Summary
We conducted a spatial analysis to identify epidemic foci and trends of HIV among men who have sex with men (MSM) in China. Assorted spatial analyses reveal concentrated HIV epidemic among young MSM in Chinese cities, calling for intensive interventions.
Keywords: spatial analysis, HIV/AIDS, trend, men who have sex with men, China.
Abstract
Background.
Studies have shown a recent upsurge in human immunodeficiency virus (HIV) burden among men who have sex with men (MSM) in China, especially in urban areas. For intervention planning and resource allocation, spatial analyses of HIV/AIDS case-clusters were required to identify epidemic foci and trends among MSM in China.
Methods.
Information regarding MSM recorded as HIV/AIDS cases during 2006–2015 were extracted from the National Case Reporting System. Demographic trends were determined through Cochran-Armitage trend tests. Distribution of case-clusters was examined using spatial autocorrelation. Spatial-temporal scan was used to detect disease clustering. Spatial correlations between cases and socioenvironmental factors were determined by spatial regression.
Results.
Between 2006 and 2015, in China, 120 371 HIV/AIDS cases were identified among MSM. Newly identified HIV/AIDS cases among self-reported MSM increased from 487 cases in 2006 to >30 000 cases in 2015. Among those HIV/AIDS cases recorded during 2006–2015, 47.0% were 20–29 years old and 24.9% were aged 30–39 years. Based on clusters of HIV/AIDS cases identified through spatial analysis, the epidemic was concentrated among MSM in large cities. Spatial-temporal clusters contained municipalities, provincial capitals, and main cities such as Beijing, Shanghai, Chongqing, Chengdu, and Guangzhou. Spatial regression analysis showed that sociodemographic indicators such as population density, per capita gross domestic product, and number of county-level medical institutions had statistically significant positive correlations with HIV/AIDS among MSM.
Conclusions.
Assorted spatial analyses revealed an increasingly concentrated HIV epidemic among young MSM in Chinese cities, calling for targeted health education and intensive interventions at an early age.
Since the first report of AIDS [1] in 1981, the worldwide burden of human immunodeficiency virus (HIV)/AIDS among men who have sex with men (MSM) has increased dramatically. China has been no exception [2]. After its first AIDS-related death being reported in 1985 [3], HIV had spread across all 31 provinces and autonomous regions of the country by 1998. The epidemic had gradually concentrated among injection drug users and MSM. In recent years, the main transmission route of HIV in China has shifted from injecting drug use to sexual transmission. Changes in economic situation, social norms, and behavioral patterns were attributed as potentially influential factors for this change [4].
The size of the largely hidden, steadily growing MSM population in the country was estimated to be between 3.1 and 6.3 million in 2007 [5]. The National Sentinel Surveillance System of China further revealed that HIV prevalence among MSM had increased from 5.7% in 2010 to 7.5% in 2013 [6]. National incidence of self-reported HIV cases also increased in this population, from 0.39 in 2000 to 0.98 per 100 person-years in 2010 [7].
Based on findings from independent studies, high HIV prevalence exists among MSM in specific regions, such as Guangzhou (11.4% in 2013) [8], Zhejiang (13.8%) [9], Harbin (9.5% in 2011) [10], and Chongqing (15.4% in 2010) [11], along with 15 other cities in China (6.27% in 2011) [12]. Yet there exists a dearth of information regarding the country-wide epidemiological distribution and spatial trends of HIV/AIDS cases among MSM. Moreover, the location of the case clusters, and their correlation with relevant socioenvironmental factors, remains unknown.
Use of spatial analysis has become increasingly common in HIV research, specifically for the assessment of geographic distribution of infection [13, 14], identification of high-risk and space-time clusters [15], as well as exploration of spatial relationships between HIV and social covariates [16]. A better understanding of long-term trends and nationwide spatial clustering of HIV cases among MSM would provide public health professionals and policymakers with scientifically informed insights for developing appropriate targeted responses, including efficient program planning and intervention delivery. Tracking the evolution of the HIV epidemic and identifying high-risk areas would provide useful information for carrying out preventive measures in these areas.
Thus, to address the paucity of relevant information regarding epidemiological trends and spatial distribution, we conducted a spatial analysis of HIV/AIDS cases among MSM reported to the Web-based National Case Reporting System (CRS) of China between 2006 and 2015.
MATERIALS AND METHODS
Data Collection
In 2005, China introduced a Web-based HIV/AIDS CRS, to which all medical institutions and local Centers for Disease Control and Prevention (CDCs) at the county, city, and provincial levels could enter case report data of identified HIV/AIDS cases using automated forms [17]. Shortly thereafter, in 2008, the Comprehensive Response Information Management System (CRIMS) was launched to further standardize data collection methods and to increase the efficiency of data management for meaningful utilization. Data for this study were gathered from face-to-face or telephone-based follow-up interviews with newly identified CRS cases and were completed within 10 working days after appearance in the system. Demographic information (eg, age, sex, occupation, marriage, address) and data on high-risk behaviors were collected using standardized case report forms.
Data Management
All identified HIV/AIDS cases transmitted through self-reported homosexual contact between 2006 and 2015 and reported to the CRS were included in this study, excluding cases where addresses were unknown. To protect the privacy of participants, prior to the data analysis, all personal identifiers were removed from the database for this study. The corresponding national standard geocodes at the provincial, city, and county levels were included in the analysis, to identify the location of the reported cases. Electronic maps were obtained from China CDCs. ArcGIS 10.3 software (Esri Inc, Redlands, California) was used to create maps. SPSS version 18.0 software (SPSS IBM Inc, Armonk, New York) was used to process and analyze data. Population data at the provincial and county levels were obtained from the Chinese National Bureau of Statistics.
Trend Analysis
Trends in demographic characteristics among HIV/AIDS cases through homosexual contact during the study period were analyzed to identify potential change using the Cochran-Armitage test with an assumed α of .05.
Spatial Autocorrelation
Autocorrelation analysis was used to determine the distribution of the clusters of HIV/AIDS infection among MSM. In the Moran analyses, we used the population-level annual diagnosis rate to detect the clusters. For the population-level annual diagnosis rate, we used the total number of male adults as the denominator and the number of cases identified each year in each city as the nominator, as the total numbers of MSM are not available in the majority of Chinese cities.
General Moran index and local Moran index were used as measures of autocorrelation, as per the standard method detailed by Peng et al [18]. We used the general Moran index to detect if there were clusters of HIV/AIDS at the population level (annual diagnosis rate in China). Local Moran index, also called LISA (local indicator of spatial association), was used to identify where the specific local clusters occurred. Four types of spatial autocorrelations were observed: (1) low-high, a low value was surrounded by high values; (2) high-high, a high value was surrounded by high values; (3) high-low, a high value was surrounded by low values; and (4) low-low, a low value was surrounded by low values. Association between areas of similar values (such as high-high and low-low) were defined as positive spatial autocorrelation, whereas association between areas of dissimilar values (low-high and high-low) were considered negative autocorrelation [19]. In the current study, we focused on high-high types, which were determined between clusters of counties with a high number of population-level annual HIV/AIDS diagnosis rates surrounded by other counties having similar scenarios. Local spatial autocorrelation was also conducted at the county level to detect local clusters of HIV/AIDS among MSM.
Temporal-Spatial Clustering Analysis
Spatial scan statistics (SaTScan) software (version 9.4.1, www.satscan.org) was used to detect disease clustering simultaneously in time and space [20]. A cylinder scanning window was used for probe scanning. The bottom of the cylinder represented the area of the scanned space, while the height of the cylinder depicted the scanning interval. Log likelihood ratio was calculated to compare risk outside and inside the scan window during the scanning process. An associated P value, based on Monte Carlo hypothesis testing, was used to evaluate if the observed clustering of cases was random [21]. This study used retrospective space-time scan analysis combined with Poisson distribution model. Assuming α = .05, clustering for which the determined P value was <.05 was reported as statistically significant. For the same reason we mentioned above, we used the total number of male adults as the population data to perform temporal-spatial clustering analysis.
Spatial Regression Analysis
Using GeoDa 1.6.7 software (http://geodacenter.asu.edu/software/downloads), spatial regression analysis was conducted to determine the spatial correlation of HIV/AIDS cases in 2010 and 3 socioenvironmental factors: (1) population density in 2010 (county population in 1000s / [county area in km2]); (2) gross domestic product (GDP) per capita in 2010 (local GDP in 10000 Yuan / county population); and (3) number of county-level medical institutions in 2010 as an index of local health service delivery [22]. Initially, ordinary least squares regression was performed to determine spatial dependence followed by comparison of models for spatial error and spatial lag. Queen’s weight was used as the estimates from the spatial regression.
RESULTS
Demographic Characteristics of the HIV/AIDS Cases among MSM by Year
A total of 120 371 HIV/AIDS cases were identified in China among MSM between 2006 and 2015. Altogether, 985 cases (0.8%) without specific district- or county-level addresses were excluded. Identified HIV/AIDS cases were geographically distributed among self-reported MSM across the country. Overall, 2618 counties (91.7% of all 2854 counties in China) reported HIV/AIDS cases among MSM between 2006 and 2015. Four municipalities and 27 provincial capitals (20.0% of the country’s population) accounted for 50.1% of all identified cases. Among analyzed cases, 47.0% were 20–29 years old and 24.9% were aged 30–39 years; 66.0% were single, and 41.0% had at least a college degree.
Geographical Distribution and Trend Analysis
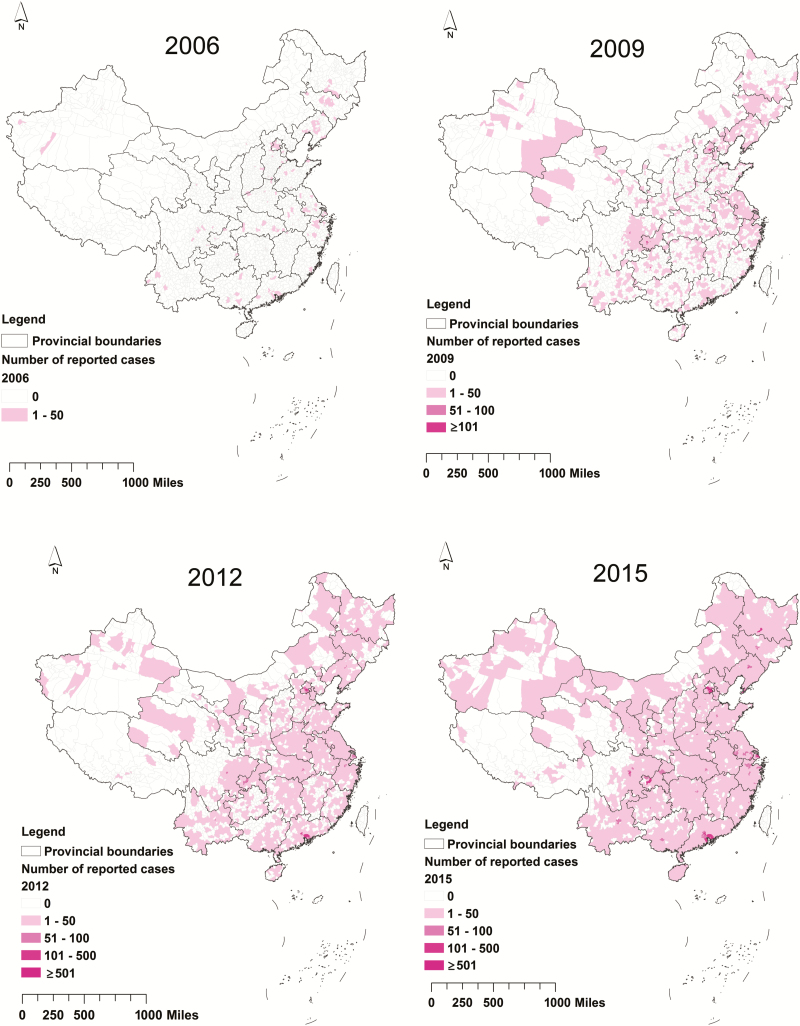
In 2015, 2390 districts or counties reported HIV/AIDS cases among MSM whereas in 2006, MSM cases were found in only 195 districts or counties (Figure 1). In 2006, only 2 districts in Beijing reported >20 cases, while in 2015, 42 districts or counties from large cities (eg, Beijing, Shanghai, and Chongqing) reported >100 cases.
Figure 1.
Geographical distribution of the human immunodeficiency virus/AIDS cases reported among men who have sex with men at the county level in the years 2006, 2009, 2012, and 2015 in China.
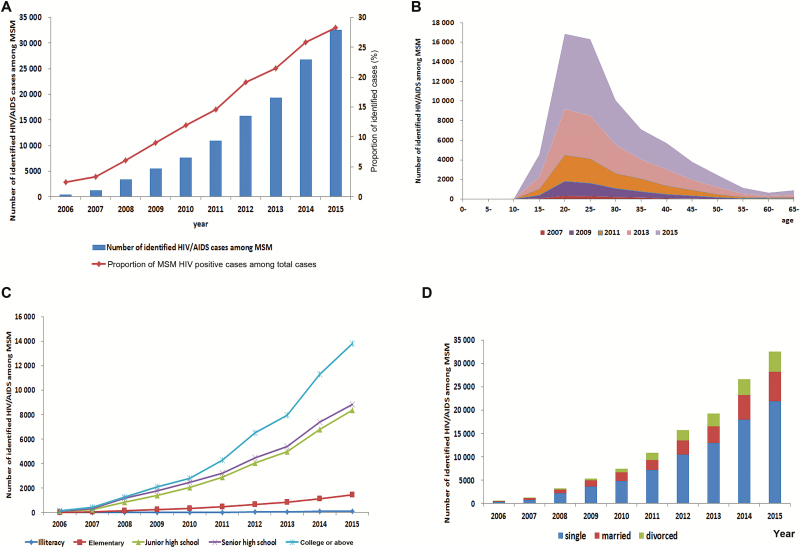
The rate of infection through homosexual transmission steadily increased between 2006 and 2015. There were >30 000 cases in 2015, 65.9 times the number in 2006 (P < .001; Figure 2A). The median age was 28–29 years during the study period. The number of cases between 20 and 39 years also increased during this period, but the proportion of cases aged 20–39 decreased from 81.3% in 2007 to 71.1% in 2015 (P < .001; Figure 2B). The proportion of cases among individuals with a college degree or above increased from 36.2% in 2006 to 42.4% in 2015 (P < .001; Figure 2C). Similarly, the proportion of cases among single MSM also significantly increased over the study period (P < .001; Figure 2D).
Figure 2.
A, Proportional distribution of transmission route of identified human immunodeficiency virus (HIV)/AIDS cases among men who have sex with men (MSM) by year. B, Number of identified HIV/AIDS cases among MSM by age. C, Number of identified HIV/AIDS cases among MSM by education. D, Number of identified HIV/AIDS cases among MSM by marriage.
Spatial Clustering of HIV/AIDS Cases Among MSM
General spatial autocorrelation was conducted for the newly diagnosed HIV/AIDS cases among MSM for each year (Table 1). All Moran index values were larger than zero, with the z value >1.96 (P< .001). The results indicated potential clustering of the HIV/AIDS epidemic among MSM in the whole country every year.
Table 1.
Results of General Spatial Autocorrelation for the Population-Level Annual Human Immunodeficiency Virus/AIDS Diagnosis Rate of Men Who Have Sex with Men in China, 2006–2015
| Year | Moran Index | z Value | P Value |
|---|---|---|---|
| 2006 | 0.298 | 84.627 | <.001 |
| 2007 | 0.344 | 78.621 | <.001 |
| 2008 | 0.324 | 74.239 | <.001 |
| 2009 | 0.311 | 72.023 | <.001 |
| 2010 | 0.348 | 98.584 | <.001 |
| 2011 | 0.340 | 97.251 | <.001 |
| 2012 | 0.240 | 74.311 | <.001 |
| 2013 | 0.345 | 97.999 | <.001 |
| 2014 | 0.328 | 93.161 | <.001 |
| 2015 | 0.373 | 84.713 | <.001 |
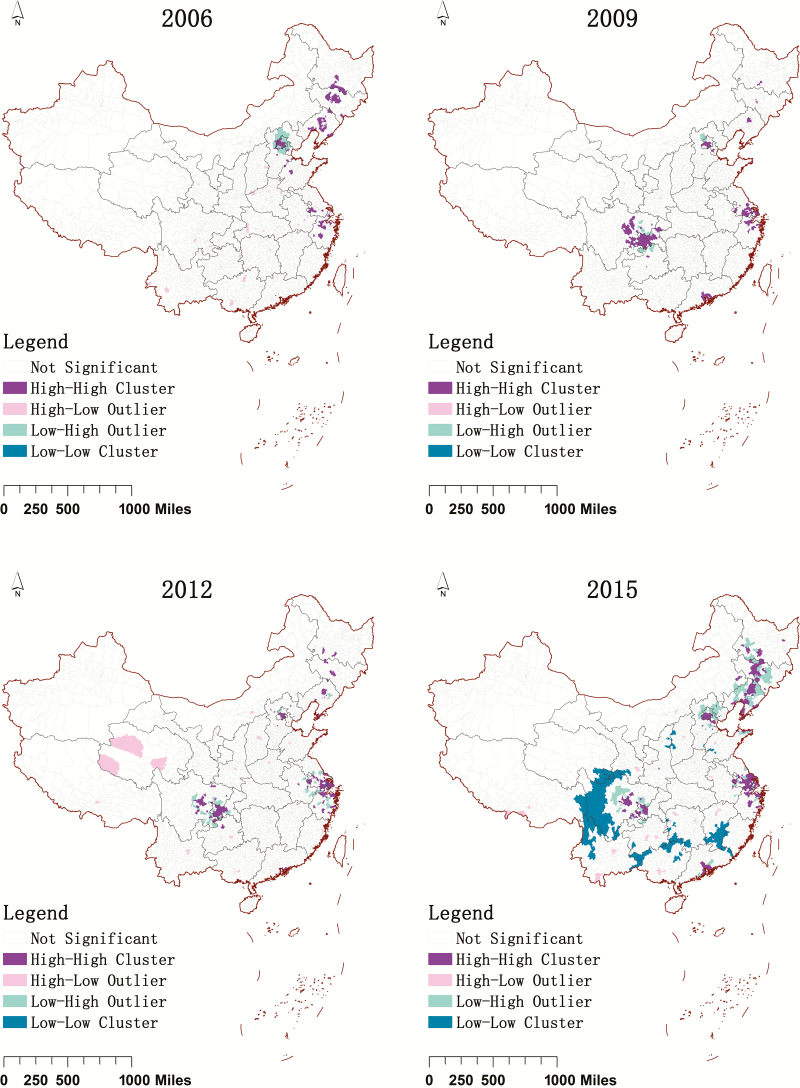
Local Moran index was also used to detect the clusters of the population-level annual diagnosis rate by year (Figure 3). In 2006, the high-high clusters were mainly located in eastern and southern China, including Beijing, Tianjin, Hebei, Liaoning, Jilin, Heilongjiang, Shanghai, Jiangsu, Shandong, Zhejiang, and Guangdong. After 2008, the high-high clusters spread to southwest Chongqing municipality, Sichuan, and Guizhou. In 2015, the high-high clusters spread further to Neimeng, Anhui, and Shaanxi. Low-low clusters formed in 2015 in the western boundary of Sichuan, south of Jiangxi, along the northern boundary of Guangxi, and in the northwest of Yunnan.
Figure 3.
Local clusters of the population-level annual human immunodeficiency virus/AIDS diagnosis rate of men who have sex with men at county level by year, China, 2006–2015.
Spatial-Temporal Clusters
Spatial-temporal clustering analysis was used to examine 10 clusters between 2006 and 2015 (Supplementary Figure 1 and Table 2). Cluster 1 (the most evident cluster) was located in Beijing during 2009 to 2015. The cluster had a relative risk of 10.95 (P< .001). Additionally, 9 statistically significant secondary clusters were identified, all of which contained municipalities, provincial capitals, and main cities. Most clusters were aggregated between 2008 and 2015, with the majority of data aggregated from 2011.
Table 2.
Retrospective Space-Time Scan Analysis of Human Immunodeficiency Virus/AIDS Cases among Men Who Have Sex with Men Using the Discrete Poisson Model in China, 2006–2015
| Cluster | Dates | Main Cities in Cluster | (Coordinates), Radius | Relative Risk | P Value |
|---|---|---|---|---|---|
| 1 | 2009–2015 | Beijing | (39.936042 N, 116.359938 E), 34.95 km | 10.95 | <.001 |
| 2 | 2011–2015 | Chengdu and Chongqing | (29.990926 N, 105.356151 E), 178.08 km | 4.17 | <.001 |
| 3 | 2011–2015 | Guangzhou and Shenzhen | (22.703132 N, 113.865107 E), 85.08 km | 5.43 | <.001 |
| 4 | 2011–2015 | Shanghai, Hangzhou, and Ningbo | (31.032896 N, 121.195448 E), 158.83 km | 3.78 | <.001 |
| 5 | 2012–2015 | Shenyang, Changchun, and Harbin | (44.747261 N, 122.790547 E), 342.31 km | 4.3 | <.001 |
| 6 | 2011–2015 | Xi’an | (34.217323 N, 108.926541 E), 21.74 km | 7.15 | <.001 |
| 7 | 2012–2015 | Dalian | (38.904087 N, 121.617278 E), 38.88 km | 9.78 | <.001 |
| 8 | 2012–2015 | Nanjing and Hefei | (32.047815 N, 118.112098 E), 89.82 km | 3.46 | <.001 |
| 9 | 2011–2015 | Wuhan | (30.560565 N, 114.367800 E), 33.52 km | 4.85 | <.001 |
| 10 | 2008–2015 | Guiyang | (26.624374 N, 106.717334 E), 10.42 km | 7.77 | <.001 |
Spatial scan analysis of HIV/AIDS cases among MSM at county level in the years 2006, 2009, 2012, and 2015 in China showed that clusters increased gradually by year (Supplementary Figure 2). The clusters in 2006 were mainly located in eastern China, including Beijing, Liaoning, Jilin, Heilongjiang, Jiangsu, and Zhejiang. The clusters in 2015 spread to 28 provinces in China, with most of the clusters located in municipalities, provincial capitals, and main cities.
Spatial Regression Analysis
We analyzed the spatial correlation of newly identified HIV/AIDS cases among MSM with population density, per capita GDP, and number of county-level medical institutions. Spatial lag model was found more appropriate in comparison to error modeling. These 3 factors were positively associated with new HIV/AIDS cases among MSM (Table 3).
Table 3.
Result of Spatial Regression Analysis among Human Immuno deficiency Virus-Infected Men Who Have Sex with Men in China, 2006–2015
| Ordinary Least Squares | Spatial Lag Model | |||
|---|---|---|---|---|
| Variable | Coefficient | t Statistic | Coefficient | z Value |
| ρa | 0.493 | 24.337b | ||
| Constant | –1.559 | –7.366b | –1.790 | –9.609b |
| No. of medical institutions | 0.132 | 14.209b | 0.116 | 13.865b |
| Per capita gross domestic product | 0.134 | 3.882b | 0.063 | 2.066c |
| Population density | 0.867 | 19.514b | 0.507 | 12.376b |
| R 2 | 0.214 | 0.391 | ||
aRegression coefficient of spatial lag variable.
b P < .001.
c P < .05.
DISCUSSION
A body of research over the past few decades has identified MSM as a high-risk population for acquisition of HIV. Few studies, however, have examined the Chinese HIV epidemic among MSM using spatial-temporal distribution over time. Our study summarizes key geographical aspects of this epidemic, to help appropriate stakeholders design tailored prevention programs and more effectively allocate resources.
It was found that HIV/AIDS cases reported among MSM increased rapidly during 2006–2015 in China. There existed major clustering of the epidemic foci among MSM in municipalities, provincial capitals, and cities with large populations and high economic growth. Using all HIV/AIDS cases among MSM reported to the CRS between 2006 and 2015, long-term trends were explored at the national level, and spatial clusters of the epidemic were identified using spatial autocorrelation and spatial-temporal clustering analysis.
The growing proportion of cases infected through homosexual contact indicated an upsurge of the HIV/AIDS epidemic in this hard-to-reach population in China during the past decade, which could be explained in numerous ways. First, there has been a dramatic increase in HIV antibody testing in China, in parallel with the implementation of the Four Frees One Care policy in 2004 [23]. Between 2002 and 2009, the self-reported testing rate increased from 10.8% to 51.2% [24]. Second, remarkable socioeconomic reforms and dramatic technological advances have altered patterns of sexual activity, mobility, and communication over the last decade. Digital connectivity and the use of mobile applications has become an increasingly common platform for establishing sexual relationships, especially among hidden networks of MSM [25, 26]. Between 2012 and 2015, BLUED, China’s smartphone-based application for meeting sexual partners, saw an increase from 4 million to >22 million users [27]. Third, consistently high-risk behaviors among Chinese MSM could be another important reason. Furthermore, preventive services to control the HIV epidemic are still largely lagging behind the countrywide need. Low HIV testing rates, multiple sexual partners, and low rates of consistent condom use were reported among Chinese MSM [28, 29]. Further scaling-up of the programs targeting improvements in testing, condom use, and test-and-treat policies could be effective in slowing the transmission of HIV among MSM [30, 31].
Spatial autocorrelation during 2006–2015 revealed a spread in HIV epidemic clusters among MSM from a few large cities in eastern China to most of the municipalities and provincial capitals countrywide. This was consistent with another recent report that HIV incidence among MSM was much higher in large cities compared with smaller ones [32]. Temporal-spatial scan identified time windows, mainly concentrated between 2011 and 2015, indicating a rapid upsurge of the epidemic during this period. Although homosexuality is still largely regarded as unacceptable by Chinese society, attitudes appear to be changing slowly.
The spatial regression analysis showed that population density, per capita GDP, and number of medical institutions showed significant positive correlations with the number of reported HIV/AIDS cases. These identified correlates of spatial clustering were similar to those identified in another research study conducted in Chongqing [33]. The cultural diversity in China makes MSM less likely to reveal their sexual practices [34]. It may be that in some parts of the country there is less acceptance of homosexuality, which may in turn impact the clusters we detected in this study.
The current study has several limitations. First, the number of identified HIV/AIDS cases among MSM might be affected by increased HIV antibody testing. In the past 10 years, HIV testing has expanded greatly in China, especially in urban areas. This expansion could create detection bias, as more cases can be diagnosed because there is more testing done. Second, there are differences between the MSM HIV epidemic and non-MSM HIV epidemic in China. For example, cases transmitted through blood transfusion are mainly located in rural areas of central China, and cases transmitted through injection drug use are mainly located in southwest and western China. Detection bias could be one of the reasons, as MSM are less likely to self-identify in rural areas due to stigma. Third, owing to the potential risk of stigmatization, many HIV-infected MSM could have refrained from self-identification as MSM. As cases were self-reported, this study thus might have depicted the scenario among an underestimated number of MSM in relation to the whole country. Furthermore, positively screened cases often fail to undergo the confirmatory tests and therefore might not be recorded in the CRS. However, these problems were partially adjusted by the conscious intensification of the HIV/AIDS reporting system in this country. Fourth, for the Moran analyses and SaTScan, we used the total number of male adults as the denominator instead of the total number of MSM in each city, which may introduce bias to the study.
In conclusion, there has been a rise in HIV infection among MSM in recent years in China. Most cases of HIV infection among MSM occurred in men aged 20–39 years and were localized in large Chinese cities. Focused attention, implementation of intervention strategies, and prevention programs targeting young MSM in identified key areas are urgently required to control the spread of this disease among MSM in China.
Supplementary Material
Notes
Author contributions. Q. Q., W. G., Y. C., and J. S. designed this study; Q. Q., N. Z., W. T., and T. M. wrote the main manuscript text; Q. Q., L. W., and W. G. analyzed the data; and Q. Q., Z. D., L. W., and C. C. collected the data. All authors reviewed the manuscript.
Acknowledgments. The authors acknowledge the staff members of the HIV/AIDS Case Reporting System in China. The authors thank Yaojun Zhang from Renmin University of China, Liqun Fang from the Academy of Military Medical Science of China, and Larry Han from the University of North Carolina at Chapel Hill (UNC) for their comments on modified versions of this report.
Financial support. This study was supported by the China National AIDS Program, Multidisciplinary HIV and TB Implementation Sciences Training in China (grant number 4U2RTW006918); National Institutes of Health (NIH) (National Institute of Allergy and Infectious Diseases [NIAID] grant number 1R01AI114310, FIC grant number 1D43TW009532); NIH Fogarty International Center (grant number 5R25TW009340); and UNC Center for AIDS Research (grant number NIAID 5P30AI050410).
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Piot P, Plummer FA, Mhalu FS, Lamboray JL, Chin J, Mann JM. AIDS: an international perspective. Science 1988; 239:573–9. [DOI] [PubMed] [Google Scholar]
- 2. Beyrer C, Sullivan P, Sanchez J, et al. The increase in global HIV epidemics in MSM. AIDS 2013; 27:2665–78. [DOI] [PubMed] [Google Scholar]
- 3. Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China’s response to HIV/AIDS. Lancet 2007; 369:679–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zheng W, Zhou X, Zhou C, Liu W, Li L, Hesketh T. Detraditionalisation and attitudes to sex outside marriage in China. Cult Health Sex 2011; 13:497–511. [DOI] [PubMed] [Google Scholar]
- 5. Wang L, Wang N, Wang L, et al. The 2007 estimates for people at risk for and living with HIV in China: progress and challenges. J Acquir Immune Defic Syndr 2009; 50:414–8. [DOI] [PubMed] [Google Scholar]
- 6. Li D, Ge L, Wang L, et al. Trend on HIV prevalence and risk behaviors among men who have sex with men in China from 2010 to 2013. Zhonghua Liu Xing Bing Xue Za Zhi 2014; 35:542–6. [PubMed] [Google Scholar]
- 7. Zhang L, Chow EP, Jing J, et al. HIV prevalence in China: integration of surveillance data and a systematic review. Lancet Infect Dis 2013; 13:955–63. [DOI] [PubMed] [Google Scholar]
- 8. Zhong F, Liang B, Xu H, et al. Increasing HIV and decreasing syphilis prevalence in a context of persistently high unprotected anal intercourse, six consecutive annual surveys among men who have sex with men in Guangzhou, China, 2008 to 2013. PLoS One 2014; 9:e103136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pan X, Wu M, Ma Q, et al. High prevalence of HIV among men who have sex with men in Zhejiang, China: a respondent-driven sampling survey. BMJ Open 2015; 5:e008466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang L, Zhang D, Yu B, et al. Prevalence of HIV infection and associated risk factors among men who have sex with men (MSM) in Harbin, P. R. China. PLoS One 2013; 8:e58440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li X, Wu G, Lu R, et al. HIV-testing behavior and associated factors among MSM in Chongqing, China: results of 2 consecutive cross-sectional surveys from 2009 to 2010. Medicine 2014; 93:e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Qi J, Zhang D, Fu X, et al. High risks of HIV transmission for men who have sex with men—a comparison of risk factors of HIV infection among MSM associated with recruitment channels in 15 cities of China. PLoS One 2015; 10:e0121267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bautista CT, Sateren WB, Sanchez JL, Singer DE, Scott P. Geographic mapping of HIV infection among civilian applicants for United States military service. Health Place 2008; 14:608–15. [DOI] [PubMed] [Google Scholar]
- 14. Carrel M, Janko M, Mwandagalirwa MK, et al. Changing spatial patterns and increasing rurality of HIV prevalence in the Democratic Republic of the Congo between 2007 and 2013. Health Place 2016; 39:79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hixson BA, Omer SB, del Rio C, Frew PM. Spatial clustering of HIV prevalence in Atlanta, Georgia and population characteristics associated with case concentrations. J Urban Health 2011; 88:129–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wabiri N, Shisana O, Zuma K, Freeman J. Assessing the spatial nonstationarity in relationship between local patterns of HIV infections and the covariates in South Africa: a geographically weighted regression analysis. Spat Spatiotemporal Epidemiol 2016; 16:88–99. [DOI] [PubMed] [Google Scholar]
- 17. Mao Y, Wu Z, Poundstone K, Wang C, Qin Q, Ma Y, et al. Development of a unified web-based national HIV/AIDS information system in China. Int J Epidemiol 2010; 39(suppl 2:ii79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Peng ZH, Cheng YJ, Reilly KH, et al. Spatial distribution of HIV/AIDS in Yunnan province, People’s Republic of China. Geospat Health 2011; 5:177–82. [DOI] [PubMed] [Google Scholar]
- 19. Martinez AN, Mobley LR, Lorvick J, Novak SP, Lopez A, Kral AH. Spatial analysis of HIV positive injection drug users in San Francisco, 1987 to 2005. Int J Environ Res Public Health 2014; 11:3937–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kulldorff M, Athas WF, Feurer EJ, Miller BA, Key CR. Evaluating cluster alarms: a space-time scan statistic and brain cancer in Los Alamos, New Mexico. Am J Public Health 1998; 88:1377–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hjalmars U, Kulldorff M, Gustafsson G, Nagarwalla N. Childhood leukaemia in Sweden: using GIS and a spatial scan statistic for cluster detection. Stat Med 1996; 15(7–9):707–15. [DOI] [PubMed] [Google Scholar]
- 22. Sheng LY, Yan JH. China statistical yearbook for regional economy. Beijing, China: China Statistics Press, 2012. [Google Scholar]
- 23. Hao Y, Cui Y, Sun X, et al. A retrospective study of HIV/AIDS situation: a ten-year implementation of “four frees and one care” policy in China. Zhonghua Ji Bing Kong Zhi Za Zhi 2014; 18:369–74. [Google Scholar]
- 24. Chow EP, Wilson DP, Zhang L. The rate of HIV testing is increasing among men who have sex with men in China. HIV Med 2012; 13:255–63. [DOI] [PubMed] [Google Scholar]
- 25. Bien CH, Best JM, Muessig KE, Wei C, Han L, Tucker JD. Gay apps for seeking sex partners in China: implications for MSM sexual health. AIDS Behav 2015; 19:941–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhang D, Bi P, Lv F, Tang H, Zhang J, Hiller JE. Internet use and risk behaviours: an online survey of visitors to three gay websites in China. Sex Transm Infect 2007; 83:571–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Danlan. BLUED data: more than 22 million users. Available at: http://www.danlan.org/disparticle_52645.htm Accessed 30 April 2016. [Google Scholar]
- 28. Wang X, Lan G, Shen Z, et al. HIV and syphilis prevalence trends among men who have sex with men in Guangxi, China: yearly cross-sectional surveys, 2008-2012. BMC Infect Dis 2014; 14:367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Han L, Wei C, Muessig KE, Bien CH, Meng G, Emch ME, et al. HIV test uptake among MSM in China: implications for enhanced HIV test promotion campaigns among key populations. Global Public Health 2016:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Beyrer C, Baral SD, van Griensven F, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet 2012; 380:367–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Luo S, Han L, Lu H, et al. Evaluating the impact of test-and-treat on the HIV epidemic among MSM in China using a mathematical model. PLoS One 2015; 10:e0126893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cui Y, Guo W, Li D, et al. Estimating HIV incidence among key affected populations in China from serial cross-sectional surveys in 2010-2014. J Int AIDS Soc 2016; 19:20609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zhang Y, Xiao Q, Zhou L, et al. The AIDS epidemic and economic input impact factors in Chongqing, China, from 2006 to 2012: a spatial-temporal analysis. BMJ Open 2015; 5:e006669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Yoshioka MR, Schustack A. Disclosure of HIV status: cultural issues of Asian patients. AIDS Patient Care STDS 2001; 15:77–82. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.