Abstract
Background:
Subacromial impingement syndrome (SAIS) is the most common disorder of the shoulder. The evidence for the effectiveness of treatment options is inconclusive and limited. Therefore, there is a need for more evidence in this regard, particularly for long-term outcomes.
Hypothesis:
Platelet-rich plasma (PRP) would be an effective method in treating subacromial impingement.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
This was a single-blinded randomized clinical trial with 1-, 3-, and 6-month follow-up. Sixty-two patients were randomly placed into 2 groups, receiving either PRP or exercise therapy. The outcome parameters were pain, shoulder range of motion (ROM), muscle force, functionality, and magnetic resonance imaging findings.
Results:
Both treatment options significantly reduced pain and increased shoulder ROM compared with baseline measurements. Both treatments also significantly improved functionality. However, the treatment choices were not significantly effective in improving muscle force. Trend analysis revealed that in the first and third months, exercise therapy was superior to PRP in pain, shoulder flexion and abduction, and functionality. However, in the sixth month, only shoulder abduction and total Western Ontario Rotator Cuff score were significantly different between the 2 groups.
Conclusion:
Both PRP injection and exercise therapy were effective in reducing pain and disability in patients with SAIS, with exercise therapy proving more effective.
Keywords: exercise therapy, PRP, subacromial impingement syndrome
The incidence of subacromial impingement syndrome (SAIS) increases as the population ages.38 SAIS is the most common disorder of the shoulder, accounting for 44% to 65% of all complaints of shoulder pain,7,38,40 and results from an inflammation and degeneration of the anatomic structures in the subacromial space.21,31 Some of the structures that can be impaired include the subacromial bursa, tendons of the rotator cuff, coracoacromial ligament, and long head of the biceps.
There are 2 types of treatment for SAIS: nonsurgical and surgical. Some of the nonsurgical treatment options that are recommended include exercise therapy, subacromial corticosteroid injection, rest, nonsteroidal anti-inflammatory drugs (NSAIDs), physical modalities (eg, therapeutic ultrasound, electrotherapy, manual therapy), and taping.7,18,31,37
The use of platelet-rich plasma (PRP) as a biological solution for injuries to tendons of the rotator cuff has achieved popularity over the past several years.7 PRP is blood plasma with a high platelet concentration that, once activated, releases various growth factors involved in the tissue repair process.15 There is some evidence demonstrating a positive effect of PRP in tendinopathies4,12 and osteoarthritis of the knee3; however, the evidence in rotator cuff tendinopathy is limited.
In spite of increased PRP use in clinical settings, we found only 3 randomized controlled trials that evaluated the effectiveness of PRP injection in treating rotator cuff tendinopathy nonsurgically.24,35,39
On the other hand, although inconclusive, current evidence suggests that physical therapy is effective in treating patients with SAIS.1,10,14,23,26,27,30,34 For those patients who seek nonsurgical treatment in the early stages of SAIS, therapeutic exercise combined with other therapies (eg, Kinesio taping, acupuncture, localized corticosteroid injection, and ultrasound) is recommended.7 However, there is a need for further evidence of the effectiveness of both PRP and exercise in treating patients with SAIS. We conducted a randomized controlled trial (RCT) comparing PRP injections with exercise therapy. Our hypothesis was that PRP would be more effective at reducing pain and improving function than exercise therapy.
Methods
Study Design
This study was a parallel-group, single-blinded RCT with 1-, 3-, and 6-month follow-ups conducted from April 2013 to October 2014. All clinical assessments and treatments were performed at a university hospital in Tehran, Iran. This study was approved by the ethics committee of Iran University of Medical Science, and all participants provided informed consent. The trial was registered in the Iranian Registry of Clinical Trials.
Sample Size
With the repeated-measures design of the study in mind, G*Power 3.1.5 software (Heinrich-Heine-Universität Düsseldorf) was used to calculate the required sample size. We considered an effect size equal to 0.4 in our sample size calculation. Based on a power of 80% and a 2-tailed α of .05, we calculated that the sample size required per group was 18. Assuming a 15% loss to follow-up, the final sample size required was 21 patients per group.
Patient Recruitment
For the purposes of recruiting patients, advertising posters were put up in several local hospitals. Moreover, a number of medical practitioners interested in shoulder pathologies were notified of the objectives of the study by email and were asked to introduce their patients to us. A total of 72 volunteer patients came forward. SAIS was diagnosed via a clinical assessment. Patients underwent shoulder magnetic resonance imaging (MRI) for diagnosis confirmation. The 3-mm cuts were taken in T1-weighted, T2-weighted, proton density sequences in 3 planes (sagittal, coronal, and axial) using a 1.5-T MAGNETOM Essenza, a Tim system MRI (Siemens).
Of these 72 patients, 62 were included in this study (Figure 1). The inclusion criteria were (1) a minimum age of 40 years, (2) shoulder pain lasting at least 3 months prior to the study, (3) platelet count of more than 100,000, and (4) positive result in at least 3 of the following tests: empty can test, Speed test, Jobe test, Neer impingement sign, and Hawkins-Kennedy test. Exclusion criteria consisted of (1) radicular pain; (2) presence of pathologies such as frozen shoulder, calcific tendinitis, biceps dislocation, and a superior labrum anterior posterior lesion; (3) previous surgery within 6 months; (4) inflammatory diseases such as rheumatoid arthritis, polymyalgia rheumatica, or fibromyalgia; (5) full-thickness rotator cuff tear on MRI; (6) ligamentous laxity (positive sulcus test) or shoulder dislocation (positive apprehension test); (7) corticosteroid injection within 3 months prior to the study; (8) physical therapy 6 months prior to the study; (9) fear of MRI; and (10) contraindication to MRI.
Figure 1.
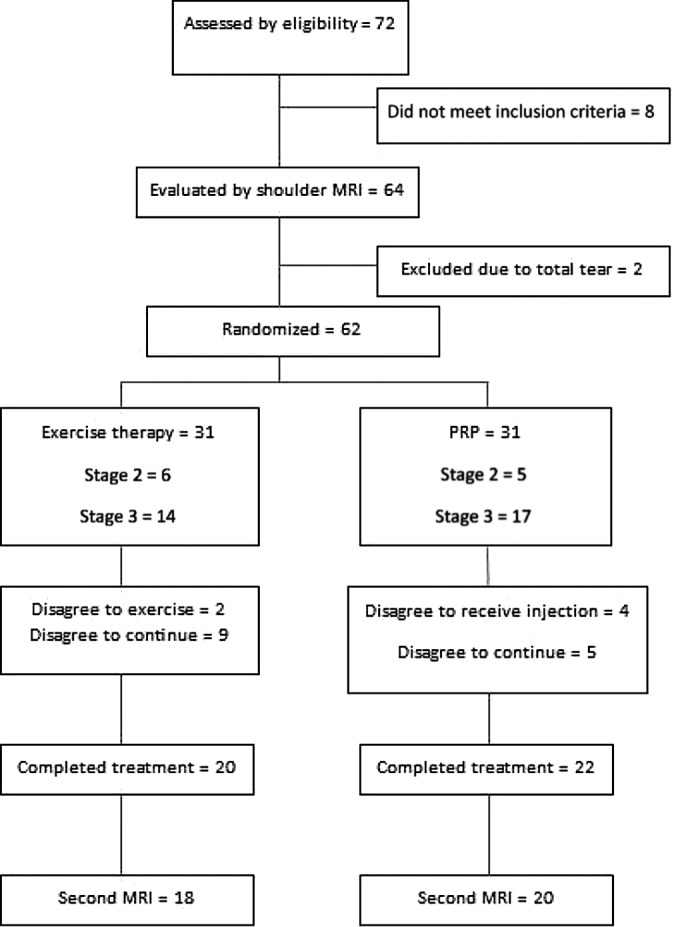
The CONSORT (Consolidated Standards of Reporting Trials) flowchart of the study.
Group Allocation
Because of the possibility of sample attrition, all 62 patients who had already met the inclusion criteria were recruited for this study. To eliminate the effect of confounding variables in the design stage, SAIS stage in shoulder MRI was considered as a confounder; thus, 2 different sequences were used to randomly allocate patients into the treatment groups: the first sequence for stages 1 and 2 and the second sequence for patients with stage 3 SAIS (only partial tear). After assessing the MRI findings for each patient, we used the proper sequence of randomization. After that, random number generator software was used for randomization. In this single-blinded RCT, only the assessor was blinded to group assignment. One group received PRP injections and the other exercise therapy. The CONSORT (Consolidated Standards of Reporting Trials) flowchart of the study is given in Figure 1.
Interventions
Participants were requested to refrain from receiving other forms of intervention for 6 months. They were, however, advised to take 500 mg of paracetamol if the pain in their shoulder during rest was more than a 5 on 10-point visual analog scale (VAS). Patients were also advised to avoid painful activities and to continue their usual daily activities during the study.
Platelet-Rich Plasma Group
Patients in the PRP group were injected twice: once at the beginning of the study and again 1 month after the first visit. On each occasion, an aliquot of 25 mL of venous blood was collected from each patient using a syringe containing 2.5 mL of anticoagulant citrate dextrose solution. The samples were projected into a Tubex Autotube System (Moohan Enterprise) and were centrifuged at 1300 rpm for 10 minutes. The separated plasma was subsequently centrifuged at 2770 rpm for 8 minutes. As a result, 5 mL of PRP was prepared. One milliliter of this PRP was sent to a laboratory for platelet counting. It was revealed that the obtained PRP had a platelet concentration of approximately 900,000 ± 15,000 platelets per mm3, almost 3 times the size of the baseline blood platelet count. The leukocytes obtained from the centrifugation were also measured to be 5000 to 10,000 per mm3.
The remainder of the obtained PRP (4 mL) was injected into the injured tendons under sterile conditions without any activator within 30 minutes of centrifugation. More specifically, 3 mL of PRP was injected into the partial tear in the tendon or, in the case of patients with tendinopathy, into hypoechogenic areas using an 18-gauge catheter guided by a 10-MHz ultrasound machine (Mindray). The other 1 mL was injected into the subacromial space from the lateral posterior side of the arm at an angle of 45° to the horizon without ultrasound guidance.
Patients were advised to avoid ice packs and excessive use of their shoulder joint within 48 hours after injection. In addition, they were asked not to take NSAIDs or aspirin for a period of 12 days, starting from 1 week before the injection and ending on the fifth day after injection. They were also asked not to eat onion, garlic, or dogwood over the same period, as these foods are known to affect platelet counts. They did not participate in exercise therapy for 6 months.
Exercise Therapy Group
Patients in the exercise therapy group received supervised exercise therapy in the hospital once a week for 3 months and performed the therapy exercises at home on the other days of the week. After this supervised period, the hospital program was terminated, but the patients were asked to continue the exercises at home for 6 months. No supervision was provided during this latter period.
Each exercise session began with warm-up aerobic activities lasting for 10 to 15 minutes and ended with ice packs being applied on the affected areas for 20 minutes to relieve pain. A number of images showing how each exercise should be performed were also provided.
The exercises were performed in 4 phases (see the Appendix). Each patient, depending on his or her condition, started with phase 1 and progressed to phase 4. Phase 1 was aimed at achieving passive range of motion (ROM) without pain. For this purpose, the isometric shoulder exercise and the passive ROM exercise were performed in all directions 8 to 10 times per day. Postural exercises (eg, chin tuck and scapular retraction) and glenohumeral ROM exercises were also performed 15 to 20 times per day. In the event of a 50% increase in the ROM, the active-assistive ROM exercise was performed in all directions with the help of a strap. Also in this phase, cross-body and neck stretches were performed 4 times a day, each for a length of 10 seconds. Mobilization exercises were performed once per week.
When a patient was able to perform the passive and active-assistive ROM exercises fully and painlessly, phase 2 (active ROM exercises) began. Shoulder abduction or scaption (scapular plane elevation) was performed by elevating the arm in the scapular plane to an angle of less than 60°. Strength training was performed on the external and internal rotator cuff muscles while the arms were placed at the sides of the body. This exercise was in the form of 3 sets per day, each with 10 repetitions. The stretching exercises performed in phase 1 were also performed in phase 2, but their duration was increased to 15 to 20 seconds.
The aim of phase 3 was to strengthen the muscles of the rotator cuff and scapula. Scaption was performed at an angle greater than 60°. The exercises intended to strengthen the rotator cuff muscles responsible for external and internal rotation of the humerus were performed at a 90° angle to shoulder abduction. The reverse-fly, shoulder extension, and bent-over row exercises were performed using an elastic band or a 1- to 1.5-kg weight in 3 sets of 10 repetitions each.
In phase 4, the exercises intended to train the scapular muscles were performed using a medicine ball. The exercises for strengthening the muscles of the rotator cuff and biceps were performed in 3 sets of 15 repetitions with a gradual increase of 25% to 50% in external resistance.
Outcome Parameters
The primary outcome parameter was pain. In addition to baseline measurement, patients underwent follow-up 1, 3, and 6 months later. Pain was measured using a 10-point VAS, with higher scores on the scale showing more pain.
The secondary outcome parameters were shoulder ROM, muscle strength, patient-reported outcome measures (Disabilities of the Arm, Shoulder, and Hand [DASH] and Western Ontario Rotator Cuff Index [WORC]), and MRI findings. As for shoulder-active ROM, a goniometer was used to measure flexion, extension, abduction, internal rotation in 90° of shoulder abduction, and external rotation in 90° of shoulder abduction. Muscle strength was assessed for shoulder flexion, abduction, and internal rotation via manual muscle strength testing and was measured on a scale from 0 (no active ROM) to 5 (full active ROM).36
The WORC consists of 21 items in 5 categories: pain and physical symptoms, sports and recreation, work, lifestyle, and emotions. If a category score is closer to 100, the shoulder is in a poorer condition. However, a total score that is closer to 100 indicates that the shoulder is in a better condition.33
The DASH questionnaire contains 30 items and measures the ability to do various activities of the upper extremities, including carrying loads and tools, overhead activities, key turning, writing, and many other activities of daily living. As the DASH score gets closer to 100, the shoulder is considered to be in a poorer condition.32
MRIs of each patient were taken at the beginning of the study and again 6 months later. A musculoskeletal radiologist who had more than 10 years of experience assessed the MRIs of the patients for signs of tendinopathy (ie, signal change without loss of tendon integrity), partial tears in the tendons of the biceps or the rotator cuff (ie, partial tears involving less than 50% of the tendon thickness), or pathologies in the subacromial space such as bursitis. The difference between baseline and follow-up observations was classified as either improvement, no change, or worsening.
Statistical Analysis
Data obtained from the patients were analyzed using Stata software (version 12; StataCorp). Normal distribution of the continuous variables was determined using the Shapiro-Wilk test. The data pertinent to these variables are shown as either mean ± SD or median, as appropriate. The categorical variables were analyzed using the chi-square test.
Pretreatment differences between the 2 groups were determined using t tests. To determine the treatment effect, the data were analyzed using either a random-effects mixed model or a generalized estimating equations model, as appropriate. For all tests, statistical significance was set at an α level of <.05 (2-tailed).
Results
Compliance
Patients receiving exercise therapy exhibited good compliance with treatment throughout the study period: 68.96% of the patients in the exercise group attended the 3-month course of exercise therapy (at home and in the hospital). They followed virtually all instructions. Patients in the PRP group also exhibited good compliance: 77.27% of them had both injections performed.
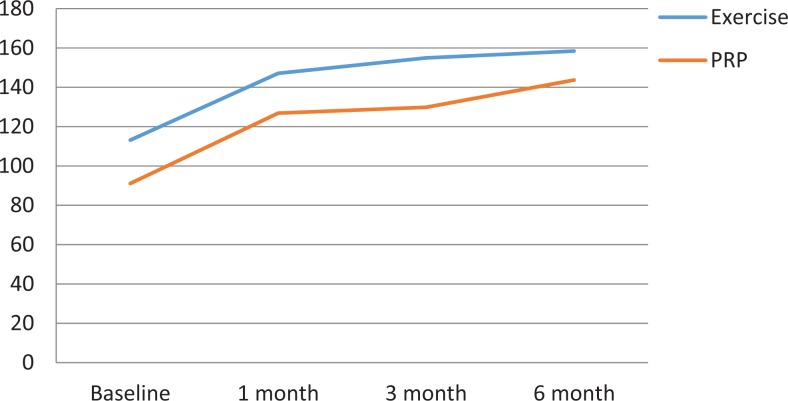
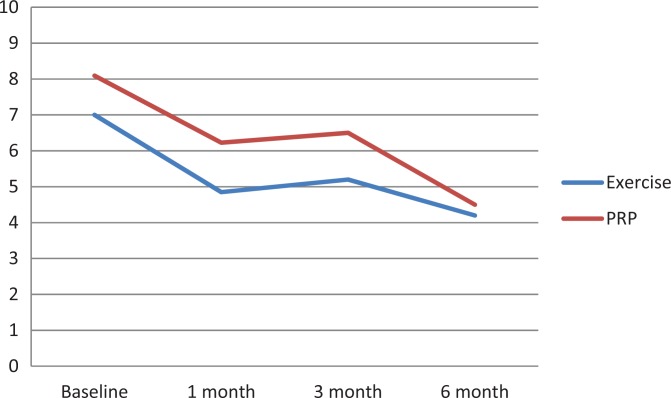
Effect of Treatment
The difference between the 2 groups was not significant at the beginning of the study considering the variables in question (Table 1). Both treatments resulted in improvement in pain (VAS) and function (total WORC and DASH) scores. The improvement in all areas of shoulder ROM was significant in the exercise group, but for the PRP group it was significant in all areas except external rotation. Improvement in muscle force did not reach significance.
TABLE 1.
Baseline Characteristics of the Participants in the 2 Study Groupsa
| Variable | PRP (n = 22) | Exercise (n = 20) | P Value |
|---|---|---|---|
| Age, y, mean ± SD | 52.5 ± 7.3 | 53.9 ± 10.6 | .61 |
| Female patients, n (%) | 13 (59.09) | 14 (70.00) | .46 |
| Right side affected, No. of patients (%) | 12 (54.54) | 10 (50.00) | .78 |
| Pain (VAS), mean ± SD | 8.1 ± 1.7 | 7.0 ± 2.3 | .09 |
| ROM, deg, mean ± SD | |||
| Flexion | 91.1 ± 40.6 | 113.1 ± 46.2 | .10 |
| Extension | 43.9 ± 15.0 | 47.25 ± 10.7 | .42 |
| Abduction | 69.8 ± 35.4 | 80.1 ± 39.5 | .37 |
| Internal rotation | 19.5 ± 25.0 | 18.7 ± 11.6 | .89 |
| External rotation | 89.9 ± 15.2 | 76.2 ± 28.5 | .06 |
| Muscle force, No. of patients (%)b | |||
| Flexion | 10 (45.45) | 15 (75.00) | .06 |
| Abduction | 10 (45.45) | 15 (75.00) | .06 |
| Internal rotation | 10 (45.45) | 15 (75.00) | .06 |
| Total WORC, mean ± SD | 33.9 ± 13.1 | 42.98 ± 21.0 | .10 |
| DASH, mean ± SD | 54.2 ± 18.6 | 50.5 ± 19.4 | .53 |
| MRI findings, No. of patients (%) | |||
| Tendinopathy of the supraspinatus | 5 (22.72) | 6 (30.00) | .72 |
| Partial tear of the supraspinatus | 16 (72.72) | 14 (70.00) | .49 |
| Tendinopathy of the biceps | 3 (13.63) | 5 (25.00) | .43 |
| Acromiohumeral distance <10 mm | 5 (22.72) | 6 (30.00) | .72 |
| Partial tear of the subscapularis | 1 (4.54) | 0 | .31 |
aDASH, Disabilities of the Arm, Shoulder, and Hand score; MRI, magnetic resonance imaging; PRP, platelet-rich plasma; ROM, range of motion; VAS, visual analog scale; WORC, Western Ontario Rotator Cuff Index.
bMuscle force indicates the number of patients who have full force (a score of 5 on a 0-5 scale via manual muscle strength testing).
Tables 2 to 4 and Figures 2 to 4 show the effect of treatment, time, and differences between groups. As can be seen in Table 4, the 2 study groups were significantly different in some parameters. At the 1-month follow-up, the exercise group saw better results than the PRP group in VAS, total WORC, abduction ROM, and force of internal rotation. At the 3-month follow-up, the exercise group had better results than the PRP group in VAS, total WORC, DASH, abduction ROM, forward flexion ROM, force of flexion, force of internal rotation, and force of abduction. Finally, at the 6-month follow-up, the exercise group had better results than PRP only for total WORC and abduction ROM.
TABLE 2.
The Effect of Treatment and Time in the 2 Study Groupsa
| 1st Month | 3rd Month | 6th Month | P Value | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | PRP (n = 22) | Exercise (n = 20) | PRP (n = 22) | Exercise (n = 20) | PRP (n = 22) | Exercise (n = 20) | Effect of Treatment | Effect of Time |
| Pain (VAS) | 6.2 ± 0.4 | 4.8 ± 0.4 | 6.5 ± 0.4 | 5.2 ± 0.4 | 4.5 ± 0.4 | 4.2 ± 0.4 | <.01 | <.01 |
| ROM, deg | ||||||||
| Flexion | 126.8 ± 7.4 | 147.1 ± 7.7 | 129.8 ± 7.4 | 154.9 ± 7.7 | 143.6 ± 7.4 | 158.4 ± 7.7 | <.01 | <.01 |
| Extension | 54.6 ± 2.5 | 53.9 ± 2.7 | 57.2 ± 2.5 | 59.7 ± 2.7 | 56.5 ± 2.5 | 59.6 ± 2.7 | .27 | <.01 |
| Abduction | 103.5 ± 8.7 | 129.2 ± 9.2 | 103.4 ± 8.7 | 138.5 ± 9.2 | 118.8 ± 8.7 | 146.5 ± 9.2 | <.01 | <.01 |
| Internal rotation | 35.0 ± 5.1 | 43.2 ± 5.3 | 43.5 ± 5.1 | 55.5 ± 5.3 | 57.4 ± 5.1 | 62.2 ± 5.3 | .10 | <.01 |
| External rotation | 93.1 ± 3.9 | 88.0 ± 4.1 | 91.1 ± 3.9 | 95.0 ± 4.1 | 92.0 ± 3.9 | 95.5 ± 4.1 | .31 | .03 |
| Muscle force, No. of patients (%)b | ||||||||
| Flexion | 16 (72.72) | 19 (95.00) | 20 (90.90) | 19 (95.00) | 21 (95.45) | 19 (95.00) | .12 | .31 |
| Abduction | 16 (72.72) | 19 (95.00) | 20 (90.90) | 18 (90.00) | 21 (95.45) | 19 (95.00) | .12 | .30 |
| Internal rotation | 15 (68.18) | 19 (95.00) | 20 (90.90) | 19 (95.00) | 21 (95.45) | 19 (95.00) | .10 | .31 |
| Total WORC | 45.9 ± 4.1 | 59.6 ± 4.4 | 46.4 ± 4.1 | 68.4 ± 4.4 | 58.7 ± 4.1 | 73.1 ± 4.4 | <.01 | <.01 |
| DASH | 45.1 ± 3.9 | 35.0 ± 4.1 | 44.3 ± 3.9 | 30.7 ± 4.1 | 33.0 ± 3.9 | 26.2 ± 4.1 | <.01 | <.01 |
aValues are expressed as mean ± SD unless indicated otherwise. DASH, Disabilities of the Arm, Shoulder, and Hand score; PRP, platelet-rich plasma; ROM, range of motion; VAS, visual analog scale; WORC, Western Ontario Rotator Cuff Index.
bMuscle force indicates the number of patients who have full force (a score of 5 on a 0-5 scale via manual muscle strength testing).
TABLE 3.
Change in Outcome Parameters From Baseline to Follow-up for the PRP and Exercise Groupsa
| Variable | PRP | Exercise |
|---|---|---|
| Pain (VAS) | ||
| 1st month | −1.86 (−2.84 to −0.88) | −2.15 (−3.18 to −1.12) |
| 3rd month | −1.60 (−2.57 to −0.61) | −1.80 (−2.83 to −0.77) |
| 6th month | −3.60 (−4.57 to −2.68) | −2.80 (−3.83 to −1.77) |
| ROM, deg | ||
| Flexion | ||
| 1st month | 35.77 (22.31 to 49.23) | 34.00 (19.88 to 48.12) |
| 3rd month | 38.77 (25.31 to 52.23) | 41.85 (27.73 to 55.96) |
| 6th month | 53.63 (39.17 to 66.09) | 45.30 (31.18 to 59.41) |
| Extension | ||
| 1st month | 10.63 (4.91 to 16.35) | 6.65 (0.65 to 12.64) |
| 3rd month | 13.31 (7.59 to 19.03) | 12.45 (6.45 to 18.44) |
| 6th month | 12.60 (6.87 to 18.30) | 12.40 (6.40 to 18.39) |
| Abduction | ||
| 1st month | 33.68 (17.92 to 49.44) | 49.10 (32.57 to 65.62) |
| 3rd month | 33.59 (17.83 to 49.34) | 58.35 (41.82 to 74.87) |
| 6th month | 49.04 (33.28 to 64.80) | 66.35 (49.82 to 82.87) |
| Internal rotation | ||
| 1st month | 15.50 (5.92 to 25.07) | 24.55 (14.50 to 34.59) |
| 3rd month | 24.04 (14.46 to 33.62) | 36.80 (26.75 to 46.84) |
| 6th month | 37.90 (28.33 to 47.48) | 43.55 (33.50 to 53.59) |
| External rotation | ||
| 1st month | 3.27 (−2.19 to 8.73) | 11.75 (6.07 to 17.48) |
| 3rd month | 1.45 (−4.01 to 6.91) | 18.75 (13.01 to 24.48) |
| 6th month | 2.09 (−4.01 to 7.55) | 19.25 (13.51 to 24.98) |
| Muscle force score | ||
| Flexion | ||
| 1st month | 0.31 (0.15 to 0.47) | 0.13 (0.02 to 0.24) |
| 3rd month | 0.46 (0.30 to 0.62) | 0.16 (0.03 to 0.30) |
| 6th month | 0.49 (0.33 to 0.66) | 0.17 (0.03 to 0.31) |
| Abduction | ||
| 1st month | 0.31 (0.14 to 0.47) | 0.13 (0.01 to 0.25) |
| 3rd month | 0.41 (0.24 to 0.58) | 0.16 (0.02 to 0.30) |
| 6th month | 0.48 (0.31 to 0.65) | 0.18 (0.03 to 0.33) |
| Internal rotation | ||
| 1st month | 0.28 (0.12 to 0.44) | 0.11 (0.01 to 0.22) |
| 3rd month | 0.46 (0.30 to 0.62) | 0.15 (0.02 to 0.29) |
| 6th month | 0.50 (0.34 to 0.66) | 0.16 (0.02 to 0.30) |
| Total WORC | ||
| 1st month | 11.92 (3.81 to 20.03) | 16.65 (8.14 to 25.16) |
| 3rd month | 12.44 (4.33 to 20.55) | 25.46 (16.95 to 33.97) |
| 6th month | 24.73 (16.62 to 32.84) | 30.10 (21.59 to 38.60) |
| DASH | ||
| 1st month | −9.14 (−16.46 to −1.82) | −15.47 (−23.15 to −7.80) |
| 3rd month | −10.00 (−17.32 to −2.68) | −19.84 (−27.52 to −12.16) |
| 6th month | −21.20 (−28.52 to −13.88) | −24.35 (−32.03 to −16.67) |
aValues are expressed as mean difference together with 95% confidence interval in parentheses. DASH, Disabilities of the Arm, Shoulder, and Hand score; PRP, platelet-rich plasma; ROM, range of motion; VAS, visual analog scale; WORC, Western Ontario Rotator Cuff Index.
TABLE 4.
Difference in Outcome Parameters at Follow-up Between the PRP and Exercise Groupsa
| Variable | 1st Month | 3rd Month | 6th Month | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Difference | 95% CI | P Value | Mean Difference | 95% CI | P Value | Mean Difference | 95% CI | P Value | |
| Pain (VAS) | 1.3 | 0.08 to 2.6 | .03 | 1.3 | 0.005 to 2.5 | .04 | 0.3 | −0.999 to 1.5 | .65 |
| ROM | |||||||||
| Flexion | −20.2 | −41.4 to 0.9 | .06 | −25.1 | −46.3 to −3.9 | .02 | −14.7 | −35.9 to 6.4 | .17 |
| Extension | 5.1 | −6.2 to 16.5 | .37 | −3.6 | −15.0 to 7.7 | .52 | −3.5 | −14.8 to 7.8 | .54 |
| Abduction | −25.7 | −50.9 to −0.5 | .04 | −35.1 | −60.2 to −9.9 | <.01 | −27.6 | −52.7 to −2.4 | .03 |
| Internal rotation | −8.2 | −22.9 to 6.4 | .26 | −11.9 | −26.6 to 2.7 | .10 | −4.8 | −19.5 to 9.8 | .51 |
| External rotation | 0.7 | −6.7 to 8.2 | .85 | −2.4 | −9.8 to −4.9 | .51 | −3.1 | −10.4 to 4.2 | .40 |
| Muscle force | |||||||||
| Flexion | 0.09 | 0.003 to 0.194 | .05 | 0.11 | 0.02 to 0.21 | .01 | 0.02 | 0.004 to 0.095 | .51 |
| Abduction | 0.07 | 0.02 to 0.17 | .18 | 0.11 | 0.01 to 0.21 | .01 | 0.04 | 0.01 to 0.12 | .24 |
| Internal rotation | 0.11 | 0.01 to 0.22 | .02 | 0.14 | 0.04 to 0.24 | .006 | 0.02 | 0.004 to 0.095 | .55 |
| Total WORC | −13.7 | −25.7 to −1.7 | .02 | −22.0 | −34.0 to −10.0 | <.01 | −14.3 | −26.3 to −2.3 | .02 |
| DASH | 10.0 | −1.09 to 21.1 | .07 | 13.5 | 2.4 to 24.6 | .01 | 6.8 | −4.2 to 17.9 | .22 |
aNegative values in mean difference indicate that the mean score of the domain in the exercise group was lower than in the platelet-rich plasma group. DASH, Disabilities of the Arm, Shoulder, and Hand score; ROM, range of motion; VAS, visual analog scale; WORC, Western Ontario Rotator Cuff Index.
Figure 2.
Comparison of flexion range of motion (ROM) between the 2 groups. PRP, platelet-rich plasma.
Figure 3.
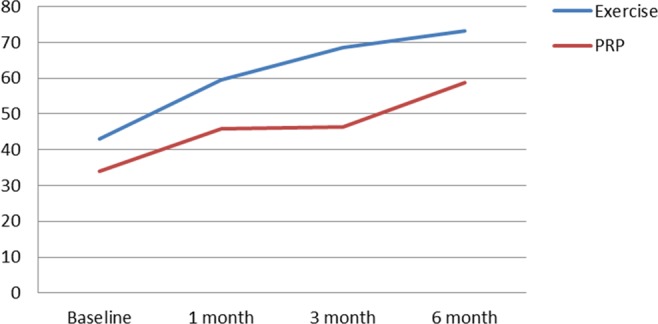
Comparison of total Western Ontario Rotator Cuff Index (WORC) between the 2 groups. PRP, platelet-rich plasma.
Figure 4.
Comparison of pain visual analog scale (VAS) between the 2 groups. PRP, platelet-rich plasma.
MRI Findings
A total of 38 patients (20 PRP, 18 exercise therapy) agreed to undergo both MRIs, one at the beginning of the study and the other 6 months after the study began. According to the MRI data obtained, none of the patients underwent any change in the pathology of the biceps or the acromiohumeral distance. Improvement in the appearance of supraspinatus tendinopathy was seen in 4 patients (3 PRP [P = .06] and 1 exercise therapy [P = .1]). Chi-square tests yielded P = .34, which indicated no significant difference between the 2 methods according to rate of improvement.
Discussion
The main finding of the present research was that the shoulder pain emanating from SAIS can be reduced through either PRP injection or exercise therapy. At final follow-up, there was no significant difference between the 2 groups in our primary outcome measure (pain), but the exercise therapy group had significantly higher WORC scores and abduction ROM.
The use of PRP in the surgical treatment of rotator cuff tendinopathy has been shown to expedite healing.16,22,25,41,42 However, a study found that the nonsurgical use of PRP injection neither reduces pain nor improves functionality any better than placebo in patients with tendinopathy or partial tear of the rotator cuff who received exercise therapy.24 In the current study, 2 PRP injections were given 30 days apart. The injections were made both into areas of tendinopathy and into the bursa. The continued clinical improvement seen in our patients could be related to the difference in PRP technique.
The improved results obtained during the 3-month follow-up could be related to a delayed effect of the first PRP injection or to a boosting effect of the second injection. These results echo those reported by Rha et al39 but disagree with the findings of Randelli et al,37 who reported that the effect of PRP injection decreased after 3 to 6 months as well as after 12 months. This difference can be attributed to the fact that the patients in the study by Randelli et al37 received only 1 PRP injection whereas in the present study and in that by Rha et al,39 there were 2 injections administered. Another explanation is that while the present research evaluated the effect of PRP injection on partial rotator cuff tears, Randelli et al37 studied the effect of PRP injection on full-thickness rotator cuff tears. Similarly, in studies that investigated the effect of PRP injection on full-thickness rotator cuff tears,5,6,41 PRP injection failed to prove effective in reducing pain and improving shoulder functionality.
The inconclusive results reported in the literature about the effect of PRP injection are also attributable to the fact that different studies use different formulations of PRP. For instance, there is controversy about the use of leukocyte-rich PRP (L-PRP). Whereas some studies have claimed that L-PRP has the antibacterial property of regulating immunity and is the preferred treatment for pain relief in the medium- and long-term,2,13 some researchers believe that the presence of leukocytes in PRP is a cause of inflammation, and the likelihood of repair decreases as the inflammation at the site of injection increases.11,28,29 In the present research, the leukocyte content of the injected PRP was 1 to 1.5 times as high as that of the baseline PRP, suggesting that the presence of leukocytes does not disturb the healing process.
A final point to reiterate is that we found no significant effect of PRP injection on external rotation ROM, a condition also observed by Kesikburun et al,24 while in the exercise group, external rotation ROM was improved similar to other ranges of shoulder motion. We believe that this could be because the amount of external rotation in the PRP group was nearly in the normal range at the baseline (89.9°) but in the exercise group it was 76.2°, which was improved by exercise and mobilization.
The present study also provides more evidence in support of a healing effect of exercise therapy in patients with SAIS. Similarly, the results of other studies23,26,27 indicate that exercise alone is an effective way of reducing pain and improving functionality in such patients. However, unlike our research, Fleming et al17 and Kuhn27 did not report a significant improvement in shoulder ROM. This dissimilarity is perhaps because our exercise protocol focused on both passive and active-assistive exercises and shoulder mobilization in phase 1, but in some of the RCTs evaluated in the study by Kuhn,27 the exercise protocol was limited to pendulum exercises.
We also observed the greatest level of pain relief and the largest increase in flexion, extension, and abduction ROM in the first month of treatment, and this effect improved with the passage of time, as observed 6 months after the first visit. Similar findings are reported in the literature with regard to the positive short-term (6-12 weeks) role of exercise therapy in reducing pain, strengthening the muscles of the rotator cuff, stabilizing the scapula, and increasing shoulder ROM on pain reduction.10,20,30
From another perspective, the frequency at which exercise therapy was provided in the present research was 5 times a week, and the findings align with those of Calis et al,10 who showed that completing exercises 5 days a week for 3 weeks significantly increased flexion, abduction, internal rotation, and external rotation ROM and improved functionality. In addition, the results of the present research, like those of Calis et al,10 indicate that performing more frequent exercises per week can bring about a more significant increase in shoulder ROM.
Concerning the prolonged beneficial effect of exercise therapy, our study cannot provide evidence because the length of the follow-up period was rather limited (ie, a maximum of 6 months). However, Hallgren et al,19 in a clinical trial with a follow-up of 1 year, found that a specific SAIS exercise protocol performed for 3 weeks decreases the need for surgery, suggesting that the effect of exercise therapy persists for at least 1 year. In addition, the studies by Brox et al8,9 show that the effects of 3 to 6 months of strengthening exercises twice per week continue to be seen for 2.5 years.
The present research found no difference between 3 and 6 months of exercise therapy, which may be because the benefits of therapy plateau after 3 months. However, supervision was discontinued after 3 months in this study. In other words, it is possible that the patients did not continue their exercise protocol as prescribed and thereby achieved minimal improvement throughout the rest of the experiment. This shows the importance of supervised exercise as a source of motivation.
Finally, the results show that although patients with SAIS clinically improved as a result of the 2 treatment options under study, paraclinical (ie, MRI) data hardly changed. This finding concurs with the results reported in another study that showed that despite clinical improvement seen with physical therapy, sonography data did not show any tangible change even 9 months after treatment.34
Limitations
As with any research, our study is not without limitations. A major limitation was the absence of a control group without treatment or with placebo injection. Other limitations included the short length of the follow-up period and crude measurement of muscle strength (manual muscle testing instead of a dynamometer).
Conclusion
This study showed that both PRP injection and exercise therapy can significantly reduce pain and improve shoulder ROM and functionality in patients with SAIS, with these beneficial effects lasting for 6 months. In spite of our hypothesis, exercise therapy was found to be more effective than the other treatment option until 3 months after initiation. Moreover, neither treatment choice significantly improved shoulder muscle force. What is more, even though the treatments resulted in clinical improvement, MRI findings did not change.
Acknowledgment
This study was part of a postgraduate MD thesis supported by Iran University of Medical Sciences, Tehran, Iran. The authors would like to give special thanks to Iran University of Medical Sciences. They also thank Mr Mahmood Soleimani, Dr Feras Hakkak, Mrs Pishgah, and Ms Beitollahi for their help with manuscript editing.
Appendix
Four Phases of the Exercise Protocol
Phase 1: Isometric, stretching, pendulum, and passive range of motion exercises.
Phases 2 and 3: Shoulder active-assisted and active range of motion strengthening exercises for shoulder and scapula.
Phase 4: Scapular stabilization.

Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded and supported by the Iran University of Medical Sciences grant 92-01-30-21391.
Ethical approval for this study was obtained from the Research Ethics Committee of the Iran University of Medical Sciences (2013.04.19-21391-89429).
References
- 1. Ainsworth R, Lewis JS. Exercise therapy for the conservative management of full thickness tears of the rotator cuff: a systematic review. Br J Sports Med. 2007;41:200–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Andia I, Latorre P, Gomez M, Burgos-Alonso N, Abate M, Maffulli N. Platelet-rich plasma in the conservative treatment of painful tendinopathy: a systematic review and meta-analysis of controlled studies. Br Med Bull. 2014;110:99–115. [DOI] [PubMed] [Google Scholar]
- 3. Angoorani H, Mazaherinezhad A, Marjomaki O, Younespour S. Treatment of knee osteoarthritis with platelet-rich plasma in comparison with transcutaneous electrical nerve stimulation plus exercise: a randomized clinical trial. Med J Islamic Republic Iran. 2015;29:223. [PMC free article] [PubMed] [Google Scholar]
- 4. Balasubramaniam U, Dissanayake R, Annabell L. Efficacy of platelet-rich plasma injections in pain associated with chronic tendinopathy: a systematic review. Phys Sportsmed. 2015;43:253–261. [DOI] [PubMed] [Google Scholar]
- 5. Barber FA, Hrnack SA, Snyder SJ, Hapa O. Rotator cuff repair healing influenced by platelet-rich plasma construct augmentation. Arthroscopy. 2011;27:1029–1035. [DOI] [PubMed] [Google Scholar]
- 6. Bergeson AG, Tashjian RZ, Greis PE, Crim J, Stoddard GJ, Burks RT. Effects of platelet-rich fibrin matrix on repair integrity of at-risk rotator cuff tears. Am J Sports Med. 2012;40:286–293. [DOI] [PubMed] [Google Scholar]
- 7. Bhattacharyya R, Edwards K, Wallace AW. Does arthroscopic sub-acromial decompression really work for sub-acromial impingement syndrome: a cohort study. BMC Musculoskelet Disord. 2014;15:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brox JI, Gjengedal E, Uppheim G, et al. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prospective, randomized, controlled study in 125 patients with a 2½-year follow-up. J Shoulder Elbow Surg. 1999;8:102–111. [DOI] [PubMed] [Google Scholar]
- 9. Brox JI, Staff PH, Ljunggren AE, Brevik JI. Arthroscopic surgery compared with supervised exercises in patients with rotator cuff disease (stage II impingement syndrome). BMJ. 1993;307:899–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Calis H, Berberoglu N, Calis M. Are ultrasound, laser and exercise superior to each other in the treatment of subacromial impingement syndrome? A randomized clinical trial. Eur J Phys Rehabil Med. 2011;47:375–380. [PubMed] [Google Scholar]
- 11. Carofino B, Chowaniec DM, McCarthy MB, et al. Corticosteroids and local anesthetics decrease positive effects of platelet-rich plasma: an in vitro study on human tendon cells. Arthroscopy. 2012;28:711–719. [DOI] [PubMed] [Google Scholar]
- 12. Di Matteo B, Filardo G, Kon E, Marcacci M. Platelet-rich plasma: evidence for the treatment of patellar and Achilles tendinopathy—a systematic review. Musculoskelet Surg. 2015;99:1–9. [DOI] [PubMed] [Google Scholar]
- 13. Dohan DM, Choukroun J, Diss A, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part III: leucocyte activation: a new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2006;101:e51–e55. [DOI] [PubMed] [Google Scholar]
- 14. Dong W, Goost H, Lin X-B, et al. Treatments for shoulder impingement syndrome: a PRISMA systematic review and network meta-analysis. Medicine (Baltimore). 2015;94:e510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg. 2004;114:1502–1508. [DOI] [PubMed] [Google Scholar]
- 16. Ersen A, Demirhan M, Atalar A, Kapicioğlu M, Baysal G. Platelet-rich plasma for enhancing surgical rotator cuff repair: evaluation and comparison of two application methods in a rat model. Arch Orthop Trauma Surg. 2014;134:405–411. [DOI] [PubMed] [Google Scholar]
- 17. Fleming JA, Seitz AL, Ebaugh DD. Exercise protocol for the treatment of rotator cuff impingement syndrome. J Athl Train. 2010;45:483–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Haahr JP, Østergaard S, Dalsgaard J, et al. Exercises versus arthroscopic decompression in patients with subacromial impingement: a randomised, controlled study in 90 cases with a one year follow up. Ann Rheum Dis. 2005;64:760–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hallgren HCB, Holmgren T, Öberg B, Johansson K, Adolfsson LE. A specific exercise strategy reduced the need for surgery in subacromial pain patients. Br J Sports Med. 2014;48:1431–1436. [DOI] [PubMed] [Google Scholar]
- 20. Hanratty CE, McVeigh JG, Kerr DP, et al. The effectiveness of physiotherapy exercises in subacromial impingement syndrome: a systematic review and meta-analysis. Semin Arthritis Rheum. 2012;42:297–316. [DOI] [PubMed] [Google Scholar]
- 21. Holmgren T, Hallgren HB, Öberg B, Adolfsson L, Johansson K. Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study. BMJ. 2012;344:e787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jo CH, Kim JE, Yoon KS, Shin S. Platelet-rich plasma stimulates cell proliferation and enhances matrix gene expression and synthesis in tenocytes from human rotator cuff tendons with degenerative tears. Am J Sports Med. 2012;40:1035–1045. [DOI] [PubMed] [Google Scholar]
- 23. Kelly SM, Wrightson PA, Meads CA. Clinical outcomes of exercise in the management of subacromial impingement syndrome: a systematic review. Clin Rehabil. 2010;24:99–109. [DOI] [PubMed] [Google Scholar]
- 24. Kesikburun S, Tan AK, Yılmaz B, Yaşar E, Yazıcıoğlu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy a randomized controlled trial with 1-year follow-up. Am J Sports Med. 2013;41:2609–2616. [DOI] [PubMed] [Google Scholar]
- 25. Kobayashi M, Itoi E, Minagawa H, et al. Expression of growth factors in the early phase of supraspinatus tendon healing in rabbits. J Shoulder Elbow Surg. 2006;15:371–377. [DOI] [PubMed] [Google Scholar]
- 26. Kromer TO, Tautenhahn UG, de Bie RA, Staal JB, Bastiaenen CH. Effects of physiotherapy in patients with shoulder impingement syndrome: a systematic review of the literature. J Rehabil Med. 2009;41:870–880. [DOI] [PubMed] [Google Scholar]
- 27. Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Surg. 2009;18:138–160. [DOI] [PubMed] [Google Scholar]
- 28. Loftus ML, Endo Y, Adler RS. Retrospective analysis of postinjection ultrasound imaging after platelet-rich plasma or autologous blood: observational review of anatomic distribution of injected material. AJR Am J Roentgenol. 2012;199:W501–W505. [DOI] [PubMed] [Google Scholar]
- 29. Lopez-Vidriero E, Goulding KA, Simon DA, Sanchez M, Johnson DH. The use of platelet-rich plasma in arthroscopy and sports medicine: optimizing the healing environment. Arthroscopy. 2010;26:269–278. [DOI] [PubMed] [Google Scholar]
- 30. Michaleff ZA, Kamper SJ. PEDro systematic review update: the effectiveness of physiotherapy exercises in subacromical impingement syndrome. Br J Sports Med. 2013;47:927–928. [DOI] [PubMed] [Google Scholar]
- 31. Michener LA, Yesilyaprak SSS, Seitz AL, Timmons MK, Walsworth MK. Supraspinatus tendon and subacromial space parameters measured on ultrasonographic imaging in subacromial impingement syndrome. Knee Surg Sports Traumatol Arthrosc. 2015;23:363–369. [DOI] [PubMed] [Google Scholar]
- 32. Mousavi SJ, Hadian MR, Abedi M, Montazeri A. Translation and validation study of the Persian version of the Western Ontario Rotator Cuff Index. Clin Rheumatol. 2009;28:293–299. [DOI] [PubMed] [Google Scholar]
- 33. Mousavi SJ, Parnianpour M, Abedi M, et al. Cultural adaptation and validation of the Persian version of the Disabilities of the Arm, Shoulder and Hand (DASH) outcome measure. Clin Rehabil. 2008;22:749–757. [DOI] [PubMed] [Google Scholar]
- 34. Nejati P, Akbari F. Exercise therapy for total tear of rotator cuff: a case report. Asian J Sports Med. 2014;5:67–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nejati P, Ghahremaninia A, Mzaherinezhad A. The effect of platelet-rich plasma (PRP) on improvement in pain and symptoms of shoulder subacromial impingement syndrome. Arak Univ Med Sci J. 2015;18:97–105. [Google Scholar]
- 36. Peterson-Kendall F, Kendall-McCreary E, Geise-Provance P, McIntyre-Rodgers M, Romani W. Muscles Testing and Function With Posture and Pain. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 37. Randelli P, Arrigoni P, Ragone V, Aliprandi A, Cabitza P. Platelet rich plasma in arthroscopic rotator cuff repair: a prospective RCT study, 2-year follow-up. J Shoulder Elbow Surg. 2011;20:518–528. [DOI] [PubMed] [Google Scholar]
- 38. Randelli P, Randelli F, Ragone V, et al. Regenerative medicine in rotator cuff injuries. BioMed Res Int. 2014;2014:129515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rha D-W, Park G-Y, Kim Y-K, Kim MT, Lee SC. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: a randomized controlled trial. Clin Rehabil. 2013;27:113–122. [DOI] [PubMed] [Google Scholar]
- 40. Roddy E, Zwierska I, Hay EM, et al. Subacromial impingement syndrome and pain: protocol for a randomised controlled trial of exercise and corticosteroid injection (the SUPPORT trial). BMC Musculoskelet Disord. 2014;15:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Rodeo SA, Delos D, Williams RJ, Adler RS, Pearle A, Warren RF. The effect of platelet-rich fibrin matrix on rotator cuff tendon healing a prospective, randomized clinical study. Am J Sports Med. 2012;40:1234–1241. [DOI] [PubMed] [Google Scholar]
- 42. Uggen JC, Dines J, Uggen CW, et al. Tendon gene therapy modulates the local repair environment in the shoulder. J Am Osteopath Assoc. 2005;105:20–21. [PubMed] [Google Scholar]