Abstract
Pimavanserin (Nuplazid) for the treatment of hallucinations and delusions associated with Parkinson’s disease
INTRODUCTION
Parkinson’s disease (PD) causes a gradual degeneration of nerve cells in a portion of the midbrain called the substantia nigra, which results in a constellation of motor abnormalities, such as bradykinesia, resting tremor, cogwheel rigidity, and postural instability, as well as neuropsychiatric symptoms, including depression, dementia, apathy, hallucinations, and delusions. In patients with PD, neurons die, leading to a lack of the available dopamine in the brain that is responsible for transmitting signals between the areas of the brain that control the coordination of smooth and balanced muscle movement.
Although PD is classified as a movement disorder, approximately 20% to 50% of PD patients develop psychosis, with the most common symptoms being hallucinations and/or delusions.1–6 This may be intrinsic to the disease or a result of adverse effects from the drugs used to treat the motor symptoms (i.e., dopamine agonists, anticholinergics). For some patients, the neuropsychiatric symptoms cause greater morbidity than the motor complications.7
PD-associated psychosis is often not recognized, and very few patients report these symptoms to their providers.5 Regardless of its severity, PD-associated psychosis leads to significantly increased disability, caregiver burden, nursing home placement, morbidity, and mortality, and can negatively affect a patient’s quality of life.8–10 Its clinical features do not resemble other psychotic disorders, such as schizophrenia, because it is developed after a primary diagnosis of PD and primarily consists of paranoid delusions, visual hallucinations, and/or other sensory disturbances, all of which worsen over time. Visual hallucinations of people, animals, or inanimate objects are the most commonly reported symptoms and are mostly observed during the evening hours when stimulation is low.5 Although they occur less frequently, auditory, tactile, olfactory, and gustatory hallucinations have been reported to accompany visual hallucinations.11–12 Currently, no assessment scale for psychosis in PD has been well established.
The absence of standardized diagnostic criteria for PD-associated psychosis, even in the most recent Diagnostic and Statistical Manual of Mental Disorders, led to the formation of the Parkinson’s Disease Working Group in 2007, sponsored by the National Institute of Neurological Disorders and Stroke and the National Institute of Mental Health. The group’s primary goal is to distinguish PD-associated psychosis from other forms of psychosis.13
Underlying medical conditions (e.g., infection in the elderly), pre-existing psychiatric disorders, particularly in the early stages (e.g., dementia with Lewy bodies), and polypharmacy should be considered and ruled out prior to initiating treatment of psychosis in PD.14–16
The first-line strategy in the management of psychosis in PD is the gradual removal of the multiple medications used to manage motor symptoms in the following order: anticholinergics, selegiline, amantadine, dopamine agonists, catechol-O-methyltransferase inhibitors, and lastly, levodopa/carbidopa.17–18
Despite their boxed warnings,19 second-generation antipsychotics have often been used off-label for treating the psychosis associated with PD, but they have led to the worsening of motor symptoms.20 Although it was recommended for the treatment of PD psychosis in a 2007 meta-analysis,21 clozapine is not approved by the Food and Drug Administration (FDA) to treat PD-associated psychosis. In addition, clozapine is often avoided due to its potential for drug-induced agranulocytosis and its risk evaluation and mitigation strategy (REMS) program.20
Pimavanserin (Nuplazid, Acadia Pharmaceuticals, Inc.), approved by the FDA in 2016, is a first-in-class atypical antipsychotic that does not induce clinically significant antagonism of dopaminergic, adrenergic, histaminergic, or muscarinic receptors. It is the first FDA-approved drug indicated for the treatment of the hallucinations and delusions in PD-associated psychosis.22
DESCRIPTION
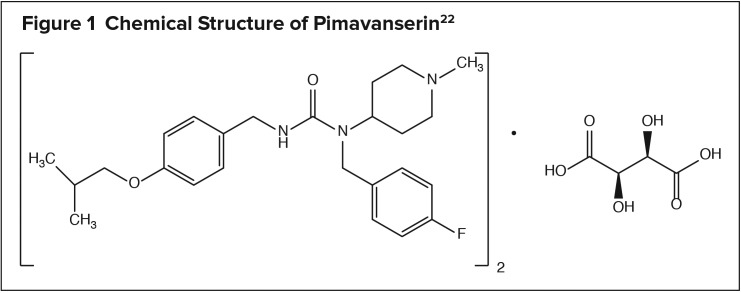
Pimavanserin, an atypical anti-psychotic, is present in Nuplazid as pimavanserin tartrate salt with the chemical name urea, N-[(4-fluorophenyl)methyl]-N-(1-methyl-4-piperidinyl)-N’-[[4-(2-methylpropoxy)phenyl]methyl]-,(2R,3R)-2,3-dihydroxybutanedioate (2:1). The drug’s chemical structure is illustrated in Figure 1. Pimavanserin tartrate is freely soluble in water. Its molecular formula is (C25H34FN3O2)2 • C4H6O6, and its molecular weight is 1005.20 (tartrate salt). The molecular formula of pimavanserin free base is C25H34FN3O2, and its molecular weight is 427.55.22
Figure 1.
Chemical Structure of Pimavanserin22
Pimavanserin is a round, white to off-white, immediate-release, film-coated, once-daily oral tablet containing 20 mg of pimavanserin tartrate, which is equivalent to 17 mg of pimavanserin free base, and inactive ingredients.22
MECHANISM OF ACTION
Although the exact mechanism of action of pimavanserin is unknown, a combination of inverse agonist and antagonist activity at the serotonin 2A receptors (5-HT2A) and, to a lesser extent, at the 5-HT2C receptors, has been theorized. During clinical trials, pimavanserin showed no appreciable binding affinity for dopamine (including D2), histamine, muscarinic, or adrenergic receptors.22
PHARMACOKINETICS
Pimavanserin and its major active N-desmethylated metabolite AC-279 have demonstrated a time to maximum plasma concentration of six hours (range, four to 24 hours) with mean plasma half-lives of approximately 57 hours for pimavanserin and 200 hours for AC-279. In the presence of high-fat meals, its maximum plasma concentration and area under the curve were decreased by 9% and increased by 8%, respectively. Pimavanserin has dose-proportional pharmaco-kinetics after single oral doses from 17 to 255 mg (0.5–7.5 times the dosage recommendation) and yields similar results in both patients with PD and healthy individuals. The bioavailability of pimavanserin oral tablets and oral solution is identical.22
Pimavanserin had a mean (SD) apparent volume of distribution of 2,173 (307) L following the administration of one 34-mg dose. It is approximately 95% plasma-protein–bound, which is dose-dependent and demonstrates no significant change over dosing time from days 1 through 14. The drug is metabolized predominantly by cytochrome P450 (CYP) 3A4 and CYP3A5 and to a lesser extent by CYP2J2, CYP2D6, and other CYP and flavin-containing monooxygenase enzymes. It does not cause clinically significant CYP3A4 inhibition or induction.22
Approximately 0.55% and 1.53% of pimavanserin are eliminated unchanged in the urine and feces after 10 days, respectively, following a 34-mg dose; pimavanserin and AC-279 were detected in the urine at less than 1% of the administered dose.22
Patients with normal renal function and those with mild-to-moderate renal dysfunction demonstrated similar pimavanserin exposure based on population pharmacokinetic analysis. No studies were conducted in patients with severe renal impairment or mild-to-severe hepatic dysfunction. The pharmacokinetics of pimavanserin were not affected by age, gender, ethnicity, or weight. The maximum plasma concentration and area under the curve for pimavanserin increased by 1.5-fold and threefold, respectively, during drug interaction studies with a strong CYP3A4 inhibitor (i.e., ketoconazole).22
PIVOTAL CLINICAL TRIAL
A six-week, randomized, placebo-controlled, parallel-group study (N = 199) was conducted to establish the efficacy of pimavanserin 34 mg once daily as a treatment for hallucinations and delusions associated with PD psychosis. The trial included men and women 40 years of age and older in the outpatient setting with a diagnosis of PD established at least one year prior to the study who had severe and frequent psychotic symptoms (hallucinations and/or delusions) that started after diagnosis and warranted antipsychotic treatment. Patients were randomized 1:1 to receive pimavanserin 34 mg once daily or placebo once daily. Inclusion criteria included Folstein Mini–Mental State Examination score of 21 or greater, ability to self-report symptoms, and stability on PD medications prior to and throughout the study period.22
Primary efficacy was evaluated based on change from baseline to week 6 total score using the PD-Adapted Scale for the Assessment of Positive Symptoms (SAPS–PD), a nine-item assessment for which each item is scored on a scale of 0 to 5 (0 = no symptoms; 5 = severe/frequent symptoms), with a total score ranging from 0 to 45. Higher SAPS–PD total scores indicate greater severity of illness.22
As measured by central, independent, and blinded raters using the SAPS–PD scale, pimavanserin 34 mg (n = 95) demonstrated significant efficacy over placebo (n = 90) in decreasing the frequency and/or severity of hallucinations and delusions. An effect was seen on both the hallucination and delusion components of the SAPS–PD. Using the Unified Parkinson’s Disease Rating Scale Parts II and III during the six-week double-blind treatment period, pimavanserin 34 mg did not show an effect on motor function when compared with placebo.22
SAFETY PROFILE
Warnings and Precautions
The prescribing information for pimavanserin contains a boxed warning for increased mortality in elderly patients (65 years of age or older) with dementia-related psychosis. Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Pimavanserin is not indicated for the treatment of patients with dementia-related psychosis unrelated to PD-associated hallucinations and delusions.22
Pimavanserin prolongs the QT interval, and its use should be avoided in patients with known QT prolongation or in combination with other drugs known to prolong the QT interval. This includes some antiarrhythmics (e.g., quinidine, procainamide, amiodarone), certain anti-psychotic medications (e.g., ziprasidone, chlorpromazine, thioridazine), and certain antibiotics (e.g., gatifloxacin, moxifloxacin) (Table 1). See the full prescribing information for details about clinically important drug interactions.22
Table 1.
Drug Interactions With Pimavanserin22
| Drugs | Clinical Effect | Intervention |
|---|---|---|
| QT Interval Prolongation | ||
| Class 1A antiarrhythmics (quinidine, procainamide, disopyramide) |
Pimavanserin may potentially add to the effects of increased QT interval when administered with these drugs, increasing the risk of cardiac arrhythmia | Avoid the combination of pimavanserin and drugs known to prolong QT interval |
| Class 3 antiarrhythmics (amiodarone, sotalol) | ||
| Antipsychotics (ziprasidone, chlorpromazine, thioridazine) | ||
| Antibiotics (gatifloxacin, moxifloxacin) | ||
| Strong CYP3A4 Inhibitors | ||
| Itraconazole, ketoconazole, clarithromycin, indinavir | Pimavanserin plasma level may be increased when administered with a strong CYP3A4 inhibitor | Reduction of pimavanserin dosage may be needed when administered concomitantly with a strong CYP3A4 inhibitor |
| Strong CYP3A4 Inducers | ||
| Rifampin, carbamazepine, phenytoin, St. John’s wort | Pimavanserin plasma level may be decreased when administered with a strong CYP3A4 inducer | Increase of pimavanserin dosage may be needed when administered concomitantly with a strong CYP3A4 inducer |
CYP3A4 = cytochrome P450 3A4
Pimavanserin should also be avoided in patients with a history of cardiac arrhythmias, as well as other circumstances that may increase the risk of the occurrence of torsades de pointes and/or sudden death, including symptomatic bradycardia, hypokalemia or hypomagnesemia, and the presence of congenital prolongation of the QT interval.22
Adverse Events
In clinical trials, the most common adverse events that occurred in 5% or more of pimavanserin-treated patients and at twice the rate of placebo were peripheral edema, nausea, and confusional state. Hallucinations, constipation, and gait disturbances were also observed at an incidence of 2% or greater in pimavanserin-treated patients and at twice the rate of placebo. Treatment was discontinued in 8% (16 of 202) of pimavanserin-treated patients and in 4% (10 of 231) of placebo-treated patients due to hallucinations (2% versus less than 1%, respectively), urinary tract infection (1% versus less than 1%, respectively), and fatigue (1% versus 0%, respectively).22
Use in Specific Populations
Pregnancy and Lactation
No data are available regarding pimavanserin-induced major congenital malformations, miscarriage, or other birth defects in humans. In animal studies, no developmental effects were observed when oral pimavanserin was administered at up to 10 or 12 times the maximum recommended human dose (MRHD) of 34 mg daily to rats and rabbits, respectively. However, maternal toxicity and lower pup survival and body weight were reported following administration of two times the MRHD of pimavanserin to pregnant rats during pregnancy and lactation.22
Pimavanserin has not been studied for excretion in human milk, the effects on the breastfed infant, or the effects on milk production. The manufacturer recommends weighing the risks versus the benefits of treatment prior to the initiation of pimavanserin during lactation.22
Renal and Hepatic Impairment
Dose adjustment of pimavanserin in patients with mild-to-moderate renal impairment (creatinine clearance [CrCl] of 30 mL/min or greater) is not required, but use of the drug in patients with severe renal impairment (CrCL of less than 30 mL/min) or with any hepatic impairment is not recommended.22
Drug–Drug Interactions
Coadministration of pimavanserin and strong CYP3A4 inhibitors (e.g., itraconazole, ketoconazole, clarithromycin, indinavir) increases the plasma concentration of pimavanserin; therefore, a dose reduction of pimavanserin is recommended. Patients should be monitored for efficacy, and a dose increase may be needed if pimavanserin is administered with strong CYP3A4 inducers (e.g., rifampin, phenytoin, carbamazepine, St. John’s wort).22
No dosage adjustment is required when carbidopa/levodopa is administered concomitantly with pimavanserin based on pharmacokinetic studies.22
DOSAGE AND ADMINISTRATION
The recommended dose of pimavanserin is 34 mg taken orally as two 17-mg tablets once daily with or without food and without titration. With strong CYP3A4 inhibitors (e.g., ketoconazole), the recommended dose of pimavanserin is 17 mg once daily. Monitor patients for reduced efficacy and potentially increase the dose when pimavanserin is administered with strong CYP3A4 inducers.22
P&T COMMITTEE CONSIDERATIONS
Pimavanserin significantly reduced PD-associated psychotic symptoms compared with placebo in clinical studies and is the only FDA-approved treatment for this condition. Other atypical antipsychotics have shown efficacy, but have been found to worsen patients’ motor symptoms.20 Although clozapine has demonstrated efficacy in treating PD-associated psychosis in clinical studies, it is not approved by the FDA for this indication. In addition, the boxed warning for clozapine is extensive and includes a REMS requirement,20 making pimavanserin an alternative worthy of formulary consideration.
The average wholesale price for a one-month supply of pimavanserin at the recommended daily dose of 34 mg (as two 17-mg tablets) is $2,560.23
CONCLUSION
Psychotic symptoms are common in Parkinson’s disease as a result of patho-physiological changes involving many factors, including the motor symptoms of the disease; the drug-related adverse effects of treatment; multiple neuro-chemicals (i.e., dopamine, serotonin, acetylcholine); changes in sleep and perception; and the patient’s genetics. PD-associated psychosis, which is associated with significantly increased morbidity and mortality, had no FDA-approved treatment until the agency OK’d pimavanserin in 2016. Although this new treatment has demonstrated its efficacy and relative safety, additional studies—including those of longer duration, larger sample size, and more specific patient populations—are needed to enhance pimavanserin’s safety and efficacy profile.
Footnotes
Disclosures: The author reports no financial or commercial relationships in regard to this article.
REFERENCES
- 1.Forsaa EB, Larsen JP, Wentzel-Larsen T, et al. A 12-year population-based study of psychosis in Parkinson disease. Arch Neurol. 2010;67(8):996–1001. doi: 10.1001/archneurol.2010.166. [DOI] [PubMed] [Google Scholar]
- 2.Fénelon G, Alves G. Epidemiology of psychosis in Parkinson’s disease. J Neuro Sci. 2010;289(1–2):12–17. doi: 10.1016/j.jns.2009.08.014. [DOI] [PubMed] [Google Scholar]
- 3.Cummings J, Isaacson S, Mills R, et al. Pimavanserin for patients with Parkinson’s disease psychosis: a randomised, placebo-controlled phase 3 trial. Lancet. 2014;383(9916):533–540. doi: 10.1016/S0140-6736(13)62106-6. [DOI] [PubMed] [Google Scholar]
- 4.Factor SA, Feustel PJ, Friedman JH, et al. Longitudinal outcome of Parkinson’s disease patients with psychosis. Neurology. 2003;60(11):1756–1761. doi: 10.1212/01.wnl.0000068010.82167.cf. [DOI] [PubMed] [Google Scholar]
- 5.Fénelon G, Mahieux F, Huron R, Ziegler M. Hallucinations in Parkinson’s disease: prevalence, phenomenology, and risk factors. Brain. 2000;123(pt 4):733–745. doi: 10.1093/brain/123.4.733. [DOI] [PubMed] [Google Scholar]
- 6.Sanchez-Ramos JR, Ortoll R, Paulson GW. Visual hallucinations associated with Parkinson disease. Arch Neurol. 1996;53(12):1265–1268. doi: 10.1001/archneur.1996.00550120077019. [DOI] [PubMed] [Google Scholar]
- 7.Weiss HD, Marsh L. Impulse control disorders and compulsive behaviors associated with dopaminergic therapies in Parkinson disease. Neurol Clin Pract. 2012;2(4):267–274. doi: 10.1212/CPJ.0b013e318278be9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schrag A, Ben-Shlomo Y, Quinn N. How common are complications of Parkinson’s disease? J Neurol. 2002;249(4):419–423. doi: 10.1007/s004150200032. [DOI] [PubMed] [Google Scholar]
- 9.Goetz CG, Fan W, Leurgans S, et al. The malignant course of “benign hallucinations” in Parkinson disease. Arch Neurol. 2006;63(5):713–716. doi: 10.1001/archneur.63.5.713. [DOI] [PubMed] [Google Scholar]
- 10.Mack J, Rabins P, Anderson K, et al. Prevalence of psychotic symptoms in a community-based Parkinson disease sample. Am J Geriatr Psychiatry. 2012;20(2):123–132. doi: 10.1097/JGP.0b013e31821f1b41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marsh L, Williams JR, Rocco M, et al. Psychiatric comorbidities in patients with Parkinson disease and psychosis. Neurology. 2004;63(2):293–300. doi: 10.1212/01.wnl.0000129843.15756.a3. [DOI] [PubMed] [Google Scholar]
- 12.Aarsland D, Larsen JP, Cummins JL, Laake K. Prevalence and clinical correlates of psychotic symptoms in Parkinson disease: a community-based study. Arch Neurol. 1999;56(5):595–601. doi: 10.1001/archneur.56.5.595. [DOI] [PubMed] [Google Scholar]
- 13.Ravina B, Marder K, Fernandez HH, et al. Diagnostic criteria for psychosis in Parkinson’s disease: report of an NINDS/NIMH work group. Mov Disord. 2007;22(8):1061–1068. doi: 10.1002/mds.21382. [DOI] [PubMed] [Google Scholar]
- 14.Wint DP, Okun MS, Fernandez HH. Psychosis in Parkinson’s disease. J Geriatr Psychiatry Neurol. 2004;17(3):127–136. doi: 10.1177/0891988704267457. [DOI] [PubMed] [Google Scholar]
- 15.Goetz CG, Vogel C, Tanner CM, et al. Early dopaminergic drug-induced hallucinations in parkinsonian patients. Neurology. 1998;51(3):811–814. doi: 10.1212/wnl.51.3.811. [DOI] [PubMed] [Google Scholar]
- 16.Henderson MJ, Mellers JDC. Psychosis in Parkinson’s disease: between a rock and a hard place. Int Rev Psychiatry. 2000;12:319–334. [Google Scholar]
- 17.Fernandez HH, Friedman JF. The role of atypical antipsychotics in the treatment of movement disorders. CNS Drugs. 1999;11(6):467–483. [Google Scholar]
- 18.Friedman JH, Fernandez HH. The non-motor problems of Parkinson’s disease. Neurology. 2000;6:18–27. [Google Scholar]
- 19.Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294(15):1934–1943. doi: 10.1001/jama.294.15.1934. [DOI] [PubMed] [Google Scholar]
- 20.Shotbolt P, Samuel M, David A. Quetiapine in the treatment of psychosis in Parkinson’s disease. Ther Adv Neurol Disord. 2010;3(6):339–350. doi: 10.1177/1756285610389656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frieling H, Hillemacher T, Ziegenbein M, et al. Treating dopamimetic psychosis in Parkinson’s disease: structured review and meta-analysis. Eur Neuropsychopharmacol. 2007;17(3):165–171. doi: 10.1016/j.euroneuro.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Nuplazid (pimavanserin) prescribing information. San Diego, California: Acadia Pharmaceuticals, Inc.; 2016. [Google Scholar]
- 23.Red Book Online. Ann Arbor, Michigan: Truven Health Analytics; [Accessed April 7, 2017]. [Google Scholar]