse pregnancy outcome? Obstetrics, 9 (31): 8–10. [Google Scholar]
- 24.Lobstein S, Faber R, Tillmann HL. (2011). Prevalence of Hepatitis B among Pregnant Women and Its Impact on Pregnancy and Newborn Complications at a Tertiary Hospital in the Eastern Part of Germany. Digestion, 83 (1–2): 76–82. [DOI] [PubMed] [Google Scholar]
- 25.Higgins JPT, Green S. (2008). Cochrane handbook for systematic reviews of interventions Version 5.0.0: The Cochrane Collaboration. http://handbook.cochrane.org/v5.0.0/.
- 26.RevMan. Review Manager (RevMan) [Computer program] (2008). RevMan. Version 5.0 for Windows. Copenhagen: The Nordic Cochrane Centre, the Cochrane Collaboration; http://community.cochrane.org/tools/review-production-tools/revman-5/about-revman-5 [Google Scholar]
- 27.Stata Corp (2009). Stata Statistical Software: Release 11. College Station, TX: StataCorp LP; http://www.stata.com/support/faqs/resources/citing-software-documentation-faqs/ [Google Scholar]
- 28.Aghamohammadi A, Nooritajer M. (2011). Maternal Hbsag Carrier and Pregnancy Outcome. Aust J Basic Appl Sci, 5(3): 607–610. [Google Scholar]
- 29.Tse KY, Ho LF, Lao T. (2005). The impact of maternal HBs Ag carrier statuson pregnancy outcomes: A case–control study. J Hepatol, 43 (5):771–5. [DOI] [PubMed] [Google Scholar]
- 30.Lert-amornpong S, Caengow S, Chutaputti A. (2007). The Association of Pregnancy Outcomes and HBs Ag Positive. Thai J Gastroenterol, 8 (3): 115–118. [Google Scholar]
- 31.TO WW, Cheung W, Mok Km. (2003). Hepatitis B surface antigen carrier status and its correlation to gestational hypertension. Aust N Z J Obstet Gynaecol, 43 (2): 119–122. [DOI] [PubMed] [Google Scholar]
- 32.Sirinart S, Kuntharee T, Pannee S, Theera T. (2014). Pregnancy outcomes among carriers of Hepatitis B virus. Int J Gynaecol Obstet, 126 (2): 106–10. [DOI] [PubMed] [Google Scholar]
- 33.Huang X, Tan H, Li X, Zhou S, Wu Wen S, Luo M. (2014). Maternal chronic HBV infection would not increase the risk of pregnancy-induced hypertension--results from pregnancy cohort in Liuyang rural China. PLoS One, 9 (12): e114248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Borenstein M, Hedges L, Rothstein H. (2007). Meta-analysis: fixed effect vs. random effects. John Wiley and Sons Ltd Inc, pp: 11–21. [Google Scholar]
- 35.Lindheimer A, Katz AI. ( 1989 . ). Preeclampsia: pathophysiology, diagnosis, and management . Annu Rev Med, 40 : 233 –50. [DOI] [PubMed] [Google Scholar]