Abstract
Introduction
Native Americans (NA) form a unique cohort of colon cancer (CC) patients among whom the variability in demographics and cancer characteristics remains unclear.
Methods
We abstracted the national estimates for NA with CC using the Surveillance, Epidemiology, and End Result (SEER) database. Trend analysis of incidence, variation in location and patient demographic analysis were performed.
Results
A total number of 26,674 NA with CC were reported during the 12-year study period. While the overall incidence of CC decreased by 12% during the study period, incidence increased by 38% in NA. Incidence of CC was more prevalent and higher increase (42%) seen in NA females than males (p=0.02; 34%). Stage III tumors represented 29% of all CC, sigmoid colon the most common site location (38%) with 72% of all tumors being moderately differentiated. 55% tumors were localized in left, 36% in right and 9% in transverse colon. 92% of the NA were insured.
Conclusion
Incidence of CC continues to rise in NA with majority of CC presented at higher stage and moderate differentiation.
INTRODUCTION
Colon cancer (CC) is an important contributor to worldwide cancer mortality and morbidity (1). CC is the third most common cancer and the second most common cause of cancer-related mortality in the United States (2). Although there is an overall declining prevalence of CC in the United States for the last three decades (3), the estimation for 2015 was still 93,090 new CC cases being diagnosed and 50,310 deaths from CC reported (4). Many factors contribute to the incidence of CC including race/ethnicity, gender, diet/environment, socioeconomic status, etc. Many of these variables have been explored in several previous studies but there are still many unanswered questions remaining.
Among the variables affecting rates of CC, race/ethnicity remains a large contributing factor. The racial disparities among African Americans and Hispanics in the incidence of CC are established (5, 6). Native Americans (NA) form a unique cohort of patients among whom the data and trends on CC and its characteristics remains unclear. Studies have shown higher incidence of CC among African Americans as well NA (3). Hispanics show a lower overall incidence rate of CC as compared to Non-Hispanic Whites (3). Although there are declining overall rates of CC in the US, this pattern does not hold true within the NA population (5). Considering steadily high rates of CC present in the United States, a need to further address the state of this disease in the NA population is required.
In an effort to elucidate this area in the literature, the aim of this study was to assess the variability in demographics and characteristics among NA patients with CC in the United States.
METHODS
Data Source
This study is a retrospective analysis of the Surveillance, Epidemiology, and End Results (SEER) database, a program supported by the National Cancer Institute (7). The SEER database is among the most accurate and complete cancer registries in the United States with data on both incidence and survival. The database includes 18 cancer registries, including state, central, metropolitan, and the Alaska Native registries. It contains data from approximately 28 percent of the U.S. population (8). This estimate includes 26 percent of African Americans, 38 percent of Hispanics, 44 percent of American Indians and Alaska Natives, 50 percent of Asians, and 67 percent of Hawaiian/Pacific Islanders (9). The specific database used excluded new cancer cases from the time period July – December 2015 due to the impact that Hurricane Katrina had on Louisiana's population (10).
Patient Population
Patients with a CC diagnosis from 2000-2012 were identified from the SEER database. The patient population consisted of 355,115 patients with a CC diagnosis, of which 6.9% were NA patients with CC. Patients with rectal cancer were excluded.
Data Points Collected
The data collected on the patients included year of CC diagnosis, gender, location of CC (ascending colon, transverse colon, and descending colon), stage of CC, and insurance status.
Outcome Measures
Patients were stratified into groups based on year of CC diagnosis, gender, location of CC, stage of CC, and insurance status. The outcome measures were incidence of CC, incidence based on gender, location of CC, stage of CC, differentiation of CC, and patient insurance status. The incidence data were obtained as proportion of Native American patients with colon cancer divided by the total number of Native American patients. We obtained the proportions from the database without the crude numbers.
Statistical Analysis
Data are reported as mean ± standard deviation (SD) for continuous descriptive variables, median (range) for ordinal descriptive variables, and the proportion for categorical variables. To analyze data, we used the Student t test for parametric variables and the Mann-Whitney U test for nonparametric variables. Trend analysis was performed to assess for variation in outcomes over the years. Variables were considered significant at p ≤ 0.05. All statistical analyses were performed using Statistical Package for Social Sciences (SPSS, Version 20; SPSS, Inc., Chicago, IL).
RESULTS
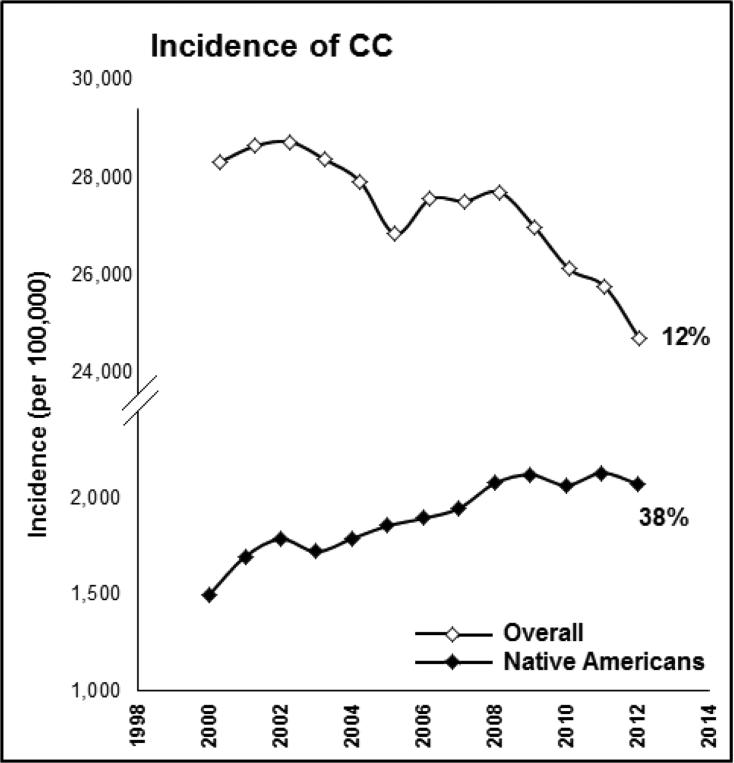
After analysis of the SEER database, 355,115 patients with CC were identified from across the United States, of which 6.9% (n=26,674) Native American patients with CC were included. The overall incidence of CC showed 12% decrease (p=0.009) from 28,322/100,000 to 24,699/100,000 from 2000 to 2012. During the same time, incidence of CC increased significantly (p=0.031) in Native Americans by 38% from 1,501/100,000 to 2,075/100,000 patients (Figure 1).
Figure 1.
Trends in overall incidence of colon cancer and incidence in Native Americans between 2000 and 2012.
Among Native Americans, there was a significant increase in incidence of CC in both male (34%, p=0.02) and female patients (42%, p=0.03) with higher prevalence of CC seen in females compared to males (p=0.02).
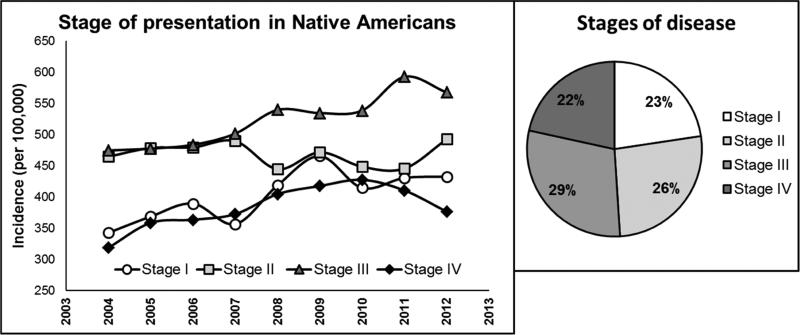
As documented in Figure 2, trends in incidence of stage I, III and IV CC was increasing with 23% of patients presented with Stage I while 29% patients presenting with Stage III. Patient had a trend (51%t vs 49%, p=0.12) towards presentation in higher stage (stage III/IV) which remained unchanged over the years.
Figure 2.
Trends in incidence of CC by the stage of presentation in Native Americans.
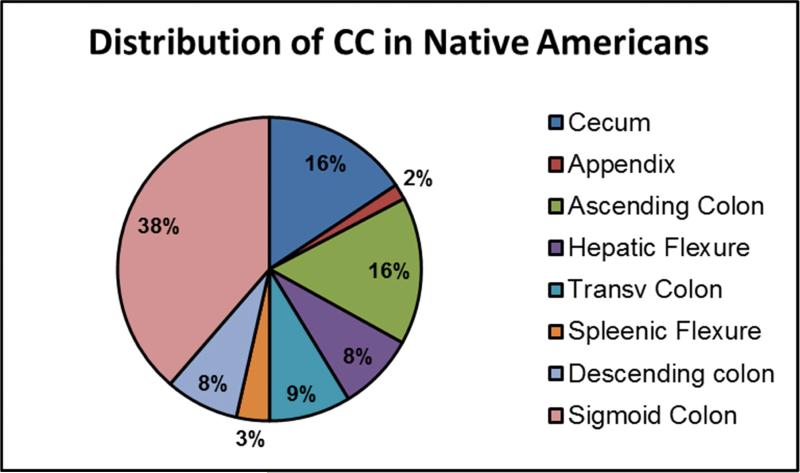
Figure 3 demonstrates distribution in location of CC tumors among Native American patients with sigmoid colon being the most common site representing 38% of all tumors. In a summary, 55% of all tumors were localized in left colon while 36% in right colon, suggesting that left-sided CC is prevalent in Native Americans with the majority of CC tumors being moderately differentiated (72%). There was a trend towards decrease (p=0.1) in the incidence of sigmoid CC over the years. There were 71% patients insured, 21% patients had Medicaid, and 3% patients were uninsured. There was no difference in insurance status over the years.
Figure 3.
Distribution in location of CC among Native Americans.
DISCUSSION
Racial disparities in the incidence of CC are established in the literature (3). However, targeted analysis of CC incidence and characteristics of CC in Native Americans are still sparse at best. Results of this study demonstrate that there are significant disparities in the incidence and characteristics of CC in Native Americans compared to general US population. Alarmingly increasing trend in incidence of CC was observed in Native Americans despite overall decreasing trends seen nationally. This study adds critical key information on incidence rates of CC among a population of Native American patients.
Trend analysis of incidence data between 2000 and 2012 revealed that incidence of CC among Native Americans increased by 38% and continued to rise in the past decade. Higher incidence has previously been demonstrated in the rate of CC among NA (11). Previous study has shown that incidence of colorectal cancer was decreasing between 1991 and 2011 in all racial/ethnic groups except for Native Americans (5). Results from our study that analyzed the SEER data between 2000 and 2012 confirm and accentuate these findings showing 38% increase in incidence of CC within this racial/ethnic group. These findings of increasing incidence rates of CC in Native Americans lead investigators to question the causes of this trend.
Analysis of CC incidence based on gender in this study showed a higher prevalence in Native American females compared to males while previous studies for time periods 2006-2010 and 2004-2014 showed higher rates of CC incidence in males when compared to females (5, 11). Our study also revealed that the highest number of all CC tumors were stage III at the time of diagnosis with the most common location in the sigmoid colon and majority of tumors being moderately differentiated. The findings of significantly increasing incidence of CC in Native Americans, surprisingly higher incidence in females and the late stage of disease at the time of diagnosis suggests a need for more aggressive screening measures in this population. Females are traditionally the caretakers of the family within the Native American population which could stop them or delay seeking health care services on a normal basis. This could be one of the causes contributing significantly to higher rates of CC within this gender group. Subsequently, these missed/delayed screening opportunities translate into more advanced stages of CC at diagnosis. This ultimately feeds the cycle of increasing incidence and mortality rates of Native Americans with CC that have been previously demonstrated (5, 12).
Insurance status of patients was assessed in this study and showed that a large majority of the Native American patients with CC were insured. However, there was no difference in insurance status over the years. Although most of the patients included in this study were insured at the time of diagnosis, lack of insurance is another variable that contributes to a lack of screening and/or access to any health care services. Studies have shown an association between lack of insurance and increased CC related-deaths (6). Despite national efforts to increase insurance coverage among patients, this does not appear to have reflected among Native American population. We believe this requires further investigation and assessment to better understand the role of insurance coverage among patients from this racial/ethnic group.
Lack of awareness and proper education could be contributing factors of the increase incidence of CC in NA. In addition, the effect of cultural barriers could not be discounted especially since a significant majority of the patients have health insurance. Cultural sensitivity is imperative when educating NA on the importance of early screening for colorectal cancer.
This study has its inherent limitations including being a retrospective analysis of a national cancer database that represents approximately 28% of the population of the United States. Patients were categorized as Native Americans based on the variable in the SEER database. There could be variations within this category including the percentage of Native American blood required to classify a patient as Native American. This study also did not take into account rural versus urban dwelling patients, which can introduce a substantial amount of error into the incidence of CC because of the variability in access to health care facilities that exists between rural versus urban locations. This study did not address age of patients with CC. Although the SEER database is the largest cancer registry in the United States, it records only a proportion of the Native American population. However, even despite this limitation, we were able to demonstrate significant trends in outcomes among Native American patients with colon cancer. Despite these limitations, this study has explored the disparities in incidence of CC in Native American patients over the period from 2000-2012.
CONCLUSION
Demographic and disease variability exists among Native American patients with CC in the United States. The incidence of CC among Native Americans continued to rise in the past decade despite national decreasing trends. Furthermore, patients continued to present at a higher stage of CC with moderate differentiation. In addition, no difference in insurance status rates over the years was noted. Evaluating CC screening practices among Native American patients may shed light on potential causes of the disparities demonstrated in this study. However, further research is required to fully understand the reasons for the differences among Native American patients with CC to help improve patient outcomes.
ACKNOWLEDGEMENT
This work was supported in part by an NCI Cancer Center Support Grant P30 CA023074 (CCSG).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no financial or proprietary interest in the subject matter or materials discussed in the manuscript.
REFERENCES
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Statistics - Colon Cancer Alliance - Prevention, Research, Patient Support. [March 7, 2016];Colon Cancer Alliance. Available at: http://www.ccalliance.org/get-information/what-is-colon-cancer/statistics/.
- 3.Siegel R, DeSantis C, Jemal A. Colorectal cancer statistics, 2014. [March 7, 2016];CA: A Cancer Journal for Clinicians. 2014 64:104–117. doi: 10.3322/caac.21220. doi: 10.3322/caac.21220. Available at: http://onlinelibrary.wiley.com/doi/10.3322/caac.21220/full. [DOI] [PubMed] [Google Scholar]
- 4.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 5.A Snapshot of Colorectal Cancer. National Cancer Institute; [March 7, 2016]. Available at: http://www.cancer.gov/research/progress/snapshots/colorectal. [Google Scholar]
- 6.Tawk R, Abner A, Ashford A, Brown CP. Differences in Colorectal Cancer Outcomes by Race and Insurance. National Center for Biotechnology Information; [March 7, 2016]. Available at: http://www.ncbi.nlm.nih.gov/pubmed/26703651. [Google Scholar]
- 7.Surveillance, Epidemiology, and End Results (SEER) Program ( www.seer.cancer.gov) SEER*Stat Database: Incidence – SEER 18 Regs Research Data + Hurricane Katrina Impacted Louisiana Cases, Nov 2014 Sub (1973-2012 varying) – Linked to County Attributes – Total U.S., 1969-2013 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2015, based on the November 2014 submission.
- 8. [March 7, 2016];Data Flow in NCI's SEER Registries. Available at: http://seer.cancer.gov/about/factsheets/seer_data_flow_.pdf.
- 9.Surveillance, Epidemiology, and End Results Program [March 7, 2016];Overview of the SEER Program. Available at: http://seer.cancer.gov/about/overview.html.
- 10.Surveillance, Epidemiology, and End Results Program [March 7, 2016];SEER Adjustments for Areas Impacted by Hurricanes Katrina and Rita. Available at: http://seer.cancer.gov/data/hurricane.html.
- 11.American Cancer Society . Cancer Facts & Figures 2014. American Cancer Society; Atlanta: 2014. [March 7, 2016]. Available at: http://www.cancer.org/acs/groups/content/@research/documents/webcontent/acspc-042151.pdf. [Google Scholar]
- 12.Cueto CV, Szeja S, Wertheim BC, Ong ES, Tsikitis VL. Disparities in Treatment and Survival of White and Native American Patients with Colorectal Cancer: A SEER Analysis. J Am Coll Surg. 2011;213(4):469–74. doi: 10.1016/j.jamcollsurg.2011.05.026. [DOI] [PubMed] [Google Scholar]