Abstract
Introduction
We assessed the efficacy of a brief, 8-h teaching program, using an objective structured clinical examination (OSCE) for the use of a pocket ultrasound device (echoscope) focused on bed side diagnosis of subclinical ascites in chronic liver disease.
Patients and methods
Ten cirrhotic patients, five with subclinical ascites and five without, were selected during ultrasound examination performed with a high performance equipment for screening of hepatocellular carcinoma. Five post graduate medical doctors residents in Gastroenterology or Internal Medicine underwent a brief, 8-h theoretical and hands-on examinations training. The methodology to assess the correct competence consisted in two phases defined by actions and answers to questions.
Results
The evaluation of the technical efficacy was positive in all five students. The diagnostic efficacy for the ten patients examined consisted in no false positive diagnosis of ascites and one false negative.
Conclusions
In this preliminary experience, the use of a pocket ultrasound device (echoscope) for diagnosis of subclinical ascites in the context of a short structured teaching program and examination was efficient.
Keywords: Cirrhosis, Ascites, Echoscopy, Teaching assessment, Ultrasound
Riassunto
Abbiamo valutato l’efficacia didattica di un breve corso della durata di 8 ore secondo l’esame clinico strutturato ed oggettivo (OSCE) per l’uso di un ecografo tascabile (ecoscopio) per la diagnosi al letto dell’ascite subclinica in pazienti con epatopatia cronica. Pazienti e Metodi: Dieci pazienti cirrotici, cinque con ascite subclinica e cinque senza, sono stati selezionati durante esami ecografici effettuati per la sorveglianza dell’epatocarcinoma con apparecchiatura ecografica di alto livello. Cinque medici specializzandi in Gastroenterologia o Medicina Interna hanno ricevuto otto ore di insegnamento teorico e pratico. Il metodo per accertare la competenza acquisita ha consistito in due fasi definite da specifiche azioni e risposte a domande. Risultati: La valutazione della efficacia tecnica ha dato risultato positivo in tutti gli studenti. La efficacia diagnostica sulla presenza o assenza di ascite subclinica nei dieci pazienti esaminati è risultata in nessun caso falso positivo e un caso falso negativo. Conclusioni: in questa esperienza preliminare l’uso di un ecografo tascabile appreso nel contesto di un breve programma didattico strutturato per la diagnosi di ascite subclinica si è dimostrato efficace.
Introduction
The term echoscope means the use of a small sonographic device as aid to physical diagnosis at the bed side [1]. For example during a physical examination to detect the border of the liver or the spleen or to detect doubtful or subclinical ascites or to further characterize a pulsatile abdominal mass. Adding a pocket ultrasound device examination to a physical examination is considered a promising approach to reducing waiting times and healthcare costs [1].
To date, only one standardized and objective structured clinical examination (OSCE) tool as previously defined [2, 3] was reported for the assessment of the “FAST” algorithm in trauma patients [4]. In emergency medicine the use in daily practice of the so called focused abdominal sonography for trauma (FAST) is now standardized by means of well-designed teaching programs.
Overall, the values of reliability and accuracy of this assessment tool are high enough to be used also for examinations in the field of general abdominal ultrasound as recently proposed [5].
The onset of ascites in cirrhosis or in advanced chronic liver disease indicates a poor prognosis and the mortality rate increases up to 20% at 1 year and 50% at 2 years [6].
No data exist on the natural history of grade 1 ascites defined as ascites only detectable by ultrasound (no treatment required), and it is not known how frequently patients will develop grade 2 (moderate) or 3 (large) ascites [7].
Aim of this study is to assess the efficacy of a brief teaching program using an OSCE for the use of a pocket ultrasound (echoscope) device focused for bed side diagnosis of subclinical ascites in chronic liver disease. Authors do not have any conflict of interest to declare.
Materials and methods
Equipment: pocket Ultrasound Vscan (GE Healthcare, Milwaukee, WI, USA) with phased array probe and high performance equipment Aloka Alfa-10 ultrasound with standard convex abdominal probe.
Five cirrhotic patients without ascites and five with subclinical ascites were selected by an expert sonographer medical doctor (SA, LG) performing ultrasound examinations with high performance equipment during screening for hepatocellular carcinoma. Subclinical ascites is defined as ultrasound detectable minimal fluid collection of 1 or 2 cm around the liver or spleen or between intestinal loops or in the pelvis.
All patients gave informed consent.
Five post graduate medical doctors residents in Gastroenterology or Internal Medicine underwent a brief 8-h training: 4 h of theoretical background on ultrasound physics, semantics, artifacts on images and dynamic video tape and 4 h of hands-on examinations.
Hands-on sessions were performed with standard high level ultrasound equipment and with a pocket ultrasound in patients with or without ascites.
The aim was to acquire ability in correct orientation of the probe, gain and depth regulation to obtain good quality static images, communication of breathing commands to the patient, explanation of frozen image obtained in the 5 preferred sites of fluid accumulation in patients in supine position as shown in Fig. 1.
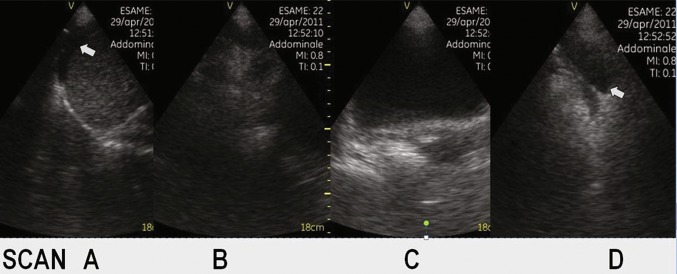
Fig. 1.
Identification of the five scans focused for ultrasound ascites diagnosis. a Right upper abdomen, b right iliac fossa, c Pelvis, d left iliac fossa, e left upper abdomen
At the end of the training each operator was asked to examine five previously selected patient without and five with subclinical ascites with the pocket ultrasound device (Fig. 2).
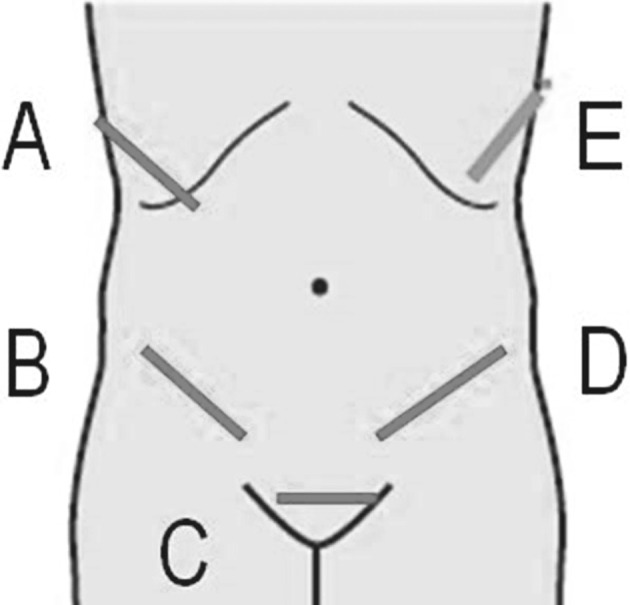
Fig. 2.
Ultrasound images obtained by Echoscope. In scan a anechoic fluid free collection between diaphragm and right liver surface (white arrow). Scan b right iliac fossa with colon gas. Scan c posterior to the bladder a small anechoic fluid collection. Scan d ascites in left iliac fossa (white arrow)
Competence was evaluated by means of a standardized and OSCE [3, 4].
The methodology to assess the correct competence consisted in two phases defined by actions and answers to questions in different time and way summarized with the term Station.
Station 1: an echoscope ready to use at bedside of a patient in supine position, a Check list with questions. Answers allowed in 4 min for question 1: (a) correct setting of the transducer (b) perform the 5 abdominal scheduled scans (c) store 1 picture for each scan.
Station 2: examine each of the 5 pictures stored (a, b, c, d, e as shown in Fig. 1) and write the answer in 1 min with description of the presence or absence of ascites. Question 2 a, b, c, d, e (yes or no).
The examiner observing single stored pictures obtained by each student had to complete the examiner check list. For Station 1: correct answer (y\n) to question 1 (a, b, c); and for Station 2: correct answer (yes or no) to question 2 (a, b, c, d, e).
Results
Evaluation of the technical efficacy requested in Station 1 was correct in all five students for the ten patients examined. Students were able to obtain good quality pictures of the five abdominal scheduled areas (Table 1).
Table 1.
Results to examiner questions in the five cirrhotic patients without ascites
| ID student | Appropriate results of all three Q1 questions (a b c) | Number of correct results of the five Q2 questions (a b c d e) | Appropriate results of all five Q2 questions (a b c d e) |
|---|---|---|---|
| 1 | Y | 5 | TN |
| 2 | Y | 5 | TN |
| 3 | Y | 5 | TN |
| 4 | Y | 5 | TN |
| 5 | Y | 5 | TN |
True negative results regarding the absence of ascites in all
Y yes appropriate result, TN true negative, Q1 question related to station 1; (a) correct setting of the transducer (b) perform the 5 abdominal scheduled scans (c) store 1 picture for each scan; Q2 question related to station 2; description of the presence or absence of ascites in each of the 5 pictures stored (a b c d e)
Evaluation of answers for Station 2 related to the five patients without ascites found true negative diagnosis for all the students (no fluid in any of the five scheduled abdominal scans) that means no false positive diagnosis of ascites.
For the five patients with subclinical ascites true positive examinations were defined when at least in one of the five scheduled scans ascites was depicted.
Results showed true positive diagnosis in four of the five patients. That means a false negative diagnosis of subclinical ascites in one patient (Table 2).
Table 2.
Results to examiner question in the five cirrhotic patients with subclinical ascites: only student 3 gave false negative results (failed to reveal ascites in all 5 scans), student 4 failed to reveal ascites in 2 out of 5 scheduled scans
| ID student | Appropriate results of all three Q1 questions (a b c) | Number of correct results of the five Q2 questions (a b c d e) | Appropriate results of the five Q2 questions (a b c d e) |
|---|---|---|---|
| 1 | Y | 5 | TP |
| 2 | Y | 5 | TP |
| 3 | Y | 0 | FNa |
| 4 | Y | 3 | TPb |
| 5 | Y | 5 | TP |
Y yes appropriate result, FN false negative, TP true positive, Q1 question related to station 1; (a) correct setting of the transducer (b) perform the 5 abdominal scheduled scans (c) store 1 picture for each scan; Q2 question related to station 2; description of the presence or absence of ascites in each of the 5 pictures stored (a b c d e)
aFalse Negative abcde
bFalse negative bce
Discussion
Decompensated cirrhosis is defined by the presence of physically detectable ascites, variceal bleeding, encephalopathy and/or jaundice [6]. Moreover, since ascites is most frequently the first of these signs to appear, it is usually considered a landmark sign of decompensated cirrhosis. Transition from a compensated to a decompensated stage occurs at a rate of 5–7%/year [6, 8].
Ultrasound is able to find small amount of ascites in compensated cirrhosis during screening for hepatocellular carcinoma as incidental diagnosis, to clarify doubtful findings after physical examination, for a semi-quantitative determination if clinically detectable. Ultrasound furthermore let us guide the needle for diagnostic and therapeutic paracentesis.
Diagnosis of subclinical ascites in cirrhosis is so far not recommended and when incidentally discovered there are no specific indications for treatment [7]. In Child Pugh functional classification of cirrhosis and in the recent definition of decompensation stage, ascites is defined only when detectable with physical examination [6].
Therefore the clinical perception of ascites is undoubtedly subjective and thus limits the value of the Child Pugh classification.
No data exist on the natural history of grade 1 ascites defined as ascites only detectable by ultrasound who need no treatment, and the timing of development of clinically significative ascites is not known [7].
Ultrasound teaching programs are not always well standardized and focused on each clinical problem [1]. There is a proof of concept that medical students can be taught basic ultrasound skills with limited didactic and hands-on instructions with the potential of using these skills in the patient clinics as an adjunct to routine physical diagnosis [9]. Similarly our study, though limited to few study cases, has proven the ability to train young medical doctors for the sonographic diagnosis of subclinical ascites, in a few hours.
In this preliminary experience the use of a pocket ultrasound device for diagnosis of subclinical ascites in the context of a short structured teaching program and examination was efficient with no false positive results.
In the bed side ultrasound era further experience could help us to understand more about the pathophysiology of ascites occurrence and stage migration from advanced chronic liver disease to decompensation.
Author contributions
Salmi Andrea designed and performed the research, analysis of the data and critical review. Lanzani Giovanna acquisition of data, drafting the article or making critical revisions related to important intellectual content of the manuscript. Campagnola Pietro performed the research, analysis of the data and critical review; Frulloni Luca analysis of the data and critical review.
Compliance with ethical standards
Conflict of interest
The authors declare that no potential conflict of interest financial or not.
Ethical approval
In this study patients received an abdominal ultrasound as part of scheduled examinations in good clinical practice for surveillance of hepatocellular carcinoma in cirrhosis.
Informed consent
Patients gave their informed consents to be additionally studied with a pocket ultrasound device during teaching sessions.
Footnotes
Adding a pocket ultrasound device examination to a physical examination is considered a promising approach to reducing waiting times and healthcare costs but we are lacking of well-designed teaching programs. We assessed the efficacy of a brief 8-h teaching program using an objective structured clinical examination for the use of a pocket ultrasound (echoscope) device focused for bed side diagnosis of subclinical ascites in chronic liver disease.
References
- 1.Colli A, Prati D, Fraquelli M, Segato S, Vescovi PP, Colombo F, Balduini C, Della Valle S, Casazza G. The use of a pocket-sized ultrasound device improves physical examination: results of an in- and outpatient cohort study. PLoS ONE. 2015;10(3):e0122181. doi: 10.1371/journal.pone.0122181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harden RM, Stevenson M, Downie WW, Wilson GM. Assessment of clinical competence using objective structured examination. Br Med J. 1975;1(5955):447–451. doi: 10.1136/bmj.1.5955.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cuschieri A, Gleeson FA, Harden RM, Wood RA. A new approach to a final examination in surgery Use of the objective structured clinical examination. Ann R Coll Surg Engl. 1979;61(5):400–405. [PMC free article] [PubMed] [Google Scholar]
- 4.Sisley AC, Johnson SB, Erickson W, Fortune JB. Use of an objective structured clinical examination (OSCE) for the assessment of physician performance in the ultrasound evaluation of trauma. J Trauma. 1999;47(4):627–631. doi: 10.1097/00005373-199910000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Hofer M, Kamper L, Sadlo M, Sievers K, Heussen N. Evaluation of an OSCE assessment tool for abdominal ultrasound courses. Ultraschall Med. 2011;32(2):184–190. doi: 10.1055/s-0029-1246049. [DOI] [PubMed] [Google Scholar]
- 6.D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44(1):217–231. doi: 10.1016/j.jhep.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 7.European Association for the Study of the Liver EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53(3):397–417. doi: 10.1016/j.jhep.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 8.D’Amico G, Pasta L, Morabito A, D’Amico M, Caltagirone M, Malizia G, Tinè F, Giannuoli G, Traina M, Vizzini G, Politi F, Luca A, Virdone R, Licata A, Pagliaro L. Competing risks and prognostic stages of cirrhosis: a 25-year inception cohort study of 494 patients. Aliment Pharmacol Ther. 2014;39(10):1180–1193. doi: 10.1111/apt.12721. [DOI] [PubMed] [Google Scholar]
- 9.Angtuaco TL, Hopkins RH, DuBose TJ, Bursac Z, Angtuaco MJ, Ferris EJ. Sonographic physical diagnosis 101: teaching senior medical students basic ultrasound scanning skills using a compact ultrasound system. Ultrasound Q. 2007;23(2):157–160. doi: 10.1097/01.ruq.0000263847.00185.28. [DOI] [PubMed] [Google Scholar]