Abstract
IN BRIEF This article provides a description of mindfulness and mindful eating and addresses the application of mindful eating as a component of diabetes self-management education. Mindful eating helps individuals cultivate awareness of both internal and external triggers to eating, interrupt automatic eating, and eat in response to the natural physiological cues of hunger and satiety. Mindful eating interventions have been effective in facilitating improvement in dysregulated eating and dietary patterns. Through practice over time, eating mindfully can interrupt habitual eating behaviors and provide greater regulation of food choice. More research is needed to determine the long-term impact of mindful eating programs.
The concept of mindfulness has attracted considerable attention in behavioral medicine, weight regulation, and diabetes management. In 2012, 34% of U.S. adults used a complementary health approach, and meditation was among the top five most commonly used approaches (1). Research among people with diabetes has found that a mindfulness approach improved depressive symptoms, anxiety, well-being, diabetes-related distress, and health-related quality of life (2–4). The impact of mindfulness interventions on A1C has been mixed (5). Some studies have found no significant change in A1C (2,4), whereas others have found a significant reduction in A1C (6,7). Mindfulness training in general has been associated with improvements in weight (8), abdominal fat (9), and telomerase activity (10). Furthermore, mindfulness-based interventions may be effective for eating behaviors, including binge eating, emotional eating, and external eating (11).
Thus, considerable research suggests that mindfulness interventions offer promise for treating dysregulated eating and the psychological morbidity associated with medical illness and for mitigating stress and enhancing emotional well-being. Mindful eating, in particular, may improve eating patterns by increasing fruit and vegetable consumption (12,13), reducing intake of energy-dense foods (14), and reducing the frequency or severity of binge eating (15).
The purpose of this article is to define and explain mindfulness, mindful meditation, and mindful eating; discuss why mindful eating may be beneficial in diabetes self-management; and provide suggestions for incorporating mindful practice into diabetes self-management education (DSME). At the outset, it is vital to explain what is meant by mindfulness to assist in discussions relevant to mindful eating.
What Is Mindfulness?
Mindfulness is an awareness or state of consciousness that emerges through purposely paying attention in the present moment without judgment regarding the events occurring moment by moment (16). Mindfulness approaches are not relaxation or mood-management techniques; rather, they are a form of mental training to alleviate the automatic or reactive modes of mind (17). The cultivation and practice of mindfulness, primarily through meditation, is believed to mediate observed effects on mood and behavior. Broadly conceptualized, mindfulness is a nonelaborative, nonjudgmental, present-centered awareness in which each thought, feeling, or sensation that arises in the attentional field is acknowledged and accepted as it is (17). Thoughts and feelings are observed without reacting to them in an automatic, habitual pattern of reactivity. This state of self-observation can introduce a “space” between an individual’s perception and response and enable one to respond more reflectively.
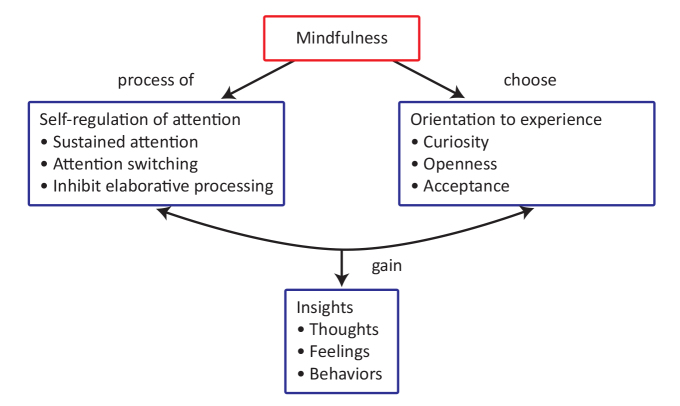
From a conceptual framework, mindfulness includes two primary components (Figure 1) (17). The first involves the self-regulation of attention on the immediate experience to acknowledge mental events in the present moment. Sustained attention to maintain a state of vigilance for prolonged periods of time is needed. Many meditation practices focus sustained attention on the breath so that thoughts, feelings, and sensations can be detected. The breath is used as a focal point because it is always present; by slowing down and focusing on the breath, a shift in awareness occurs. Skill in attention switching allows one to bring attention back to the breath when inevitably a thought, feeling, or sensation is acknowledged. Attention includes experiencing events in the mind and body; thoughts (e.g., Am I doing this right?) or events (e.g., My nose itches) are considered objects of observation, not distractions. Once acknowledged, attention is brought back to the breath, preventing further elaboration.
FIGURE 1.
Key components of mindfulness (17).
The second component of mindfulness involves adopting a particular orientation toward the present experience, with curiosity, openness, and acceptance (17). All experiences are seen as relevant and subject to observation. The goal is not to suppress thoughts and feelings or to produce a state such as relaxation. A decision is made to be open to the reality of the present moment and receptive to whatever happens to occur in the field of awareness. Through observation, a greater understanding of the nature of thoughts and feelings can be obtained. Noticing how a feeling evokes a judgmental thought and then the judgmental thought heightens the unpleasantness of the feeling is one example of the process of observation. The impermanence, or transient nature, of thoughts and feelings is a central point. Thoughts are recognized simply as thoughts that are not “real.” In summary, mindfulness is a skill that can be developed with practice that focuses on altering the impact of and response to thoughts, feelings, and sensations.
Applying Mindfulness to Eating Behaviors
The practice of mindfulness may promote more healthful eating behaviors. Mindful eating can interrupt automatic and inattentive responding to external food cues and emotional triggers that generally provoke habitual responses and unnecessary food consumption (18). Automatic eating can include emotional, impulsive, and habitual eating (19). Through training and practice, mindfulness can prevent the quick reaction of the impulsive system and allow for a more deliberate process to occur.
One common meditation exercise is to eat a single raisin mindfully, as if for the first time. This exercise is specific to food consumption and involves noticing the appearance, color, texture, and smell of the raisin before placing it in the mouth and then chewing it with deliberate attention to taste and sensory stimuli. By eating a raisin without impulse, distraction, or emotional interference, one can break the automatic cycle of eating.
Mindfulness-Based Eating Awareness Training (MB-EAT) is one intervention designed to promote mindful eating (20). MB-EAT draws on traditional mindfulness meditation techniques such as the raisin meditation and guided meditation to address issues pertaining to weight and eating-related self-regulation. The intervention addresses the role of hunger and satiety cues and stresses eating in response to those cues instead of eating in response to automatic patterns. Each intervention session incorporates meditation practice, particularly eating-related guided meditations, to focus attention on sensations, thoughts, and emotions related to hunger, satiety, and eating triggers. Several eating-related meditations use food, beginning with the raisin meditation, moving toward more complex foods, and culminating with making food choices mindfully between just two foods, then at a potluck meal, and finally at a restaurant buffet. “Mini” meditations are encouraged before eating as a way to bring awareness to the present moment. Participants are asked to take a few deep breaths, become aware of sensations in the body, including hunger, and then choose how to respond. The process can enable participants to think about which foods they want to eat and how much to eat based on their hunger level.
MB-EAT places an emphasis on inner wisdom (i.e., mindful awareness of inner experiences) and outer wisdom (i.e., personal use of nutrition knowledge and solutions to challenging situations) to help participants incorporate knowledge regarding the energy and nutrient content of food and individual health needs into everyday food choices. A core component of MB-EAT is a focus on the processes involved in sensory-specific satiety, in which taste buds decrease their sensitivity to taste after a relatively small amount of a food (21). Tuning into the immediate experience of taste and then becoming aware when the pleasure or satisfaction from a specific food decreases helps individuals maximize pleasure from smaller food portions. An example of this is provided in Table 1 (22).
TABLE 1.
Sample Mindful Eating Exercise (22)
| The next time you eat, select one food to pay attention to. This exercise is more effective if it is a food without a lot of complex flavors. |
| • Notice the taste of the food in the first bite. |
| • Then, take another bite. How does the taste change as you continue to chew? Is your enjoyment going up, down, or staying the same? At what point does the flavor begin to decrease? |
| • Continue to eat and notice how the taste continues to change. Tune in to the changing flavor. |
In summary, MB-EAT is designed to help individuals cultivate awareness of both internal and external triggers to eating, interrupt automatic eating, and eat in response to the natural physiological cues of hunger and satiety.
Are Mindful Eating Interventions Effective?
MB-EAT was originally developed for people with binge eating disorder (BED) (15). BED is characterized by frequent episodes of consuming unusually large quantities of food, followed by feelings of lack of control, distress, and guilt. Mindful meditation may modify the dysregulated processes associated with BED and be an effective treatment approach. Mindful eating also may be an effective intervention for minimizing weight gain and promoting weight loss given its focus on disrupting automatic eating (8). Table 2 summarizes the studies conducted to date that incorporated mindful eating meditation techniques as a primary intervention in adult samples. Two of the studies implemented MB-EAT for BED (15,21), two implemented an adaption of MB-EAT for non-BED samples (7,9), and a fifth implemented an intervention for obese individuals that incorporated MB-EAT elements (23). A sixth study specifically targeted restaurant eating to help participants develop self-regulation skills when dining out to prevent weight gain but was not adapted from the original MB-EAT curriculum (24).
TABLE 2.
Interventions Focused on Mindful Eating and Eating-Related Outcomes in Adult Samples
| Reference | Sample | Research Design | Mindfulness Intervention Components | Selected Results |
|---|---|---|---|---|
| Kristeller & Hallett, 1999 (15) | Women with BMI >27 kg/m2 with diagnosed BED (n = 18) | Pre- and post-test design with post-test assessment at 3-week follow-up; no comparison condition | MB-EAT intervention: seven group sessions included general, eating, and mini meditations; homework included daily meditation and mindful eating exercises | • Significant change at 3-week follow-up in frequency of binge episodes, eating control, hunger awareness, and satiety awareness* (all P <0.001) |
| Dalen et al., 2010 (23) | Adults (70% female) with BMI ≥30 kg/m2 recruited through YMCA (n = 10) | Pre- and post-test design with 3-month follow-up; no comparison condition | Mindful Eating and Living intervention: six weekly, 2-hour group sessions included sitting, eating, and walking meditations and light yoga; homework included 10 minutes daily of meditation and mindful eating practice | • Significant change at 3-month follow-up in cognitive restraint of eating (P = 0.03), disinhibited eating (P = 0.02), and scores on binge eating scale (P = 0.001) |
| Daubenmier et al., 2011 (9) | Premenopausal women with BMI 25–40 kg/m2 who reported being stressed (n = 47) | Randomized controlled trial with waitlist control condition | Included components of MB-EAT intervention: nine weekly, 2.5-hour group sessions and one 7-hour silent retreat included body scan, light yoga, and sitting, eating, loving kindness, and forgiveness meditations; homework included 30-minute meditations 6 days/week and mindful eating practice | • Significant difference between groups in the change in external-based eating (P = 0.046) • Significant reduction among obese participants only in the treatment group in cortisol awakening response (P = 0.03) |
| Kristeller et al., 2013 (21) | Adults (88% female) with BMI ≥28 kg/m2 meeting behavioral criteria for BED (n = 140) | Randomized controlled trial with 3- to 6-month follow-up; comparison conditions included psychoeducational cognitive-behavioral (PECB) treatment and waitlist control conditions | MB-EAT intervention: nine weekly and three monthly 1.5-hour group sessions included general, guided eating, mini, forgiveness, and walking meditations, seated yoga, body scan, and healing self-touch; homework included daily meditation and mindful eating practice | • Significant reduction in binge eating episodes and quantity of food consumed during binge for MB-EAT and PECB groups compared to control group at 1-month follow-up (all P <0.05). • Post-intervention difference occurred between MB-EAT and PECB in the change in hunger susceptibility (P <0.05), disinhibited eating (P <0.08), and food availability (P <0.07) |
| Miller et al., 2012; Miller et al., 2014 (7,12) | Adults (63% female) aged 35–65 years with type 2 diabetes ≥1 year, BMI ≥27 kg/m2, and A1C ≥7% (n = 68) | Randomized controlled trial with 1- and 3-month follow-up; comparison condition included DSME | MB-EAT-D intervention: eight weekly and two biweekly 2.5-hour group sessions included general, guided eating, mini, and forgiveness meditations and general information regarding nutrition and diabetes management; homework included meditation practice 6 days/week, mindful eating practice, and self-monitoring of food intake, activity, and glucose levels | • Significant reduction in weight, A1C, energy intake, glycemic index, and glycemic load for MB-EAT-D and DSME groups at 3-month follow-up (all P ≤0.03); significant increase in servings of vegetable and fruit/fruit juice post-intervention and meat, fish, poultry, and eggs at 3-month follow-up for MB-EAT-D (all P ≤0.03) • Significant reduction in eating self-efficacy, cognitive restraint of eating, disinhibited eating, and hunger susceptibility (all P <0.02) post-intervention and at 3-month follow-up for MB-EAT-D |
| Timmerman & Brown, 2012 (24) | Perimenopausal women aged 40–59 years who reported eating out ≥3 times/week (n = 43) | Randomized controlled trial with 6-week follow-up and waitlist control condition | Mindful Restaurant Eating intervention: six weekly, 2-hour group sessions included personalized weekly goals, mindful eating and guided mindfulness meditations, and principles of weight management to prevent weight gain | • Significant difference between groups post-intervention in mean energy and fat (grams) intake, diet-related self-efficacy, and barriers to managing intake when eating out (all P ≤0.02) |
Questionnaire(s) used to assess these outcomes are not specified. See study citations for a description of the other questionnaires used.
Study findings revealed significant improvement in dysregulated eating, including binge episodes and disinhibited eating (i.e., susceptibility to compulsive overeating), cognitive restraint of eating, and awareness of hunger cues post-intervention across studies (12,15,21,23). In the study conducted among adults with type 2 diabetes, the MB-EAT intervention was modified for diabetes self-management (MB-EAT-D), rather than for BED. The intervention incorporated training in mindful meditation, mindful eating, and bodily awareness of hunger and satiety cues. Basic information regarding energy, carbohydrate, and fat intake was provided to assist with diabetes management, and participants were encouraged to self-monitor food intake, physical activity, and glucose levels. Among participants randomized to MB-EAT-D, a significant but modest mean (± SE) reduction in weight (–1.53 ± 0.54 kg, P = 0.005) and significant improvement in A1C (–0.83 ± 0.24%, P = 0.0008) was observed 3 months after the intervention (7). Cognitive control or restraint toward eating, disinhibited eating, and eating self-efficacy also improved (all P <0.001) (12). Participants reported greater ability to minimize overeating in various situations and less eating beyond satiety (lower disinhibition). These findings indicate that training in mindful eating may help people with diabetes develop more healthful eating patterns.
Can Mindful Eating Be Incorporated Into DSME?
Given the findings regarding mindful eating effects on weight, A1C, and eating-related outcomes, incorporating principles from mindful eating may be beneficial in DSME (Table 3). Previous research has included a variety of meditation practices and suggests that mindfulness interventions become more effective for weight regulation when they specifically target eating behaviors (19). People may try to learn and practice meditation from a CD or book. However, it is usually more effective to practice meditation in a group with an instructor. Thus, group-based DSME classes could be a viable avenue for delivering mindful eating techniques. Diabetes educators or group facilitators should be trained in mindfulness meditation and have a consistent practice.
TABLE 3.
| Explore areas in which you could initiate a mindful eating approach to food consumption (e.g., during dinner at home). |
| • Identify a time during the day and location for practicing 10–20 minutes of sitting meditation (e.g., preferably in the morning in a quiet space in a chair or on the floor on a cushion) to focus on the breath. When your attention wanders, bring it back to the breath. Gradually increase the time spent in meditation practice. |
| • Practice doing mini meditations by focusing on the breath and becoming aware of bodily sensations of hunger and satiety before and during meals and snacks. |
| • Become aware of eating triggers such as thoughts, feelings, or environmental cues other than true hunger that prompt a desire to eat. Ask: “Am I truly hungry or do I want to eat for another reason?” |
| • Become aware of how hunger changes during a meal by noticing hunger before the meal and the sensations that occur as the meal progresses. |
| • Know when to stop eating by paying attention to the taste of a favorite food (e.g., potato chips). Notice when the flavor and enjoyment of the taste itself wanes. Identify when to stop eating. |
| • Experiment with eating other favorite foods (e.g., nuts or ice cream) mindfully by noticing the initial flavor, sensations during each bite, and when the initial burst of flavor wanes. |
| • Notice your hunger and fullness 5–10 minutes after completing a meal. Continue to check these sensations during the next 1–3 hours. What insights can be gained? |
| • Practice eating a meal mindfully at a restaurant. Consider what to order, engage in a mini meditation, assess your level of hunger, determine how much to eat once the meal arrives based on satiety and your enjoyment of the food, and check in regularly with your hunger and fullness as the meal progresses. |
| • Create a list of alternative coping strategies to use when you are triggered to engage in emotional eating (e.g., reading a book, engaging in a hobby, or calling a friend). |
| • Self-monitor and record your dietary intake and glucose levels before and 1–2 hours after meals to determine how food affects your postprandial glucose response. |
Caveats Regarding Mindfulness
A few caveats regarding mindfulness should be noted. First, as a rule, it is not enough to remind oneself to “just let go” to be mindful (16). In the early stages of becoming more mindful, most of us are unaware of our habitual eating patterns. One cannot immediately decide to live in the present moment and then instantly realize the state of being. Rather, a mindful state develops over time and with regular practice, both formally and informally, on a daily basis. Second, more DSME practitioners need to receive training in mindfulness and meditation to be able to offer this approach to a broader array of people with diabetes. Currently, there is no formal academic credentialing process; however, training is available through reputable institutions (Table 4). Third, the long-term impact of mindful eating on diabetes outcomes is unknown. Longer follow-up is needed to determine whether study participants continue to engage in mindful eating as a way of life. Fourth, most of the mindful eating research completed has been conducted in primarily female samples. More research is needed to identify better ways to attract men to these interventions and the acceptability and outcomes of a mindfulness approach among men. Finally, the field of mindful eating is in the early stages of empirical research. More work is needed to determine whether mindfulness mediates the relation between mindfulness training and the outcome of interest (e.g., weight regulation). Whether mindfulness is the mechanism by which mindfulness interventions work remains to be determined.
TABLE 4.
Websites Related to Mindfulness and Mindful Eating
| • Example of the raisin mindful eating exercise: http://hfhc.ext.WVU.edu/r/download/114469 |
| • Contemplative practice: https://www.mindandlife.org |
| • The Center for Mindful Eating: http://thecenterformindfuleating.org |
| • Mindfulness-Based Stress Reduction training programs: |
| ❍ University of Massachusetts Medical School, Center for Mindfulness in Medicine, Health Care and Society: http://www.umassmed.edu/cfm/training |
| ❍ Duke University Integrative Medicine Program: https://www.dukeintegrativemedicine.org/programs-training/public/mindfulness-based-stress-reduction |
| ❍ Shambhala organization: http://shambhala.org |
Conclusion
In summary, with greater awareness and attention to the present moment without judgment, individuals can respond reflexively rather than continue habitual patterns of eating and behavior that may be inconsistent with their goals and health needs. Mindfulness provides the opportunity to gain insight and reduce the pain and suffering commonly experienced with dysregulated eating. Incorporating mindfulness into DSME could be a novel approach and offer people with diabetes greater choices in meeting their self-management needs and goals.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002–2012. National Health Statistics Reports no. 79. Hyattsville, Md, National Center for Health Statistics, 2015 [PMC free article] [PubMed] [Google Scholar]
- 2.Tovote KA, Fleer J, Snippe E, et al. Individual mindfulness-based cognitive therapy and cognitive behavior therapy for treating depressive symptoms in patients with diabetes: results of a randomized controlled trial. Diabetes Care 2014;37:2427–2434 [DOI] [PubMed] [Google Scholar]
- 3.Hartmann M, Kopf S, Kircher C, et al. Sustained effects of a mindfulness-based stress-reduction intervention in type 2 diabetic patients: design and first results of a randomized controlled trial (the Heidelberger Diabetes and Stress Study). Diabetes Care 2012;35:945–947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Son J, Nyklicek I, Pop VJ, et al. The effects of a mindfulness-based intervention on emotional distress, quality of life and HbA1c in outpatients with diabetes (DiaMind): a randomized controlled trial. Diabetes Care 2013;36:823–830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Noordali F, Cumming J, Thompson JL. Effectiveness of mindfulness-based interventions on physiological and psychological complications in adults with diabetes: a systematic review. J Health Psychol 2015. Epub ahead of print (DOI: 10.1177/1359105315620293) [DOI] [PubMed] [Google Scholar]
- 6.Rosenzweig S, Reibel DK, Greeson JM, et al. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Altern Ther Health Med 2007;13:36–38 [PubMed] [Google Scholar]
- 7.Miller CK, Kristeller JL, Headings A, Nagaraja H, Miser WF. Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a pilot study. J Acad Nutr Diet 2012;112:1835–1842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olson KL, Emery CF. Mindfulness and weight loss: a systematic review. Psychosom Med 2015;77:59–67 [DOI] [PubMed] [Google Scholar]
- 9.Daubenmier J, Kristeller J, Hecht FM, et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: an exploratory randomized controlled study. J Obes 2011;2011:651936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daubenmier J, Lin J, Blackburn E, et al. Changes in stress, eating, and metabolic factors are related to changes in telomerase activity in a randomized mindfulness intervention pilot study. Psychoneuroendocrinology 2012;37:917–928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev 2014;15:453–461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller CK, Kristeller JL, Headings A, Nagaraja H. Comparison of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a randomized controlled trial. Health Educ Behav 2014;12:145–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jordan CH, Wang W, Donatoni L, Meier BP. Mindful eating: trait and state mindfulness predict healthier eating behavior. Pers Individ Dif 2014;68:107–111 [Google Scholar]
- 14.Beshara M, Hutchinson AD, Wilson C. Does mindfulness matter? Everyday mindfulness, mindful eating and self-reported serving size of energy dense foods among a sample of South Australian adults. Appetite 2013;67:25–29 [DOI] [PubMed] [Google Scholar]
- 15.Kristeller JL, Hallett CB. An exploratory study of a meditation-based intervention for binge eating disorder. J Health Psychol 1999;4:357–363 [DOI] [PubMed] [Google Scholar]
- 16.Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract 2003;10:144–156 [Google Scholar]
- 17.Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract 2004;11:230–241 [Google Scholar]
- 18.Forman EM, Shaw JA, Goldstein SP, et al. Mindful decision making and inhibitory control training as complementary means to decrease snack consumption. Appetite 2016;103:176–183 [DOI] [PubMed] [Google Scholar]
- 19.Mantzios M, Wilson JC. Mindfulness, eating behaviours, and obesity: a review and reflection on current findings. Curr Obes Rep 2015;4:141–146 [DOI] [PubMed] [Google Scholar]
- 20.Kristeller JL, Wolever RQ. Mindfulness-based eating awareness training for treating binge eating disorder: the conceptual foundation. Eat Dis 2011;19:49–61 [DOI] [PubMed] [Google Scholar]
- 21.Kristeller J, Wolever RQ, Sheets V. Mindfulness-based eating awareness training (MB-EAT) for binge eating: a randomized clinical trial. Mindfulness 2014;5:282–297 [Google Scholar]
- 22.Kristeller J. The Joy of Half a Cookie. New York, N.Y., Perigee, 2015 [Google Scholar]
- 23.Dalen J, Smith BW, Shelley BM, Sloan AL, Leahigh L, Begay D. Pilot study: mindful eating and living (MEAL): weight, eating behavior, and psychological outcomes associated with a mindfulness-based intervention for people with obesity. Complement Ther Med 2010;18:260–264 [DOI] [PubMed] [Google Scholar]
- 24.Timmerman GM, Brown A. The effect of a mindful restaurant eating intervention on weight management in women. J Nutr Educ Behav 2012;44:22–28 [DOI] [PMC free article] [PubMed] [Google Scholar]