Abstract
Rationale:
Using magnetic resonance imaging (MRI), we diagnosed pneumoconiosis by identifying the content and distribution of hydrogen protons in the water molecules in different tissues and lesions.
Patient concerns:
25 cases of CWP patients with progressive massive fibrosis (PMF) lesions.
Diagnoses:
Patients were correctly diagnosed, with one case each of Phase I and II pneumoconiosis and 23 cases of Phase III pneumoconiosis.
Interventions:
None.
Outcomes:
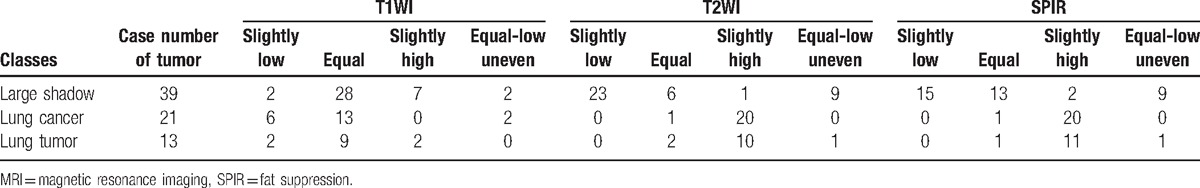
Through MRI, 39 PMF pneumoconiosis lesions exhibited equal, low or equally low, and uneven signals on T2WI and fat suppression (SPIR) (38/39, 37/39).
Lessons:
MRI has good specificity to identify the characteristics of PMF lesions of CWP, as well as has high application value for the differential diagnosis of lung cancer and other lung tumor-like lesions.
Keywords: differential diagnosis, lung tumors, magnetic resonance imaging, pneumoconiosis, progressive massive fibrosis
1. Introduction
A total of 12 kinds of pneumoconiosis exist in our national list of occupational diseases, with silicosis and coal worker pneumoconiosis (CWP) being the main types. CWP is a coal mine occupational disease that presents with pulmonary silicotic nodules or diffuse interstitial fibrotic lesions caused by inhalation of free silicon dioxide or coal dust with less than 5% silicon dioxide because of long-term employment in an environment with a high dust concentration. CWP can be divided into complex and simple CWP according to the occurrence of silicon nodules. The former has pathological changes in coal pneumoconiosis and silicosis. To date, CWP diagnosis is still based on specific occupational history and high kilovolt chest x-ray plain film. In its early stage, the lungs show extensive changes in texture, fibrous bands, and reticular shadows, and present with small pulmonary nodules with smaller diameter, irregular shape, and lower density compared with typical silicotic nodules. The decrease in lung transmittance gives the results a glass-like appearance. As the lesion progresses, large block-like shadows may develop based on initial image findings. With the rapid developments in medical digital image technology, the applications of computed radiography/digital radiography and computed tomography (CT) in pneumoconiosis diagnosis have gained increasing attention and achieved certain effectiveness.[1,2] However, diagnosis confirmation through traditional x-ray photography and CT scanning method rely mainly on the lesion morphology and material density. Distinguishing large shadows between pneumoconiosis and lung cancer tumors is difficult. Magnetic resonance imaging (MRI) diagnoses diseases by identifying the content and distribution of hydrogen protons in the water molecules in different tissues and lesions. Considering the difficulty in distinguishing large shadows between pneumoconiosis and lung cancer tumors, MRI may be effective to improve the specificity and accuracy of diagnosis and reducing the false positive rate. Moreover, reports of MRI application for pneumoconiosis are rare. In this retrospective study, MRI was employed to examine 25 CWP cases. Then, analysis was conducted by comparing the results among 34 lung tumor-like lesion cases to discuss the diagnostic and clinical application values of MRI for CWP cases.
2. Materials and methods
2.1. Subjects
A total of 25 cases of progressive massive fibrosis (PMF) lesions of CWP patients hospitalized since October 2009 were selected from the Pneumoconiosis Department. The data linking of patients required for this study was approved by the Affiliated Hospital of Xuzhou Medical University. Patients were correctly diagnosed by the professional team in pneumoconiosis diagnosis at the municipal level or above.[3] Included among these pneumoconiosis cases are 1 case each of Phase I and II pneumoconiosis and 23 cases of Phase III pneumoconiosis. All patients were male aged 63 to 89 years, with an average age of 73.6. Their large shadows had a minimum diameter larger than 1 cm and the lesions exhibited no significant changes after at least 2 years of chest radiography or CT follow-up. The pathological results from 2 cases were obtained from punctures. Moreover, 11 cases of unilateral pulmonary lesions, 14 cases of bilateral pulmonary lesions, and 1 case of merged obsolete pulmonary tuberculosis were observed. A total of 34 cases of lung tumor-like patients were from the Respiratory Medicine Department and Cardiothoracic Surgery Department. Among which, 21 cases were lung cancer patients, and 18 were male and 3 were female aged 43 to 81, with an average age of 68.2. Twenty cases were diagnosed after bronchoscopic biopsy, CT-guided puncture, or surgery. Pathological patterns showed 9 cases of squamous carcinoma, 7 cases of adenocarcinoma, 3 cases of small cell carcinoma, and 1 case of adenosquamous carcinoma. Moreover, 1 case was confirmed through clinical follow-up, but the results of its pathological pattern were not obtained. The findings included 13 peripheral lung cancer and 8 central lung cancer cases. For other chest tumor-like lesions, 1 case of pulmonary metastatic tumor, 4 cases of pulmonary benign tumors, 1 case of thymoma, 3 cases of spherical pneumonia, 2 cases of pure pulmonary atelectasis, and 2 cases of pulmonary tuberculosis were found.
2.2. Scanning method
A Philips Gyroscan Intera 1.5 T superconducting type MRI scanner with 30 mT/m of magnetic field gradient strength and 150 mT/m ms of gradient switch rate was employed. The 5-channel heart-phased array coils equipped with electrocardial vector triggering and respiratory monitoring devices were used. For chest MRI conventional CT scanning, fast spin echo technology that included T1WI, T2WI, and spectral presaturation with inversion recovery (SPIR) sequence was used for the transverse view, and the balanced turbo field echo sequence was used for the coronal view. The scanning parameters were as follows: for T1WI: repetition time (TR) 750 ms, echo time (TE) 11 ms; for T2WI: TR 3000 ms, TE 90 ms; for SPIR: TR 1600 ms, TE 70 ms; for matrix: 256 × 256, and for field of view: 370 mm × 455 mm.
2.3. Image analysis
The lesions were analyzed jointly using 2 senior/long-standing doctors with more than 20 years of working experience in imaging diagnosis. These 2 doctors have senior professional posts for imaging diagnosis and have qualifications (certificates) as pneumoconiosis imaging diagnosticians. The emphasis was on the analytical judgment for morphology, boundary, and the surrounding symptom of lesions. Moreover, MRI signals on tumors were classified according to the reference standard of the soft tissue of the chest wall that is adjacent to the tumors that included 4 classes, namely, slightly low, equal, slightly high, and uneven equal-low signals.
2.4. Data analysis
All statistical analyses were conducted using SPSS 22.0. The Chi-square test was applied to assess the results. We considered the occurrence of no significant heterogeneity when P was greater than .05.
3. Results
3.1. Among the 25 CWP cases, 14 and 11 cases of bilateral and unilateral PMF lesions were observed, respectively, with the 14 lesions located in the lower pulmonary field and the 11 cases in the upper pulmonary field
Among them, 6 lesions were quasi-circular, 11 were strip shaped, and 8 were irregularly shaped; moreover, many of them had relatively clear boundaries. However, on both sides of the chest wall and in the mediastinum adjacent to the lesions, a visible and relatively thick stripe-like stretched shadow connected to the pleura was often observed. Compared with the soft muscle tissue adjacent to the chest wall, most of the PMF lesions of pneumoconiosis showed equal signals on T1WI, with a ratio of 28/39. Furthermore, overall lesion signals were relatively even. T2WI and SPIR showed slightly low, equal, and uneven equal-low signals, and accounted for 97.4% and 94.9%, respectively. Moreover, in lesions with equal-low signals, visible flecks and streak-like shadows with even low signal and a certain amount of image characteristics were visible (Fig. 1). In 13 lesions, visible utricle-like and even long T1 long T2 liquidity signal shadows occurred. In 9 lesions, short strip arc-like long T1 long T2 signal shadows surrounding the edges were observed and were especially evident in T2WI and SPIR.
Figure 1.
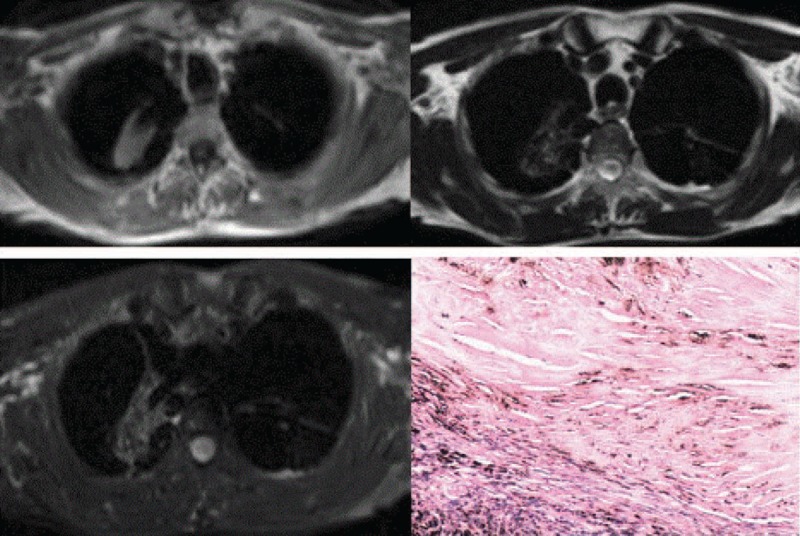
PMF lesions of CWP, with lesions showing equal signals at T1WI in MR and equal-low signals at T2WI and SPIR, wherein shadows with even low signals are seen. CWP = coal worker pneumoconiosis, MR = magnetic resonance, PMF = progressive massive fibrosis, SPIR = fat suppression.
3.2. Among the 21 lung cancer cases, 15 exhibited tumors on the right and 6 exhibited tumors on the left
Moreover, 8 cases with lesions in the upper pulmonary field, 4 in the upper-middle pulmonary field, 6 in the lower pulmonary field, and 3 beside the mediastinum were found. The tumor diameters ranged from 2.0 to 7.5 cm, including 3 cases of pulmonary atelectasis, 6 of obstructive pneumonia, 9 of pleural effusion, and 2 of intrapulmonary metastasis. Most lesions exhibited quasi-circular and irregular shadows with undefined edges. In 11 cases, signs of visible lobulation were observed. Furthermore, signs of visible spicule were found in 15 cases. The equal-low signals in the lung cancer lesions accounted for 90.5% and the high signals on T2WI and SPIR accounted for 95.2% (Fig. 2).
Figure 2.
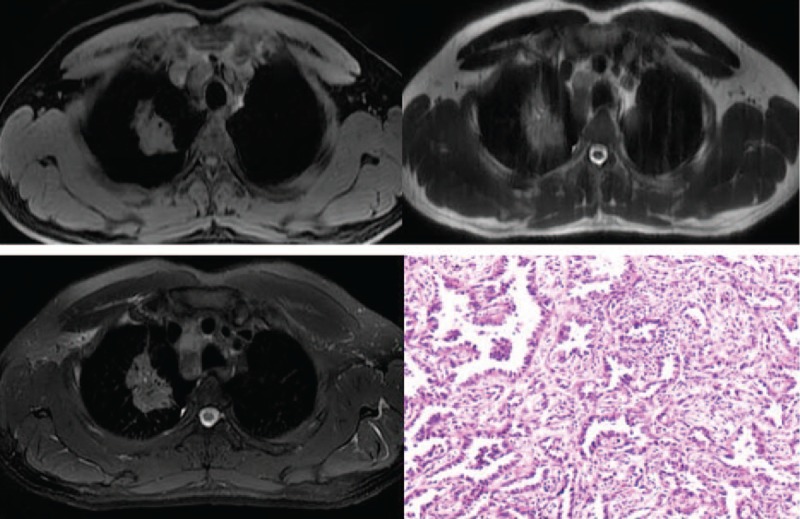
Quasi-circular and block-like shadows in the upper left lungs of lung cancer patients, with lesions showing equal signals with soft tissue adjacent to the chest wall at T1WI in MR and high signals at T2WI and SPIR. Lung adenocarcinoma. MR = magnetic resonance, SPIR = fat suppression.
3.3. In other lung tumor-like lesions, 7 and 6 cases were on the right and left lungs, respectively
Eight cases were quasi-circular, 2 were flake-block shaped, and 2 were irregularly shaped. All these cases frequently showed equal or low signal changes in T1WI and accounted for 84.6%, as well as often showed high signals in T2WI and SPIR that accounted for 76.9% and 84.6%, respectively (Fig. 3).
Figure 3.
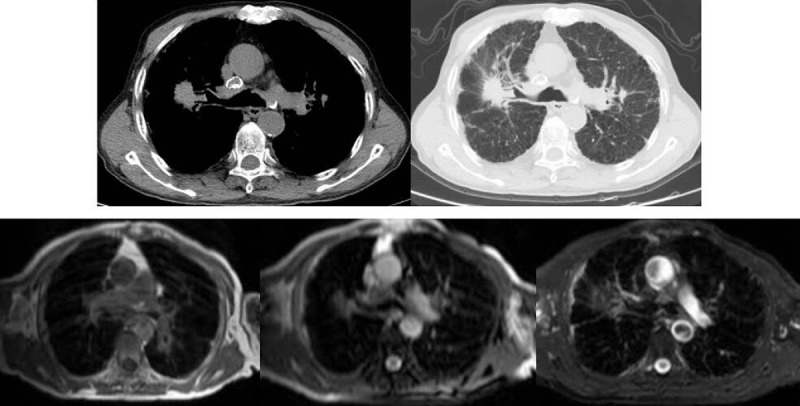
Phase I of CWP complicated by a large shadow formation, with CT scanning (figure above) suggesting the possibility of pneumoconiosis to form lung cancer. MRI showing tumors in equal-low signal shadows, consistent with the representations of large shadows of pneumoconiosis. Diagnosis confirmed after 2 years of follow-up. CT = computed tomography, CWP = coal worker pneumoconiosis, MRI = magnetic resonance imaging.
MRI signal changes in the large shadows of silicosis, lung cancer, and other lung tumors are shown in Table 1. In the chi-square test, we simplified the results into a 4-fold table by evaluating the statistics. We selected the slightly low, equal, and uneven equal-low signals as groups because of the obvious difference between CWP and lung tumor-like lesions on T2WI and SPIR. The high signal was placed in another group. We used the correcting chi-square test to make the final analysis, considering the situation of several frequencies being less than 5. In the test for T2WI and SPIR, both P = .000 and < .05, indicating that the difference was statistically significant. Signal strength difference was observed between CWP and lung tumor-like lesions on T2WI and SPIR.
Table 1.
Comparison of MRI signal changes between large shadows of pneumoconiosis and lung cancer as well as other lung tumors.
4. Discussion
4.1. Diagnostic value for CWP
CWP is a common occupational disease that causes serious harm to coal miners. According to the recent data by the National Health and Family Planning Commission, among the occupational diseases reported in 2014, approximately 90% are occupational pneumoconiosis, totalling to 26,873 cases. Among them, 11,396 are CWP from the coal mining and washing industries and accounted for more than 42.4% of the total number of pneumoconiosis cases. The early pathological changes of pneumoconiosis involve mainly the process wherein inhaled foreign dust particles cause pulmonary alveolitis of lung macrophages. Then, macrophages with fine dust gather to form dust focused inside the lung. Eventually, they are replaced by collagenous fibers that form nodular or diffuse fibroses. Later, they fuse into large block-like shadows based on nodules or interstitial fibrosis.[4,5] Through x-ray and CT scanning, the visible lesions are generally located in bilateral upper lung fields. Some begin to form single circular or quasi-circular lesions found outside the middle-upper field. Often, irregular strip-like fibrous shadows stretch to the peripheries of the block to form a pseudopod sign, which is easily confused with peripheral burr signs of lung cancer and is difficult to be identified through CT and x-ray scanning.[6] Moreover, some blocks begin to form multiple lesions that are unequal in size and distributed in both lungs and are often visible in the middle and lower lung fields, similar to pulmonary metastasis. As seen from MRI scanning and imaging results in this study, PMF lesions of CWP show equal signals on T1WI that are similar to muscular tissues adjacent to the chest wall, with the surrounding regions and boundaries relatively clear. On T2WI, they show equal-low mixed signals that have mainly low signals (Fig. 1). This finding suggests that fibrosis and calcification are main contributors to equal-low signals in T2WI. However, lesion signals in the SPIR phase did not increase significantly, suggesting essentially relatively low water content of the fibrotic tumor lesions. Strip-like or small bulb-like T2WI and SPIR high signal shadows inside lesions in few cases were caused by liquid cavities in lesions.[7] These magnetic resonance (MR) signal characteristics increase the accuracy and directness of diagnosis using MRI for determining PMF lesions of CWP compared with the other methods that merely rely on morphological indices. Moreover, this method avoids differences of physicians’ diagnostic abilities at all levels, as well as diagnostic errors from inexperienced. Furthermore, the diagnostic method using MRI for determining PMF lesions of CWP is a new method that improves upon the outdated methods that use traditional imaging techniques to determine the nature of the lesion. Currently, as MRI applications become popular, the conventional MRI is a simple method that is easy to implement and avoids damage to the human body caused by ionizing radiation; therefore, it can be popularized in clinical application.
4.2. Identification value for CWP, lung cancers, and other lung tumors
Information[8] showed that pneumoconiosis is closely related to lung cancer occurrence and development. Especially for pneumoconiosis patients with pulmonary fibrosis, lung cancer incidence is higher than that of simple pneumoconiosis. Yiping et al[9] by studying large samples concluded that the morbidity rates of lung and mediastinal cancers in the CWP group exceeds those of the general population. Honma et al[10] investigated the pathological diagnosis of 764 pneumoconiosis cases via autopsy and found that 146 lung cancer cases (148 lesions) accounted for 19.1%. Moreover, the occurrences of lung squamous cell and small cell carcinomas showed a statistically significant and positive correlation with PMF severity. PMF lesions of CWP and lung cancer lesions have main imaging representations of lung tumors. Finding the diagnostic method to identify large shadows of CWP and lung cancer tumors has been one of the important topics of image doctors. CT studies on lung cancer showed that lobulation signs, fine short spicules, vascular convergence signs, vacuole signs, and pleural indentation signs are classified as characteristic representations of lung cancer nodules according to domestic and foreign scholars. According to CT pathological comparative observations, nodules having lobulation is a basic sign of peripheral lung cancer, which has an incidence rate of 80% to 90%. However, the occurrence frequencies of different sizes of carcinoma nodules vary. If at least 2 signs exist simultaneously, the lung cancer possibility is significantly increased.[11] However, in practical clinical work, the results of most lesions do not show typical signs. In general, diagnosis confirmation through traditional x-ray photography and CT scanning method relies mainly on lesion morphology and material density. Therefore, identifying large shadows of pneumoconiosis and lung cancer tumors either by chest radiography or CT scanning is difficult.[12] MRI differentiates lesions by identifying the content and distribution of hydrogen protons in the water molecules of different tissues and lesions. The results from this study showed that because CWP has numerous fiber compositions and special pathological structures of silicosis nodules, their overall representations at T1WI, T2WI, and SPIR in MRI have equal signals and similar to those of adjacent soft tissues and equal-low signals. Moreover, they exhibited certain MR imaging characteristics. Furthermore, lung cancer tumors are formed from the proliferation of large amounts of immature tissue cells that have relatively high water content. Therefore, they are often represented as equal, low, and high signals at T1WI, T2WI, and SPIR, respectively (Fig. 2). By comparing the imaging results of these 2 in this group, we concluded that using conventional MRI techniques, PMF lesions of pneumoconiosis and lesions of lung cancer tumors can be identified efficiently, especially using T2WI and SPIR, wherein signal differences are highly distinct.[13,14] The author has employed this method in practical work to correct misdiagnosed pneumoconiosis cases for lung tumor CT (Fig. 3) many times, thereby protecting patients from tedious or invasive examinations and helping doctors quickly and reasonably formulate therapeutic plans. Concurrently, the large shadows of CWP, along with other benign lung tumors and infectious disease upon MR imaging results in T2WI and SPIR, still showed significant differences. However, this finding needs further study to confirm its clinical value because of the small types of cases.
4.3. Follow-up re-examination for CWP
Large block-like shadows in pneumoconiosis are among the most common forms of expression for late CWP. X-ray or CT scanning are commonly used for the evaluation and follow-up for large shadows of lesions in CWP patients.[15] However, the effects of ionizing radiation to the human body need to be considered and CT is limited in clinical applications because of the high toxicity and side effects of contrast media. Therefore, pneumoconiosis prevention and control researchers are always looking for alternative imaging methods. As MRI technology rapidly develops, its multidimensional imaging mode of arbitrary planar scanning and superior resolution capability for soft tissues are increasingly being used for diagnosing pulmonary lesions. The Tao et al[16] scanned 29 cases of large block-like shadow of pneumoconiosis using conventional MRI techniques and compared these techniques with those of CT. The results showed that, except for the poorly visualized fine microstructure of tumor edges, no significant differences were observed in CT with regard to tumor location, tumor internal structure, affected situation of pleural and chest wall, and lymph node representation. Koray et al[17] conducted imaging inspections on PMF of CWP using volumetric interpolated breath-hold examination (VIBE) and half acquisition single-shot fast spin echo (HASTE) sequences of rapid magnetic resonance. VIBE and HASTE techniques allow continuous data acquisition during a single breath-hold, with 100% sensitivity for lesion detection in all groups. The imaging quality of MR rapid imaging sequences using massive fibrosis lung lesions as examples was close to that of CT study. Especially, post-contrast VIBE sequence imaging has the best agreement with the gold standard CT imaging. Moreover, it prevents damage from ionizing radiation and iodinated contrast media. With the continuous development of MR devices and exploration and application of new scanning sequences, the effects of MRI in follow-ups and re-examinations for large block-like shadows of CWP will gain increasing attention.
In summary, as new magnetic resonance sequencing continuously develops, its application in lung diseases gradually obtains considerable attention. Using the unique image-forming principle of magnetic resonance to determine the nature of lung tumors will offer a new diagnostic approach in clinical practice. The results from this study make the identification of pneumoconiosis silicon blocks and lung cancer tumors become relatively simple. For the differential diagnosis among lung cancers and other lung tumor-like lesions, various technological means of magnetic resonance for comprehensive judgment are required. The conventional MRI method is simple, easy, and does not harm the human body. Moreover, it has value in practical clinical applications and worthy of popularization.
Footnotes
Abbreviations: CT = computed tomography, CWP = coal worker pneumoconiosis, HASTE = half acquisition single-shot fast spin echo, MRI = magnetic resonance imaging, PMF = progressive massive fibrosis, SPIR = fat suppression, TE = echo time, TR = repetition time, VIBE = volumetric interpolated breath-hold examination.
LZ, CW, and QY have contributed equally to this study.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Halldin CN, Petsonk EL, Laney AS. Validation of the international Labor office digitized standard images for recognition and classification of radiographs of pneumoconiosis. Academic Radiol 2014;21:305–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].De CMCS, Ferreira AS, Irion KL, et al. CT quantification of large opacities and emphysema in silicosis: correlations among clinical, functional, and radiological parameters. Lung 2014;192:543–51. [DOI] [PubMed] [Google Scholar]
- [3].Wang X, Wu S, Song Q, et al. Occupational health and safety challenges in China–focusing on township-village enterprises. Arch Environ Occup Health 2011;66:3–11. [DOI] [PubMed] [Google Scholar]
- [4].Petsonk EL, Rose C, Cohen R. Coal mine dust lung disease: new lessons from an old exposure. Am J Respir Crit Care Med 2013;187:1178–85. [DOI] [PubMed] [Google Scholar]
- [5].Kimura K, Ohtsuka Y, Kaji H, et al. Progression of pneumoconiosis in coalminers after cessation of dust exposure: a longitudinal study based on periodic chest X-ray examinations in Hokkaido, Japan. Intern Med 2010;49:1949–56. [DOI] [PubMed] [Google Scholar]
- [6].Qichung Z, Zhonghui L, Lijun P. 4 cases of pneumonectomy in silicosis misdiagnosed as lung cancer. Zhonghua Laodong Weisheng Zhiyebing Zazhi 2004;21:232–6. [PubMed] [Google Scholar]
- [7].Jung IJ, Seog HP. MR characteristics of progressive massive fibrosis. J Thorac Imaging 2000;15:144–50. [DOI] [PubMed] [Google Scholar]
- [8].Katabami M, Dosaka-Akita H, Honma K, et al. Pneumoconiosis-related lung cancers: preferential occurrence from diffuse interstitial fibrosis-type pneumoconiosis. Am J Respir Care Med 2000;162:295–300. [DOI] [PubMed] [Google Scholar]
- [9].Yiping H, Chungjen T, Chiajen L. Cancer risk among patients with coal worker pneumoconiosis in Tastuiwan: a nationwide population-based study. Int J Cancer 2014;134:1021–5. [DOI] [PubMed] [Google Scholar]
- [10].Honma K, Keizo C, Kiyonobu K. Silicosis, mixed dust pneumoconiosis, and lung cancer. Am J Ind Med 1998;32:613–7. [DOI] [PubMed] [Google Scholar]
- [11].Lee HY, Goo JM, Lee HJ, et al. Usefulness of concurrent reading using thin-section and thick-section CT images in subcentimetre solitary pulmonary nodules. Clin Radiol 2009;64:127–32. [DOI] [PubMed] [Google Scholar]
- [12].Cai ZC, Wang SS, Chen YX, et al. Image features and clinical significance of pneumoconiosis with large shadow. Zhonghua Laodong Weisheng Zhiyebing Zazhi 2016;34:214–7. [DOI] [PubMed] [Google Scholar]
- [13].Eichinger M, Optazatie DE, Kopp SA, et al. Morphologic and functional scoring of cystic fibrosis lung disease using MRI. Eur J Radiol 2012;81:13–21. [DOI] [PubMed] [Google Scholar]
- [14].Harders SW, Balyasnikown S, Fischer BM. Functional imaging in lung cancer. Clin Physiol Funct Imaging 2014;34:340–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Arakawa H, Fujimoto K, Honma K, et al. Progression from near-normal to end-stage lungs in chronic interstitial pneumonia related to silica exposure: long-term CT observations. Am J Roentgenol 2008;191:1040–6. [DOI] [PubMed] [Google Scholar]
- [16].Tao Z, Guangwei J, Quan W, et al. Contrastive analysis on CT and MRI for tumor-like fibrosis of coal worker pneumoconiosis. J Clin Radiol 2015;34:1748–51. [Google Scholar]
- [17].Koray H, Tanzer S, Meltem T, et al. Fast MRI evaluation of pulmonary progressie massive fibrpsis with VIBE and HASTE sequences: comparison with CT. Diagn Interv Radiol 2010;16:30–7. [DOI] [PubMed] [Google Scholar]


