Abstract
Background
Atrial fibrillation (AF) is one of the most critical and frequent arrhythmias precipitating morbidities and mortalities. The complete blood count (CBC) test is an important blood test in clinical practice and is routinely used in the workup of cardiovascular diseases. This systematic review with meta-analysis aimed to determine the strength of evidence for evaluating the association of hematological parameters in the CBC test with new-onset and recurrent AF.
Material/Methods
We conducted a meta-analysis of observational studies evaluating hematologic parameters in patients with new-onset AF and recurrent AF. A comprehensive subgroup analysis was performed to explore potential sources of heterogeneity.
Results
The literature search of all major databases retrieved 2150 studies. After screening, 70 studies were analyzed in the meta-analysis on new-onset AF and 23 studies on recurrent AF. Pooled analysis on new-onset AF showed platelet count (PC) (weighted mean difference (WMD)=WMD of −26.39×109/L and p<0.001), mean platelet volume (MPV) (WMD=0.42 FL and p<0.001), white blood cell (WBC) (WMD=−0.005×109/L and p=0.83), neutrophil to lymphocyte ratio (NLR) (WMD=0.89 and p<0.001), and red blood cell distribution width (RDW) (WMD=0.61% and p<0.001) as associated factors. Pooled analysis on recurrent AF revealed PC (WMD=−2.71×109/L and p=0.59), WBC (WMD=0.20×109/L (95% CI: 0.08 to 0.32; p=0.002), NLR (WMD=0.37 and p<0.001), and RDW (WMD=0.28% and p<0.001).
Conclusions
Hematological parameters have significant ability to predict occurrence and recurrence of AF. Therefore, emphasizing the potential predictive role of hematological parameters for new-onset and recurrent AF, we recommend adding the CBC test to the diagnostic modalities of AF in clinical practice.
MeSH Keywords: Atrial Fibrillation, Blood Platelets, Diagnosis, Meta-Analysis
Background
Atrial fibrillation (AF) is one of the most critical and frequent arrhythmias precipitating morbidities and mortalities such as hemodynamic instability, thromboembolism, and stroke, increasing hospital re-admissions and, consequently, health care costs. In general, AF negatively affects patient quality of life [1]. AF alone is associated with 1.5% to 1.9% increase in risk of mortality in a wide spectrum of ages in both genders [2]. Moreover, the situation is likely to worsen since the number of people with AF is expected to double by 2050 [2,3].
The pathophysiological mechanism in AF is highly complex and multifactorial [3]. Prothrombotic state, inflammation, and oxidative stress may play important roles in the occurrence of supraventricular arrhythmia [4]. Introduction of practical and available diagnostic methods and their wider use allows for better identification of patients with new-onset or recurrent AF [3,4]. Traditionally, the major focus in diagnosis and management of AF has been patient medical history, examination, and detection of AF and paroxysmal AF (PAF) using cardiac monitoring.
Complete blood count (CBC) is an important blood test routinely used in clinical practice for workup of cardiovascular diseases [5]. The relationship between blood parameters in CBC tests and clinical outcomes in patients with ST-segment elevation myocardial infarction has been well documented [5]. However, the diagnostic performance of blood parameters for AF, alone and in combination with other diseases, is still unknown.
Various studies have reported the association of hematological parameters with new-onset and recurrent AF, but the data have been largely inconclusive. This systematic review with meta-analysis sought to determine the strength of evidence in terms of the potential association between a large number of hematologic parameters that can be easily obtained using the CBC test and new-onset and recurrent AF.
Material and Methods
Literature search
A comprehensive literature search was conducted in electronic scientific databases (Medline/PubMed, Embase, Web of Science, and Google Scholar) from their inception through November 30, 2016 to identify relevant studies on the association between blood parameters in CBC tests and new-onset and recurrent AF. Predefined search terms were as follows: “white blood cell count”, “WBC”, “leucocyte”, “neutrophil to lymphocyte ratio”, “NLR”, “platelet count”, “mean platelet volume”, “MPV”, “platelet distribution width” “PDW”, “red blood cell count”, “RBC count”, “red blood cell distribution width”, “RDW”, and “atrial fibrillation” or “supraventricular arrhythmia”. No restrictions were applied regarding sample size of studies, language, and time of publication. To assess additional studies not indexed in common databases, all retrieved references of the enrolled studies, recent published review articles, and meta-analyses were also checked.
Study selection
Studies were included in the analysis when they met the following criteria: 1) human subjects; 2) cohort or case-control studies; 3) comparative studies between AF and non-AF-cohorts in terms of blood parameters; 4) studies comparing patients with recurrent AF (re-occurrence of AF in patients with history of treatment with anti-arrhythmic or electrophysiological interventions for AF) with those with non-recurrent AF focusing on blood parameters. Manuscripts that did not undergo peer-review, abstracts from congress presentations only, and gray literature were not included.
Primary and secondary blood parameters
Platelet count, MPV, PDW, WBC count, NLR, RBC count, and RDW were considered primary blood parameters. MCV, MCHC, HCT, and Hb were defined as secondary parameters.
Data extraction and outcome measures
Six investigators (S.A-H-S, A.S, S.Y, T.L, M-P. S, and J-S. J) independently extracted the data. Discrepancies were resolved by a consensus standardized abstraction checklist used for recording data in each included study. Disagreements were discussed and resolved by senior authors (A.W, A.F-P, G.B.Z, G.D.S and H.C). The following items were extracted from the included studies: author name; publication year; country; study design; sample size; mean age; gender; coexistent cardiovascular diseases, and risk factors, such as diabetes mellitus, hypertension, and history of myocardial infarction; percentage of used anticoagulants; AF type; and details of blood parameters. In order to examine heterogeneity among trials, subgroup analyses of disparities in patients’ characteristics were carried out for: (1) the era of publication (pre-2000 vs. post-2000); (2) geographical area (Asia, Europe, Africa, North-America, South-America, and Oceania); (3) study design (case-control vs. cohort); (4) sample size of studies (≤300 vs. >300); (5) mean age (≤60 vs. >60 years); (6) percentage of male patients (≤70% vs. >70%); (7) presence of diabetes (≤30% vs. >30%); (8) presence of hypertension (≤70% vs. >70%); (9) cigarette smoking (≤30% vs. >30%); (10) presence of myocardial infarction (≤20% vs. >20%); (11) use of cardiovascular drugs, such as diuretics, angiotensin converting enzyme inhibitors, statins and beta-blockers (for each: ≤70% vs. >70%); (12) AF-classification (chronic vs. non-chronic); (13) type of AF (paroxysmal, persistent, permanent); and (12) anticoagulation (code-1: not receiving anticoagulants in both groups; code-2: all participants receiving anticoagulants in both groups; code-3: range of percentages between both groups >50%; code-4: range of percentages between both groups <50%; code-5: no information available about anticoagulation in both groups; and code-6: anticoagulation information not available for 1 group only).
Homogenization of extracted data
Continuous data are expressed as mean ± standard deviation (SD). For studies reporting interquartile ranges, the mean was estimated according to the formula [minimum+maximum+2(median)]/4 and SD was calculated based on the formula (maximum–minimum)/4 for groups with sample sizes of n ≤70 and (maximum–minimum)/6 for sample sizes of >70 [6].
Quality assessment and statistical analysis
The Newcastle-Ottawa scale was independently used by 3 investigators (S.A-H-S, M.G, and L.M) to assess the quality of studies [7]. Total scores ranged from 0 (worst quality) to 9 (best quality) for case-control or cohort studies. Data were analyzed by STATA 11.0 using METAN and METABIAS modules. For non-categorical data, pooled effect size measured was the weighted mean difference (WMD) with 95% CI. P value of <0.1 for Q test or I2 >50% showed significant heterogeneity among the studies. Heterogeneity among trials was examined by applying a random-effects model when indicated. Publication bias was assessed using the Begg tests. P value of <0.05 was considered statistically significant.
Results
Literature search strategy and included studies
Overall, 2150 studies were retrieved from the literature search and screened databases. We excluded 1179 studies (63.55%) after detailed evaluation during the first review due to unnecessary information (n=750), inadequate report of endpoints of interest (n=370), or report of non-matched data based on mean ±SD or median [minimum–maximum] (n=59). In total, 971 potentially relevant full-text articles were screened, with 70 studies being analyzed in the meta-analysis on new-onset AF and 23 studies on recurrent AF (Supplementary Table 1) [8–77].
Association of hematologic parameters with new-onset AF
Platelet count
A total of 6468 cases were selected from 48 studies, of which 3098 were allocated to the AF group and 3370 to the SR group. Mean platelet count was 236.9×109/L in the AF group and 239.9×109/L in the SR group (details in Tables 1 and 2). Using a random-effects model, pooled analysis revealed that the mean platelet count was considerably lower in patients with AF than in patients with SR, with a WMD of −26.39×109/L (95% CI: −27.80 to −24.99; p<0.001, Figure 1). Significant heterogeneity was observed among the studies (I2=92.9%; heterogeneity p<0.001).
Table 1.
Characteristics of included studies for meta-analysis of association of hematologic parameters with AF.
| First Author | Year | Country | Design | N-AF | N-SR | Age-AF | Age-SR | Male-AF | Male-SR | AC-AF | AC-SR | Type of AF | NOS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Occurrence of AF | |||||||||||||
| Balci (Male subjects) [8] | 2016 | Turkey | Case-control | 18 | 17 | ND | ND | 100 | 100 | ND | ND | ND | 8 |
| Balci (Female subjects) [8] | 2016 | Turkey | Case-control | 65 | 88 | ND | ND | 0 | 0 | ND | ND | ND | 8 |
| Gurses [9] | 2016 | Turkey | Case-control | 86 | 86 | 56.6 | 56.4 | 51.2 | 53.5 | ND | ND | Combined types | 9 |
| Karatas [10] | 2016 | Turkey | Case-control | 40 | 581 | 65.7 | 56.4 | 70 | 75 | 100 | 100 | ND | 8 |
| Korantzopoulos [11] | 2016 | Greece | Case-control | 32 | 69 | 78 | 75 | 47 | 46 | 60 | 0 | Combined types | 9 |
| Akdag [12] | 2015 | Turkey | Case-control | 96 | 52 | 63.6 | 64.5 | 64 | 56 | 54.16 | ND | Combined types | 9 |
| Akyuz [13] | 2015 | Turkey | Case-control | 40 | 50 | 63 | 61.5 | 72.5 | 72 | 20 | 14 | Combined types | 7 |
| Chavaria [14] | 2015 | USA | Cohort | 40 | 250 | 70.6 | 60.7 | 65 | 84 | ND | ND | ND | 6 |
| Drabik (Persistent AF) [15] | 2015 | Poland | Case-control | 47 | 50 | 60.8 | 59.4 | 65.95 | 64 | 38.3 | 26 | Persistent | 9 |
| Drabik (Paroxysmal AF) [15] | 2015 | Poland | Case-control | 41 | 50 | 60.6 | 59.4 | 46.3 | 64 | 51.2 | 26 | Paroxysmal | 9 |
| Acet (Paroxysmal AF) [16] | 2014 | Turkey | Case-control | 71 | 63 | 63 | 61.1 | 42 | 46 | ND | ND | Paroxysmal | 9 |
| Acet (Persistent and permanent AF) [16] | 2014 | Turkey | Case-control | 63 | 63 | 64.6 | 61.1 | 41 | 46 | ND | ND | Combined types | 9 |
| Arik (effective INR) [17] | 2014 | Turkey | Case-control | 125 | 123 | 70.4 | 68.9 | 41.6 | 39.8 | ND | ND | Permanent | 8 |
| Arik (ineffective INR) [17] | 2014 | Turkey | Case-control | 125 | 123 | 70 | 68.9 | 36 | 39.8 | ND | ND | Permanent | 8 |
| Distelmaier [18] | 2014 | USA | Case-control | 66 | 132 | 73.5 | 73.5 | 61 | 61 | ND | ND | ND | 7 |
| Erdogan (with normal ventricular rate) [19] | 2014 | Turkey | Case-control | 34 | 33 | 70.5 | 68.6 | 47.05 | 51.51 | 66.6 | 0 | Permanent | 10 |
| Erdogan (with high ventricular rate) [19] | 2014 | Turkey | Case-control | 30 | 33 | 69 | 68.6 | 46.6 | 51.51 | 83.3 | 0 | Permanent | 10 |
| Zheng [20] | 2014 | China | Case-control | 117 | 100 | 64.37 | 59.1 | 57.26 | 60 | ND | ND | ND | 8 |
| Xu (without thrombotic events) [21] | 2014 | China | Cohort | 57 | 58 | 65.19 | 67 | 50.9 | 50 | 50.9 | 15.5 | ND | 7 |
| Xu (with thrombotic events) [21] | 2014 | China | Cohort | 57 | 58 | 68.95 | 67 | 52.6 | 50 | 49.1 | 15.5 | ND | 7 |
| Gungor [22] | 2014 | Turkey | Case-control | 117 | 60 | 48.3 | 46.1 | 60.6 | 55 | 75.2 | 8.3 | Combined types | 9 |
| Liu [23] | 2014 | China | Case-control | 133 | 101 | ND | ND | ND | ND | ND | ND | Paroxysmal | 8 |
| Sarikaya [24] | 2014 | Turkey | Case-control | 63 | 63 | 71.09 | 70.97 | 47.8 | 52.2 | ND | ND | ND | 8 |
| Sonmez [25] | 2014 | Turkey | Case-control | 52 | 33 | 70 | 70 | 34.61 | 39.39 | 59.61 | 36.36 | Persistent | 8 |
| Ulu [26] | 2014 | Turkey | Case-control | 25 | 32 | ND | ND | ND | ND | ND | ND | ND | 7 |
| Berge [27] | 2013 | Norway | Cohort | 63 | 126 | 75 | 75 | 71.42 | 70.63 | 8 | 33 | Combined types | 9 |
| Ertas (without stroke) [28] | 2013 | Turkey | Case-control | 87 | 24 | 69 | 38 | 44 | 58 | 58 | 0 | ND | 6 |
| Ertas (with stroke) [28] | 2013 | Turkey | Case-control | 39 | 24 | 71 | 38 | 36 | 58 | 51 | 0 | ND | 6 |
| Gungor [29] | 2013 | Turkey | Case-control | 70 | 70 | 42.2 | 42.9 | 68.5 | 64.3 | ND | ND | Combined types | 7 |
| Turgut [30] | 2013 | Turkey | Case-control | 81 | 81 | 64 | 62 | 51 | 53 | 28 | 20 | ND | 7 |
| Jaremo (healthy control) [31] | 2013 | Sweden | Cohort | 58 | 24 | 69 | 66 | 79.3 | 54.16 | 12.06 | 0 | ND | 8 |
| Jaremo (disease control) [31] | 2013 | Sweden | Cohort | 58 | 72 | 69 | 74 | 79.3 | 56.9 | 12.06 | 41.66 | ND | 8 |
| Sahin [32] | 2013 | Turkey | Case-control | 72 | 72 | 65.01 | 64.72 | 48.2 | 51.3 | ND | ND | Persistent | 7 |
| Tekin [33] | 2013 | Turkey | Case-control | 107 | 112 | 74 | 73 | 31 | 40 | ND | ND | ND | 7 |
| Turfan (without stroke) [34] | 2013 | Turkey | Cohort | 77 | 58 | 63 | 56 | 57.4 | 51.7 | 44.3 | 0 | ND | 7 |
| Turfan (with stroke) [34] | 2013 | Turkey | Cohort | 63 | 58 | 69 | 56 | 52.4 | 51.7 | 41.3 | 0 | ND | 7 |
| Feng [35] | 2012 | China | Case-control | 185 | 189 | 65.9 | 65.7 | 62.7 | 60.8 | 76.8 | 83.1 | Combined types | 8 |
| Liu (Paroxysmal AF) [36] | 2012 | China | Cohort | 50 | 51 | 64.3 | 64.4 | 64 | 61 | 100 | 0 | Paroxysmal | 8 |
| Liu (Persistent AF) [36] | 2012 | China | Cohort | 56 | 51 | 67.2 | 64.4 | 61 | 61 | 100 | 0 | Persistent | 8 |
| Yoshizaki [37] | 2012 | Japan | Cohort | 24 | 152 | 74 | 66 | 75 | 77 | ND | ND | ND | 8 |
| Hayashi (Paroxysmal AF) [38] | 2011 | Japan | Case-control | 14 | 13 | 53.1 | 62.8 | 93 | 92 | 100 | 100 | Paroxysmal | 7 |
| Hayashi (Chronic AF) [38] | 2011 | Japan | Case-control | 14 | 13 | 60.1 | 62.8 | 93 | 92 | 100 | 100 | ND | 7 |
| Fu [39] | 2011 | China | Case-control | 90 | 79 | 54.1 | 54.8 | 70 | 57 | 22 | 0 | Combined types | 8 |
| Liu [40] | 2011 | China | Case-control | 50 | 401 | 61.8 | 54.9 | 54 | 48.87 | ND | ND | Combined types | 8 |
| Letsas (Paroxysmal AF) [41] | 2010 | Greece | Case-control | 45 | 48 | 67.4 | 61.3 | 62 | 56 | ND | ND | Paroxysmal | 9 |
| Letsas (Permanent AF) [41] | 2010 | Greece | Case-control | 41 | 48 | 71.9 | 61.3 | 63 | 56 | ND | ND | Permanent | 9 |
| Luan (Persistent AF) [42] | 2010 | China | Case-control | 27 | 26 | 62.04 | 44.46 | 55.56 | 46.15 | ND | ND | Persistent | 8 |
| Luan (Paroxysmal AF) [42] | 2010 | China | Case-control | 29 | 26 | 57.52 | 44.46 | 58.62 | 46.15 | ND | ND | Paroxysmal | 8 |
| Alberti [43] | 2009 | Italy | Case-control | 17 | 34 | 68.1 | 60.8 | 47.05 | 47.05 | 0 | 0 | Persistent | 7 |
| Dai [44] | 2009 | China | Case-control | 242 | 280 | 56.09 | 50.04 | 79.8 | 69.6 | ND | ND | Combined types | 8 |
| Ichiki [45] | 2009 | Japan | Case-control | 48 | 24 | 54 | 49 | 81.25 | 79.16 | ND | ND | Paroxysmal | 9 |
| Yao (Persistent AF) [46] | 2009 | China | Case-control | 72 | 78 | 55.4 | 52.8 | 79.2 | 74.4 | 15.3 | 7.7 | Persistent | 7 |
| Yao (Paroxysmal AF) [46] | 2009 | China | Case-control | 261 | 78 | 53.9 | 52.8 | 75.5 | 74.4 | 12.3 | 7.7 | Paroxysmal | 7 |
| Colkesen [47] | 2008 | Turkey | Case-control | 103 | 87 | 63 | 45 | 55 | 21 | 50 | 14 | Paroxysmal | 8 |
| Choudhury (disease control) [48] | 2008 | UK | case-control | 121 | 71 | 62.58 | 64.04 | 76 | 72 | 37.2 | 47.4 | ND | 6 |
| Choudhury (healthy control) [48] | 2008 | UK | case-control | 121 | 56 | 62.58 | 62.03 | 76 | 68 | 37.2 | 0 | ND | 6 |
| Pirat [49] | 2007 | Turkey | Case-control | 18 | 21 | 53 | 46 | 55 | 48 | ND | ND | ND | 7 |
| Yip [50] | 2006 | Taiwan | Case-control | 62 | 20 | 66.2 | 65.3 | 66.1 | 60 | 58.1 | 0 | ND | 9 |
| Kamath (Paroxysmal and persistent AF) [51] | 2003 | UK | Case-control | 31 | 31 | 61 | 66 | 61.3 | 41.9 | 0 | 0 | Combined types | 6 |
| Kamath (Permanent AF) [51] | 2003 | UK | Case-control | 93 | 31 | 66 | 66 | 63.4 | 41.9 | 0 | 0 | Permanent | 6 |
| Kamath (Paroxysmal AF) [52] | 2002 | UK | Case-control | 29 | 29 | 61 | 65 | 55.17 | 41.37 | 37.9 | 0 | Paroxysmal | 7 |
| Kamath (Permanent AF) [52] | 2002 | UK | Case-control | 87 | 29 | 65 | 65 | 63.21 | 41.37 | 37.9 | 0 | Permanent | 7 |
| Kamath [53] | 2002 | UK | Case-control | 93 | 50 | 70 | 70 | 62.36 | 46 | 0 | 0 | ND | 6 |
| Kamath [54] | 2002 | UK | Case-control | 34 | 23 | 73 | ND | 50 | ND | 0 | 0 | ND | 6 |
| Peverill [55] | 2001 | Australia | Case-control | 79 | 84 | 63 | 47 | 83.5 | 85.7 | ND | ND | ND | 8 |
| Kahn (without stroke) [56] | 1997 | Canada | Case-control | 50 | 31 | ND | 65 | ND | 38.7 | 0 | 0 | ND | 7 |
| Kahn (with stroke) [56] | 1997 | Canada | Case-control | 25 | 11 | ND | 65 | ND | 63.6 | 0 | 0 | ND | 7 |
| Lip [57] | 1996 | UK | Case-control | 51 | 26 | 70.4 | ND | ND | ND | 0 | 0 | ND | 6 |
| Gustafsson (without stroke) [58] | 1990 | Sweden | Case-control | 20 | 20 | 77 | 77 | ND | ND | 0 | 0 | ND | 8 |
| Gustafsson (with stroke) [58] | 1990 | Sweden | Case-control | 20 | 20 | 77 | 77 | ND | ND | 0 | 0 | ND | 8 |
| Recurrence of AF | |||||||||||||
| Gurses [9] | 2016 | Turkey | Case-control | 12 | 74 | 57.5 | 56.1 | 66.7 | 48.7 | ND | ND | Combined types | 9 |
| Hongliang Li [59] | 2016 | China | Case-control | 35 | 69 | 62 | 63 | 40 | 47.8 | 51.4 | 52.2 | Paroxysmal | 7 |
| Yanagisawa (without heart failure) [60] | 2016 | Japan | Cohort | 269 | 409 | 61.1 | 61.1 | 77 | 75 | ND | ND | Combined types | 7 |
| Yanagisawa (with heart failure) [60] | 2016 | Japan | Cohort | 42 | 37 | 64.2 | 63 | 62 | 87 | ND | ND | Combined types | 7 |
| Aksu [61] | 2015 | Turkey | Cohort | 7 | 42 | 65.01 | 54.29 | 57 | 48 | ND | ND | Paroxysmal | 9 |
| Gurses [62] | 2015 | Turkey | Cohort | 70 | 229 | 56.3 | 55.1 | 58.6 | 43.7 | 48.57 | 34.11 | Combined types | 9 |
| Karavelioglu [63] | 2015 | Turkey | Cohort | 87 | 131 | 65.8 | 63 | 35.63 | 46.56 | ND | ND | Paroxysmal | 7 |
| Wen [64] | 2015 | China | Cohort | 15 | 60 | 63.67 | 63.57 | ND | ND | ND | ND | Combined types | 9 |
| Guo Xueyuan [65] | 2014 | China | Cohort | 124 | 255 | 49.6 | 49.73 | 72.9 | 74.2 | ND | ND | ND | 9 |
| Aribas [66] | 2013 | Turkey | Cohort | 46 | 103 | 61 | 59 | ND | ND | 100 | 100 | Persistent | 9 |
| Bing Li [67] | 2013 | China | Cohort | 80 | 208 | 56 | 58 | 72.5 | 69.7 | ND | ND | Paroxysmal | 9 |
| Canpolat [68] | 2013 | Turkey | Cohort | 60 | 191 | 57.3 | 53.1 | 60 | 49.7 | ND | ND | ND | 8 |
| Im [69] | 2013 | South Korea | Cohort | 107 | 392 | 56.5 | 56.3 | 73.8 | 73.5 | ND | ND | Combined types | 9 |
| Xiao-nan HE [70] | 2013 | China | Cohort | 106 | 224 | 60 | 59 | 62.4 | 70.2 | ND | ND | Paroxysmal | 6 |
| Ferro [71] | 2012 | Italy | Cohort | 50 | 94 | 70.3 | 71.6 | 52 | 61 | 100 | 100 | Persistent | 8 |
| Smit [72] | 2012 | Netherland | Cohort | 30 | 70 | 63 | 65 | 73.3 | 74.3 | ND | ND | Persistent | 7 |
| Wang (Paroxysmal AF) [73] | 2012 | China | Cohort | 41 | 62 | 58 | 57 | 32.5 | 37.1 | ND | ND | Paroxysmal | 7 |
| Wang (Persistent AF) [73] | 2012 | China | Cohort | 30 | 25 | 53 | 52 | 73.3 | 76 | ND | ND | Persistent | 7 |
| Liu (Paroxysmal AF) [74] | 2011 | China | Cohort | 19 | 58 | 55 | 57 | 84.2 | 67 | 100 | 100 | Paroxysmal | 8 |
| Liu (Persistent AF) [74] | 2011 | China | Cohort | 17 | 27 | 55.2 | 50.9 | 88.2 | 81.5 | 100 | 100 | Persistent | 8 |
| Vizzardi [75] | 2009 | Italy | Cohort | 46 | 60 | 69 | 69 | 59 | 63 | ND | ND | Persistent | 7 |
| Letsas [76] | 2009 | Germany | Cohort | 28 | 44 | 53.3 | 55.8 | 86 | 77 | ND | ND | Combined types | 7 |
| Korantzopoulos [77] | 2005 | Greece | Cohort | 9 | 21 | 67 | 70 | 44.4 | 52.38 | ND | ND | Persistent | 8 |
Table 2.
Information about markers and these levels in each study
| First author | Markers | Levels |
|---|---|---|
| Occurrence of AF | ||
| Balci (Male subjects) [8] | MPV | MPV [AF: 9.3±0.4 vs. SR: 8.65±0.3] |
| Balci (Female subjects) [8] | MPV | MPV [AF: 8.9±0.3 vs. SR: 9±0.2] |
| Gurses [9] | WBC | WBC [AF: 7.6±3.3 vs. SR: 7.1±0.9] |
| Karatas [10] | PC, MPV, WBC, NLR, RDW, Hb | PC [AF: 230±69.3 vs. SR: 240±77.5] MPV [AF: 9.5±1.7 vs. SR: 8.7±1] WBC [AF: 12.8±5.6 vs. SR: 11.9±4.4] NLR [AF: 6.3±6.3 vs. SR: 5.1±4.7] RDW [AF: 13.9±1.7 vs. SR: 13.4±1.4] Hb [AF: 13.8±1.7 vs. SR: 13.9±1.6] |
| Korantzopoulos [11] | WBC, RDW, Hb | WBC [AF: 6.46±0.35 vs. SR: 7.21±0.8] RDW [AF: 14.6±0.45 vs. SR: 13.77±0.22] Hb [AF: 13.05±0.50 vs. SR: 13.35±0.60] |
| Akdag [12] | PC, MPV, WBC, NLR, Hb | PC [AF: 265.6±73.4 vs. SR: 248.2±67.2] MPV [AF: 8.9±1.1 vs. SR: 7.8±1] WBC [AF: 7.3±1.9 vs. SR: 6.9 ±1.8] NLR [AF: 3.6±1.5 vs. SR: 2.9±1.3] Hb [AF: 14.3±1.1 vs. SR: 14.5±1] |
| Akyuz [13] | PC, MPV, Hb | PC [AF: 277±79 vs. SR: 264±82] MPV [AF: 9.8±0.6 vs. SR: 8.4±0.6] Hb [AF: 12.7±1.3 vs. SR: 13.1±1.4] |
| Chavaria [14] | PC, WBC, NLR, Hb | PC [AF: 242.2±54.1 vs. SR: 243.2±66.2] WBC [AF: 12.4±3.9 vs. SR: 11±3.59] NLR [AF: 3.55±3.15 vs. SR: 4.19±3.55] Hb [AF: 14±1.7 vs. SR: 14.3±1.7] |
| Drabik (Persistent AF) [15] | PC, WBC | PC [AF: 202±20.5 vs. SR: 219±16.5] WBC [AF: 7.3±0.6 vs. SR: 6.45±0.7] |
| Drabik (Paroxysmal AF) [15] | PC, WBC | PC [AF: 210.25±15.75 vs. SR: 219±16.5] WBC [AF: 6.07±0.42 vs. SR: 6.45±0.7] |
| Acet (Paroxysmal AF) [16] | PC, WBC, NLR, Hb | PC [AF: 248.9±59 vs. SR: 259.8±95.9] WBC [AF: 11.5±2.5 vs. SR: 9.8±2] NLR [AF: 2.5 ±0.6 vs. SR: 1.8±0.4] Hb [AF: 13.8±1.7 vs. SR: 13.3±1.6] |
| Acet (Persistent and permanent AF) [16] | PC, WBC, NLR, Hb | PC [AF: 268.6±98 vs. SR: 259.8±95.9] WBC [AF: 10.9±2 vs. SR: 9.8±2] NLR [AF: 3.4±0.6 vs. SR: 1.8±0.4] Hb [AF: 13.9±1.7 vs. SR: 13.3±1.6] |
| Arik (effective INR) [17] | PC, MPV, PDW, WBC, Hb | PC [AF: 258.25±53.83 vs. SR: 255.75±41.5] MPV [AF: 7.56±0.63 vs. SR: 7.63±0.68] PDW [AF: 17.05±0.86 vs. SR: 17.52±0.71] WBC [AF: 7.47±1.23 vs. SR: 7.38±1.11] Hb [AF: 12.95±0.96 vs. SR: 13.47±0.75] |
| Arik (ineffective INR) [17] | PC, MPV, PDW, WBC, Hb | PC [AF: 238.75±41.16 vs. SR: 255.75±41.5] MPV [AF: 8.26±0.63 vs. SR: 7.63±0.68] PDW [AF: 17.50±1.13 vs. SR: 17.52±0.71] WBC [AF: 7.49±1.21 vs. SR: 7.38±1.11] Hb [AF: 12.95±0.81 vs. SR: 13.47±0.75] |
| Distelmaier [18] | PC, WBC, RBC, RDW, MCV, MCHC, HCT, Hb | PC [AF: 202±14.75 vs. SR: 215±14.16] WBC [AF: 9.96±1.42 vs. SR: 9.18±0.88] RBC [AF: 4.57±0.22 vs. SR: 4.23±0.12] RDW [AF: 13.9±0.3 vs. SR: 13.62±0.25] MCV [AF: 90.5±1.67 vs. SR: 90.78±0.82] MCHC [AF: 33.87±0.35 vs. SR: 33.47±0.28] HCT [AF: 41.07±1.92 vs. SR: 38.4±1.13] Hb [AF: 13.95±0.65 vs. SR: 12.85±0.35] |
| Erdogan (with normal ventricular rate) [19] | PC, MPV, WBC, HCT, Hb | PC [AF: 245.6±114.9 vs. SR: 238.4±66.6] MPV [AF: 7.82±1.2 vs. SR: 7.68±0.70] WBC [AF: 7.52±2.06 vs. SR: 7.55±1.89] HCT [AF: 39.7±5.2 vs. SR: 40.3±3.4] Hb [AF: 14±1.9 vs. SR: 13.9±1.3] |
| Erdogan (with high ventricular rate) [19] | PC, MPV, WBC, HCT, Hb | PC [AF: 225.5±76.3 vs. SR: 238.4±66.6] MPV [AF: 8.05±0.6 vs. SR: 7.68±0.70] WBC [AF: 7.47±1.47 vs. SR: 7.55±1.89] HCT [AF: 40.7±3.8 vs. SR: 40.3±3.4] Hb [AF: 14.3±1.3 vs. SR: 13.9±1.3] |
| Zheng [20] | WBC | WBC [AF: 5.6±1.14 vs. SR: 5.46±1.21] |
| Xu (without thrombotic events) [21] | PC, MPV, Hb | PC [AF: 205±31 vs. SR: 209±41] MPV [AF: 10.6±1.9 vs. SR: 8.7±0.8] Hb [AF: 14.5±1.4 vs. SR: 14.6±1.1] |
| Xu (with thrombotic events) [21] | PC, MPV, Hb | PC [AF: 206±42 vs. SR: 209±41] MPV [AF: 11.7±2 vs. SR: 8.7±0.8] Hb [AF: 14.6±1.3 vs. SR: 14.6±1.1] |
| Gungor [22] | PC, MPV, WBC, NLR, RDW, MCV, Hb | PC [AF: 249.4±59.4 vs. SR: 253.4±61.1] MPV [AF: 8.99±0.65 vs. 9.14±0.98] WBC [AF: 7.21±1.62 vs. SR: 6.81±1.17] NLR [AF: 2.04±0.94 vs. SR: 1.93±0.64] RDW [AF: 13.45±0.2 vs. SR: 12.57±0.27] MCV [AF: 90.2±5.4 vs. SR: 89.2±3.6] Hb [AF: 14.5±1.4 vs. SR: 14.2±1.2] |
| Liu [23] | RDW | RDW [AF: 12.71±0.9 vs. SR: 12.45±0.62] |
| Sarikaya [24] | RDW, Hb | RDW [AF: 15.13±1.58 vs. 14.05±1.15] Hb [AF: 13.74±1.38 vs. SR: 13.88±1.62] |
| Sonmez [25] | PC, NLR, Hb | PC [AF: 231±60 vs. 247±67] NLR [AF: 2.7±1.1 vs. SR: 2.1±1] Hb [AF: 13.3±1.6 vs. SR: 13.1±1.8] |
| Ulu [26] | PC, PDW, MPV | PC [AF: 236.44±63.92 vs. SR: 233.32±86.24] PDW [AF: 12.64±1.43 vs. SR: 11.76±1.41] MPV [AF: 11.47±0.93 vs. SR: 10.37±1.07] |
| Berge [27] | PC, Hb | PC [AF: 230±7.5 vs. SR: 261.25±4.16] Hb [AF: 14.6±0.2 vs. SR: 14.7±0.06] |
| Ertas (without stroke) [28] | PC, WBC, NLR, RDW, Hb | PC [AF: 232±55 vs. SR: 258±54] WBC [AF: 7.8±1.8 vs. SR: 7±1.4] NLR [AF: 3.1±2.1 vs. SR: 2.05±0.9] RDW [AF: 14.3±1.8 vs. SR: 13.2±0.9] Hb [AF: 13±1.4 vs. SR: 14±1.7] |
| Ertas (with stroke) [28] | PC, WBC, NLR, RDW, Hb | PC [AF: 240±82 vs. SR: 258±54] WBC [AF: 8.6±2.8 vs. SR: 7±1.4] NLR [AF: 5.6±3.4 vs. SR: 2.05±0.9] RDW [AF: 14.1±1.7 vs. SR: 13.2±0.9] Hb [AF: 13±1.6 vs. SR: 14±1.7] |
| Gungor [29] | WBC, Hb | WBC [AF: 6.5±1.5 vs. SR: 6.2±1.1] Hb [AF: 14.7±1.5 vs. SR: 14.9±1.3] |
| Turgut [30] | PC, MPV | PC [AF: 274±82 vs. SR: 253±83] MPV [AF: 9±0.2 vs. SR: 8.4±0.2] |
| Jaremo (healthy control) [31] | PC | PC [AF: 241±64 vs. 260±78] |
| Jaremo (disease control) [31] | PC | PC [AF: 241±64 vs. 265±84] |
| Sahin [32] | MPV, WBC, NLR | MPV [AF: 8.31±1.12 vs. SR: 7.99±1.39] WBC [AF: 7.86±2.04 vs. 7.67±2.03] NLR [AF: 2.87±1.3 vs. 2.2±1.56] |
| Tekin [33] | PC, MPV, WBC, HCT | PC [AF: 242±90 vs. 243±67] MPV [AF: 9.49±1.08 vs. 9.09±1.13] WBC [AF: 7.48±2.15 vs. 6.94±1.68] HCT [AF: 40.22±4.8 vs. 41.45±4.79] |
| Turfan (without stroke) [34] | PC, MPV, Hb | PC [AF: 264±94 vs. 213±72] MPV [AF: 9.1±1 vs. 8.6±1.3] Hb [AF: 12.8±1.1 vs. 12.7±1.2] |
| Turfan (with stroke) [34] | PC, MPV, Hb | PC [AF: 245±73 vs. 213±72] MPV [AF: 9.7±0.9 vs. 8.6±1.3] Hb [AF: 13±1.4 vs. 12.7±1.2] |
| Feng [35] | PC, MPV, WBC, RBC, MCV | PC [AF: 213.3±82.5 vs. SR: 217.6±81.9] MPV [AF: 9.95±1.32 vs. SR: 9.02±1.16] WBC [AF: 6.91±3.24 vs. SR: 6.88±3.35] RBC [AF: 4.47±0.68 vs. 4.56±0.71] MCV [AF: 93.8±5.2 vs. 94.1±5.3] |
| Liu (Paroxysmal AF) [36] | WBC | WBC [AF: 6.76±1.85 vs. SR: 6.34±1.89] |
| Liu (Persistent AF) [36] | WBC | WBC [AF: 6.37±1.66 vs. SR: 6.34±1.89] |
| Yoshizaki [37] | WBC | WBC [AF: 11.1±5.2 vs. SR: 10.6±4] |
| Hayashi (Paroxysmal AF) [38] | PC, WBC | PC [AF: 260±83 vs. SR: 190±77] WBC [AF: 5.8±4.2 vs. SR: 5.3±3] |
| Hayashi (Chronic AF) [38] | PC, WBC | PC [AF: 200±14 vs. SR: 190±77] WBC [AF: 5.6±3.8 vs. SR: 5.3±3] |
| Fu [39] | PC | PC [AF: 210±55.5 vs. SR: 221.1±51.1] |
| Liu [40] | WBC | WBC [AF: 6.5±1.9 vs. SR: 7.2±2.2] |
| Letsas (Paroxysmal AF) [41] | WBC | WBC [AF: 7.7±2.19 vs. SR: 7.15±1.87] |
| Letsas (Permanent AF) [41] | WBC | WBC [AF: 6.97±1.9 vs. SR: 7.15±1.87] |
| Luan (Persistent AF) [42] | WBC | WBC [AF: 6.13±1.66 vs. SR: 6.13±1.95] |
| Luan (Paroxysmal AF) [42] | WBC | WBC [AF: 6.9±1.28 vs. SR: 6.13±1.95] |
| Alberti [43] | PC, WBC | PC [AF: 185.6±10 vs. SR: 243.3±9.4] WBC [AF: 5.6±0.3 vs. SR: 6.3±0.3] |
| Dai [44] | WBC | WBC [AF: 7.32±1.89 vs. SR: 6.57±1.91] |
| Ichiki [45] | WBC | WBC [AF: 4.6±0.3 vs. SR: 5.3±0.5] |
| Yao (Persistent AF) [46] | WBC | WBC [AF: 5.76±0.28 vs. SR: 5.69±0.35] |
| Yao (Paroxysmal AF) [46] | WBC | WBC [AF: 5.69±0.31 vs. SR: 5.69±0.35] |
| Colkesen [47] | PC, MPV, WBC | PC [AF: 242±13 vs. SR: 236±53] MPV [AF: 10±2 vs. SR: 8.3±1.50] WBC [AF: 7.58±2.35 vs. SR: 7.47±2.08] |
| Choudhury (disease control) [48] | PC, MPV, WBC, HCT, Hb | PC [AF: 259.9±66.3 vs. SR: 261.1±63.4] MPV [AF: 7.6±1.4 vs. SR: 7.8±1.9] WBC [AF: 7.1±1.8 vs. SR: 7.1±2.2] HCT [AF: 42.3±4.3 vs. SR: 41.6±3.9] Hb [AF: 14.6±1.6 vs. SR: 13.9±1.5] |
| Choudhury (healthy control) [48] | PC, MPV, WBC, HCT, Hb | PC [AF: 259.9±66.3 vs. SR: 266.9±56.1] MPV [AF: 7.6±1.4 vs. SR: 7.4±0.97] WBC [AF: 7.1±1.8 vs. SR: 6.4±1.8] HCT [AF: 42.3±4.3 vs. SR: 40.6±33.7] Hb [AF: 14.6±1.6 vs. SR: 14.1±1.2] |
| Pirat [49] | WBC | WBC [AF: 7.45±1.59 vs. SR: 6.7±0.98] |
| Yip [50] | PC, WBC | PC [AF: 204±57 vs. SR: 209±49] WBC [AF: 6.7±1.5 vs. SR: 6.6±1.7] |
| Kamath (Paroxysmal and persistent AF) [51] | PC, HCT | PC [AF: 280±81 vs. SR: 253±51] HCT [AF: 45±4 vs. SR: 42±3] |
| Kamath (Permanent AF) [51] | PC, HCT | PC [AF: 264±75 vs. SR: 253±51] HCT [AF: 43±5 vs. SR: 42±3] |
| Kamath (Paroxysmal AF) [52] | PC, HCT | PC [AF: 279±73 vs. SR: 252±53] HCT [AF: 43±5 vs. SR: 42±3] |
| Kamath (Permanent AF) [52] | PC, HCT | PC [AF: 266±76 vs. SR: 252±53] HCT [AF: 43±5 vs. SR: 42±3] |
| Kamath [53] | PC | PC [AF: 253±77 vs. SR: 261±62] |
| Kamath [54] | PC | PC [AF: 253±67 vs. SR: 270±49] |
| Peverill [55] | PC, MPV, MCV, HCT | PC [AF: 218±55 vs. SR: 241±59] MPV [AF: 9.7±1.4 vs. SR: 9.9±1.4] MCV [AF: 89±6 vs. SR: 88±7] HCT [AF: 42±5 vs. SR: 39±4] |
| Kahn (without stroke) [56] | PC, Hb | PC [AF: 230±98 vs. SR: 233±49] Hb [AF: 14.9±1.3 vs. SR: 13.4±1.5] |
| Kahn (with stroke) [56] | PC, Hb | PC [AF: 253±82 vs. SR: 242±77] Hb [AF: 14.1±1.2 vs. SR: 14.3±1.7] |
| Lip [57] | PC | PC [AF: 242±67 vs. SR: 224±63] |
| Gustafsson (without stroke) [58] | PC | PC [AF: 172.25±8.75 vs. SR: 234.75±10.75] |
| Gustafsson (with stroke) [58] | PC | PC [AF: 179±18.5 vs. SR: 234.75±10.75] |
| Recurrence of AF | ||
| Gurses [9] | WBC | WBC [AF: 7.5±3.9 vs. SR: 7.6±3.2] |
| Hongliang Li [59] | PC, WBC, RDW, Hb | PC [AF: 219.77±44.15 vs. SR: 199.32±52.58] WBC [AF: 6.51±1.84 vs. SR: 7.41±14.65] RDW [AF: 12.81±0.94 vs. SR: 12.37±0.56] Hb [AF: 14.11±1.85 vs. SR: 13.94±1.21] |
| Yanagisawa (without heart failure) [60] | WBC, RDW, MCV, Hb | WBC [AF: 5.5±1.4 vs. SR: 5.3±1.6] RDW [AF: 13.3±0.8 vs. SR: 13.2±0.8] MCV [AF: 92.3±4.4 vs. SR: 92±4.2] Hb [AF: 14±1.5 vs. SR: 14±1.5] |
| Yanagisawa (with heart failure) [60] | WBC, RDW, MCV, Hb | WBC [AF: 5.7±1.5 vs. SR: 6.1±1.6] RDW [AF: 14.5±2 vs. SR: 13.5±0.9] MCV [AF: 91.3±6.4 vs. SR: 92.3±4.6] Hb [AF: 13.3±2.3 vs. SR: 14.1±1.8] |
| Aksu [61] | MPV [AF: 8.81±1.4 vs. SR: 8.7±1.88] WBC [AF: 6.97±1.6 vs. SR: 7.38±1.7] NLR [AF: 2.5±0.78 vs. SR: 1.83±0.63] RDW [AF: 16.1±1.44 vs. SR: 14.87±0.48] WBC [AF: 13.3±1.34 vs. SR: 13.72±1.17] |
|
| Gurses [62] | PC, WBC, RDW, Hb | PC [AF: 221.8±56.3 vs. SR: 228.4±68.8] WBC [AF: 7.82±2.43 vs. SR: 7.44±1.89] RDW [AF: 14.3±0.93 vs. SR: 13.52±0.93] Hb [AF: 14.19±1.85 vs. SR: 13.92±1.76] |
| Karavelioglu [63] | PC, WBC, NLR, HCT, Hb | PC [AF: 234±65.1 vs. SR: 258.1±93.4] WBC [AF: 7.6±2.64 vs. SR: 7.93±2.42] NLR [AF: 2.8±1.59 vs. SR: 2.13±1.04] HCT [AF: 40.1±5.1 vs. SR: 41.1±5.2] Hb [AF: 13.6±2.9 vs. SR: 13.8±2.9] |
| Wen [64] | PC, WBC, NLR, Hb | PC [AF: 196±59 vs. SR: 198±44] WBC [AF: 6.36±1.56 vs. SR: 5.63±1.2] NLR [AF: 2.16±1.23 vs. SR: 1.94±0.94] Hb [AF: 12.6±1.8 vs. SR: 13.1±1.7] |
| Guo Xueyuan [65] | WBC, NLR, Hb | WBC [AF: 8.17±1.7 vs. SR: 7.84±1.6] NLR [AF: 1.9±1.19 vs. SR: 1.81±0.1] Hb [AF: 14.84±1.57 vs. SR: 14.52±1.82] |
| Aribas [66] | WBC, NLR | WBC [AF: 7.4±2 vs. SR: 7.6±2] NLR [AF: 2.38±2.09 vs. SR: 2.23±1.23] |
| Bing Li [67] | WBC | WBC [AF: 6.7±2.2 vs. SR: 6.1±2] |
| Canpolat [68] | WBC, NLR, Hb | WBC [AF: 8.94±2.08 vs. SR: 7.46±2.34] NLR [AF: 3.53±0.95 vs. SR: 2.65±0.23] Hb [AF: 13.5±1.8 vs. SR: 13.6±1.9] |
| Im [69] | NLR | NLR [AF: 1.9±1.2 vs. SR: 2±2.14] |
| Xiao-nan HE [70] | WBC | WBC [AF: 6.2±1.8 vs. SR: 6.5±1.9] |
| Ferro [71] | WBC | WBC [AF: 7.44±1.45 vs. SR: 7.47±1.71] |
| Smit [72] | WBC | WBC [AF: 7.7±1.5 vs. SR: 7.6±2] |
| Wang (Paroxysmal AF) [73] | WBC | WBC [AF: 6.1±1.4 vs. SR: 6.1±1.4] |
| Wang (Persistent AF) [73] | WBC | WBC [AF: 6.2±1.9 vs. SR: 6.6±1.5] |
| Liu (Paroxysmal AF) [74] | WBC | WBC [AF: 6.2±2.9 vs. SR: 5.9±1.4] |
| Liu (Persistent AF) [74] | WBC | WBC [AF: 5.6±1.4 vs. SR: 6±2.4] |
| Vizzardi [75] | WBC | WBC [AF: 6.9±1.4 vs. SR: 7±5.4] |
| Letsas [76] | WBC | WBC [AF: 6.86±1.21 vs. SR: 5.79±1.39] |
| Korantzopoulos [77] | WBC | WBC [AF: 7.29±1.84 vs. SR: 6.64±1.39] |
Figure 1.
Forest plot of weighted mean difference (WMD) for association between platelet count and occurrence of AF.
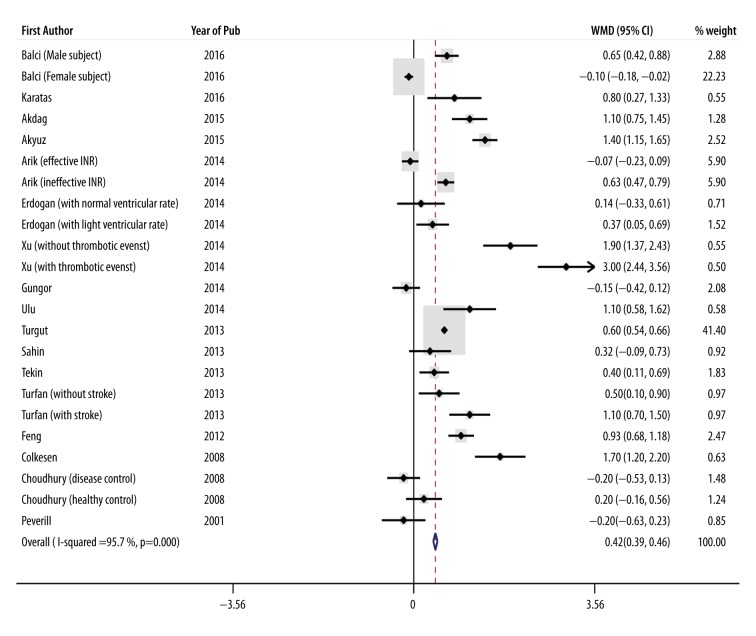
MPV
A total of 4014 cases were included from 23 studies, of which 1838 were allocated to the AF group and 2176 to the SR group. The mean level of MPV was 9.18 FL in the AF group and 8.48 FL in the SR group (details in Tables 1 and 2). Pooled analysis revealed that MPV level was significantly higher in patients with AF compared to those with SR, with a WMD of 0.42 FL (95% CI: 0.39 to 0.46; p<0.001, Figure 2) using a random-effects model. There was significant heterogeneity among the studies (I2=95.7%; heterogeneity p<0.001).
Figure 2.
Forest plot of weighted mean difference (WMD) for association between level of mean platelet volume and occurrence of AF.
PDW
A total of 553 cases were included from 3 studies, of which 275 and 278 were allocated to the AF group and the SR group, respectively. The mean level of PDW was 15.73% in the AF group and 15.60% in the SR group (details in Tables 1 and 2). Using a random-effects model, pooled analysis indicated that PDW was statistically lower in the AF group than in the SR group, with a WMD of −0.24% (95% CI: −0.39 to −0.09; p=0.001). There was significant heterogeneity among the studies (I2=88.5%; heterogeneity p<0.001)
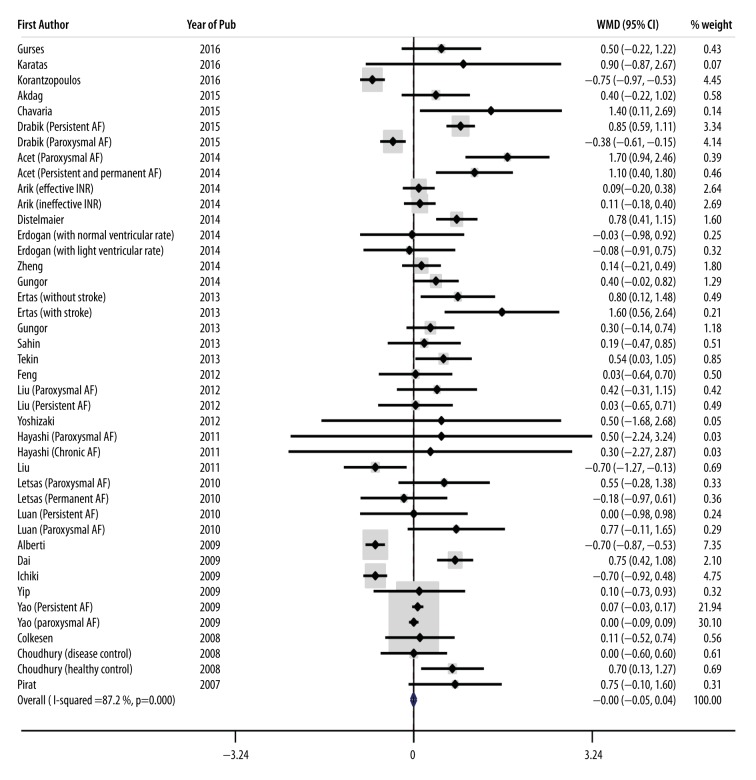
WBC
A total of 7042 patients were included from 42 studies, of which 3105 were allocated to the AF group and 3937 to the SR group. The mean WBC count was 7.49×109/L in patients with AF and 7.16×109/L in those with SR (details in Tables 1 and 2). Pooled analysis indicated that the mean count of WBC was similar in AF patients and those with SR, with a WMD of −0.005×109/L (95% CI: −0.052 to 0.042; p=0.83, Figure 3), with considerable heterogeneity among the studies (I2=87.2%; heterogeneity p<0.001).
Figure 3.
Forest plot of weighted mean difference (WMD) for association between white blood cell count and occurrence of AF.
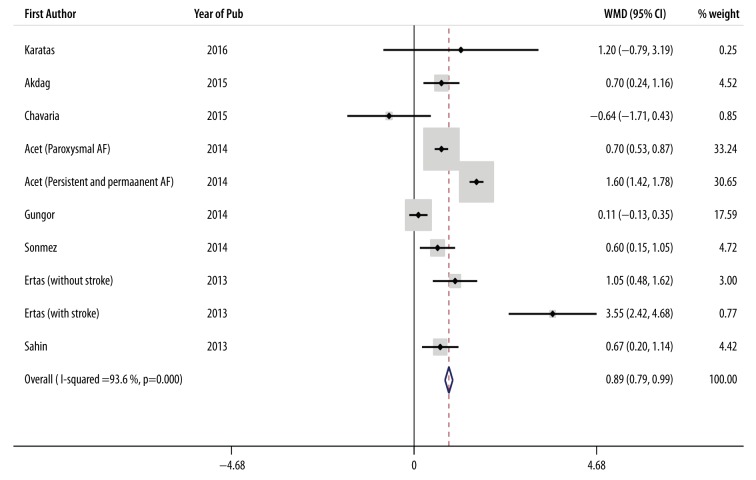
NLR
A total of 1899 cases were selected from 10 studies, of which 677 were allocated to the AF group and 1222 to the SR group. The mean NLR was 3.56 in the AF group and 2.61 in the SR group (details in Tables 1 and 2). Pooled analysis showed that the NLR was remarkably higher in patients with AF compared to controls, with a WMD of 0.89 (95% CI: 0.79 to 0.99; p<0.001, Figure 4) using a random-effects model. There was significant heterogeneity among the studies (I2=93.6%; heterogeneity p<0.001).
Figure 4.
Forest plot of weighted mean difference (WMD) for association between neutrophil to lymphocyte ratio and occurrence of AF.
RBC count
A total of 572 cases were included from 2 studies, of which 251 were allocated to the AF group and 321 to the SR group. The mean RBC count was 4.52×1012/L in the AF group and 4.39×1012/L in the SR group (details in Tables 1 and 2). Using a random-effects model, pooled analysis showed that the mean count of RBC was statistically higher in the AF group compared to the SR group, with a WMD of 0.28×1012/L (95% CI: 0.23 to 0.33; p<0.001). Significant heterogeneity was observed among the studies (I2=96.8%; heterogeneity p<0.001).
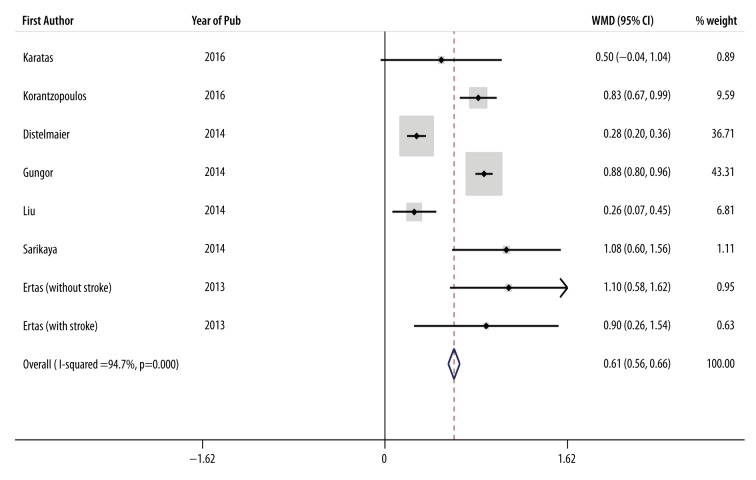
RDW
A total of 1631 cases were included from 8 studies, of which 577 were allocated to the AF group and 1054 to the SR group. The mean of RDW was 14.01% in the AF group and 13.28% in the SR group (details in Tables 1 and 2). Using a random-effects model, pooled analysis revealed that RDW was significantly higher in the AF group than in the SR group, with a WMD of 0.61% (95% CI: 0.56 to 0.66; p<0.001, Figure 5). There was significant heterogeneity among the studies (I2=94.7%; heterogeneity p<0.001)
Figure 5.
Forest plot of weighted mean difference (WMD) for association between red blood cell distribution width and occurrence of AF.
Secondary hematological parameters
MCHC was reported in 1 study, which was not included in the meta-analysis. According to pooled assessment analysis, the level of MCV (number of studies=4, WMD of −0.14 FL, 95% CI: −0.51 to 0.23; p=0.46 and I2=34%; heterogeneity p=0.2) and Hb (number of studies=27, WMD of 0.04 g/dL, 95% CI: −0.02 to 0.10; p=0.23 and I2=91.1%; heterogeneity p<0.001) were similar in both groups. Pooled analysis showed that HCT (number of studies=11, WMD of 1.79%, 95% CI: 1.43 to 2.15; p<0.001 and I2=80.6%%; heterogeneity p<0.001) was significantly higher in the AF group compared to the SR group.
Association of hematologic parameters with recurrent AF
Platelet count
A total of 696 cases were selected from 4 studies, of which 207 were allocated to recurrent AF group and 489 to the non-recurrent AF group (details in Tables 1 and 2). Pooled effects analysis showed that the mean platelet count did not differ between groups, with a WMD of −2.71×109/L (95% CI: −12.75 to 7.34; p=0.59). Significant heterogeneity was observed among the studies (I2=69.4%; heterogeneity p=0.02).
WBC
A total of 3716 patients were included from 22 studies, of which 1223 were allocated to the recurrent AF group and 2493 to the non-recurrent AF group (details in Tables 1 and 2). The mean WBC count was 6.89×109/L in patients with recurrent AF and 6.79×109/L in those with non-recurrent AF. Pooled analysis revealed that the mean count of WBC was statistically higher in the recurrent group compared to the non-recurrent group, with a WMD of 0.20×109/L (95% CI: 0.08 to 0.32; p=0.002, Figure 6), with considerable heterogeneity among the studies (I2=54.7%; heterogeneity p=0.001).
Figure 6.
Forest plot of weighted mean difference (WMD) for association between white blood cell count and recurrence of AF.
NLR
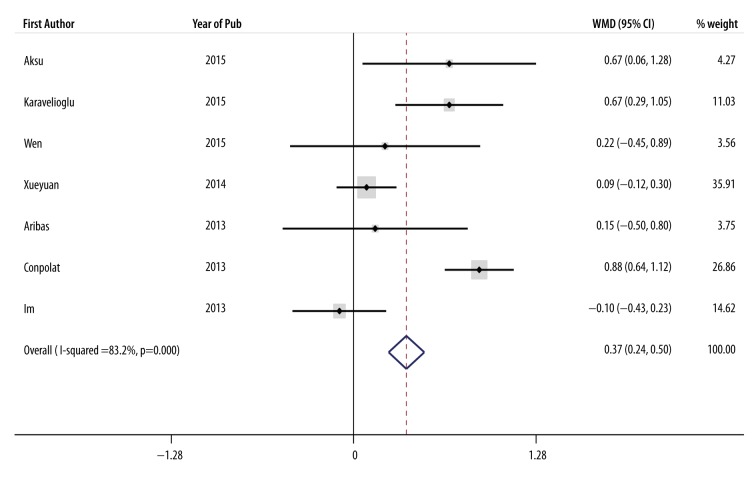
A total of 1620 cases were selected from 7 studies, of which 446 were allocated to the recurrent AF group and 1174 to the non-recurrent AF group (details in Tables 1 and 2). Pooled assessment analysis indicated that the NLR was significantly higher in patients suffering from recurrent AF compared to the non-recurrent group, with a WMD of 0.37 (95% CI: 0.24 to 0.50; p<0.001, Figure 7). There was significant heterogeneity among the studies (I2=83.2%; heterogeneity p<0.001).
Figure 7.
Forest plot of weighted mean difference (WMD) for association between neutrophil to lymphocyte ratio and recurrence of AF.
RDW
A total of 1209 cases were included from 5 studies, of which 423 were allocated to the recurrent AF group and 786 to the non-recurrent AF group (details in Tables 1 and 2). Using a random-effects model, pooled analysis revealed that RDW was considerably higher in the recurrent AF group than in the non-recurrent group, with a WMD of 0.28% (95% CI: 0.18 to 0.38; p<0.001, Figure 8). There was significant heterogeneity among the studies (I2=87.5%; heterogeneity p<0.001).
Figure 8.
Forest plot of weighted mean difference (WMD) for association between red blood cell distribution width and recurrence of AF.
Secondary hematological parameters
MCV and Hb were investigated in at least 2 studies, which were included in the meta-analysis. According to pooled assessment analysis, the levels of MCV (number of studies=2, WMD of 0.21, 95% CI: −0.43 to 0.85; p=0.52 and I2=1.6%; heterogeneity p=0.31) and Hb (number of studies=9, WMD of 0.04 g/dL, 95% CI: −0.12 to −0.19; p=0.64 and I2=13.6%; heterogeneity p=0.32) were similar in both groups.
Other parameters
There was an insufficient number of studies for analysis on association between MPV, RBC count, and HCT and recurrent AF.
Publication bias and subgroup analysis
Begg tests suggested that all of the analyses were without publication bias except for association between Hb and recurrent AF. Extra details of characteristics of each study for exploration of heterogeneity factors are presented in Supplementary Table 2. Details of subgroup analysis are reported in detail in Supplementary Table 3.
Discussion
AF is one of the most common cardiac arrhythmias in developing and developed countries, precipitating morbidities and mortalities [78,79]. Various mechanisms are involved in AF, such as inflammation, oxidative stress, and prothrombotic state [79,80]. Therefore, the complications of this arrhythmia and their negative effects on quality of life can be decreased by more accurate recognition of mechanisms, timely diagnosis, and appropriate treatment. Although taking patient history, considering the history of cardiac arrhythmia, clinical examinations, ECG, and Holter monitoring can assist in diagnosis and control of AF, some routine diagnostic actions which are performed daily in clinical practice might be of higher value than previously thought [81]. CBC is a routine lab test for most patients, particularly those with cardiovascular diseases hospitalized in cardiology and cardiac surgery wards, as well as CCUs or ICUs [81]. Hematological parameters in CBC tests can indicate hemodynamic status and are appropriate predictors for clinical outcomes of these patients [81]. Varastehravan et al. reported that hematological parameters had considerable ability in prognosis of ST-segment resolution in patients with ST-segment elevation myocardial infarction receiving streptokinase therapy [5].
In the present study, we investigated the association of hematological parameters with new-onset and recurrent AF in order to understand which hematological parameters could be reliable predictors of each type of AF. Although the majority of physicians and researchers have believed that platelet count in cases with new-onset AF is higher than in patients with SR, our findings revealed that the number of platelets was significantly lower in cases with new-onset AF compared to those with SR, resulting in the likelihood of lower platelet count to predict new-onset AF.
Our subgroup analysis showed an inverse relationship between platelet count and new-onset AF in cases of persistent AF, but this relationship was not found in cases of paroxysmal and permanent AF. On the other hand, there was no significant relationship between platelet count and new-onset AF in patients with chronic AF. According to our findings, sample size of the studies, age, diabetes mellitus, differences regarding treatment with anticoagulants, and type of AF are factors of heterogeneity. The present study found no remarkable relationship between platelet count and recurrent AF; therefore, platelet count could be a potential predictor for new-onset AF, but it does not appear to be a significant factor associated with recurrent AF. Regarding the results of this study, PDW was considerably lower in cases with new-onset AF compared to those with SR. Thus, PDW and platelet count both had an inverse relationship with the new-onset AF.
MPV is known as an important biomarker of platelet activity. Large platelets secrete many critical mediators of coagulation, inflammation, thrombosis, and atherosclerosis. Evidence shows a close relationship between MPV and cardiovascular risk factors, such as diabetes mellitus, hypertension, and hypercholesterolemia [82,83]. Interestingly, in a recent study, Sansanayudh et al. reported an association between MPV and coronary artery disease (CAD). Patients with CAD and slow coronary blood flow had larger MPV than in the control group. They concluded that MPV might be used for risk stratification or to raise diagnostic accuracy of the traditional risk stratification markers in CAD patients [84].
The results of our study showed that MPV was also considerably higher in cases with new-onset AF compared to those with SR. According to our subgroup analysis, there was also a direct relationship between MPV and new-onset AF in both chronic and non-chronic AF. Sample sizes of the studies, differences in treatment with anticoagulants, and type of AF appeared to be factors of heterogeneity. Owing to insufficient number of studies on the association between PDW and MPV with recurrent AF, no analysis was performed in this regard.
There is a known relationship between inflammation and development of AF. Activities in hematopoietic tissues producing inflammatory leukocytes are closely associated with systemic inflammation, arterial inflammation, and cardiovascular events; however, their association with AF is unclear [85].
The findings of this study demonstrated that WBC count was not significantly different between cases of new-onset AF compared to those of SR; therefore, WBC is not proposed as a reliable predictor. The present study also confirmed that WBC count was not associated with new-onset AF for chronic and non-chronic AF. Our subgroup analysis indicated that risk factors such as diabetes mellitus, hypertension, and cigarette smoking could be factors of heterogeneity. On the other hand, our results revealed that WBC count was statistically higher in cases of recurrent AF compared to those with non-recurrent AF. Consequently, it can be stated that WBC count might be considered a predictor for recurrent AF, but not for new-onset AF. It also implies that possible inflammatory mechanisms are more active in patients who develop recurrent AF despite anti-arrhythmic therapy for AF. As a result, considering inflammatory markers as a valuable tool to detect the risk of recurrent AF after pharmacological interventions and electrophysiology could greatly help in terms of timely diagnosis of AF recurrence.
The neutrophil to lymphocyte ratio is a new systemic inflammatory marker and a prognostic indicator of cardiovascular diseases [86,87]. The results of this study show that NLR is directly associated with new-onset and recurrent AF and generally could be an appropriate and efficient predictor for this disease. In our subgroup analysis, NLR also had this predictive ability for paroxysmal and persistent AF, while the association of NLR with permanent and chronic AF could not be detected due to the lack of relevant studies.
RDW is a parameter used to measure variability in the size of circulatory red blood cells obtained in CBC tests. Higher RDW reflects the presence of anisocytosis, which is associated with impaired erythropoiesis and RBC degradation appearing as chronic inflammation and a high level of oxidative stress [88].
Several studies suggested that RDW can predict poor outcomes in patients with heart failure, stable CAD, and acute myocardial infarction [89–91]. Similarly, our study showed that RDW was clearly higher in cases with new-onset AF compared to cases with SR. However, RDW was significantly increased in patients with recurrent AF versus non-recurrent AF, providing strong evidence that RDW can predicting both new-onset and recurrent AF. Only 2 studies investigated RBC count and its impact on AF, in which pooled analysis showed that RBC count was statistically higher in the AF group than in the SR group. No study was found investigating the relationship between this hematological parameter and recurrent AF.
Anemia increases the risk of cardiovascular complications, such as thromboembolic events, bleeding, and mortality in anticoagulated patients with AF. Patients with anemia and AF are supposed to be closely monitored while under treatment with all types of anticoagulants [92]. In the present study, Hb, HCT, MCV, and MCHC were examined as secondary hematological parameters. Pooled analysis found no significant differences in Hb levels comparing cases of new-onset AF with cases of SR. Notably, our subgroup analysis showed that the status of treatment with anticoagulants was not defined in a significant number of studies. Therefore, we had no information on whether patients enrolled in these studies had been receiving anticoagulant therapy. Concerning general findings, it appears that Hb is not a potential predictor for new-onset AF; however, this might change in the future by defining the therapeutic strategies with anticoagulants as well as the number of patients under treatment. On the other hand, there was an interesting finding about the type of AF. When the studies were sorted in terms of chronic and non-chronic AF, the level of Hb was considerably higher in non-chronic AF and significantly lower in chronic AF. This finding suggests that the type of AF in terms of acute or chronic pattern might have different effects on Hb changes. The merged results rejected any relationship between Hb and new-onset AF; however, based on our subgroup analysis, we believe that after categorizing the types of AF into chronic and non-chronic, Hb might be a predictor. The results also indicated that the level of Hb was similar in patients with recurrent AF and those with non-chronic AF. Performing subgroup analysis, we found that the lack of association of Hb changes with recurrent AF was not influenced by any factor. Therefore, we strongly corroborate the lack of association between this hematological parameter and recurrent AF.
MCV is a measure of the average red blood cell. Based on our results, the level of MCV did not significantly differ between cases of new-onset AF versus SR cases, thus MCV could not be suggested as a predictor for new-onset AF. Also, our subgroup analysis strongly supported this finding.
Only 2 studies investigated the association of MCV and recurrent AF, and the merged analysis showed that the level of MCV was not significantly related to new-onset AF. HCT is a test for measuring the volume of RBC in relation to the total volume of blood. In the present study, the percentage of HCT was notably higher in cases of new-onset AF versus SR cases. Our subgroup analysis revealed that HCT can predict new-onset AF in non-chronic AF, but this ability was not seen in chronic AF. Due to the insufficient number of studies, we were unable to evaluate the relationship between HCT and recurrent AF.
Lip et al. reported that anticoagulants can reduce the level of hemostatic and hematologic factors in AF patients and, consequently, differences in treatment strategies with anticoagulants in various studies could be considered as a factor of heterogeneity [93–95]. Our subgroup analysis of platelet count, RDW, MCV, HCT, and WBC indicated that differences in using anticoagulants could play a considerable role in the existence of heterogeneity.
It should also be noted that in the meta-analysis on non-experimental studies, more heterogeneity was found, which can be explained by the following: 1) less controlled biases; 2) more confounding factors; and 3) differences in defining outcomes. Millions of CBC tests are performed daily for a large number of hospitalized patients with cardiovascular diseases throughout the world. In the present study, we found that CBC tests, apart from their ability to show a number of various pathologies already well known in clinical practice, might also play a significant role in diagnosis of various types of cardiac arrhythmias. Therefore, in addition to taking patient history, ECG, and Holter monitoring, the information from CBC in terms of AF should also be taken into account as an important diagnostic parameter. Therefore, we should be aware that, despite being one the most routine laboratory tests, the usefulness of CBC should not be underestimated.
Conclusions
Indeed, according to the results of previous research on potential predictive role of various CBC tests on the occurrence of AF that were conglomerated in our meta-analysis, CBC tests are a relatively easy to use and inexpensive tool to provide additional information on potential AF. Although CBC testing cannot replace standard diagnostics, they may be a valuable method to get some additional information in clinical diagnostics. In general, considering the results of this study, we conclude that lower platelet count and PDW, as well as higher MPV, NLR, RBC, RDW, and HTC, could be associated with new-onset AF. We strongly emphasize that MPV, NLR, and RDW have better predictive value in clinical practice for AF. Patients with AF who are under treatment are at high risk of recurrent AF; as a result, CBC is of particular importance for these patients. Our results also indicated that WBC, NLR, and PDW are hematological parameters with significant ability to predict recurrent AF. Therefore, emphasizing the potential predictive role of hematological parameters for new-onset and recurrent AF, we strongly recommend adding CBC testing to the diagnostic modalities of AF in clinical practice.
Supplementary Tables
Supplementary Table 1.
Included, and excluded studies according to primary hematological parameters.
| Clinical outcomes and biomarkers | Studies were identified and screened [n] | Studies were excluded according to title, abstract or full text (Secondary exclude) [n] | Studies were included [n] | Data for occurrence and recurrence [n] |
|---|---|---|---|---|
| Platelet count | 292 | 254 | 38 approved articles with totally 52 enrolled data for meta-analysis (48 studies |
Occurrence: 48 Recurrence: 4 |
| Mean platelet volume | 147 | 129 | 18 approved articles with totally 24 enrolled data for meta-analysis |
Occurrence: 23 Recurrence: 1 |
| Platelet distribution width | 11 | 9 | 2 approved articles with totally 3 enrolled data for meta-analysis |
Occurrence: 3 Recurrence: 0 |
| White blood cell | 348 | 299 | 49 approved articles with totally 64 enrolled data for meta-analysis |
Occurrence: 42 Recurrence: 22 |
| Neutrophil to lymphocyte ratio | 41 | 26 | 15 approved articles with totally 17 enrolled data for meta-analysis |
Occurrence: 10 Recurrence: 7 |
| Red blood cell | 83 | 81 | 2 approved articles with totally 2 enrolled data for meta-analysis |
Occurrence: 2 Recurrence: 0 |
| Red blood cell distribution width | 49 | 38 | 11 approved articles with totally 13 enrolled data for meta-analysis |
Occurrence: 8 Recurrence: 5 |
Supplementary Table 2.
Extra details of characteristics of each study for exploration of heterogeneity factors.
| First Author | Geographic Area | Total N | Total age | Total male | Total DM | Total HTN | Total CS | Total Diuretic | Total ACEI | Total. Statin | Total BB | AC-code | Chronic or not |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Occurrence of AF | |||||||||||||
| Balci (Male subjects) [8] | European | 35 | ND | 100 | ND | ND | ND | ND | ND | ND | ND | 5 | ND |
| Balci (Female subjects) [8] | European | 153 | ND | 0 | ND | ND | ND | ND | ND | ND | ND | 5 | ND |
| Gurses [9] | European | 172 | 56.5 | 52.35 | 13.95 | 51.75 | ND | ND | ND | ND | ND | 5 | Non-chronic |
| Karatas [10] | European | 621 | 61.05 | 72.5 | 23 | 45.5 | 64 | ND | ND | 0 | ND | 2 | Non-chronic |
| Korantzopoulos [11] | European | 101 | 76.5 | 46.5 | 27.5 | 88.5 | ND | ND | ND | ND | ND | 3 | Non-chronic |
| Akdag [12] | European | 148 | 64.05 | 60 | 16.5 | 22 | 23.5 | ND | ND | ND | ND | 6 | Combined types |
| Akyuz [13] | European | 90 | 62.25 | 72.25 | 29 | 42.5 | 34.25 | 14.5 | 20.75 | 32.5 | 23 | 4 | Combined types |
| Chavaria [14] | North America | 290 | 65.65 | 74.5 | 29.05 | 65.65 | 55.05 | ND | ND | ND | ND | 5 | ND |
| Drabik (Persistent AF) [15] | European | 97 | 60.1 | 64.975 | 20 | 48.85 | 22.85 | ND | 52.25 | 53.15 | 60.6 | 4 | Non-chronic |
| Drabik (Paroxysmal AF) [15] | European | 91 | 60 | 55.15 | 16.4 | 46.05 | 20 | ND | 54.05 | 47.45 | 57.25 | 4 | Non-chronic |
| Acet (Paroxysmal AF) [16] | European | 134 | 62.05 | 44 | 16.5 | 18 | 21.5 | ND | ND | ND | ND | 5 | Non-chronic |
| Acet (Persistent and permanent AF) [16] | European | 126 | 62.85 | 43.5 | 21.5 | 24 | 28.5 | ND | ND | ND | ND | 5 | Combined types |
| Arik (effective INR) [17] | European | 248 | 69.65 | 40.7 | 6.05 | 68.95 | 13.7 | 27 | 59.25 | ND | 59.7 | 5 | chronic |
| Arik (ineffective INR) [17] | European | 248 | 69.45 | 37.9 | 6.85 | 65.35 | 12.1 | 24.2 | 55.65 | ND | 61.3 | 5 | chronic |
| Distelmaier [18] | North America | 198 | 73.5 | 61 | 24 | 60.5 | ND | ND | ND | ND | ND | 5 | Non-chronic |
| Erdogan (with normal ventricular rate) [19] | European | 67 | 69.55 | 49.28 | 10 | 65 | 6 | 17 | 53.5 | 10 | 43.3 | 3 | chronic |
| Erdogan (with high ventricular rate) [19] | European | 63 | 68.8 | 49.055 | 13.3 | 56.5 | 8 | 25 | 52 | 3.5 | 43.3 | 3 | chronic |
| Zheng [20] | Asian | 217 | 61.735 | 58.63 | 10.84 | 49.275 | 32.74 | ND | ND | ND | ND | 5 | ND |
| Xu (without thrombotic events) [21] | Asian | 115 | 66.095 | 50.45 | 37.4 | 53.1 | 38.25 | ND | 42.6 | 29.55 | 43.55 | 4 | chronic |
| Xu (with thrombotic events) [21] | Asian | 115 | 67.975 | 51.3 | 36.5 | 57.5 | 31.25 | ND | 40.8 | 26.05 | 40.95 | 4 | chronic |
| Gungor [22] | European | 177 | 47.2 | 57.8 | 3.35 | 14.75 | 23.15 | ND | ND | ND | 10.6 | 3 | ND |
| Liu [23] | Asian | 234 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 5 | Non-chronic |
| Sarikaya [24] | European | 126 | 71.03 | 50 | 38 | 100 | ND | ND | ND | ND | ND | 5 | ND |
| Sonmez [25] | European | 85 | 70 | 37 | 24.21 | 63.255 | ND | 14.16 | 47.17 | 15.41 | 35.6 | 4 | Non-chronic |
| Ulu [26] | European | 57 | ND | ND | 0 | 0 | ND | ND | ND | ND | ND | 5 | ND |
| Berge [27] | European | 189 | 75 | 71.025 | 8 | 48 | ND | 19 | 21 | 34.5 | 28 | 4 | Combined types |
| Ertas (without stroke) [28] | European | 111 | 53.5 | 51 | 8.5 | 32.5 | 2 | ND | 17 | ND | 30 | 3 | ND |
| Ertas (with stroke) [28] | European | 63 | 54.5 | 47 | 10 | 47 | 5 | ND | 24 | ND | 16.5 | 3 | ND |
| Gungor [29] | European | 140 | 42.55 | 66.4 | 0 | 0 | 31 | ND | ND | ND | ND | 5 | ND |
| Turgut [30] | European | 162 | 63 | 52 | 100 | 65.5 | 41.5 | 6.5 | 23.5 | 18 | 16.5 | 4 | chronic |
| Jaremo (healthy control) [31] | European | 82 | 67.5 | 66.73 | 5.17 | 21.55 | 2.585 | 18.9 | 13.79 | 14.655 | 41.3 | 4 | ND |
| Jaremo (disease control) [31] | European | 130 | 71.5 | 68.1 | 12.75 | 43.75 | 9.485 | 28.65 | 26.25 | 25.05 | 55.92 | 4 | ND |
| Sahin [32] | European | 144 | 64.865 | 49.75 | 100 | 66.5 | 44.5 | ND | ND | ND | ND | 5 | Non-chronic |
| Tekin [33] | European | 219 | 73.5 | 35.5 | 13.5 | 68.5 | 19 | ND | ND | ND | ND | 5 | chronic |
| Turfan (without stroke) [34] | European | 135 | 59.5 | 54.55 | 15.6 | 33.1 | 55.5 | ND | ND | ND | ND | 4 | ND |
| Turfan (with stroke) [34] | European | 121 | 62.5 | 52.05 | 24.6 | 27 | 50.6 | ND | ND | ND | ND | 4 | ND |
| Feng [35] | Asian | 374 | 65.8 | 61.75 | 17.65 | 53.2 | 25.65 | 23 | 41.95 | 44.85 | 42.5 | 4 | ND |
| Liu (Paroxysmal AF) [36] | Asian | 101 | 64.35 | 62.5 | 5 | 32.5 | ND | ND | 21 | 15 | 34 | 3 | Non-chronic |
| Liu (Persistent AF) [36] | Asian | 107 | 65.8 | 61 | 6.5 | 35 | ND | ND | 29 | 13.5 | 35 | 3 | Non-chronic |
| Yoshizaki [37] | Asian | 176 | 70 | 76 | 32 | 65 | 52.5 | ND | 37.55 | 38.85 | 10.6 | 5 | Non-chronic |
| Hayashi (Paroxysmal AF) [38] | Asian | 27 | 57.95 | 92.5 | 14.5 | 48.5 | ND | ND | 40.5 | 26 | ND | 2 | Non-chronic |
| Hayashi (Chronic AF) [38] | Asian | 27 | 61.45 | 92.5 | 11.05 | 52 | ND | ND | 37 | 26 | ND | 2 | chronic |
| Fu [39] | Asian | 169 | 54.45 | 63.5 | ND | ND | 42.45 | ND | ND | 12.9 | 6.1 | 4 | Combined types |
| Liu [40] | Asian | 451 | 58.35 | 51.435 | ND | 100 | 23.7 | 14.85 | 71.55 | 61.15 | 42.7 | 5 | Combined types |
| Letsas (Paroxysmal AF) [41] | European | 93 | 64.35 | 59 | 6 | 60.5 | ND | ND | 43 | 15.5 | 34 | 5 | Non-chronic |
| Letsas (Permanent AF) [41] | European | 89 | 66.6 | 59.5 | 11 | 63 | ND | ND | 52.5 | 13.5 | 35.5 | 5 | chronic |
| Luan (Persistent AF) [42] | Asian | 53 | 53.25 | 50.855 | 0 | 26.21 | 30.2 | ND | ND | ND | ND | 5 | Non-chronic |
| Luan (Paroxysmal AF) [42] | Asian | 55 | 50.99 | 52.385 | 0 | 24.93 | 30.9 | ND | ND | ND | ND | 5 | Non-chronic |
| Alberti [43] | European | 51 | 64.45 | 47.05 | ND | ND | ND | ND | ND | ND | ND | 1 | Non-chronic |
| Dai [44] | Asian | 522 | 53.065 | 74.7 | 6.1 | 17 | ND | ND | ND | ND | ND | 5 | Non-chronic |
| Ichiki [45] | Asian | 72 | 51.5 | 80.205 | 16 | 37.5 | ND | ND | 8 | 15 | ND | 5 | Non-chronic |
| Yao (Persistent AF) [46] | Asian | 150 | 54.1 | 76.8 | 7.4 | 0 | 42.4 | ND | ND | 8.1 | 13.2 | 4 | Non-chronic |
| Yao (Paroxysmal AF) [46] | Asian | 339 | 53.35 | 74.95 | 4.25 | 0 | 46.55 | ND | ND | 6.6 | 7.85 | 4 | Non-chronic |
| Colkesen [47] | European | 190 | 54 | 38 | 18.5 | 41.5 | ND | ND | ND | 28 | ND | 4 | Non-chronic |
| Choudhury (disease control) [48] | European | 192 | 63.31 | 74 | 10.5 | 66.4 | ND | 33.15 | 55.7 | 46.5 | 43.7 | 4 | ND |
| Choudhury (healthy control) [48] | European | 177 | 62.305 | 72 | 4.1 | 31.8 | ND | 17.75 | 26.85 | 14.45 | 21.9 | 4 | ND |
| Pirat [49] | European | 39 | 49.5 | 51.5 | 8 | 26.5 | 32 | ND | 24.5 | ND | 38 | 5 | Non-chronic |
| Yip [50] | Asian | 82 | 65.75 | 63.05 | 9.7 | 34.7 | 5.65 | ND | 23.4 | 15.3 | ND | 3 | chronic |
| Kamath (Paroxysmal and persistent AF) [51] | European | 62 | 63.5 | 51.6 | ND | ND | ND | ND | ND | ND | ND | 1 | Non-chronic |
| Kamath (Permanent AF) [51] | European | 124 | 66 | 52.65 | ND | ND | ND | ND | ND | ND | ND | 1 | chronic |
| Kamath (Paroxysmal AF) [52] | European | 58 | 63 | 48.27 | 6.85 | 24.135 | 5.17 | ND | ND | ND | ND | 4 | Non-chronic |
| Kamath (Permanent AF) [52] | European | 116 | 65 | 52.29 | 5.15 | 30.45 | 5.17 | ND | ND | ND | ND | 4 | chronic |
| Kamath [53] | European | 143 | 70 | 54.18 | 5.375 | 29.565 | ND | ND | ND | ND | ND | 1 | ND |
| Kamath [54] | European | 57 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 1 | chronic |
| Peverill [55] | Oceania | 163 | 55 | 84.6 | ND | ND | ND | ND | ND | ND | ND | 5 | ND |
| Kahn (without stroke) [56] | North America | 81 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 1 | chronic |
| Kahn (with stroke) [56] | North America | 36 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 1 | chronic |
| Lip [57] | European | 77 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 1 | chronic |
| Gustafsson (without stroke) [58] | European | 40 | 77 | ND | 10 | 25 | 25 | ND | ND | ND | ND | 1 | ND |
| Gustafsson (with stroke) [58] | European | 40 | 77 | ND | 12.5 | 27.5 | 30 | ND | ND | ND | ND | 1 | ND |
| Recurrence of AF | |||||||||||||
| Gurses [9] | European | 86 | 56.8 | 57.7 | 15.8 | 48.55 | ND | ND | 21.2 | 16.5 | ND | 5 | Non-chronic |
| Hongliang Li [59] | Asian | 104 | 62.5 | 43.9 | 24.45 | 46.1 | 37.45 | ND | 41 | 49.65 | 42.4 | 4 | Non-chronic |
| Yanagisawa (without heart failure) [60] | Asian | 678 | 61.1 | 76 | 12.5 | 46 | ND | 3.5 | 35 | ND | 31.5 | 5 | Non-chronic |
| Yanagisawa (with heart failure) [60] | Asian | 79 | 63.6 | 74.5 | 20 | 38 | ND | 77.5 | 58 | ND | 81.5 | 5 | Non-chronic |
| Aksu [61] | European | 49 | 59.65 | 52.5 | 16.5 | 48.5 | 47 | ND | ND | ND | ND | 5 | Non-chronic |
| Gurses [62] | European | 299 | 55.7 | 51.15 | 13.2 | 42.4 | 31 | ND | ND | ND | ND | 4 | Non-chronic |
| Karavelioglu [63] | European | 218 | 64.4 | 41.095 | 18 | 58.5 | 21 | ND | 23.5 | 10.5 | 67 | 5 | Non-chronic |
| Wen [64] | Asian | 75 | 63.62 | ND | 7.5 | 57.5 | 20 | ND | ND | 30 | ND | 5 | Non-chronic |
| Guo Xueyuan [65] | Asian | 379 | 49.665 | 73.55 | 0 | 0 | ND | ND | ND | ND | ND | 5 | ND |
| Aribas [66] | European | 149 | 60 | ND | 29 | 62.5 | 18.5 | ND | ND | ND | ND | 2 | Non-chronic |
| Bing Li [67] | Asian | 288 | 57 | 71.1 | 28.65 | 55.05 | 38.15 | ND | 38 | 14.2 | 27.7 | 5 | Non-chronic |
| Canpolat [68] | European | 251 | 55.2 | 54.85 | 15.15 | 44.35 | 36.55 | ND | 51.25 | 18.05 | ND | 5 | Non-chronic |
| Im [69] | Asian | 499 | 56.4 | 73.65 | 15.55 | 43.9 | ND | ND | ND | ND | ND | 5 | Non-chronic |
| Xiao-nan HE [70] | Asian | 330 | 59.5 | 66.3 | ND | 48.65 | ND | ND | 50 | 14 | 52 | 5 | Non-chronic |
| Ferro [71] | European | 144 | 70.95 | 56.5 | 14 | 87.5 | 5 | ND | 46.5 | 22.5 | ND | 2 | Non-chronic |
| Smit [72] | European | 100 | 64 | 73.8 | 11.9 | 65.95 | 15 | 41.2 | 69.05 | 36.65 | 89.3 | 5 | Non-chronic |
| Wang (Paroxysmal AF) [73] | Asian | 103 | 57.5 | 34.8 | ND | 41.65 | ND | ND | ND | ND | 4.24 | 5 | Non-chronic |
| Wang (Persistent AF) [73] | Asian | 55 | 52.5 | 74.65 | ND | 50.35 | ND | ND | ND | ND | 5.65 | 5 | Non-chronic |
| Liu (Paroxysmal AF) [74] | Asian | 77 | 56 | 75.6 | ND | 37.3 | ND | ND | ND | ND | ND | 2 | Non-chronic |
| Liu (Persistent AF) [74] | Asian | 44 | 53.05 | 84.85 | ND | 51.2 | ND | ND | ND | ND | ND | 2 | Non-chronic |
| Vizzardi [75] | European | 106 | 69 | 61 | 12.05 | ND | ND | ND | 8 | ND | ND | 5 | Non-chronic |
| Letsas [76] | European | 72 | 54.55 | 81.5 | 21.5 | 21.5 | ND | ND | 23 | 14.5 | ND | 5 | Non-chronic |
| Korantzopoulos [77] | European | 30 | 68.5 | 48.39 | 7.1 | 64.25 | 4.75 | 30.95 | 35.7 | 5.55 | ND | 5 | Non-chronic |
Supplementary Table 3.
Subgroup-analysis.
| Subgroup | Studies (N) | WMD (95% CI) | I-squared and Heterogeneity-P-value and Effect-P-value respectively | Is this general item as heterogeneity factor? 1.Yes, probably 2. No |
|---|---|---|---|---|
| Occurrence of AF | ||||
|
| ||||
| Platelet count | ||||
|
| ||||
| Year of Publication | No | |||
| >2000 | 43 | −23.75 (−25.22 to −22.29) | 91% and 0.001 and 0.001 | |
| ≤2000 | 5 | −56.50 (−61.45 to −51.55) | 90.7% and 0.001 and 0.001 | |
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 7 | −3.88 (−10.98 to 3.22) | 13.8% and 0.324 and 0.284 | |
| European | 36 | −29.41 (−30.95 to −27.88) | 93.7% and 0.001 and 0.001 | |
| Africa | – | – | – | |
| North American | 4 | −12.11 (−16.25 to −7.96) | 0.0% and 0.476 and 0.001 | |
| South American | – | – | – | |
| Australia | 1 | −23 (−40.50 to −5.49) | – | |
|
| ||||
| Design of study | No | |||
| Cohort | 8 | −29.09 (−31.01 to −27.16) | 92.4% and 0.001 and 0.001 | |
| Case-control | 40 | −23.30 (−25.36 to −21.25) | 93% and 0.001 and 0.001 | |
|
| ||||
| Number of population | No | |||
| >300 | 2 | −6.33 (−19.68 to 7.03) | 0.0% and 0.689 and 0.353 | |
| ≤300 | 46 | −26.61 (−28.02 to −25.20) | 93.1% and 0.001 and 0.001 | |
|
| ||||
| Mean age | No | |||
| >60 years | 35 | −27.69 (−29.13 to −26.25) | 94% and 0.001 and 0.001 | |
| ≤60 years | 8 | −2.68 (−9.46 to 4.10) | 78.4% and 0.001 and 0.438 | |
|
| ||||
| Male | No | |||
| >70% | 9 | −29.76 (−31.69 to −27.83) | 83.8% and 0.001 and 0.001 | |
| ≤70% | 32 | −15.69 (−17.94 to −13.43) | 90.5% and 0.001 and 0.001 | |
|
| ||||
| Diabetes mellitus | Yes, probably | |||
| >30% | 3 | −0.27 (−9.57 to 9.01) | 35.9% and 0.210 and 0.953 | |
| ≤30% | 35 | −24.77 (−26.27 to −23.26) | 92.2% and 0.001 and 0.001 | |
|
| ||||
| Hypertension | No | |||
| >70% | – | – | – | |
| ≤70% | 39 | −24.91 (−26.38 to −23.44) | 92.5% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | No | |||
| >30% | 10 | −16.36 (−21.68 to −11.04) | 92.8% and 0.001 and 0.001 | |
| ≤30% | 20 | −22.62 (−25.67 to −19.56) | 92.4% and 0.001 and 0.001 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 13 | −28.39 (−30.26 to −26.52) | 85.7% and 0.001 and 0.001 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 22 | −25.47 (−27.18 to −23.76) | 86.5% and 0.001 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 21 | −25.33 (−27.06 to −23.61) | 88% and 0.001 and 0.001 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 21 | −25.36 (−27.06 to −23.66) | 86.6% and 0.001 and 0.001 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | 10 | −52.72 (−56.32 to −49.12) | 92.3% and 0.001 and 0.001 | |
| 2 | 3 | 1.69 (−17.11 to 20.53) | 67.3% and 0.047 and 0.860 | |
| 3 | 6 | −10.36 (−21.43 to 0.69) | 0.0% and 0.703 and 0.066 | |
| 4 | 19 | −24.85 (−26.58 to −23.13) | 91.6% and 0.001 and 0.001 | |
| 5 | 9 | −11.38 (−14.88 to −7.88) | 36.4% and 0.127 and 0.001 | |
| 6 | 1 | 17.40 (−6.03 to 40.83) | – | |
|
| ||||
| AF | Yes, probably | |||
| Chronic | 16 | −2.80 (−7.77 to 2.16) | 18.1% and 0.246 and 0.268 | |
| Non-chronic | 11 | −20.88 (−23.55 to −18.20) | 95.7% and 0.001 and 0.001 | |
|
| ||||
| Type of AF | Yes, probably | |||
| Paroxysmal | 5 | −3.72 (−9.24 to 1.79) | 72.1% and 0.006 and 0.186 | |
| Persistent | 3 | −41.93 (−46.40 to −37.46) | 97.4% and 0.001 and 0.001 | |
| Permanent | 6 | −5.09 (−11.96 to 1.78) | 55.3% and 0.048 and 0.147 | |
|
| ||||
| Mean platelet volume | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | 3 | 1.37 (1.16 to 1.58) | 95.9% and 0.001 and 0.001 | |
| European | 19 | 0.39 (0.35 to 0.43) | 95.2% and 0.001 and 0.001 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | 1 | −0.20 (−0.63 to 0.23) | – | |
|
| ||||
| Design of study | No | |||
| Cohort | 4 | 1.37 (1.14 to 1.60) | 94.7% and 0.001 and 0.001 | |
| Case-control | 19 | 0.39 (0.35 to 0.43) | 95.4% and 0.001 and 0.001 | |
|
| ||||
| Number of population | Yes, probably | |||
| >300 | 2 | 0.90 (0.67 to 1.13) | 0.0% and 0.666 and 0.001 | |
| ≤300 | 21 | 0.41 (0.36 to 0.45) | 96% and 0.001 and 0.001 | |
|
| ||||
| Mean age | No | |||
| >60 years | 16 | 0.58 (0.54 to 0.63) | 94.1and 0.001 and 0.001 | |
| ≤60 years | 4 | 0.23 (0.05 to 0.42) | 93.5% and 0.001 and 0.012 | |
|
| ||||
| Male | No | |||
| >70% | 6 | 0.59 (0.46 to 0.71) | 93.9% and 0.001 and 0.001 | |
| ≤70% | 16 | 0.40 (0.36 to 0.44) | 96.4% and 0.001 and 0.001 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | 4 | 0.63 (0.57 to 0.69) | 96.8% and 0.001 and 0.001 | |
| ≤30% | 16 | 0.49 (0.42 to 0.57) | 92.7% and 0.001 and 0.001 | |
|
| ||||
| Hypertension | No | |||
| >70% | – | – | – | |
| ≤70% | 20 | 0.58 (0.53 to 0.62) | 93.8% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | No | |||
| >30% | 8 | 0.68 (0.62 to 0.74) | 94.7% and 0.001 and 0.001 | |
| ≤30% | 8 | 0.37 (0.28 to 0.45) | 92.1% and 0.001 and 0.001 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 9 | 0.54 (0.49 to 0.59) | 94.3% and 0.001 and 0.001 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 11 | 0.57 (0.52 to 0.62) | 95.8% and 0.001 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 11 | 0.66 (0.60 to 0.71) | 94.7% and 0.001 and 0.001 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 12 | 0.55 (0.50 to 0.60) | 95.8% and 0.001 and 0.001 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | – | – | – | |
| 2 | 1 | 0.80 (0.26 to 1.33) | – | |
| 3 | 3 | 0.081 (−0.109 to 0.272) | 66.1% and 0.053 and 0.404 | |
| 4 | 10 | 0.67 (0.62 to 0.73) | 95.1% and 0.001 and 0.001 | |
| 5 | 8 | 0.108 (0.046 to 0.17) | 93.6% and 0.001 and 0.001 | |
| 6 | 1 | 1.10 (0.75 to 1.45) | – | |
|
| ||||
| AF | No | |||
| Chronic | 8 | 0.55 (0.49 to 0.60) | 95.7% and 0.001 and 0.001 | |
| Non-chronic | 3 | 0.85 (0.58 to 1.13) | 88.6% and 0.001 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 1 | 1.70 (1.20. to 2.19) | – | |
| Persistent | 1 | 0.32 (−0.09 to 0.73) | – | |
| Permanent | 4 | 0.28 (0.17 to 0.38) | 91.7% and 0.001 and 0.001 | |
|
| ||||
| WBC | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | 15 | 0.001 (−0.058 to 0.06) | 80.8% and 0.001 and 0.973 | |
| European | 25 | −0.05 (−0.13 to 0.023) | 89.3% and 0.001 and 0.159 | |
| Africa | – | – | – | |
| North American | 2 | 0.828 (0.46 to 1.187) | 0.0% and 0.365 and 0.001 | |
| South American | – | – | ||
| Australia | – | – | ||
|
| ||||
| Design of study | Yes, probably | |||
| Cohort | 4 | 0.370 (−0.083 to 0.823) | 13.2% and 0.326 and 0.109 | |
| Case-control | 38 | −0.009 (−0.057 to 0.039) | 88.2% and 0.001 and 0.708 | |
|
| ||||
| Number of population | No | |||
| >300 | 5 | 0.035 (−0.047 to 0.117) | 84.8% and 0.001 and 0.403 | |
| ≤300 | 37 | −0.025 (−0.083 to 0.033) | 87.7% and 0.001 and 0.398 | |
|
| ||||
| Mean age | No | |||
| >60 years | 27 | −0.060 (−0.140 to 0.019) | 88.3% and 0.001 and 0.136 | |
| ≤60 years | 15 | 0.025 (−0.033 to 0.084) | 85.2% and 0.001 and 0.397 | |
|
| ||||
| Male | No | |||
| >70% | 11 | 0.009 (−0.051 to 0.070) | 86.4% and 0.001 and 0.761 | |
| ≤70% | 31 | −0.027 (−0.102 to 0.048) | 87.8% and 0.001 and 0.481 | |
|
| ||||
| Diabetes mellitus | Yes, probably | |||
| >30% | 2 | 0.216 (−0.419 to 0.852) | 0.0% and 0.789 and 0.505 | |
| ≤30% | 38 | 0.055 (0.005 to 0.104) | 85% and 0.001 and 0.030 | |
|
| ||||
| Hypertension | Yes, probably | |||
| >70% | 2 | −0.743 (−0.952 to −0.535) | 0.0% and 0.873 and 0.001 | |
| ≤70% | 39 | 0.097 (0.046 to 0.147) | 80.5% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | Yes, probably | |||
| >30% | 11 | 0.053 (−0.010 to 0.115) | 26.4% and 0.193 and 0.102 | |
| ≤30% | 16 | 0.231 (0.123 to 0.339) | 83.9% and 0.001 and 0.001 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 8 | 0.061 (−0.102 to 0.224) | 41.9% and 0.099 and 0.464 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | 1 | −0.70 (−1.269 to −0.131) | – | |
| ≤70% | 21 | 0.012 (−0.086 to 0.111) | 83.2% and 0.001 and 0.804 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 21 | −0.00 (−0.057 to 0.506) | 81.8% and 0.001 and 0.990 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 21 | 0.071 (0.015 to 0.127) | 76.2% and 0.001 and 0.012 | |
|
| ||||
| Anti-coagulant status codes | Yes, Probably | |||
| 1 | 1 | −0.70 (−0.875 to −0.525) | – | |
| 2 | 3 | 0.661 (−0.627 to 1.949) | 0.0% and 0.924 and 0.314 | |
| 3 | 9 | −0.232 (−0.397 to −0.067) | 85.4% and 0.001 and 0.006 | |
| 4 | 8 | 0.054 (−0.006 to 0.115) | 87.6% and 0.001 and 0.077 | |
| 5 | 20 | 0.132 (0.030 to 0.233) | 85% and 0.001 and 0.011 | |
| 6 | 1 | 0.400 (−0.220 to 1.020) | – | |
|
| ||||
| AF | Yes, probably | |||
| Chronic | 8 | 0.125 (−0.048 to 0.299) | 0.0% and 0.833 and 0.156 | |
| Non-chronic | 22 | −0.050 (−0.102 to 0.001) | 92% and 0.001 and 0.056 | |
|
| ||||
| Type of AF | Yes, probably | |||
| Paroxysmal | 9 | −0.087 (−0.161 to −0.014) | 88.6% and 0.001 and 0.020 | |
| Persistent | 6 | −0.019 (−0.101 to 0.062) | 95.2% and 0.001 and 0.641 | |
| Permanent | 5 | 0.069 (−0.120 to 0.259) | 0.0% and 0.958 and 0.473 | |
|
| ||||
| NLR | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | – | – | – | |
| European | 9 | 0.901 (0.802 to 1.000) | 94% and 0.001 and 0.001 | |
| Africa | – | – | – | |
| North American | 1 | −0.640 (−1.711 to 0.431) | – | |
| South American | – | – | ||
| Australia | – | – | ||
|
| ||||
| Design of study | No | |||
| Cohort | 1 | −0.640 (−1.711 to 0.431) | – | |
| Case-control | 9 | 0.901 (0.802 to 1.000) | 94% and 0.001 and 0.001 | |
|
| ||||
| Number of population | No | |||
| >300 | 1 | 1.200 (−0.789 to 3.189) | – | |
| ≤300 | 9 | 0.887 (0.789 to 0.986) | 94.3% and 0.001 and 0.001 | |
|
| ||||
| Mean age | No | |||
| >60 years | 7 | 1.030 (0.919 to 1.141) | 91.5% and 0.001 and 0.001 | |
| ≤60 years | 3 | 0.365 (0.152 to 0.579) | 95.1% and 0.001 and 0.001 | |
|
| ||||
| Male | Yes, probably | |||
| >70% | 2 | −0.277 (−1.170 to 0.716) | 60.8% and 0.110 and 0.637 | |
| ≤70% | 8 | 0.901 (0.801 to 1.00) | 94.7% and 0.001 and 0.001 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | 1 | 0.670 (0.201 to 1.139) | – | |
| ≤30% | 9 | 0.898 (0.797 to 0.999) | 94.3% and 0.001 and 0.001 | |
|
| ||||
| Hypertension | ||||
| >70% | All of studies: ≤70% | |||
| ≤70% | ||||
|
| ||||
| Cigarette smoking | No | |||
| >30% | 3 | 0.492 (0.072 to 0.912) | 62.5% and 0.069 and 0.022 | |
| ≤30% | 6 | 0.928 (0.824 to 1.032) | 96.2% and 0.001 and 0.001 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 1 | 0.600 (0.146 to 1.054) | – | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 3 | 1.025 (0.687 to 1.364) | 91.2% and 0.001 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 2 | 0.630 (0.187 to 1.072) | 0.0% and 0.564 and 0.005 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | 0.408 (0.215 to 0.601) | 92.8% and 0.001 and 0.001 | |
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | – | – | – | |
| 2 | 1 | 1.200 (−0.789 to 3.189) | – | |
| 3 | 3 | 0.365 (0.152 to 0.579) | 95.1% and 0.001 and 0.001 | |
| 4 | 1 | 0.600 (0.146 to 1.054) | – | |
| 5 | 4 | 1.081 (0.962 to 1.199) | 95.4% and 0.001 and 0.001 | |
| 6 | 1 | 0.700 (0.236 to 1.164) | – | |
|
| ||||
| AF | No | |||
| Chronic | – | – | – | |
| Non-chronic | 4 | 0.689 (0.538 to 0.840) | 0.0% and 0.935 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 1 | 0.700 (0.529 to 0.871) | – | |
| Persistent | 2 | 0.634 (0.308 to 0.960) | 0.0% and 0.833 and 0.001 | |
| Permanent | – | – | – | |
|
| ||||
| RDW | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 1 | 0.260 (0.065 to 0.455) | – | |
| European | 6 | 0.873 (0.806 to 0.941) | 0.0% and 0.613 and 0.001 | |
| Africa | - | – | – | |
| North American | 1 | 0.280 (0.196 to 0.364) | – | |
| South American | - | – | – | |
| Australia | - | – | ||
|
| ||||
| Design of study | ||||
| Cohort | All of studies: case-control | |||
| Case-control | ||||
|
| ||||
| Number of population | No | |||
| >300 | 1 | 0.500 (−0.039 to 1.039) | – | |
| ≤300 | 7 | 0.615 (0.564 to 0.666) | 95.5% and 0.001 and 0.001 | |
|
| ||||
| Mean age | Yes, probably | |||
| >60 years | 4 | 0.412 (0.338 to 0.485) | 92.8% and 0.001 and 0.001 | |
| ≤60 years | 3 | 0.885 (0.809 to 0.961) | 0.0% and 0.716 and 0.001 | |
|
| ||||
| Male | No | |||
| >70% | 1 | 0.500 (−0.039 to 1.039) | – | |
| ≤70% | 6 | 0.641 (0.588 to 0.694) | 95.8% and 0.001 and 0.001 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | - | – | – | |
| ≤30% | 7 | 0.640 (0.587 to 0.692) | 95% and 0.001 and 0.001 | |
|
| ||||
| Hypertension | Yes, probably | |||
| >70% | 2 | 0.856 (0.700 to 1.011) | 0.0% and 0.337 and 0.001 | |
| ≤70% | 5 | 0.612 (0.556 to 0.668) | 96.4% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | No | |||
| >30% | 1 | 0.500 (−0.039 to 1.039) | – | |
| ≤30% | 3 | 0.885 (0.809 to 0.961) | 0.0% and 0.716 and 0.001 | |
|
| ||||
| Medication: Diuretic | ||||
| >70% | No Data | |||
| ≤70% | ||||
|
| ||||
| Medication: ACEI | No | |||
| >70% | - | – | – | |
| ≤70% | 2 | 1.021 (0.615 to 1.426) | 0.0% and 0.636 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | - | – | – | |
| ≤70% | 1 | 0.500 (−0.039 to 1.039) | – | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | - | – | – | |
| ≤70% | 3 | 0.885 (0.809 to 0.961) | 0.0% and 0.716 and 0.001 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | - | – | – | |
| 2 | 1 | 0.500 (−0.039 to 1.039) | – | |
| 3 | 4 | 0.875 (0.806 to 0.944) | 0.0% and 0.796 and 0.001 | |
| 4 | - | – | – | |
| 5 | 3 | 0.297 (0.221 to 0.373) | 80.7% and 0.006 and 0.001 | |
| 6 | - | – | – | |
|
| ||||
| AF | No | |||
| Chronic | - | – | – | |
| Non-chronic | 4 | 0.379 (0.310 to 0.448) | 91.6% and 0.001 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 1 | 0.260 (0.065 to 0.455) | – | |
| Persistent | - | – | – | |
| Permanent | - | – | – | |
|
| ||||
| MCV | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | 1 | −0.300 (−1.364 to 0.764) | – | |
| European | 1 | 1.000 (−0.337 to 2.337) | – | |
| Africa | - | – | – | |
| North American | 1 | −0.280 (−0.706 to 0.146) | – | |
| South American | - | – | – | |
| Australia | 1 | 1.000 (−0.998 to 2.998) | – | |
|
| ||||
| Design of study | ||||
| Cohort | All of studies: Case-control | |||
| Case-control | ||||
|
| ||||
| Number of population | No | |||
| >300 | 1 | −0.300 (−1.364 to 0.764) | – | |
| ≤300 | 3 | −0.116 (−0.514 to 0.283) | 55% and 0.108 and 0.569 | |
|
| ||||
| Mean age | No | |||
| >60 years | 2 | −0.283 (−0.679 to 0.113) | 0.0% and 0.162 and 0.973 | |
| ≤60 years | 2 | 1.000 (−0.111 to 2.111) | 0.0% and 1.000 and 0.078 | |
|
| ||||
| Male | No | |||
| >70% | 1 | 1.000 (−0.998 to 2.998) | – | |
| ≤70% | 3 | −0.179 (−0.559 to 0.200) | 38.5% and 0.197 and 0.354 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | - | – | – | |
| ≤30% | 3 | −0.179 (−0.559 to 0.200) | 38.5% and 0.197 and 0.354 | |
|
| ||||
| Hypertension | No | |||
| >70% | - | – | – | |
| ≤70% | 3 | −0.179 (−0.559 to 0.200) | 38.5% and 0.197 and 0.354 | |
|
| ||||
| Cigarette smoking | No | |||
| >30% | - | – | – | |
| ≤30% | 2 | 0.204 (−0.628 to 1.037) | 55% and 0.136 and 0.631 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | - | – | – | |
| ≤70% | 1 | −0.300 (−1.364 to 0.764) | – | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | - | – | – | |
| ≤70% | 1 | −0.300 (−1.364 to 0.764) | – | |
|
| ||||
| Medication: Statin | No | |||
| >70% | - | – | – | |
| ≤70% | 1 | −0.300 (−1.364 to 0.764) | – | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | - | – | – | |
| ≤70% | 2 | 0.204 (−0.628 to 1.037) | 55% and 0.136 and 0.631 | |
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | – | – | – | |
| 2 | – | – | – | |
| 3 | 1 | 1.000 (−0.337 to 2.337) | – | |
| 4 | 1 | −0.300 (−1.364 to 0.764) | – | |
| 5 | 2 | −0.224 (−0.641 to 0.193) | 33.7% and 0.219 and 0.292 | |
| 6 | – | – | – | |
|
| ||||
| AF | No | |||
| Chronic | – | – | – | |
| Non-chronic | 1 | −0.280 (−0.706 to 0.146) | – | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | – | – | – | |
| Persistent | – | – | – | |
| Permanent | – | – | – | |
|
| ||||
| HCT | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | – | – | – | |
| European | 9 | 0.552 (0.004 to 1.100) | 53.4% and 0.028 and 0.048 | |
| Africa | – | – | – | |
| North American | 1 | 2.670 (2.168 to 3.172) | – | |
| South American | – | – | – | |
| Australia | 1 | 3.000 (1.605 to 4.395) | – | |
|
| ||||
| Design of study | ||||
| Cohort | All of studies: Case-control | |||
| Case-control | ||||
|
| ||||
| Number of population | ||||
| >300 | All of studies: ≤300 | |||
| ≤300 | ||||
|
| ||||
| Mean age | No | |||
| >60 years | 10 | 1.704 (1.334 to 2.075) | 81.4% and 0.001 and 0.001 | |
| ≤60 years | 1 | 3.000 (1.605 to 4.395) | – | |
|
| ||||
| Male | No | |||
| >70% | 3 | 1.666 (0.767 to 2.566) | 67% and 0.048 and 0.001 | |
| ≤70% | 8 | 1.813 (1.423 to 2.203) | 84.6% and 0.001 and 0.001 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | – | – | – | |
| ≤30% | 8 | 1.691 (1.299 to 2.083) | 84.6% and 0.001 and 0.001 | |
|
| ||||
| Hypertension | No | |||
| >70% | – | – | – | |
| ≤70% | 8 | 1.691 (1.299 to 2.083) | 84.6% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | No | |||
| >30% | – | – | – | |
| ≤30% | 5 | −0.064 (−0.805 to 0.678) | 39.4% and 0.158 and 0.867 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | 0.402 (−0.488 to 1.292) | 0.0% and 0.753 and 0.376 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | 0.402 (−0.488 to 1.292) | 0.0% and 0.753 and 0.376 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | 0.402 (−0.488 to 1.292) | 0.0% and 0.753 and 0.376 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | 0.402 (−0.488 to 1.292) | 0.0% and 0.753 and 0.376 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | 2 | 1.819 (0.693 to 2.945) | 65.9% and 0.087 and 0.002 | |
| 2 | – | – | – | |
| 3 | 2 | −0.021 (−1.381 to 1.340) | 0.0% and 0.477 and 0.976 | |
| 4 | 4 | 0.852 (0.001 to 1.704) | 0.0% and 0.985 and 0.050 | |
| 5 | 3 | 2.230 (1.787 to 2.673) | 93.9% and 0.001 and 0.001 | |
| 6 | – | – | – | |
|
| ||||
| AF | No | |||
| Chronic | 5 | 0.062 (−0.635 to 0.759) | 46.9% and 0.110 and 0.861 | |
| Non-chronic | 3 | 2.611 (2.141 to 3.082) | 18.5% and 0.293 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 1 | 1.000 (−1.122 to 3.122) | – | |
| Persistent | – | – | – | |
| Permanent | 4 | 0.617 (−0.215 to 1.450) | 0.0% and 0.603 and 0.146 | |
|
| ||||
| Hb | ||||
|
| ||||
| Year of publication | No | |||
| >2000 | 25 | 0.024 (−0.038 to 0.087) | 91.1% and 0.001 and 0.444 | |
| ≤2000 | 2 | 1.076 (0.522 to 1.630) | 85.2% and 0.009 and 0.001 | |
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 2 | −0.048 (−0.366 to 0.271) | 0.0% and 0.758 and 0.769 | |
| European | 21 | −0.150 (−0.219 to −0.081) | 76.8% and 0.001 and 0.001 | |
| Africa | – | – | – | |
| North American | 4 | 0.994 (0.840 to 1.149) | 89.4% and 0.001 and 0.001 | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | Yes, probably | |||
| Cohort | 6 | −0.093 (−0.142 to −0.044) | 0.0% and 0.488 and 0.001 | |
| Case-control | 21 | 0.102 (0.024 to 0.181) | 92.8% and 0.001 and 0.011 | |
|
| ||||
| Number of population | No | |||
| >300 | 1 | −0.100 (−0.643 to 0.443) | – | |
| ≤300 | 26 | 0.039 (−0.023 to 0.102) | 91.4% and 0.001 and 0.216 | |
|
| ||||
| Mean age | No | |||
| >60 years | 20 | 0.033 (−0.032 to 0.098) | 92.5% and 0.001 and 0.317 | |
| ≤60 years | 5 | −0.077 (−0.297 to 0.143) | 73.5% and 0.005 and 0.494 | |
|
| ||||
| Male | No | |||
| >70% | 6 | −0.040 (−0.143 to 0.063) | 75.1% and 0.001 and 0.447 | |
| ≤70% | 19 | 0.062 (−0.017 to 0.140) | 92.7% and 0.001 and 0.123 | |
|
| ||||
| Diabetes mellitus | Yes, probably | |||
| >30% | 2 | −0.048 (−0.366 to 0.271) | 0.0% and 0.758 and 0.769 | |
| ≤30% | 23 | 0.027 (−0.036 to 0.091) | 91.8% and 0.001 and 0.401 | |
|
| ||||
| Hypertension | Yes, probably | |||
| >70% | 2 | −0.275 (−0.481 to 0.070) | 0.0% and 0.583 and 0.009 | |
| ≤70% | 23 | 0.055 (−0.011 to 0.120) | 91.6% and 0.001 and 0.102 | |
|
| ||||
| Cigarette smoking | Yes, probably | |||
| >30% | 8 | −0.054 (−0.223 to 0.114) | 0.0% and 0.597 and 0.529 | |
| ≤30% | 10 | −0.308 (−0.422 to −0.193) | 80.8% and 0.001 and 0.001 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 9 | −0.184 (−0.267 to −0.100) | 84.9% and 0.001 and 0.001 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 13 | −0.192 (−0.272 to −0.112) | 80.6% and 0.001 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 10 | −0.017 (−0.114 to 0.079) | 58% and 0.011 and 0.729 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 14 | −0.172 (−0.251 to −0.094) | 80.8% and 0.001 and 0.001 | |
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | 2 | 1.076 (0.522 to 1.630) | 85.2% and 0.009 and 0.001 | |
| 2 | 1 | −0.100 (−0.643 to 0.443) | – | |
| 3 | 6 | −0.183 (−0.355 to −0.011) | 73.3% and 0.002 and 0.037 | |
| 4 | 9 | −0.005 (−0.100 to 0.090) | 63.2% and 0.005 and 0.913 | |
| 5 | 8 | 0.148 (0.049 to 0.247) | 96.8% and 0.001 and 0.004 | |
| 6 | 1 | −0.200 (−0.550 to 0.150) | – | |
|
| ||||
| AF | No | |||
| Chronic | 8 | −0.320 (−0.443 to −0.196) | 85.2% and 0.001 and 0.001 | |
| Non-chronic | 5 | 0.543 (0.418 to 0.668) | 96.1% and 0.001 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 1 | 0.500 (−0.059 to 1.059) | – | |
| Persistent | 1 | 0.200 (−0.553 to 0.953) | – | |
| Permanent | 4 | −0.458 (−0.596 to −0.320) | 68.5% and 0.023 and 0.001 | |
|
| ||||
| Occurrence of AF | ||||
|
| ||||
| Platelet count | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 2 | 14.48 (−1.95 to 30.91) | 28.6% and 0.237 and 0.084 | |
| European | 2 | −12.96 (−25.66 to −0.272) | 40.8% and 0.194 and 0.045 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | No | |||
| Cohort | 3 | 0.217 (−0.188 to 0.622) | 50.9% and 0.130 and 0.294 | |
| Case-control | 1 | 20.45 (1.27 to 39.63) | – | |
|
| ||||
| Number of population | ||||
| >300 | All of studies: ≤300 | |||
| ≤300 | ||||
|
| ||||
| Mean age | No | |||
| >60 years | 3 | −0.132 (−13.084 to 12.82) | 78.8% and 0.009 and 0.984 | |
| ≤60 years | 1 | −6.60 (−22.517 to 9.317) | – | |
|
| ||||
| Male | No | |||
| >70% | – | – | – | |
| ≤70% | 3 | −2.78 (−13.37 to 7.79) | 79.6% and 0.007 and 0.606 | |
|
| ||||
| Diabetes mellitus | ||||
| >30% | All of studies: ≤30% | |||
| ≤30% | ||||
|
| ||||
| Hypertension | ||||
| >70% | All of studies: ≤70% | |||
| ≤70% | ||||
|
| ||||
| Cigarette smoking | Yes, probably | |||
| >30% | 2 | 4.43 (−7.81 to 16.80) | 77.9% and 0.033 and 0.478 | |
| ≤30% | 2 | −17.38 (−34.94 to 0.174) | 22.3% and 0.257 and 0.052 | |
|
| ||||
| Medication: Diuretic | ||||
| >70% | No Data | |||
| ≤70% | ||||
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 2 | 0.238 (−13.93 to 14.41) | 89.4% and 0.002 and 0.974 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 3 | −0.132 (−13.08 to 12.82) | 78.8% and 0.009 and 0.984 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 2 | 0.238 (−13.93 to 14.41) | 89.4% and 0.002 and 0.974 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | – | – | – | |
| 2 | – | – | – | |
| 3 | – | – | – | |
| 4 | 2 | 4.432 (−7.817 to 16.68) | 77.9% and 0.033 and 0.478 | |
| 5 | 2 | −17.38 (−34.94 to 0.174) | 22.3% and 0.257 and 0.052 | |
| 6 | – | – | – | |
|
| ||||
| AF | ||||
| Chronic | All of studies: non–chronic | |||
| Non-chronic | ||||
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 2 | 0.238 (−13.93 to 14.41) | 89.4% and 0.002 and 0.974 | |
| Persistent | – | – | – | |
| Permanent | – | – | – | |
|
| ||||
| WBC | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 11 | 0.136 (−0.013 to 0.284) | 34.7% and 0.121 and 0.073 | |
| European | 11 | 0.347 (0.120 to 0.574) | 65.1% and 0.001 and 0.003 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | Yes, probably | |||
| Cohort | 20 | 0.202 (0.077 to 0.326) | 58.6% and 0.001 and 0.002 | |
| Case-control | 2 | −0.344 (−2.282 to 1.594) | 0.0% and 0.710 and 0.728 | |
|
| ||||
| Number of population | No | |||
| >300 | 3 | 0.146 (−0.030 to 0.321) | 63.6% and 0.064 and 0.103 | |
| ≤300 | 19 | 0.254 (0.077 to 0.430) | 55.1% and 0.002 and 0.005 | |
|
| ||||
| Mean age | Yes, probably | |||
| >60 years | 10 | 0.097 (−0.076 to 0.269) | 0.0% and 0.498 and 0.272 | |
| ≤60 years | 12 | 0.310 (0.131 to 0.489) | 68.7% and 0.001 and 0.001 | |
|
| ||||
| Male | No | |||
| >70% | 9 | 0.251 (0.093 to 0.410) | 49.4% and 0.045 and 0.002 | |
| ≤70% | 11 | 0.107 (−0.108 to 0.323) | 62.4% and 0.003 and 0.328 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | – | – | – | |
| ≤30% | 17 | 0.286 (0.149 to 0.423) | 55.7% and 0.003 and 0.001 | |
|
| ||||
| Hypertension | No | |||
| >70% | 1 | −0.030 (−0.560 to 0.50) | – | |
| ≤70% | 20 | 0.215 (0.087 to 0.344) | 58.1% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | Yes, probably | |||
| >30% | 5 | 0.707 (0.376 to 1.037) | 63% and 0.029 and 0.001 | |
| ≤30% | 6 | 0.032 (−0.261 to 0.325) | 0.0% and 0.416 and 0.832 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | 1 | −0.40 (−1.087 to 0.287) | – | |
| ≤70% | 3 | 0.202 (−0.012 to 0.417) | 0.0% and 0.776 and 0.064 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 13 | 0.217 (0.067 to 0.367) | 68.8% and 0.001 and 0.005 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 11 | 0.321 (0.117 to 0.525) | 71.9% and 0.001 and 0.002 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | 2 | −0.159 (−0.654 to 0.335) | 0.0% and 0.322 and 0.528 | |
| ≤70% | 7 | 0.083 (−0.087 to 0.252) | 42.1% and 0.110 and 0.339 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | – | – | – | |
| 2 | 4 | −0.097 (−0.476 to 0.282) | 0.0% and 0.860 and 0.617 | |
| 3 | – | – | – | |
| 4 | 2 | 0.341 (−0.269 to 0.952) | 0.0% and 0.482 and 0.273 | |
| 5 | 16 | 0.230 (0.095 to 0.365) | 64.5% and 0.001 and 0.001 | |
| 6 | – | – | – | |
|
| ||||
| AF | No | |||
| Chronic | – | – | – | |
| Non-chronic | 21 | 0.181 (0.049 to 0.314) | 56.3% and 0.001 and 0.007 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 7 | −0.036 (−0.291 to 0.218) | 25.6% and 0.233 and 0.781 | |
| Persistent | 7 | −0.077 (−0.383 to 0.229) | 0.0% and 0.887 and 0.621 | |
| Permanent | – | – | – | |
|
| ||||
| NLR | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 3 | 0.047 (−0.124 to 0.218) | 0.0% and 0.552 and 0.588 | |
| European | 4 | 0.750 (0.565 to 0.936) | 35.1% and 0.201 and 0.001 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | ||||
| Cohort | All of studies: cohort | |||
| Case-control | ||||
|
| ||||
| Number of population | No | |||
| >300 | 2 | 0.035 (−0.142 to 0.212) | 0.0% and 0.340 and 0.698 | |
| ≤300 | 5 | 0.712 (0.533 to 0.891) | 41.9% and 0.142 and 0.001 | |
|
| ||||
| Mean age | Yes, probably | |||
| >60 years | 3 | 0.476 (0.183 to 0.770) | 21.4% and 0.280 and 0.001 | |
| ≤60 years | 4 | 0.346 (0.207 to 0.485) | 90.8% and 0.001 and 0.001 | |
|
| ||||
| Male | No | |||
| >70% | 2 | 0.035 (−0.142 to 0.212) | 0.0% and 0.340 and 0.698 | |
| ≤70% | 3 | 0.804 (0.610 to 0.997) | 0.0% and 0.593 and 0.001 | |
|
| ||||
| Diabetes mellitus | ||||
| >30% | All of studies: ≤30% | |||
| ≤30% | ||||
|
| ||||
| Hypertension | ||||
| >70% | All of studies: ≤70% | |||
| ≤70% | ||||
|
| ||||
| Cigarette smoking | No | |||
| >30% | 2 | 0.851 (0.626 to 1.077) | 0.0% and 0.530 and 0.001 | |
| ≤30% | 3 | 0.476 (0.183 to 0.770) | 21.4% and 0.280 and 0.001 | |
|
| ||||
| Medication: Diuretic | ||||
| >70% | No data | |||
| ≤70% | ||||
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 2 | 0.819 (0.615 to 1.023) | 0.0% and 0.360 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 3 | 0.767 (0.572 to 0.963) | 45.6% and 0.159 and 0.001 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | 0.670 (0.291 to 1.049) | – | |
| ≤70% | 1 | – | ||
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | – | – | – | |
| 2 | 1 | 0.150 (−0.499 to 0.799) | – | |
| 3 | – | – | – | |
| 4 | – | – | – | |
| 5 | 6 | 0.379 (0.250 to 0.507) | – | |
| 6 | – | – | – | |
|
| ||||
| AF | No | |||
| Chronic | – | – | – | |
| Non-chronic | 6 | 0.527 (0.370 to 0.684) | 80% and 0.001 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 2 | 0.670 (0.349 to 0.991) | 0.0% and 1.000 and 0.001 | |
| Persistent | 1 | 0.150 (−0.499 to 0.799) | – | |
| Permanent | – | – | – | |
|
| ||||
| RDW | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 3 | 0.165 (0.051 to 0.279) | 79.1% and 0.008 and 0.005 | |
| European | 2 | 0.803 (0.560 to 1.045) | 0.0% and 0.425 and 0.001 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | No | |||
| Cohort | 4 | 0.264 (0.155 to 0.372) | 90.3% and 0.001 and 0.001 | |
| Case-control | 1 | 0.440 (0.102 to 0.778) | – | |
|
| ||||
| Number of population | No | |||
| >300 | 1 | 0.100 (−0.023 to 0.223) | – | |
| ≤300 | 4 | 0.705 (0.516 to 0.894) | 31.2% and 0.225 and 0.001 | |
|
| ||||
| Mean age | Yes, probably | |||
| >60 years | 3 | 0.165 (0.051 to 0.279) | 79.1% and 0.008 and 0.005 | |
| ≤60 years | 2 | 0.803 (0.560 to 1.045) | 0.0% and 0.425 and 0.001 | |
|
| ||||
| Male | Yes, probably | |||
| >70% | 2 | 0.129 (0.008 to 0.250) | 85.1% and 0.010 and 0.036 | |
| ≤70% | 3 | 0.680 (0.483 to 0.877) | 43.8% and 0.169 and 0.001 | |
|
| ||||
| Diabetes mellitus | ||||
| >30% | All of studies: ≤30% | |||
| ≤30% | ||||
|
| ||||
| Hypertension | ||||
| >70% | ≤70% | |||
| ≤70% | ||||
|
| ||||
| Cigarette smoking | No | |||
| >30% | 3 | 0.680 (0.483 to 0.877) | 43.8% and 0.169 and 0.001 | |
| ≤30% | – | – | – | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | 1 | (0.329 to 1.671) | – | |
| ≤70% | 1 | 0.100 (−0.023 to 0.223) | – | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 3 | 0.165 (0.051 to 0.279) | 79.1% and 0.008 and 0.005 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 1 | 0.440 (0.102 to 0.778) | – | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | 1 | 1.000 (0.329 to 1.671) | – | |
| ≤70% | 2 | 0.140 (0.024 to 0.255) | 70.8% and 0.064 and 0.018 | |
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | – | – | – | |
| 2 | – | – | – | |
| 3 | – | – | – | |
| 4 | 2 | 0.661 (0.460 to 0.861) | 60.3% and 0.113 and 0.001 | |
| 5 | 3 | 0.143 (0.023 to 0.263) | 81.2% and 0.005 and 0.020 | |
| 6 | – | – | – | |
|
| ||||
| AF | ||||
| Chronic | All of studies: non–chronic | |||
| Non-chronic | ||||
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 2 | 0.511 (0.188 to 0.834) | 46.9% and 0.170 to 0.002 | |
| Persistent | – | – | – | |
| Permanent | – | – | – | |
|
| ||||
| Hb | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | 5 | 0.046 (−0.133 to 0.226) | 43.2% and 0.133 and 0.613 | |
| European | 4 | 0.007 (−0.306 to 0.319) | 0.0% and 0.539 and 0.967 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | No | |||
| Cohort | 8 | 0.029 (−0.131 to 0.189) | 23.1% and 0.246 and 0.723 | |
| Case-control | 1 | 0.170 (−0.506 to 0.846) | – | |
|
| ||||
| Number of population | No | |||
| >300 | 2 | 0.095 (−0.099 to 0.288) | 54.4% and 0.139 and 0.336 | |
| ≤300 | 7 | −0.070 (−0.331 to 0.191) | 1.2% and 0.451 and 0.598 | |
|
| ||||
| Mean Age | No | |||
| >60 years | 5 | −0.057 (−0.258 to 0.144) | 3.0% and 0.390 and 0.576 | |
| ≤60 years | 4 | 0.177 (−0.069 to 0.422) | 1.5% and 0.385 and 0.159 | |
|
| ||||
| Male | No | |||
| >70% | 3 | 0.056 (−0.133 to 0.245) | 65.4% and 0.056 and 0.563 | |
| ≤70% | 5 | 0.035 (−0.248 to 0.319) | 0.0% and 0.672 and 0.807 | |
|
| ||||
| Diabetes mellitus | ||||
| >30% | All of studies: ≤30% | |||
| ≤30% | ||||
|
| ||||
| Hypertension | ||||
| >70% | All of studies: ≤70% | |||
| ≤70% | ||||
|
| ||||
| Cigarette smoking | No | |||
| >30% | 4 | 0.070 (−0.233 to 0.374) | 0.0% and 0.582 and 0.650 | |
| ≤30% | 2 | −0.314 (−0.933 to 0.306) | 0.0% and 0.645 and 0.321 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | 1 | −0.800 (−1.706 to 0.106) | – | |
| ≤70% | 1 | 0.00 (−0.231 to 0.231) | – | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 5 | −0.047 (−0.238 to 0.144) | 0.0% and 0.494 and 0.630 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | −0.096 (−0.442 to 0.250) | 0.0% and 0.734 and 0.587 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | 1 | −0.800 (−1.706 to 0.106) | – | |
| ≤70% | 3 | 0.002 (−0.208 to 0.213) | 0.0% and 0.782 and 0.984 | |
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | – | – | – | |
| 2 | – | – | – | |
| 3 | – | – | – | |
| 4 | 2 | 0.236 (−0.161 to 0.632) | 0.0% and 0.814 and 0.244 | |
| 5 | 7 | 0.00 (−0.169 to 0.169) | 25.5% and 0.234 and 0.998 | |
| 6 | – | – | – | |
|
| ||||
| AF | No | |||
| Chronic | – | – | – | |
| Non-chronic | 8 | −0.031 (−0.204 to 0.142) | 0.0% and 0.513 and 0.727 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 3 | −0.070 (−0.531 to 0.391) | 0.0% and 0.603 and 0.766 | |
| Persistent | – | – | – | |
| Permanent | – | – | – | |
Footnotes
Source of support: Departmental sources
References
- 1.Macle L, Cairns J, Leblanc K, et al. 2016 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation. Can J Cardiol. 2016;32:1170–85. doi: 10.1016/j.cjca.2016.07.591. [DOI] [PubMed] [Google Scholar]
- 2.Ali-Hassan-Sayegh S, Mirhosseini SJ, Rezaeisadrabadi M, et al. Antioxidant supplementations for prevention of atrial fibrillation after cardiac surgery: An updated comprehensive systematic review and meta-analysis of 23 randomized controlled trials. Interact Cardiovasc Thorac Surg. 2014;18:646–54. doi: 10.1093/icvts/ivu020. [DOI] [PubMed] [Google Scholar]
- 3.Fuster V, Rydén LE, Cannom DS, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2011;57:e101–98. doi: 10.1016/j.jacc.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 4.Kornej J, Apostolakis S, Bollmann A, Lip GY. The emerging role of biomarkers in atrial fibrillation. Can J Cardiol. 2013;29:1181–93. doi: 10.1016/j.cjca.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 5.Varasteh-Ravan HR, Ali-Hassan-Sayegh S, Shokraneh S, et al. Relationship of admission mean platelet volume, platelet distribution width and white blood cells with ST resolution in patients with acute ST segment elevation myocardial infarction treated with streptokinase without history of previous cardiovascular surgery. Perspect Clin Res. 2013;4:125–29. doi: 10.4103/2229-3485.111792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wells GA SB, O’Connell D, Peterson J, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. 2011. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 8.Gülcihan Balcı K, Maden O, Balcı MM, et al. The association between mean platelet volume and spontaneous echocardiographic contrast or left atrial thrombus in patients with mitral stenosis. Anatol J Cardiol. 2016;16(11):863–67. doi: 10.14744/AnatolJCardiol.2015.6675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gurses KM, Kocyigit D, Yalcin MU, et al. Monocyte toll-like receptor expression in patients with atrial fibrillation. Am J Cardiol. 2016;117:1463–67. doi: 10.1016/j.amjcard.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 10.Karataş MB, Çanga Y, İpek G, et al. Association of admission serum laboratory parameters with new-onset atrial fibrillation after a primary percutaneous coronary intervention. Coron Artery Dis. 2016;27:128–34. doi: 10.1097/MCA.0000000000000333. [DOI] [PubMed] [Google Scholar]
- 11.Korantzopoulos P, Kyrlas K, Liu T, et al. Red blood cell distribution width and atrial fibrillation in patients with sick sinus syndrome. J Cardiol. 2016;67:551–54. doi: 10.1016/j.jjcc.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Akdag S, Simsek H, Sahin M, et al. Association of epicardial adipose tissue thickness and inflammation parameters with CHA2DS2-VASASc score in patients with nonvalvular atrial fibrillation. Ther Clin Risk Manag. 2015;11:1675–81. doi: 10.2147/TCRM.S94955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Akyüz A, Akkoyun DÇ, Değirmenci H, Alp R. Atrial fibrillation is associated with increased mean platelet volume and apnea hypopnea index in patients with obstructive sleep apnea. Angiology. 2015;66:525–30. doi: 10.1177/0003319714548567. [DOI] [PubMed] [Google Scholar]
- 14.Chavarria N, Wong C, Hussain H, et al. Persistent elevation of neutrophil/lymphocyte ratio associated with new onset atrial fibrillation following percutaneous coronary intervention for acute ST segment elevation myocardial infarction. J Ayub Med Coll Abbottabad. 2015;27:441–47. [PubMed] [Google Scholar]
- 15.Drabik L, Wołkow P, Undas A. Denser plasma clot formation and impaired fibrinolysis in paroxysmal and persistent atrial fibrillation while on sinus rhythm: association with thrombin generation, endothelial injury and platelet activation. Thromb Res. 2015;136:408–14. doi: 10.1016/j.thromres.2015.05.028. [DOI] [PubMed] [Google Scholar]
- 16.Acet H, Ertaş F, Akıl MA, et al. New inflammatory predictors for non-valvular atrial fibrillation: Echocardiographic epicardial fat thickness and neutrophil to lymphocyte ratio. Int J Cardiovasc Imaging. 2014;30:81–89. doi: 10.1007/s10554-013-0317-4. [DOI] [PubMed] [Google Scholar]
- 17.Arik OZ, Ozkan B, Kutlu R, et al. Relationship between platelet indices and international normalized ratio in patients with non valvular atrial fibrillation. Platelets. 2014;25:311–16. doi: 10.3109/09537104.2013.821603. [DOI] [PubMed] [Google Scholar]
- 18.Distelmaier K, Maurer G, Goliasch G. Blood count in new onset atrial fibrillation after acute myocardial infarction – a hypothesis generating study. Indian J Med Res. 2014;139:579–84. [PMC free article] [PubMed] [Google Scholar]
- 19.Erdogan D, Uysal BA, Aksoy F, et al. Strict heart rate control attenuates prothrombotic state and platelet activity in patients with non-valvular permanent atrial fibrillation. Clin Hemorheol Microcirc. 2014;56:219–29. doi: 10.3233/CH-131710. [DOI] [PubMed] [Google Scholar]
- 20.Zheng DD, Ji SN, Chen C, et al. Association of Interleukin-10 promotor polymorphisms with atrial fibrillation in Han Chinese. Int J Clin Exp Med. 2014;7:4199–206. [PMC free article] [PubMed] [Google Scholar]
- 21.Xu XF, Jiang FL, Ou MJ, Zhang ZH. The association between mean platelet volume and chronic atrial fibrillation and the presence of thrombotic events. Biomed Rep. 2015;3:388–94. doi: 10.3892/br.2015.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Güngör B, Özcan KS, Erdinler İ, et al. Elevated levels of RDW is associated with non-valvular atrial fibrillation. J Thromb Thrombolysis. 2014;37:404–10. doi: 10.1007/s11239-013-0957-1. [DOI] [PubMed] [Google Scholar]
- 23.Liu T, Shao Q, Miao S, et al. Red cell distribution width as a novel, inexpensive marker for paroxysmal atrial fibrillation. Int J Cardiol. 2014;171:e52–53. doi: 10.1016/j.ijcard.2013.11.112. [DOI] [PubMed] [Google Scholar]
- 24.Sarikaya S, Şahin Ş, Akyol L, et al. Is there any relationship between RDW levels and atrial fibrillation in hypertensive patient? Afr Health Sci. 2014;14:267–72. doi: 10.4314/ahs.v14i1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sonmez O, Ertem FU, Vatankulu MA, et al. Novel fibro-inflammation markers in assessing left atrial remodeling in non-valvular atrial fibrillation. Med Sci Monit. 2014;20:463–70. doi: 10.12659/MSM.890635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ulu SM, Ozkeçeci G, Akci O, et al. Mean platelet volume, in predicting severity of mitral regurgitation and left atrial appendage thrombosis. Blood Coagul Fibrinolysis. 2014;25:119–24. doi: 10.1097/MBC.0b013e328364c453. [DOI] [PubMed] [Google Scholar]
- 27.Berge T, Ulimoen SR, Enger S, et al. Impact of atrial fibrillation on inflammatory and fibrinolytic variables in the elderly. Scand J Clin Lab Invest. 2013;73:326–33. doi: 10.3109/00365513.2013.780093. [DOI] [PubMed] [Google Scholar]
- 28.Ertaş G, Sönmez O, Turfan M, et al. Neutrophil/lymphocyte ratio is associated with thromboembolic stroke in patients with non-valvular atrial fibrillation. J Neurol Sci. 2013;324:49–52. doi: 10.1016/j.jns.2012.09.032. [DOI] [PubMed] [Google Scholar]
- 29.Gungor B, Ekmekci A, Arman A, et al. Assessment of interleukin-1 gene cluster polymorphisms in lone atrial fibrillation: New insight into the role of inflammation in atrial fibrillation. Pacing Clin Electrophysiol. 2013;36:1220–27. doi: 10.1111/pace.12182. [DOI] [PubMed] [Google Scholar]
- 30.Turgut O, Zorlu A, Kilicli F, et al. Atrial fibrillation is associated with increased mean platelet volume in patients with type 2 diabetes mellitus. Platelets. 2013;24:493–97. doi: 10.3109/09537104.2012.725876. [DOI] [PubMed] [Google Scholar]
- 31.Järemo P, Eriksson M, Lindahl TL, et al. Platelets and acute cerebral infarction. Platelets. 2013;24:407–11. doi: 10.3109/09537104.2012.712168. [DOI] [PubMed] [Google Scholar]
- 32.Sahin S, Sarikaya S, Alcelik AY, et al. Neutrophil to lymphocyte ratio is a useful predictor of atrial fibrillation in patients with diabetes mellitus. Acta Med Medit. 2013;29:847–51. [Google Scholar]
- 33.Tekin G, Tekin YK, Sivri N, Yetkin E. Mean platelet volume in patients with nonvalvular atrial fibrillation. Blood Coagul Fibrinolysis. 2013;24:537–39. doi: 10.1097/MBC.0b013e32835facb3. [DOI] [PubMed] [Google Scholar]
- 34.Turfan M, Erdogan E, Ertas G, et al. Usefulness of mean platelet volume for predicting stroke risk in atrial fibrillation patients. Blood Coagul Fibrinolysis. 2013;24:55–58. doi: 10.1097/MBC.0b013e32835a0850. [DOI] [PubMed] [Google Scholar]
- 35.Feng C, Mei W, Luo C, et al. Relationship between mean platelet volume and coronary blood flow in patients with atrial fibrillation. Heart Lung Circ. 2013;22:43–49. doi: 10.1016/j.hlc.2012.08.052. [DOI] [PubMed] [Google Scholar]
- 36.Liu L, Lee J, Fu G, et al. Activation of peripheral blood CD3(+) T-lymphocytes in patients with atrial fibrillation. Int Heart J. 2012;53:221–24. doi: 10.1536/ihj.53.221. [DOI] [PubMed] [Google Scholar]
- 37.Yoshizaki T, Umetani K, Ino Y, et al. Activated inflammation is related to the incidence of atrial fibrillation in patients with acute myocardial infarction. Intern Med. 2012;51:1467–71. doi: 10.2169/internalmedicine.51.7312. [DOI] [PubMed] [Google Scholar]
- 38.Hayashi M, Takeshita K, Inden Y, et al. Platelet activation and induction of tissue factor in acute and chronic atrial fibrillation: Involvement of mononuclear cell-platelet interaction. Thromb Res. 2011;128:e113–18. doi: 10.1016/j.thromres.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 39.Fu R, Wu S, Wu P, Qiu J. A study of blood soluble P-selectin, fibrinogen, and von Willebrand factor levels in idiopathic and lone atrial fibrillation. Europace. 2011;13:31–36. doi: 10.1093/europace/euq346. [DOI] [PubMed] [Google Scholar]
- 40.Liu T, Zhang X, Korantzopoulos P, et al. Uric acid levels and atrial fibrillation in hypertensive patients. Intern Med. 2011;50:799–803. doi: 10.2169/internalmedicine.50.4587. [DOI] [PubMed] [Google Scholar]
- 41.Letsas KP, Korantzopoulos P, Filippatos GS, et al. Uric acid elevation in atrial fibrillation. Hellenic J Cardiol. 2010;51:209–13. [PubMed] [Google Scholar]
- 42.Luan Y, Guo Y, Li S, et al. Interleukin-18 among atrial fibrillation patients in the absence of structural heart disease. Europace. 2010;12:1713–18. doi: 10.1093/europace/euq321. [DOI] [PubMed] [Google Scholar]
- 43.Alberti S, Angeloni G, Tamburrelli C, et al. Platelet-leukocyte mixed conjugates in patients with atrial fibrillation. Platelets. 2009;20:235–41. doi: 10.1080/09537100902954370. [DOI] [PubMed] [Google Scholar]
- 44.Dai S, Zhang S, Guo Yh, et al. C-reactive protein and atrial fibrillation in idiopathic dilated cardiomyopathy. Clin Cardiol. 2009;32:E45–50. doi: 10.1002/clc.20430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ichiki H, Orihara K, Hamasaki S, et al. The role of infection in the development of non-valvular atrial fibrillation: up-regulation of Toll-like receptor 2 expression levels on monocytes. J Cardiol. 2009;53:127–35. doi: 10.1016/j.jjcc.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 46.Yao SY, Chu JM, Chen KP, et al. Inflammation in lone atrial fibrillation. Clin Cardiol. 2009;32:94–98. doi: 10.1002/clc.20290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Colkesen Y, Acil T, Abayli B, et al. Mean platelet volume is elevated during paroxysmal atrial fibrillation: A marker of increased platelet activation? Blood Coagul Fibrinolysis. 2008;19:411–14. doi: 10.1097/MBC.0b013e3283049697. [DOI] [PubMed] [Google Scholar]
- 48.Choudhury A, Chung I, Panja N, et al. Soluble CD40 ligand, platelet surface CD40 ligand, and total platelet CD40 ligand in atrial fibrillation: Relationship to soluble P-selectin, stroke risk factors, and risk factor intervention. Chest. 2008;134:574–81. doi: 10.1378/chest.07-2745. [DOI] [PubMed] [Google Scholar]
- 49.Pirat B, Atar I, Ertan C, et al. Comparison of C-reactive protein levels in patients who do and do not develop atrial fibrillation during electrophysiologic study. Am J Cardiol. 2007;100:1552–55. doi: 10.1016/j.amjcard.2007.06.056. [DOI] [PubMed] [Google Scholar]
- 50.Yip HK, Chang LT, Sun CK, et al. Platelet activation in patients with chronic nonvalvular atrial fibrillation. Int Heart J. 2006;47:371–79. doi: 10.1536/ihj.47.371. [DOI] [PubMed] [Google Scholar]
- 51.Kamath S, Blann AD, Chin BS, Lip GY. Platelet activation, haemorheology and thrombogenesis in acute atrial fibrillation: A comparison with permanent atrial fibrillation. Heart. 2003;89:1093–95. doi: 10.1136/heart.89.9.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kamath S, Chin BS, Blann AD, Lip GY. A study of platelet activation in paroxysmal, persistent and permanent atrial fibrillation. Blood Coagul Fibrinolysis. 2002;13:627–36. doi: 10.1097/00001721-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 53.Kamath S, Blann AD, Chin BS, et al. A study of platelet activation in atrial fibrillation and the effects of antithrombotic therapy. Eur Heart J. 2002;23:1788–95. doi: 10.1053/euhj.2002.3259. [DOI] [PubMed] [Google Scholar]
- 54.Kamath S, Blann AD, Caine GJ, et al. Platelet P-selectin levels in relation to plasma soluble P-selectin and beta-thromboglobulin levels in atrial fibrillation. Stroke. 2002;33:1237–42. doi: 10.1161/01.str.0000013739.82306.7f. [DOI] [PubMed] [Google Scholar]
- 55.Peverill RE, Graham R, Gelman J, et al. Haematologic determinants of left atrial spontaneous echo contrast in mitral stenosis. Int J Cardiol. 2001;81:235–42. doi: 10.1016/s0167-5273(01)00572-1. [DOI] [PubMed] [Google Scholar]
- 56.Kahn SR, Solymoss S, Flegel KM. Nonvalvular atrial fibrillation: Evidence for a prothrombotic state. CMAJ. 1997;157:673–81. [PMC free article] [PubMed] [Google Scholar]
- 57.Lip GY, Lip PL, Zarifis J, et al. Fibrin D-dimer and beta-thromboglobulin as markers of thrombogenesis and platelet activation in atrial fibrillation. Effects of introducing ultra-low-dose warfarin and aspirin. Circulation. 1996;94:425–31. doi: 10.1161/01.cir.94.3.425. [DOI] [PubMed] [Google Scholar]
- 58.Gustafsson C, Blomback M, Britton M, et al. Coagulation factors and the increased risk of stroke in nonvalvular atrial fibrillation. Stroke. 1990;21:47–51. doi: 10.1161/01.str.21.1.47. [DOI] [PubMed] [Google Scholar]
- 59.Li H, Liu T, Xu G, et al. Red blood cell distribution width and the recurrence of atrial fibrillation after ablation in patients with paroxysmal non-valvular symptomatic atrial fibrillation. Int J Cardiol. 2016;203:834–36. doi: 10.1016/j.ijcard.2015.11.077. [DOI] [PubMed] [Google Scholar]
- 60.Yanagisawa S, Inden Y, Kato H, et al. Elevated red blood cell distribution width predicts recurrence after catheter ablation for atrial fibrillation in patients with heart failure – comparison with non-heart failure patients. Circ J. 2016;80:627–38. doi: 10.1253/circj.CJ-15-1152. [DOI] [PubMed] [Google Scholar]
- 61.Aksu T, Baysal E, Guler TE, et al. Predictors of atrial fibrillation recurrence after cryoballoon ablation. J Blood Med. 2015;6:211–17. doi: 10.2147/JBM.S81551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gurses KM, Yalcin MU, Kocyigit D, et al. Red blood cell distribution width predicts outcome of cryoballoon-based atrial fibrillation ablation. J Interv Card Electrophysiol. 2015;42:51–58. doi: 10.1007/s10840-014-9959-y. [DOI] [PubMed] [Google Scholar]
- 63.Karavelioğlu Y, Karapınar H, Yüksel M, et al. Neutrophil to lymphocyte ratio is predictor of atrial fibrillation recurrence after cardioversion with amiodarone. Clin Appl Thromb Hemost. 2015;21:5–9. doi: 10.1177/1076029613518368. [DOI] [PubMed] [Google Scholar]
- 64.Wen SN, Liu N, Li SN, et al. Catheter ablation of atrial fibrillation in patients with rheumatoid arthritis. J Cardiol. 2015;66:320–25. doi: 10.1016/j.jjcc.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 65.Guo X, Zhang S, Yan X, et al. Postablation neutrophil/lymphocyte ratio correlates with arrhythmia recurrence after catheter ablation of lone atrial fibrillation. Chin Med J (Engl) 2014;127:1033–38. [PubMed] [Google Scholar]
- 66.Arıbaş A, Akıllı H, Gül EE, et al. Can neutrophil/lymphocyte ratio predict recurrence of non-valvular atrial fibrillation after cardioversion? Anadolu Kardiyol Derg. 2013;13:123–30. doi: 10.5152/akd.2013.036. [DOI] [PubMed] [Google Scholar]
- 67.Li SB, Yang F, Jing L, et al. Myeloperoxidase and risk of recurrence of atrial fibrillation after catheter ablation. J Investig Med. 2013;61:722–27. doi: 10.2310/JIM.0b013e3182857fa0. [DOI] [PubMed] [Google Scholar]
- 68.Canpolat U, Aytemir K, Yorgun H, et al. Role of preablation neutrophil/lymphocyte ratio on outcomes of cryoballoon-based atrial fibrillation ablation. Am J Cardiol. 2013;112:513–19. doi: 10.1016/j.amjcard.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 69.Im SI, Shin SY, Na JO, et al. Usefulness of neutrophil/lymphocyte ratio in predicting early recurrence after radiofrequency catheter ablation in patients with atrial fibrillation. Int J Cardiol. 2013;168:4398–400. doi: 10.1016/j.ijcard.2013.05.042. [DOI] [PubMed] [Google Scholar]
- 70.He XN, Li SN, Zhan JL, et al. Serum uric acid levels correlate with recurrence of paroxysmal atrial fibrillation after catheter ablation. Chin Med J (Engl) 2013;126:860–64. [PubMed] [Google Scholar]
- 71.Ferro D, Franciosa P, Cangemi R, et al. Serum levels of vitamin E are associated with early recurrence of atrial fibrillation after electric cardioversion. Circ Arrhythm Electrophysiol. 2012;5:327–33. doi: 10.1161/CIRCEP.111.968248. [DOI] [PubMed] [Google Scholar]
- 72.Smit MD, Maass AH, De Jong AM, et al. Role of inflammation in early atrial fibrillation recurrence. Europace. 2012;14:810–17. doi: 10.1093/europace/eur402. [DOI] [PubMed] [Google Scholar]
- 73.Wang H, Liu J, Fang P, et al. Big endothelin-1 as a predictor of atrial fibrillation recurrence after primary ablation only in patients with paroxysmal atrial fibrillation. Herz. 2012;37:919–25. doi: 10.1007/s00059-012-3626-9. [DOI] [PubMed] [Google Scholar]
- 74.Liu J, Fang PH, Dibs S, et al. High-sensitivity C-reactive protein as a predictor of atrial fibrillation recurrence after primary circumferential pulmonary vein isolation. Pacing Clin Electrophysiol. 2011;34:398–406. doi: 10.1111/j.1540-8159.2010.02978.x. [DOI] [PubMed] [Google Scholar]
- 75.Vizzardi E, Nodari S, Zanini G, et al. High sensitivity C-reactive protein: A predictor for recurrence of atrial fibrillation after successful cardioversion. Intern Emerg Med. 2009;4:309–13. doi: 10.1007/s11739-009-0235-6. [DOI] [PubMed] [Google Scholar]
- 76.Letsas KP, Weber R, Bürkle G, et al. Pre-ablative predictors of atrial fibrillation recurrence following pulmonary vein isolation: The potential role of inflammation. Europace. 2009;11:158–63. doi: 10.1093/europace/eun309. [DOI] [PubMed] [Google Scholar]
- 77.Korantzopoulos P, Kolettis TM, Kountouris E, et al. Variation of inflammatory indexes after electrical cardioversion of persistent atrial fibrillation. Is there an association with early recurrence rates? Int J Clin Pract. 2005;59:881–85. doi: 10.1111/j.1368-5031.2005.00569.x. [DOI] [PubMed] [Google Scholar]
- 78.Tan C, OuYang M, Kong D, Zhou X. Association between the left atrial and left atrial appendages systole strain rate in patients with atrial fibrillation. Med Sci Monit. 2016;22:4974–77. doi: 10.12659/MSM.901831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hu X, Jiang J, Ma Y, Tang A. Novel P wave indices to predict atrial fibrillation recurrence after radiofrequency ablation for paroxysmal atrial fibrillation. Med Sci Monit. 2016;22:2616–23. doi: 10.12659/MSM.896675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sabashnikov A, Weymann A, Haldar S, et al. Position of totally thoracoscopic surgical ablation in the treatment of atrial fibrillation: An alternative method of conduction testing. Med Sci Monit Basic Res. 2015;21:76–80. doi: 10.12659/MSMBR.894239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mirhosseini SJ, Ali-Hassan-Sayegh S, Forouzannia SK. What is the exact predictive role of preoperative white blood cell count for new-onset atrial fibrillation following open heart surgery? Saudi J Anaesth. 2013;7:40–42. doi: 10.4103/1658-354X.109807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: A link Between thrombosis and inflammation? Curr Pharm Des. 2011;17:47–58. doi: 10.2174/138161211795049804. [DOI] [PubMed] [Google Scholar]
- 83.Ünübol M, Ayhan M, Güney E. The relationship between mean platelet volume with microalbuminuria and glycemic control in patients with type II diabetes mellitus. Platelets. 2012;23:475–80. doi: 10.3109/09537104.2011.634934. [DOI] [PubMed] [Google Scholar]
- 84.Sansanayudh N, Anothaisintawee T, Muntham D, et al. Mean platelet volume and coronary artery disease: a systematic review and meta-analysis. Int J Cardiol. 2014;175:433–40. doi: 10.1016/j.ijcard.2014.06.028. [DOI] [PubMed] [Google Scholar]
- 85.Joseph P, Ishai A, MacNabb M, et al. Atrial fibrillation is associated with hematopoietic tissue activation and arterial inflammation. Int J Cardiovasc Imaging. 2016;32:113–19. doi: 10.1007/s10554-015-0766-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chatterjee S, Chandra P, Guha G, et al. Pre-procedural elevated white blood cell count and neutrophil-lymphocyte (N/L) ratio are predictors of ventricular arrhythmias during percutaneous coronary intervention. Cardiovasc Hematol Disord Drug Targets. 2011;11:58–60. doi: 10.2174/187152911798346981. [DOI] [PubMed] [Google Scholar]
- 87.Uthamalingam S, Patvardhan EA, Subramanian S, et al. Utility of the neutrophil to lymphocyte ratio in predicting long-term outcomes in acute decompensated heart failure. Am J Cardiol. 2011;107:433–38. doi: 10.1016/j.amjcard.2010.09.039. [DOI] [PubMed] [Google Scholar]
- 88.Evans TC, Jehle D. The red blood cell distribution width. J Emerg Med. 1991;9(Suppl 1):71–74. doi: 10.1016/0736-4679(91)90592-4. [DOI] [PubMed] [Google Scholar]
- 89.van Kimmenade RR, Mohammed AA, Uthamalingam S, et al. Red blood cell distribution width and 1-year mortality in acute heart failure. Eur J Heart Fail. 2010;12:129–36. doi: 10.1093/eurjhf/hfp179. [DOI] [PubMed] [Google Scholar]
- 90.Dabbah S, Hammerman H, Markiewicz W, Aronson D. Relation between red cell distribution width and clinical outcomes after acute myocardial infarction. Am J Cardiol. 2010;105:312–17. doi: 10.1016/j.amjcard.2009.09.027. [DOI] [PubMed] [Google Scholar]
- 91.Tonelli M, Sacks F, Arnold M, et al. Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation. 2008;117:163–68. doi: 10.1161/CIRCULATIONAHA.107.727545. [DOI] [PubMed] [Google Scholar]
- 92.Westenbrink BD, Alings M, Connolly SJ, et al. Anemia predicts thromboembolic events, bleeding complications and mortality in patients with atrial fibrillation: Insights from the RE-LY trial. J Thromb Haemost. 2015;13:699–707. doi: 10.1111/jth.12874. [DOI] [PubMed] [Google Scholar]
- 93.Lip GY, Lowe GD, Rumley A, Dunn FG. Increased markers of thrombogenesis in chronic atrial fibrillation: Effects of warfarin treatment. Br Heart J. 1995;73:527–33. doi: 10.1136/hrt.73.6.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Weymann A, Ali-Hasan-Al-Saegh S, Sabashnikov A, et al. Platelets cellular and functional characteristics in patients with atrial fibrillation: a comprehensive meta-analysis and systematic review. Med Sci Monit Basic Res. 2017;23:58–86. doi: 10.12659/MSMBR.902557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Weymann A, Sabashnikov A, Ali-Hasan-Al-Saegh S, et al. Predictive role of coagulation, fibrinolytic, and endothelial markers in patients with atrial fibrillation, stroke, and thromboembolism: a meta-analysis, meta-regression, and systematic review. Med Sci Monit Basic Res. 2017;23:97–140. doi: 10.12659/MSMBR.902558. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1.
Included, and excluded studies according to primary hematological parameters.
| Clinical outcomes and biomarkers | Studies were identified and screened [n] | Studies were excluded according to title, abstract or full text (Secondary exclude) [n] | Studies were included [n] | Data for occurrence and recurrence [n] |
|---|---|---|---|---|
| Platelet count | 292 | 254 | 38 approved articles with totally 52 enrolled data for meta-analysis (48 studies |
Occurrence: 48 Recurrence: 4 |
| Mean platelet volume | 147 | 129 | 18 approved articles with totally 24 enrolled data for meta-analysis |
Occurrence: 23 Recurrence: 1 |
| Platelet distribution width | 11 | 9 | 2 approved articles with totally 3 enrolled data for meta-analysis |
Occurrence: 3 Recurrence: 0 |
| White blood cell | 348 | 299 | 49 approved articles with totally 64 enrolled data for meta-analysis |
Occurrence: 42 Recurrence: 22 |
| Neutrophil to lymphocyte ratio | 41 | 26 | 15 approved articles with totally 17 enrolled data for meta-analysis |
Occurrence: 10 Recurrence: 7 |
| Red blood cell | 83 | 81 | 2 approved articles with totally 2 enrolled data for meta-analysis |
Occurrence: 2 Recurrence: 0 |
| Red blood cell distribution width | 49 | 38 | 11 approved articles with totally 13 enrolled data for meta-analysis |
Occurrence: 8 Recurrence: 5 |
Supplementary Table 2.
Extra details of characteristics of each study for exploration of heterogeneity factors.
| First Author | Geographic Area | Total N | Total age | Total male | Total DM | Total HTN | Total CS | Total Diuretic | Total ACEI | Total. Statin | Total BB | AC-code | Chronic or not |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Occurrence of AF | |||||||||||||
| Balci (Male subjects) [8] | European | 35 | ND | 100 | ND | ND | ND | ND | ND | ND | ND | 5 | ND |
| Balci (Female subjects) [8] | European | 153 | ND | 0 | ND | ND | ND | ND | ND | ND | ND | 5 | ND |
| Gurses [9] | European | 172 | 56.5 | 52.35 | 13.95 | 51.75 | ND | ND | ND | ND | ND | 5 | Non-chronic |
| Karatas [10] | European | 621 | 61.05 | 72.5 | 23 | 45.5 | 64 | ND | ND | 0 | ND | 2 | Non-chronic |
| Korantzopoulos [11] | European | 101 | 76.5 | 46.5 | 27.5 | 88.5 | ND | ND | ND | ND | ND | 3 | Non-chronic |
| Akdag [12] | European | 148 | 64.05 | 60 | 16.5 | 22 | 23.5 | ND | ND | ND | ND | 6 | Combined types |
| Akyuz [13] | European | 90 | 62.25 | 72.25 | 29 | 42.5 | 34.25 | 14.5 | 20.75 | 32.5 | 23 | 4 | Combined types |
| Chavaria [14] | North America | 290 | 65.65 | 74.5 | 29.05 | 65.65 | 55.05 | ND | ND | ND | ND | 5 | ND |
| Drabik (Persistent AF) [15] | European | 97 | 60.1 | 64.975 | 20 | 48.85 | 22.85 | ND | 52.25 | 53.15 | 60.6 | 4 | Non-chronic |
| Drabik (Paroxysmal AF) [15] | European | 91 | 60 | 55.15 | 16.4 | 46.05 | 20 | ND | 54.05 | 47.45 | 57.25 | 4 | Non-chronic |
| Acet (Paroxysmal AF) [16] | European | 134 | 62.05 | 44 | 16.5 | 18 | 21.5 | ND | ND | ND | ND | 5 | Non-chronic |
| Acet (Persistent and permanent AF) [16] | European | 126 | 62.85 | 43.5 | 21.5 | 24 | 28.5 | ND | ND | ND | ND | 5 | Combined types |
| Arik (effective INR) [17] | European | 248 | 69.65 | 40.7 | 6.05 | 68.95 | 13.7 | 27 | 59.25 | ND | 59.7 | 5 | chronic |
| Arik (ineffective INR) [17] | European | 248 | 69.45 | 37.9 | 6.85 | 65.35 | 12.1 | 24.2 | 55.65 | ND | 61.3 | 5 | chronic |
| Distelmaier [18] | North America | 198 | 73.5 | 61 | 24 | 60.5 | ND | ND | ND | ND | ND | 5 | Non-chronic |
| Erdogan (with normal ventricular rate) [19] | European | 67 | 69.55 | 49.28 | 10 | 65 | 6 | 17 | 53.5 | 10 | 43.3 | 3 | chronic |
| Erdogan (with high ventricular rate) [19] | European | 63 | 68.8 | 49.055 | 13.3 | 56.5 | 8 | 25 | 52 | 3.5 | 43.3 | 3 | chronic |
| Zheng [20] | Asian | 217 | 61.735 | 58.63 | 10.84 | 49.275 | 32.74 | ND | ND | ND | ND | 5 | ND |
| Xu (without thrombotic events) [21] | Asian | 115 | 66.095 | 50.45 | 37.4 | 53.1 | 38.25 | ND | 42.6 | 29.55 | 43.55 | 4 | chronic |
| Xu (with thrombotic events) [21] | Asian | 115 | 67.975 | 51.3 | 36.5 | 57.5 | 31.25 | ND | 40.8 | 26.05 | 40.95 | 4 | chronic |
| Gungor [22] | European | 177 | 47.2 | 57.8 | 3.35 | 14.75 | 23.15 | ND | ND | ND | 10.6 | 3 | ND |
| Liu [23] | Asian | 234 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 5 | Non-chronic |
| Sarikaya [24] | European | 126 | 71.03 | 50 | 38 | 100 | ND | ND | ND | ND | ND | 5 | ND |
| Sonmez [25] | European | 85 | 70 | 37 | 24.21 | 63.255 | ND | 14.16 | 47.17 | 15.41 | 35.6 | 4 | Non-chronic |
| Ulu [26] | European | 57 | ND | ND | 0 | 0 | ND | ND | ND | ND | ND | 5 | ND |
| Berge [27] | European | 189 | 75 | 71.025 | 8 | 48 | ND | 19 | 21 | 34.5 | 28 | 4 | Combined types |
| Ertas (without stroke) [28] | European | 111 | 53.5 | 51 | 8.5 | 32.5 | 2 | ND | 17 | ND | 30 | 3 | ND |
| Ertas (with stroke) [28] | European | 63 | 54.5 | 47 | 10 | 47 | 5 | ND | 24 | ND | 16.5 | 3 | ND |
| Gungor [29] | European | 140 | 42.55 | 66.4 | 0 | 0 | 31 | ND | ND | ND | ND | 5 | ND |
| Turgut [30] | European | 162 | 63 | 52 | 100 | 65.5 | 41.5 | 6.5 | 23.5 | 18 | 16.5 | 4 | chronic |
| Jaremo (healthy control) [31] | European | 82 | 67.5 | 66.73 | 5.17 | 21.55 | 2.585 | 18.9 | 13.79 | 14.655 | 41.3 | 4 | ND |
| Jaremo (disease control) [31] | European | 130 | 71.5 | 68.1 | 12.75 | 43.75 | 9.485 | 28.65 | 26.25 | 25.05 | 55.92 | 4 | ND |
| Sahin [32] | European | 144 | 64.865 | 49.75 | 100 | 66.5 | 44.5 | ND | ND | ND | ND | 5 | Non-chronic |
| Tekin [33] | European | 219 | 73.5 | 35.5 | 13.5 | 68.5 | 19 | ND | ND | ND | ND | 5 | chronic |
| Turfan (without stroke) [34] | European | 135 | 59.5 | 54.55 | 15.6 | 33.1 | 55.5 | ND | ND | ND | ND | 4 | ND |
| Turfan (with stroke) [34] | European | 121 | 62.5 | 52.05 | 24.6 | 27 | 50.6 | ND | ND | ND | ND | 4 | ND |
| Feng [35] | Asian | 374 | 65.8 | 61.75 | 17.65 | 53.2 | 25.65 | 23 | 41.95 | 44.85 | 42.5 | 4 | ND |
| Liu (Paroxysmal AF) [36] | Asian | 101 | 64.35 | 62.5 | 5 | 32.5 | ND | ND | 21 | 15 | 34 | 3 | Non-chronic |
| Liu (Persistent AF) [36] | Asian | 107 | 65.8 | 61 | 6.5 | 35 | ND | ND | 29 | 13.5 | 35 | 3 | Non-chronic |
| Yoshizaki [37] | Asian | 176 | 70 | 76 | 32 | 65 | 52.5 | ND | 37.55 | 38.85 | 10.6 | 5 | Non-chronic |
| Hayashi (Paroxysmal AF) [38] | Asian | 27 | 57.95 | 92.5 | 14.5 | 48.5 | ND | ND | 40.5 | 26 | ND | 2 | Non-chronic |
| Hayashi (Chronic AF) [38] | Asian | 27 | 61.45 | 92.5 | 11.05 | 52 | ND | ND | 37 | 26 | ND | 2 | chronic |
| Fu [39] | Asian | 169 | 54.45 | 63.5 | ND | ND | 42.45 | ND | ND | 12.9 | 6.1 | 4 | Combined types |
| Liu [40] | Asian | 451 | 58.35 | 51.435 | ND | 100 | 23.7 | 14.85 | 71.55 | 61.15 | 42.7 | 5 | Combined types |
| Letsas (Paroxysmal AF) [41] | European | 93 | 64.35 | 59 | 6 | 60.5 | ND | ND | 43 | 15.5 | 34 | 5 | Non-chronic |
| Letsas (Permanent AF) [41] | European | 89 | 66.6 | 59.5 | 11 | 63 | ND | ND | 52.5 | 13.5 | 35.5 | 5 | chronic |
| Luan (Persistent AF) [42] | Asian | 53 | 53.25 | 50.855 | 0 | 26.21 | 30.2 | ND | ND | ND | ND | 5 | Non-chronic |
| Luan (Paroxysmal AF) [42] | Asian | 55 | 50.99 | 52.385 | 0 | 24.93 | 30.9 | ND | ND | ND | ND | 5 | Non-chronic |
| Alberti [43] | European | 51 | 64.45 | 47.05 | ND | ND | ND | ND | ND | ND | ND | 1 | Non-chronic |
| Dai [44] | Asian | 522 | 53.065 | 74.7 | 6.1 | 17 | ND | ND | ND | ND | ND | 5 | Non-chronic |
| Ichiki [45] | Asian | 72 | 51.5 | 80.205 | 16 | 37.5 | ND | ND | 8 | 15 | ND | 5 | Non-chronic |
| Yao (Persistent AF) [46] | Asian | 150 | 54.1 | 76.8 | 7.4 | 0 | 42.4 | ND | ND | 8.1 | 13.2 | 4 | Non-chronic |
| Yao (Paroxysmal AF) [46] | Asian | 339 | 53.35 | 74.95 | 4.25 | 0 | 46.55 | ND | ND | 6.6 | 7.85 | 4 | Non-chronic |
| Colkesen [47] | European | 190 | 54 | 38 | 18.5 | 41.5 | ND | ND | ND | 28 | ND | 4 | Non-chronic |
| Choudhury (disease control) [48] | European | 192 | 63.31 | 74 | 10.5 | 66.4 | ND | 33.15 | 55.7 | 46.5 | 43.7 | 4 | ND |
| Choudhury (healthy control) [48] | European | 177 | 62.305 | 72 | 4.1 | 31.8 | ND | 17.75 | 26.85 | 14.45 | 21.9 | 4 | ND |
| Pirat [49] | European | 39 | 49.5 | 51.5 | 8 | 26.5 | 32 | ND | 24.5 | ND | 38 | 5 | Non-chronic |
| Yip [50] | Asian | 82 | 65.75 | 63.05 | 9.7 | 34.7 | 5.65 | ND | 23.4 | 15.3 | ND | 3 | chronic |
| Kamath (Paroxysmal and persistent AF) [51] | European | 62 | 63.5 | 51.6 | ND | ND | ND | ND | ND | ND | ND | 1 | Non-chronic |
| Kamath (Permanent AF) [51] | European | 124 | 66 | 52.65 | ND | ND | ND | ND | ND | ND | ND | 1 | chronic |
| Kamath (Paroxysmal AF) [52] | European | 58 | 63 | 48.27 | 6.85 | 24.135 | 5.17 | ND | ND | ND | ND | 4 | Non-chronic |
| Kamath (Permanent AF) [52] | European | 116 | 65 | 52.29 | 5.15 | 30.45 | 5.17 | ND | ND | ND | ND | 4 | chronic |
| Kamath [53] | European | 143 | 70 | 54.18 | 5.375 | 29.565 | ND | ND | ND | ND | ND | 1 | ND |
| Kamath [54] | European | 57 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 1 | chronic |
| Peverill [55] | Oceania | 163 | 55 | 84.6 | ND | ND | ND | ND | ND | ND | ND | 5 | ND |
| Kahn (without stroke) [56] | North America | 81 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 1 | chronic |
| Kahn (with stroke) [56] | North America | 36 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 1 | chronic |
| Lip [57] | European | 77 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 1 | chronic |
| Gustafsson (without stroke) [58] | European | 40 | 77 | ND | 10 | 25 | 25 | ND | ND | ND | ND | 1 | ND |
| Gustafsson (with stroke) [58] | European | 40 | 77 | ND | 12.5 | 27.5 | 30 | ND | ND | ND | ND | 1 | ND |
| Recurrence of AF | |||||||||||||
| Gurses [9] | European | 86 | 56.8 | 57.7 | 15.8 | 48.55 | ND | ND | 21.2 | 16.5 | ND | 5 | Non-chronic |
| Hongliang Li [59] | Asian | 104 | 62.5 | 43.9 | 24.45 | 46.1 | 37.45 | ND | 41 | 49.65 | 42.4 | 4 | Non-chronic |
| Yanagisawa (without heart failure) [60] | Asian | 678 | 61.1 | 76 | 12.5 | 46 | ND | 3.5 | 35 | ND | 31.5 | 5 | Non-chronic |
| Yanagisawa (with heart failure) [60] | Asian | 79 | 63.6 | 74.5 | 20 | 38 | ND | 77.5 | 58 | ND | 81.5 | 5 | Non-chronic |
| Aksu [61] | European | 49 | 59.65 | 52.5 | 16.5 | 48.5 | 47 | ND | ND | ND | ND | 5 | Non-chronic |
| Gurses [62] | European | 299 | 55.7 | 51.15 | 13.2 | 42.4 | 31 | ND | ND | ND | ND | 4 | Non-chronic |
| Karavelioglu [63] | European | 218 | 64.4 | 41.095 | 18 | 58.5 | 21 | ND | 23.5 | 10.5 | 67 | 5 | Non-chronic |
| Wen [64] | Asian | 75 | 63.62 | ND | 7.5 | 57.5 | 20 | ND | ND | 30 | ND | 5 | Non-chronic |
| Guo Xueyuan [65] | Asian | 379 | 49.665 | 73.55 | 0 | 0 | ND | ND | ND | ND | ND | 5 | ND |
| Aribas [66] | European | 149 | 60 | ND | 29 | 62.5 | 18.5 | ND | ND | ND | ND | 2 | Non-chronic |
| Bing Li [67] | Asian | 288 | 57 | 71.1 | 28.65 | 55.05 | 38.15 | ND | 38 | 14.2 | 27.7 | 5 | Non-chronic |
| Canpolat [68] | European | 251 | 55.2 | 54.85 | 15.15 | 44.35 | 36.55 | ND | 51.25 | 18.05 | ND | 5 | Non-chronic |
| Im [69] | Asian | 499 | 56.4 | 73.65 | 15.55 | 43.9 | ND | ND | ND | ND | ND | 5 | Non-chronic |
| Xiao-nan HE [70] | Asian | 330 | 59.5 | 66.3 | ND | 48.65 | ND | ND | 50 | 14 | 52 | 5 | Non-chronic |
| Ferro [71] | European | 144 | 70.95 | 56.5 | 14 | 87.5 | 5 | ND | 46.5 | 22.5 | ND | 2 | Non-chronic |
| Smit [72] | European | 100 | 64 | 73.8 | 11.9 | 65.95 | 15 | 41.2 | 69.05 | 36.65 | 89.3 | 5 | Non-chronic |
| Wang (Paroxysmal AF) [73] | Asian | 103 | 57.5 | 34.8 | ND | 41.65 | ND | ND | ND | ND | 4.24 | 5 | Non-chronic |
| Wang (Persistent AF) [73] | Asian | 55 | 52.5 | 74.65 | ND | 50.35 | ND | ND | ND | ND | 5.65 | 5 | Non-chronic |
| Liu (Paroxysmal AF) [74] | Asian | 77 | 56 | 75.6 | ND | 37.3 | ND | ND | ND | ND | ND | 2 | Non-chronic |
| Liu (Persistent AF) [74] | Asian | 44 | 53.05 | 84.85 | ND | 51.2 | ND | ND | ND | ND | ND | 2 | Non-chronic |
| Vizzardi [75] | European | 106 | 69 | 61 | 12.05 | ND | ND | ND | 8 | ND | ND | 5 | Non-chronic |
| Letsas [76] | European | 72 | 54.55 | 81.5 | 21.5 | 21.5 | ND | ND | 23 | 14.5 | ND | 5 | Non-chronic |
| Korantzopoulos [77] | European | 30 | 68.5 | 48.39 | 7.1 | 64.25 | 4.75 | 30.95 | 35.7 | 5.55 | ND | 5 | Non-chronic |
Supplementary Table 3.
Subgroup-analysis.
| Subgroup | Studies (N) | WMD (95% CI) | I-squared and Heterogeneity-P-value and Effect-P-value respectively | Is this general item as heterogeneity factor? 1.Yes, probably 2. No |
|---|---|---|---|---|
| Occurrence of AF | ||||
|
| ||||
| Platelet count | ||||
|
| ||||
| Year of Publication | No | |||
| >2000 | 43 | −23.75 (−25.22 to −22.29) | 91% and 0.001 and 0.001 | |
| ≤2000 | 5 | −56.50 (−61.45 to −51.55) | 90.7% and 0.001 and 0.001 | |
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 7 | −3.88 (−10.98 to 3.22) | 13.8% and 0.324 and 0.284 | |
| European | 36 | −29.41 (−30.95 to −27.88) | 93.7% and 0.001 and 0.001 | |
| Africa | – | – | – | |
| North American | 4 | −12.11 (−16.25 to −7.96) | 0.0% and 0.476 and 0.001 | |
| South American | – | – | – | |
| Australia | 1 | −23 (−40.50 to −5.49) | – | |
|
| ||||
| Design of study | No | |||
| Cohort | 8 | −29.09 (−31.01 to −27.16) | 92.4% and 0.001 and 0.001 | |
| Case-control | 40 | −23.30 (−25.36 to −21.25) | 93% and 0.001 and 0.001 | |
|
| ||||
| Number of population | No | |||
| >300 | 2 | −6.33 (−19.68 to 7.03) | 0.0% and 0.689 and 0.353 | |
| ≤300 | 46 | −26.61 (−28.02 to −25.20) | 93.1% and 0.001 and 0.001 | |
|
| ||||
| Mean age | No | |||
| >60 years | 35 | −27.69 (−29.13 to −26.25) | 94% and 0.001 and 0.001 | |
| ≤60 years | 8 | −2.68 (−9.46 to 4.10) | 78.4% and 0.001 and 0.438 | |
|
| ||||
| Male | No | |||
| >70% | 9 | −29.76 (−31.69 to −27.83) | 83.8% and 0.001 and 0.001 | |
| ≤70% | 32 | −15.69 (−17.94 to −13.43) | 90.5% and 0.001 and 0.001 | |
|
| ||||
| Diabetes mellitus | Yes, probably | |||
| >30% | 3 | −0.27 (−9.57 to 9.01) | 35.9% and 0.210 and 0.953 | |
| ≤30% | 35 | −24.77 (−26.27 to −23.26) | 92.2% and 0.001 and 0.001 | |
|
| ||||
| Hypertension | No | |||
| >70% | – | – | – | |
| ≤70% | 39 | −24.91 (−26.38 to −23.44) | 92.5% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | No | |||
| >30% | 10 | −16.36 (−21.68 to −11.04) | 92.8% and 0.001 and 0.001 | |
| ≤30% | 20 | −22.62 (−25.67 to −19.56) | 92.4% and 0.001 and 0.001 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 13 | −28.39 (−30.26 to −26.52) | 85.7% and 0.001 and 0.001 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 22 | −25.47 (−27.18 to −23.76) | 86.5% and 0.001 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 21 | −25.33 (−27.06 to −23.61) | 88% and 0.001 and 0.001 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 21 | −25.36 (−27.06 to −23.66) | 86.6% and 0.001 and 0.001 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | 10 | −52.72 (−56.32 to −49.12) | 92.3% and 0.001 and 0.001 | |
| 2 | 3 | 1.69 (−17.11 to 20.53) | 67.3% and 0.047 and 0.860 | |
| 3 | 6 | −10.36 (−21.43 to 0.69) | 0.0% and 0.703 and 0.066 | |
| 4 | 19 | −24.85 (−26.58 to −23.13) | 91.6% and 0.001 and 0.001 | |
| 5 | 9 | −11.38 (−14.88 to −7.88) | 36.4% and 0.127 and 0.001 | |
| 6 | 1 | 17.40 (−6.03 to 40.83) | – | |
|
| ||||
| AF | Yes, probably | |||
| Chronic | 16 | −2.80 (−7.77 to 2.16) | 18.1% and 0.246 and 0.268 | |
| Non-chronic | 11 | −20.88 (−23.55 to −18.20) | 95.7% and 0.001 and 0.001 | |
|
| ||||
| Type of AF | Yes, probably | |||
| Paroxysmal | 5 | −3.72 (−9.24 to 1.79) | 72.1% and 0.006 and 0.186 | |
| Persistent | 3 | −41.93 (−46.40 to −37.46) | 97.4% and 0.001 and 0.001 | |
| Permanent | 6 | −5.09 (−11.96 to 1.78) | 55.3% and 0.048 and 0.147 | |
|
| ||||
| Mean platelet volume | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | 3 | 1.37 (1.16 to 1.58) | 95.9% and 0.001 and 0.001 | |
| European | 19 | 0.39 (0.35 to 0.43) | 95.2% and 0.001 and 0.001 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | 1 | −0.20 (−0.63 to 0.23) | – | |
|
| ||||
| Design of study | No | |||
| Cohort | 4 | 1.37 (1.14 to 1.60) | 94.7% and 0.001 and 0.001 | |
| Case-control | 19 | 0.39 (0.35 to 0.43) | 95.4% and 0.001 and 0.001 | |
|
| ||||
| Number of population | Yes, probably | |||
| >300 | 2 | 0.90 (0.67 to 1.13) | 0.0% and 0.666 and 0.001 | |
| ≤300 | 21 | 0.41 (0.36 to 0.45) | 96% and 0.001 and 0.001 | |
|
| ||||
| Mean age | No | |||
| >60 years | 16 | 0.58 (0.54 to 0.63) | 94.1and 0.001 and 0.001 | |
| ≤60 years | 4 | 0.23 (0.05 to 0.42) | 93.5% and 0.001 and 0.012 | |
|
| ||||
| Male | No | |||
| >70% | 6 | 0.59 (0.46 to 0.71) | 93.9% and 0.001 and 0.001 | |
| ≤70% | 16 | 0.40 (0.36 to 0.44) | 96.4% and 0.001 and 0.001 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | 4 | 0.63 (0.57 to 0.69) | 96.8% and 0.001 and 0.001 | |
| ≤30% | 16 | 0.49 (0.42 to 0.57) | 92.7% and 0.001 and 0.001 | |
|
| ||||
| Hypertension | No | |||
| >70% | – | – | – | |
| ≤70% | 20 | 0.58 (0.53 to 0.62) | 93.8% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | No | |||
| >30% | 8 | 0.68 (0.62 to 0.74) | 94.7% and 0.001 and 0.001 | |
| ≤30% | 8 | 0.37 (0.28 to 0.45) | 92.1% and 0.001 and 0.001 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 9 | 0.54 (0.49 to 0.59) | 94.3% and 0.001 and 0.001 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 11 | 0.57 (0.52 to 0.62) | 95.8% and 0.001 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 11 | 0.66 (0.60 to 0.71) | 94.7% and 0.001 and 0.001 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 12 | 0.55 (0.50 to 0.60) | 95.8% and 0.001 and 0.001 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | – | – | – | |
| 2 | 1 | 0.80 (0.26 to 1.33) | – | |
| 3 | 3 | 0.081 (−0.109 to 0.272) | 66.1% and 0.053 and 0.404 | |
| 4 | 10 | 0.67 (0.62 to 0.73) | 95.1% and 0.001 and 0.001 | |
| 5 | 8 | 0.108 (0.046 to 0.17) | 93.6% and 0.001 and 0.001 | |
| 6 | 1 | 1.10 (0.75 to 1.45) | – | |
|
| ||||
| AF | No | |||
| Chronic | 8 | 0.55 (0.49 to 0.60) | 95.7% and 0.001 and 0.001 | |
| Non-chronic | 3 | 0.85 (0.58 to 1.13) | 88.6% and 0.001 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 1 | 1.70 (1.20. to 2.19) | – | |
| Persistent | 1 | 0.32 (−0.09 to 0.73) | – | |
| Permanent | 4 | 0.28 (0.17 to 0.38) | 91.7% and 0.001 and 0.001 | |
|
| ||||
| WBC | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | 15 | 0.001 (−0.058 to 0.06) | 80.8% and 0.001 and 0.973 | |
| European | 25 | −0.05 (−0.13 to 0.023) | 89.3% and 0.001 and 0.159 | |
| Africa | – | – | – | |
| North American | 2 | 0.828 (0.46 to 1.187) | 0.0% and 0.365 and 0.001 | |
| South American | – | – | ||
| Australia | – | – | ||
|
| ||||
| Design of study | Yes, probably | |||
| Cohort | 4 | 0.370 (−0.083 to 0.823) | 13.2% and 0.326 and 0.109 | |
| Case-control | 38 | −0.009 (−0.057 to 0.039) | 88.2% and 0.001 and 0.708 | |
|
| ||||
| Number of population | No | |||
| >300 | 5 | 0.035 (−0.047 to 0.117) | 84.8% and 0.001 and 0.403 | |
| ≤300 | 37 | −0.025 (−0.083 to 0.033) | 87.7% and 0.001 and 0.398 | |
|
| ||||
| Mean age | No | |||
| >60 years | 27 | −0.060 (−0.140 to 0.019) | 88.3% and 0.001 and 0.136 | |
| ≤60 years | 15 | 0.025 (−0.033 to 0.084) | 85.2% and 0.001 and 0.397 | |
|
| ||||
| Male | No | |||
| >70% | 11 | 0.009 (−0.051 to 0.070) | 86.4% and 0.001 and 0.761 | |
| ≤70% | 31 | −0.027 (−0.102 to 0.048) | 87.8% and 0.001 and 0.481 | |
|
| ||||
| Diabetes mellitus | Yes, probably | |||
| >30% | 2 | 0.216 (−0.419 to 0.852) | 0.0% and 0.789 and 0.505 | |
| ≤30% | 38 | 0.055 (0.005 to 0.104) | 85% and 0.001 and 0.030 | |
|
| ||||
| Hypertension | Yes, probably | |||
| >70% | 2 | −0.743 (−0.952 to −0.535) | 0.0% and 0.873 and 0.001 | |
| ≤70% | 39 | 0.097 (0.046 to 0.147) | 80.5% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | Yes, probably | |||
| >30% | 11 | 0.053 (−0.010 to 0.115) | 26.4% and 0.193 and 0.102 | |
| ≤30% | 16 | 0.231 (0.123 to 0.339) | 83.9% and 0.001 and 0.001 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 8 | 0.061 (−0.102 to 0.224) | 41.9% and 0.099 and 0.464 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | 1 | −0.70 (−1.269 to −0.131) | – | |
| ≤70% | 21 | 0.012 (−0.086 to 0.111) | 83.2% and 0.001 and 0.804 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 21 | −0.00 (−0.057 to 0.506) | 81.8% and 0.001 and 0.990 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 21 | 0.071 (0.015 to 0.127) | 76.2% and 0.001 and 0.012 | |
|
| ||||
| Anti-coagulant status codes | Yes, Probably | |||
| 1 | 1 | −0.70 (−0.875 to −0.525) | – | |
| 2 | 3 | 0.661 (−0.627 to 1.949) | 0.0% and 0.924 and 0.314 | |
| 3 | 9 | −0.232 (−0.397 to −0.067) | 85.4% and 0.001 and 0.006 | |
| 4 | 8 | 0.054 (−0.006 to 0.115) | 87.6% and 0.001 and 0.077 | |
| 5 | 20 | 0.132 (0.030 to 0.233) | 85% and 0.001 and 0.011 | |
| 6 | 1 | 0.400 (−0.220 to 1.020) | – | |
|
| ||||
| AF | Yes, probably | |||
| Chronic | 8 | 0.125 (−0.048 to 0.299) | 0.0% and 0.833 and 0.156 | |
| Non-chronic | 22 | −0.050 (−0.102 to 0.001) | 92% and 0.001 and 0.056 | |
|
| ||||
| Type of AF | Yes, probably | |||
| Paroxysmal | 9 | −0.087 (−0.161 to −0.014) | 88.6% and 0.001 and 0.020 | |
| Persistent | 6 | −0.019 (−0.101 to 0.062) | 95.2% and 0.001 and 0.641 | |
| Permanent | 5 | 0.069 (−0.120 to 0.259) | 0.0% and 0.958 and 0.473 | |
|
| ||||
| NLR | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | – | – | – | |
| European | 9 | 0.901 (0.802 to 1.000) | 94% and 0.001 and 0.001 | |
| Africa | – | – | – | |
| North American | 1 | −0.640 (−1.711 to 0.431) | – | |
| South American | – | – | ||
| Australia | – | – | ||
|
| ||||
| Design of study | No | |||
| Cohort | 1 | −0.640 (−1.711 to 0.431) | – | |
| Case-control | 9 | 0.901 (0.802 to 1.000) | 94% and 0.001 and 0.001 | |
|
| ||||
| Number of population | No | |||
| >300 | 1 | 1.200 (−0.789 to 3.189) | – | |
| ≤300 | 9 | 0.887 (0.789 to 0.986) | 94.3% and 0.001 and 0.001 | |
|
| ||||
| Mean age | No | |||
| >60 years | 7 | 1.030 (0.919 to 1.141) | 91.5% and 0.001 and 0.001 | |
| ≤60 years | 3 | 0.365 (0.152 to 0.579) | 95.1% and 0.001 and 0.001 | |
|
| ||||
| Male | Yes, probably | |||
| >70% | 2 | −0.277 (−1.170 to 0.716) | 60.8% and 0.110 and 0.637 | |
| ≤70% | 8 | 0.901 (0.801 to 1.00) | 94.7% and 0.001 and 0.001 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | 1 | 0.670 (0.201 to 1.139) | – | |
| ≤30% | 9 | 0.898 (0.797 to 0.999) | 94.3% and 0.001 and 0.001 | |
|
| ||||
| Hypertension | ||||
| >70% | All of studies: ≤70% | |||
| ≤70% | ||||
|
| ||||
| Cigarette smoking | No | |||
| >30% | 3 | 0.492 (0.072 to 0.912) | 62.5% and 0.069 and 0.022 | |
| ≤30% | 6 | 0.928 (0.824 to 1.032) | 96.2% and 0.001 and 0.001 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 1 | 0.600 (0.146 to 1.054) | – | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 3 | 1.025 (0.687 to 1.364) | 91.2% and 0.001 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 2 | 0.630 (0.187 to 1.072) | 0.0% and 0.564 and 0.005 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | 0.408 (0.215 to 0.601) | 92.8% and 0.001 and 0.001 | |
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | – | – | – | |
| 2 | 1 | 1.200 (−0.789 to 3.189) | – | |
| 3 | 3 | 0.365 (0.152 to 0.579) | 95.1% and 0.001 and 0.001 | |
| 4 | 1 | 0.600 (0.146 to 1.054) | – | |
| 5 | 4 | 1.081 (0.962 to 1.199) | 95.4% and 0.001 and 0.001 | |
| 6 | 1 | 0.700 (0.236 to 1.164) | – | |
|
| ||||
| AF | No | |||
| Chronic | – | – | – | |
| Non-chronic | 4 | 0.689 (0.538 to 0.840) | 0.0% and 0.935 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 1 | 0.700 (0.529 to 0.871) | – | |
| Persistent | 2 | 0.634 (0.308 to 0.960) | 0.0% and 0.833 and 0.001 | |
| Permanent | – | – | – | |
|
| ||||
| RDW | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 1 | 0.260 (0.065 to 0.455) | – | |
| European | 6 | 0.873 (0.806 to 0.941) | 0.0% and 0.613 and 0.001 | |
| Africa | - | – | – | |
| North American | 1 | 0.280 (0.196 to 0.364) | – | |
| South American | - | – | – | |
| Australia | - | – | ||
|
| ||||
| Design of study | ||||
| Cohort | All of studies: case-control | |||
| Case-control | ||||
|
| ||||
| Number of population | No | |||
| >300 | 1 | 0.500 (−0.039 to 1.039) | – | |
| ≤300 | 7 | 0.615 (0.564 to 0.666) | 95.5% and 0.001 and 0.001 | |
|
| ||||
| Mean age | Yes, probably | |||
| >60 years | 4 | 0.412 (0.338 to 0.485) | 92.8% and 0.001 and 0.001 | |
| ≤60 years | 3 | 0.885 (0.809 to 0.961) | 0.0% and 0.716 and 0.001 | |
|
| ||||
| Male | No | |||
| >70% | 1 | 0.500 (−0.039 to 1.039) | – | |
| ≤70% | 6 | 0.641 (0.588 to 0.694) | 95.8% and 0.001 and 0.001 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | - | – | – | |
| ≤30% | 7 | 0.640 (0.587 to 0.692) | 95% and 0.001 and 0.001 | |
|
| ||||
| Hypertension | Yes, probably | |||
| >70% | 2 | 0.856 (0.700 to 1.011) | 0.0% and 0.337 and 0.001 | |
| ≤70% | 5 | 0.612 (0.556 to 0.668) | 96.4% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | No | |||
| >30% | 1 | 0.500 (−0.039 to 1.039) | – | |
| ≤30% | 3 | 0.885 (0.809 to 0.961) | 0.0% and 0.716 and 0.001 | |
|
| ||||
| Medication: Diuretic | ||||
| >70% | No Data | |||
| ≤70% | ||||
|
| ||||
| Medication: ACEI | No | |||
| >70% | - | – | – | |
| ≤70% | 2 | 1.021 (0.615 to 1.426) | 0.0% and 0.636 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | - | – | – | |
| ≤70% | 1 | 0.500 (−0.039 to 1.039) | – | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | - | – | – | |
| ≤70% | 3 | 0.885 (0.809 to 0.961) | 0.0% and 0.716 and 0.001 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | - | – | – | |
| 2 | 1 | 0.500 (−0.039 to 1.039) | – | |
| 3 | 4 | 0.875 (0.806 to 0.944) | 0.0% and 0.796 and 0.001 | |
| 4 | - | – | – | |
| 5 | 3 | 0.297 (0.221 to 0.373) | 80.7% and 0.006 and 0.001 | |
| 6 | - | – | – | |
|
| ||||
| AF | No | |||
| Chronic | - | – | – | |
| Non-chronic | 4 | 0.379 (0.310 to 0.448) | 91.6% and 0.001 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 1 | 0.260 (0.065 to 0.455) | – | |
| Persistent | - | – | – | |
| Permanent | - | – | – | |
|
| ||||
| MCV | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | 1 | −0.300 (−1.364 to 0.764) | – | |
| European | 1 | 1.000 (−0.337 to 2.337) | – | |
| Africa | - | – | – | |
| North American | 1 | −0.280 (−0.706 to 0.146) | – | |
| South American | - | – | – | |
| Australia | 1 | 1.000 (−0.998 to 2.998) | – | |
|
| ||||
| Design of study | ||||
| Cohort | All of studies: Case-control | |||
| Case-control | ||||
|
| ||||
| Number of population | No | |||
| >300 | 1 | −0.300 (−1.364 to 0.764) | – | |
| ≤300 | 3 | −0.116 (−0.514 to 0.283) | 55% and 0.108 and 0.569 | |
|
| ||||
| Mean age | No | |||
| >60 years | 2 | −0.283 (−0.679 to 0.113) | 0.0% and 0.162 and 0.973 | |
| ≤60 years | 2 | 1.000 (−0.111 to 2.111) | 0.0% and 1.000 and 0.078 | |
|
| ||||
| Male | No | |||
| >70% | 1 | 1.000 (−0.998 to 2.998) | – | |
| ≤70% | 3 | −0.179 (−0.559 to 0.200) | 38.5% and 0.197 and 0.354 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | - | – | – | |
| ≤30% | 3 | −0.179 (−0.559 to 0.200) | 38.5% and 0.197 and 0.354 | |
|
| ||||
| Hypertension | No | |||
| >70% | - | – | – | |
| ≤70% | 3 | −0.179 (−0.559 to 0.200) | 38.5% and 0.197 and 0.354 | |
|
| ||||
| Cigarette smoking | No | |||
| >30% | - | – | – | |
| ≤30% | 2 | 0.204 (−0.628 to 1.037) | 55% and 0.136 and 0.631 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | - | – | – | |
| ≤70% | 1 | −0.300 (−1.364 to 0.764) | – | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | - | – | – | |
| ≤70% | 1 | −0.300 (−1.364 to 0.764) | – | |
|
| ||||
| Medication: Statin | No | |||
| >70% | - | – | – | |
| ≤70% | 1 | −0.300 (−1.364 to 0.764) | – | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | - | – | – | |
| ≤70% | 2 | 0.204 (−0.628 to 1.037) | 55% and 0.136 and 0.631 | |
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | – | – | – | |
| 2 | – | – | – | |
| 3 | 1 | 1.000 (−0.337 to 2.337) | – | |
| 4 | 1 | −0.300 (−1.364 to 0.764) | – | |
| 5 | 2 | −0.224 (−0.641 to 0.193) | 33.7% and 0.219 and 0.292 | |
| 6 | – | – | – | |
|
| ||||
| AF | No | |||
| Chronic | – | – | – | |
| Non-chronic | 1 | −0.280 (−0.706 to 0.146) | – | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | – | – | – | |
| Persistent | – | – | – | |
| Permanent | – | – | – | |
|
| ||||
| HCT | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | – | – | – | |
| European | 9 | 0.552 (0.004 to 1.100) | 53.4% and 0.028 and 0.048 | |
| Africa | – | – | – | |
| North American | 1 | 2.670 (2.168 to 3.172) | – | |
| South American | – | – | – | |
| Australia | 1 | 3.000 (1.605 to 4.395) | – | |
|
| ||||
| Design of study | ||||
| Cohort | All of studies: Case-control | |||
| Case-control | ||||
|
| ||||
| Number of population | ||||
| >300 | All of studies: ≤300 | |||
| ≤300 | ||||
|
| ||||
| Mean age | No | |||
| >60 years | 10 | 1.704 (1.334 to 2.075) | 81.4% and 0.001 and 0.001 | |
| ≤60 years | 1 | 3.000 (1.605 to 4.395) | – | |
|
| ||||
| Male | No | |||
| >70% | 3 | 1.666 (0.767 to 2.566) | 67% and 0.048 and 0.001 | |
| ≤70% | 8 | 1.813 (1.423 to 2.203) | 84.6% and 0.001 and 0.001 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | – | – | – | |
| ≤30% | 8 | 1.691 (1.299 to 2.083) | 84.6% and 0.001 and 0.001 | |
|
| ||||
| Hypertension | No | |||
| >70% | – | – | – | |
| ≤70% | 8 | 1.691 (1.299 to 2.083) | 84.6% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | No | |||
| >30% | – | – | – | |
| ≤30% | 5 | −0.064 (−0.805 to 0.678) | 39.4% and 0.158 and 0.867 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | 0.402 (−0.488 to 1.292) | 0.0% and 0.753 and 0.376 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | 0.402 (−0.488 to 1.292) | 0.0% and 0.753 and 0.376 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | 0.402 (−0.488 to 1.292) | 0.0% and 0.753 and 0.376 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | 0.402 (−0.488 to 1.292) | 0.0% and 0.753 and 0.376 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | 2 | 1.819 (0.693 to 2.945) | 65.9% and 0.087 and 0.002 | |
| 2 | – | – | – | |
| 3 | 2 | −0.021 (−1.381 to 1.340) | 0.0% and 0.477 and 0.976 | |
| 4 | 4 | 0.852 (0.001 to 1.704) | 0.0% and 0.985 and 0.050 | |
| 5 | 3 | 2.230 (1.787 to 2.673) | 93.9% and 0.001 and 0.001 | |
| 6 | – | – | – | |
|
| ||||
| AF | No | |||
| Chronic | 5 | 0.062 (−0.635 to 0.759) | 46.9% and 0.110 and 0.861 | |
| Non-chronic | 3 | 2.611 (2.141 to 3.082) | 18.5% and 0.293 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 1 | 1.000 (−1.122 to 3.122) | – | |
| Persistent | – | – | – | |
| Permanent | 4 | 0.617 (−0.215 to 1.450) | 0.0% and 0.603 and 0.146 | |
|
| ||||
| Hb | ||||
|
| ||||
| Year of publication | No | |||
| >2000 | 25 | 0.024 (−0.038 to 0.087) | 91.1% and 0.001 and 0.444 | |
| ≤2000 | 2 | 1.076 (0.522 to 1.630) | 85.2% and 0.009 and 0.001 | |
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 2 | −0.048 (−0.366 to 0.271) | 0.0% and 0.758 and 0.769 | |
| European | 21 | −0.150 (−0.219 to −0.081) | 76.8% and 0.001 and 0.001 | |
| Africa | – | – | – | |
| North American | 4 | 0.994 (0.840 to 1.149) | 89.4% and 0.001 and 0.001 | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | Yes, probably | |||
| Cohort | 6 | −0.093 (−0.142 to −0.044) | 0.0% and 0.488 and 0.001 | |
| Case-control | 21 | 0.102 (0.024 to 0.181) | 92.8% and 0.001 and 0.011 | |
|
| ||||
| Number of population | No | |||
| >300 | 1 | −0.100 (−0.643 to 0.443) | – | |
| ≤300 | 26 | 0.039 (−0.023 to 0.102) | 91.4% and 0.001 and 0.216 | |
|
| ||||
| Mean age | No | |||
| >60 years | 20 | 0.033 (−0.032 to 0.098) | 92.5% and 0.001 and 0.317 | |
| ≤60 years | 5 | −0.077 (−0.297 to 0.143) | 73.5% and 0.005 and 0.494 | |
|
| ||||
| Male | No | |||
| >70% | 6 | −0.040 (−0.143 to 0.063) | 75.1% and 0.001 and 0.447 | |
| ≤70% | 19 | 0.062 (−0.017 to 0.140) | 92.7% and 0.001 and 0.123 | |
|
| ||||
| Diabetes mellitus | Yes, probably | |||
| >30% | 2 | −0.048 (−0.366 to 0.271) | 0.0% and 0.758 and 0.769 | |
| ≤30% | 23 | 0.027 (−0.036 to 0.091) | 91.8% and 0.001 and 0.401 | |
|
| ||||
| Hypertension | Yes, probably | |||
| >70% | 2 | −0.275 (−0.481 to 0.070) | 0.0% and 0.583 and 0.009 | |
| ≤70% | 23 | 0.055 (−0.011 to 0.120) | 91.6% and 0.001 and 0.102 | |
|
| ||||
| Cigarette smoking | Yes, probably | |||
| >30% | 8 | −0.054 (−0.223 to 0.114) | 0.0% and 0.597 and 0.529 | |
| ≤30% | 10 | −0.308 (−0.422 to −0.193) | 80.8% and 0.001 and 0.001 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | – | – | – | |
| ≤70% | 9 | −0.184 (−0.267 to −0.100) | 84.9% and 0.001 and 0.001 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 13 | −0.192 (−0.272 to −0.112) | 80.6% and 0.001 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 10 | −0.017 (−0.114 to 0.079) | 58% and 0.011 and 0.729 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 14 | −0.172 (−0.251 to −0.094) | 80.8% and 0.001 and 0.001 | |
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | 2 | 1.076 (0.522 to 1.630) | 85.2% and 0.009 and 0.001 | |
| 2 | 1 | −0.100 (−0.643 to 0.443) | – | |
| 3 | 6 | −0.183 (−0.355 to −0.011) | 73.3% and 0.002 and 0.037 | |
| 4 | 9 | −0.005 (−0.100 to 0.090) | 63.2% and 0.005 and 0.913 | |
| 5 | 8 | 0.148 (0.049 to 0.247) | 96.8% and 0.001 and 0.004 | |
| 6 | 1 | −0.200 (−0.550 to 0.150) | – | |
|
| ||||
| AF | No | |||
| Chronic | 8 | −0.320 (−0.443 to −0.196) | 85.2% and 0.001 and 0.001 | |
| Non-chronic | 5 | 0.543 (0.418 to 0.668) | 96.1% and 0.001 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 1 | 0.500 (−0.059 to 1.059) | – | |
| Persistent | 1 | 0.200 (−0.553 to 0.953) | – | |
| Permanent | 4 | −0.458 (−0.596 to −0.320) | 68.5% and 0.023 and 0.001 | |
|
| ||||
| Occurrence of AF | ||||
|
| ||||
| Platelet count | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 2 | 14.48 (−1.95 to 30.91) | 28.6% and 0.237 and 0.084 | |
| European | 2 | −12.96 (−25.66 to −0.272) | 40.8% and 0.194 and 0.045 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | No | |||
| Cohort | 3 | 0.217 (−0.188 to 0.622) | 50.9% and 0.130 and 0.294 | |
| Case-control | 1 | 20.45 (1.27 to 39.63) | – | |
|
| ||||
| Number of population | ||||
| >300 | All of studies: ≤300 | |||
| ≤300 | ||||
|
| ||||
| Mean age | No | |||
| >60 years | 3 | −0.132 (−13.084 to 12.82) | 78.8% and 0.009 and 0.984 | |
| ≤60 years | 1 | −6.60 (−22.517 to 9.317) | – | |
|
| ||||
| Male | No | |||
| >70% | – | – | – | |
| ≤70% | 3 | −2.78 (−13.37 to 7.79) | 79.6% and 0.007 and 0.606 | |
|
| ||||
| Diabetes mellitus | ||||
| >30% | All of studies: ≤30% | |||
| ≤30% | ||||
|
| ||||
| Hypertension | ||||
| >70% | All of studies: ≤70% | |||
| ≤70% | ||||
|
| ||||
| Cigarette smoking | Yes, probably | |||
| >30% | 2 | 4.43 (−7.81 to 16.80) | 77.9% and 0.033 and 0.478 | |
| ≤30% | 2 | −17.38 (−34.94 to 0.174) | 22.3% and 0.257 and 0.052 | |
|
| ||||
| Medication: Diuretic | ||||
| >70% | No Data | |||
| ≤70% | ||||
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 2 | 0.238 (−13.93 to 14.41) | 89.4% and 0.002 and 0.974 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 3 | −0.132 (−13.08 to 12.82) | 78.8% and 0.009 and 0.984 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | – | – | |
| ≤70% | 2 | 0.238 (−13.93 to 14.41) | 89.4% and 0.002 and 0.974 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | – | – | – | |
| 2 | – | – | – | |
| 3 | – | – | – | |
| 4 | 2 | 4.432 (−7.817 to 16.68) | 77.9% and 0.033 and 0.478 | |
| 5 | 2 | −17.38 (−34.94 to 0.174) | 22.3% and 0.257 and 0.052 | |
| 6 | – | – | – | |
|
| ||||
| AF | ||||
| Chronic | All of studies: non–chronic | |||
| Non-chronic | ||||
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 2 | 0.238 (−13.93 to 14.41) | 89.4% and 0.002 and 0.974 | |
| Persistent | – | – | – | |
| Permanent | – | – | – | |
|
| ||||
| WBC | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 11 | 0.136 (−0.013 to 0.284) | 34.7% and 0.121 and 0.073 | |
| European | 11 | 0.347 (0.120 to 0.574) | 65.1% and 0.001 and 0.003 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | Yes, probably | |||
| Cohort | 20 | 0.202 (0.077 to 0.326) | 58.6% and 0.001 and 0.002 | |
| Case-control | 2 | −0.344 (−2.282 to 1.594) | 0.0% and 0.710 and 0.728 | |
|
| ||||
| Number of population | No | |||
| >300 | 3 | 0.146 (−0.030 to 0.321) | 63.6% and 0.064 and 0.103 | |
| ≤300 | 19 | 0.254 (0.077 to 0.430) | 55.1% and 0.002 and 0.005 | |
|
| ||||
| Mean age | Yes, probably | |||
| >60 years | 10 | 0.097 (−0.076 to 0.269) | 0.0% and 0.498 and 0.272 | |
| ≤60 years | 12 | 0.310 (0.131 to 0.489) | 68.7% and 0.001 and 0.001 | |
|
| ||||
| Male | No | |||
| >70% | 9 | 0.251 (0.093 to 0.410) | 49.4% and 0.045 and 0.002 | |
| ≤70% | 11 | 0.107 (−0.108 to 0.323) | 62.4% and 0.003 and 0.328 | |
|
| ||||
| Diabetes mellitus | No | |||
| >30% | – | – | – | |
| ≤30% | 17 | 0.286 (0.149 to 0.423) | 55.7% and 0.003 and 0.001 | |
|
| ||||
| Hypertension | No | |||
| >70% | 1 | −0.030 (−0.560 to 0.50) | – | |
| ≤70% | 20 | 0.215 (0.087 to 0.344) | 58.1% and 0.001 and 0.001 | |
|
| ||||
| Cigarette smoking | Yes, probably | |||
| >30% | 5 | 0.707 (0.376 to 1.037) | 63% and 0.029 and 0.001 | |
| ≤30% | 6 | 0.032 (−0.261 to 0.325) | 0.0% and 0.416 and 0.832 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | 1 | −0.40 (−1.087 to 0.287) | – | |
| ≤70% | 3 | 0.202 (−0.012 to 0.417) | 0.0% and 0.776 and 0.064 | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 13 | 0.217 (0.067 to 0.367) | 68.8% and 0.001 and 0.005 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 11 | 0.321 (0.117 to 0.525) | 71.9% and 0.001 and 0.002 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | 2 | −0.159 (−0.654 to 0.335) | 0.0% and 0.322 and 0.528 | |
| ≤70% | 7 | 0.083 (−0.087 to 0.252) | 42.1% and 0.110 and 0.339 | |
|
| ||||
| Anti-coagulant status codes | Yes, probably | |||
| 1 | – | – | – | |
| 2 | 4 | −0.097 (−0.476 to 0.282) | 0.0% and 0.860 and 0.617 | |
| 3 | – | – | – | |
| 4 | 2 | 0.341 (−0.269 to 0.952) | 0.0% and 0.482 and 0.273 | |
| 5 | 16 | 0.230 (0.095 to 0.365) | 64.5% and 0.001 and 0.001 | |
| 6 | – | – | – | |
|
| ||||
| AF | No | |||
| Chronic | – | – | – | |
| Non-chronic | 21 | 0.181 (0.049 to 0.314) | 56.3% and 0.001 and 0.007 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 7 | −0.036 (−0.291 to 0.218) | 25.6% and 0.233 and 0.781 | |
| Persistent | 7 | −0.077 (−0.383 to 0.229) | 0.0% and 0.887 and 0.621 | |
| Permanent | – | – | – | |
|
| ||||
| NLR | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 3 | 0.047 (−0.124 to 0.218) | 0.0% and 0.552 and 0.588 | |
| European | 4 | 0.750 (0.565 to 0.936) | 35.1% and 0.201 and 0.001 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | ||||
| Cohort | All of studies: cohort | |||
| Case-control | ||||
|
| ||||
| Number of population | No | |||
| >300 | 2 | 0.035 (−0.142 to 0.212) | 0.0% and 0.340 and 0.698 | |
| ≤300 | 5 | 0.712 (0.533 to 0.891) | 41.9% and 0.142 and 0.001 | |
|
| ||||
| Mean age | Yes, probably | |||
| >60 years | 3 | 0.476 (0.183 to 0.770) | 21.4% and 0.280 and 0.001 | |
| ≤60 years | 4 | 0.346 (0.207 to 0.485) | 90.8% and 0.001 and 0.001 | |
|
| ||||
| Male | No | |||
| >70% | 2 | 0.035 (−0.142 to 0.212) | 0.0% and 0.340 and 0.698 | |
| ≤70% | 3 | 0.804 (0.610 to 0.997) | 0.0% and 0.593 and 0.001 | |
|
| ||||
| Diabetes mellitus | ||||
| >30% | All of studies: ≤30% | |||
| ≤30% | ||||
|
| ||||
| Hypertension | ||||
| >70% | All of studies: ≤70% | |||
| ≤70% | ||||
|
| ||||
| Cigarette smoking | No | |||
| >30% | 2 | 0.851 (0.626 to 1.077) | 0.0% and 0.530 and 0.001 | |
| ≤30% | 3 | 0.476 (0.183 to 0.770) | 21.4% and 0.280 and 0.001 | |
|
| ||||
| Medication: Diuretic | ||||
| >70% | No data | |||
| ≤70% | ||||
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 2 | 0.819 (0.615 to 1.023) | 0.0% and 0.360 and 0.001 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 3 | 0.767 (0.572 to 0.963) | 45.6% and 0.159 and 0.001 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | – | 0.670 (0.291 to 1.049) | – | |
| ≤70% | 1 | – | ||
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | – | – | – | |
| 2 | 1 | 0.150 (−0.499 to 0.799) | – | |
| 3 | – | – | – | |
| 4 | – | – | – | |
| 5 | 6 | 0.379 (0.250 to 0.507) | – | |
| 6 | – | – | – | |
|
| ||||
| AF | No | |||
| Chronic | – | – | – | |
| Non-chronic | 6 | 0.527 (0.370 to 0.684) | 80% and 0.001 and 0.001 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 2 | 0.670 (0.349 to 0.991) | 0.0% and 1.000 and 0.001 | |
| Persistent | 1 | 0.150 (−0.499 to 0.799) | – | |
| Permanent | – | – | – | |
|
| ||||
| RDW | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | Yes, probably | |||
| Asian | 3 | 0.165 (0.051 to 0.279) | 79.1% and 0.008 and 0.005 | |
| European | 2 | 0.803 (0.560 to 1.045) | 0.0% and 0.425 and 0.001 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | No | |||
| Cohort | 4 | 0.264 (0.155 to 0.372) | 90.3% and 0.001 and 0.001 | |
| Case-control | 1 | 0.440 (0.102 to 0.778) | – | |
|
| ||||
| Number of population | No | |||
| >300 | 1 | 0.100 (−0.023 to 0.223) | – | |
| ≤300 | 4 | 0.705 (0.516 to 0.894) | 31.2% and 0.225 and 0.001 | |
|
| ||||
| Mean age | Yes, probably | |||
| >60 years | 3 | 0.165 (0.051 to 0.279) | 79.1% and 0.008 and 0.005 | |
| ≤60 years | 2 | 0.803 (0.560 to 1.045) | 0.0% and 0.425 and 0.001 | |
|
| ||||
| Male | Yes, probably | |||
| >70% | 2 | 0.129 (0.008 to 0.250) | 85.1% and 0.010 and 0.036 | |
| ≤70% | 3 | 0.680 (0.483 to 0.877) | 43.8% and 0.169 and 0.001 | |
|
| ||||
| Diabetes mellitus | ||||
| >30% | All of studies: ≤30% | |||
| ≤30% | ||||
|
| ||||
| Hypertension | ||||
| >70% | ≤70% | |||
| ≤70% | ||||
|
| ||||
| Cigarette smoking | No | |||
| >30% | 3 | 0.680 (0.483 to 0.877) | 43.8% and 0.169 and 0.001 | |
| ≤30% | – | – | – | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | 1 | (0.329 to 1.671) | – | |
| ≤70% | 1 | 0.100 (−0.023 to 0.223) | – | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 3 | 0.165 (0.051 to 0.279) | 79.1% and 0.008 and 0.005 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 1 | 0.440 (0.102 to 0.778) | – | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | 1 | 1.000 (0.329 to 1.671) | – | |
| ≤70% | 2 | 0.140 (0.024 to 0.255) | 70.8% and 0.064 and 0.018 | |
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | – | – | – | |
| 2 | – | – | – | |
| 3 | – | – | – | |
| 4 | 2 | 0.661 (0.460 to 0.861) | 60.3% and 0.113 and 0.001 | |
| 5 | 3 | 0.143 (0.023 to 0.263) | 81.2% and 0.005 and 0.020 | |
| 6 | – | – | – | |
|
| ||||
| AF | ||||
| Chronic | All of studies: non–chronic | |||
| Non-chronic | ||||
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 2 | 0.511 (0.188 to 0.834) | 46.9% and 0.170 to 0.002 | |
| Persistent | – | – | – | |
| Permanent | – | – | – | |
|
| ||||
| Hb | ||||
|
| ||||
| Year of publication | ||||
| >2000 | All of studies: after 2000 | |||
| ≤2000 | ||||
|
| ||||
| Geographic area | No | |||
| Asian | 5 | 0.046 (−0.133 to 0.226) | 43.2% and 0.133 and 0.613 | |
| European | 4 | 0.007 (−0.306 to 0.319) | 0.0% and 0.539 and 0.967 | |
| Africa | – | – | – | |
| North American | – | – | – | |
| South American | – | – | – | |
| Australia | – | – | – | |
|
| ||||
| Design of study | No | |||
| Cohort | 8 | 0.029 (−0.131 to 0.189) | 23.1% and 0.246 and 0.723 | |
| Case-control | 1 | 0.170 (−0.506 to 0.846) | – | |
|
| ||||
| Number of population | No | |||
| >300 | 2 | 0.095 (−0.099 to 0.288) | 54.4% and 0.139 and 0.336 | |
| ≤300 | 7 | −0.070 (−0.331 to 0.191) | 1.2% and 0.451 and 0.598 | |
|
| ||||
| Mean Age | No | |||
| >60 years | 5 | −0.057 (−0.258 to 0.144) | 3.0% and 0.390 and 0.576 | |
| ≤60 years | 4 | 0.177 (−0.069 to 0.422) | 1.5% and 0.385 and 0.159 | |
|
| ||||
| Male | No | |||
| >70% | 3 | 0.056 (−0.133 to 0.245) | 65.4% and 0.056 and 0.563 | |
| ≤70% | 5 | 0.035 (−0.248 to 0.319) | 0.0% and 0.672 and 0.807 | |
|
| ||||
| Diabetes mellitus | ||||
| >30% | All of studies: ≤30% | |||
| ≤30% | ||||
|
| ||||
| Hypertension | ||||
| >70% | All of studies: ≤70% | |||
| ≤70% | ||||
|
| ||||
| Cigarette smoking | No | |||
| >30% | 4 | 0.070 (−0.233 to 0.374) | 0.0% and 0.582 and 0.650 | |
| ≤30% | 2 | −0.314 (−0.933 to 0.306) | 0.0% and 0.645 and 0.321 | |
|
| ||||
| Medication: Diuretic | No | |||
| >70% | 1 | −0.800 (−1.706 to 0.106) | – | |
| ≤70% | 1 | 0.00 (−0.231 to 0.231) | – | |
|
| ||||
| Medication: ACEI | No | |||
| >70% | – | – | – | |
| ≤70% | 5 | −0.047 (−0.238 to 0.144) | 0.0% and 0.494 and 0.630 | |
|
| ||||
| Medication: Statin | No | |||
| >70% | – | – | – | |
| ≤70% | 4 | −0.096 (−0.442 to 0.250) | 0.0% and 0.734 and 0.587 | |
|
| ||||
| Medication: Beta-Blocker | No | |||
| >70% | 1 | −0.800 (−1.706 to 0.106) | – | |
| ≤70% | 3 | 0.002 (−0.208 to 0.213) | 0.0% and 0.782 and 0.984 | |
|
| ||||
| Anti-coagulant status codes | No | |||
| 1 | – | – | – | |
| 2 | – | – | – | |
| 3 | – | – | – | |
| 4 | 2 | 0.236 (−0.161 to 0.632) | 0.0% and 0.814 and 0.244 | |
| 5 | 7 | 0.00 (−0.169 to 0.169) | 25.5% and 0.234 and 0.998 | |
| 6 | – | – | – | |
|
| ||||
| AF | No | |||
| Chronic | – | – | – | |
| Non-chronic | 8 | −0.031 (−0.204 to 0.142) | 0.0% and 0.513 and 0.727 | |
|
| ||||
| Type of AF | No | |||
| Paroxysmal | 3 | −0.070 (−0.531 to 0.391) | 0.0% and 0.603 and 0.766 | |
| Persistent | – | – | – | |
| Permanent | – | – | – | |