Abstract
PSMA PET is increasingly being used in imaging of recurrent prostate carcinoma. A case with suspected recurrent Prostate carcinoma (PCa), raised PSA (Prostate specific antigen) and suspected spinal metastases was referred for whole body Ga-68-PSMA PET/MRI.
The study revealed PSMA avid recurrent prostate mass and extensive osseous metastases. Abnormal PSMA uptake in the thyroid gland prompted USG-guided FNAC which revealed Hurthle cell neoplasm. Histopathological examination (HPE) of excised gland showed multiple Hurthle cell adenomas in both lobes of thyroid along with foci of papillary thyroid carcinoma which on immunohistochemistry were thyroglobulin positive and PSA negative.
Keywords: Hurthle cell adenoma, PET/MRI, PSMA, prostate carcinoma, thyroid carcinoma
Case report
A 66-year-old male with the history of prostate carcinoma, who underwent transurethral resection of the prostate 2 years back with raised PSA level and suspected spinal metastases, was referred for Ga-68-PSMA whole-body simultaneous PET/MRI scan for restaging. A bulky T2W hypointense mass was noted in residual prostate involving right seminal vesicle [Figure 1a] with the base of the bladder and mesorectal fascia, showing diffusion restriction [Figure 1b and 1c], increased Ktrans [Figure 1d] and increased PSMA uptake SUV max = 12.1 to 21.1 [Figure 1e and 1f]. No enlarged/PSMA avid nodes were seen. Widespread PSMA avid marrow lesions were seen extensively involving the spine [Figure 1g and 1h] and the remaining skeleton with SUV max = 8.5 to 27.5 [Figure 1i].
Figure 1.
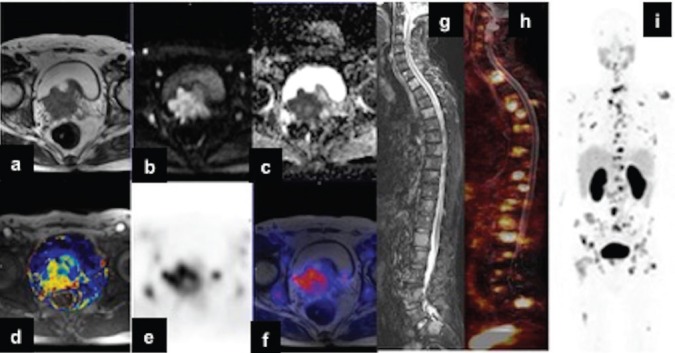
Representative PET/MRI images of a bulky hypointense mass (a) axial T2 is noted in residual prostate showing diffusion restriction (b) DWI with b = 800 and (c) ADC, (d) increased Ktrans and (e) increased PSMA uptake (f) fused PET/MRI. No enlarged/PSMA avid nodes were seen. Sagittal STIR (g) and fused PET/MRI (h) images showing PSMA avid marrow lesions. MIP PET (i) image showing wide spread PSMA avid metastases in the remaining skeleton.
Further, an enlarged thyroid gland showing multiple nodules of varying intensity and sizes involving both lobes [Figure 2a–2c] was observed with focal increased PSMA uptake [Figure 2d–2f] on the left side with SUV max = 5.9. No enlarged/ PSMA avid nodes were seen in bilateral neck.
Figure 2.
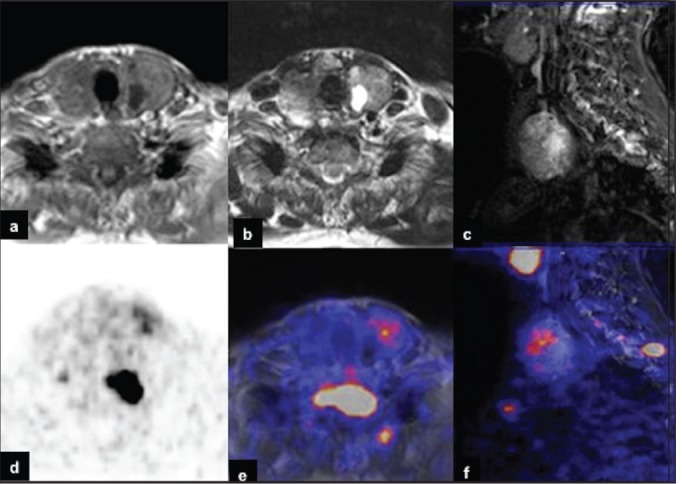
Representative PET/MRI image of an enlarged thyroid gland showing multiple nodules (a-c) axial T1; T2 and sagittal STIR respectively and focal areas of PSMA uptake (d-f) axial PET; axial fused PET/MRI and sagittal fused PET/MRI respectively.
USG-guided FNAC of thyroid was done which was reported as Hurthle cell neoplasm. Subsequently, total thyroidectomy was performed and the excised gland was sent for HPE which revealed multiple large nodules in both lobes consistent with Hurthle cell adenoma [Figure 3a]. In addition, small sub centimeter foci showing tubule-papillary architecture of papillary carcinoma [Figure 3b] were also noted in both lobes of thyroid. Subsequently, immunohistochemistry analysis was carried out and the thyroid lesions were found to show intense expression for thyroglobulin [Figure 3c] and no expression for PSA [Figure 3d] thereby ruling out metastases from PCa and proving that it is a primary thyroid neoplasm. A small pretracheal node sampled during surgery was reported to have metastases from papillary thyroid carcinoma based on its follicular architecture [Figure 3e and 3f]. The pretracheal node was positive for thyroglobulin and negative for PSA [Figure 3g and 3h]. Central compartment neck lymph nodes showed no evidence of metastases. There was no lymphovascular, perineural, capsular invasion and extension into the perithyroidal soft tissue associated with any of the tumors.
Figure 3.
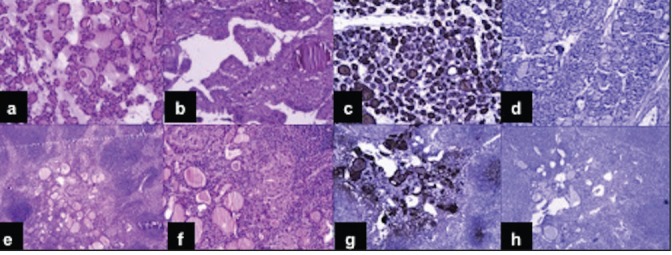
Histopathological examination showed (a) multiple large nodules in both lobes consistent with Hurthle cell adenoma, 10X, comprising of microfollicles lined by cuboidal cells showing abundant deeply eosinophilic cytoplasm. (b) Sub centimeter foci showing tubule-papillary architecture of papillary carcinoma (10X). (c,d) Immunohistochemistry analysis in thyroid lesions showing intense expression for thyroglobulin (10X) and no expression for PSA (10X). (e,f) A small pretracheal metastatic node from papillary thyroid carcinoma (4X and 10X respectively). (g,h) The node showed positive expression for thyroglobulin (10X) and negative expression for PSA negative (4X).
Discussion
PSMA based simultaneous PET/MRI is a novel imaging technique which has been used in diagnosis of recurrent prostate carcinoma.[1] PSMA uptake has been demonstrated in both non-prostatic neoplastic[2,3,4,5,6] and non-neoplastic lesions.[7,8] PSMA uptake is also seen in both benign[9] and malignant neoplasms of thyroid.[10,11,12] Although rare, metastatic spread to the thyroid gland from primary PCa has been reported in the past.[13,14] In this patient, metastases to the thyroid was a distinct possibility in view of widespread metastatic disease not observed in this case. So, in a case of PSMA avid thyroid lesion, it is important to differentiate metastases with primary thyroid neoplasm with biopsy before initiating further treatment.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest
Acknowledgment:
Pradeep Negi for technical help in study acquisition and preparation of manuscript
References
- 1.Afshar-Oromieh A, Haberkorn U, Schlemmer HP, Fenchel M, Eder M, Eisenhut M, et al. Comparison of PET/CT and PET/MRI hybrid systems using a 68Ga-labelled PSMA ligand for the diagnosis of recurrent prostate cancer: Initial experience. Eur J Nucl Med Mol Imaging. 2014;41:887–97. doi: 10.1007/s00259-013-2660-z. [DOI] [PubMed] [Google Scholar]
- 2.Huang YT, Fong W, Thomas P. Rectal Carcinoma on 68Ga-PSMA PET/CT. Clin Nucl Med. 2016;41:e167–8. doi: 10.1097/RLU.0000000000001072. [DOI] [PubMed] [Google Scholar]
- 3.Sasikumar A, Joy A, Nanabala R, Pillai MR, Thomas B. Vikraman KR, 68Ga-PSMA PET/CT imaging in primary hepatocellular carcinoma. Eur J Nucl Med Mol Imaging. 2016;43:795–6. doi: 10.1007/s00259-015-3297-x. [DOI] [PubMed] [Google Scholar]
- 4.Law WP, Fiumara F, Fong W, Miles KA. Gallium-68 PSMA uptake in adrenal adenoma. J Med Imaging Radiat Oncol. 2016;60:514–7. doi: 10.1111/1754-9485.12357. [DOI] [PubMed] [Google Scholar]
- 5.Nomura N, Pastorino S, Jiang P, Lambert G, Crawford JR, Gymnopoulos M, et al. Prostate specific membrane antigen (PSMA) expression in primary gliomas and breast cancer brain metastases. Cancer Cell Int. 2014;14:26. doi: 10.1186/1475-2867-14-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rischpler C, Maurer T, Schwaiger M, Eiber M. Intense PSMA-expression using 68Ga-PSMA PET/CT in a paravertebral schwannoma mimicking prostate cancer metastasis. Eur J Nucl Med Mol Imaging. 2016;43:193–4. doi: 10.1007/s00259-015-3235-y. [DOI] [PubMed] [Google Scholar]
- 7.Rowe SP, Deville C, Paller C, Cho SY, Fisherman EK, Pomper MG, et al. Uptake of 18F-DCFPyL in Paget's Disease of Bone, an Important Potential Pitfall in Clinical Interpretation of PSMA PET Studies. Tomography. 2015;1:81–4. doi: 10.18383/j.tom.2015.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kobe C, Maintz D, Fischer T, Drzezga A, Chang DH. Prostate-Specific Membrane Antigen PET/CT in Splenic Sarcoidosis. Clin Nucl Med. 2015;40:897–8. doi: 10.1097/RLU.0000000000000827. [DOI] [PubMed] [Google Scholar]
- 9.Kanthan GL, Drummond J, Schembri GP, Izard MA, Hsiao E. Follicular Thyroid Adenoma Showing Avid Uptake on 68Ga PSMA-HBED-CC PET/CT. Clin Nucl Med. 2016;41:331–2. doi: 10.1097/RLU.0000000000001084. [DOI] [PubMed] [Google Scholar]
- 10.Verburg FA, Krohn T, Heinzel A, Mottaghy FM, Behrendt FF. First evidence of PSMA expression in differentiated thyroid cancer using [68Ga] PSMA-HBED-CC PET/CT. Eur J Nucl Med Mol Imaging. 2015;42:1622–3. doi: 10.1007/s00259-015-3065-y. [DOI] [PubMed] [Google Scholar]
- 11.Sager S, Vatankulu B, Uslu L, Sonmezoglu K. Incidental Detection of Follicular Thyroid Carcinoma in Ga-68 PSMA PET/CT Imaging. J Nucl Med Technol. 2016;44:199–200. doi: 10.2967/jnmt.115.171660. [DOI] [PubMed] [Google Scholar]
- 12.Taywade SK, Damle NA, Bal C. PSMA Expression in Papillary Thyroid Carcinoma: Opening a New Horizon in Management of Thyroid Cancer.? Clin Nucl Med. 2016;41:e263–5. doi: 10.1097/RLU.0000000000001148. [DOI] [PubMed] [Google Scholar]
- 13.Selimoglu H, Duran C, Saraydaroglu O, Guclu M, Kiyici S, Ersoy C, et al. Prostate cancer metastasis to thyroid gland. Tumori. 2007;93:292–5. [PubMed] [Google Scholar]
- 14.Albsoul NM, Obeidat FN, Hadidy AM, Alzoubi MN, Taib AA, Shahait AD. Isolated multiple bilateral thyroid metastases from prostatic adenocarcinoma: Case report and literature review. Endocr Pathol. 2013;24:36–9. doi: 10.1007/s12022-013-9232-4. [DOI] [PubMed] [Google Scholar]


