Abstract
Objectives: Few studies have assessed how the diagnostic criteria for posttraumatic stress disorder (PTSD) apply to older children and adolescents. With the introduction of a new, developmentally sensitive set of criteria for very young children (age 6 years and younger) in Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), this raises new questions about the validity of the criteria for older children and adolescents. The current study investigated how diagnostic changes in DSM-5 impact diagnosis rates in 7–18-year olds.
Methods: PTSD, impairment, and comorbid psychopathology were assessed in 135 trauma-exposed, treatment-seeking participants. Children (ages 7–12) were examined separately from adolescents (ages 13–18) to assess for potential developmental differences.
Results: A significantly higher proportion of 7–12-year-old children met criteria for DSM-5 diagnosis (53%) compared to Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) (37%). However, among 13–18-year-old adolescents, the proportions diagnosed with DSM-5 (73%) and DSM-IV (74%) did not differ. Participants who met criteria for DSM-5 only (17%) did not differ from those diagnosed with DSM-IV in terms impairment or comorbidity. Using the newly accepted age 6 years and younger criteria resulted in a significantly higher proportion of 7–12-year-old (but not 13–18-year olds) children meeting criteria compared to DSM-IV or DSM-5. However, these children showed less impairment and comorbidity than those diagnosed with DSM-IV.
Conclusion: These findings suggest that DSM-5 criteria may be more developmentally sensitive than DSM-IV criteria, and may lead to higher prevalence rates of PTSD for 7–12-year-old children, but not for adolescents. Using the very young children criteria for 7–12-year-old children may further increase prevalence, but capture children with less severe psychopathology.
Keywords: : posttraumatic stress disorder, DSM-5, diagnostic criteria, children, adolescents
Introduction
In response to a growing body of literature on the diagnostic criteria for posttraumatic stress disorder (PTSD), several substantial changes were made in the most recent version of the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5; American Psychiatric Association 2013). Perhaps the most important to child psychology and psychiatry was the inclusion of a separate set of developmentally appropriate criteria for very young children (age 6 years and younger). However, children aged 7–18 continue to be evaluated for PTSD using the same criteria as adults. Using adult criteria for children may be developmentally inappropriate, and may result in underdiagnosis. The goal of the current study was to investigate how the diagnostic changes in the DSM-5 impact diagnosis rates within a trauma-exposed, treatment-seeking sample of 7–18-year-old children.
Changes to the PTSD criteria in DSM-5 include the deletion, addition, clarification, and reorganization of symptoms. In cluster A, the definition of a trauma was clarified such that sexual violence and repeated exposure to aversive details (among first responders, for example) are specifically mentioned, and learning a trauma has occurred to a family member or close friend has been added. Criterion A2, which required a person to respond to the trauma with intense fear, helplessness, or horror, was deleted in response to research showing that the presence (or absence) of this symptom was irrelevant for the development of PTSD (Brewin et al. 2000; Karam et al. 2010; Bovin and Marx 2011; Friedman et al. 2011). Cluster B intrusion symptoms remained largely unchanged, although minor clarifications were made. Influenced by factor analytic work supporting a four-factor structure over a three-factor structure of PTSD symptoms (King et al. 1998; Asmundson et al. 2000; McWilliams et al. 2005; Saul et al. 2008), the avoidance/numbing symptoms were divided into two clusters; an avoidance cluster (cluster C) and a negative alterations in cognitions and mood cluster (cluster D). Although the avoidance symptoms are only slightly reworded, now at least one avoidance symptom is required for a diagnosis (Friedman 2013). Two symptoms were added to cluster D, including distorted cognitions about the trauma resulting in self-blame or blaming others, and a persistent negative emotional state. In addition, the symptom regarding a sense of foreshortened future has been expanded to include persistent and exaggerated negative beliefs about oneself, others, or the world. Finally, the arousal and reactivity cluster, now cluster E, includes an additional symptom of reckless or self-destructive behavior (Miller et al. 2004; Cavanaugh et al. 2010; Cavanaugh 2013).
In addition to the changes described above, the DSM-5 also outlined a separate set of PTSD diagnostic criteria for very young children (age 6 years and younger). The Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV; American Psychiatric Association 2000) acknowledged developmental differences in children with “notes” included with several PTSD symptoms, but the diagnostic algorithm applied to children was the same as for adults. Furthermore, no children younger than the age of 15 were included in the DSM-IV field trials (Kilpatrick et al. 1998). There was concern in the field that some symptoms were developmentally inappropriate for children (Scheeringa et al. 1995; Perrin et al. 2000; Pynoos et al. 2009), and research showed that using the DSM-IV criteria in very young children resulted in very low rates of children meeting criteria despite being highly symptomatic (Scheeringa et al. 2011). Alternative criteria for very young children were proposed, in which symptoms were adjusted to be more behaviorally anchored and developmentally sensitive, and thresholds were adjusted to be more lenient. Given that very young children lack the verbal and abstract cognitive abilities to articulate their internal experiences, recommendations included dropping criterion A2 and only requiring one avoidance/numbing symptom. Also, other symptoms were revised to include child appropriate manifestations of behavior, such as including social withdrawal as a sign of feelings of detachment, and adding temper tantrums as an example of irritable behavior with angry outbursts.
Several studies suggested the revised criteria were more developmentally appropriate and successfully captured the highly symptomatic children who did not meet diagnosis using DSM-IV criteria (De Young et al. 2011; Scheeringa et al. 2012), and these changes were adopted by the DSM-5 for very young children. While this represents a major step in improving PTSD criteria to be developmentally sensitive, there remains a gap in the literature. Relatively little research has examined the diagnostic criteria for PTSD in children ages 7–18 (Scheeringa et al. 2011). Some research supports separating avoidance and numbing symptoms in this age group (Yule et al. 1994; Anthony et al. 1999; Saul et al. 2008), similar to the revised four-factor structure found in adults and used in DSM-5. Other work suggests the DSM-IV criteria may have been too stringent for school-age children, but more appropriate for adolescents (Scheeringa et al. 2006). Developmentally, school-age children may have difficulty understanding emotions, and linking thoughts and emotions, which results in a limited ability to report their experience and their emotions (Salmon and Bryant 2002). As such, it has been suggested that the three-symptom threshold for DSM-IV criterion C may have been too high for school-age children, but appropriate for adolescents (Scheeringa et al. 2006, 2011). If this is the case, the DSM-5 criteria for very young children, which require only one avoidance/negative alternation in cognitions symptom, may be more suitable for school-age children, while the adult DSM-5 PTSD criteria may be appropriate for adolescents.
A few studies have compared DSM-IV criteria to DSM-5 criteria in older adolescents and young adults. In an online survey of 585 nonclinical college students, Elhai et al. (2012) found no significant differences between DSM-IV and DSM-5 prevalence estimates. However, this study was conducted using an early draft of DSM-5 criteria, which were more stringent, requiring three cluster D and three cluster E symptoms for diagnosis rather than two symptoms in each. Carmassi et al. (2013) compared criteria using self-reported symptoms in a nonclinical sample of 512 high school seniors who had survived an earthquake. Results showed only a slightly higher DSM-5 prevalence rate (39.8% vs. 37.5%) with good consistency across DSM-IV and DSM-5 (kappa = 0.73). In a sample of 325 adolescents and young adults who survived a terrorist attack, Hafstad et al. (2014) showed that using DSM-IV and DSM-5 criteria resulted in similar prevalence rates (11.1% and 11.75%, respectively), but overlap was poor. That is, of those who met DSM-IV criteria, 41% did not meet DSM-5 criteria, and of those who met DSM-5 criteria, 42% did not meet DSM-IV criteria. Overall, the research comparing DSM-IV to DSM-5 PTSD criteria in older adolescents suggests only slightly higher DSM-5 prevalence rates, but the actual level of overlap remains unclear. However, most of these studies combine older adolescents with young adults, and to our knowledge, no study to date has used a treatment-seeking sample of adolescents.
In a literature search using PsycINFO (search terms [posttraumatic stress disorder OR PTSD] AND DSM-5 AND children), the authors found only one study comparing DSM-IV to DSM-5 criteria in 7–12-year-old children. Danzi and La Greca (2016) used two samples of 7–11-year-old children exposed to hurricanes to compare DSM-IV, DSM-5, and ICD-11 diagnostic rates using self-report measures. The authors found slightly higher diagnostic rates using DSM-IV compared to DSM-5, with similar impairment levels across groups. It should be noted, however, that three DSM-5 symptoms were not assessed in one of the two samples included in this study, which may have resulted in an underestimate of diagnosis rates.
Importantly, previous studies have suggested that the alternative criteria for children age 6 years and younger (Scheeringa et al. 2006) may also be appropriate for preadolescent children (Meiser-Stedman et al. 2008; Iselin et al. 2010). Across these studies, using the alternative criteria resulted in a higher diagnosis rate than the DSM-IV criteria for preadolescent children (Scheeringa et al. 2006; Meiser-Stedman et al. 2008; Iselin et al. 2010). For example, Meiser-Stedman et al. (2008) showed that using the alternative criteria resulted in twice as many 7–10-year-old children meeting PTSD criteria 6 months after a trauma compared to DSM-IV. Iselin et al. (2010) compared the DSM-IV diagnostic algorithm to four alternative PTSD diagnostic algorithms in a sample of 6–15-year-old children following a traumatic brain injury (TBI). Of all the algorithms tested, the DSM-IV algorithm diagnosed the fewest children and was not related to psychosocial functioning, whereas the alternate criteria proposed by Scheeringa et al. (2006) was significantly associated with poorer psychosocial functioning, and was recommended by the authors as the best method to use when diagnosing PTSD in pediatric samples following TBI. Although the findings in older adolescents suggest only slightly higher prevalence rates when using DSM-5 over DSM-IV, it is possible that changes in DSM-5 will result in higher prevalence rates for preadolescents. That is, the deletion of the A2 criterion and the addition and expansion of symptoms in clusters D and E may be more consequential in this age group than it has been shown to be in older adolescents.
While examining prevalence rates is important when comparing evolving diagnostic criteria, the diagnostic rates alone are insufficient to determine which criteria set is most appropriate or useful. To evaluate the utility of a criteria set, meaningful external measures, such as impairment and comorbid psychopathology, can be helpful. For example, it is important for a diagnostic category to capture those individuals experiencing significant impairment as a result of their symptoms, and distinguish those individuals from others with low levels of impairment. Furthermore, given the established comorbidity between PTSD and other forms of psychopathology (Kessler et al. 1995; Scheeringa et al. 2003), it would be expected that those meeting new diagnostic criteria for PTSD would continue to exhibit higher levels of comorbid disorders compared to undiagnosed individuals.
In this study, we sought to compare DSM-IV to DSM-5 PTSD criteria in a treatment-seeking sample of older children and adolescents. We predicted that using DSM-5 criteria would result in a higher rate of diagnosis of PTSD than DSM-IV criteria. We also predicted that those diagnosed by DSM-5 only would have equivalent impairment and comorbidity to those diagnosed with DSM-IV, and greater impairment and comorbidity than those who are undiagnosed, suggesting that individuals who are now captured by the new criteria have equivalent pathology and need for treatment. Furthermore, we examined older children (ages 7–12) separately from adolescents (ages 13–18) to assess for potential developmental differences. We predicted that the change to DSM-5 criteria would have a larger impact on diagnostic rates in children compared to adolescents. Finally, the appropriateness of using the age 6 years and younger criteria for 7–12-year-old children was evaluated. We expected that using the very young children criteria would result in a higher rate of diagnosis, and that diagnosed children would exhibit significant impairment and comorbidity.
Methods
Participants
Participants in this study included 135 trauma-exposed 7–18-year olds (n = 76 age 7–12; n = 59 age 13–18) and their primary caregivers who were evaluated to participate in a PTSD treatment study described in detail elsewhere (Scheeringa and Weems 2014). Briefly, participants were referred by clinicians, social service agencies, advocacy centers, schools, or were self-referred. Of the 141 participants evaluated in the laboratory, 6 were excluded or withdrew during the evaluation. Potential participants were excluded if they had a history of serious head trauma, moderate intellectual disability, autism, blindness, deafness, kidney/liver ailments, epilepsy, seizures, bipolar disorder, psychosis, or if they were non-English speaking, severely disabled, acutely suicidal or homicidal, or receiving current counseling outside of the study. Median parent-reported family income was US $20,001–$30,000 (range <$10,000 to >$90,000). Additional participant demographics are provided in Table 1.
Table 1.
Participant Demographics
| Variable | n | % |
|---|---|---|
| Sex: female | 71 | 53% |
| Race: | ||
| Black or African American | 73 | 54% |
| White | 44 | 33% |
| American Indian or Alaskan Native | 3 | 2% |
| Mixed ethnicity | 15 | 11% |
| Ethnicity: Hispanic or Latino | 28 | 21% |
| Mother employed | 77 | 57% |
| Male caregiver employed | 72 | 53% |
| Child lives with biological father | 31 | 23% |
| M | SD | |
| Age | 12.71 | 3.41 |
| Mother age | 42.37 | 10.17 |
| Mother education (years) | 13.79 | 2.66 |
| Father age | 41.68 | 8.97 |
| Male caregiver education (years) | 12.64 | 2.57 |
Procedures
This study was approved by the Tulane University Committee on the use of human subjects. On arrival to the laboratory, written informed consent and assent were obtained from all caregivers and youth included in the study. Although this project involved 12 sessions of treatment, data for this study came solely from intake assessments before the beginning of treatment. Results regarding treatment success are reported elsewhere (Scheeringa and Weems 2014) and are beyond the scope of the current study. Caregivers and youth completed diagnostic interviews and self-report measures during intake.
Measures
Children's Depression Inventory (CDI; Kovacs 1992). The CDI was used to assess depressive symptoms in children and adolescents. Caregivers completed the parent version of the questionnaire, which comprised 17 items rated on a 4-point scale ranging from 0 (not at all) to 3 (much or most of the time). Youth completed the child version, which assesses 27 items scored from 0 to 2. In the present study, the items demonstrated good internal consistency with Cronbach's alpha values of 0.88 and 0.86 for child and parent report, respectively.
Screen for Child Anxiety-Related Emotional Disorders (SCARED; Birmaher et al. 1999). The SCARED is a child self-report and parent-report rating form designed to screen children for anxiety disorders, including symptoms of generalized anxiety, separation anxiety, panic, and social phobia. Both the parent and child forms include 41 items rated on a 0 (not true or hardly ever true) to 2 (very true or often true) scale. In the current study, the internal consistency of the total scale was excellent for parent report (alpha = 0.94) and child report (alpha = 0.94).
Swanson, Nolan, and Pelham Rating Scale (SNAP-IV). The SNAP-IV is a version of the SNAP (Swanson et al. 1983), which was revised to reflect DSM-IV diagnostic criteria. It is a parent-report questionnaire that assesses symptoms of DSM-IV disorders on a 0 (not at all) to 3 (very much) scale. For the current study, the 30 items assessing attention-deficit/hyperactivity disorder and oppositional defiant disorder were combined to create a scale reflecting disruptive behavior (alpha = 0.96).
National Institute of Mental Health Diagnostic Interview Schedule for Children, Version 4.0 (DISC-IV; Schaffer et al. 2000). Symptoms of PTSD were assessed using the DISC-IV, a widely used, structured diagnostic interview used to assess symptoms of DSM-IV disorders. Interviews were conducted with parents and youth separately by trained research assistants.
Because not all DSM-5 symptoms of PTSD are included in the DISC-IV, items from other child- and parent-report measures were used to supplement the DISC-IV interview to capture data on the symptoms added to the diagnostic criteria. While using child- and parent-report measures in lieu of structured interview questions to assess every symptom is a limitation, this strategy allowed for a reasonable estimate of prevalence rates. Furthermore, this method is consistent with previous research (Koffel et al. 2012; Scheeringa et al. 2012; Danzi and La Greca 2016). Specifically, for the parent report of DSM-5 age 6 years and younger criteria, criterion C3 (substantially increased frequency of negative emotional states [fear, guilt, sadness, shame, confusion]) was assessed using two items from the CDI (“My child looks sad” and “My child cries or looks tearful”) and one item from the SCARED (“My child gets really frightened for no reason at all”). Similarly, for child report, two items from the CDI (“I am sad all the time” and “I feel like crying every day”) and one item from the SCARED (“I get really frightened for no reason at all”) were used.
For DSM-5 criteria, the parent-report CDI item “My child does not like himself or herself” was used for criterion D2 (persistent and exaggerated negative beliefs or expectations about oneself, others, or the world). For child report, two CDI items (“I am bad” and “bad things will happen to me”) were used. For criterion D3 (persistent, distorted cognitions about the cause or consequences of the trauma that lead to blame of self or others), one parent-report CDI item (“My child blames himself or herself for things”) and one child-report CDI item (“bad things are my fault”) were used. For criterion D4 (persistent negative emotional state [fear, horror, anger, guilt, shame]), one item from the SNAP (“My child is often angry and resentful”) and one item from the SCARED (“My child gets really frightened for no reason at all”) were used for parent report, and one item from the SCARED (“I get really frightened for no reason at all”) was used for child report.
In addition, one item from the CDI child version (“I think about killing myself”) was used to assess criterion E2 (reckless or self-destructive behavior). The CDI parent version did not contain a comparable item. Because “I think about killing myself” is a thought and the new symptom is worded as a behavior, and there exists little empirical guidance on how reckless or self-destructive behavior ought to be operationalized at this point, we calculated the prevalence of criterion E with and without the CDI item assessing suicidal ideation. The prevalence of criterion E in the full sample decreased from 79.9% to 77.0% when the CDI item was omitted, suggesting that the endorsement of suicidal ideation had little influence on whether an individual met the threshold for criterion E. Furthermore, when this item was omitted, it resulted in no change in prevalence of PTSD diagnosis.
For the CDI and SCARED child report and SCARED parent report, an item was considered endorsed if it was scored 1 or 2; for parent-reported CDI and SNAP, an item was considered endorsed if it was scored 2 or 3. A combined diagnosis was determined using a “best estimate” approach, consistent with recommendations from previous research (Scheeringa et al. 2006; Meiser-Stedman et al. 2008). That is, a symptom was considered endorsed if either the parent or child endorsed it.
Items pulled from child- and parent-report measures did not assess whether the symptoms were specific to the trauma and only present since the trauma. If the CDI or SCARED items existed before traumatic experiences and were not truly PTSD symptoms, this potentially could have led to higher than true endorsement rates for PTSD. However, the average endorsement rate of CDI and SCARED items (32% for both parent and child report) was similar to the average endorsement rate for DISC-IV items (35% and 30% for parent and child report, respectively).
Impairment was also assessed using the DISC-IV. Six items assessed domains of impairment, including caretaker relationships, ability to function outside of the home, peer relationships, difficulty at school, teacher relationships, and emotional distress. Severity of impairment in each domain was also rated on a continuous scale. These data were used to create two variables, one reflecting the number of domains impaired and the second reflecting the severity of overall impairment.
Data analysis
Rates of diagnosis for DSM-IV and DSM-5 criteria were compared using McNemar's test and agreement between diagnoses was calculated using the kappa statistic. Participants were coded as (0) undiagnosed, (1) diagnosed by DSM-5 but not diagnosed by DSM-IV criteria (“DSM-5 only”), or (2) diagnosed by DSM-IV. It should be noted that the latter group included individuals diagnosed by DSM-IV and DSM-5 as well as individuals diagnosed by DSM-IV only; distinguishing between these groups was not central to the hypotheses, and the subgroup of individuals diagnosed with DSM-IV only was too small to be meaningfully compared to other groups. Independent samples t-tests were used to compare groups in terms of impairment (domains of impairment and impairment severity) and comorbidity (scores on the CDI, SCARED, and SNAP). In addition, because no differences were hypothesized between those diagnosed by DSM-5 only and those diagnosed with DSM-IV, 80% confidence intervals (CIs) for group mean differences were also examined. If the 80% CIs include 0, this strengthens conclusions about equivalency between groups. The same strategy was also used to evaluate the appropriateness of using the very young children criteria with children ages 7–12. For child-reported depression, the Mann–Whitney U test was used rather than t-tests due to mild skew. For each variable assessed, data were missing for three or fewer individuals. One adolescent was missing data for criterion A2, and thus DSM-IV diagnosis. Given the small proportion of missing data, values were not imputed. To correct for multiple comparisons, Bonferroni corrections were used when significant differences between groups were predicted. All analyses were conducted using IBM SPSS 22.0.
Results
DSM-IV compared to DSM-5
Endorsement rates for DSM-IV and DSM-5 criteria are presented in Table 2. It was expected that using DSM-5 criteria would result in a higher diagnosis rate than DSM-IV criteria, especially among 7–12-year-old children. For the full sample, a higher proportion of participants met criteria for DSM-5 diagnosis (61.5%) than DSM-IV diagnosis (53.0%) and this difference was significant (p = 0.013). This same pattern was observed when examining only 7–12-year-old children (52.6% vs. 36.8%; p = 0.002). However, among adolescents, the proportions diagnosed with DSM-5 and DSM-IV did not differ (72.9% vs. 74.1%; p = 1.000). The kappa statistic was used to examine agreement between diagnostic criteria sets. For the overall sample, agreement was good (kappa = 0.74); however, agreement was lower among older children (kappa = 0.64) compared to adolescents (kappa = 0.87).
Table 2.
Endorsement Rates for DSM-IV and DSM-5 Posttraumatic Stress Disorder Criteria
| Criteria | Full sample, % | Children, % | Adolescents, % |
|---|---|---|---|
| DSM-IV: meets diagnosis | 53.0 | 36.8 | 74.1 |
| A. Exposure to trauma (2 of 2) | 98.5 | 97.4 | 100.0 |
| B. Re-experiencing/intrusion (1 of 5) | 85.9 | 86.8 | 84.7 |
| C. Persistent avoidance/numbing (3 of 7) | 56.3 | 39.5 | 78.0 |
| D. Increased arousal/reactivity (2 of 5) | 77.0 | 73.7 | 81.4 |
| F. Distress or impairment | 91.9 | 88.2 | 96.6 |
| DSM-5: meets diagnosis | 61.5 | 52.6 | 72.9 |
| A. Exposure to trauma (1 of 4) | 100.0 | 100.0 | 100.0 |
| B. Re-experiencing/intrusion (1 of 5) | 85.9 | 86.8 | 84.7 |
| C. Persistent avoidance (1 of 2) | 82.2 | 80.3 | 84.7 |
| D. Negative cognitions/mood (2 of 7) | 76.1 | 69.3 | 84.7 |
| E. Increased arousal/reactivity (2 of 6) | 79.9 | 77.3 | 83.1 |
| G. Distress or impairment | 91.9 | 88.2 | 96.6 |
| DSM-5 (very young children): meets diagnosis | 73.3 | 69.7 | 78.0 |
| A. Exposure to trauma (1 of 3) | 100.0 | 100.0 | 100.0 |
| B. Re-experiencing/intrusion (1 of 5) | 85.9 | 86.8 | 84.7 |
| C. Avoidance/negative cognition/mood (1 of 6) | 94.0 | 94.7 | 93.2 |
| D. Increased arousal/reactivity (2 of 5) | 77.0 | 73.7 | 81.4 |
| F. Distress or impairment | 91.9 | 88.2 | 96.6 |
DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, fifth edition.
Results showed that 17.1% of participants (n = 14) did not meet criteria for DSM-IV PTSD, but did meet criteria for DSM-5 PTSD. In other words, 17.1% of participants would have been undiagnosed using DSM-IV criteria. Of these participants, only one was an adolescent and 13 were children. It was hypothesized that these youth diagnosed with DSM-5 only would exhibit similar levels of impairment to those who were diagnosed with DSM-IV. Results from independent samples t-tests showed that DSM-5-only subjects did not differ from those diagnosed with DSM-IV criteria in terms of domains of impairment or severity of impairment. Furthermore, 80% CIs for group mean differences included 0, providing evidence of equivalence between groups (Table 3). It was also hypothesized that DSM-5-only youth would exhibit similar levels of comorbidity to those who were diagnosed with DSM-IV. DSM-5-only participants did not significantly differ from those diagnosed with DSM-IV criteria in terms of depression (CDI parent and child report), anxiety (SCARED parent and child report), or disruptive behaviors (SNAP parent report). Furthermore, 80% CIs for group differences included 0 for all variables except child-reported depression.
Table 3.
Children and Adolescents Diagnosed with DSM-5 Criteria Only Compared to Those Diagnosed with DSM-IV and to Those Undiagnosed
| DSM-IV | Undiagnosed | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| DSM-5 only M (SD) | M (SD) | t (df) | p | 80% CI | M (SD) | t (df) | p | d | |
| Impairment | |||||||||
| Domains | 4.43 (1.16) | 4.62 (1.13) | −0.578 (83) | 0.565 | [−0.62, 0.24] | 2.27 (1.88) | 5.280 (34.625) | >0.001 | 1.24 |
| Severity | 11.00 (3.31) | 11.20 (3.64) | −0.188 (83) | 0.851 | [−1.55, 1.16] | 5.10 (4.90) | 4.225 (61) | >0.001 | 1.28 |
| Comorbidity | |||||||||
| CDI-parent | 21.57 (8.00) | 24.51 (9.46) | −1.086 (83) | 0.281 | [−6.43, 0.56] | 16.75 (7.77) | 2.029 (60) | 0.047 | 0.62 |
| CDI-childa | 6.50b | 10.00b | −1.54 (367.00)c | 0.123 | [−5.00, −1.00] | 5.00b | −1.71 (235.00)c | 0.088 | 0.22d |
| SCARED-parent | 33.92 (13.97) | 28.68 (16.91) | 1.053 (82) | 0.295 | [−1.19, 11.68] | 18.94 (11.53) | 3.960 (58) | >0.001 | 1.24 |
| SCARED-child | 37.64 (19.35) | 36.94 (15.48) | 0.148 (83) | 0.883 | [−5.40, 6.80] | 23.47 (15.39) | 2.848 (59) | 0.006 | 0.87 |
| SNAP-parent | 44.57 (26.23) | 37.48 (22.97) | 1.029 (81) | 0.307 | [−1.82, 16.00] | 29.69 (20.41) | 2.223 (57) | 0.030 | 0.68 |
The DSM-IV columns (including 80% CI) display results of the comparison between those diagnosed with DSM-5 only and those diagnosed with DSM-IV. The Undiagnosed columns (including d) display results of the comparison between those diagnosed with DSM-5 only and those who were undiagnosed. Bold p-values indicate significance after Bonferroni correction. Bold CIs contain 0.
Mann–Whitney U test.
Median.
z-Value and (Mann–Whitney U statistic).
Effect size r.
CI, confidence interval; CDI, Children's Depression Inventory; d, Cohen's d; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, fifth edition; SCARED, Screen for Child Anxiety-Related Emotional Disorders; SNAP, Swanson, Nolan, and Pelham Rating Scale.
It was also hypothesized that DSM-5-only youth would exhibit greater impairment and comorbidity than those who were undiagnosed. Table 3 shows results from independent samples t-tests using a Bonferroni corrected alpha level (7 comparisons; p < 0.007). DSM-5-only participants endorsed significantly higher domains of impairment, severity of impairment, and anxiety (SCARED parent and child report) compared to those who were undiagnosed. DSM-5-only participants also endorsed higher depression (CDI parent and child report) and disruptive behaviors (SNAP parent report) than those who were undiagnosed, but these differences did not reach significance after Bonferroni correction.
Only three participants (one child and two adolescents) were diagnosed with DSM-IV, but undiagnosed by DSM-5 criteria. The one child did not meet criteria for cluster D; the two adolescents did not meet criteria for cluster C.
Diagnostic criteria for children age 6 years and younger
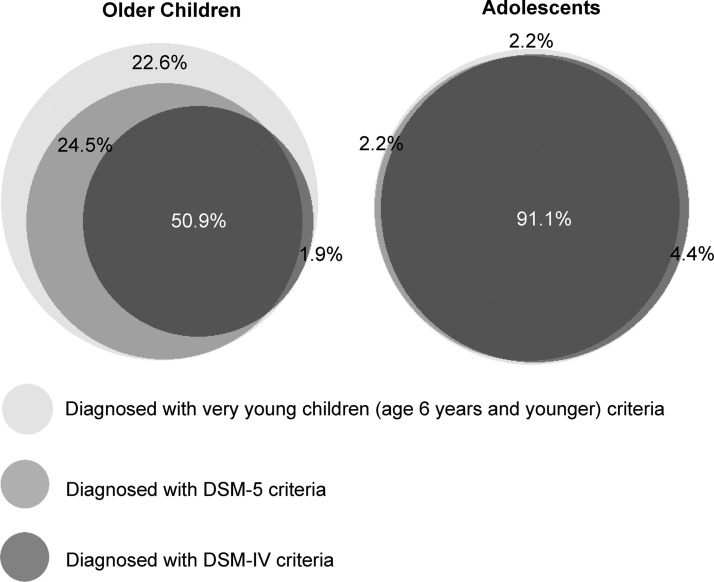
The endorsement rates using the PTSD criteria for children age 6 years and younger are presented in Table 2. Among 7–12-year-old children, a significantly higher proportion of participants met criteria for age 6 years and younger diagnosis (69.7%) compared to DSM-IV criteria (36.8%, p < 0.001) and DSM-5 criteria (52.6%; p < 0.001). However, among 13–18-year-old adolescents, the proportions diagnosed with age 6 years and younger criteria (78.8%) did not differ significantly from the proportion diagnosed with DSM-IV (74.1%; p = 0.500) or with DSM-5 (72.9%, p = 0.250). Among 7–12-year-old children, the age 6 years and younger criteria captured 25 participants (32.9%) who were undiagnosed with DSM-IV criteria and 13 participants (17.1%) who were undiagnosed with DSM-5 criteria (Fig. 1).
FIG. 1.
Overlap among posttraumatic stress disorder criteria sets. The left diagram represents all 7–12-year-old children and the right diagram represents all 13–18-year-old adolescents who were diagnosed using one or more criteria sets (n = 53 and n = 45, respectively). For 7–12-year-old children, 50.9% met criteria for PTSD by all three diagnostic algorithms, 1.9% met criteria by DSM-IV and very young children criteria but not DSM-5, 24.5% met criteria by DSM-5 and very young children criteria but not DSM-IV, and 22.6% met criteria only by very young children criteria. In contrast, for 13–18-year-old adolescents, 91.1% met criteria for PTSD by all three diagnostic algorithms. Venn diagrams were created using BioVenn (Hulsen et al. 2008). DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, fifth edition; PTSD, posttraumatic stress disorder.
Impairment and comorbidity variables for 7–12-year-old children who were diagnosed with age 6 years and younger criteria, but undiagnosed by DSM-IV (“very young children only”), were compared to those who met DSM-IV criteria (Table 4). Contrary to predictions, results from independent samples t-tests showed that very young children-only subjects endorsed significantly lower domains of impairment, severity of impairment, and depression (CDI parent and child report) compared to those diagnosed with DSM-IV criteria. Furthermore, 80% CIs for each of these variables, as well as parent-reported anxiety, did not include 0. However, 80% CIs did include 0 for child-reported anxiety (SCARED) and parent-reported disruptive behaviors (SNAP), suggesting equivalence between groups for these variables.
Table 4.
Seven- to Twelve-Year-Old Children Diagnosed Only with Very Young Children Criteria Compared to Those Diagnosed by DSM-IV and to Those Undiagnosed
| DSM-IV | Undiagnosed | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Very young children only M (SD) | M (SD) | t (df) | p | 80% CI | M (SD) | t (df) | p | d | |
| Impairment | |||||||||
| Domains | 3.48 (1.69) | 4.57 (1.17) | −2.763 (51) | 0.008 | [−1.60, −0.58] | 1.87 (2.16) | 2.892 (46) | 0.006 | 0.84 |
| Severity | 8.08 (4.87) | 11.04 (3.51) | −2.507 (43.169) | 0.016 | [−4.49, −1.42] | 4.17 (5.28) | 2.666 (46) | 0.011 | 0.77 |
| Comorbidity | |||||||||
| CDI-parent | 18.92 (7.62) | 25.79 (8.03) | −3.185 (51) | 0.002 | [−9.67, −4.07] | 15.68 (8.40) | 1.386 (45) | 0.173 | 0.41 |
| CDI-childa | 5.00b | 7.50b | −2.00 (238.00)c | 0.045 | [−5.00, −1.00] | 4.50b | −0.87 (234.50)c | 0.385 | 0.13d |
| SCARED-parent | 25.48 (14.01) | 32.61 (16.82) | −1.621 (49) | 0.111 | [−12.84, −1.42] | 20.00 (12.29) | 1.392 (43) | 0.171 | 0.42 |
| SCARED-child | 32.24 (18.18) | 35.50 (14.90) | −0.717 (51) | 0.477 | [−9.16, 2.64] | 26.95 (17.20) | 1.007 (44) | 0.320 | 0.30 |
| SNAP-parent | 39.57 (25.81) | 47.32 (19.02) | −1.198 (39.592) | 0.238 | [−16.19, 0.68] | 30.81 (22.87) | 1.186 (42) | 0.242 | 0.36 |
The DSM-IV columns (including 80% CI) display results of the comparison between those diagnosed only with very young children criteria and those diagnosed with DSM-IV. The Undiagnosed columns (including d) display results of the comparison between those diagnosed only with very young children criteria and those who were undiagnosed. Bold p-values indicate significance after Bonferroni correction. Bold CIs contain 0.
Mann–Whitney U test.
Median.
z-Value and (Mann–Whitney U statistic).
Effect size r.
CI, confidence interval; CDI, Children's Depression Inventory; d, Cohen's d; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition; SCARED, Screen for Child Anxiety-Related Emotional Disorders; SNAP, Swanson, Nolan, and Pelham Rating Scale.
Table 4 also shows results from independent samples t-tests comparing 7–12-year-old children who were diagnosed with only the very young children criteria to those who were undiagnosed, using a Bonferroni corrected alpha level (7 comparisons; p < 0.007). Very young children-only participants endorsed significantly higher domains of impairment compared to those who were undiagnosed. Finally, very young children-only participants also endorsed higher severity of impairment, depression (CDI parent and child report), anxiety (SCARED parent and child report), and disruptive behaviors (SNAP parent report) than those who were undiagnosed, but these differences did not reach significance.
Discussion
The goal of the current article was to evaluate the recently revised DSM-5 PTSD criteria in a trauma-exposed, treatment-seeking sample of older children and adolescents for the first time. Consistent with predictions and consistent with research on older adolescents and adults (Carmassi et al. 2013; Hafstad et al. 2014), the 13–18-year-old adolescents in this sample had a similar prevalence rate whether using DSM-IV or DSM-5 criteria. Only one adolescent met criteria for DSM-5 PTSD that would not have met criteria under DSM-IV. Because a significantly higher proportion of 7–12-year-old youths met criteria for DSM-5 relative to DSM-IV, the switch to DSM-5 criteria will likely lead to significantly higher prevalence rates of PTSD for 7–12-year-old children, but not for adolescents.
In this sample, revisions to the avoidance/numbing criteria appear to have the greatest effect on prevalence rates. While only 39.5% of children met DSM-IV criterion C, this rate increased to 80.3% for DSM-5 criterion C and 69.3% for criterion D. The removal of criterion A2 had little impact on prevalence.
Given that the change in PTSD criteria impacted those who met the criteria, it was important to investigate the level of pathology endorsed by individuals who did not meet DSM-IV criteria but did meet DSM-5 criteria. As predicted, results showed that individuals diagnosed by DSM-5 only reported similar levels of impairment and comorbidity compared to those diagnosed by DSM-IV, and greater impairment and comorbidity than those who were undiagnosed (although not all differences reached significance). This suggests that individuals who were undiagnosed using DSM-IV criteria and now meet DSM-5 criteria will likely have similar levels of pathology and need for treatment, and provides preliminary evidence to support the changes to PTSD criteria in DSM-5.
Based on previous work suggesting that the alternative criteria for very young children may also be appropriate for preadolescent children (Scheeringa et al. 2006; Meiser-Stedman et al. 2008; Iselin et al. 2010), the impact of using these criteria for 7–12-year-old children was evaluated. Using the criteria for very young children resulted in a significantly higher number of 7–12-year olds meeting criteria compared to DSM-IV or DSM-5 criteria. In contrast, adolescents aged 13–18 had a similar prevalence rate regardless of the diagnostic system used, suggesting that the adult criteria are sufficient for the 13–18-year age group.
Comparing the 7–12-year-old individuals who were undiagnosed by DSM-IV but diagnosed using the very young children criteria to those who met DSM-IV criteria revealed that those diagnosed only with the very young children criteria had lower levels of impairment and comorbidity (some that reached significance). Furthermore, those only diagnosed with the very young children criteria did not differ from those who were undiagnosed in terms of comorbidity. These results may be interpreted to suggest that the very young children criteria are too lenient for children ages 7–12, and would result in diagnosing children who have levels of impairment and psychopathology that are too low. However, results also showed that those only diagnosed with the very young children criteria reported significantly higher domains of impairment than children who were undiagnosed in this sample. It is important to note that even the undiagnosed participants were trauma-exposed, treatment-seeking individuals, most of whom endorsed some PTSD symptoms, impairment, and comorbid problems. Thus, before concluding that the very young children criteria are too lenient for 7–12-year-old children, it may be beneficial to further examine these criteria in a sample with a broader range of severity.
On a similar note, although those diagnosed with the very young child criteria only had lower impairment and comorbidity than those who met DSM-IV criteria, it does not necessarily follow that these children are not deserving of a diagnosis and in need of treatment. Previous research shows that PTSD is underdiagnosed in children (Miele and O'Brien 2010), and even those who meet subthreshold DSM-IV criteria demonstrate substantial functional impairment and distress (Carrion et al. 2002). In the current study, despite endorsing significantly fewer domains of impairment than those diagnosed with DSM-IV, older children who were diagnosed with the very young children criteria only reported impairment in an average of 3.48 domains. Thus, the results from this study suggest that using the very young children criteria for 7–12-year-old children will likely capture children with less severe psychopathology than DSM-IV criteria, which may be an appropriate and desired consequence. While a treatment-seeking sample may be the most relevant for examining diagnostic criteria, it is important to note that the results of this study may not generalize to the population of trauma-exposed, nontreatment-seeking children, and the diagnostic algorithms may show a different pattern of endorsement in such samples. Thus, additional research, particularly in nontreatment-seeking populations, is needed to determine whether the age 6 years and younger criteria should be extended to include children through the age of 12, or whether more stringent symptom thresholds (but less stringent than adult criteria) are more appropriate for 7–12-year-old children.
An important limitation to note in this study was the assessment of DSM-5 PTSD symptoms. While DSM-IV PTSD symptoms were assessed using a “gold-standard” structured clinical interview, the symptoms added to the DSM-5 criteria were obtained using items from child- and parent-reported measures, and did not map perfectly onto the criteria. For example, criterion E2 (reckless or self-destructive behavior) included child report of suicidal ideation, but not other behaviors that contribute to that symptom such as dangerous driving, risky sexual behavior, excessive alcohol or drug use, or self-injurious behavior. However, this omission likely did not have a substantial impact on the results of the current study, as several previous studies have reported low endorsement rates for this symptom (Miller et al. 2012; Hafstad et al. 2014). Also, items pulled from child- and parent-report measures did not assess whether the symptoms were specific to the trauma and only present since the trauma, which may have led to higher than true endorsement rates for those symptoms. Although a limitation, the use of these questionnaires to supplement diagnostic data allowed for this initial examination of the diagnostic changes. Future work in this area should aim to use structured diagnostic interviews to assess all symptoms.
Conclusions
This study evaluated DSM-5 PTSD diagnostic criteria in a trauma-exposed, treatment-seeking sample of older children and adolescents. Results supported the new DSM-5 criteria over DSM-IV and showed that DSM-5 may lead to higher PTSD prevalence rates in 7–12-year-old children, but not adolescents. In addition, the current study explored the appropriateness of using the DSM-5 PTSD criteria for very young children with 7–12-year-old children. Results suggest that although children captured with these criteria may have less severe psychopathology than those diagnosed with DSM-IV criteria, they exhibit substantial impairment and comorbid symptoms. Additional research is needed to determine the most appropriate symptom thresholds for this age group.
Clinical Significance
If the finding that using DSM-5 PTSD criteria results in more 7–12-year-old children meeting diagnosis than using DSM-IV criteria is replicated, this will have clear implications for treatment and research. Children who previously did not meet criteria for PTSD diagnosis will now qualify for a diagnosis. Providing appropriate recommendations for empirically supported psychotherapeutic and psychopharmacological treatment relies on accurate diagnosis. Thus, the recent change in PTSD conceptualization will ideally lead to an increase in the number of children receiving appropriate care.
Disclosures
No competing financial interests exist.
References
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed., Text Revision. Washington (DC), American Psychiatric Association, 2000 [Google Scholar]
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Arlington (Virginia), American Psychiatric Publishing, 2013 [Google Scholar]
- Anthony JL, Lonigan CJ, Hecht SA: Dimensionality of posttraumatic stress disorder symptoms in children exposed to disaster: Results from confirmatory factor analysis. J Abnorm Psychol 108:326–336, 1999 [DOI] [PubMed] [Google Scholar]
- Asmundson GJG, Frombach I, McQuaid J, Pedrelli P, Lenos R, Stein MB: Dimensionality of posttraumatic stress symptoms: A confirmatory factor analysis of DSM-IV symptom clusters and other symptom models. Behav Res Ther 38:203–214, 2000 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiapetta L, Bridge J, Monga S, Baugher M: Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. J Am Acad Child Adolesc Psychiatry 38:1230–1236, 1999 [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP: The importance of the peritraumatic experience in defining traumatic stress. Psych Bull 137:47–67, 2011 [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Rose R: Fear, helplessness, and horror in posttraumatic stress disorder: Investigating DSM-IV criterion A2 in victims of violent crime. J Trauma Stress 13:499–509, 2000 [DOI] [PubMed] [Google Scholar]
- Carmassi C, Akiskal HS, Yong SS, Stratta P, Calderani E, Massimetti E, Akiskal KK, Rossi A, Dell'Osso L: Post-traumatic stress disorder in DSM-5: Estimates of prevalence and criteria comparison versus DSM-IV-TR in a non-clinical sample of earthquake survivors. J Affect Disord 151:843–848, 2013 [DOI] [PubMed] [Google Scholar]
- Carrion VG, Weems CF, Ray R, Reiss AL: Toward and empirical definition of pediatric PTSD: The phenomenology of PTSD symptoms in youth. J Am Acad Child Adolesc Psychiatry 41:166–173, 2002 [DOI] [PubMed] [Google Scholar]
- Cavanaugh CE: The influence of posttraumatic stress on unprotected sex among sexually active adolescent girls and boys involved in the child welfare system of the United States. J Adolesc 36:835–837, 2013 [DOI] [PubMed] [Google Scholar]
- Cavanaugh CE, Hansen NB, Sullivan TP: HIV sexual risk behavior among low-income women experiencing intimate partner violence: The role of posttraumatic stress disorder. AIDS Behav 14:318–327, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danzi BA, La Greca AM: DSM-IV, DSM-5, and IDC-11: Identifying children with posttraumatic stress disorder after disasters. J Child Psychol Psychiatry 2016:1444–1452, 2016 [DOI] [PubMed] [Google Scholar]
- De Young AC, Kenardy JA, Cobham VE: Diagnosis of posttraumatic stress disorder in preschool children. J Clin Child Adolesc Psychol 40:375–384, 2011 [DOI] [PubMed] [Google Scholar]
- Elhai JD, Miller ME, Ford JD, Biehn TL, Palmieri PA, Frueh BC: Posttraumatic stress disorder in DSM-5: Estimates of prevalence and symptom structure in a nonclinical sample of college students. J Anxiety Disord 26:58–64, 2012 [DOI] [PubMed] [Google Scholar]
- Friedman MJ: Finalizing PTSD in DSM-5: Getting here from there and where to go next. J Trauma Stress 26:548–559, 2013 [DOI] [PubMed] [Google Scholar]
- Friedman MJ, Resick PA, Bryant RA, Brewin CR: Considering PTSD for DSM-5. Depress Anxiety 28:750–769, 2011 [DOI] [PubMed] [Google Scholar]
- Hafstad GS, Dyb G, Jensen TK, Steinberg AM, Pynoos RS: PTSD prevalence and symptom structure of DSM-5 criteria in adolescents and young adults surviving the 2011 shooting in Norway. J Affect Disord 169:40–46, 2014 [DOI] [PubMed] [Google Scholar]
- Hulsen T, de Vlieg J, Alkema W: BioVenn—A web application for the comparison and visualization of biological lists using area-proportional Venn diagrams. BMC Genomics 9:488, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iselin G, LeBrocque R, Kenardy J, Anderson V, McKinlay L: Which method of posttraumatic stress disorder classification best predicts psychosocial function in children with traumatic brain injury? J Anxiety Disord 24:774–779, 2010 [DOI] [PubMed] [Google Scholar]
- Karam EG, Andrews G, Bromet E, Petukhova M, Ruscio AM, Salamoun M, Sampson N, Stein DJ, Alonso J, Andrade LH, Angermeyer M, Demyttenaere K, de Girolamo G, de Graaf R, Florescu S, Gureje O, Kaminer D, Kotov R, Lee S, Lepine J-P, Medina-Mora ME, Oakley Brown MA, Posada-Villa J, Sagar R, Shalev AY, Takeshima T, Tomov T, Kessler RC: The role of criterion A2 in the DSM-IV diagnosis of posttraumatic stress disorder. Biol Psychiatry 68:465–473, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 52:1048–1060, 1995 [DOI] [PubMed] [Google Scholar]
- Kilpatrick D, Resnik H, Freedy J, Pelcovitz D, Resick P, Roth S, van der Kolk B: Posttraumatic stress disorder field trial: Evaluation of the PTSD construct–Criteria A through E. In: DSM-IV Sourcebook. Edited by Widiger T, Frances A, Pincus H, Ross R, First M, Davis W, Kline M. DSM-IV Sourcebook. Washington, DC, American Psychiatric Association, 1998, pp. 803–844 [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW: Confirmatory factor analysis of the clinician-administered PTSD scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychol Assess 10:90–96, 1998 [Google Scholar]
- Koffel E, Polusny MA, Arbisi PA, Erbes CR: A preliminary investigation of the new and revised symptoms of posttraumatic stress disorder in DSM-5. Depress Anxiety 29:731–738, 2012 [DOI] [PubMed] [Google Scholar]
- Kovacs M: Children's Depression Inventory. North Tonawanda (New York), Multi-Health System, 1992 [Google Scholar]
- McWilliams LA, Cox BJ, Asmundson GJG: Symptom structure of posttraumatic stress disorder in a nationally representative sample. J Anxiety Disord 19:626–641, 2005 [DOI] [PubMed] [Google Scholar]
- Meiser-Stedman R, Smith P, Glucksman E, Yule W, Dalgleish T: The posttraumatic stress disorder diagnosis in preschool- and elementary school-age children exposed to motor vehicle accidents. Am J Psychiatry 165:1326–1337, 2008 [DOI] [PubMed] [Google Scholar]
- Miele D, O'Brien EJ: Underdiagnosis of posttraumatic stress disorder in at risk youth. J Trauma Stress 23:591–598, 2010 [DOI] [PubMed] [Google Scholar]
- Miller MW, Koloupek DG, Dillon AL, Keane TM: Externalizing and internalizing subtypes of combat-related PTSD: A replication and extension using the PSY-5 scales. J Abnorm Psychol 113:636–645, 2004 [DOI] [PubMed] [Google Scholar]
- Miller MW, Wolf EJ, Kilpatrick D, Resnick H, Marx BP, Holowka DW, Keane TM, Rosen RC, Friedman MJ: The prevalence and latent structure of proposed DSM-5 posttraumatic stress disorder symptoms in U.S. national and veteran samples. Psychol Trauma 5:501–512, 2012 [Google Scholar]
- Perrin S, Smith P, Yule W: Practitioner review: The assessment and treatment of post-traumatic stress disorder in children and adolescents. J Child Psychol Psychiatry 41:277–289, 2000 [PubMed] [Google Scholar]
- Pynoos RS, Steinberg AM, Layne CM, Briggs EC, Ostrowski SA, Fairbank JA: DSM-V PTSD diagnostic criteria for children and adolescents: A developmental perspective and recommendations. J Trauma Stress 22:391–398, 2009 [DOI] [PubMed] [Google Scholar]
- Salmon K, Bryant RA: Posttraumatic stress disorder in children: The influence of developmental factors. Clin Psychol Rev 22:163–188, 2002 [DOI] [PubMed] [Google Scholar]
- Saul AL, Grant KE, Carter JS: Post-traumatic reactions in adolescents: How well do the DSM-IV PTSD criteria fit in the real life experience of trauma exposed youth? J Abnorm Child Psychol 36:915–925, 2008 [DOI] [PubMed] [Google Scholar]
- Schaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME: NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry 39:28–38, 2000 [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Myers L, Putnum FW, Zeanah CH: Diagnosing PTSD in early childhood: An empirical assessment of four approaches. J Trauma Stress 25:359–367, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Weems CF: Randomized placebo-controlled D-Cycloserine with cognitive behavior therapy for pediatric posttraumatic stress. J Child Adolesc Psychopharmacol 24:69–77, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Wright MJ, Hunt JP, Zeanah CH: Factors affecting the diagnosis and prediction of PTSD symptomatology in children and adolescents. Am J Psychiatry 163:644–651, 2006 [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Cohen JA: PTSD in children and adolescents: Toward an empirically based algorithm. Depress Anxiety 28:770–782, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Drell MJ, Larrieu JA: Two approaches to the diagnosis of posttraumatic stress disorder in infancy and early childhood. J Am Acad Child Adolesc Psychiatry 34:191–200, 1995 [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Myers L, Putnam FW: New findings on alternative criteria for PTSD in preschool children. J Am Acad Child Adolesc Psychiatry 42:561–570, 2003 [DOI] [PubMed] [Google Scholar]
- Swanson JM, Sandman CA, Deutsch C, Baren M: Methylphenidate Hydrochloride given with or before breakfast: I. behavioral, cognitive, and electrophysiologic effects. Pediatrics 72:49–55, 1983 [PubMed] [Google Scholar]
- Yule W, Ten Bruggencate S, Joseph S: Principal components analysis of the impact of events scale in adolescents who survived a shipping disaster. Pers Indiv Differ 16:685–691, 1994 [Google Scholar]