Abstract
Background
Imported malaria is an increasing problem. The arrival of 224 African refugees presented the opportunity to investigate the diagnosis and management of imported malaria within the Quebec health care system.
Methods
The refugees were visited at home 3–4 months after arrival in Quebec. For 221, a questionnaire was completed and permission obtained for access to health records; a blood sample for malaria testing was obtained from 210.
Results
Most of the 221 refugees (161 [73%]) had had at least 1 episode of malaria while in the refugee camps. Since arrival in Canada, 87 (39%) had had symptoms compatible with malaria for which medical care was sought. Complete or partial records were obtained for 66 of these refugees and for 2 asymptomatic adults whose children were found to have malaria: malaria had been appropriately investigated in 55 (81%); no malaria smear was requested for the other 13. Smears were reported as positive for 20 but confirmed for only 15 of the 55; appropriate therapy was verified for 10 of the 15. Of the 5 patients with a false-positive diagnosis of malaria, at least 3 received unnecessary therapy. Polymerase chain reaction testing of the blood sample obtained at the home visit revealed malaria parasites in 48 of the 210 refugees (23%; 95% confidence interval [CI] 17%– 29%). The rate of parasite detection was more than twice as high among the 19 refugees whose smears were reported as negative but not sent for confirmation (47%; 95% CI 25%– 71%).
Interpretation
This study has demonstrated errors of both omission and commission in the response to refugees presenting with possible malaria. Smears were not consistently requested for patients whose presenting complaints were not “typical” of malaria, and a large proportion of smears read locally as “negative” were not sent for confirmation. Further effort is required to ensure optimal malaria diagnosis and care in such high-risk populations.
In many industrialized countries, the incidence of imported malaria is rising because of changing immigration patterns and refugee policies as well as increased travel to malaria-endemic regions.1,2,3,4,5,6,7,8,9,10 Imported malaria is not rare in Canada (300–1000 cases per year),3 the United States2,3,4 or other industrialized countries.5,6,7,8,9,10 Malaria can be a serious challenge in these countries because of its potentially rapid and lethal course.11,12,13,14 The task of front-line health care providers is made particularly difficult by the protean clinical presentations of malaria. Classic periodic fevers (tertian or quartan) are seen infrequently.9,15,16,17,18,19 Atypical and subtle presentations are especially common in individuals who have partial immunity (e.g., immigrants and refugees from disease-endemic areas) or are taking malaria prophylaxis (e.g., travellers).9,16,17 Even when malaria is considered, an accurate diagnosis can remain elusive or can be delayed as a result of inadequate or distant specialized laboratory support.19,20
In Quebec, the McGill University Centre for Tropical Diseases collaborates with the Laboratoire de santé publique du Québec to raise awareness of imported malaria, to offer training and quality-assurance testing, and to provide reference diagnostic services. A preliminary diagnosis is typically made by the local laboratory, and smears (with or without staining) are sent to the McGill centre, where they are reviewed within 2–48 hours, depending on the urgency of the request. Initial medical decisions are usually based on local findings and interpretations. Although malaria is a reportable disease, there is no requirement to use the reference service.
On Aug. 9, 2000, 224 refugees from Tanzanian camps landed in Montréal aboard an airplane chartered by Canadian immigration authorities. Over the ensuing 5 weeks, the McGill University Centre for Tropical Diseases noted an increase in demand for malaria reference services and an apparent small “epidemic” of imported malaria. This “epidemic” prompted us to investigate the performance of the health care system in the diagnosis and management of imported malaria.
Methods
Refugee families were contacted by Quebec immigration authorities; all agreed to a home visit. Home visits were completed 3–4 months (mean 105 days) after the refugees' arrival in Quebec. For 221 of the 224 refugees, demographic and clinical information (e.g., on malaria prophylaxis and treatment and on health care contacts since arrival) was collected on a questionnaire, a release-of-information form was completed, and records for all health care contacts (office, clinic and hospital) were requested; a blood sample was obtained by heel or finger prick or venepuncture from 210 and anticoagulated with ethylenediamine tetra-acetates) for malaria testing by microscopic examination (Giemsa-stained thin and thick smears), antigen capture assays (OptiMAL, Portland, Ore., and ICT, Brookvale, Australia), and pan-species and species-specific polymerase chain reaction (PCR).21,22
The study was approved by the Research Ethics Committee of the McGill University Health Centre at the Montréal General Hospital.
Results
In Quebec, refugees are typically dispersed in family groups to smaller communities or metropolitan-area suburbs throughout the province. For the group studied, the host communities were relatively small (median population 60 000, range 18 000–1.5 million).23 For almost 40% of the group, the communities had populations of less than 100 000 and no tertiary-care hospital.
During the 5 weeks after arrival of the refugees, the McGill University Centre for Tropical Diseases received 36 requests for laboratory confirmation and many telephone consultations for diagnosis and treatment of malaria. Of the 36 submitted slides, 15 were confirmed as positive, 11 for Plasmodium falciparum (parasitemia [proportion of blood cells containing parasites] range 0.3%–7%).22
The refugees had been airlifted from camps in Tanzania but originated from Burundi (52%), the Democratic Republic of the Congo (39%), Rwanda (5%) and Tanzania (4%). Of the 221 studied, 124 were male and 97 female. The mean age was 17 (range < 1–51) years; more than half (128/221) were 15 years of age or younger. The mean stay in a refugee camp was 3.1 (range 1–7) years. Of the 221 refugees, 161 (73%) had had at least 1 episode of clinical malaria and a variety of treatments while in the refugee camps. Few (38 [17%]) had taken malaria prophylaxis in the camps, and the regimens had been suboptimal (e.g., chloroquine or sulfadoxine– pyrimethamine).24,25 Bed nets had not been used.
Of the 221 refugees, 87 (39%) had had symptoms compatible with malaria (Table 1), for which they had sought medical care at hospitals or clinics, during their first 3– 4 months in Canada. No significant differences other than pregnancy existed between these 87 refugees and the other 134. Most had sought care within 30 days of arrival (median 14, range 2– 118 days). The median duration of symptoms before care was sought was 3.5 (range 1– 10) days. Complete or partial medical records were obtained for 66 of the 87 refugees and for 2 asymptomatic adults whose children were found to have malaria. There were no major demographic differences between these 68 subjects and the 21 whose records could not be reviewed.
Table 1
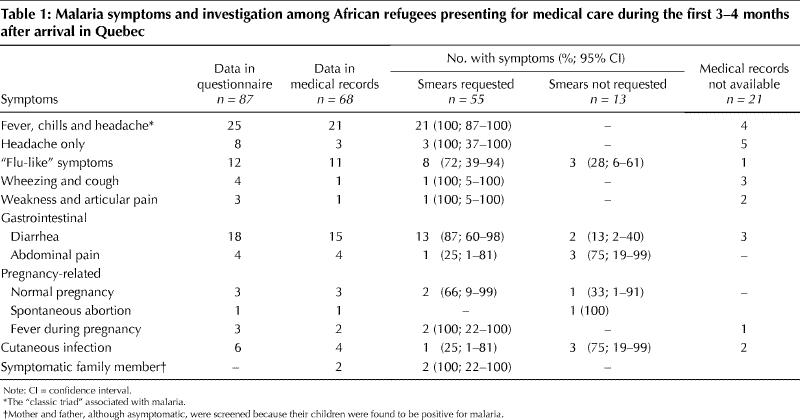
According to the medical records, malaria was investigated by thin and thick smears in 55 of the 68 subjects; no record of a malaria smear could be found for the other 13. Malaria testing was requested for all 21 refugees presenting with “classic” malaria symptoms (high fever, chills and headache) but not for 3 of the 11 refugees with “flu-like” symptoms, 5 of the 19 children with gastrointestinal complaints or the 1 woman with a spontaneous abortion.
A probable diagnosis of malaria was made by primary laboratories for 20 of the 68 refugees whose records were available for review (Fig. 1). Most reports (15/20) stated simply “malaria” or “malaria species”; the remainder identified P. falciparum. Parasitemia was estimated in only 5 of the reports: mean 1.8% ± 2%, range 0.001%– 5%. Three-quarters of the 20 probable diagnoses were confirmed by the McGill University Centre for Tropical Diseases: as P. falciparum (11), P. ovale (2) and mixed P. falciparum/P. ovale (2) infections. Of the 15 confirmed cases, 7 were in children 15 years of age or younger, 6 of whom had “classic” malaria symptoms. In 3 of the 5 false-positive cases, the symptoms were also typical for malaria; the other 2 refugees were pregnant women. Only 1 person (an adult) with the classic triad of fever, chills and headache had a negative smear and an unconfirmed diagnosis. Most of the remaining negative smears were from people with “flu-like” symptoms, gastrointestinal complaints or weakness. From the medical records, appropriate therapy was verified in only 10 of the 15 confirmed cases; at least 3 of the 5 patients with a false-positive initial diagnosis received antimalarial drugs inappropriately.
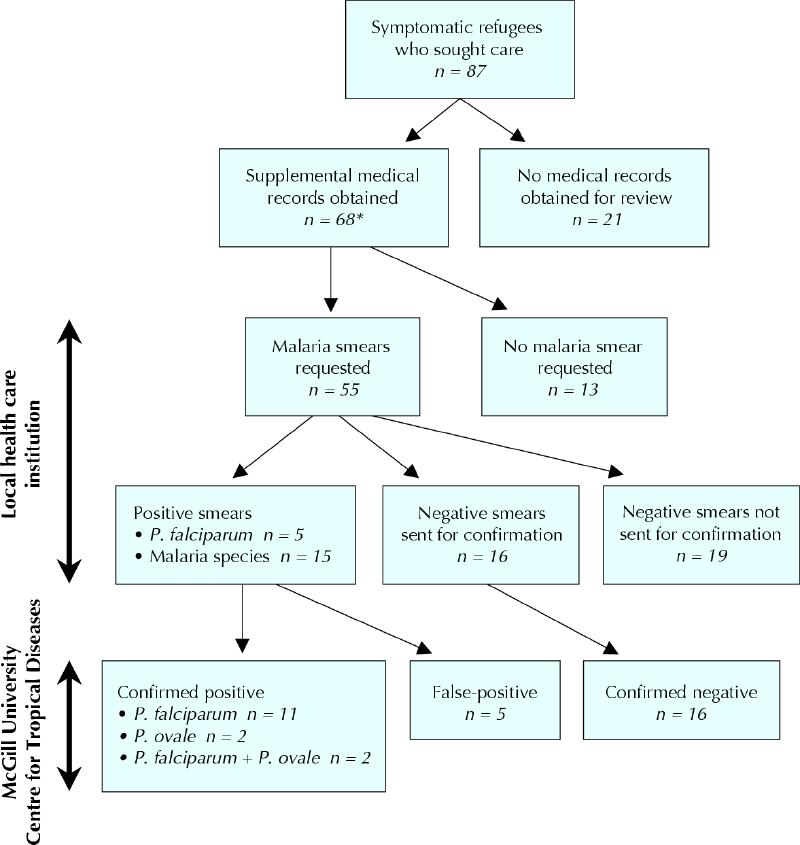
Fig. 1: Laboratory investigation for possible malaria among 87 African refugees in Quebec who sought health care because of symptoms compatible with malaria. P = Plasmodium. *Includes 2 asymptomatic adults whose children were found to have malaria.
Malaria infection was documented by PCR in 48 of the 210 refugees who provided a blood sample for the study (23%; 95% confidence interval [CI] 17%–29%). Of the 13 for whom malaria testing had never been requested, 3 (23%; 95% CI 6%– 54%) were PCR-positive for P. falciparum. Of the 19 for whom a negative malaria smear had been reported but not confirmed, 9 (47%; 95% CI 25%– 71%) were PCR-positive for P. falciparum. The rate of parasite detection among the 134 refugees who had not sought medical care during their first 3– 4 months in Canada was 18% (95% CI 12%– 26%).
Interpretation
The number of imported malaria cases in industrialized countries is steadily increasing because of shifting immigration patterns and refugee policies as well as changes in business and leisure travel.2,3,4,5,6,7,8,9,10 There is currently no consensus on the best approach to screening immigrants and refugees for malaria. Possible approaches include the status quo (no screening), mass antimalaria treatment and “screen-and-treat” protocols.26,27,28,29,30
Immigration policies can influence when, where and how malaria will present in immigrants and refugees. For example, the policy of dispersing family groups to communities throughout Quebec had a striking impact on the pattern of malaria cases that we observed. Indeed, the McGill University Centre for Tropical Diseases was first alerted by the unusual distribution of requests for reference services rather than by a change in request volume. As might be expected under these conditions,19,31 we identified several errors of omission (e.g., failure to suspect malaria and failure to determine parasite species) as well as errors of commission (e.g., inappropriate therapy). “Classic” clinical presentations of malaria are often not observed in populations of immigrants and refugees.9,15,16,17,18,19 The rate of failure to request a malaria smear in symptomatic cases was particularly high in our study (19% [13/68]) compared with previous studies,32 which suggests a lack of experience in the treating institutions in Quebec. These lapses were particularly disturbing because 7 of the 13 cases were in children and pregnant women, groups most vulnerable to malaria complications.15,33,34
Even when appropriate smears were requested, diagnostic problems still arose despite several years of effort to improve diagnostic capabilities through training and a targeted quality-assurance (QA) program. Although it was encouraging that 15 of the 20 “positive” slides sent to the McGill tropical diseases centre were confirmed as positive, only 5 primary laboratories felt confident enough to identify the parasite species. Lack of precision can result in overtreatment and undertreatment of malaria19,31,35,36 and, occasionally, deaths.12,13,14 Overtreatment is the logical consequence of a false-positive diagnosis, as occurred in 3 of the 5 such cases that we identified. In a recent QA exercise, 2% of Ontario laboratories reported negative smears as malaria-positive,35 whereas Quebec data suggested a false-positive rate of up to 7% and a false-negative rate of 25%– 40% for smears with low parasite densities (McGill University Centre for Tropical Diseases–Laboratoire de santé publique du Québec QA program: unpublished data, 2002). Preparation of both thin and thick smears and regular training have been identified as major determinants of malaria diagnostic competence.19,35,36,37,38 False-positive diagnoses are the least troubling errors we identified, however, since malaria treatments are relatively nontoxic, and a bias to treat symptomatic individuals is appropriate.
False-negative results, on the other hand, are a major concern. Unfortunately, the true malaria status of the 19 refugees whose smears were reported as negative but not sent for confirmation is unknown. More than twice as many of these subjects (47%; 95% CI 25%– 71%) than of the 134 refugees who had not sought medical care (18%; 95% CI 12%– 26%) were PCR-positive at the time of the home visit. The likelihood that many of the refugees in this study were partially immune certainly contributed to the challenges for clinicians (subtle presentations)9,16,17,18,19 and laboratories (low parasitemia)19,35,36 and may explain why no deaths or complications occurred.
A similar refugee-associated malaria “outbreak” has been reported in the United States,31 and it is likely that similar small “outbreaks” associated with immigrants and refugees occur regularly but go unrecognized.3 In our assessment of how Quebec's health care system managed imported malaria, we have demonstrated that errors of both omission and commission continue to occur despite a comprehensive, province-wide program to enhance malaria diagnostic competence. This study has also highlighted limitations in record-keeping (e.g., missing information on malaria treatment) and the fact that decisions taken by immigration authorities at various levels of government (e.g., on screening and refugee-settlement policies) can have a significant impact on the management of such “exotic” infections. Our findings suggest that screening for malaria should be considered for refugees from malaria-endemic regions and further emphasize the importance of continued education of both medical and laboratory staff about imported malaria.
Acknowledgments
We thank Lyne Cedilotte, Irene McArthur and Ewa Rydzik for their technical assistance. We also thank Neil Heywood at Citizenship and Immigration Canada and Suzanne Jutras at Immigration-Québec, and their colleagues, for their assistance in approaching and communicating with the refugees.
Footnotes
This article has been peer reviewed.
Contributors: All of the authors participated in the design and conduct of the study and in critical review of the manuscript. Momar Ndao was responsible for polymerase chain reaction diagnostics and helped with the data analysis. Etienne Bandyayera organized the database, performed all statistical tests and wrote the first draft. Evelyne Kokoskin was responsible for smear and antigen diagnostics. Theresa Gyorkos supervised creation of the data set and data analysis. David Diemert assisted in patient recruitment, interviews and specimen collection. Dick MacLean supervised clinical laboratory analyses. Ron St. John helped secure access to subjects, secured funding and assisted in study logistics. Brian Ward was responsible for the overall project concept and completion.
This study was supported by Health Canada grants 4500013744, 222000-02201-20HG-254000 and HT070-010033. It was presented in part at the 60th meeting of the American Society for Tropical Medicine and Hygiene in Denver, Colo., in December 2002.
Competing interests: None declared.
Correspondence to: Dr. Brian Ward, McGill University Centre for Tropical Diseases, Montréal General Hospital, 1650 Cedar Ave., Rm. D7-153, Montréal QC H3G 1A4; fax 514 934-8347; brian.ward@mcgill.ca
References
- 1.Sachs JD. A new global effort to control malaria. Science 2002;298:122-4. [DOI] [PubMed]
- 2.Freedman DO. Imported malaria: here to stay. Am J Med 1992;93:239-42. [DOI] [PubMed]
- 3.MacLean JD, Demers AM, Ndao M, Kokoskin E, Ward BJ, Gyorkos TW. Twenty years of malaria surveillance in Canada: epidemics missed, lessons learned. Emerg Infect Dis 2004;10:1195-201. [DOI] [PMC free article] [PubMed]
- 4.Jerrard DA, Broder JS, Hanna JR, Colletti JE, Grundmann KA, Geroff AJ, et al. Malaria: a rising incidence in the United States. J Emerg Med 2002;23:23-33. [DOI] [PubMed]
- 5.Kockaerts Y, Vanhees S, Knockaert DC, Verhaegen J, Lontie M, Peetermans WE. Imported malaria in the 1990s: a review of 101 patients. Eur J Emerg Med 2001;8:287-90. [DOI] [PubMed]
- 6.Kain KC, Keystone JS. Malaria in travelers. Epidemiology, disease and prevention. Infect Dis Clin North Am 1998;12:267-84. [DOI] [PubMed]
- 7.Williams JP, Chitre M, Sharland M. Increasing Plasmodium falciparum malaria in southwest London: a 25 year observational study. Arch Dis Child 2002; 86: 428-30. [DOI] [PMC free article] [PubMed]
- 8.Legros F, Danis M. Surveillance of malaria in European Union countries. Euro Surveill 1998;3:45-7. [DOI] [PubMed]
- 9.Robinson P, Jenney AW, Tachado M, Yung A, Manitta J, Taylor K, et al. Imported malaria treated in Melbourne, Australia: epidemiology and clinical features in 246 patients. J Travel Med 2001;8:76-81. [DOI] [PubMed]
- 10.Nakamura-Uchiyama F, Hiromatsu K, Ishiwata K, Sakamoto Y, Nawa Y. The current status of parasitic diseases in Japan. Intern Med 2003;42:222-36. [DOI] [PubMed]
- 11.Bruneel F, Hocqueloux L, Alberti C, Wolff M, Chevret S, Bedos JP, et al. The clinical spectrum of severe imported falciparum malaria in the intensive care unit: report of 188 cases in adults. Am J Respir Crit Care Med 2003; 167: 684-9. [DOI] [PubMed]
- 12.Kain KC, MacPherson DW, Kelton T, Keystone JS, Mendelson J, MacLean JD. Malaria deaths in visitors to Canada and in Canadian travellers: a case series. CMAJ 2001;164(5):654-9. [PMC free article] [PubMed]
- 13.Stoppacher R, Adams SP. Malaria deaths in the United States: case report and review of deaths, 1979-8. J Forensic Sci 2003;48:404-8. [PubMed]
- 14.Humar A, Sharma S, Zoutman D, Kain CK. Fatal falciparum malaria in Canadian travellers. CMAJ 1997;156(8):1165-7. [PMC free article] [PubMed]
- 15.Taylor TE, Strickland GT. Malaria. In: Strickland GT, editor. Hunter's tropical medicine and emerging infectious diseases. Philadelphia: WB Saunders; 2000. p. 614-42.
- 16.Svenson JE, MacLean JD, Gyorkos TW, Keystone J. Imported malaria. Clinical presentation and examination of symptomatic travelers. Arch Intern Med 1995;155:861-8. [DOI] [PubMed]
- 17.Van den Ende J, Morales I, Van den Abbeele K, Clerinx J, Colebunders R, Kager P, et al. Changing epidemiological and clinical aspects of imported malaria in Belgium. J Travel Med 2001;8:19-25. [DOI] [PubMed]
- 18.Chandramoham D, Jaffar S, Greenwood B. Use of clinical algorithms for diagnosing malaria. Trop Med Int Health 2002;7:45-52. [DOI] [PubMed]
- 19.Kain KC, Harrington MA, Tennyson S, Keystone JS. Imported malaria: prospective analysis of problems in diagnosis and management. Clin Infect Dis 1998;27:142-9. [DOI] [PubMed]
- 20.Viani RM, Bromberg K. Pediatric imported malaria in New York: delayed diagnosis. Clin Pediatr (Phila) 1999;38:333-7. [DOI] [PubMed]
- 21.Snounou G. Detection and identification of the four malaria parasite species infecting humans by PCR amplification. Methods Mol Biol 1996;50:263-91. [DOI] [PubMed]
- 22.Ndao M, Bandyayera E, Kokoskin E, Gyorkos TW, Ward BJ. Malaria outbreak in Quebec, Canada: comparison of blood smear, antigen detection and nested PCR for screening refugees from malaria endemic regions. J Clin Microbiol 2004;42:2694-700. [DOI] [PMC free article] [PubMed]
- 23.Institut de la statistique du Québec, Gouvernement du Québec. 2001 census. Available: www.stat.gouv.qc.ca/regions/index_2001_an.htm (accessed 2004 Oct 18).
- 24.East African Network for Monitoring Antimalarial Treatment (EANMAT). Monitoring antimalarial drug resistance within national malaria control programmes: the EANMAT experience. Trop Med Int Health 2001;6:891-8. [DOI] [PubMed]
- 25.Roper C, Pearce R, Bredenkamp B, Gumede J, Drakeley C, Mosha F, et al. Antifolate antimalarial resistance in southeast Africa: a population-based analysis. Lancet 2003;361:1174-81. [DOI] [PubMed]
- 26.Slutsker L, Tipple M, Keane V, McCance C, Campbell CC. Malaria in East African refugees resettling to the United States; development of strategies to reduce the risk of imported malaria. J Infect Dis 1995;171:489-93. [DOI] [PubMed]
- 27.Miller JM, Boyd HA, Ostrowski SR, Cookson ST, Parise ME, Gonzaga PS, et al. Malaria and intestinal parasites and schistosomiasis among Barawan Somali refugees resettling to the United States: a strategy to reduce morbidity and decrease the risk of imported infections. Am J Trop Med Hyg 2000; 62: 115-21. [DOI] [PubMed]
- 28.Stauffer WM, Kamat D, Walker P. Screening of international immigrants, refugees, and adoptees. Prim Care 2002;29:879-905. [DOI] [PubMed]
- 29.Paxton LA, Slutsker L, Schultz LJ, Luby SP, Meriwether R, Matson P, et al. Imported malaria in Montagnard refugees settling in North Carolina: implications for prevention and control. Am J Trop Med Hyg 1996;54:54-7. [DOI] [PubMed]
- 30.Sullivan P. Poor conditions in refugee camps make malaria screening difficult: expert. CMAJ 2000;163(8):1036. [PMC free article] [PubMed]
- 31.Molyneux M, Fox R. Diagnosis and treatment of malaria in Britain. BMJ 1993;306:1175-80. [DOI] [PMC free article] [PubMed]
- 32.Gimnig JE, Vulule JM, Lo TQ, Kamau L, Kolczak MS, Phillips-Howard PA, et al. Impact of permethrin-treated bed nets on entomologic indices in an area of intense year-round malaria transmission. Am J Trop Med Hyg 2003; 68: 16-22. [PubMed]
- 33.Okoko BJ, Enwere G, Ota MO. The epidemiology and consequences of maternal malaria: a review of immunological basis. Acta Trop 2003;87:193-205. [DOI] [PubMed]
- 34.Brabin JB, Ganley Y. Imported malaria in children in the UK. Arch Dis Child 1997; 77:76-81. [DOI] [PMC free article] [PubMed]
- 35.Thomson S, Lohmann RC, Crawford L, Dubash R, Richardson H. External quality assessment in the examination of blood films for malarial parasites within Ontario, Canada. Arch Pathol Lab Med 2000;124:57-60. [DOI] [PubMed]
- 36.Hawthorne M, Chiodini PL, Snell JJ, Moody AH, Ramsay A. Parasitology: United Kingdom National Quality Assessment Scheme. J Clin Pathol 1992; 45: 968-74. [DOI] [PMC free article] [PubMed]
- 37.Makler MT, Gibbins B. Laboratory diagnosis of malaria. Clin Lab Med 1991;11:941-56. [PubMed]
- 38.Hemme F, Gay F. Internal quality control of the malaria microscopy diagnosis for 10 laboratories on the Thai–Myanmar border. Southeast Asian J Trop Med Public Health 1998;29:529-36. [PubMed]


