Abstract
This article presents a novel visual analytics (VA)‐based clinical decision support (CDS) tool prototype that was designed as a collaborative work between Renaissance Computing Institute and Duke University. Using Major Depressive Disorder data from MindLinc electronic health record system at Duke, the CDS tool shows an approach to leverage data from comparative population (patients with similar medical profile) to enhance a clinicians’ decision making process at the point of care. The initial work is being extended in collaboration with the University of North Carolina CTSA to address the key challenges of CDS, as well as to show the use of VA to derive insight from large volumes of Electronic Health Record patient data. Clin Trans Sci 2011; Volume 4: 369–371
Keywords: electronic health records, patient data, clinical decision support, visual analytics, comparative effectiveness research, evidence‐based medicine
Introduction
The University of North Carolina (UNC) at Chapel Hill and Duke University are recipients of individual Clinical and Translational Science Awards (CTSA) grants in the past. To support clinical and translational research, each of these universities have established individual clinical data warehouses with data from their respective hospital electronic health record (EHR) systems, and are also engaged in research projects that can directly impact patient care. With the data warehouses available, researchers at both universities have access to aggregate patient‐level longitudinal data from their respective institutions. Clinical decision support (CDS) system‐based applications offer promising ways to use clinical warehouse data for patient care. Both UNC and Duke are interested in collaboratively investigating potential new ways to improve effectiveness of physician‐oriented CDS systems that can improve efficiency in selection of treatment and improve the quality of care.
A panel of medical informatics experts representing some of the top‐tier programs in the nation noted the tremendous potential of CDS in clinical care, as well as the barriers to fully realize their utility. 1 These experts identified 10 grand challenges to improve CDS and ensure its wider use. The top four challenges they identified deal with (1) human–computer interface, (2) patient data summaries at the interface, (3) user interface (UI) functions to support prioritization and filtering of CDS recommendations, and (4) combining recommendations with the comorbidities of patients. These four grand challenges motivate the need for new UI approaches for CDS systems to go beyond basic access and view functions.
We present here a point‐of‐care physician oriented CDS tool prototype. Using a visual analytics (VA) approach, the CDS tool UI presents data summaries of patient and comparative population (patients with similar medical profiles) in an interactive visual format. The presented CDS tool was designed as collaborative work between Renaissance Computing Institute and Duke, and the scope of the work is limited to Major Depressive Disorder (MDD) data from the MindLinc EHR (details in next section). This initial work is extended in collaboration with UNC CTSA to address the four key challenges highlighted earlier, and also make a case for the use of VA to derive insight from the large volumes of EHR‐level patient data. Although the presented work is based on patients with MDD, the identified approaches to improve the utility of CDS can be extended to other chronic medical conditions.
MindLinc—EHR Data
More than a decade ago, Dr. Kenneth Gersing at Duke University led the development of an electronic medical record system for behavioral health known as the MindLinc system. 2 Currently, the MindLinc system feeds the largest psychiatry registry in the world, containing nearly 200,000 patients, representing about 2 million visits, and collected from 30 organizations in the United States. The psychiatric data collected includes diagnoses, medications, adverse reactions, as well as outcomes.
The sample de‐identified MDD dataset from MindLinc system that is used for the development of the CDS tool prototype includes 33,536 patient encounters from 3,016 unique patients. The final, compiled MDD dataset included data on prescribed medications, comorbid conditions, demographics (race, gender, and age), visit type (inpatient, outpatient, or emergency), and treatment outcomes. Using the MDD dataset from the MindLinc EHR system, we present a prototype UI that uses VA to aggregate and effectively render the large volume of EHR data.
Dashboard Style VA‐Based UI for Clinical Decision
The discussion in prior sections identify two primary needs to be addressed at the UI level: (1) approaches to reduce cognitive overload from large volumes of EHR data for data interpretation, and (2) approaches for the UI display to support quick and easy data interaction to gather data insight for an informed decision.
VA offers a promising approach to generate visual summaries from data aggregates. Figure 1 shows VA‐based visual data views used to present different characteristics of patient and comparative population information. At the UI level, the physician starts by entering the patient medical record number (pseudo MRN 15057). The CDS tool uses patient MRN as seed data to identify data for patient, and the comparative population. Data results are aggregated and summarized in the form of data views at the UI level to show: (1) patient demographics; (2) visual summary of the medications and their treatment outcome response computed from the identified comparative population; (3) visual display of the comorbid conditions for the patient and identified comparative population; (4) treatment outcome response of the presenting patient in the context of the recommended clinical guideline (guideline for MDD shown); (5) profile overview of the patient’s response to treatment as recorded within the EHRs; (6) projected patient responses to the selected medication (yellow highlight in Figure 2) computed from comparative population data; (7) profile view of the prescribed medications over their different time frames; and (8) quantified patient visit type data (outpatient, inpatient and emergency). At the UI level, all these different data views are coupled together. Any change to data in a single view triggers simultaneous coordinated updates to all the other data views. For example, Figure 2 shows changed% patient improved count for bupropion with a different set of comorbid choices.
Figure 1.
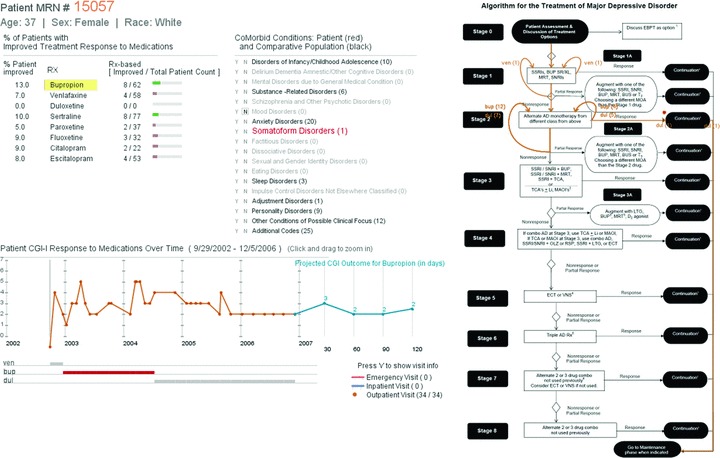
Dashboard view of the visual analytics based clinical decision support tool: (1) Patient demographics, (2) Comparative response to medications, (3) Patient and comparative population comorbidities, (4) Guideline—patient visit view, (5) Temporal view of the patient response to treatment, (6) Projected response to selected medication, (7) Time duration of prescribed medication, and (8) Patient visit type information.
Figure 2.
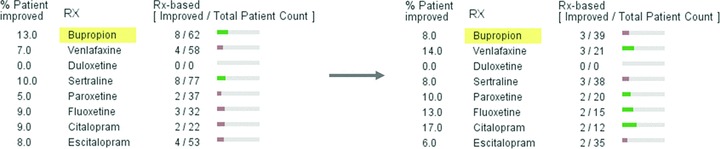
Shows %patient improved count dropped from 13% (left‐hand image) to 8% (right‐hand image) for bupropion when different set of comorbid condition filters are selected.
Discussion and Future Work
The presented CDS tool seeks to bridge the gap between evidence and clinical practice by presenting information in a visual format. The visual display of aggregate data summaries from comparative population offers an easy way to understand large volumes of data, while clearly communicating the underlying quantitative information. CDS tool shown here demonstrates the flexibility that VA offers to aggregate, visualize, and distill large volumes of EHR data at the UI level.
As a potential path forward, we will explore ways to integrate this work with an instance of the MindLinc system. We will perform UI‐level usability tests to evaluate the effectiveness of the visual‐based UI in clinical decision‐making processes. To ease the MindLinc integration process, the initial development work will use a shadow database backend that preserves the MindLinc referential integrity and table relations. We are looking to extend the UI to other chronic conditions (like epilepsy) that are available through North Carolina Translational and Clinical Sciences (NC TraCS) Data Warehouse. 3 We plan to publish our approach and the main findings associated with the CDS tool prototype, and would seek collaboration with other CTSA sites. Finally, we are investigating the use of clinical guidelines as a way to identify biases inherent in the data to ensure partialities do not misinform decision‐making processes.
Acknowledgments
This work was supported by funds from RENCI; a research institute jointly sponsored by University of North Carolina, NC, Duke University, and North Carolina State University. We would also like to thank Ricardo Pietrobon for his comments during the initial development phase; and Bruce Burchett for help with initial MindLinc EHR dataset.
References
- 1. Sittig DF, Wright A, Osheroff JA, Middleton B, Teich JM, Ash JS, Campbell E, Bates DW. Grand challenges in clinical decision support. J Biomed Inform. 2008; 41(2): 387–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gersing K, Krishnan R. Clinical computing: clinical management research information system (CRIS). Psychiatr Serv. 2003; 54(9): 1199–1200. [DOI] [PubMed] [Google Scholar]
- 3. Mostafa J, Moore C. The North Carolina Translational and Clinical Sciences Institute: activities of the biomedical informatics CORE. Clin Transl Sci. 2010; 3(3): 71–72. [DOI] [PMC free article] [PubMed] [Google Scholar]


