Abstract
Infected nonunions of tibia pose many challenges to the treating surgeon and the patient. Challenges include recalcitrant infection, complex deformities, sclerotic bone ends, large bone gaps, shortening, and joint stiffness. They are easy to diagnose and difficult to treat. The ASAMI classification helps decide treatment. The nonunion severity score proposed by Calori measures many parameters to give a prognosis. The infection severity score uses simple clinical signs to grade severity of infection. This determines number of surgeries and allows choice of hardware, either external or internal for definitive treatment. Co-morbid factors such as smoking, diabetes, nonsteroidal anti-inflammatory drug use, and hypovitaminosis D influence the choice and duration of treatment. Thorough debridement is the mainstay of treatment. Removal of all necrotic bone and soft tissue is needed. Care is exercised in shaping bone ends. Internal fixation can help achieve union if infection was mild. Severe infections need external fixation use in a second stage. Compression at nonunion site achieves union. It can be combined with a corticotomy lengthening at a distant site for equalization. Soft tissue deficit has to be covered by flaps, either local or microvascular. Bone gaps are best filled with the reliable technique of bone transport. Regenerate bone may be formed proximally, distally, or at both sites. Acute compression can fill bone gaps and may need a fibular resection. Gradual reduction of bone gap happens with bone transport, without need for fibulectomy. When bone ends dock, union may be achieved by vertical or horizontal compression. Biological stimulus from iliac crest bone grafts, bone marrow aspirate injections, and platelet concentrates hasten union. Bone graft substitutes add volume to graft and help fill defects. Addition of rh-BMP-7 may help in healing albeit at a much higher cost. Regeneration may need stimulation and augmentation. Induced membrane technique is an alternative to bone transport to fill gaps. It needs large amounts of bone graft from iliac crest or femoral canal. This is an expensive method physiologically and economically. Infection can resorb the graft and cause failure of treatment. It can be done in select cases after thorough eradication of infection. Patience and perseverance are needed for successful resolution of infection and achieving union.
Keywords: Infection, infection severity score, tibia, nonunion, regenerate bone, gap nonunion, antibiotic cement, bone transport, induced membrane technique
MeSH terms: Bone cements, bone regeneration, bone diseases, infections
INTRODUCTION
Infected nonunions of the tibia pose significant challenges for complete resolution and functional restoration. The infection is chronic and resistant to treatment. Bones are osteoporotic, deformed, sclerotic, and nonreactive at the nonunion site. There are formidable gaps to fill and large discrepancies to equalize. Tibia and fibula are differentially deficient. Stiffness of the ankle and knee creates functional handicaps. Prolonged treatment causes psychological, social, and economic hardships.
Tibia is subcutaneous and easily loses its soft tissue cover in trauma. True extent of the soft tissue loss may not be obvious externally as there may be significant soft tissue injury internally. The trend toward early internal fixation may add insult to injury and result in devascularization and florid infection.
Multiple failed surgeries add fibrosis, shortening, and a weakened morale. Many attempts at union exhaust bone graft donor sites. Osteoporosis results from prolonged inability to bear weight. Walking with supports prevents many from resuming work and forces social isolation. Hypoproteinemia and anemia result from sero-purulent wound discharge and chronic negative nitrogen balance. Poor appetite from immobility leads to malnourishment.
The bony gap results initially from acute traumatic bone loss at the site of the injury.1 High energy trauma causes gradually increasing zone of cellular death and the gap increases with successive debridements. Persistent infection eats away at the bone ends as do multiple attempts at union.
A multidisciplinary team approach2 works best. The surgical team needs skills in limb lengthening, deformity correction, and bone transport techniques.3,4,5,6,7,8 They must have the appetite for unglamorous task of debridement, perhaps repeatedly. Over and above the specific reconstructive techniques, they need patience and motivation to guide the patient through prolonged treatment. Local turn around flaps and microvascular free flaps may be needed for wound closure. Infectious diseases consultants help choose antibiotic therapy. Radiologists help in interpreting scans for planning debridement and resection.
Diagnosis and investigations
Infected nonunions are easy to diagnose and difficult to treat. Abnormal mobility is common in most gap nonunions of tibia. Many masquerade as malunions with little mobility, especially with a united fibula. Long leg films reveal extent of bony involvement, limb alignment, and length discrepancy. X-rays reveal sequestra, osteoporosis, deformities, and extent of the bony gap. Oblique X-rays can reveal the gap and confirm the diagnosis of a nonunion.
Raised acute phase reactant levels confirm active infection and help monitor prognosis. Routine tests reveal anemia, hypoproteinemia, and comorbidities. Serological marker testing for hepatitis B surface antigen,9 HIV,10 and hepatitis C11 is mandatory. Multiple transfusions and surgeries make these patients susceptible for viral infections. High chances of splash, pinprick, and contact with body fluids or sera of patients make the surgical team susceptible to developing infection. The risk is compounded by large open wounds needing multiple dressings and external fixation pin site care. This risk is continuous and prolonged. Patients are at higher risk for complications. They can be treated conservatively with a brace and made to walk partial weightbearing. Reconstructive surgery can be started after viral markers settle.
Classification of infected nonunions
Classification of infected nonunions should have prognostic value and help choose treatment. ASAMI classification is commonly used [Table 1]. Infection is classified as active or dormant. The nonunion severity score (NUSS) formulated by Calori et al.,12 helps to understand the difficulties in treating nonunions and considers many factors. Higher NUSS scores correlate with difficulty in achieving union. They recommend amputation over reconstruction for scores more than 75. NUSS [Table 2] grades infection only as previously infected or septic. It does not grade severity of infection.
Table 1.
ASAMI classification of nonunions
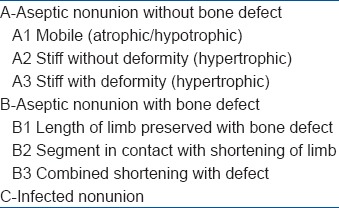
Table 2.
Nonunion severity score
Analyzing hundreds of infected nonunions has helped the author create a classification to quantify the severity of the infection. This could help in grading severity of infection and prognosis for the need for specific or repeated surgical treatment for the infection.
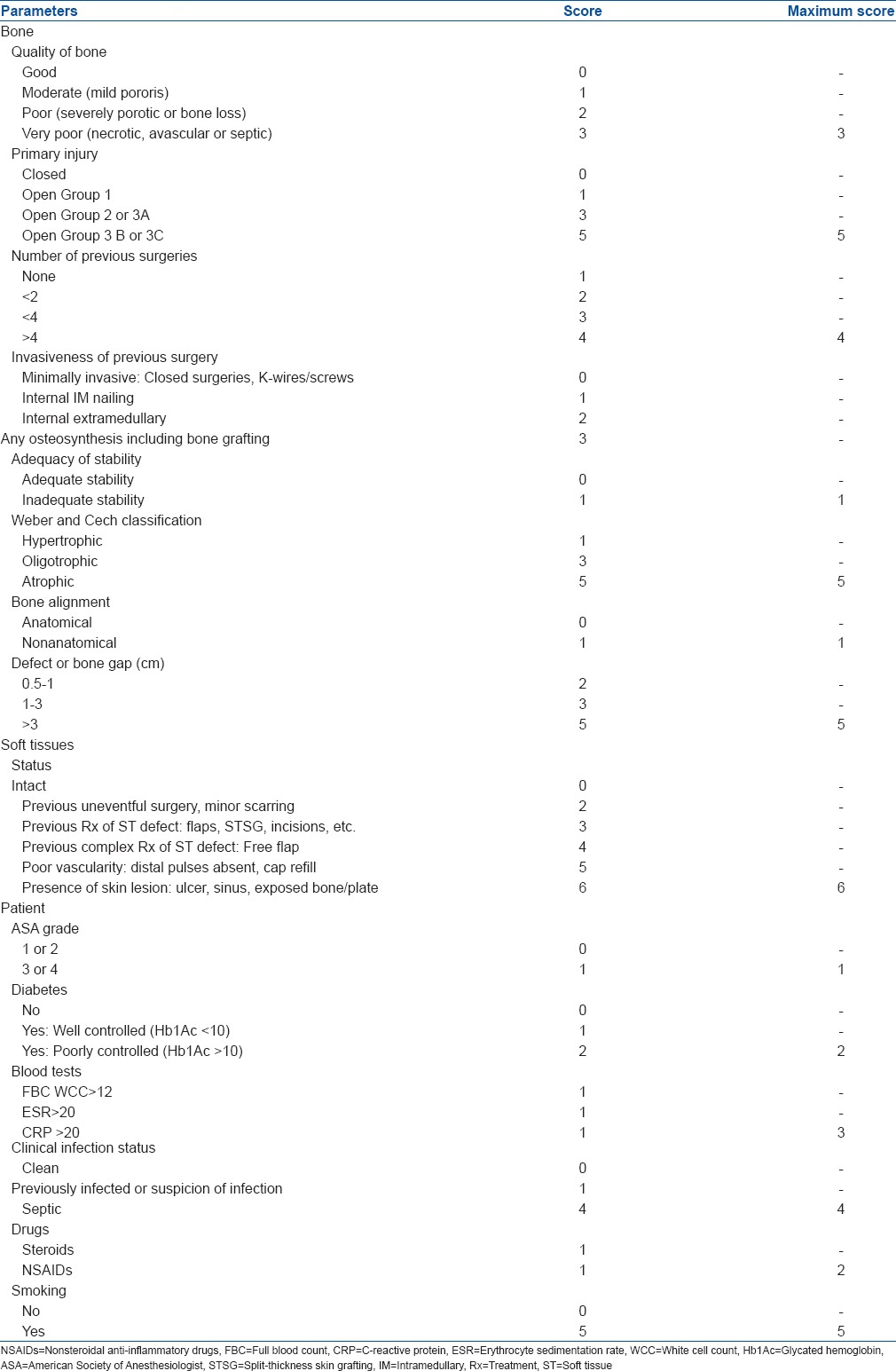
Infection severity score
The infection severity score (ISS)13 grades severity of infection by analyzing six clinical parameters. The classification system [Table 3] considers the history and clinical and radiological data. The score is easy to calculate. Maximum score is 25, which is converted to 100. Higher scores point to need for a second debridement and possibility of incomplete eradication or recurrence of infection. It could suggest using external rather than internal fixation in the second stage as a definitive modality to achieve union.
Table 3.
Infection severity score
Lower scores point to ease of eradication of the infection. Lower scores could allow definitive internal fixation in the second stage or external fixation in the same stage. ISS would help grade residual infection if any.
Control of infection by debridement
Debridement remains the cornerstone of treatment of infection.14,15 Large sinus tracks and infected scars need excision. Loose implants, broken screws, and locking bolts need removal. Granulation tissue and pus must be removed thoroughly. Curettes and scoops must be used to break loculi. Use flexible and rigid reamers to open the canal at both ends. Cultures are taken from the depths of the wound and antibiotics started only after sensitivity testing.
Debridement of soft tissue may lead to loss of cover which may best be filled with a muscle flap.16 The muscle flap brings much needed vascularity and helps in early union and complete eradication of infection.
Resecting bone from partial defects and irregularly shaped bony ends converts the nonunion site to matching horizontal surfaces. Large resections will create significant shortening. Regeneration in the tibia may be slow to form and harden; hence, it will be difficult to equalize limb lengths. Diabetics,17,18 anemic19 patients and smokers20 form bone poorly.
Infected tibial nonunions commonly have bony defects anteriorly and medially. This results in varus and recurvatum deformity. One option is to resect the minimum amount and telescope bony ends into one another for better contact and stability. Another method is to create oblique and matching bone ends, which will be compressed perpendicular to the plane of the bone ends. Excision is not mandatory for sclerotic bone ends.
Sustained compression can improve its vascularity, reduce sclerosis, and help it to unite.
Local antibiotic delivery systems
Removing fibrous tissue, necrotic bone, and opening the marrow canal improve blood supply and allow nutrients and antibiotics to reach the site. An antibiotic impregnated cement block obliterates dead space. It allows elution of the antibiotic in very high concentrations at the local site,21,22 in many multiples of the minimum inhibitory concentration (MIC). Acrylic bone cement is fashioned into intramedullary (IM) rods (with a core of a K wire or Rush nail/V nail). The rod is inserted from proximal portal after reaming. In deformed canals, one cement rod is inserted in the proximal canal and another in the distal through the nonunion site. Cement beads are strung on an SS wire in the extramedullary portion. Adding the antibiotic powder or liquid toward the end of polymerization ensures higher elution of antibiotics.23
The cement can be fashioned into a block to occupy the entire bony gap. Alternatively, the cement may be fashioned as a cylinder and Rush or Ender nails passed through it to secure the cement block to the bone.
Recently, a large diameter nail with a dual core of antibiotic cement around a metal rod has been used for compound fractures with great effect.24 This could be used for treatment of infected nonunions without significant bony gaps as well.
In smaller gaps, an absorbable carrier may make the second surgery unnecessary. The use of calcium sulfate25 cement paste or powder and absorbable chitosan polymer26 carriers are good alternatives. In mild infection, debridement and definitive surgeries may be performed together. With ISS score less than 25–30, after thorough debridement and local antibiotic delivery systems, one may take a chance with repeat internal fixation. Stable fixation with ABC rods itself can lead to union in about 10–15% of cases.
Using internal fixation increases risk of recurrent infection in patients with higher ISS scores. Combined surgery of debridement and external fixation may be safe when the ISS score is less than or equal to 40. Higher ISS scores warrant staged surgery.
Definitive surgery to achieve union
After control of infection, the tasks that remain are achieving union, correcting deformities, equalizing limb length, and filling defects and bone gaps. Union needs three basic requirements: stable fixation, biological stimulation, and restored function. Stable fixation can be achieved by any external or internal fixation devices. Iliac crest bone grafting is the gold standard27 and provides osteoconductive, osteoinductive, and osteogenic material to give biological stimulus. Grafts may also be harvested from the opposite upper tibia or trochanter.28 Posterolateral29 and central bone grafting30 achieve union by approaching the nonunion away from the infected site and achieving fusion between tibia and the fibula over the interosseous membrane. Older methods such as Phemister bone grafting with creation of thin osteoperiosteal flaps were also tried in potentially infected tibial nonunions by Jayaswal et al.,31 Open cancellous bone grafting known as Papineau method was popular especially in metaphyseal defects with minimal overlying soft tissue loss.32 A modified Papineau method was used by Kaushik et al.,33 who used a vacuum assisted closure (VAC) after debridement and after bone grafting till soft tissue cover surgery.
The Ilizarov fixator has revolutionized the treatment of infected tibial nonunions.34,35 It is minimally invasive and is able to reliably achieve union, lengthen and correct complex deformities, and allow the patient to walk. It gives sustained gradual compression at nonunion site, either in a vertical or in a horizontal mode [Figures 1 and 2]. Fibulectomy and sustained compression at nonunion site are the choice when there is minimal shortening.
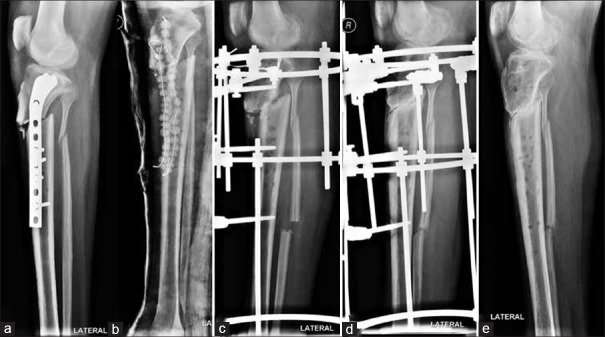
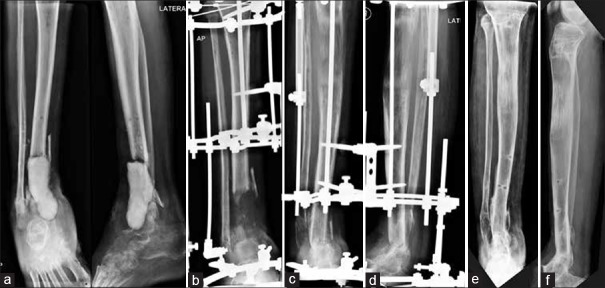
Figure 1.
Oblique view of leg bones with knee showing (a) upper tibial infected nonunion (b) After infection control (c) Ilizarov apparatus in situ (d). If vertical compression is given, it causes vertical displacement of nonunion ends. With the help of washers, horizontal compression achieved perpendicular to plane of nonunion (e) Good union. No loss of length
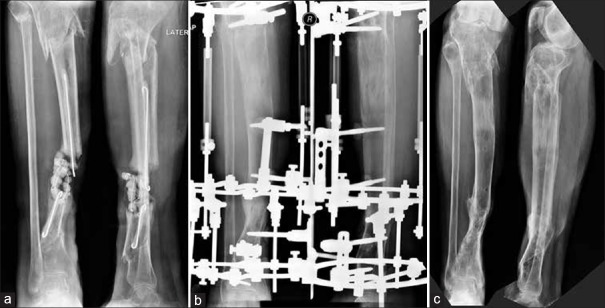
Figure 2.
X-ray leg bones with knee and ankle joint showing (a) Infected segmental nonunion after cure of infection with rods and beads (b) Ilizarov fixator in situ to achieve horizontal compression perpendicular to plane of nonunion (c) achieved union at both levels. Fibulaectomy done. No lengthening
Tibia can be lengthened through corticotomy if limb is short. Compression at the nonunion and lengthening at corticotomy site happen simultaneously for smaller discrepancies [Figure 3]. If the shortening is larger or the gap is greater, bone transport technique (sequential distraction-compression osteosynthesis) helps fill the gap. Many features of the Ilizarov fixator are shared by the Limb Reconstruction System (LRS) fixator, with added advantages of being surgeon and patient-friendly.36 Being monolateral is an advantage, but it is poorer in correcting complex deformities and fixation of osteoporotic bone with small fragments.
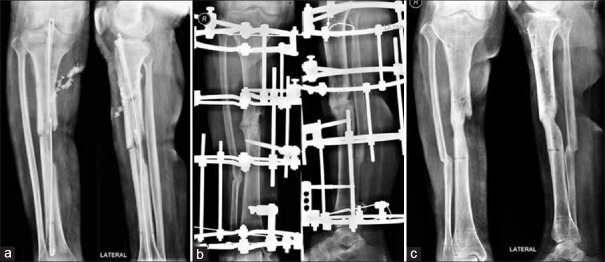
Figure 3.
X-ray anteroposterior and lateral views with knee and ankle joints showing (a) Infected nonunion lower tibia. Beads inserted (b) Ilizarov fixator applied. Acute compression at nonunion site done gradually at low rate hence no angular deformity at nonunion site despite an irregular shaped defect. Simultaneous lengthening at upper level to equalize lengths (c) Union achieved at distal end with good regenerate at proximal corticotomy site and no limb length discrepancy
RECONSTRUCTION OF BONY DEFECT AND GAP
After infection is controlled and the antibiotic carrier removed, filling the bony gap can happen by three strategies. Bone transport technique3,4,5,6,7,8 with its variations of technique and hardware is the established method. The alternative is to use the induced membrane technique described by Masquelet et al.,37,38,39,40,41 and fill up the gap with the help of vascularized bone grafts42,43 and/or substitutes.44,45
BONE TRANSPORT TECHNIQUE
Bone transport technique is one of the great inventions of the 20th century. It enables filling up large gaps of bone, in many instances without the need for bone grafting or bone graft substitutes. External devices such as the Ilizarov, LRS, and Taylor Spatial Frame (TSF)46 fixators are most commonly used. IM nails can guide the bone transport and reduce external fixation duration in select cases albeit with a high risk of residual or recurrent infection.47 Acute or subacute compression fills the bone gap if it is less than 3 cm. Lengthening can be performed at a distant tibial level.
Technique for tibia
Fixation is needed at three levels for a gap in the middle of the tibia: above the corticotomy, above the gap in the middle, and in the lower tibia. We prefer to include the femur in the assembly for better stability in treating a proximal tibial nonunion. With the gap in the lower third of the tibia or a lower tibial corticotomy, adding a foot frame improves stability. Fixation in the upper tibia can be achieved by one or two wires and two half pins. Half pins may not have a good hold in osteoporotic proximal tibiae. Three or four wires (at least two being olives) are needed to achieve good stability on one ring. Larger proximal fragment is fixed with three wires on the ring and a fourth dropped wire attached to a post. The middle or transported fragment is best fixed with two half pins. Distally, a combination of wires and half pins is needed to achieve stability.
For smaller gaps, acute compression may fill the defect, and larger gaps may be filled by gradual compression. A fibulectomy allows acute compression of tibial bone ends. Acute compression is followed by lengthening.48 Soft tissue defects can be filled acutely tilting the rings of the external fixator and angulating the bone inside.49 This allows suture or closure of the wound. After soft tissue healing, the rings are gradually straightened and bony deformity corrected. Bone transport gradually reduces the gap and allows the bones to come in contact without fibular resection [Figure 4].
Figure 4.
X-ray anteroposterior and lateral views showing (a) Infected gap in M3 tibia. Very poor fibrotic soft tissues. Free flap failed because recipient vessel was not found intact (b) Proximal tibial bone transport. Docking and compression without bone grafting (c) Using ilizarov technique achieved union. Good alignment
If the bony ends are uniform and matched in shape, sustained compression will promote union. Compression given at a high rate on irregular bony ends will result in angular deviation. Union without a deformity is possible by compressing at a much lower rate: i.e. 1 mm every 12 days [Figure 5].
Figure 5.
X-ray leg bones with knee joint anteroposterior and lateral views showing (a) Infected tibial nonunion. Irregular bony ends. Had we resected bone till achieving horizontal bony surfaces, it would have created a lot of shortening (b) we gave compression at rate of one-fourth mm twice a week to achieve compression but not cause an angular deviation. No bone grafting done (c) Sound union, after ilizarov construct removal
DOCKING SITE
Docking site malalignment is common and needs to be corrected. Using a TSF fixator46 will make it easy to correct malalignment at the docking site. There may be skin invagination and valley formation at docking site. The skin is undermined and released. An inferiorly based fasciocutaneous flap easily covers an upper or middle tibial soft tissue defect [Figure 6]. Diameter mismatch at docking site will give rise to tenuous union.
Figure 6.
(a) Clinical photograph showing severe soft tissue loss and bone loss in upper tibia. Debridement and beads seen. Inferiorly based fasciocutaneous flap was done for cover. X-ray leg bones with knee joint anteroposterior view (c) Clinical photograph showing full stent of frame across the knee. Femur included in frame for stability. (d) X-ray anteroposterior and lateral views showing that distal tibial corticotomy done for filling gap (e) X-ray anteroposterior and lateral views of leg bones with knee and ankle joint showing sound union. No deformity, no limb length discrepancy (LLD) and no infection persists
Union at the docking site can be hastened and cross-section area widened using iliac crest bone grafting.50 Injection of bone marrow aspirate at the nonunion site helps if iliac crest graft sites are exhausted. Adding demineralized bone matrix (DBM),51 beta tricalcium phosphate, or hydroxyapatite enhances the marrow aspirate. Platelet concentrates or gel can be used along with BMP if affordable.52 These modalities can be used repeatedly. The bony edges can be freshened50 and internal stability achieved by invaginating one end into the other to achieve faster healing at the nonunion site.
If the nonunion surfaces are oblique instead of being horizontal, compression is best achieved in a side to side manner. Fracture surfaces are compressed in a plane perpendicular to it. Another option for increasing vascularity at nonunion site is to drill several fine wire holes53 across the nonunion site. This creates new vascular channels and speeds up healing.
REGENERATE PROBLEMS
Regenerate bone at proximal end of tibia in adults may take a long time to form and harden. Instability of fixation causes the regenerate bone to deform in valgus and procurvatum. Stable initial fixation may deteriorate over time. After 5–6 months, wires and pins may loosen at their bony interface and may need augmentation. The increased resistance of scarred posterior soft tissues also leads to procurvatum at the regenerate. Adding bone grafts, bone marrow aspirate, or bisphosphonates54 improves regenerate quality. Smokers20 and those on nonsteroidal anti-inflammatory drugs55 tend to have poorer regenerate formation. The accordion manoeuvre56 consists of several cycles of compression and distraction at the regenerate site to improve bone quality. Hypovitaminosis D57 and anemia19 are the common causes of poor regenerate formation. If the soft tissue cover in proximal tibia is poor, thin, and adherent, it can lead to poor bone formation that does not form early and harden quickly.
Walking and resumption of employment also help in early healing. Significant whole body exercises are a part of physiotherapy at Prof. Ilizarov's Kurgan institute. An integral part of the treatment consists of making the patient walk for as many as 4–6 hr a day. The task of the surgical team is keeping the patient free from pain and task of the patient is to walk for several hours a day. This improves appetite and vascularity to the lower limb and promotes early healing.
Role of the fibula
The fibula tends to heal quickly and prevent adequate compression at the nonunion site. Watch for early union of fibula and resect it when the docking site is being opened, freshened, or grafted. A tibiofibular synostosis near the nonunion site prevents proper compression and delays the union. The fibula is fixed at its upper end to enhance stability and fixed at the lower level to maintain the lateral malleolus in the ankle joint.
MASQUELET-INDUCED MEMBRANE TECHNIQUE
Masquelet induced membrane technique is an alternative to bone transport. It does not regenerate bone but relies on grafting, and may be done with external or internal fixation. The first stage consists of debridement. An antibiotic cement block is inserted in the bony gap. A membrane similar to the periosteum forms over it. It has high cellular content and secretes growth factors. The membrane is at its most active at 3 weeks.37 Incise the membrane; enucleate the cement block; and fill the cavity by various grafts. Larger gaps can be filled with reamer-irrigator-aspirator (RIA) graft58,59 or graft harvested from the upper tibia. Bone marrow aspirate can be added as well. Beta-tricalcium phosphate or hydroxyapatite ceramic blocks to increase osteoconductivity and increase the volume of graft can be added. Soft tissues must be covered and the wound closed without tension. This may need local or free flaps, preferably before embarking on this method.
The chief drawback of this technique is the need for large amounts of bone graft. The iliac crest does not yield large amounts without morbidity. Graft sites may be exhausted. The RIA enables harvest of 60 to 80 cc of marrow graft from the opposite femoral canal. RIA graft can have high harvest morbidity. It may result in loss of large volumes of blood during harvest. Lowering of 2 to 3 g of Hb levels are known60,61 after RIA harvest. This precludes its use in anemic patients. The disposables for harvesting the RIA graft are expensive. It can result in fractures due to eccentric reaming of the canal.
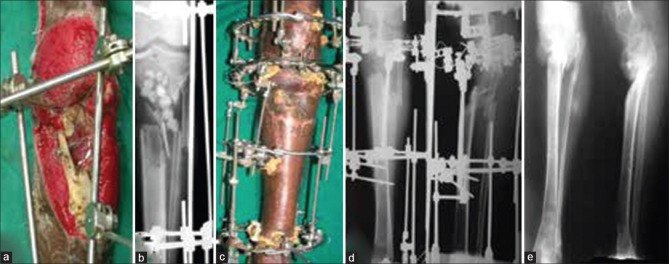
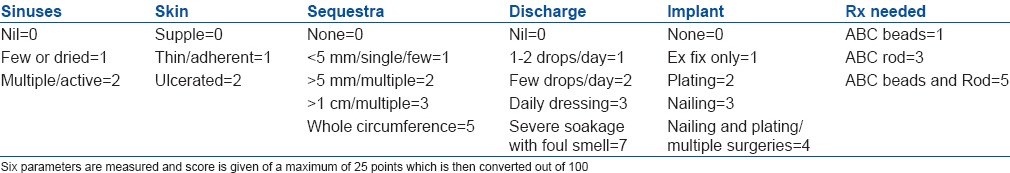
Recurrent infection leads to partial or complete loss of the graft. This has happened in the experience of the author as well [Figure 7].
Figure 7.
(a) X-ray leg bones with ankle joint anteriposterior and lateral views showing large gap after debridement. Cement block used (b-d) X-ray anterioposterior and lateral views showing reamer irrigator-aspirator graft inserted after nucleating cement block from membrane at 4 weeks and membrane sutured. Graft completely resorbed due to mild recrudescence of infection. Problem solved with Proximal to distal bone transport. Bone transport is most reliable method. Masquelet method may not work in all cases (e and f) X-ray anteroposterior and lateral views showing sound union
FREE VASCULARIZED FIBULAR GRAFT
Microvascular fibular grafting to bridge large gaps was very popular before the advent of the Ilizarov technique. A skin paddle helped cover soft tissue defects as well. The fibula and tibial diameter mismatch necessitated prolonged protection. Stress fractures were common and it took a long time for the fibula to hypertrophy. A recipient vessel far away from the injured zone for successful microvascular anastomosis is chosen. The fibula may face difficulties in uniting at one of the ends. Infection and anastomotic failure could result in significant morbidity. Combining the free vascularized fibula with the Ilizarov fixator combines benefits of both methods to fill up gaps in infected nonunions.42,43
ADVANTAGES AND BENEFITS OF THE BONE TRANSPORT TECHNIQUE
Bone transport techniques are a robust biological solution and can be used in all circumstances. Even if mild infection persists, it will not cause failure of the entire process as can happen with the induced membrane technique. Regenerate bone forms at a distant pristine level and is unaffected by any flare-up of infection at the nonunion site. The bone gap gradually decreases without high physiological or economic cost and morbidity. Majority of cases unite at the docking site by sustained compression, without bone grafting.62
Regenerate bone may form despite hypoproteinemia and anemia. Bone transport though prolonged is more certain of success. It is inexpensive physiologically and economically. It allows equalization of limb length and correction of deformities. It allows the patient to walk and resume work, which can partially offset the disadvantages of prolonged external fixation.
Alternative Philosophy for Treatment of Infected Nonunions
Hernigou et al.,63 state that theoretically one may consider the treatment of infected nonunions from two schools of thought. The treatment modalities outlined here all fall under the category of “eliminate infection first” strategy. Despite advantages, they cite need for great surgical expertise and significant complications. They propose method of “union first.” Here, bone marrow aspirate is concentrated in a cell separator and injected in the infected nonunion fracture site. This method is an accepted method in the treatment of aseptic nonunions.64 In their recent article, Hernigou iterates that the bone marrow aspirate concentrate also provides a high concentration of granulocytes and macrophages, which not only provide progenitors that stimulate bone healing but also cure the infection in the absence of antibiotic therapy. They used this modality only for gaps less than 15 mm. Severity of infection was not specified. As florid infection with a copious discharge and large sequestrae would definitely not respond to this “union first” method and nor would infected nonunions with large gaps.
Noninvasive Modalities
Electrical stimulation, low-intensity pulsed ultrasound, extracorporeal shock wave
“Bone growth stimulators,” including electrical stimulation, low-intensity pulsed ultrasound (LIPUS), and extracorporeal shock waves kindle interest for their packaged ease and noninvasive nature. They also happen to be a big market considering that at least 10% of all fractures would go on to delayed and nonunion.
However, Mollon et al.,65 in a meta-analysis of randomized controlled trials, could not show a significant impact of electromagnetic stimulation on long bone nonunions. Biglari et al.,66 found that a small number of their patients given LIPUS experienced successful treatment. They also conclude that its use resulted in a clear delay in the time of treatment.
Complications
Inadequate debridement and improper antibiotics lead to recrudescence of infection. It may also result from poor immune and nutritional status of the patient. Patient may need repeat debridement before definitive surgery or after successful union. Antibiotic therapy must follow culture and sensitivity testing. Antibiotic efficiency and penetration improve by adding enzyme preparations.67 A high protein, high caloric diet, high doses of Vitamin C,68,69 and parenteral nutrition could help.
Persistent nonunion after prolonged treatment is not uncommon. Sclerotic and nonreactive bony ends may not respond only to acute compression. Maintenance compression is needed. Biological stimulation may need to be added repeatedly. The diamond concept70,71,72 uses BMP which may be unaffordable. Unprocessed bone marrow aspirate can be injected repeatedly at nonunion site. Bone marrow is concentrated and a high number of colony forming unit fibroblasts of mononuclear cells are injected.64 Platelet concentrates can also be used to increase the local content of growth factors. These are easy, inexpensive and can be used repeatedly. Prolonged walking and resuming work also help.
Failure can be caused by fixator fatigue. New external fixation pins to enhance the strength of the fixation are added. Inability to see bone ends clearly in anteroposterior, lateral, and oblique x-rays is a surprising cause of failure to achieve union [Chart 1].
Chart 1.
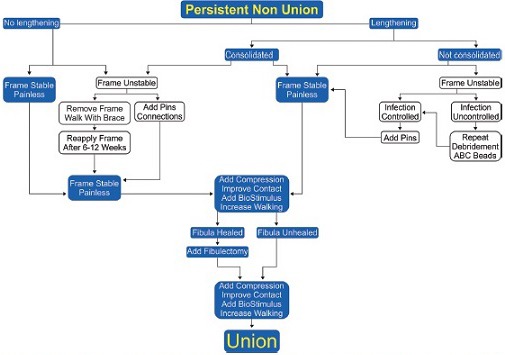
Algorithm for dealing with persistent nonunion while in the Ilizarov fixator. This can be a common problem. Augmentation of fixation is needed frequently with new pins. Fistulectomy helps achieve proper compression at Docking site or nonunion site. Biological augmentation is bone grafts, bone marrow injections, platelet concentrates and BG substitutes. BMP, if affordable
Controversies
Hybrid fixation is a controversial method for treating infected gap nonunions. A locking nail is inserted after debridement and enables rapid bone transport.73 Reduction in axial deviation and external fixation time and improved patient comfort are the advantages. Debridement followed by bone transport with EF may be immediately converted to IM nailing after docking.74 Recrudescence of infection is not uncommon in both methods. Using the ISS could help in determining which patients could safely have hybrid fixation.
CONCLUSION
The main principles of treatment of infected nonunions of the tibia are (1) radical and thorough debridement, (2) compression of nonunion by external fixation with lengthening or bone transport, (3) conversion to internal or hybrid fixation in less severe infections, and (4) augmentation of healing by bone grafting, bone marrow injections, platelet concentrates, and DBM. The Masquelet induced membrane technique holds promise and may offer good results in select cases.
Ilizarov fixator has advantages of continuous compression to achieve union, lengthening to fill bone gaps and equalize lengths, correct deformities, and resume walking and employment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Keating JF, Simpson AH, Robinson CM. The management of fractures with bone loss. J Bone Joint Surg Br. 2005 Feb;87(2):142–50. doi: 10.1302/0301-620x.87b2.15874. [DOI] [PubMed] [Google Scholar]
- 2.Bose D, Kugan R, Stubbs D, McNally M. Management of infected nonunion of the long bones by a multidisciplinary team. Bone Joint J. 2015;97-B:814–7. doi: 10.1302/0301-620X.97B6.33276. [DOI] [PubMed] [Google Scholar]
- 3.Dendrinos GK, Kontos S, Lyritsis E. Use of the Ilizarov technique for treatment of nonunion of the tibia associated with infection. J Bone Joint Surg Am. 1995;77:835–46. doi: 10.2106/00004623-199506000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Mora R, Pedrotti L, Bertani B, Quattrini F. Treatment of infected nonunions. In: Mora R, editor. Nonunion of the Long Bones: Diagnosis and Treatment with Compression-Distraction Techniques. New York: Springer; 2006. pp. 199–223. [Google Scholar]
- 5.Borzunov DY, Balaev PI, Subramanyam KN. Reconstruction by bone transport after resection of benign tumors of tibia: A retrospective study of 38 patients. Indian J Orthop. 2015;49:516–22. doi: 10.4103/0019-5413.164042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giannikas KA, Maganaris CN, Karski MT, Twigg P, Wilkes RA, Buckley JG. Functional outcome following bone transport reconstruction of distal tibial defects. J Bone Joint Surg Am. 2005;87:145–52. doi: 10.2106/JBJS.C.01550. [DOI] [PubMed] [Google Scholar]
- 7.Aronson J. Limb-lengthening, skeletal reconstruction, and bone transport with the Ilizarov method. J Bone Joint Surg Am. 1997;79:1243–58. doi: 10.2106/00004623-199708000-00019. [DOI] [PubMed] [Google Scholar]
- 8.Iacobellis C, Berizzi A, Aldegheri R. Bone transport using the Ilizarov method: A review of complications in 100 consecutive cases. Strategies Trauma Limb Reconstr. 2010;5:17–22. doi: 10.1007/s11751-010-0085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shapiro CN, Tokars JI, Chamberland ME. Use of the hepatitis-B vaccine and infection with hepatitis B and C among orthopaedic surgeons. The American Academy of Orthopaedic Surgeons Serosurvey Study Committee. J Bone Joint Surg Am. 1996;78:1791–800. doi: 10.2106/00004623-199612000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Wijesekera MP, Graham SM, Lalloo DG, Simpson H, Harrison WJ. Fracture management in HIV positive individuals: A systematic review. Int Orthop. 2016;40:2429–45. doi: 10.1007/s00264-016-3285-1. [DOI] [PubMed] [Google Scholar]
- 11.Javidan P, Walker RH. Take care with type C: Serious considerations in the selection of patients with hepatitis C for total joint arthroplasty. J Bone Joint Surg Am. 2015;97:e77. doi: 10.2106/JBJS.O.00929. [DOI] [PubMed] [Google Scholar]
- 12.Calori GM, Phillips M, Jeetle S, Tagliabue L, Giannoudis PV. Classification of nonunion: Need for a new scoring system? Injury. 2008;39(Suppl 2):S59–63. doi: 10.1016/S0020-1383(08)70016-0. [DOI] [PubMed] [Google Scholar]
- 13.Chaudhary Milind M. Infected gap nonunions of femur. In: Kulkarni GS, Babhulkar S, editors. Guidelines in Fracture Management, Nonunion in Long Bone II. Ch. 25. Noida: Thieme Publisher; 2016. pp. 309–24. [Google Scholar]
- 14.Calhoun JH. Schenker MD, et al., editors. Optimal timing of operative debridement: A known unknown: Commentary on an article by Mara L. “Does timing to operative debridement affect infectious complications in open long-bone fractures? A systematic review”. J Bone Joint Surg Am. 2012;94:e90. doi: 10.2106/JBJS.L.00239. [DOI] [PubMed] [Google Scholar]
- 15.Schenker ML, Yannascoli S, Baldwin KD, Ahn J, Mehta S. Does timing to operative debridement affect infectious complications in open long-bone fractures? A systematic review. J Bone Joint Surg Am. 2012;94:1057–64. doi: 10.2106/JBJS.K.00582. [DOI] [PubMed] [Google Scholar]
- 16.Lowenberg DW, Buntic RF, Buncke GM, Parrett BM. Long term results and costs of muscle flap coverage with Ilizarov bone transport in lower limb salvage. J Orthop Trauma. 2013;27:576–81. doi: 10.1097/BOT.0b013e31828afde4. [DOI] [PubMed] [Google Scholar]
- 17.Graves DT, Alblowi J, Paglia DN, O’Connor JP, Lin S. Impact of Diabetes on Fracture Healing. J Exp Clin Med. 2011;3(1):3–8. [Google Scholar]
- 18.Flouzat-Lachaniette CH, Heyberger C, Bouthors C, Roubineau F, Chevallier N, Rouard H, Herigou P. Osteogenic progenitors in bone marrow aspirates have clinical potential for tibial nonunions healing in diabetic patients. International Orthopaedics (SICOT) 2016;40:1375–1379. doi: 10.1007/s00264-015-3046-6. [DOI] [PubMed] [Google Scholar]
- 19.Varecka T.F., Wiesner L. The influence of hemorrhagic anemia on fracture healing. Orthopaedic Proceedings. 2012 May;94-B(SUPP XXI):60. [Google Scholar]
- 20.Patel RA, Wilson RF, Patel PA, Palmer RM. The effect of smoking on bone healing: A systematic review. Bone Joint Res. 2013;2:102–11. doi: 10.1302/2046-3758.26.2000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bistolfi A, Massazza G, Verné E, Massè A, Deledda D, Ferraris S, et al. Antibiotic-loaded cement in orthopedic surgery: A review. ISRN Orthop 2011. 2011 doi: 10.5402/2011/290851. 290851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gogia JS, Meehan JP, Di Cesare PE, Jamali AA. Local antibiotic therapy in osteomyelitis. Semin Plast Surg. 2009;23:100–7. doi: 10.1055/s-0029-1214162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang YH, Tai CL, Hsu HY, Hsieh PH, Lee MS, Ueng SW. Liquid antibiotics in bone cement: An effective way to improve the efficiency of antibiotic release in antibiotic loaded bone cement. Bone Joint Res. 2014;3:246–51. doi: 10.1302/2046-3758.38.2000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Craveiro-Lopes N. Treatment of open fractures of the tibia with locked intramedullary nail with a core release of antibiotics (Safe Dualcore Universal). Comparative study with a standard locked intramedullary nail. J Limb Lengthening Reconstr. 2016;2:17–22. [Google Scholar]
- 25.Ślósarczyk A, Czechowska J, Paszkiewicz Z, Zima A. New bone implant material with calcium sulfate and Ti modified hydroxyapatite. J Achiev Mater Manuf Eng. 2010;43:170–7. [Google Scholar]
- 26.Noel SP, Courtney H, Bumgardner JD, Haggard WO. Chitosan films: A potential local drug delivery system for antibiotics. Clin Orthop Relat Res. 2008;466:1377–82. doi: 10.1007/s11999-008-0228-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones CB, Mayo KA. Nonunion treatment: Iliac crest bone graft techniques. J Orthop Trauma. 2005;19(10 Suppl):S11–3. doi: 10.1097/00005131-200511101-00004. [DOI] [PubMed] [Google Scholar]
- 28.Myeroff C, Archdeacon M. Autogenous bone graft: Donor sites and techniques. J Bone Joint Surg Am. 2011;93:2227–36. doi: 10.2106/JBJS.J.01513. [DOI] [PubMed] [Google Scholar]
- 29.Simon JP, Stuyck J, Hoogmartens M, Fabry G. Posterolateral bone grafting for nonunion of the tibia. Acta Orthop Belg. 1992;58:308–13. [PubMed] [Google Scholar]
- 30.Ryzewicz M, Morgan SJ, Linford E, Thwing JI, de Resende GV, Smith WR. Central bone grafting for nonunion of fractures of the tibia: A retrospective series. J Bone Joint Surg Br. 2009;91:522–9. doi: 10.1302/0301-620X.91B4.21399. [DOI] [PubMed] [Google Scholar]
- 31.Jayaswal A, Bhan S, Dave PK, Chandra P. Modified Phemister grafting in potentially infected nonunion of tibial shaft fractures. Int Surg. 1985;70:67–70. [PubMed] [Google Scholar]
- 32.May JW, Jr, Jupiter JB, Weiland AJ, Byrd HS. Clinical classification of posttraumatic tibial osteomyelitis. J Bone Joint Surg Am. 1989;71:1422–8. [PubMed] [Google Scholar]
- 33.Kaushik SK, Solanki B, Pathania VP, Khan A. Outcome of modified Papineau technique with vacuum-assisted closer system in the treatment of chronic osteomyelitis and infected nonunion of tibia. Int J Sci Study. 2016;3:231–4. [Google Scholar]
- 34.Baruah RK. Ilizarov methodology for infected nonunion of the Tibia: Classic circular transfixion wire assembly vs. hybrid assembly. Indian J Orthop. 2007;41:198–203. doi: 10.4103/0019-5413.33682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kanakaris NK, Tosounidis TH, Giannoudis PV. Surgical management of infected nonunions: An update. Injury. 2015;46(Suppl 5):S25–32. doi: 10.1016/j.injury.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 36.Rohilla R, Wadhwani J, Devgan A, Singh R, Khanna M. Prospective randomised comparison of ring versus rail fixator in infected gap nonunion of tibia treated with distraction osteogenesis. Bone Joint J. 2016;98-B:1399–405. doi: 10.1302/0301-620X.98B10.37946. [DOI] [PubMed] [Google Scholar]
- 37.Pelissier P, Masquelet AC, Bareille R, Pelissier SM, Amedee J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthop Res. 2004;22:73–9. doi: 10.1016/S0736-0266(03)00165-7. [DOI] [PubMed] [Google Scholar]
- 38.Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am. 2010 Jan;41(1):27–37. doi: 10.1016/j.ocl.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 39.El-Alfy BS, Ali AM. Management of segmental skeletal defects by the induced membrane technique. Indian J Orthop. 2015;49:643–8. doi: 10.4103/0019-5413.168757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Scholz AO, Gehrmann S, Glombitza M, Kaufmann RA, Bostelmann R, Flohe S, et al. Reconstruction of septic diaphyseal bone defects with the induced membrane technique. Injury. 2015;46(Suppl 4):S121–4. doi: 10.1016/S0020-1383(15)30030-9. [DOI] [PubMed] [Google Scholar]
- 41.Aho OM, Lehenkari P, Ristiniemi J, Lehtonen S, Risteli J, Leskelä HV. The mechanism of action of induced membranes in bone repair. J Bone Joint Surg Am. 2013;95:597–604. doi: 10.2106/JBJS.L.00310. [DOI] [PubMed] [Google Scholar]
- 42.Kovoor CC, Jayakumar R, George V, Padmanabhan V, Guild A, Viswanath S. Vascularized fibular graft in infected tibial bone loss. Indian J Orthop. 2011;45:330–5. doi: 10.4103/0019-5413.82337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Semaya Ael-S, Badawy E, Hasan M, El-Nakeeb RM. Management of posttraumatic bone defects of the tibia using vascularised fibular graft combined with Ilizarov external fixator. Injury. 2016;47:969–75. doi: 10.1016/j.injury.2016.01.033. [DOI] [PubMed] [Google Scholar]
- 44.De Long WG, Jr, Einhorn TA, Koval K, McKee M, Smith W, Sanders R, et al. Bone grafts and bone graft substitutes in orthopaedic trauma surgery. A critical analysis. J Bone Joint Surg Am. 2007;89:649–58. doi: 10.2106/JBJS.F.00465. [DOI] [PubMed] [Google Scholar]
- 45.Finkemeier CG. Bone-grafting and bone-graft substitutes. J Bone Joint Surg Am. 2002;84-A:454–64. doi: 10.2106/00004623-200203000-00020. [DOI] [PubMed] [Google Scholar]
- 46.Rozbruch SR, Pugsley JS, Fragomen AT, Ilizarov S. Repair of tibial nonunions and bone defects with the Taylor Spatial Frame. J Orthop Trauma. 2008;22:88–95. doi: 10.1097/BOT.0b013e318162ab49. [DOI] [PubMed] [Google Scholar]
- 47.Eralp L, Kocaoglu M, Yusof NM, Bulbul M. Distal tibial reconstruction with use of a circular external fixator and an intramedullary nail. The combined technique. J Bone Joint Surg Am. 2007;89:2218–24. doi: 10.2106/JBJS.F.01579. [DOI] [PubMed] [Google Scholar]
- 48.El-Rosasy MA. Acute shortening and re-lengthening in the management of bone and soft-tissue loss in complicated fractures of the tibia. J Bone Joint Surg Br. 2007;89:80–8. doi: 10.1302/0301-620X.89B1.17595. [DOI] [PubMed] [Google Scholar]
- 49.Nho SJ, Helfet DL, Rozbruch SR. Temporary intentional leg shortening and deformation to facilitate wound closure using the Ilizarov/Taylor spatial frame. J Orthop Trauma. 2006;20:419–24. doi: 10.1097/00005131-200607000-00010. [DOI] [PubMed] [Google Scholar]
- 50.Lovisetti G, Sala F, Miller AN, Thabet AM, Zottola V, Capitani D. Clinical reliability of closed techniques and comparison with open strategies to achieve union at the docking site. Int Orthop. 2012;36:817–25. doi: 10.1007/s00264-011-1260-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hatzokos I, Stavridis SI, Iosifidou E, Karataglis D, Christodoulou A. Autologous bone marrow grafting combined with demineralized bone matrix improves consolidation of docking site after distraction osteogenesis. J Bone Joint Surg Am. 2011;93:671–8. doi: 10.2106/JBJS.J.00514. [DOI] [PubMed] [Google Scholar]
- 52.Calori GM, Tagliabue L, Gala L, d’Imporzano M, Peretti G, Albisetti W. Application of rhBMP-7 and platelet-rich plasma in the treatment of long bone nonunions: A prospective randomised clinical study on 120 patients. Injury. 2008;39:1391–402. doi: 10.1016/j.injury.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 53.Morgan BW, Rogers MJ, Jackson M, Livingstone JA, Monsell F, Atkins RM. The Technique of microdrilling: Stimulation of bone union in patients treated with circular frames with established nonunion. Orthopaedic Proceedings. 2008 Aug;90-B(Supp III):504. [Google Scholar]
- 54.Kiely P, Ward K, Bellemore CM, Briody J, Cowell CT, Little DG. Bisphosphonate rescue in distraction osteogenesis: A case series. J Pediatr Orthop. 2007;27:467–71. doi: 10.1097/01.bpb.0000271326.41363.d1. [DOI] [PubMed] [Google Scholar]
- 55.Pountos I, Georgouli T, Calori GM, Giannoudis PV. Do nonsteroidal anti-inflammatory drugs affect bone healing? A critical analysis. ScientificWorldJournal 2012. 2012 doi: 10.1100/2012/606404. 606404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alzahrani MM, Anam EA, Makhdom AM, Villemure I, Hamdy RC. The effect of altering the mechanical loading environment on the expression of bone regenerating molecules in cases of distraction osteogenesis. Front Endocrinol (Lausanne) 2014;5:214. doi: 10.3389/fendo.2014.00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gorter EA, Krijnen P, Schipper IB. Vitamin D deficiency in adult fracture patients: Prevalence and risk factors. Eur J Trauma Emerg Surg. 2016;42:369–78. doi: 10.1007/s00068-015-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kanakaris NK, Morell D, Gudipati S, Britten S, Giannoudis PV. Reaming Irrigator Aspirator system: Early experience of its multipurpose use. Injury. 2011;42(Suppl 4):S28–34. doi: 10.1016/S0020-1383(11)70009-2. [DOI] [PubMed] [Google Scholar]
- 59.Giannoudis PV, Tzioupis C, Green J. Surgical techniques: How I do it? The Reamer/Irrigator/Aspirator (RIA) system. Injury. 2009;40:1231–6. doi: 10.1016/j.injury.2009.07.070. [DOI] [PubMed] [Google Scholar]
- 60.Qvick LM, Ritter CA, Mutty CE, Rohrbacher BJ, Buyea CM, Anders MJ. Donor site morbidity with reamer-irrigator-aspirator (RIA) use for autogenous bone graft harvesting in a single centre 204 case series. Injury. 2013;44:1263–9. doi: 10.1016/j.injury.2013.06.008. [DOI] [PubMed] [Google Scholar]
- 61.Pape HC, Tarkin IS. Reamer irrigator aspirator: A new technique for bone graft harvesting from the intramedullary canal. Oper Tech Orthop. 2008;18:108–13. [Google Scholar]
- 62.Chaudhary M, Jain S, Vigneshwaran P, Lakhani P. Infected lower tibial nonunions without bone grafting – Reliable union using the Ilizarov technique. J Limb Lengthening Reconstr. 2015;1:21–8. [Google Scholar]
- 63.Hernigou P, Trousselier M, Roubineau F, Bouthors C, Chevallier N, Rouard H, et al. Local transplantation of bone marrow concentrated granulocytes precursors can cure without antibiotics infected nonunion of polytraumatic patients in absence of bone defect. Int Orthop. 2016;40:2331–8. doi: 10.1007/s00264-016-3147-x. [DOI] [PubMed] [Google Scholar]
- 64.Hernigou P, Poignard A, Beaujean F, Rouard H. Percutaneous autologous bone-marrow grafting for nonunions. Influence of the number and concentration of progenitor cells. J Bone Joint Surg Am. 2005;87:1430–7. doi: 10.2106/JBJS.D.02215. [DOI] [PubMed] [Google Scholar]
- 65.Mollon B, da Silva V, Busse JW, Einhorn TA, Bhandari M. Electrical stimulation for long-bone fracture-healing: A meta-analysis of randomized controlled trials. J Bone Joint Surg Am. 2008;90:2322–30. doi: 10.2106/JBJS.H.00111. [DOI] [PubMed] [Google Scholar]
- 66.Biglari B, Yildirim TM, Swing T, Bruckner T, Danner W, Moghaddam A. Failed treatment of long bone nonunions with low intensity pulsed ultrasound. Arch Orthop Trauma Surg. 2016;136:1121–34. doi: 10.1007/s00402-016-2501-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shahid S. Role of systemic enzymes in infections. WebmedCentral Complement Med. 2011;2:WMC002495. [Google Scholar]
- 68.Grbic R, Miric DJ, Kisic B, Popovic L, Nestorovic V, Vasic A. Sequential analysis of oxidative stress markers and Vitamin C status in acute bacterial osteomyelitis. Mediators Inflamm 2014. 2014 doi: 10.1155/2014/975061. 975061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vernon D’ Silva BS, Suchetha Kumari N, Naveen P, Shetty V, Shetty L. A comparative study of oxidative stress in diabetic and non-diabetic osteomyelitis. RJPBCS. 2011;2:342–7. [Google Scholar]
- 70.Giannoudis PV, Gudipati S, Harwood P, Kanakaris NK. Long bone nonunions treated with the diamond concept: A case series of 64 patients. Injury. 2015;46(Suppl 8):S48–54. doi: 10.1016/S0020-1383(15)30055-3. [DOI] [PubMed] [Google Scholar]
- 71.Calori GM, Giannoudis PV. Enhancement of fracture healing with the diamond concept: The role of the biological chamber. Injury. 2011;42:1191–3. doi: 10.1016/j.injury.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 72.Giannoudis PV, Einhorn TA, Schmidmaier G, Marsh D. The diamond concept – Open questions. Injury. 2008;39(Suppl 2):S5–8. doi: 10.1016/S0020-1383(08)70010-X. [DOI] [PubMed] [Google Scholar]
- 73.Kocaoglu M, Eralp L, Rashid HU, Sen C, Bilsel K. Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. J Bone Joint Surg Am. 2006;88:2137–45. doi: 10.2106/JBJS.E.01152. [DOI] [PubMed] [Google Scholar]
- 74.Emara KM, Allam MF. Ilizarov external fixation and then nailing in management of infected nonunions of the tibial shaft. J Trauma. 2008;65:685–91. doi: 10.1097/TA.0b013e3181569ecc. [DOI] [PubMed] [Google Scholar]