Abstract
Background
In clinical trials alcohol brief intervention (BI) in adult primary care has been efficacious in reducing alcohol consumption, but we know little about its impact on health outcomes. Hypertension is a prevalent and costly chronic condition in the U.S. and worldwide, and alcohol use is a modifiable hypertension risk factor.
Objective
To evaluate the effect of receiving BI for unhealthy drinking on blood pressure (BP) control among adult hypertensive patients by analyzing secondary data from a clustered, randomized controlled trial on alcohol screening, brief intervention and referral to treatment (SBIRT) implementation by primary care physicians (PCP intervention arm) and non-physician providers and medical assistants (NPP&MA intervention arm) in a large, integrated health care delivery system.
Design
Observational, prospective cohort study.
Subjects
3,811 adult hypertensive primary care patients screening positive for past-year heavy drinking at baseline, of which 1,422 (37%) had an electronic health record BP measure at baseline and 18-month follow-up.
Main Outcome Measures
Change in BP and controlled BP (systolic/diastolic BP <140/90 mmHg).
Results
Overall no significant associations were found between alcohol BI and BP change at 18-month follow-up when analyzing the combined sample of subjects in both intervention arms. However, moderation analyses found that receiving BI for positive past-year unhealthy drinking was positively associated with better BP control at 18 months in the PCP intervention arm, and for those with lower heavy drinking frequency and poor BP control at the index screening.
Conclusions
Our findings suggest that hypertensive patients may benefit from receiving physician brief intervention for unhealthy alcohol use in primary care. Findings also highlight potential population-level benefits of alcohol BI if widely applied, suggesting a need for the development of innovative strategies to facilitate SBIRT delivery in primary care settings.
Keywords: alcohol screening and brief intervention, hypertension, blood pressure control
1. Introduction
Alcohol brief intervention (BI) in adult primary care has been found efficacious in clinical trials in reducing alcohol consumption, especially among non-dependent, at-risk drinkers (Ballesteros, Duffy, Querejeta, Arino, & Gonzalez-Pinto, 2004; Jonas et al., 2012; E. F. Kaner et al., 2007; Whitlock et al., 2004). However, implementation of alcohol BI in routine adult primary care remains a challenge. Further, evidence from clinical trials of the efficacy of BI has not been well translated into real-world settings. While a recent review of systematic reviews and meta-analyses (Faries, Leon, Haro, & Obenchain, 2010) supports the effectiveness of BI at reducing alcohol related problems across a wide range of patients in primary care, findings from limited evaluations of implementation studies in adult primary care found no significant effects of BI on drinking outcomes (Hilbink, Voerman, van Beurden, Penninx, & Laurant, 2012; E. Kaner et al., 2013; Williams et al., 2014).
The literature is even more limited on the impact of alcohol BI on health outcomes. The high burden of unhealthy drinking and alcohol use disorders among adult primary care patients with chronic conditions is well recognized, especially among those with hypertension, diabetes and depression (Babor et al., 2012; Boschloo et al., 2012; Cook & Cherpitel, 2012; Engler, Ramsey, & Smith, 2013; Klatsky, 2004; Mertens, Weisner, Ray, Fireman, & Walsh, 2005; Timko, Kong, Vittorio, & Cucciare, 2016). Hypertension is an important condition to assess, as it affects about one-third of the U.S. adult population (Lewington et al., 2002; Shaw, Handler, Wall, & Kanter, 2014), and when uncontrolled contributes significantly to morbidity and mortality (Egan, Zhao, & Axon, 2010; Vasan et al., 2001). Excessive alcohol consumption is associated with adverse blood pressure (BP) changes (Klatsky, 2004; Miller, Anton, Egan, Basile, & Nguyen, 2005) and noncompliance with antihypertensive treatment (Bryson et al., 2008; Cook & Cherpitel, 2012). Thus, BI to reduce risky drinking would seem to offer promise for improving health outcomes such as hypertension. A recent review (Timko et al., 2016) concluded that findings from the few studies that have been conducted suggest positive effects of alcohol BI on BP outcomes among hypertensive patients. However, out of the six studies on alcohol BI among patients with hypertension, only three examined BP outcomes, and two of these had very small sample sizes. Expanding the scientific knowledge base on the relationship between alcohol BI and health outcomes for primary care patients with chronic conditions is a critical gap.
This observational, prospective cohort study aims to evaluate the effect of BI for unhealthy drinking on BP control among adult hypertensive patients through secondary analysis of data from a clustered, randomized controlled implementation trial comparing alcohol screening, brief intervention or referral to treatment (SBIRT) delivered by physicians versus non-physician providers versus usual care (Mertens et al., 2015). We examine the effect of BI on BP and BP control, taking into consideration initial BP control status and drinking level. The original trial found significant differences in SBIRT implementation outcomes across delivery models, with screening rates highest if performed by medical assistants, but BI or referral rates among patients screening positive highest if delivered by primary care physicians. Informed by these findings and the literature, we hypothesize that the association between receiving BI and BP will be moderated by study intervention arm, baseline unhealthy drinking level and baseline BP status.
2. Methods
2.1. Settings and sample
The Alcohol Drinking as a Vital Sign (ADVISe) trial evaluated alcohol SBIRT implementation in a large, integrated health care delivery system by randomizing 54 adult primary care clinics to three intervention arms: 1) PCP intervention arm, with SBIRT delivered by primary care physicians, 2) NPP&MA intervention arm, in which medical assistants (MAs) screened and non-physician providers (NPPs) such as clinical health educators, behavioral medicine specialists or registered nurses delivered brief intervention and referral to treatment, and 3) usual care as Control arm. In both intervention arms, providers were trained to deliver the same intervention, drawn from the NIAAA Guide (National Institute on Alcohol Abuse and Alcoholism, 2005). Patients who screened positive on the unhealthy drinking questions would receive brief intervention consisting of providers stating their concern and advising them to cut back to low risk limits or abstain, as outlined in the NIAAA Guide (National Institute on Alcohol Abuse and Alcoholism, 2005). Providers were trained in brief motivational intervention, and to: 1) incorporate salient medical conditions if possible, 2) ask patients how ready they were to make the recommended changes, and 3) assist in goal-setting to reduce or quit drinking if the patient was willing. Patients were also given the NIAAA publication “Tips for Cutting Down on Drinking” (National Institute on Alcohol Abuse and Alcoholism, 2007).
In the first year of the study, 639,613 unique patients had visits across all study sites. The trial found low screening and intervention rates in the Control arm (Mertens et al., 2015). Thus, we include only patients in the two intervention arms in this study (218,667 in PCP intervention arm; 223,147 in NPP&MA intervention arm). Among them, 176,273 (39.9%) were screened with the evidence-based NIH screener asking the number of times they exceeded the CDC/NIH daily drinking limits in the past year (no more than 4 drinks for men; no more than 3 for women and seniors) (National Institute on Alcohol Abuse and Alcoholism, 2005; P. C. Smith, Schmidt, Allensworth-Davies, & Saitz, 2009). Of those screened, 18,689 (10.6%) reported at least one day drinking above daily limits; among them 1,878 (10%) received BI per the electronic health record (EHR). See Mertens et al. for details of the methods (Mertens et al., 2015).
For this current study, the analytical sample consisted of those in the ADVISe year 1 cohort who: (1) were in the PCP or NPP&MA intervention arm, (2) exceeded CDC/NIH daily drinking limits in the past year (National Institute on Alcohol Abuse and Alcoholism, 2005; P. C. Smith et al., 2009) and (3) had a hypertension diagnosis in the year prior to the index screening (N=3,811). Of these, 1,422 (37.3%) had an EHR recorded BP measure at both index screening and 18-month follow-up (allowing a 90-day window from 45 days prior to 45 days after the exact follow-up date).
2.2. Measures
The outcome measures were change in BP, and “controlled BP” (systolic/diastolic BP <140/90 mmHg), at 18-month follow-up per EHR records. For multiple EHR measures, the first was used.
The predictor of interest was receipt of BI for unhealthy drinking, measured as having a visit in which a brief intervention was recorded at, or within 45 days of, the positive screening visit. We allowed a 45-day window because providers were trained to schedule a follow-up visit for the BI within 6 weeks if unable to complete during the screening visit. We examined the EHR tool (containing fields for providers to record brief interventions) and also the diagnostic “V-code” for “Counseling, Alcohol Prevention” as indication of brief intervention or referral (as per the training).
We examined three potential moderators: (1) intervention arm (PCP or NPP&MA intervention arms), (2) baseline unhealthy drinking days (<8 or 8+ days in past year) and (3) baseline BP control status (controlled or uncontrolled, defined based on whether systolic/diastolic BP <140/90 mmHg). Baseline unhealthy drinking days were dichotomized as <8 or 8+ days in past year, because prior research found that a threshold of 8 times or more predicted dependence risk and has been used to distinguish severity in studies of brief interventions (Saitz, Cheng, Allensworth-Davies, Winter, & Smith, 2014).
Patient demographic (age, gender, race/ethnicity) and clinical characteristics (medical and psychiatric comorbidities) were extracted from the EHR. We also identified presence of a psychiatric diagnosis (i.e., psychoses, neurotic, personality and other psychiatric disorders) and presence of a chronic disease diagnosis (i.e., Arthritis, Chronic Pain, Diabetes Mellitus, Asthma, Ischemic Heart Disease, Congestive Heart Failure, Stroke/Cerebrovascular Accident, Epilepsy, Parkinson’s Disease, End-Stage Renal Disease, HIV, Osteoporosis, Chronic Obstructive Pulmonary Disease) in the year prior to each patient’s index screening using data extracted from the EHR. The demographic and clinical variables were used for assessing differences between those with and without documented BIs, and for generating the proper inverse probability weights to account for the potential selection and attrition biases (see Statistical Analysis below).
2.3. Statistical Analysis
We compared differences in patient characteristics at index screening, and BP at index screening and 18-month follow-up, between those with and without documented BIs by conducting t-tests for continuous variables and chi-square tests for categorical variables. We next fit general linear and logistic regression models to examine associations between documented BI and change in BP and controlled BP at 18 months, respectively, and addressed issues of potential treatment selection bias and attrition bias with inverse probability weighting (IPW) (Seaman & White, 2013; Xu et al., 2010). We first fit a logistic regression model predicting documented BI at index screening, using a set of potential predictors identified a priori (demographics, comorbidity, unhealthy drinking frequency and BP at index screening, clinic and intervention arm) (the treatment model), and next fit a logistic regression model predicting having a follow-up BP measure, including the same set of predictors used in the treatment model and an indicator for documented BI at index screening (the missingness model). The set of potential predictors that were included in the treatment and missingness models were factors found to be associated with receiving BI in the parent trial (Mertens et al., 2015) or in the bivariate analyses of the current study. We then generated a stabilized weight for each subject using the predicted values from both models. Finally, we fit weighted general linear and logistic regression models to examine the association between documented BI and BP outcomes, and examined the potential moderating effects of intervention arm, baseline unhealthy drinking days and baseline BP control status. For the moderation analyses, all main effects and potential interaction terms with BI were included initially; if interaction terms were statistically significant, all main effects and all relevant lower-order interaction terms involved were retained. Analyses were conducted using SAS 9.3.
3. Results
3.1. Baseline Characteristics and BP Change between Those with and Without alcohol BI
No significant differences were found in average age or gender distribution between those with and without a documented BI, but there were higher proportions of Asian Pacific Islanders, Hispanics or other racial/ethnic groups, and higher proportions of patients with an alcohol use disorders, among those with a documented BI (Table 1). When analyzing subjects in both intervention arms combined together, no significant differences in either average systolic and diastolic BP at index screening, or change in systolic and diastolic BP at 18 months, were found between those with and without a documented BI. However, results from stratified analyses by intervention arm indicated that there were significantly greater declines in BP at 18 months for those with documented BIs in the PCP intervention arm only (mean/standard deviation= −6.4/21.5 vs. 0.7/19.1, p<0.05 and −5.0/10.7 vs. −0.6/11.2, p<0.01 for systolic and diastolic BP change at 18 months, respectively).
Table 1.
Patient characteristics at index screening and blood pressure at index screening and 18-month follow-up among adult hypertensive patients who did and did not receive alcohol brief intervention (N=1422)
| BI (N=115) |
No BI (N=1307) |
P value | |
|---|---|---|---|
| Age in years, mean (SD) | 56.6 (11.4) | 58.6 (13.0) | NS |
| Female gender (%) | 24.4 | 30.9 | NS |
| Race/ethnicity (%) | |||
| African American | 7.2 | 7.8 | 0.0399 |
| Asian Pacific Islander | 10.8 | 7.4 | |
| Hispanic | 23.4 | 16.9 | |
| White | 49.6 | 63.3 | |
| Other | 9.0 | 4.6 | |
| Diagnosis of comorbid conditions received in the year prior to index screening (%) | |||
| Alcohol use disorders | 29.6 | 9.6 | <0.0001 |
| Drug use disorders | 4.4 | 1.7 | 0.0607 |
| Psychiatric | 26.1 | 23.0 | NS |
| Other chronic conditions | 59.1 | 60.0 | NS |
| SBP at index screening, mean (SD) | 134.0 (17.6) | 133.0 (16.8) | NS |
| DBP at index screening, mean (SD) | 79.1 (11.9) | 77.9 (11.8) | NS |
| Change in SBP at 18 months, mean (SD) | −5.1 (21.2) | −3.2 (21.3) | NS |
| Change in DBP at 18 months, mean (SD) | −3.8 (12.4) | −2.2 (12.6) | NS |
Notes: All blood pressure measurements are expressed as mmHg. BI=brief intervention. DBP=diastolic blood pressure. NS=Non-significant at p<0.05 level. SBP=systolic blood pressure. SD=standard deviation.
3.2. Main Effects of BI on BP Outcomes in IPW Models without Interaction Terms
Findings from the weighted general linear models without interaction terms between BI and the three potential moderators found no significant main effects of alcohol BI on changes in either SBP (adjusted mean decline of 3.83 and 3.40 mmHg for those with and without documented BI) or DBP (adjusted mean decline of 1.33 and 2.45 mmHg for those with and without documented BI) at 18-month follow-up among all hypertensive patients screening positive for unhealthy drinking. Findings from the weighted logistic regression model without the interaction terms between BI and the three potential moderators found a negative association between alcohol BI and having controlled BP at 18 months (odds ratio [95% confidence interval]=0.59 [0.40, 0.87], p<0.01) among all hypertensive patients screening positive for unhealthy drinking.
3.3. Moderation Analyses of Intervention Arm, Baseline Unhealthy Drinking Days and Baseline BP Control Status
We examined the potential moderating effects of intervention arm, baseline unhealthy drinking days and baseline BP control status on the associations between alcohol BI and BP outcomes by fitting weighted general linear and logistic regression models with the interaction terms of BI and each of the three moderators. Results from the weighted general linear models including the interaction terms between BI and the three potential moderators suggest a positive association between documented BI and greater BP decline at 18 months for those with lower unhealthy drinking frequency (<8 heavy drinking days/past year)(Saitz et al., 2014) at index screening (p<0.01 for the 2-way interaction terms of BI and unhealthy drinking frequency at index screening, and p=0.05 for the 3-way interaction terms of BI, unhealthy drinking frequency at index screening and intervention arm); this positive BI effect among those with only 1–7 heavy drinking days was found for patients in both PCP and NPP&MA intervention arms (adjusted mean decline of systolic BP was 22.1 and 17.5 mmHg, respectively, for those with documented BI, compared to 6.2 and 7.8 mmHg, respectively, for those without; p<0.1 in the PCP arm and p<0.01 in the NPP&MA arm) (Figure 1). Documented BI was also associated with greater diastolic BP decline among those with only 1–7 heavy drinking days (adjusted mean decline was 6.7 mmHg for those with documented BI, compared to 3.1 mmHg for those without) but the difference was not statistically significant (not shown). For those reporting 1–7 past-year heavy drinking days whose BP was not well controlled at index screening, the adjusted mean decline of systolic BP was 37.8 mmHg for those with documented BI, compared to 17.2 mmHg among those without (p<0.01) (Figure 2).
Figure 1.
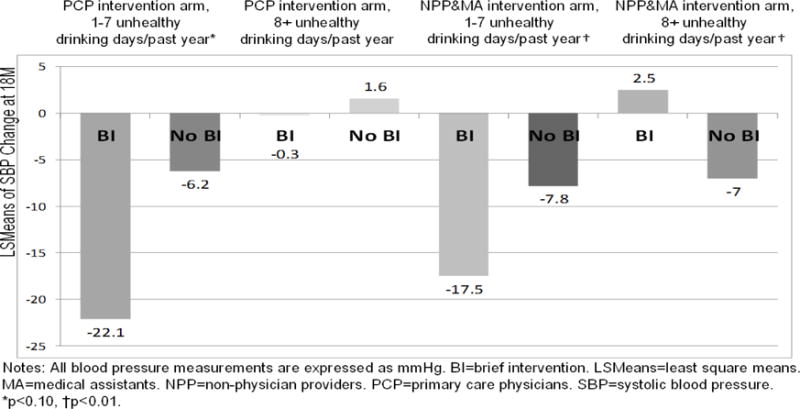
Moderating Effects of Intervention Arm and Unhealthy Drinking Level at Index Screening on Systolic Blood Pressure Change at 18 Months
Figure 2.
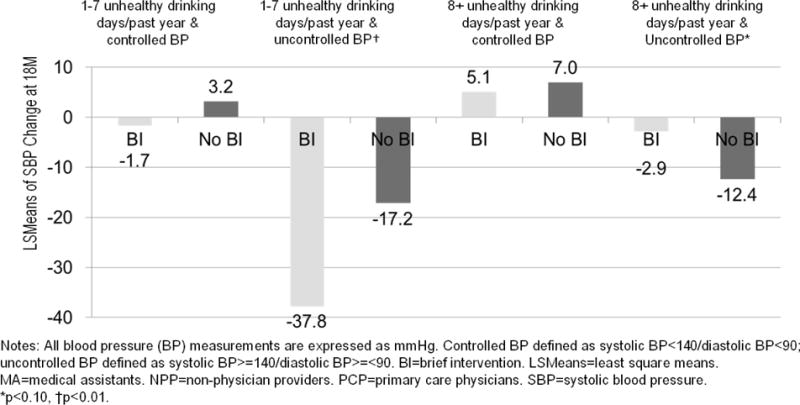
Moderating Effects of Unhealthy Drinking Level and Blood Pressure Control Status at Index Screening on Systolic Blood Pressure Change at 18 Months
Results from the weighted logistic regression models including the interaction terms between BI and the three potential moderators suggest that associations between documented BI and having controlled BP at 18 months vary by intervention arm and unhealthy drinking frequency at index screening (p<0.05 and P<0.0001 for the 2-way interaction terms of each with documented BI, respectively, and p=0.05 for the 3-way interaction terms of BI, unhealthy drinking frequency at index screening and intervention arm): among those in the PCP intervention arm who reported only 1–7 past-year heavy drinking days at index screening, receiving BI was associated with 7 and 17 times higher odds of having BP under control at 18 months, depending on whether or not their BP was under control at index screening (odds ratio [95% confidence interval]=7.12 [1.25–40.52] and 17.64 [3.13–99.46], respectively) (Figure 3). However, for those in the NPP&MA intervention arm who reported 8 or more past-year heavy drinking days at index screening, documented BI was associated with lower odds of having BP under control at 18 months (odds ratio [95% confidence interval]=0.12 [0.06–0.25] and 0.09 [0.03–0.25] for patients whose BP were and were not under control at index screening, respectively).
Figure 3.
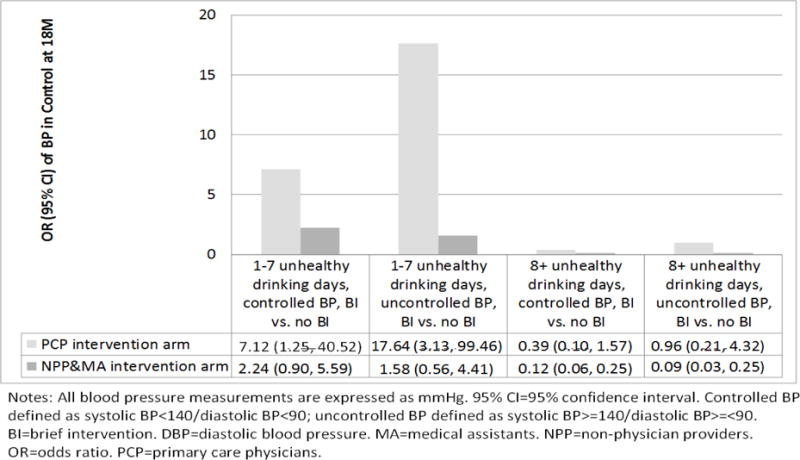
Moderating Effects of Intervention Arm, Unhealthy Drinking Level and Blood Pressure (BP) Control Status at Index Screening on BP Control Status at 18 Months
3.4. Exploratory Analyses on the mechanisms of the associations between alcohol BI and BP outcomes
To explore the possibility that the association between greater BP declines and brief interventions were mediated by greater reductions in drinking, we conducted exploratory post hoc analyses among the sub-sample of those with available EHR data for all measures (N=622). Findings suggested that the associations between receiving BI and reporting no past-year unhealthy drinking days at 12 month follow-up was in the opposite directions for the intervention arms (relative risk=1.16, p=0.44 for PCP intervention arm and relative risk=0.62, p<0.01 for NPP&MA intervention arm, respectively). For the NPP&MA intervention arm, the relative risk was significantly lower than 1, suggesting that those who received non-physician provider-delivered alcohol BI were less likely to report no past-year unhealthy drinking days at 12 months. For the PCP intervention arm, although the relative risk was in the expected direction, suggesting that physician-delivered BI may be associated with no past-year unhealthy drinking days at 12 months, the p value was non-significant due to the very small sub-sample size. Informed by the literature (Faries et al., 2010; E. F. Kaner et al., 2007), we conducted separate models to examine associations between reduced heavy drinking and BP decline among patient sub-groups. Results indicated significant associations between no unhealthy drinking days at 12 months and greater systolic BP decline at 18 months for women (−7.76 vs. 0.06 mmHg, p<0.05), and a trend toward significance for Whites (−8.11 vs. −3.76 mmHg, p<0.10) (not shown). Unfortunately, the exploration analyses failed to establish the mechanisms of the associations between alcohol BI and BP outcomes observed, probably due to small subgroups sizes and limited power, and limited drinking measures available in the EHR.
4. Discussion
When examining hypertensive patients who screened positive from the two study intervention arms together, we found no significant associations between alcohol BI and BP change, and a negative association between alcohol BI and BP control, at 18-month follow-up. The original trial found screening rates much higher in the NPP&MA intervention arm (51% in the NPP&MA intervention arm vs. 9% in the PCP intervention arm), but BI or referral rates among those who screened positive much higher in the PCP intervention arm (44% in the PCP intervention arm vs. 3.4% in the NPP&MA intervention arm) (Mertens et al., 2015). Thus, one possible explanation for the null or counterintuitive findings on the overall associations between BI and BP outcomes could be due to the low BI rate in the NPP&MA intervention arm; the majority of the hypertensive patients in this intervention arm did not receive a BI, and thus were not subject to its potential beneficial effects and their hypertension continued to progress. Moreover, there may also be other unmeasured differences between patients that may account for receipt of alcohol BI within or between the intervention arm, but that cannot be statistically tested or addressed in our analyses.
However, findings from the moderation analyses suggested that the associations between receiving BI and BP outcomes could be moderated by study intervention arm, baseline unhealthy drinking level and baseline BP status. Specifically, we found that alcohol BI may be beneficial for adult primary care patients with hypertension who report unhealthy drinking, especially in the sub-group of those who had fewer than 8 heavy drinking days in the prior year (suggesting having a lower risk for alcohol dependence) (Saitz et al., 2014) and worse BP control status at screening. This is consistent with the literature that BI may not be sufficient for individuals with more severe drinking problems (Saitz, 2010). Our null findings on the overall association of BI and BP are similar to the null findings on drinking outcomes found in several large alcohol BI implementation trials (Hilbink et al., 2012; E. Kaner et al., 2013; Williams et al., 2014), and supports the notion that the effectiveness of BI may depend on a variety of factors, including clinical characteristics such as drinking and medical severity. That the BP findings were stronger for sub-group of patients in the PCP intervention arm also may indicate that physician-delivered alcohol BIs tied to salient health conditions may be particularly potent.
This study adds to the limited literature on alcohol BI and BP outcomes (Maheswaran, Beevers, & Beevers, 1992; Rose et al., 2008). Hypertension is one of the most prevalent and costly chronic conditions in the U.S. and worldwide, and alcohol use is a modifiable hypertension risk factor (Klatsky, 2004; Saitz, 2005). Many primary care patients have multiple chronic conditions (Britt, Harrison, Miller, & Knox, 2008; Fortin, Bravo, Hudon, Vanasse, & Lapointe, 2005; Fortin, Hudon, Haggerty, Akker, & Almirall, 2010; Ornstein, Nietert, Jenkins, & Litvin, 2013). While physicians today have more tools and knowledge available to effectively treat chronic conditions, they are also facing a growing challenge to address patients’ multimorbidity with limited time (Ostbye et al., 2005). To align with these clinical realities, researchers have called for a shift “from a disease orientation to a patient-goal orientation” (Bayliss, Balasubramianian, Gill, & Stange, 2014; Tinetti, Fried, & Boyd, 2012), involving identifying relevant diseases and their common modifiable risk factors (S. M. Smith, Soubhi, Fortin, Hudon, & O’Dowd, 2012), and guiding behavior change through shared decision making (Tinetti et al., 2012). Evidence of effectiveness of alcohol SBIRT on a broader array of health outcomes supports this shift, and may facilitate SBIRT implementation in primary care by addressing issues of competing disease management in limited time faced by primary care physicians (Ostbye et al., 2005). Prior research suggests that SBIRT delivery by primary care physicians, including brief advice, has been difficult to achieve in either clinical trials (E. Kaner et al., 2013) or population studies (Glass et al., 2015; McKnight-Eily et al., 2014). Providing training emphasizing the link between alcohol and chronic conditions may increase physician confidence about screening and discussing drinking among patients who have or are at risk for such conditions.
Study limitations merit attention. As with other observational studies, results cannot be interpreted as causal. Also, all measures are EHR-based and reliant on patient visits; only about one-third had follow-up BP measures, and we are able to examine only heavy drinking rather than changes in drinking frequency or quantity. Moreover, our measure of BI delivery in the EHR relied on provider documentation, and as such, may not thoroughly capture the delivery of BI, either in quantity or quality. There may also be other unmeasured differences between patients, including aspects of medical conditions or drinking not captured in the EHR data, that may account for receipt of alcohol BI in each intervention arm, but that cannot be statistically tested or addressed in our analyses. For example, although the possibility exists that interventions from physicians may have been more effective because of their status, their often long-standing relationship with their patients, or the impact of their being a physician on the relative salience to patients of their advice to reduce drinking because of their health conditions, we did not have data to assess this or whether and how contents of BI delivered may have differed between physicians and non-physician providers despite the standardized training. The current study was unable to establish the mechanisms of the associations between alcohol BI and BP outcomes observed. Prior research has found associations between alcohol misuse and antihypertensive non-adherence (Bryson et al., 2008; Cook & Cherpitel, 2012). However, such an analysis is beyond the scope of the current study. There are also other potential explanations for the findings, e.g., primary care physicians who delivered alcohol BI may also be more likely to do so for other health issues (e.g., exercise, diet) or to provide more aggressive hypertension management when needed, both of which could also potentially lead to better BP outcomes. Data on the numbers of primary care visits, changes in anti-hypertensive medication regimens and medication adherence through the course of the study were not collected for the current study, which might confound the finding that primary care physicians elicited greater reductions in BP. Comparative effectiveness research with a larger dataset and more complete and detailed measures on drinking outcomes to investigate a full suite of prevention measures on drinking and other health outcomes and the mechanisms is needed. Strengths of the study include rigorous and conservative methods for adjusting for confounding effects such as treatment selection through use of inverse probability weighting.
5. Conclusions
This study leveraged data from an SBIRT implementation trial and found that BI by primary care physicians was associated with improved BP control for hypertensive patients who were not frequent heavy drinkers. This is consistent with the literature on drinking outcomes which suggests that BI may not be sufficient for individuals with more severe drinking problems. Our findings suggest that hypertensive patients may benefit from receiving screening and physician brief intervention for unhealthy alcohol use in adult primary care. Findings also highlight potential population-level benefits of alcohol BI if widely applied, suggesting a need for the development of innovative strategies to facilitate SBIRT delivery in primary care settings. More research is needed in evaluating the impacts of SBIRT beyond drinking outcomes. Expanding the scientific knowledge base on the relationship between SBIRT and health outcomes for patients with chronic conditions may increase the uptake of SBIRT and improve clinical practice for many of the patients seen in primary care.
Highlights.
Alcohol brief intervention by physicians may be beneficial for BP control
Optimal treatment for adult hypertensive patients should include alcohol SBIRT
Future research on effectiveness of alcohol SBIRT on health outcomes is warranted
Acknowledgments
We thank Agatha Hinman for editorial assistance with the manuscript. We also thank the KPNC Chemical Dependency Quality Improvement Committee and KPNC Chemical Dependency Program Directors and Addiction Medicine Physicians for their partnership, and the physicians, medical assistants, clinical health educators, behavioral medicine specialists, nurses, and managers of KPNC’s adult and family medicine departments for their participation in the quality improvement activities related to this study. We especially thank Don Mordecai, M.D. and Sheryl Sun, M.D, for their strong leadership support of this project and of implementation of alcohol screening, brief intervention and referral to treatment within KPNC adult primary care. We thank Romain Neugebauer, Ph.D., for statistical advice.
Funding Source
This research is supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (R01AA18660).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: none.
An earlier version of this manuscript was presented, in part, at the 2015 meeting of the International Network on Brief Interventions for Alcohol Problems (INEBRIA), Atlanta, Georgia, September 25, 2015
References
- Babor T, Rehm J, Jernigan D, Vaeth P, Monteiro M, Lehman H. Alcohol, diabetes, and public health in the Americas. Revista Panamericana de Salud Publica. 2012;32(2):151–155. doi: 10.1590/s1020-49892012000800010. [DOI] [PubMed] [Google Scholar]
- Ballesteros J, Duffy JC, Querejeta I, Arino J, Gonzalez-Pinto A. Efficacy of brief interventions for hazardous drinkers in primary care: systematic review and meta-analyses. Alcoholism: Clinical and Experimental Research. 2004;28(4):608–618. doi: 10.1097/01.alc.0000122106.84718.67. [DOI] [PubMed] [Google Scholar]
- Bayliss EA, Balasubramianian BA, Gill JM, Stange KC. Perspectives in primary care: implementing patient-centered care coordination for individuals with multiple chronic medical conditions. Annals of Family Medicine. 2014;12(6):500–503. doi: 10.1370/afm.1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boschloo L, Vogelzangs N, van den Brink W, Smit JH, Veltman DJ, Beekman AT, et al. Alcohol use disorders and the course of depressive and anxiety disorders. British Journal of Psychiatry. 2012;200(6):476–484. doi: 10.1192/bjp.bp.111.097550. [DOI] [PubMed] [Google Scholar]
- Britt HC, Harrison CM, Miller GC, Knox SA. Prevalence and patterns of multimorbidity in Australia. Medical Journal of Australia. 2008;189(2):72–77. doi: 10.5694/j.1326-5377.2008.tb01919.x. [DOI] [PubMed] [Google Scholar]
- Bryson CL, Au DH, Sun H, Williams EC, Kivlahan DR, Bradley KA. Alcohol screening scores and medication nonadherence. Annals of Internal Medicine. 2008;149(11):795–804. doi: 10.7326/0003-4819-149-11-200812020-00004. [DOI] [PubMed] [Google Scholar]
- Cook WK, Cherpitel CJ. Access to health care and heavy drinking in patients with diabetes or hypertension: implications for alcohol interventions. Substance Use and Misuse. 2012;47(6):726–733. doi: 10.3109/10826084.2012.665558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. Journal of the American Medical Association. 2010;303(20):2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- Engler PA, Ramsey SE, Smith RJ. Alcohol use of diabetes patients: the need for assessment and intervention. Acta Diabetologica. 2013;50(2):93–99. doi: 10.1007/s00592-010-0200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faries D, Leon AC, Haro JM, Obenchain OL. Analysis of Observational Health Care Data Using SAS®. Cary, NC: SAS Institute; 2010. [Google Scholar]
- Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Annals of Family Medicine. 2005;3(3):223–228. doi: 10.1370/afm.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortin M, Hudon C, Haggerty J, Akker M, Almirall J. Prevalence estimates of multimorbidity: a comparative study of two sources. BMC Health Services Research. 2010;10:111. doi: 10.1186/1472-6963-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Hamilton AM, Powell BJ, Perron BE, Brown RT, Ilgen MA. Specialty substance use disorder services following brief alcohol intervention: a meta-analysis of randomized controlled trials. Addiction. 2015;110(9):1404–1415. doi: 10.1111/add.12950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbink M, Voerman G, van Beurden I, Penninx B, Laurant M. A randomized controlled trial of a tailored primary care program to reverse excessive alcohol consumption. Journal of the American Board of Family Medicine. 2012;25(5):712–722. doi: 10.3122/jabfm.2012.05.120070. [DOI] [PubMed] [Google Scholar]
- Jonas DE, Garbutt JC, Amick HR, Brown JM, Brownley KA, Council CL, et al. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2012;157(9):645–654. doi: 10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed] [Google Scholar]
- Kaner E, Bland M, Cassidy P, Coulton S, Dale V, Deluca P, et al. Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): pragmatic cluster randomised controlled trial. BMJ (Clinical Research Ed) 2013;346:e8501. doi: 10.1136/bmj.e8501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaner EF, Beyer F, Dickinson HO, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database of Systematic Reviews. 2007;(2):CD004148. doi: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- Klatsky AL. Alcohol-associated hypertension: when one drinks makes a difference. Hypertension. 2004;44(6):805–806. doi: 10.1161/01.HYP.0000146538.26193.60. [DOI] [PubMed] [Google Scholar]
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. The Lancet. 2002;360(9349):1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- Maheswaran R, Beevers M, Beevers DG. Effectiveness of advice to reduce alcohol consumption in hypertensive patients. Hypertension. 1992;19(1):79–84. doi: 10.1161/01.hyp.19.1.79. [DOI] [PubMed] [Google Scholar]
- McKnight-Eily LR, Liu Y, Brewer RD, Kanny D, Lu H, Denny CH, et al. Vital signs: communication between health professionals and their patients about alcohol use—44 states and the District of Columbia, 2011. MMWR Morbidity and Mortality Weekly Report. 2014;63(1):16–22. [PMC free article] [PubMed] [Google Scholar]
- Mertens JR, Chi FW, Weisner CM, Satre DD, Ross TB, Allen S, et al. Physician versus non-physician delivery of alcohol screening, brief intervention and referral to treatment in adult primary care: the ADVISe cluster randomized controlled implementation trial. Addiction Science & Clinical Practice. 2015;10(26):26. doi: 10.1186/s13722-015-0047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens JR, Weisner C, Ray GT, Fireman B, Walsh K. Hazardous drinkers and drug users in HMO primary care: prevalence, medical conditions, and costs. Alcoholism: Clinical and Experimental Research. 2005;29(6):989–998. doi: 10.1097/01.alc.0000167958.68586.3d. [DOI] [PubMed] [Google Scholar]
- Miller PM, Anton RF, Egan BM, Basile J, Nguyen SA. Excessive alcohol consumption and hypertension: clinical implications of current research. Journal of Clinical Hypertension (Greenwich) 2005;7(6):346–351. doi: 10.1111/j.1524-6175.2004.04463.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: a clinician’s guide, updated 2005 edition. 2005 Jan; 2007. Retrieved from http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm.
- National Institute on Alcohol Abuse and Alcoholism. (Excerpted from NIH Publication No. 07-3769).Tips for cutting down on drinking. 2007 Retrieved from http://pubs.niaaa.nih.gov/publications/Tips/tips.pdf.
- Ornstein SM, Nietert PJ, Jenkins RG, Litvin CB. The prevalence of chronic diseases and multimorbidity in primary care practice: a PPRNet report. Journal of the American Board of Family Medicine. 2013;26(5):518–524. doi: 10.3122/jabfm.2013.05.130012. [DOI] [PubMed] [Google Scholar]
- Ostbye T, Yarnall KS, Krause KM, Pollak KI, Gradison M, Michener JL. Is there time for management of patients with chronic diseases in primary care? Annals of Family Medicine. 2005;3(3):209–214. doi: 10.1370/afm.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose HL, Miller PM, Nemeth LS, Jenkins RG, Nietert PJ, Wessell AM, et al. Alcohol screening and brief counseling in a primary care hypertensive population: a quality improvement intervention. Addiction. 2008;103(8):1271–1280. doi: 10.1111/j.1360-0443.2008.02199.x. [DOI] [PubMed] [Google Scholar]
- Saitz R. Clinical practice. Unhealthy alcohol use. New England Journal of Medicine. 2005;352(6):596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- Saitz R. Alcohol screening and brief intervention in primary care: Absence of evidence for efficacy in people with dependence or very heavy drinking. Drug and Alcohol Review. 2010;29(6):631–640. doi: 10.1111/j.1465-3362.2010.00217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Cheng DM, Allensworth-Davies D, Winter MR, Smith PC. The ability of single screening questions for unhealthy alcohol and other drug use to identify substance dependence in primary care. Journal of Studies on Alcohol and Drugs. 2014;75(1):153–157. doi: 10.15288/jsad.2014.75.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Statistical Methods in Medical Research. 2013;22(3):278–295. doi: 10.1177/0962280210395740. [DOI] [PubMed] [Google Scholar]
- Shaw KM, Handler J, Wall HK, Kanter MH. Improving blood pressure control in a large multiethnic California population through changes in health care delivery, 2004–2012. Preventing Chronic Diseaase. 2014;11:E191. doi: 10.5888/pcd11.140173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. Primary care validation of a single-question alcohol screening test. Journal of General Internal Medicine. 2009;24(7):783–788. doi: 10.1007/s11606-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database of Systematic Reviews. 2012;4:CD006560. doi: 10.1002/14651858.CD006560.pub2. [DOI] [PubMed] [Google Scholar]
- Timko C, Kong C, Vittorio L, Cucciare MA. Screening and brief intervention for unhealthy substance use in patients with chronic medical conditions: a systematic review. Journal of Clinical Nursing. 2016;25(21–22):3131–3143. doi: 10.1111/jocn.13244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition—multimorbidity. Journal of the American Medical Association. 2012;307(23):2493–2494. doi: 10.1001/jama.2012.5265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. New England Journal of Medicine. 2001;345(18):1291–1297. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- Whitlock EP, Polen MR, Green CA, Orleans T, Klein J, Force USPST. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2004;140(7):557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- Williams EC, Rubinsky AD, Chavez LJ, Lapham GT, Rittmueller SE, Achtmeyer CE, et al. An early evaluation of implementation of brief intervention for unhealthy alcohol use in the US Veterans Health Administration. Addiction. 2014;109(9):1472–1481. doi: 10.1111/add.12600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu S, Ross C, Raebel MA, Shetterly S, Blanchette C, Smith D. Use of stabilized inverse propensity scores as weights to directly estimate relative risk and its confidence intervals. Value Health. 2010;13(2):273–277. doi: 10.1111/j.1524-4733.2009.00671.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


