Abstract
Background:
Busy care providers focus on the serious complications of postpartum period. This issue causes the seemingly trivial complications, such as mother's pains, fatigue, and psychological status, to be less taken into account. The study aimed to determine the effect of lavender oil aroma in the early hours of postpartum period on maternal pains, fatigue, and mood in primiparous mothers.
Methods:
This randomized clinical trial was conducted on 56 participants; 29 in intervention group and 27 in control group. The intervention group received lavender oil in three doses during the first 24 h after delivery. Sesame oil was used in the control group. Intensity of pain, fatigue, and distress level was measured by visual analog scale before and after the interventions. Besides, mood status was assessed through the positive and negative affect schedule.
Results:
The mean age of all the participants was 23.88 ± 3.88 years. After the first intervention and also in the tomorrow morning assessment, significant differences were found between the two groups regarding perineal pain (P = 0.004, P < 0.001), physical pain (P < 0.001), fatigue (P = 0.02, P < 0.001), and distress scores (P < 0.001). In addition, significant differences were found concerning the mean scores of positive (P < 0.001) and negative (P = 0.007, P < 0.001) moods between the two groups after the interventions. Repeated measures analyses showed that the two groups were significantly different over time in all the evaluated variables.
Conclusions:
Lavender oil aromatherapy starting in the first hours of postpartum period resulted in better physical and mood status compared to nonaromatic group.
Keywords: Fatigue, lavender oil aromatherapy, mood, perineal pain, postpartum
Introduction
The mothers who give birth in maternity wards are under the supervision of skilled personnel in the immediate postnatal period and are monitored regarding the life-threatening conditions, such as bleeding, hypertension, and infection.[1,2] In addition to fatal complications, mothers in the immediate postpartum period may suffer from some problems, such as perineal pain, back pain, uterine cramps, and fatigue. Busy care providers focus on the serious complications of postpartum period. This issue causes the seemingly trivial complications, such as mother's perineal pain, fatigue, and psychological status, to be less taken into account.[1,3,4] In addition, mothers may consider these problems as the natural consequences of labor and speak less about them.[5] Perineal pain as well as other physical pain in the postpartum period can lead to insomnia, fatigue, confusion, anxiety, delay in the formation of relationship between the mother and her baby, disability in caring about the newborn, and inappropriate body position during breastfeeding. In severe pain and immobility cases, there is also a risk of deep vein thrombosis.[5,6]
Perineal pain can be treated by a variety of oral analgesics, rectal suppositories, and topical anesthetics. In a previous study, only about 63% of the mothers described that painkillers were effective in relief of perineal pain.[3] In our society, sedative drugs such as mefenamic acid are routine care managements of pain such as perineal pain after delivery. Sedative drugs act in relative manners that need other complementary methods. Besides, these drugs have some serious effects that result in limiting consumption.
It should be noted that, in most cases in Iran, mediolateral incision is made for episiotomy and catgut thread is used for its repair, resulting in more perineal pain.[1,7] Therefore, a lot of women in Iran and other countries (with similar above-mentioned midwifery background) need to be relieved from perineal pain during the first 24 h postpartum.
Conventionally, fatigue and lack of energy have been accepted as the common consequences of childbirth in the postpartum period. In the past two decades, fatigue has been one of the five most important issues for women in the postpartum period. Fatigue is a condition that causes the mother to have negative feelings and be uncomfortable.[8,9]
Lavender is an aromatic plant that is widely used in aromatherapy. Researches have indicated that aromatherapy with lavender has anti-inflammatory, anti-depressant, hypnotic, sedative, muscle-relaxant, anti-bacterial, and anti-spasmodic effects.[10,11] Aromatherapy with lavender oil has been used to reduce pain and anxiety during labor, and mothers have generally evaluated this approach as an appropriate method.[12]
Considering the implementation of rooming-in method in most maternity wards, it is important that mothers experience less pain and fatigue, have a good mood to establish an appropriate emotional relationship with their infants in the early hours of postpartum period, and can breastfeed and take care of their infants. Obviously, supportive efforts from care providers result in an successful initiation of breastfeeding that causes it to be continued after release from hospital.[13] Discharge with better physical and mental conditions in turn improves women's quality of life.[14,15] Thus, the present study aims to assess the effect of lavender oil aroma in the early hours of postpartum period on maternal physical pains, fatigue, and mood in primiparous women.
Methods
Participants and setting
This clinical trial was conducted on 56 primiparous women with normal vaginal delivery in one educational hospital affiliated to Shiraz University of Medical Sciences. The participants were under the immediate postpartum care in the postpartum wards. Data collection was performed from the second half of April to late June 2014. This study was confirmed by the Ethics Committee of Shiraz University of Medical Sciences (code: CT91-6943). The investigation was also registered in the Iranian Registry of Clinical Trials as IRCT2014060910327N7.
The inclusion criteria of the study were vaginal delivery with episiotomy and without spinal or epidural anesthesia, singleton pregnancy, live and normal infant, aged 18–35 years, not suffering from severe chronic diseases such as cardiovascular and lung disease, at least 4 h later than delivery, perineal pain score ≥4 in visual analog scale (VAS), and having no history of allergy to lavender plant. On the other hand, in case the mothers were not willing to continue participation in the study, could not bear the smell of lavender essential oil, and were susceptible to complications such as hypertension, bleeding, and fever, they were excluded from the study.
In the postpartum ward, the researcher selected the participants based on the patients’ records and interviews. After description of the study objectives, the mothers were encouraged to participate in the study, and if they were willing, written informed consents were obtained from them. Due to the possible emergency problems in the first hour of postpartum, sampling was done after this period.
Tools and data collection
In the present study, physical pain was defined as back pain, muscle pain, and uterine cramps. In addition, perineal pain was considered as a pain in the external genitalia. Before the intervention, the primiparous mothers were asked to indicate the intensity of the above-mentioned pain by VAS. If the mothers showed pain intensity ≥4, they were enrolled into the study. A pain VAS scale is a 100 mm horizontal line, representing no pain at the commence and the worst possible pain at the end.[16]
A fatigue VAS scale, a 100-mm horizontal line quantifying fatigue between the anchors “no fatigue” and “fatigue as bad as can be, measured the fatigue.” With insertion of a spot on the line, the participant expressed how much fatigue she was experiencing at the study point time. Distress perception was also assessed by VAS, fixed with feeling rested at the beginning and completely distressed at the end.[17] In our study, before the first intervention, test-retest analyses showed the correlations of 0.93 and 0.90 for fatigue and peace perception, respectively.
Moreover, the mothers’ mood was evaluated by the Positive and Negative Affect Schedule (PANAS). This scale consisted of 10 items for assessing the negative moods and 10 items for evaluating the positive ones, which were mixed in the PANAS. The items of this questionnaire were responded through a Likert scale ranging from 1 to 5. Thus, the total scores of both positive and negative moods varied from 10 to 50.[18] It should be noted that the total scores of positive and negative statements were analyzed separately. In this study, for positive section of the PANAS, we obtained a Cronbach's alpha and a test-retest correlation value of 0.88 and 0.85, respectively. In addition, for negative section of the PANAS, a Cronbach's alpha and a test-retest correlation value of 0.87 and 0.89 were obtained, respectively.
Interventions
In this study, the participants were selected by convenience sampling. Then, they were randomly divided into a control and an intervention group through block randomization.
In the intervention group, lavender oil was utilized. Lavandula officinalis species was bought from the pharmacy of traditional medicine affiliated to Shiraz University of Medical Sciences and its essence was obtained using Apparatus Clevenger in the pharmacology laboratory of School of Medicine, Shiraz University of Medical Sciences. One percent lavender essential oil was provided by the laboratory technician. The researcher instilled five drops of lavender essential oil on a cotton ball and asked the participants to hold it about 20 cm from their nose for 10–15 min and breathe normally. One hour later, the participants’ physical pain, fatigue, and mood were evaluated. The intervention with lavender oil was repeated 6 h after the first intervention and at bed time. In the following morning before discharge, the participants’ physical pain, fatigue, distress, and mood were measured again. At present, there are no instructions in the Western countries in setting standards for essential oils, and oils are not regulated by the Food and Drug Administration. There is not a great amount of published rigorous research testing aromatherapy oils and techniques; therefore, consensus is lacking on these subjects. Researchers selected the dose and intervals of consumption anecdotally. Exactly 1 to 2% concentration of lavender oil was used intrapartum to manage labor pain and anxiety without any harm for mother or her fetus. Therefore, we followed this method in our study.[19]
The previous study showed that lavender aroma in infancy was not harmful.[20,21] However, in the present study, we used low concentration of lavender oil (1%), and for more caution, the mother was separated from her baby during the aromatherapy period.
In the control group, sesame oil was used as placebo similar to lavender oil in intervention group as mentioned above. Sesame oil was provided from Oila Company (manufactured in Tehran, Iran).
The participants were blinded for the types of the oils; therefore, the study was a single-blinded study. The two study groups received routine postpartum care including sedative drugs.
Sample size and statistical analysis
Based on a previous study,[22] considering α = 0.05 and power of 80%, and using the statistical formula, a 60-subject sample size was determined for the study.
The data were analyzed using SPSS statistical software version 16 (SPSS Inc., Chicago, IL, U.S.A). Besides, P < 0.05 was considered statistically significant. At first, normality of distribution of quantitative variables was assessed by one-sample Kolmogorov–Smirnov test. If the variables followed normal distribution, independent samples t-test was used; otherwise, its equivalent nonparametric test, i.e., Mann–Whitney U-test, was employed. In addition, repeated measures analysis of covariance was applied to determine changes over time in each group. Chi-square test was also used for investigation of the qualitative variables.
Results
In this study, 76 primiparous women were interviewed, 62 of whom were eligible for the study and six women were excluded from the study due to discharge from the hospital before the end of the study. After all, the data of 56 participants (29 in the intervention group and 27 in the control group) were analyzed.
The participants’ age ranged from 18 to 32 years, with a mean age of 23.88 ± 3.88 years. In addition, 51.8% (n = 29) of the participants had primary and high school education, 33.9% (n = 19) had high school diplomas, and 14.3% (n = 8) had university education. All the participants were homemakers. It should be noted that the two groups were matched regarding age (P = 0.39) and education level (P = 0.54).
The baseline severity of perineal pain was 70.55 ± 17.92 in all the participants with a minimum and maximum of 40 and 100, respectively. Before the intervention, the mean perineal pain was not statistically different between the two groups (P = 0.82). However, a significant difference was observed between the two groups after the first intervention and at the tomorrow morning assessment. The intragroup comparisons showed that the intensity of perineal pain differed only in the intervention group over time (P < 0.001) [Table 1]. According to Figure 1, two groups were different with regard to perineal pain along time.
Table 1.
Comparison of the perineal and physical pain, fatigue, distress, and Positive and Negative Affect Schedule measurements between the two groups
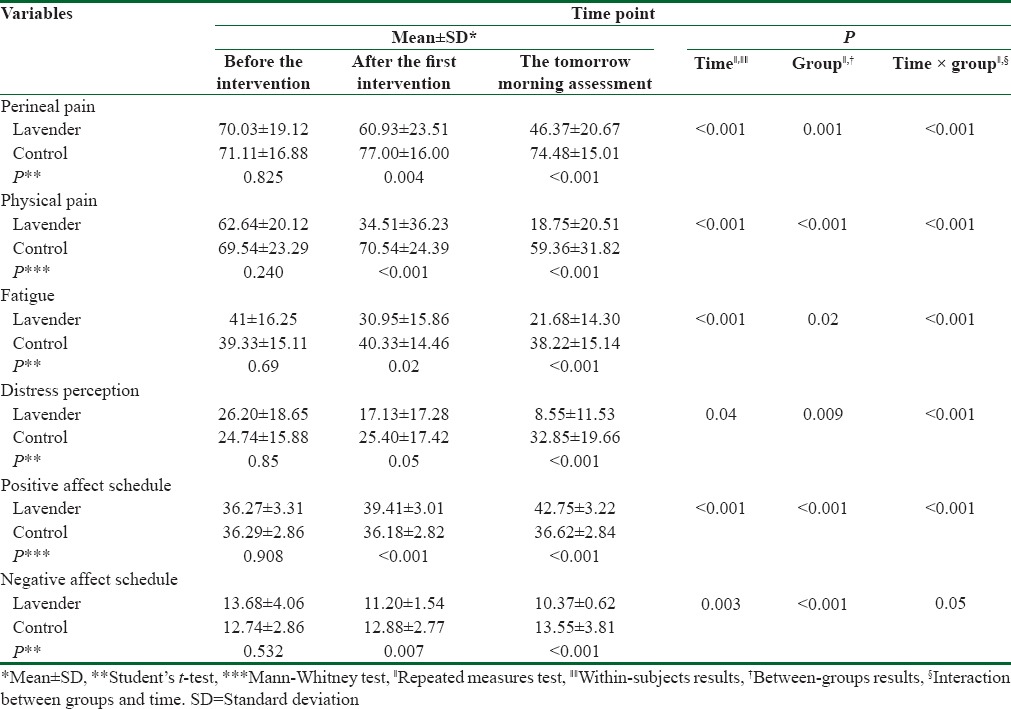
Figure 1.
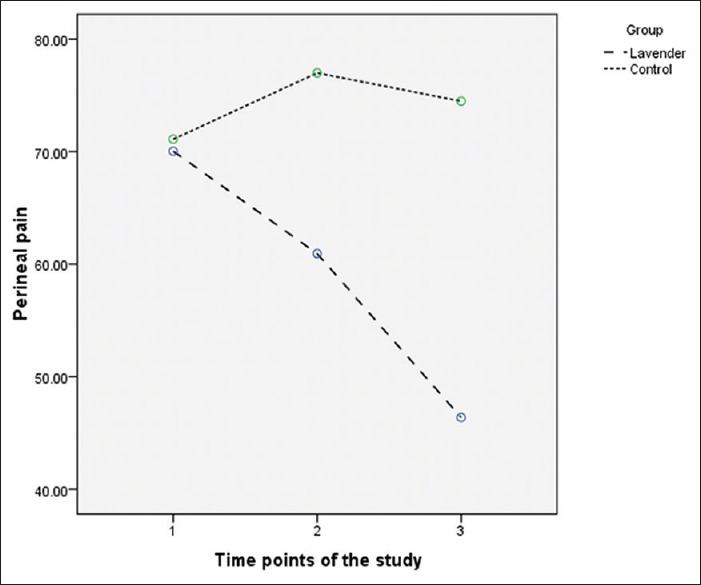
Within-groups comparison related to the perineal pain scores: The results showed, between the two groups, the difference regarding over-time reduction of the perineal pain scores was statistically significant (P < 0.001)
The baseline severity of other physical pain, such as back pain and uterine cramps, was 62.64 ± 20.12 and 69.54 ± 23.29 in the intervention and control groups, respectively, and the difference was not statistically significant. Nevertheless, a statistically significant difference was found between the two groups after the interventions (P < 0.001) [Table 1].
The baseline severity of fatigue in the whole sample was 40.19 ± 15.59, with a minimum and maximum of 8 and 88, respectively. Before the intervention, no significant difference was observed between the intervention and control groups regarding the intensity of fatigue (P = 0.69). However, significant differences were observed between the two groups after the first intervention and at the tomorrow morning assessment (P = 0.02 and P < 0.001, respectively). The intragroup comparisons also showed that the intensity of fatigue followed a descending trend in the lavender oil group, but not in control group (P < 0.001 and P = 0.44, respectively) [Table 1 and Figure 2]. Between-group analyses showed that mean scores of distress in the lavender oil group were significantly lower compared to the control group at the tomorrow morning assessment (P < 0.001). Besides, the two groups were significantly different along time [Table 1]. The highest scores of positive and negative moods were 42/50 and 24/50, respectively. The mean score of negative moods was 13.23 ± 3.53 at baseline and 11.91 ± 3.10 in the tomorrow morning assessment. These measures were, respectively, obtained as 36.28 ± 3.07 and 39.80 ± 4.32 for positive moods. The results showed no significant difference between the intervention and control groups concerning the baseline negative and positive mood scores. After the first intervention and at the tomorrow morning assessment, however, significant differences were found between the two groups regarding the negative and the positive mood scores [Table 1]. Moreover, the intragroup comparisons showed that the intervention group's positive and negative mood scores significantly differed in the three assessment times (P < 0.001) [Table 1]. The results of repeated measures analysis (time effect, group effect, and interaction between time and groups) were shown in Table 1 for all variables.
Figure 2.
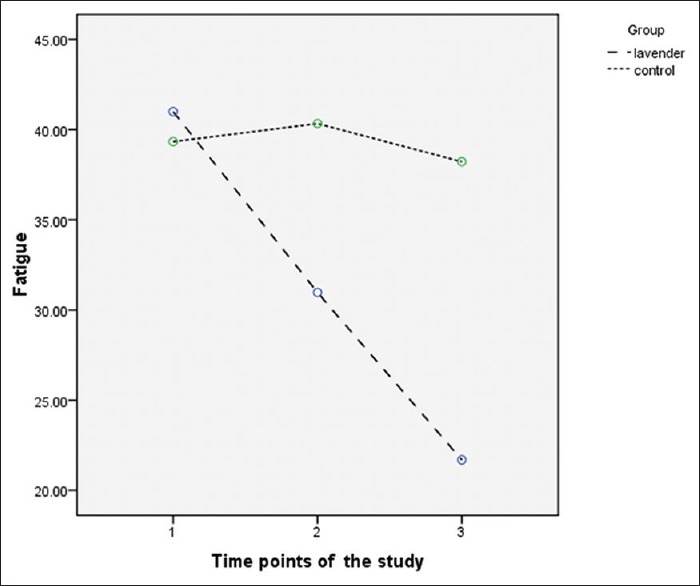
Within-groups comparison related to the fatigue scores: The results showed, between the two groups, the difference regarding over-time reduction of the fatigue scores was statistically significant (P < 0.001)
Discussion
The result showed that aromatherapy with lavender oil was effective in reducing pain, fatigue, and distress and could improve maternal mood. One of the strong points of this study was including a control group. Although mother's physical pain and fatigue may decrease by resting after delivery, the effectiveness of the intervention was determined after comparison with the control group. In addition, over-time analyses (repeated measures analyses) revealed that pain, fatigue, and distress decreased as well as mothers’ mood improved in the intervention group. Nevertheless, the following points should be noted in the control group. In this group, the severity of perineal pain increased after the first intervention and in the tomorrow morning assessment compared to before the intervention; however, the differences were not statistically significant. Furthermore, the mean intensity of fatigue importantly increased in the tomorrow morning assessment compared to before the intervention.
The negative mood scores in the PANAS questionnaire could vary from 10 to 50. Overall, our participants had a low mean score of negative moods, in such a way that the mean scores of negative moods were 13.23 ± 3.53 and 11.91 ± 3.10 before the intervention and in the tomorrow morning assessment, respectively. These low mean scores might have resulted from the euphoria of motherhood. In contrast to the intervention group, the mean scores of negative moods followed a rising trend in the control group over time. However, the differences were not statistically significant. The positive mood scores showed no significant changes in the control group over time. These findings also demonstrated the effectiveness of lavender essential oil.
We could find no similar studies investigating the effect of inhalation aromatherapy on pain relief, reduction of fatigue, and improvement of mood during the first 24 h after vaginal childbirth. However, several studies have been conducted on postcesarean delivery pain and showed that lavender aromatherapy could relieve postcesarean delivery pain.[23,24,25]
Furthermore, the effects of lavender oil sitz bath on perineal pain have been assessed in some studies. The results of the study by Sheikhan et al. showed that lavender oil sitz bath group experienced less perineal pain at 4 h and 5 days after delivery.[22] Nevertheless, Vakilian et al. reported that the intensity of perineal pain in the lavender oil sitz bath group was not less than that of the control group.[26] Different study population and accuracy in sample selection could lead to obtain dissimilar results in these studies.
Postpartum fatigue starts soon after delivery, gets more intense as time progresses, and may not be recovered spontaneously.[27] Fatigue can interfere in the activities of the new mothers and may also expose them to postpartum blues and depression. Fatigue can occur due to various factors, such as length of labor, type of delivery, postpartum hemorrhage, perineal pain, and other physical pain.[8] By shortening the duration of postpartum hospitalization, health-care providers have lower opportunity to evaluate and manage the above-mentioned complication; therefore, the first 24 h after delivery is a critical time point.
In the study conducted by Lee, aromatherapy with lavender oil inhalation was used 6 days after delivery to reduce fatigue and improve sleep. Aromatherapy was given by a necklace from 2 to 8 pm. At the end, the intervention group reported less fatigue compared to the control group.[28]
Evidence has shown the importance of mother's mood in the 1st day postpartum and gives us an idea about the need for appropriate actions. A link between the maternal mood scores in the early days of postpartum and the mood scores at 4, 6, 8, and 12 weeks after birth has been reported.[29,30,31]
The prior studies using aromatherapy in the postpartum period and maternal mood were different from the present one with respect to aromatherapy methods and assessment instruments. These studies have shown the positive effect of aromatherapy on mood in the postpartum period.[32,33] In the study by Imura et al., after 30 min aromatherapy massage, maternal blues and anxiety were measured. The anxiety scores of the aromatherapy massage group was significantly lower compared to the routine care group, and none of them had maternal blues.[32] Studies in other fields of medicine have also confirmed that lavender oil might reduce anxiety and enhance mood scores.[34,35,36]
The present study has some limitations as follows: the participants were selected from one maternity center. This group of participants may not be representative of the target population; sample size was small and we did not control some confounder variables such as duration of labor and psychological status during pregnancy; and our study was done in a short period (24 h after delivery) and the effect of such intervention was not assessed through the following days or weeks. Hence, longer studies are recommended to elucidate the effect of aromatherapy on maternal morbidities during the early and late postpartum periods.
Conclusions
In addition to the serious complications of labor and delivery that may be fatal for mothers during the first 24 h postpartum, other complications, such as physical pain and fatigue, may also upset the mothers and decrease the quality of their performance. To the best of our knowledge, this study was the first to examine the effectiveness of inhalation aromatherapy on the mothers’ perineal and physical pain, fatigue, distress, and mood during the immediate postpartum period. The findings showed that inhalation aromatherapy practice in the early hours of postpartum could reduce the mothers’ pain and fatigue and improve their mood.
Financial support and sponsorship
The study was financially supported by the Research Vice-chancellor of Shiraz University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This paper was extracted from Ms. Mahsa Shiravani's M.S. thesis in midwifery approved by Shiraz University of Medical Sciences (proposal no. 92-6943). Thanks also goes to all the participants who took part in this research.
References
- 1.Cunningham FG, Levono KJ, Bloom SL, Hauth JC, Rouse DJ, Spoong CY. Williams obstetrics. 23th ed. Ch 17, Sec 4. New York: The McGraw-Hill Companies; 2010. [Google Scholar]
- 2.Walsh D. A review of evidence around postnatal care and breastfeeding. Obstet Gynaecol Reprod Med. 2011;21:346–50. [Google Scholar]
- 3.East CE, Sherburn M, Nagle C, Said J, Forster D. Perineal pain following childbirth: Prevalence, effects on postnatal recovery and analgesia usage. Midwifery. 2012;28:93–7. doi: 10.1016/j.midw.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Yelland J, McLachlan H, Forster D, Rayner J, Lumley J. How is maternal psychosocial health assessed and promoted in the early postnatal period? Findings from a review of hospital postnatal care in Victoria, Australia. Midwifery. 2007;23:287–97. doi: 10.1016/j.midw.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Amorim Francisco A, Junqueira Vasconcellos de Oliveira SM, Barbosa da Silva FM, Bick D, Gonzalez Riesco ML. Women's experiences of perineal pain during the immediate postnatal period: A cross-sectional study in Brazil. Midwifery. 2011;27:e254–9. doi: 10.1016/j.midw.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 6.Way S. A qualitative study exploring women's personal experiences of their perineum after childbirth: Expectations, reality and returning to normality. Midwifery. 2012;28:e712–9. doi: 10.1016/j.midw.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Räisänen S, Vehviläinen-Julkunen K, Heinonen S. Need for and consequences of episiotomy in vaginal birth: A critical approach. Midwifery. 2010;26:348–56. doi: 10.1016/j.midw.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Taylor J, Johnson M. How women manage fatigue after childbirth. Midwifery. 2010;26:367–75. doi: 10.1016/j.midw.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Troy NW, Dalgas-Pelish P. The effectiveness of a self-care intervention for the management of postpartum fatigue. Appl Nurs Res. 2003;16:38–45. doi: 10.1053/apnr.2003.50001. [DOI] [PubMed] [Google Scholar]
- 10.Lee MS, Choi J, Posadzki P, Ernst E. Aromatherapy for health care: An overview of systematic reviews. Maturitas. 2012;71:257–60. doi: 10.1016/j.maturitas.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 11.Abuhamdah S, Chazot PL. Lemon balm and lavender herbal essential oils: Old and new ways to treat emotional disorders? Curr Anaesth Crit Care. 2008;19:221–6. [Google Scholar]
- 12.Pollard K. Introducing aromatherapy as a form of pain management into a delivery suite. J Assoc Chart Physiotherapists Womens Health. 2008;103:12–6. [Google Scholar]
- 13.Brand E, Kothari C, Stark MA. Factors related to breastfeeding discontinuation between hospital discharge and 2 weeks postpartum. J Perinat Educ. 2011;20:36–44. doi: 10.1891/1058-1243.20.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atlantis E, Chow CM, Kirby A, Singh MF. An effective exercise-based intervention for improving mental health and quality of life measures: A randomized controlled trial. Prev Med. 2004;39:424–34. doi: 10.1016/j.ypmed.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Connell J, Brazier J, O’Cathain A, Lloyd-Jones M, Paisley S. Quality of life of people with mental health problems: A synthesis of qualitative research. Health Qual Life Outcomes. 2012;10:138. doi: 10.1186/1477-7525-10-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8:1153–7. doi: 10.1111/j.1553-2712.2001.tb01132.x. [DOI] [PubMed] [Google Scholar]
- 17.Wolfe F. Fatigue assessments in rheumatoid arthritis: Comparative performance of visual analog scales and longer fatigue questionnaires in 7760 patients. J Rheumatol. 2004;31:1896–902. [PubMed] [Google Scholar]
- 18.Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol. 2004;43:245–65. doi: 10.1348/0144665031752934. [DOI] [PubMed] [Google Scholar]
- 19.Tillett J, Ames D. The uses of aromatherapy in women's health. J Perinat Neonatal Nurs. 2010;24:238–45. doi: 10.1097/JPN.0b013e3181ece75d. [DOI] [PubMed] [Google Scholar]
- 20.Razaghi N, Sadat Hoseini AS, Aemmi SZ, Mohebbi T, Boskabadi H. The effects of lavender scent on pain of blood sampling in term neonates. Int J Pediatr. 2015;3:535–41. doi: 10.1016/j.ctim.2019.102289. [DOI] [PubMed] [Google Scholar]
- 21.Çetinkaya B, Basbakkal Z. The effectiveness of aromatherapy massage using lavender oil as a treatment for infantile colic. Int J Nurs Pract. 2012;18:164–9. doi: 10.1111/j.1440-172X.2012.02015.x. [DOI] [PubMed] [Google Scholar]
- 22.Sheikhan F, Jahdi F, Khoei EM, Shamsalizadeh N, Sheikhan M, Haghani H. Episiotomy pain relief: Use of lavender oil essence in primiparous Iranian women. Complement Ther Clin Pract. 2012;18:66–70. doi: 10.1016/j.ctcp.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 23.Olapour A, Behaeen K, Akhondzadeh R, Soltani F, Al Sadat Razavi F, Bekhradi R. The effect of inhalation of aromatherapy blend containing lavender essential oil on cesarean postoperative pain. Anesth Pain Med. 2013;3:203–7. doi: 10.5812/aapm.9570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hadi N, Hanid AA. Lavender essence for post-cesarean pain. Pak J Biol Sci. 2011;14:664–7. doi: 10.3923/pjbs.2011.664.667. [DOI] [PubMed] [Google Scholar]
- 25.Sobhani A, Sharmi H. Effect of lavender oil on pain relief after cesarean section. J Gilan Med Univ. 2002;16:80–6. [Google Scholar]
- 26.Vakilian K, Atarha M, Bekhradi R, Chaman R. Healing advantages of lavender essential oil during episiotomy recovery: A clinical trial. Complement Ther Clin Pract. 2011;17:50–3. doi: 10.1016/j.ctcp.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 27.Taylor J, Johnson M. The role of anxiety and other factors in predicting postnatal fatigue: From birth to 6 months. Midwifery. 2013;29:526–34. doi: 10.1016/j.midw.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 28.Lee SH. Effects of aroma inhalation on fatigue and sleep quality of postpartum mothers. Korean J Women Health Nurs. 2004;10:235–43. [Google Scholar]
- 29.Yamashita H, Yoshida K, Nakano H, Tashiro N. Postnatal depression in Japanese women. Detecting the early onset of postnatal depression by closely monitoring the postpartum mood. J Affect Disord. 2000;58:145–54. doi: 10.1016/s0165-0327(99)00108-1. [DOI] [PubMed] [Google Scholar]
- 30.Hannah P, Adams D, Lee A, Glover V, Sandler M. Links between early post-partum mood and post-natal depression. Br J Psychiatry. 1992;160:777–80. doi: 10.1192/bjp.160.6.777. [DOI] [PubMed] [Google Scholar]
- 31.Adewuya AO. Early postpartum mood as a risk factor for postnatal depression in Nigerian women. Am J Psychiatry. 2006;163:1435–7. doi: 10.1176/ajp.2006.163.8.1435. [DOI] [PubMed] [Google Scholar]
- 32.Imura M, Misao H, Ushijima H. The psychological effects of aromatherapy-massage in healthy postpartum mothers. J Midwifery Womens Health. 2006;51:e21–7. doi: 10.1016/j.jmwh.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 33.Conrad P, Adams C. The effects of clinical aromatherapy for anxiety and depression in the high risk postpartum woman – A pilot study. Complement Ther Clin Pract. 2012;18:164–8. doi: 10.1016/j.ctcp.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 34.Lehrner J, Marwinski G, Lehr S, Johren P, Deecke L. Ambient odors of orange and lavender reduce anxiety and improve mood in a dental office. Physiol Behav. 2005;86:92–5. doi: 10.1016/j.physbeh.2005.06.031. [DOI] [PubMed] [Google Scholar]
- 35.Wu JJ, Cui Y, Yang YS, Kang MS, Jung SC, Park HK, et al. Modulatory effects of aromatherapy massage intervention on electroencephalogram, psychological assessments, salivary cortisol and plasma brain-derived neurotrophic factor. Complement Ther Med. 2014;22:456–62. doi: 10.1016/j.ctim.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 36.Cho MY, Min ES, Hur MH, Lee MS. Effects of aromatherapy on the anxiety, vital signs, and sleep quality of percutaneous coronary intervention patients in Intensive Care Units. Evid Based Complement Alternat Med 2013. 2013 doi: 10.1155/2013/381381. 381381. [DOI] [PMC free article] [PubMed] [Google Scholar]


