Abstract
Introduction
Previous studies of scorpion envenomation in the United States (US) have focused on Arizona and the bark scorpion, Centruroides sculpturatus. Although many other scorpion species live in the US, information about envenomations in other states is lacking.
Methods
Nationwide scorpion exposures from 2005 to 2015 were analyzed using the National Poison Data System.
Results
Of the 185,402 total exposures, Arizona (68.2%), Texas (10.3%), and Nevada (4.2%) were the top contributors. However, six other southern states reported greater than 100 cases annually, primarily during the warmer months and evening hours. Envenomations occurred most often in a home (97.8%) and were typically managed on-site (90.1%). Pain was the most common effect nationwide (88.7%). Arizona had the highest frequencies of sensory, neuromuscular, and respiratory effects along with higher hospitalization and ICU admission rates, although the latter appeared to drop over the study period. In contrast, local skin effects such as erythema and edema were more common outside of Arizona. Children under 10 years of age in Arizona and Nevada had the highest rates of systemic effects, hospitalization, and ICU admission.
Conclusions
Scorpion envenomations occurred throughout the southern US with similar seasonal and daily variations. Common clinical effects included pain, local edema, and erythema, except in Arizona and Nevada where severe systemic symptoms were more common. Systemic effects correlated with high rates of ICU admissions and intubations, especially in children under 10 years of age.
Electronic supplementary material
The online version of this article (doi:10.1007/s13181-016-0594-0) contains supplementary material, which is available to authorized users.
Keywords: Scorpions, Poison control centers, United States
Introduction
In 2014, poison control centers (PCCs) in the United States (US) received more than 16,000 reports of scorpion envenomation [1]. This was for more than any other insect and more than snakes and spiders combined. In fact, scorpion exposures accounted for nearly 30% of all reports concerning bites, stings, or envenomations. It is generally accepted that the only native US scorpion species of medical significance is the Arizona bark scorpion, Centruroides sculpturatus (previously known as C. gertschi, striped variant [2], and C. exilicauda [3]). Historically, the sting of this scorpion was the leading cause of death by envenomation in Arizona between 1929 and 1948 [4]. Consequently, most previous studies of the epidemiology of scorpion envenomations in the US have focused on Arizona and C. sculpturatus. These studies have shown that children are more severely affected [5–7] and that envenomations are most frequent in August–September [6]. Within the US, the geographic distribution of this species is thought to be limited to Arizona [2] and small parts of the neighboring states of New Mexico [8], Nevada [5], Texas, and California [9]. Other scorpions in Texas, especially C. vittatus (striped bark scorpion), also cause a large number of exposures during the summer months but only rarely result in major effects [10].
Comparing the annual nationwide case volumes reported to the American Association of Poison Control Centers (AAPCC) with those reported from Arizona and Texas, there remain several thousand annual exposures unaccounted for from other states. There is little data regarding the epidemiology, clinical effects, and outcomes from scorpion envenomation in these other states, with an overall lack of knowledge concerning the frequency and significance of these exposures. While a small number may be from travel-related inadvertently imported scorpions or pet scorpions, these likely contribute little to the overall number. We undertook this study to better understand the current distribution and impact of scorpion envenomations throughout the US.
Methods
All US PCCs submit case data to the AAPCC’s National Poison Data System (NPDS) on a near real-time basis. Data were obtained for all human scorpion exposures reported during the 11-year period from January 1, 2005 through December 31, 2015. The data analyzed included the date and time of the report, exposure and reporter site, patient age and gender, route of exposure, signs and symptoms, management site, treatments, and medical outcome. Duplicated records (n = 5), cases with a confirmed non-exposure (n = 128), and those not originating from one of the fifty US states (n = 440) were excluded. For analysis of clinical effects, only those manifestations recorded as related to the exposure were included. For analysis of treatments, only those recorded as “performed” or “recommended and performed” were included. ArcGIS (© Esri Inc., version 10.4.1) was used to generate a state-level frequency map using state boundary data from the US Census Bureau.
This study was approved by the institutional review board at Banner–University Medical Center Phoenix.
Results
There were 185,402 scorpion exposures over the 11-year study period, corresponding to an average of 16,855 cases per year nationwide. Almost all exposures were stings (sometimes coded as dermal or parenteral) except for 1510 (0.8%) coded as ingestions, with 49 of these reported as intentional. Females accounted for 105,038 (56.7%) of patients while 276 (0.1%) were unknown gender. The majority of exposures occurred in a residence (181,372; 97.8%), most reports came from a residence (165,342; 89.2%), and most were managed on-site (167,007; 90.1%).
Geographic Distribution
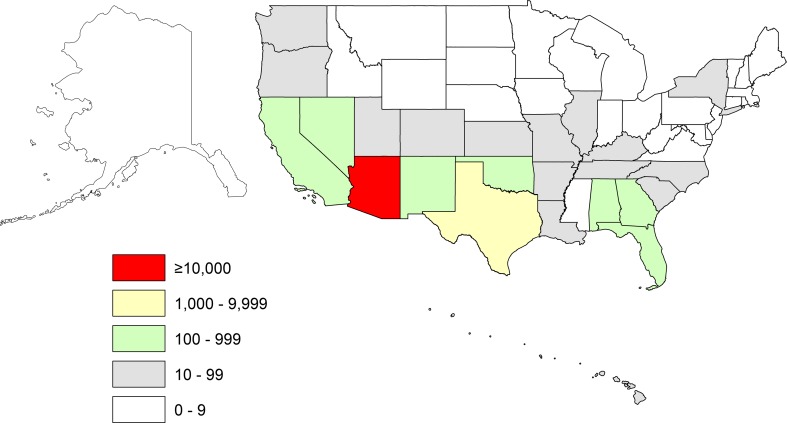
Scorpion exposures were reported from every US state and the District of Columbia, although at very low numbers for many of them (Fig. 1). Nine states reported an average of over 100 cases per year (Table 1). Arizona accounted for 126,502 (68.2%) of cases, with an annual average of 11,500. Texas had the second most with 19,168 (10.3%), corresponding to an annual average of 1743, while Nevada was third with 7775 (4.2%), yielding an annual average of 707.
Fig. 1.
Average annual scorpion exposures from 2005 to 2015 shown by state
Table 1.
Frequency of selected effects of scorpion envenomation reported in the nine states with over 100 calls per year. Percentages are relative to total exposures in each state
| State | Exposures total (annual average) | Major effects | Skin | Sensory | Neuromuscular | Respiratory | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Edema | Erythema | Pain | Numbness | Agitation | Ataxia | Nystagmus | Excess Secretions | |||
| Arizona | 126,502 (11,500) | 251 (0.20%) | 0.9% | 0.9% | 96.4% | 83.9% | 1.48% | 0.08% | 3.55% | 1.43% |
| Texas | 19,168 (1743) | 4 (0.02%) | 11.9% | 12.2% | 74.2% | 6.7% | 0.07% | 0.01% | 0.02% | 0.03% |
| Nevada | 7775 (707) | 10 (0.13%) | 9.0% | 13.0% | 78.3% | 14.9% | 0.71% | 0.15% | 0.60% | 0.26% |
| Florida | 6241 (567) | 2 (0.03%) | 13.0% | 15.1% | 70.1% | 2.1% | 0.05% | – | – | – |
| California | 5477 (498) | – | 5.5% | 6.6% | 53.9% | 3.4% | 0.15% | – | – | 0.05% |
| Georgia | 4915 (447) | – | 14.0% | 13.0% | 67.2% | 1.3% | 0.12% | – | – | 0.08% |
| Oklahoma | 3315 (301) | – | 14.1% | 15.4% | 81.2% | 4.9% | 0.33% | – | – | 0.03% |
| New Mexico | 3282 (298) | 1 (0.03%) | 19.4% | 29.2% | 75.7% | 13.4% | 0.64% | 0.03% | 0.06% | 0.24% |
| Alabama | 2133 (194) | 1 (0.05%) | 19.5% | 41.2% | 76.6% | 1.7% | 0.23% | – | – | 0.05% |
| Total | 178,808 (16,255) | 269 (0.15%) | 4.2% | 4.9% | 89.3% | 61.3% | 1.1% | 0.06% | 2.5% | 1.0% |
Several annual trends were noted. The south-central states of Texas, Oklahoma, Arkansas, and Louisiana showed large increases in exposures around a peak in 2012. Florida showed a dramatic decline in exposures from a peak of 852 cases in 2007 to just 233 in 2015. On the other hand, Nevada showed a consistent increase in the number of reports from 357 in 2005 to 1026 cases in 2015.
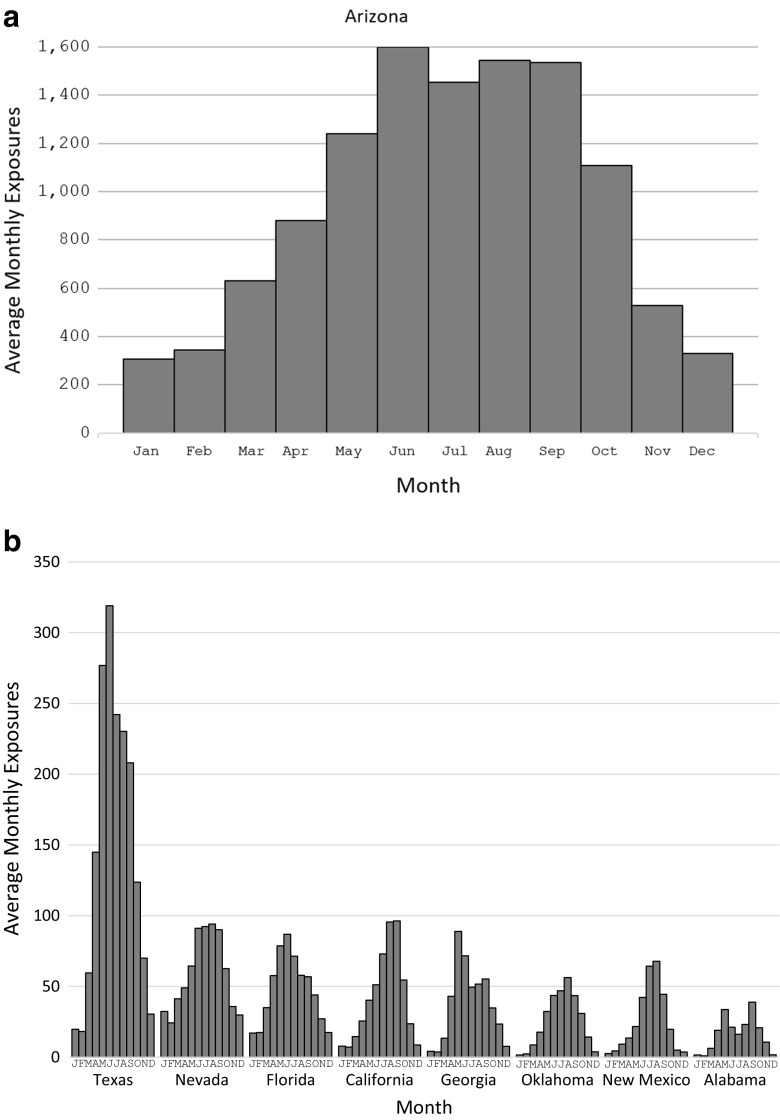
Time of Exposure
Exposures occurred throughout the year but at lower levels in colder months from December–February (Fig. 2). Even during these colder months in Arizona, monthly exposure frequency did not drop below 300 cases. Exposures began to increase in March and peaked at various times depending on the state. In Arizona and Nevada, a sustained peak from June–September was evident. Exposures in Texas, Georgia, and Florida peaked in May–June, while New Mexico and Oklahoma had later peaks in July–August. California had a late peak in August–September. Alabama appeared to have two peaks, once in May and again in September.
Fig. 2.
Monthly variation in scorpion exposure calls from 2005 to 2015 in the nine states with greater than 100 calls per year. a Arizona. b Eight other states with the most calls
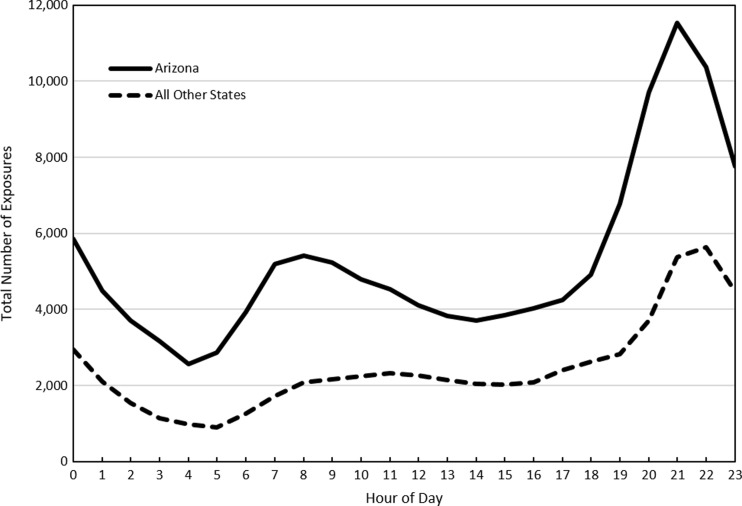
The daily pattern of exposures is shown in Fig. 3. Case frequency during the day was constant, increased after 5 PM, and peaked between 9 PM and 11 PM (8 PM–11 PM in Arizona). Unique to Arizona was a secondary peak in the morning (7–10 AM) as well. Cases were least frequent during the early morning hours of 2 AM through 6 AM. These patterns were consistent for each decade of age both in Arizona and nationwide.
Fig. 3.
Daily variation in scorpion exposure calls from 2005 to 2015
Signs and Symptoms
Major effects are defined by the AAPCC as life-threatening signs or symptoms (e.g., status epilepticus, respiratory compromise requiring intubation, cardiac or respiratory arrest) or a significant residual disability or disfigurement. Such effects were reported 276 times, with most of these in Arizona (251; 0.2% of Arizona cases) and Nevada (10; 0.1% of Nevada cases), as shown in Table 1. Notably, the annual frequency of major effects in Arizona did not change over the study period. Children under 10 years of age accounted for 184 (66.7%) of these major effects.
Five cardiac arrests were reported, though two were coded as unrelated to the scorpion exposure. Of the remaining three, two appeared to have survived. One was an infant from Arizona who reportedly experienced agitation, fasciculations, roving eye movements, and hypertension, along with dyspnea, excess secretions, and respiratory arrest. Another was a middle-aged adult in Florida documented as having respiratory depression, muscle weakness and paralysis, necrosis, and coma. Both were intubated, received chest compressions and antivenom. The remaining case was a previously reported death from Arizona in 2013.
The most common complaint from scorpion exposures nationwide was pain (164,394; 88.7%). Arizona exposures had a higher frequency of numbness (83.9%) compared to other states. Local skin findings of edema or erythema were rare in Arizona (0.9% each) but were variable elsewhere. For the eight other states receiving more than 100 reports per year, edema ranged from 5.5% in California to 19.5% in Alabama, while erythema ranged from 6.6% in California to 41.2% in Alabama. Agitation, nystagmus, and excessive secretions were relatively infrequent overall but most common in Arizona. These symptoms, along with vomiting, were much more common among children under 10 years of age.
Outcomes
Among the 16,275 (8.8%) patients referred to or evaluated at a healthcare facility (HCF), 12,542 (77%) were discharged (with or without treatment), while 1085 (8.4%) were admitted. Only two states averaged more than five hospitalizations per year: Arizona (858 total; 78/year) and Nevada (85 total; 8/year) (Table 2). Hospital admissions in these two states went to the ICU 66 and 46% of the time, respectively. Nationwide hospital admissions decreased during the study period from 146 in 2005 to 56 in 2015. This trend was due to a decrease in ICU admissions in Arizona over this time from a high of 111 in 2005 to 16 in 2015, with the most dramatic drop beginning in 2007 (see Online Resource 1).
Table 2.
Frequency of hospitalizations and selected treatments reported in the nine states with over 100 calls per year. Percentages are relative to total exposures in each state
| State | Total exposures | Hospitalizations | Benzodiazepines administered | Antivenom administered | Intubations performed | ||
|---|---|---|---|---|---|---|---|
| Non-ICU | ICU | Total | |||||
| Arizona | 126,502 | 292 (0.23%) | 566 (0.45%) | 858 (0.68%) | 2217 (1.8%) | 3307 (2.6%) | 141 (0.11%) |
| Texas | 19,168 | 12 (0.06%) | 7 (0.04%) | 19 (0.10%) | 6 (0.03%) | – | 3 (0.02%) |
| Nevada | 7775 | 46 (0.59%) | 39 (0.50%) | 85 (1.1%) | 70 (0.90%) | 28 (0.36%) | 9 (0.12%) |
| Florida | 6241 | 14 (0.22%) | 20 (0.32%) | 34 (0.54%) | – | 1 (0.02%) | 1 (0.02%) |
| California | 5477 | 6 (0.11%) | 6 (0.11%) | 12 (0.22%) | 7 (0.13%) | 4 (0.07%) | – |
| Georgia | 4915 | 14 (0.28%) | 8 (0.16%) | 22 (0.45%) | 3 (0.06%) | – | – |
| Oklahoma | 3315 | 3 (0.09%) | 1 (0.03%) | 4 (0.12%) | 3 (0.09%) | – | – |
| New Mexico | 3282 | 1 (0.03%) | 5 (0.15%) | 6 (0.18%) | 11 (0.34%) | 1 (0.03%) | 1 (0.03%) |
| Alabama | 2133 | 1 (0.05%) | – | 1 (0.05%) | – | – | – |
| Total | 178,808 | 389 (0.22%) | 652 (0.36%) | 1041 (0.58%) | 2317 (1.3%) | 3341 (1.9%) | 155 (0.09%) |
Children under 10 years of age had the highest rate of hospitalizations (2.1%) and ICU admissions (1.6%) as seen in Table 3. In this age group, 84.3% (424 of 503) of Arizona admissions and 56.5% (26 of 46) in Nevada were to an ICU. Older patients (70 years and above) also had higher hospitalization rates, although no major effects were reported in any patient over 80 years of age.
Table 3.
Frequency of selected outcomes for scorpion envenomation reported by decade of age. Percentages are relative to total exposures in each age group
| Age range (Yrs) | Total exposures | Major effects | Hospitalizations | Benzodiazepines administered | Antivenom administered | Intubations performed | ||
|---|---|---|---|---|---|---|---|---|
| Non-ICU | ICU | Total | ||||||
| 0–9 | 28,192 | 184 (0.65%) | 120 (0.43%) | 465 (1.6%) | 585 (2.1%) | 993 (3.5%) | 2376 (8.4%) | 139 (0.49%) |
| 10–19 | 24,882 | 18 (0.07%) | 41 (0.16%) | 34 (0.14%) | 75 (0.30%) | 216 (0.87%) | 252 (1.0%) | – |
| 20–29 | 25,860 | 8 (0.03%) | 55 (0.21%) | 23 (0.09%) | 78 (0.30%) | 156 (0.60%) | 98 (0.38%) | 1 (0.00%) |
| 30–39 | 25,799 | 10 (0.04%) | 49 (0.19%) | 25 (0.10%) | 74 (0.29%) | 183 (0.71%) | 91 (0.35%) | 2 (0.01%) |
| 40–49 | 23,536 | 10 (0.04%) | 39 (0.17%) | 21 (0.09%) | 60 (0.25%) | 183 (0.78%) | 112 (0.48%) | 2 (0.01%) |
| 50–59 | 20,824 | 10 (0.05%) | 45 (0.22%) | 30 (0.14%) | 75 (0.36%) | 249 (1.2%) | 127 (0.61%) | 3 (0.01%) |
| 60–69 | 14,115 | 15 (0.11%) | 64 (0.45%) | 23 (0.16%) | 87 (0.62%) | 177 (1.3%) | 131 (0.93%) | 4 (0.03%) |
| 70–79 | 6819 | 11 (0.16%) | 41 (0.60%) | 28 (0.41%) | 69 (1.0%) | 119 (1.7%) | 88 (1.3%) | 5 (0.07%) |
| ≥80 | 2886 | – | 23 (0.80%) | 12 (0.42%) | 35 (1.2%) | 53 (1.8%) | 45 (1.6%) | 1 (0.03%) |
| Unknown | 12,489 | 10 (0.08%) | 9 (0.07%) | 2 (0.02%) | 11 (0.09%) | 19 (0.15%) | 36 (0.29%) | – |
| Total | 185,402 | 276 (0.15%) | 486 (0.26%) | 663 (0.36%) | 1149 (0.62%) | 2348 (1.3%) | 3356 (1.8%) | 157 (0.08%) |
Therapies
The most frequently performed treatments were irrigation/washing (153,189; 82.6%) followed by antihistamines (14,483; 7.8%). Vasopressor use was rare, with only 32 instances recorded. Among the 155 reported intubations, 54 of these patients received antivenom. The data set does provide order of interventions. Most benzodiazepine and antivenom administrations, as well as intubations occurred in Arizona (Table 2). Again, the youngest age group of children under 10 years of age had the highest frequencies of benzodiazepine and antivenom usage as well as intubations (Table 3). Antivenom use peaked in 2010 and remained stable at a lower level from 2012 to 2015 (see Online Resource 1). Benzodiazepine use remained relatively stable during those same years while the number of reported intubations decreased by the end of the study period.
Discussion
Nearly 17,000 annual scorpion exposures were reported to US PCCs between 2005 and 2015. Nine states had an annual average of more than 100 cases, with Arizona, Texas, and Nevada being the top three. Based on these data, scorpion envenomations are occurring in many states with an annual incidence suggesting the exposures are from local (not imported) species.
Fortunately, most exposures were mild enough to be managed at home. Pain was the most commonly reported complaint nationwide. Several US scorpion species, including C. vittatus and Vaejovis spinigerus, are known to cause pain [11] and inject an α-toxin that opens sodium channels on nociceptive neurons [12].
Local skin effects of edema and erythema were infrequent in Arizona, which is typical of C. sculpturatus envenomations. The venom of another Arizona scorpion, V. spinigerus, is known to cause local edema [13, 14]. Outside of Arizona, local skin effects were reported more frequently but with considerable variation. In Texas and the neighboring states of Oklahoma, Arkansas, and Louisiana, C. vittatus is common [15, 16]. Although this species is not typically associated with local erythema or edema [11], there is a risk of hypersensitivity reactions with repeated exposures [17–19], or even on an initial exposure due to cross-reactivity from the venom of the imported fire ant (Solenopsis spp.) [18], which is endemic in an overlapping area. Farther east, Vaejovis carolinianus (southern unstriped scorpion) is concentrated in Kentucky, Tennessee, and northern Alabama and Georgia [15]. Stings from this species may cause local reactions and possibly even necrotic skin lesions [20], although this has not been systematically studied. In the Southeast US, few species are reported [15], and three of them are Centruroides: C. hentzi (Hentz striped scorpion) [15, 21]; C. gracilis (slenderbrown scorpion); and C. guanensis. We were unable to locate any studies on the effects of venom from these species in the medical literature.
Arizona exposures were unique in causing the highest frequencies of systemic symptoms like numbness, agitation, nystagmus, and excessive secretions (which were not reported in other regions). Many scorpion species are known to live in Arizona, including Hadrurus arizonensis (desert hairy scorpion) and the V. “vorhiesi” group. The latter is also known as the “sky island” Vaejovis because of their limited geographic distribution to the sky islands of Arizona and New Mexico [13, 22]. None of these are known to cause these systemic effects.
This data set included three cardiac arrests that were thought to be related to scorpion envenomation. The details of one have already been reported in the literature [1]. Interestingly, the other two cases appear to have survived. Since NPDS data relies on voluntary reports, it is likely that deaths are missed. Indeed, the Wide-ranging Online Data for Epidemiologic Research (WONDER) database from the Centers for Disease Control and Prevention (CDC), which uses death reports submitted by individual states, reported seven deaths due to scorpion envenomation between 1979 and 1999 [10]. From 1999 to 2014, another seven deaths are listed for an “underlying cause of death” of “contact with scorpions” (ICD10 = X22). Further, details such as age or state are suppressed for the 1999–2014 data due to the small number.
Although deaths have been rare recently, ICU admissions increased considerably when Arizona supplies of the goat-derived antivenom ran out in 2004 [23]. In 2007, a clinical trial of the equine Centruroides Immune F(ab')2 antivenom began (ClinicalTrials.gov Identifier NCT00624078) [24]. Notably, our data show that ICU admissions began to decrease dramatically beginning in 2007, despite the number of exposures experiencing major effects remaining consistent, supporting the effectiveness of the antivenom in preventing ICU admissions. Moreover, the number of non-ICU hospitalizations in Arizona also did not change, as these would generally be mildly envenomed patients that would not have received antivenom. Although there may have been a decrease in reporting of cases that received antivenom and then discharged home, serious cases that warranted ICU admission would have likely been reported to the PCCs in Arizona.
Children under 10 years of age had the highest frequencies of major effects, as well as vomiting, a finding which has been reported previously [25]. This age group also had the highest frequency of hospitalization and ICU admission. This nationwide pattern was primarily due to Arizona but was also evident in Nevada. The increased severity in younger patients and their greater ED usage and hospitalization is consistent with previous studies [6, 7].
A seasonal pattern to scorpion exposures was evident nationwide with the greatest activity occurring during the warmer months of the year. Arizona exhibited year-round activity with a three-month “low season” between December and February and a 4-month plateau lasting from June through September. A daily pattern was also observed with exposures more frequently reported in the evening. Arizona also exhibited a secondary peak in the morning. The seasonal variation is likely related to scorpion activity and population size while the daily variation is more likely reflective of times of increased home activity by people.
One additional finding of note was related to scorpion ingestions. Although a small number of intentional ingestions was expected, the larger number of unintentional ingestions was surprising. It is impossible to know how many of these constitute miscoding versus reports of scorpions being found in food, crawling into mouths while asleep, or even pediatric exploratory ingestions.
Limitations
There are several important limitations to this study related to the data source. NPDS data collection depends on callers reporting an exposure to the local PCC. Consequently, it is possible that the numbers reported in this study are an underestimate, especially for milder envenomations in areas where residents and healthcare providers are familiar with the clinical manifestations and treatment. Even with more severe effects, ED providers in Arizona may have become more comfortable with antivenom administration and discharge home without reporting to a PCC. Another important limitation with this data set is that since scorpion exposure is based on self-report, there is no way to confirm that a scorpion was even seen (although clinical findings at least with C. sculpturatus are relatively unique). Even if one was seen, the identity of the scorpion involved is either unknown or based on a layperson report, so no conclusions can be drawn related to specific species. As with all PCC calls, the validity of the data depends on several factors ranging from the willingness of the caller to provide appropriate information, to accurate and complete data entry at PCCs. Year-over-year changes should also be interpreted with caution because they may simply reflect differences in reporting rather than a change in exposure frequency. Finally, decisions to admit as well as admission location (ICU vs. non-ICU) are affected by many factors so regional differences should also be interpreted with caution.
Conclusions
In summary, scorpion exposures are consistently reported in almost all southern US states, usually at home, with peak exposures during warmer months and evening hours. Clinical effects were primarily pain, with varying degrees of edema and erythema; severe systemic manifestations were limited to the southwestern states—particularly Arizona and Nevada—where children under 10 years of age also had the highest rates of ICU admissions and intubations. There was a dramatic decline in ICU admissions for this age group that correlated in time with the availability of F(ab')2 antivenom during the study period. These results can help educate both healthcare providers and the public regarding the potential for scorpion envenomation and expected manifestations.
Electronic supplementary material
(PDF 178 kb)
Compliance with Ethical Standards
Funding
No funding was secured for this study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s13181-016-0594-0) contains supplementary material, which is available to authorized users.
References
- 1.Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL. 2014 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd annual report. Clin Toxicol (Phila). 2015;53(10):962–1147. doi:10.3109/15563650.2015.1102927. [DOI] [PubMed]
- 2.Stahnke HL. Some observations of the genus Centruroides marx (Buthidae, Scorpionida) and C. sculpturatus Ewing. Entomol News. 1971;82(11):281–307. [PubMed]
- 3.Valdez-Cruz NA, Dávila S, Licea A, Corona M, Zamudio FZ, García-Valdes J, et al. Biochemical, genetic and physiological characterization of venom components from two species of scorpions: Centruroides exilicauda Wood and Centruroides sculpturatus Ewing. Biochimie. 2004;86(6):387–396. doi: 10.1016/j.biochi.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Stahnke HL. The Arizona scorpion problem. Ariz Med. 1950;7(3):23–29. [Google Scholar]
- 5.Curry SC, Vance MV, Ryan PJ, Kunkel DB, Northey WT. Envenomation by the scorpion Centruroides sculpturatus. J Toxicol Clin Toxicol. 1983;21(4–5):417–449. doi: 10.3109/15563658308990433. [DOI] [PubMed] [Google Scholar]
- 6.Likes K, Banner W, Jr, Chavez M. Centruroides exilicauda envenomation in Arizona. West J Med. 1984;141(5):634–637. [PMC free article] [PubMed] [Google Scholar]
- 7.Rimsza ME, Zimmerman DR, Bergeson PS. Scorpion envenomation. Pediatrics. 1980;66(2):298–302. [PubMed] [Google Scholar]
- 8.Crawford CS, Krehoff RC. Diel activity in sympatric populations of the scorpions Centruroides sculpturatus (Buthidae) and Diplocentrus spitzeri (Diplocentridae) J Arachnol. 1975;2:195–204. [Google Scholar]
- 9.Russell FE, Madon MB. Introduction of the scorpion Centruroides exilicauda into California and its public health significance. Toxicon. 1984;22(4):658–664. doi: 10.1016/0041-0101(84)90006-0. [DOI] [PubMed] [Google Scholar]
- 10.Forrester MB, Stanley SK. Epidemiology of scorpion envenomations in Texas. Vet Hum Toxicol. 2004;46(4):219–221. [PubMed] [Google Scholar]
- 11.Baerg WJ. The effect of the venom of some supposedly poisonous arthropods. Ann Entomol Soc Am. 1924;17(3):343–352. doi: 10.1093/aesa/17.3.343. [DOI] [Google Scholar]
- 12.Rowe AH, Xiao Y, Scales J, Linse KD, Rowe MP, Cummins TR, et al. Isolation and characterization of CvIV4: a pain inducing alpha-scorpion toxin. PLoS One. 2011;6(8) doi: 10.1371/journal.pone.0023520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stahnke HL. The venomous effects of some Arizona scorpions. Science. 1938;88(2277):166–167. doi: 10.1126/science.88.2277.166. [DOI] [PubMed] [Google Scholar]
- 14.Stahnke HL. The scorpions of Arizona [dissertation] Iowa: Iowa State University; 1939. [Google Scholar]
- 15.Shelley RM, Sissom WD. Distributions of the scorpions Centruroides vittatus (Say) and Centruroides hentzi (Banks) in the United States and Mexico (Scorpiones, Buthidae) J Arachnol. 1995;23:100–110. [Google Scholar]
- 16.Yamashita T, Rhoads DD. Species delimitation and morphological divergence in the scorpion Centruroides vittatus (Say, 1821): insights from phylogeography. PLoS One. 2013;8(7) doi: 10.1371/journal.pone.0068282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.More D, Nugent J, Hagan L, Demain J, Schwertner H, Whisman B, et al. Identification of allergens in the venom of the common striped scorpion. Ann Allergy Asthma Immunol. 2004;93(5):493–498. doi: 10.1016/S1081-1206(10)61418-4. [DOI] [PubMed] [Google Scholar]
- 18.Nugent JS, More DR, Hagan LL, Demain JG, Whisman BA, Freeman TM. Cross-reactivity between allergens in the venom of the common striped scorpion and the imported fire ant. J Allergy Clin Immunol. 2004;114(2):383–386. doi: 10.1016/j.jaci.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 19.Demain JG, Goetz DW. Immediate, late, and delayed skin test responses to Centruroides vittatus scorpion venom. J Allergy Clin Immunol. 1995;95(1 Pt 1):135–137. doi: 10.1016/S0091-6749(95)70163-X. [DOI] [PubMed] [Google Scholar]
- 20.Elston DM. What’s eating you? Plain eastern stripeless scorpion (Vaejovis carolinianus) Cutis. 2006;78(6):393–394. [PubMed] [Google Scholar]
- 21.Stevenson DJ, Greer G, Elliott MJ. The distribution and habitat of Centruroides hentzi (Banks) (Scorpiones, Buthidae) in Georgia. Southeast Nat. 2012;11(4):589–598. doi: 10.1656/058.011.0404. [DOI] [Google Scholar]
- 22.Ayrey RF, Soleglad ME. New species of Vaejovis from the Santa Rita Mountains, southern Arizona (Scorpiones: Vaejovidae) Euscorpius. 2014;183:1–13. [Google Scholar]
- 23.Riley BD, LoVecchio F, Pizon AF. Lack of scorpion antivenom leads to increased pediatric ICU admissions. Ann Emerg Med. 2006;47(4):398–399. doi: 10.1016/j.annemergmed.2005.11.042. [DOI] [PubMed] [Google Scholar]
- 24.Boyer L, Degan J, Ruha AM, Mallie J, Mangin E, Alagon A. Safety of intravenous equine F(ab')2: insights following clinical trials involving 1534 recipients of scorpion antivenom. Toxicon. 2013;76:386–393. doi: 10.1016/j.toxicon.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 25.O’Connor A, Ruha AM. Clinical course of bark scorpion envenomation managed without antivenom. J Med Toxicol. 2012;8(3):258–262. doi: 10.1007/s13181-012-0233-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 178 kb)