Abstract
Objective: LithoVue™ is a novel, single-use, digital flexible ureteroscope that was released to the US market in January 2016. There are scant data regarding its performance in humans. Procedural outcomes comparing LithoVue with reusable ureteroscopes are presented in patients undergoing ureteroscopy for upper urinary tract pathology.
Patients and Methods: Clinical outcomes between two groups of patients undergoing flexible ureteroscopy for upper urinary tract pathology were analyzed. The first group underwent surgery utilizing LithoVue, and the second group used reusable fiber-optic flexible ureteroscopes. Differences in procedural outcomes, operative times, and time spent in hospital were analyzed using two-tailed t-tests and chi-squared and Fisher's exact tests.
Results: One hundred fifteen cases utilizing LithoVue and 65 cases utilizing reusable ureteroscopes were included in this study. Demographics, surgical indications, stone size, location, total stone burden, composition, procedural outcomes, and complications were comparable between groups. For all cases, LithoVue procedures lasted 54.1 ± 25.7 minutes compared with 64.5 ± 37.0 minutes for reusable scope procedures (p < 0.05) and for stone removal cases, 57.3 ± 25.1 vs 70.3 ± 36.9 minutes, respectively (p < 0.05). Scope failure occurred in 4.4% of LithoVue cases and 7.7% of reusable cases (p = 0.27).
Conclusions: LithoVue represents a feasible alternative to reusable ureteroscopes with a low rate of scope failure comparable with reusable ureteroscopes. Its use shortens procedure duration, a finding that warrants further investigation.
Keywords: : equipment design, kidney calculi, ureteroscopes, urolithiasis
Introduction
The development of reusable flexible ureteroscopes is a novel innovation to diagnose or treat upper urinary tract pathology. Ureteroscopy is a safe effective modality to access the upper urinary tract.1,2 The designs of traditional reusable ureteroscopes, however, result in progressive deterioration of scope performance. Sterilization requires dedicated equipment, staff, and time. Decontamination has failed in the past and confers a risk of transmitting infection.3,4
LithoVue™ (Boston Scientific, Marlborough, MA), a single-use, digital, disposable flexible ureteroscope, was introduced to the European market in October 20155 and launched in the United States in January 2016. Its use may mitigate the costs and burdens associated with the use of reusable flexible ureteroscopes. Preliminary work evaluating LithoVue has involved cadaveric,6 in vitro,7 in vivo,8 and ex vivo porcine model studies,9 as well as case reports10 and one clinical feasibility study.11 These studies revealed that LithoVue is comparable with existing conventional, reusable flexible ureteroscopes in terms of visual image quality, intraoperative maneuverability, and user satisfaction. Evaluation in the operative setting has been limited due to the novelty instrument.
The University of California, San Francisco (UCSF), is a high-volume tertiary care referral center for urinary stone disease. Institutional approval was obtained to trial LithoVue as a primary instrument for all ureteroscopic cases performed at UCSF. A prospective case–control series was undertaken to compare LithoVue with reusable flexible fiber-optic ureteroscopes in the diagnosis and treatment of nephrolithiasis and other upper tract pathology.
Patients and Methods
A prospective case–control study utilizing data from ureteroscopic cases was performed by two urologists (M.L.S. and T.C.) at a single facility, the UCSF Medical Center Parnassus campus. Data collection and study design were approved by the local Committee on Human Research (CHR 14-14533). All case data collected were derived from our ongoing prospectively maintained Registry for Stones of the Kidney and Ureter (ReSKU™)12 with a written consent obtained from all patients. All ureteroscopes used for this study were purchased by the institution for clinical care, and there was no funding or support provided by industry sponsors. Study cases included consecutive flexible ureteroscopic procedures in which LithoVue was utilized between March 2016 and September 2016. Study controls included consecutive cases in which reusable fiber-optic flexible ureteroscopes (URF-P6; Olympus, Tokyo, Japan) were utilized between August 2014 and April 2015. These control cases were obtained from a previously completed prospective study on reusable scope durability. Data endpoints for LithoVue study cases were collected in an identical manner to the previous study. Between 2014 and 2016, no significant changes in attending surgeon, operating room personnel, laser consoles, disposables, or surgical technique were instituted. We only included cases in which flexible ureteroscopes were used for treatment of urinary stones, work-up of hematuria or unexplained hydronephrosis, and for surveillance and treatment of urothelial carcinoma in the upper urinary tract. Planned staged procedures, ureteroscopic endoureterotomy or endopyelotomy, ureteroscopy performed concurrently with other procedures, and antegrade ureteroscopy cases were excluded.
The number, location, and total stone burden in addition to the degree of hydronephrosis were measured using computed tomography or renal ultrasonography for all stone procedures. Total stone burden was defined as the largest aggregate linear dimension from axial and coronal views.
In compiling outcome data, incidents of scope failure were defined by the operative surgeon determining scope condition being unsuitable to complete the procedure and requiring immediate scope substitution. For stone cases, residual stone status was defined based on renal ultrasound and plain film at 3 months after surgery. Residual stone status was categorized as stone free (no fragments present), insignificant residual fragment (residual fragments smaller than 2 mm), and significant residual fragment (residual fragments larger than 2 mm).13 Primary stone composition was obtained on dry stone fragments when available. Perioperative complications occurring within 30 days postoperatively were identified and classified using the Clavien-Dindo classification system.14 Procedure duration (time elapsed from endoscope insertion into the patient's body to procedure completion), operating room duration (time elapsed between the patient entering and leaving the operating room), and hospital stay (time elapsed between the patient entering the postanesthetic care unit and being discharged from the hospital) were recorded.
In comparing the LithoVue and reusable ureteroscope cohorts, chi-square and Fisher exact tests were used for qualitative data, and unpaired Student's t-test was used for continuous data. Statistical analyses were performed using Stata/SE, version 14.1 (StataCorp, College Station, TX). Data are expressed as mean ± standard deviation or percentage with p-values.
Results
One hundred twenty-nine study cases utilizing LithoVue and 74 study controls utilizing reusable fiber-optic ureteroscopes were identified for comparison. After exclusions, 115 study cases (63.9% total) and 65 study controls (36.1% total) were included in the analysis.
Patient mean age at surgery was 53.8 ± 14.4 years, with 51.1% males, and a mean body mass index (BMI) of 29.6 ± 9.0 kg/m2. Surgery was performed for urinary stone treatment (78.9%), diagnostic ureteroscopy (17.2%), and treatment of urothelial carcinoma (3.9%). The LithoVue cohort contained significantly older patients compared with the control cohort (55.8 vs 50.5 years, p < 0.05), but was otherwise similar in terms of gender, BMI, procedural indication, prestenting before surgery, use of access sheath, and laterality (Table 1).
Table 1.
Patient Demographic and Perioperative Parameters
| Parameter | Total (n = 180) | LithoVue (n = 115) | Reusable ureteroscope (n = 65) | p-value |
|---|---|---|---|---|
| Age at surgery (years), mean ± SD | 53.8 ± 14.4 | 55.8 ± 15.1 | 50.5 ± 12.6 | <0.05 |
| Gender, n (%) | ||||
| Female | 88 (48.9%) | 54 (47.0%) | 34 (52.3%) | 0.49 |
| Male | 92 (51.1%) | 61 (53.0%) | 31 (47.7%) | |
| BMI (kg/m2), mean ± SD | 29.6 ± 9.0 | 29.1 ± 8.6 | 30.6 ± 9.6 | 0.27 |
| Procedural indication, n (%) | ||||
| Stone removal | 142 (78.9%) | 92 (80.0%) | 50 (76.9%) | 0.52 |
| Diagnostic | 31 (17.2%) | 20 (17.4) | 11 (16.9%) | |
| Urothelial cancer treatment | 7 (3.9%) | 3 (2.6%) | 4 (6.2%) | |
| Procedural laterality, n (%) | ||||
| Left | 86 (47.8%) | 53 (46.1%) | 33 (50.8%) | 0.73 |
| Right | 79 (43.9%) | 53 (46.1%) | 26 (40.0%) | |
| Bilateral | 15 (8.3%) | 9 (7.8%) | 6 (9.2%) | |
| Prestenting, n (%) | 47 (26.1%) | 35 (30.4%) | 12 (18.5%) | 0.08 |
| Ureteral access sheath utilization, n (%) | 130 (72.2%) | 82 (71.3%) | 48 (73.9%) | 0.72 |
BMI = body mass index; SD = standard deviation.
Within the subset of cases performed for stone removal (n = 142), stone burden was assessed using computed tomography scan in 73.2% and ultrasound in the remainder. The ratio of imaging modality used was not statistically significantly different between the LithoVue and reusable ureteroscope cohorts. The mean number of stones treated was 1.9 ± 1.6 and the mean overall stone burden was 15.2 ± 10.7 mm and 44.7% of cases demonstrated lower pole stone on preoperative imaging. Preoperative stone and collecting system characteristics were not statistically significantly different between the LithoVue and reusable ureteroscope cohorts (Table 2).
Table 2.
Stone Characteristics for Procedures Performed for Stone Removal
| Parameter | Total (n = 142) | LithoVue (n = 92) | Reusable ureteroscope (n = 50) | p-value |
|---|---|---|---|---|
| Imaging modality to assess preoperative stone characteristics, n (%) | ||||
| CT scan | 104 (73.2%) | 70 (76.1%) | 34 (68.0%) | 0.30 |
| Ultrasound | 38 (26.8%) | 22 (23.9%) | 16 (32.0%) | |
| Number of stones, mean ± SD | 1.9 ± 1.6 | 2.0 ± 1.7 | 1.6 ± 1.3 | 0.15 |
| Total stone burden (mm), mean ± SD | 15.2 ± 10.7 | 14.7 ± 9.9 | 16.3 ± 12.2 | 0.40 |
| Lower pole stone treated, n (%) | 67 (44.7%) | 44 (45.4%) | 23 (46.0%) | 0.82 |
| Degree of hydronephrosis | ||||
| Absent | 74 (52.5%) | 48 (52.2%) | 26 (53.1%) | 0.99 |
| Mild | 35 (24.8%) | 23 (25.0%) | 12 (24.5%) | |
| Moderate to severe | 32 (22.7%) | 21 (22.8%) | 11 (22.4%) | |
CT = computed tomography.
Intraoperatively, scope failure occurred in 10 cases (5.6%) of the overall cohort, and this incidence was not statistically significantly different between the two groups (Table 3). Within LithoVue cases, two failures occurred after an attempt to pass a stiff instrument through the scope, resulting in deflection mechanism malfunction. In one case, while activating a 365-μm laser fiber with the scope's tip fully flexed downward, the fiber broke within the scope leading to working channel sidewall perforation and loss of the digital image. Use of a Bugbee™ fulgurating electrode caused image loss during Bugbee activation for one case. The final failure occurred when an error message appeared after plugging in the scope with no clear explanation of underlying cause. Within the five reusable scope failures, all were sent for repair due to either loss of image quality or significant loss of deflection.
Table 3.
Intraoperative and Postoperative Outcomes
| Parameter | Total (n = 180) | LithoVue (n = 115) | Reusable ureteroscope (n = 65) | p-value |
|---|---|---|---|---|
| All cases | ||||
| Scope failure | 10 (5.6%) | 5 (4.4%) | 5 (7.7%) | 0.27 |
| Presence of postoperative complications | 18 (10.0%) | 9 (7.8%) | 9 (13.8%) | 0.20 |
| Parameter | Total (n = 142) | LithoVue (n = 92) | Reusable ureteroscope (n = 50) | p-value |
|---|---|---|---|---|
| Case performed for stone removal | ||||
| Lithotriptor device, n (%) | ||||
| Laser lithotripsy and basket | 117 (82.4%) | 74 (80.4%) | 43 (86.0%) | 0.21 |
| Basket only | 22 (15.5%) | 17 (18.5%) | 5 (10.0%) | |
| No lithotrite | 1 (0.7%) | 0 | 1 (2.0%) | |
| Missing data | 2 (1.4%) | 1 (1.1%) | 1 (2.0%) | |
| Stone-free status, n (%) | ||||
| Stone free | 41 (52.6%) | 24 (60.0%) | 17 (44.7%) | 0.36 |
| Insignificant residual fragment | 10 (12.8%) | 5 (12.5%) | 5 (13.2%) | |
| Significant residual fragment | 27 (34.6%) | 11 (27.5%) | 16 (42.1%) | |
| Presence of postoperative complications | 14 (9.9%) | 5 (5.4%) | 9 (18.0%) | <0.05 |
| Primary stone composition, n (%) | ||||
| Calcium oxalate | 75 (52.8%) | 75 (47.8%) | 31 (62.0%) | 0.11 |
| Calcium carbonate | 13 (9.2%) | 7 (7.6%) | 6 (12.0%) | |
| Calcium phosphate | 2 (1.4%) | 0 | 2 (4.0%) | |
| Uric acid | 10 (7.0%) | 8 (8.7%) | 2 (4.0%) | |
| Struvite | 5 (3.5%) | 5 (5.4%) | 0 | |
| Cystine | 2 (1.4%) | 2 (2.2%) | 0 | |
| Other | 1 (0.7%) | 1 (1.1%) | 0 | |
During cases performed for stone removal, a combination of laser lithotripsy and basket retrieval was used in most cases (82.4%). Perioperative complications were found in 14 total cases and mostly categorized as Clavien-Dindo class 1 or 2. The complication rate was lower in the LithoVue group compared with the reusable scope group (5.4% vs 18.0%, p < 0.05). In the LithoVue cases, these included three instances of urinary tract infection, one case of postoperative ileus, and one case with severe flank pain requiring readmission. In the reusable ureteroscope controls, urinary infection was seen in three cases, significant postoperative pain in two, prerenal acute kidney injury in one, stent migration in one, and ureteral injury requiring unanticipated intervention in two. Postoperative imaging was requested of all patients, but only 54.9% of the total study group followed up with kidney, ureter, and bladder radiograph or ultrasound surveillance imaging. These demonstrated stone-free status in 52.6% of total cases, insignificant residual fragments (<2 mm) in 12.8% of cases, and significant residual fragments (larger than 2 mm) in 34.6% of total cases. Stone-free and residual fragment rates were not significantly different between the two groups. Data on stone composition were available in 108 cases (76.0% of total) and revealed calcium oxalate (52.8%) as the most common primary component (Table 3).
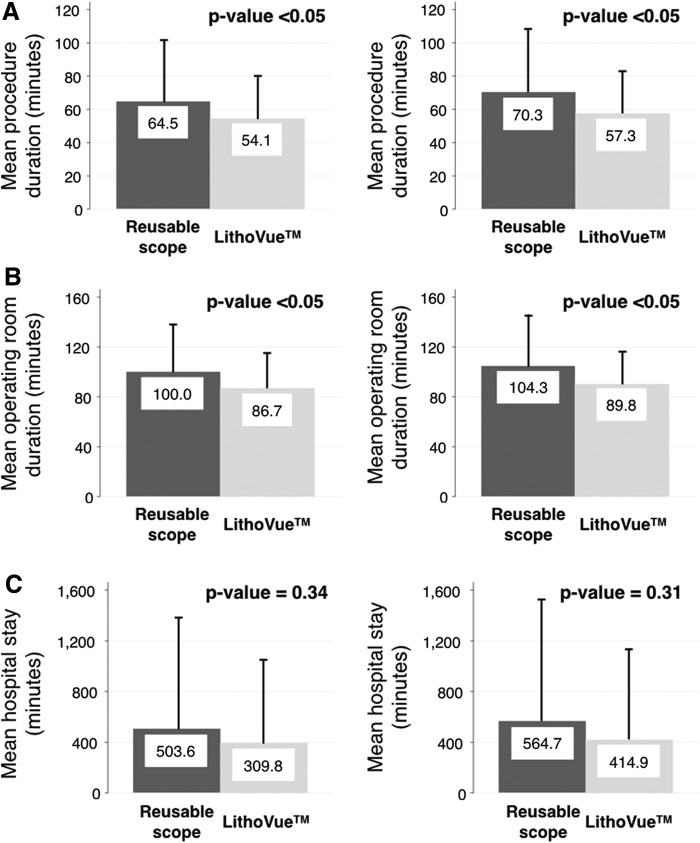
The overall mean procedure duration was 10.4 minutes shorter in the LithoVue cohort (64.5 vs 54.1 minutes, p < 0.05) compared with the reusable ureteroscope cohort. This difference widened to 13 minutes and remained statistically significant in cases performed for stone removal (70.3 vs 57.3 minutes, p < 0.05), but was not apparent for diagnostic or urothelial carcinoma procedures. The overall operating room duration was also shortened in stone removal cases (104.3 vs 89.8 minutes for LithoVue and reusable cases, respectively, p < 0.05). Mean hospital stay for all cases was 430.7 minutes and there were no statistically significant differences between the two study groups (Fig. 1).
FIG. 1.
Impact of LithoVue™ use on procedure duration and hospital stay. (A) Mean procedure duration decreased from 64.5 ± 37.0 to 54.1 ± 25.7 minutes (p < 0.05) for all procedures (left panel) and from 70.3 ± 36.9 to 57.3 ± 25.1 minutes (p < 0.05) for stone removal procedures (right panel) with the use of LithoVue. (B) Mean operating room duration decreased from 100.0 ± 38.8 to 86.7 ± 28.2 minutes (p < 0.05) for all procedures (left panel) and from 104.3 ± 39.4 to 89.8 ± 27.8 minutes (p < 0.05) for stone removal procedures (right panel) with the use of LithoVue. (C) Mean hospital stay changed from 503.6 ± 879.7 to 309.8 ± 673.2 minutes (p = 0.34) for all procedures (left panel) and from 564.7 ± 981.1 to 414.9 ± 727.8 minutes (p = 0.31) for stone removal procedures (right panel) with the use of LithoVue, differences that were not statistically significantly different. Comparisons between reusable flexible ureteroscope and LithoVue outcomes were performed using unpaired Student's t-test. Data shown are mean ± standard deviation.
With univariate regression, the use of LithoVue was associated with a 13.1-minute decrease in procedure duration, while increasing stone size was associated with significant increases in procedure duration. Using multivariate regression analysis, controlling for stone size, patient age, and BMI, the use of LithoVue was associated with a 14- and 15.5-minute shortening of procedure (p < 0.05) and operating room durations (p < 0.05), respectively. Controlling for patient age, BMI, and LithoVue use, increasing stone size by increments of 10 mm was associated with a lengthened procedure duration by 40.35 minutes (p < 0.05) and operating room duration by 38.92 minutes (p < 0.05) (Tables 4 and 5).
Table 4.
Univariate and Multivariate Analyses to Predict Procedure Duration in Minutes for Stone Removal Cases
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| Variable | Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value |
| Stone burden (mm) | ||||||
| <10 | Ref | Ref | ||||
| ≥10–20 | 12.05 | 1.43, 22.66 | <0.05 | 14.76 | 4.18, 25.34 | <0.05 |
| ≥20–30 | 27.39 | 12.68, 42.09 | <0.05 | 29.92 | 15.34, 44.50 | <0.05 |
| ≥30 | 39.57 | 24.26, 54.89 | <0.05 | 40.35 | 25.04, 55.65 | <0.05 |
| Age (years) | ||||||
| <40 | Ref | Ref | ||||
| ≥40–60 | 6.02 | −8.34, 20.37 | 0.41 | 6.60 | −6.80, 20.00 | 0.33 |
| ≥60 | 4.31 | −10.55, 19.16 | 0.57 | 9.64 | −4.38, 23.65 | 0.18 |
| BMI (kg/m2) | ||||||
| <25 | Ref | Ref | ||||
| ≥25–30 | 3.49 | −9.60, 16.58 | 0.60 | 2.40 | −9.70, 14.51 | 0.70 |
| ≥30–35 | −3.84 | −18.62, 10.94 | 0.61 | −11.35 | −24.91, 2.20 | 0.10 |
| ≥35 | 2.65 | −11.29, 16.59 | 0.71 | −1.49 | −14.16, 11.19 | 0.82 |
| LithoVue use | −13.07 | −23.41, −2.73 | <0.05 | −14.00 | −23.95, −4.04 | <0.05 |
CI = confidence interval.
Table 5.
Univariate and Multivariate Analyses to Predict Operating Room Duration in Minutes for Stone Removal Cases
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| Variable | Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value |
| Stone burden | ||||||
| <10 | Ref | Ref | ||||
| ≥10–20 | 11.23 | −0.48, 22.93 | 0.06 | 14.40 | 2.70, 26.11 | <0.05 |
| ≥20–30 | 29.33 | 12.11, 45.55 | <0.05 | 31.84 | 15.71, 47.97 | <0.05 |
| ≥30 | 39.18 | 22.28, 56.08 | <0.05 | 38.92 | 21.99, 55.85 | <0.05 |
| Age | ||||||
| <40 | Ref | Ref | ||||
| ≥40–60 | 5.05 | −10.57, 20.67 | 0.52 | 5.00 | −9.82, 19.82 | 0.51 |
| ≥60 | 3.28 | −12.90, 19.45 | 0.69 | 8.37 | −7.13, 23.87 | 0.29 |
| BMI | ||||||
| <25 | Ref | Ref | ||||
| ≥25–30 | 3.92 | −10.27, 18.11 | 0.59 | 2.86 | −10.53, 16.25 | 0.67 |
| ≥30–35 | −2.02 | −18.05, 14.01 | 0.80 | −9.31 | −24.30, 5.69 | 0.22 |
| ≥35 | 8.89 | −6.22, 24.00 | 0.25 | 5.14 | −8.89, 19.16 | 0.47 |
| LithoVue use | −14.54 | −25.77, −3.30 | <0.05 | −15.51 | −26.52, −4.50 | <0.05 |
Discussion
These data represent a case–control clinical comparison study between LithoVue and flexible reusable fiber-optic ureteroscopes. The paradigm of disposable ureteroscopes may be clinically valuable for several reasons. Previous studies have demonstrated that LithoVue represents a feasible alternative to reusable ureteroscopes in terms of visual imaging, scope performance, and user satisfaction.11 In light of growing concerns over severe infections transmitted with reusable duodenoscopes,15 utilizing a single-use ureteroscope may help allay fears of both patients and providers that a reusable ureteroscope might one day be discovered to be a source of an infection.16 Single-use products may be easier for facilities, reducing the system stressors placed on the hospital and central processing by the needs of scope reprocessing and maintenance. In line with these potential advantages, understanding the clinical performance of LithoVue bears exploration.
While the clinical benefits of disposable ureteroscopes are not well understood, we found that LithoVue cases were, on average, 10 minutes shorter and resulted in almost a quarter of an hour less total time in the operating room compared with reusable fiber-optic ureteroscopes. LithoVue was also associated with a statistically significantly decreased complication rate compared with the use of reusable scopes. Our reusable ureteroscope cohort experienced a threefold increased rate of complications compared with LithoVue use, and while none resulted in long-term patient morbidity, these different overall rates were striking.
These time savings might impact clinical utility in several ways. A 10–15-minute time reduction, while not a large absolute number of minutes, represents on average a 10%–20% time reduction in procedure length. With our institutional cost per minute in the operating room, this might represent around $250 savings, although these cost savings might change between institutions based on multiple factors. This cost factor certainly warrants further study. From purely a time efficiency standpoint, in aggregate, shortening the procedural time may increase the number of cases that can be performed per day when multiple cases are planned back to back, leading to a net increased access for patients in need of ureteroscopic care. With regard to a difference in complication rate, at face value, this clinical benefit of utilizing a disposable scope appears compelling. Complications related to ureteroscopy occur at a relatively low rate compared with other procedures1 and generally comprise less severe Clavien-Dindo scores.17 However, decreasing the complication rate for ureteroscopy optimizes speed to full patient recovery.
While these observations underscore the idea that LithoVue use may be associated with clinical benefits over reusable ureteroscopes, our study was not directed toward understanding the etiology for these differences. We can, however, speculate on factors that might account for differences in procedural length and complication rate. First, we compared digital disposable scopes with fiber-optic reusable scopes. The disposable scope is lighter than the reusable scope and flexes like a new scope with every case. These intrinsic characteristics might account for faster performance of LithoVue in our study. However, it is also possible that the difference in procedure length might be due to fundamental differences that exist between digital and fiber-optic scopes. Others have demonstrated that digital scopes outperform fiber-optic scopes in terms of visual image and this difference may account for increased efficiency during cases related to procedural length.18 While we cannot be certain of an explanation for this time difference, in looking at the effect of stone size on procedure time, these two factors were directly correlated, providing a positive control for our multivariate analysis and some confirmation that these procedure duration differences warrant further study. With regard to the difference in complication rates, the fact that the complications occurring in the control reusable scope group were not related to infection indicates that these differences were possibly reflective of the study design rather than a factor intrinsically related to the ureteroscopes themselves. If there were differences in infection rates between the two groups, one might consider the reprocessing of reusable scopes as a reason to account for these differences16; however, this was not the case.
Several study design aspects bear consideration. Our study was not randomized, and the control group was derived from an unpublished quality control study previously completed 1 year before the LithoVue cohort data collection. This control group represents a convenient control since their data collection was completed in an identical manner to the contemporary LithoVue cohort. In addition, no procedural, surgical site, or staff differences occurred between the two time periods, and the two cohorts were comparable with regard to demographics. However, it is certainly possible that factors related to the cohorts themselves might have been different. If, for example, the control cohort represented a more complex type of patient in dimensions not measured by demographics and BMI, they may be expected to experience a higher complication rate. This might include difference in comorbidity that would lead patients to different clinical outcomes, for example. We also recognize that a larger number of patients were enrolled into the LithoVue cohort over a shorter period of time compared with the control cohort. In looking back at institutional differences between the study periods, it appears that we have experienced increasing case volume for ureteroscopy at our institution since 2013. This may be explained by an institutional effort initiated in 2015 to drive increased hospital volume growth that affected outreach efforts as well as provider payments. We therefore think that while there is value to the current study, in that it demonstrates possible areas of clinical benefit for the disposable ureteroscope, our study underscores the need for a randomized control trial comparing reusable digital ureteroscopes with digital disposable scopes.
The qualitative performance and cost-effectiveness of LithoVue also warrant discussion. The need for scope replacement, maintenance, and repair is one area that has been studied with regard to flexible ureteroscope usage.19,20 Regarding failure of LithoVue, we experienced five occurrences of scope failure intraoperatively. The overall LithoVue failure rate of 4.4% was comparable with that of our reusable ureteroscopes (7.7%) and consistent with recent failure rates reported in the literature for reusable ureteroscopes.3,4,19 In addition, limited studies regarding cost analysis for disposable scopes have been performed,21 indicating that these scopes may be comparable in cost-effectiveness with reusable scopes. Both the questions of qualitative and cost benefits for LithoVue are of interest, but beyond the scope of the current study.
From a clinical performance perspective, we found comparable postoperative stone-free status between our two study groups, demonstrating that implementation of LithoVue can be done safely with preservation of clinical outcomes. To ensure that no learning curve effects impacted clinical performance in the LithoVue cohort, we divided this study cohort in half based on case number. When comparing these two groups with regard to procedure time and complication rate, there was no difference (data not shown) reflecting that there may not be a large learning curve involved with adopting LithoVue.22 Another important note to make is that ultrasound imaging was used preoperatively in about one-fourth of patients and may not accurately assess stone burden.23 However, the ratio of imaging modality used was similar between the LithoVue and reusable cohorts. Therefore, any effect of imaging modality on assessment of stone burden should have been relatively uniform between the two cohorts. Although significant residual stone fragments were found in one-third of our patients, this relatively high number is comparable with published studies24 and did not differ between the case and control groups. These results should be viewed with the caveat that LithoVue is new enough such that long-term clinical outcomes beyond 3 months were not available for patients. In addition, we found that ∼1/3 of our patients did not return for follow-up after surgery and so our stone-free results are limited by this loss to follow-up.
In considering our study results, several additional shortcomings should also be accounted for. Most cases were performed for the treatment of urolithiasis and our results may therefore not be generalizable to other upper urinary tract pathologies. Importantly, the study controls utilized fiber-optic reusable flexible ureteroscopes. LithoVue is a digital scope, and while performance characteristics between fiber-optic and digital ureteroscopes are similar, differences may exist in image quality, flexion, and durability.25,26 Therefore, our results may be most applicable for institutions and surgeons currently using fiber-optic ureteroscopes rather than reusable digital ureteroscopes. Moreover, the control cohort utilized repaired scopes rather than newly purchased ones, and we were unable to ascertain the number of repairs or prior uses for each scope at study initiation. Overall, however, we believe our study represents a first clinical comparison between current paradigms of reusable ureteroscopes and the next generation of disposable ureteroscopes.
Conclusions
We present a case–cohort study of a large single-center experience with LithoVue. Our data suggest that LithoVue represents a feasible safe alternative to reusable flexible ureteroscopes. Compared with the reusable fiber-optic flexible ureteroscope, LithoVue use was associated with a shorter procedure and overall operating room duration. However, these findings warrant further investigation.
Abbreviations Used
- BMI
body mass index
- CI
confidence interval
- CT
computed tomography
- ReSKU™
Registry for Stones of the Kidney and Ureter
- SD
standard deviation
- UCSF
University of California, San Francisco
Acknowledgments
Authors have received salary support from the following grants: NIH P20-DK-100863 (M.L.S., T.C.), NIH R21-DK-109433 (T.C.), and K12-DK-07-006: Multidisciplinary K12 Urologic Research Career Development Program (T.C.). No funding or surgical instruments were provided by industry sponsors.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.de la Rosette J, Denstedt J, Geavlete P, et al. . The clinical research office of the endourological society ureteroscopy global study: Indications, complications, and outcomes in 11,885 patients. J Endourol 2014;28:131–139 [DOI] [PubMed] [Google Scholar]
- 2.Turk C, Petrik A, Sarica K, et al. . EAU guidelines on interventional treatment for urolithiasis. Eur Urol 2016;69:475–482 [DOI] [PubMed] [Google Scholar]
- 3.Carey RI, Gomez CS, Maurici G, et al. . Frequency of ureteroscope damage seen at a tertiary care center. J Urol 2006;176:607–610; discussion 610 [DOI] [PubMed] [Google Scholar]
- 4.Carey RI, Martin CJ, Knego JR. Prospective evaluation of refurbished flexible ureteroscope durability seen in a large public tertiary care center with multiple surgeons. Urology 2014;84:42–45 [DOI] [PubMed] [Google Scholar]
- 5.Buttice S, Sener TE, Netsch C, et al. . LithoVue: A new single-use digital flexible ureteroscope. Cent European J Urol 2016;69:302–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Proietti S, Dragos L, Molina W, et al. . Comparison of new single-use digital flexible ureteroscope versus nondisposable fiber optic and digital ureteroscope in a cadaveric model. J Endourol 2016;30:655–659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaplan A, Radvak D, Shin R, et al. . Evaluation of a novel single use flexible ureteroscope. J Urol 2016;195:e473. [DOI] [PubMed] [Google Scholar]
- 8.Wiseman O, Keeley F, Traxier O, et al. . Comparison of a new single-use digital flexible ureteroscope (Lithovue™) to a non-disposable fibre-optic flexible ureteroscope in a live porcine model. J Urol 2016;195:e682 [Google Scholar]
- 9.Eisner B. Evaluating the image quality of a novel single-use digital flexible ureteroscope. J Endourol 2015;29:A348 [Google Scholar]
- 10.Leveilee R, Fell K. Impressive performance: New disposable digital ureteroscope allows for extreme lower pole access and use of 365 μm holmium laser fiber. J Endourol Case Rep 2016;2:114–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doizi S, Kamphuis G, Giusti G, et al. . First clinical evaluation of a new single-use flexible ureteroscope (LithoVue): A European prospective multicentric feasibility study. World J Urol 2016. [Epub ahead of Print]; DOI: 10.1007/s00345-016-1936-x [DOI] [PubMed] [Google Scholar]
- 12.Chang HC, Tzou DT, Usawachintachit M, et al. . Rationale and design of the registry for stones of the kidney and ureter (ReSKU™): A prospective, observational registry to study the natural history of urolithiasis patients. J Endourol 2016;30:1332–1338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghani KR, Wolf JS., Jr. What is the stone-free rate following flexible ureteroscopy for kidney stones? Nat Rev Urol 2015;12:363. [DOI] [PubMed] [Google Scholar]
- 14.Clavien PA, Barkun J, de Oliveira ML, et al. . The Clavien-Dindo classification of surgical complications: Five-year experience. Ann Surg 2009;250:187–196 [DOI] [PubMed] [Google Scholar]
- 15.Epstein L, Hunter JC, Arwady MA, et al. . New Delhi metallo-beta-lactamase-producing carbapenem-resistant Escherichia coli associated with exposure to duodenoscopes. JAMA 2014;312:1447–1455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang CL, Su LH, Lu CM, et al. . Outbreak of ertapenem-resistant Enterobacter cloacae urinary tract infections due to a contaminated ureteroscope. J Hosp Infect 2013;85:118–124 [DOI] [PubMed] [Google Scholar]
- 17.Hyams ES, Munver R, Bird VG, et al. . Flexible ureterorenoscopy and holmium laser lithotripsy for the management of renal stone burdens that measure 2 to 3 cm: A multi-institutional experience. J Endourol 2010;24:1583–1588 [DOI] [PubMed] [Google Scholar]
- 18.Somani BK, Al-Qahtani SM, de Medina SD, et al. . Outcomes of flexible ureterorenoscopy and laser fragmentation for renal stones: Comparison between digital and conventional ureteroscope. Urology 2013;82:1017–1019 [DOI] [PubMed] [Google Scholar]
- 19.Knudsen B, Miyaoka R, Shah K, et al. . Durability of the next-generation flexible fiberoptic ureteroscopes: A randomized prospective multi-institutional clinical trial. Urology 2010;75:534–538 [DOI] [PubMed] [Google Scholar]
- 20.Kramolowsky E, McDowell Z, Moore B, et al. . Cost analysis of flexible ureteroscope repairs: Evaluation of 655 procedures in a community-based practice. J Endourol 2016;30:254–256 [DOI] [PubMed] [Google Scholar]
- 21.Martin CJ, McAdams SB, Abdul-Muhsin H, et al. . The economic implications of a reusable flexible digital ureteroscope: A cost-benefit analysis. J Urol 2016. [Epub ahead of print]; DOI: 10.1016/j.juro.2016.09.085 [DOI] [PubMed] [Google Scholar]
- 22.Usawachintachit M, Masic S, Allen IE, et al. . Adopting ultrasound guidance for prone percutaneous nephrolithotomy: Evaluating the learning curve for the experienced surgeon. J Endourol 2016;30:856–863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ganesan V, De S, Greene D, et al. . Accuracy of ultrasonography for renal stone detection and size determination: Is it good enough for management decisions? BJU Int 2016. [Epub ahead of print]; DOI: 10.1111/bju.13605 [DOI] [PubMed] [Google Scholar]
- 24.Pearle MS. Is ureteroscopy as good as we think? J Urol 2016;195(4P1):823–824 [DOI] [PubMed] [Google Scholar]
- 25.Multescu R, Geavlete B, Georgescu D, et al. . Conventional fiberoptic flexible ureteroscope versus fourth generation digital flexible ureteroscope: A critical comparison. J Endourol 2010;24:17–21 [DOI] [PubMed] [Google Scholar]
- 26.Binbay M, Yuruk E, Akman T, et al. . Is there a difference in outcomes between digital and fiberoptic flexible ureterorenoscopy procedures? J Endourol 2010;24:1929–1934 [DOI] [PubMed] [Google Scholar]