Abstract
Liver hepatocytes (Hep) are known to be central players during the inflammatory response to systemic infection. Interestingly, the protein tyrosine phosphatases (PTP) SHP-1, has been recognized as a major regulator of inflammation; however their implication in the control of Hep-mediated inflammatory response is still unknown. To study its implication in the regulation of the Hep-mediated inflammatory response during endotoxemia, Cre-Lox mice with a Hep-specific Ptpn6 deletion (Ptpn6 H-KO) were injected with LPS. In contrast to the wild-type mice (Ptpn6 f/f) that started to die by 24 hrs post-inoculation, the Ptpn6 H-KO mice exhibited mortality by 6 hrs. In parallel, higher amounts of metabolic markers, pro-inflammatory mediators and circulating cytokines were detected in Ptpn6 H-KO mice. Primary Hep obtained from Ptpn6 H-KO, also showed increased secretion of pro-inflammatory cytokines and nitric oxide (NO) comparatively to its wild type (Ptpn6 f/f) counterpart. Pharmacological approaches to block TNF-α and NO production protected both the Ptpn6 f/f and the Ptpn6 H-KO mice against deadly LPS-mediated endotoxemia. Collectively, these results establish hepatocyte SHP-1 is a critical player regulating systemic inflammation. Our findings further suggest that SHP-1 activation could represent a new therapeutic avenue to better control inflammatory-related pathologies.
Introduction
Sepsis is a systemic, hyper-inflammatory immune condition triggered in response to invading pathogens1, and responsible for the death of millions of human worldwide2. It is characterized by uncontrolled production of pro-inflammatory mediators in the systemic circulation resulting from dysregulated host innate inflammatory response toward infection3. Persistence of a high level of pro-inflammatory mediators in the systemic circulation induces multi-organ failure or multi-organ dysfunction syndrome leading to patient death4. Sepsis involves excessive production of pro-inflammatory cytokines, such as Tumor necrosis factor alpha (TNF-α)5, Interleukin 1 beta (IL-1β)6 and Interleukin 6 (IL-6)7, which in turn hyper-activate different immune and non-immune cell types for the production of nitric oxide (NO)8 and reactive oxygen species (ROS)9.
Uncontrolled activation of phagocytes NF-κB and mitogen-activated protein kinase (MAPK) signalling cascades upon bacterial endotoxin stimulation have been found to be critical for the sepsis-induced hyper-production of various inflammatory mediators. For instance, mice deficient for MAPK phosphatase dual specificity phosphatase 1 (DUSP1)10 and MAP kinase phosphatase 1 (MKP-1)11 showed exacerbated Lipopolysaccharide (LPS)-induced endotoxemia conducting to rapid death and to be paralleled by enhance MAPK signalling pathway activation and augmented pro-inflammatory cytokines secretion10, 11. Therefore, modulation of the NF-κB and MAPK pathways may be useful for controlling sepsis-induced pathological manifestations.
Importantly, in addition to phagocytes being involved in the secretion of these inflammatory mediators, it is known that human hepatocytes directly stimulated with bacterial endotoxin can produce large amount of NO and pro-inflammatory cytokines that can significantly contribute to systemic inflammation development12–14 establishing liver as a crucial organ for the regulation of sepsis-induced pathology. In this regard, the Signal transducer and activator of transcription 3 (STAT3) signalling axis in hepatocytes has been identified as a profound negative regulator of the sepsis-associated, dysregulated inflammatory response15.
In addition to transcriptional regulatory mechanisms, ablation or suppression of selective anti-inflammatory signalling networks in hepatocytes may be important for the development of sepsis. One potential candidate is the protein tyrosine phosphatase SHP-1 since it is highly expressed in hepatocytes16 and is known to exert anti-inflammatory effects17. SHP-1 is a protein tyrosine phosphatase with two Src homology 2 domains and acts as a critical negative regulator of both innate and acquired immune responses18, 19. SHP-1 has been associated with several human inflammatory diseases. Psoriatic inflammatory skin disease patients exhibit a deficiency in the expression of SHP-1 in T cells20 and the macrophages of multiple sclerosis patients display SHP-1 deficiency21. Moreover, a previous report suggested that altered expression of SHP-1 in mast cells is associated with human allergies and asthmatic disease22. SHP-1 signalling within hepatocytes controls a variety of physiological and pathological processes23, 24; however, the significance of hepatocyte-specific SHP-1 has not been elucidated under systemic inflammatory conditions.
In the present study, the role of hepatocyte-specific SHP-1 signalling in the regulation of sepsis-induced inflammation was explored. We used hepatocyte-specific SHP-1 deficient mice (Ptpn6 H-KO) and studied the impact of SHP-1 signalling within hepatocytes in murine model of systemic inflammation induced by LPS. Compared to their wild-type counterparts (Ptpn6 f/f), the LPS-injected Ptpn6 H-KO mice exhibited increased mortality in association with higher amounts of lipopolysaccharide binding protein (LBP), serum amyloid A (SAA), and NO in the serum, and prolonged activation of MAPK in the liver, leading to a greater production of various pro-inflammatory cytokines. This study reveals a novel role of hepatocyte SHP-1 in controlling the production of inflammatory mediators during systemic inflammation, thus suggesting that the PTPase is a key player of the close link between hepatocyte metabolism and the immune system.
Results
Ptpn6H-KO mice are highly susceptible to LPS-induced endotoxemia and multiple organ failure
The liver is the central regulator of inflammation25 and the protein tyrosine phosphatase SHP-1 plays a crucial role in regulating inflammation18, 19. However, the function of hepatocyte-specific SHP-1 during LPS-induced endotoxic shock has not been studied to date. Therefore, we examined whether hepatocyte SHP-1 had any influence on the regulation of systemic inflammation during endotoxemia. We induced endotoxemia in the Ptpn6 f/f and Ptpn6 H-KO mice by injecting various doses of LPS intraperitoneally and measured survival and body temperature as indicators of LPS-mediated intoxication. At a relatively low dose of LPS challenge (5 mg/kg body weight), there was no statistically significant difference in survival (Fig. 1A) and body temperature (Fig. 1D) between the Ptpn6 H-KO and Ptpn6 f/f mice. Although, the survival of the Ptpn6 H-KO mice was affected to a greater extent compared to the Ptpn6 f/f mice. In contrast, we observed that at higher dose of LPS challenge (10 mg/kg body weight), all of the Ptpn6 H-KO mice died within 36 h. At the same dose of LPS challenge, nearly 70% of the Ptpn6 f/f mice survived past 72 h (Fig. 1B). Moreover, we observed a significant reduction in body temperature in the Ptpn6 H-KO mice compared to the Ptpn6 f/f mice at the same dose (10 mg/kg body weight) of LPS challenge (Fig. 1E). When the dose of LPS was further increased (30 mg/kg body weight), all the Ptpn6 H-KO mice died within 12 hours, whereas most of the Ptpn6 f/f mice survived f or greater than 12 hours (Fig. 1C). Furthermore, at this higher dose of LPS, we observed a significant decrease in the body temperature of the Ptpn6 H-KO mice compared to the Ptpn6 f/f mice starting as early as 1 h post-LPS challenge (Fig. 1F).
Figure 1.
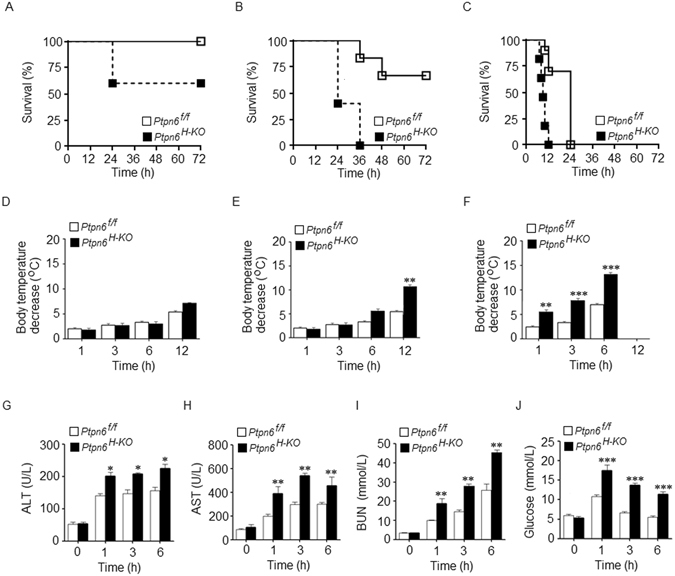
Ptpn6 H-KO mice are highly susceptible to multiple organ failure and endotoxemia. Survival curve of Ptpn6 f/f (WT) and Ptpn6 H-KO (KO) mice after LPS challenge of (A) 5 mg/kg body weight (n = 11 for WT mice and n = 10 for KO mice), (B) 10 mg/kg body weight (n = 11 for WT mice and n = 12 KO mice), and (C) 30 mg/kg body weight (n = 17 for WT mice and n = 18 for KO mice). P ≤ 0.03 for 10 mg/kg body weight and P ≤ 0.005 for 30 mg/kg body weight. Decrease in body temperature of Ptpn6 f/f and Ptpn6 H-KO mice after LPS challenge of (D) 5 mg/kg body weight, (E) 10 mg/kg body weight, and (F) 30 mg/kg body weight. Significant differences in body temperature reduction between Ptpn6 H-KO and Ptpn6 f/f mice at the indicated time points denoted with **P ≤ 0.05 and ***P ≤ 0.01. Serum levels of (G) ALT, (H) AST, (I) BUN and (J) Glucose in Ptpn6 f/f and Ptpn6 H-KO mice after LPS challenge (30 mg/kg body weight). Significant differences between LPS challenge Ptpn6 H-KO and Ptpn6 f/f mice at the indicated time points denoted with *P ≤ 0.05, **P ≤ 0.01 and ***P ≤ 0.01. Data are presented as mean ± SEM (n = 3–6 in each group).
To examine the effects of SHP-1 deficiency in hepatocytes on the function of key organs, we measured the amount of alanine aminotransferase (ALT) and aspartate transaminase (AST) in the serum to determine liver function and blood urea nitrogen (BUN) to determine renal function in the Ptpn6 H-KO and Ptpn6 f/f mice following LPS challenge (30 mg/kg body weight). Interestingly, we observed that LPS induced significantly higher amounts of ALT, AST (Fig. 1G,H) and BUN (Fig. 1I) in the Ptpn6 H-KO mice compared to that of the Ptpn6 f/f mice. In addition, LPS challenge induced hyperglycemia in both the Ptpn6 H-KO and Ptpn6 f/f mice during early time points (1 hour); however, it was only sustained at the later time points in the Ptpn6 H-KO mice (Fig. 1J).
Collectively, our results indicate that the Ptpn6 H-KO mice are highly susceptible to multiple organs failure compared to the Ptpn6 f/f mice after LPS administration and that hepatocyte SHP-1 plays a crucial role in regulating the sensitivity of mice to endotoxemia.
LPS challenge induced an exacerbated inflammatory response in Ptpn6H-KO mice by modulating MAPK activation
It is now well established that the lethality of endotoxemia is due to the dysregulated over-production of different pro-inflammatory mediators, including different cytokines and nitric oxide (NO). Therefore, we analyzed the expression of different pro-inflammatory mediators in the serum of the Ptpn6 H-KO and Ptpn6 f/f mice at different time points following LPS challenge (30 mg/kg body weight). We observed that the Ptpn6 H-KO mice produced higher levels of TNF-α, IL-1β and IL-6 as compared to their Ptpn6 f/f counterparts at all-time points in response to LPS challenge (Fig. 2A–C). A very significant increase in the plasma nitrate levels was measured in the Ptpn6 H-KO mice compared to that of the Ptpn6 f/f mice at 3 and 6 h following LPS challenge (Fig. 2D). In addition, we observed a significant augmentation of inducible nitric oxide synthase (iNOS) expression in the liver of the Ptpn6 H-KO mice compared to that of the Ptpn6 f/f mice during LPS challenge (Fig. 2E). Since the activation of MAPK is a crucial determinant for the production of LPS-induced inflammatory mediators9, we examined whether hepatocyte-specific SHP-1 deficiency had any influence on the regulation of MAPK signalling pathways during endotoxin shock. Interestingly, we observed that LPS induced rapid phosphorylation or activation of various MAPKs (p38, JNK1/2 and ERK1/2) in the liver of both the Ptpn6 H-KO and Ptpn6 f/f mice immediately after challenge (1 hour). The phosphorylation of these MAPKs diminished with time (3 and 6 hours) in the Ptpn6 f/f mice, but the Ptpn6 H-KO mice exhibited a sustained phosphorylation of these MAPKs even 3 h after LPS challenge (Fig. 2F). Previous reports suggested that acute phase proteins, including LBP26, SAA27 and Apolipoprotein E (ApoE)28, produced by the liver during inflammation play a stimulatory role in enhancing the extent and pathology of inflammation. Therefore, we determined whether SHP-1 deficiency in hepatocytes modulated the expression of LBP, SAA and ApoE after LPS challenge. We observed a significant enhancement in the amount of LBP, SAA and ApoE protein at 1, 3 and 6 hours post-LPS challenge in the Ptpn6 H-KO mice compared to the Ptpn6 f/f mice, as evidenced by whole serum western blot analysis (Fig. 2G).
Figure 2.
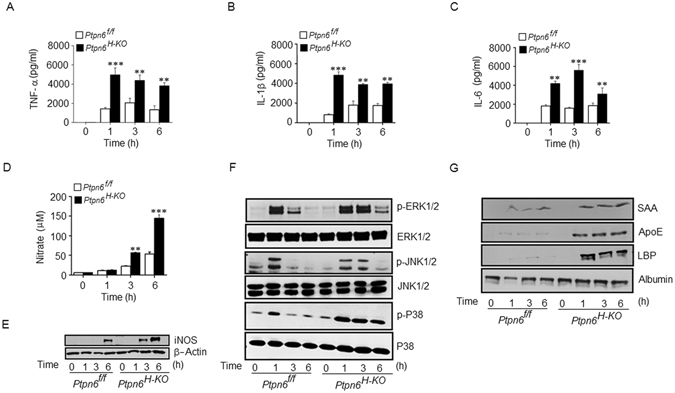
LPS challenge induced an exacerbated inflammatory response in the Ptpn6 H-KO mice by modulating MAPK activation. Serum concentration of (A) TNF-α (B) IL-1β, (C) IL-6 and (D) nitric oxide in Ptpn6 H-KO and Ptpn6 f/f mice after LPS challenge (30 mg/kg body weight). Data are presented as mean ± SEM (n = 6 in each group) **P ≤ 0.05 and ***P ≤ 0.01. Liver levels of (E) iNOS and (F) phospho-JNK1/2, phospho-ERK1/2 and phospho-p38, and serum levels of (G) SAA, ApoE and LBP in Ptpn6 H-KO and Ptpn6 f/f mice after LPS challenge (30 mg/kg body weight). The blots shown here are cropped from full length gel. Full-length blots are included in the Supplementary Information file. (E) iNOS in Supplementary Information 1 (F) phospho-JNK1/2, phospho-ERK1/2 and phospho-p38 in Supplementary Information 2 and serum levels of (G) SAA, ApoE and LBP in Ptpn6 H-KO and Ptpn6 f/f mice Supplementary Information 3.
Therefore, these observations suggest that hepatocyte-specific SHP-1 has an important role in regulating the production of inflammatory mediators by modulating MAPK activation in the liver during endotoxemia and in regulating acute phase protein secretion by the liver during LPS-induced inflammation.
LPS challenge induced greater neutrophil recruitment and NO production in the peritoneum of Ptpn6H-KO mice
LPS intoxication enhances peritoneal cavity inflammation through the recruitment of various inflammatory cells and their subsequent activation to produce high levels of inflammatory mediators29. In an attempt to characterize this response further, we studied NO generation, and total cell and neutrophil recruitment to the peritoneal cavity of the Ptpn6 H-KOand Ptpn6 f/f mice 6 h after LPS challenge. We detected a significantly higher amount of NO in the peritoneal lavage of the Ptpn6 H-KO mice compared to that of the Ptpn6 f/f mice 6 h post-LPS challenge (Fig. 3A). In addition, the total number of cells recruited to the peritoneal cavity of the Ptpn6 H-KO mice was found to be significantly higher compared to the Ptpn6 f/f mice after 6 h of LPS challenge (Fig. 3B). Moreover, the amount of neutrophils in the peritoneal fluid of the Ptpn6 H-KO was found to be markedly higher compared to the Ptpn6 f/f mice following 6 h of LPS challenge (Fig. 3C). Collectively, our observations indicate that hepatocyte specific SHP-1 has a crucial role in neutrophil immigration to the peritoneum during endotoxemia.
Figure 3.
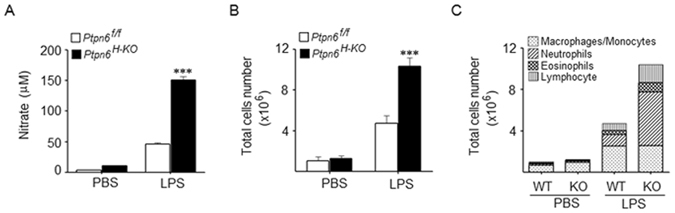
Nitric oxide, total cell number and neutrophil recruitment in peritoneum of Ptpn6 H-KO mice were significantly higher during LPS challenge. (A) NO production, (B) total cell count, and (C) neutrophil accumulation in the peritoneal fluid of Ptpn6 H-KO and Ptpn6 f/f mice after LPS challenge (10 mg/kg body weight). Data are presented as mean ± SEM (n = 6 in each group) ***P ≤ 0.01.
Ptpn6H-KO hepatocytes produce higher levels of inflammatory mediators during LPS challenge in vitro
To strengthen our in vivo findings, we carried out further experiments to characterize the consequences of SHP-1 deficiency on the hepatocyte-mediated production of different inflammatory mediators in vitro. We observed that LPS (1 µg/ml) induced a higher level of TNF-α, IL-1β and IL-6 expression in hepatocytes from Ptpn6 H-KO mice compared to hepatic cells from Ptpn6 f/f mice at 12 h and 24 h (Fig. 4A–C). Furthermore, hepatocytes from the Ptpn6 H-KO mice exhibited a very significant increase in NO production compared to hepatocytes of the Ptpn6 f/f mice, especially at 12 and 24 h post-LPS stimulation (Fig. 4D). However, we observed no significant difference in pro-inflammatory cytokine production and NO generation in the peritoneal macrophages isolated from both Ptpn6 H-KO and Ptpn6 f/f mice following LPS stimulation (Fig. 4E–H). Collectively, our observations indicate that hepatocyte SHP-1 has a pivotal role in modulating the inflammatory response to LPS.
Figure 4.
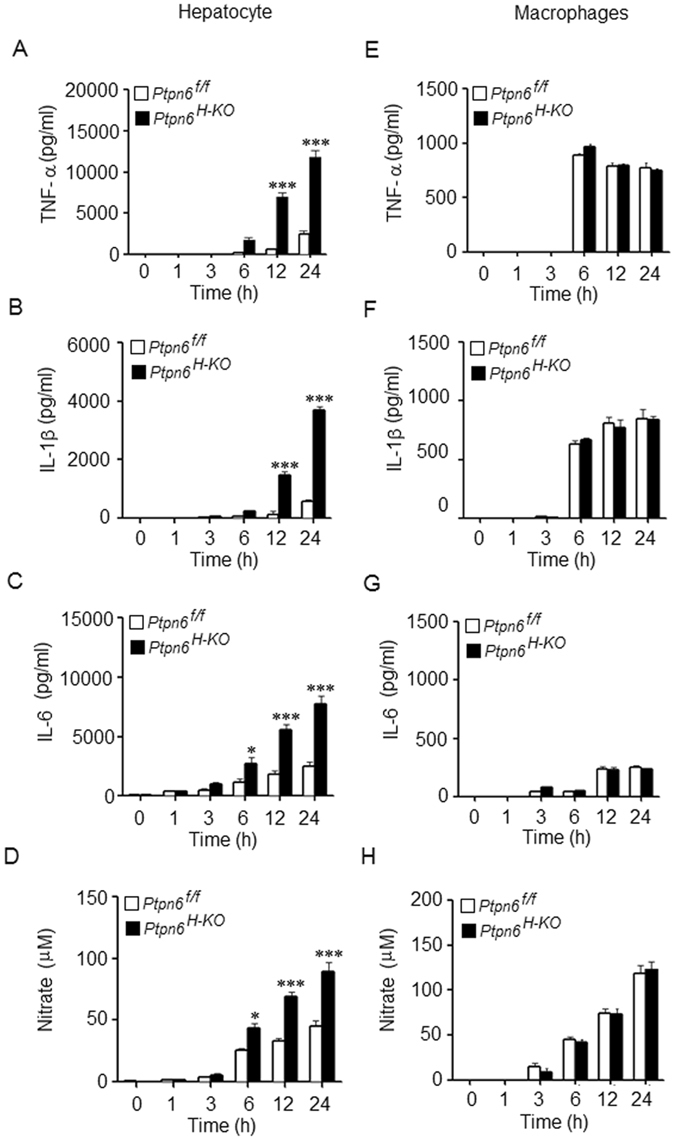
LPS induced inflammatory mediators in hepatocytes of Ptpn6 H-KO mice. Production of (A) TNF-α, (B) IL-1β, (C) IL-6 and (D) Nitric oxide by hepatocytes isolated from Ptpn6 H-KO and Ptpn6 f/f mice after LPS stimulation (1 μg/ml). Data are presented as mean ± SEM of three samples in three independent experiments. Production of (E) TNF-α, (F) IL-1β, (G) IL-6 and (H) nitric oxide by peritoneal macrophages isolated from Ptpn6 H-KO and Ptpn6 f/f mice after LPS stimulation (1 μg/ml). Data are presented as mean ± SEM of three samples in three independent experiments. *P ≤ 0.05, **P ≤ 0.01 and ***P ≤ 0.001.
LPS induced sustained MAPK activation in the hepatocytes of Ptpn6H-KO mice in vitro
To validate our in vivo findings, we performed experiments to examine whether SHP-1 deficiency had any significant influence on the activation of MAPK in hepatocytes after LPS stimulation in vitro. Rapid phosphorylation of MAPK induced by LPS was significantly abrogated in hepatocytes of Ptpn6 f/f mice compared to that of hepatocytes of Ptpn6 H-KO mice at later time points (45 and 60 min) (Fig. 5). To further confirm that the negative regulation of MAPK activation during LPS stimulation was solely dependent on the deficiency of SHP-1, we analyzed the activation of different MAPK in the peritoneal macrophages of the Ptpn6 H-KO and Ptpn6 f/f mice following LPS stimulation. We observed no significant difference in the status of MAPK activation in the peritoneal macrophages isolated from the Ptpn6 H-KO and Ptpn6 f/f mice at early as well as late time points of LPS stimulation (Fig. 5). Thus, these results clearly demonstrate that hepatocyte SHP-1 is a crucial negative regulator of the activation of various MAPK in response to LPS stimulation.
Figure 5.
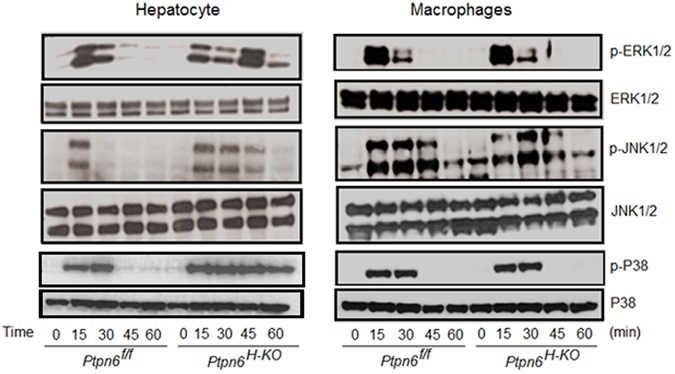
Attenuation of MAPKs activation in Ptpn6 f/f hepatocyte after LPS stimulation. Western blot of phospho-ERK1/2, phospho-JNK1/2 and phospho-p38 in hepatocytes and peritoneal macrophages isolated from Ptpn6 H-KO and Ptpn6 f/f mice treated with LPS (1 μg/ml). The blots shown here are cropped from full length gel. Full-length blots are included in the Supplementary Information file. Phospho-ERK1/2, phospho-JNK1/2 and phospho-p38 in hepatocytes in Supplementary Information 4, Phospho-ERK1/2, phospho-JNK1/2 and phospho-p38 in peritoneal macrophages in Supplementary Information 5.
Treatment with TNF-α inhibitor pentoxifylline and/or iNOS/NO inhibitor aminoguanidine rescued Ptpn6H-KO mice against deadly LPS challenge
Our previous data indicated that LPS challenge induces a larger amount of TNF-α and NO in Ptpn6 H-KO mice as compared to Ptpn6 f/f mice (Fig. 2A,D). Therefore, we pre-treated the Ptpn6 H-KO and Ptpn6 f/f mice with pentoxifylline (PTX) (TNF-α inhibitor), aminoguanidine (AMG) (iNOS inhibitor), or both to determine whether the elevated levels of TNF-α and/or NO were responsible for the increased death of the Ptpn6 H-KO mice following LPS challenge. Interestingly, we observed that pentoxifylline treatment rescued approximately 70% of the Ptpn6 H-KO mice (Fig. 6A), that aminoguanidine treatment rescued approximately 50% of the Ptpn6 H-KO mice (Fig. 6B) while the combined treatment was found to rescue approximately 70% of the Ptpn6 H-KO mice (Fig. 6C). In addition, pentoxifylline treatment significantly decreased the concentration of TNF-α (Fig. 6D) and other cytokines (supplementary Fig. 1A,B) in the serum. Moreover, the concentration of NO in serum was moderately changed by pentoxifylline treatment (Fig. 6G). In contrast, aminoguanidine treatment significantly decreased the concentration of NO in the serum (Fig. 6H), but the concentration of TNF-α (Fig. 6E) and other cytokines (supplementary Fig. 2A,B) in the serum remained unaltered. The combination of pentoxifylline and aminoguanidine significantly decreased the concentration of TNF-α (Fig. 6F), NO (Fig. 6I) and other pro-inflammatory cytokines in the serum (supplementary Fig. 3A,B). Furthermore, we observed no significant difference in the body temperature between the Ptpn6 H-KO and the Ptpn6 f/f mice that were treated with aminoguanidine, pentoxifylline or their combination (supplementary Fig. 4A–C)
Figure 6.
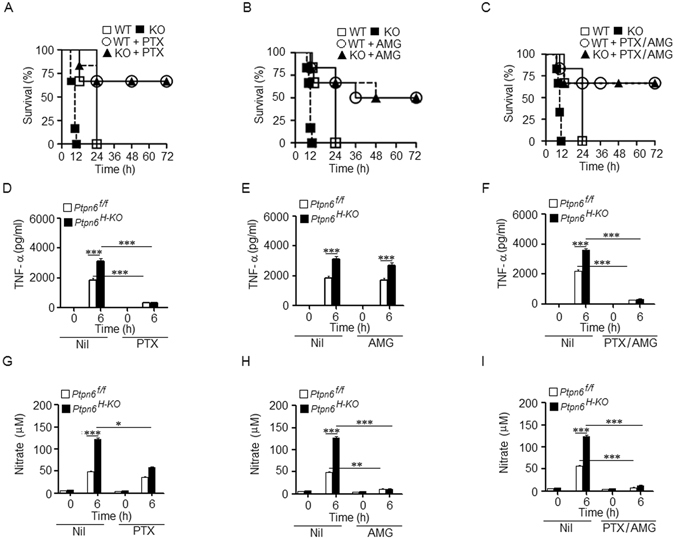
TNF-α and/or iNOS/NO inhibitors rescued Ptpn6 H-KO challenged with LPS. Survival curve of Ptpn6 H-KO and Ptpn6 f/f mice treated with (A) pentoxifylline, (B) aminoguanidine or (C) their combination after LPS challenge (30 mg/kg body weight). Kaplan-Meier analysis demonstrates a significant difference in the survival of both Ptpn6 H-KO and Ptpn6 f/f mice treated with pentoxifylline, aminoguanidine or their combination compared to no treatment. Serum levels of TNF-α in Ptpn6 H-KO and Ptpn6 f/f mice treated with (D) pentoxifylline, (E) aminoguanidine or (F) their combination after LPS challenge (30 mg/kg body weight). Serum levels of NO in Ptpn6 H-KO and Ptpn6 f/f mice treated with (G) pentoxifylline, (H) aminoguanidine or (I) their combination after LPS challenge (30 mg/kg body weight). Data are presented as mean ± SEM, n = 6. *P ≤ 0.05, **P ≤ 0.01 and ***P ≤ 0.001.
Therefore, these findings demonstrate that the inhibition of TNF-α or NO release by their inhibitors can abrogate the increased sensitivity of the Ptpn6 H-KO mice to LPS-induced endotoxemia.
Discussion
The pathophysiology of sepsis involves dysregulation of the inflammatory response, leading to an imbalance between pro- and anti-inflammatory mediators30. The liver is an immunocompetent organ that plays a key role in regulating sepsis-induced pathology31. SHP-1 deficiency is associated with several types of chronic inflammatory disorders and malignancies20–22, which has raised substantial interest in this phosphatase. SHP-1 signalling within hepatocytes controls a variety of physiological and pathological processes23, 24; however, the significance of hepatocyte-specific SHP-1 has not yet been elucidated under LPS-induced, systemic inflammatory conditions.
Herein we report the first demonstration that hepatocyte SHP-1 deficiency leads to exacerbated levels of circulating inflammation-related biomarkers, pro-inflammatory cytokines and mortality upon LPS challenge, revealing the cardinal role played by hepatic SHP-1 in the regulation of inflammatory response during systemic inflammation. More precisely, we found that SHP-1 in hepatocytes plays a critical role in the negative regulation of MAPK signalling -known to be involved in pro-inflammatory cytokines production by these cells- as revealed by the rapid and prolonged activation of MAPK upon LPS bacterial endotoxin challenge in vivo. In parallel, the increased circulating LPS-induced pro-inflammatory cytokines measured in Ptpn6 H-KO mice versus Ptpn6 f/f mice further reinforced the cardinal role of SHP-1 as regulator of hepatocyte in septic inflammation.
Importantly, it is known that during LPS- induced endotoxemia, animal death is accompanied by major dysfunctions of vital organs that can be monitored by measuring levels of circulating ALT, AST, BUN and glucose32 of utmost interest, the extreme sensitivity of Ptpn6 H-KO mice to LPS-mediated endotoxemia and death was also reflected by rapid and intense collapse of organs’ function as exacerbated levels of these pathological markers were detected. This strongly suggests that hepatocyte SHP-1 acts as a vital suppressor of inflammatory responses, thereby protecting the host from shock, multiple organ failure, and mortality after exposure to LPS.
However, the mechanism whereby hepatocyte controls LPS-induced hyper-inflammation and multiple organ failure in the host is still only partially elucidated. Our findings have established that the MAPK signalling pathways regulating pro-inflammatory cytokines and NO synthesis in hepatocytes during LPS challenge is not properly controlled in the absence of SHP-1, therefore resulting in the overproduction of pro-inflammatory mediators. A previous report suggested that MAPK, mainly JNK1/2 and p38, control TNF-α biosynthesis by stabilizing TNF-α mRNA and by augmenting its translation33. Thus, the sustained activation of JNK1/2 and p38 in the liver of the Ptpn6 H-KO mice after LPS challenge could explain the prolonged TNF-α biosynthesis in the Ptpn6 H-KO mice. A likely explanation for the shock and multiple organ failure might be that the increased amount of TNF-α triggers a considerable elevation in NO synthase activity, leading to multiple organ failure. Of interest, previous studies using MAPK phosphatase (DUSP1 and MKP-1) KO mice10, 11 reported that their sensitivity and death were also augmented, further supporting our observations. But of utmost importance, and a key difference from those previous studies that used systemic KO mice, our hepatocyte specific SHP-1 KO mice revealed the extent to which liver hepatocytes are critical in the regulation of septic inflammation. Additionally, by focusing our study on hepatocytes, we also revealed that SHP-1 is an important regulator of various acute phase proteins known to be important biomarkers during inflammation26–28.
Liver is the first organ being encountered by the blood draining the peritoneum and endotoxin induced peritonitis -known to be a common cause of sepsis34. In this regard, we showed that in absence of hepatocyte SHP-1, LPS-mediated inflammatory cells recruitment in the peritoneal cavity was also exacerbated, in particular for neutrophils. These data further revealed that abnormal recruitment of inflammatory cells in peritoneal environment during endotoxemia could be an important step leading to augmented amount of pro-inflammatory cytokines detected in animals. Whereas previous studies have suggested that the response of hepatocytes to LPS is complex, requiring cell-cell interaction between hepatocytes and other cells present in the liver, such as Kupffer cells and sinusoidal endothelial cells35. However, our data indicate, suggested by others36, that LPS can directly stimulate hepatocytes to release various inflammatory related mediators. In fact, using an in vitro approach, we observed that primary hepatocytes isolated from Ptpn6 H-KO and Ptpn6 f/f mice and subjected to LPS stimulation in culture showed marked modulation of MAPKs and secretion of major pro-inflammatory cytokines. These findings establish a cell-autonomous role for hepatocytes and that other cells are not essential to endotoxin stimulation in the context of our studies. Importantly, here again, the greater sensitivity of Ptpn6 H-KO mice hepatocytes toward LPS was reflected by rapid and sustained phosphorylation of the three major MAPK subfamilies (ERK1/2, JNK1/2, and p38) and the greater production of pro-inflammatory cytokines comparatively to the Ptpn6 f/f mice. Notably, the finding of increased cytokine expression in relation to SHP-1 deficiency in vitro was in accordance with our in vivo studies where serum levels of TNF-α, IL-1β, and IL-6 were increased in the Ptpn6 H-KO mice compared to the Ptpn6 f/f mice during endotoxemia. Furthermore, the in vitro demonstration that there was no significant difference in MAPK activation or in the generation of inflammatory mediators by peritoneal macrophages isolated from both Ptpn6 H-KO and Ptpn6 f/f mice in response to LPS clearly demonstrate that hepatocyte SHP-1 is a key negative regulator of liver MAPK activation and consequent functional activation such as attenuation of various inflammatory mediators in response to bacterial endotoxin.
TNF-α is known to be a major proinflammatory mediator of endotoxemia37 enhancing the pathophysiological response of sepsis by inducing the release of active substances, such as other proinflammatory cytokines and NO38. As mentioned earlier, we have observed a strong correlation between exacerbated TNF-α/NO production and rapid death of Ptpn6 H-KO mice over more resistant Ptpn6 f/f mice. Using pentoxifylline -a TNF-α inhibitor- and aminoguanidine -a NO inhibitor- alone or in combination, we tested the importance of these latters and their correlation with the rapid death of our Ptpn6 H-KO mice. We found that pentoxifylline afforded equal significant protection against LPS-induced shock in both Ptpn6 H-KO and Ptpn6 f/f mice, and that the TNFα antagonizing effect of pentoxifylline was also associated with the reduction of other injurious circulating pro-inflammatory cytokines, namely IL-6 and IL-1β. Additionally, aminoguanidine treatment was found to protect against endotoxemia by attenuating NO production in both Ptpn6 H-KO and Ptpn6 f/f mice. The combination of both inhibiting molecules, while exerting protection against LPS-induced endotoxemia, did not show any synergism, indicating that the pathophysiology of sepsis in the Ptpn6 H-KO mice was not strictly dependent on TNF-α or NO.
In conclusion, this study provided strong in vivo and cellular evidences that hepatocyte SHP-1 plays a cardinal role in the production of inflammatory mediators that contribute to endotoxemia. Our data further suggest that the development of anti- endotoxemia therapy concurring to induce SHP-1 activity could represent a new avenue to consider, as actual therapies mainly focusing at specifically blocking TNF-α and other pro-inflammatory cytokines showed limited successes.
Materials and Methods
Animals and Genotyping
Mice C57BL/6J background (6–8 weeks old) was housed under controlled temperature (23 °C) and a 12-hour light/dark cycle with water and food in pathogen-free condition. All research involving mice was carried out according to the regulations of the Canadian Council of Animal Care and was approved by the McGill University Animal Care Committee under ethics protocol number 5925. Mice were euthanized at established humane endpoints using CO2 asphyxiation followed by cervical dislocation or by using isoflurane if perfusion was performed.
Hepatocyte-specific SHP-1 knockout mice (Ptpn6 H-KO) were generated on a pure C57/BL6 background by crossing mice homozygous for floxed SHP-1 (Ptpn6 f/f)39 with Alb-Cre mice (B6.Cg-Tg[Alb-cre]21Mgn/J, stock 3574; (The Jackson Laboratory). Genomic DNA was extracted from ear samples using the DNA RED Extract-N-Amp PCR kit (Sigma), and genotyping was performed as described elsewhere23, 24.
LPS injection and endotoxemia
Ptpn6 f/f and Ptpn6 H-KO mice were injected intraperitoneally (i.p.) with pyrogen-free PBS or the LPS derived from Escherichia coli Serotype 055:B5 (Sigma, St. Louis) dissolved in pyrogen-free PBS (5, 10 and 30 mg/kg body weight). In a separate experiment, an inhibitor of TNF-α, Pentoxifylline was given (i.p.) at a dose of 150 mg/kg 1 hour before LPS challenge40. In another experiment, mice were treated twice a day with the iNOS inhibitor amino guanidine hemisulfate salt (Sigma) 8 mg dissolved in 100 µl PBS as described41. Survival of the mice was monitored every 3 h for 72 h. Body temperature of the mice was measured at indicated time points using a thermometer. For serum cytokine and nitric oxide assay, sera were collected at 0, 1, 3 and 6 h after the LPS injection.
Blood Biochemistry in LPS treated mice
After the intraperitoneal injection of LPS (30 mg/kg body weight), blood samples were obtained from the tail vein at 0, 1, 3 and 6 hours post-inoculation to measure different parameter (blood glucose, blood alanine aminotransferase (ALT), blood aspartate transaminase (AST) and blood urea nitrogen (BUN). Levels of serum glucose, ALT, AST and BUN were measured with a VITROS 250/350/950/5,1 FS and 4600 Chemistry Systems and the VITROS 5600 Integrated System made by Ortho Clinical Diagnostics.
Isolation and Culture of Mouse Primary Hepatocytes
Livers were perfused in anesthetized mice and primary Hepatocytes were isolated from Ptpn6 f/f and Ptpn6 H-KO mice as previously described42.
Preparation of Mouse Peritoneal Macrophage
To isolate peritoneal macrophages, peritoneal exudates cells were isolated from the peritoneal cavity with cold PBS and used the adherent cells as peritoneal macrophages43 for further experiments.
Measurement of Nitric oxide and Cytokines
Hepatocytes and Peritoneal macrophages isolated from Ptpn6 H-KO and Ptpn6 f/f mice were stimulated with LPS (1 µg/ml) for different time points (1, 3, 6, 12, and 24 h). Pro-inflammatory cytokines in the culture supernatants and serum were measured by ELISA. TNF-α, IL-1β and IL-6 were measured by ELISA according to the manufacturer’s instructions (SET TO GO kit, eBiosciences, San Diego, CA, USA). Concentration of NO was measured using Griess reagents as previously described44.
Peritoneal lavage
Mice receiving LPS (10 mg/kg body weight) or PBS by i.p. injection were euthanized after 6 h, and total cell counts were made for lavage fluid using a haemocytometer. Cell suspension applied onto a microscope glass-slide using a Cytospin apparatus. The slide was then stained using the Diff-Quik stain (Siemens Healthcare, Newark, DE, USA) and blind differential counting was performed on these slides by microscopy.
Western blotting
Western blotting was performed as previously described44. List of antibodies used: Actin (Sigma, A5316); Anti-phospho-JNK1/2 (Cell signalling, Ipswich, MA, USA), Anti-phospho-ERK1/2 (Cell signalling, Ipswich, MA, USA), Anti- phosphop-38 (Cell signalling, Ipswich, MA, USA) and total p38 MAPK (Cell signaling, Ipswich, MA, USA), JNK1/2 (Cell signaling, Ipswich, MA, USA) and ERK1/2. Anti-SAA (Santa Cruz Biotechnology, CA), Anti-Apo E (Millipore), Albumin (Santa Cruz Biotechnology, CA), and Anti- LBP (Santa Cruz, CA).
Statistical Analysis
Statistical analyses were performed using the unpaired Student’s t-test. Error bars represent ± S.E.M. Kaplan-Meier curves were used to show survival over time. The data were analyzed using Graph Pad Prism software (version 5.0). *P < 0.05, **P < 0.01 and ***P < 0.001.
Electronic supplementary material
Acknowledgements
This work was supported by grants from the Canadian Institutes in Health Research (CIHR) to M.O. M.O. is member and co-director of the FQRNT Host-Parasite Interaction provincial network. M.O. is a Burroughs Wellcome Fund Awardee in Molecular Parasitology. We cordially thank Dr. Vanessa Diniz Atayde and Kristin M. Van Den Ham for their assistance in editing the manuscript.
Author Contributions
Conceived and designed the experiments: A.A., M.O. Performed the experiments: A.A., M.O., C.M. Analyzed the data: A.A., M.O. Wrote the paper: A.A., M.O., A.M.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-02512-7
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aziz M, Jacob A, Yang WL, Matsuda A, Wang P. Current trends in inflammatory and immunomodulatory mediators in sepsis. J Leukoc Biol. 2013;93(3):329–342. doi: 10.1189/jlb.0912437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levy MM, et al. Surviving Sepsis Campaign. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med. 2010;38(2):367–374. doi: 10.1097/CCM.0b013e3181cb0cdc. [DOI] [PubMed] [Google Scholar]
- 3.Gårdlund B, et al. Plasma levels of cytokines in primary septic shock in humans: correlation with disease severity. J Infect Dis. 1995;172(1):296–301. doi: 10.1093/infdis/172.1.296. [DOI] [PubMed] [Google Scholar]
- 4.Pinsky MR, et al. Serum cytokine levels in human septic shock. Relation to multiple-system organ failure and mortality. Chest. 1993;103(2):565–575. doi: 10.1378/chest.103.2.565. [DOI] [PubMed] [Google Scholar]
- 5.Waage A, Halstensen A, Espevik T. Association between tumour necrosis factor in serum and fatal outcome in patients with meningococcal disease. Lancet 14. 1987;1(8529):355–357. doi: 10.1016/S0140-6736(87)91728-4. [DOI] [PubMed] [Google Scholar]
- 6.Girardin E, Grau GE, Dayer JM, Roux-Lombard P, Lambert PH. Tumor necrosis factor and interleukin-1 in the serum of children with severe infectious purpura. N Engl J Med. 1988;319(7):397–400. doi: 10.1056/NEJM198808183190703. [DOI] [PubMed] [Google Scholar]
- 7.Damas P, et al. Cytokine serum level during severe sepsis in human IL-6 as a marker of severity. Ann Surg. 1992;215(4):356–362. doi: 10.1097/00000658-199204000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Titheradge MA. Nitric oxide in septic shock. Biochim Biophys Acta. 1999;1411(2-3):437–455. doi: 10.1016/S0005-2728(99)00031-6. [DOI] [PubMed] [Google Scholar]
- 9.Mogensen TH. Pathogen recognition and inflammatory signaling in innate immune defenses. Clin Microbiol Rev. 2009;22(2):240–273. doi: 10.1128/CMR.00046-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hammer M, et al. Dual specificity phosphatase 1 (DUSP1) regulates a subset of LPS-induced genes and protects mice from lethal endotoxin shock. J Exp Med. 2006;203(1):15–20. doi: 10.1084/jem.20051753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao Q, et al. MAP kinase phosphatase 1 controls innate immune responses and suppresses endotoxic shock. J Exp Med. 2006;203(1):131–140. doi: 10.1084/jem.20051794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nussler AK, et al. Stimulation of the nitric oxide synthase pathway in human hepatocytes by cytokines and endotoxin. J Exp Med. 1992;176(1):261–264. doi: 10.1084/jem.176.1.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruminy P, et al. Gene transcription in hepatocytes during the acute phase of a systemic inflammation:from transcription factors to target genes. Inflamm Res. 2001;50(8):383–390. doi: 10.1007/PL00000260. [DOI] [PubMed] [Google Scholar]
- 14.Rao SS, Rattanakovit K, Patcharatrakul T. Diagnosis and management of chronic constipation in adults. Nat Rev Gastroenterol Hepatol. 2016;13(5):295–305. doi: 10.1038/nrgastro.2016.53. [DOI] [PubMed] [Google Scholar]
- 15.Sakamori R, et al. Signal transducer and activator of transcription 3 signaling within hepatocytes attenuates systemic inflammatory response and lethality in septic mice. Hepatology. 2007;46(5):1564–1573. doi: 10.1002/hep.21837. [DOI] [PubMed] [Google Scholar]
- 16.Dubois MJ, et al. The SHP-1 protein tyrosine phosphatase negatively modulates glucose homeostasis. Nat Med. 2006;12(5):549–556. doi: 10.1038/nm1397. [DOI] [PubMed] [Google Scholar]
- 17.Qian H, et al. An HNF1α-regulated feedback circuit modulates hepatic fibrogenesis via the crosstalk between hepatocytes and hepatic stellate cells. Cell Res. 2015;25(8):930–945. doi: 10.1038/cr.2015.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kanwal Z, et al. Deficiency in hematopoietic phosphatase ptpn6/Shp1 hyperactivates the innate immune system and impairs control of bacterial infections in zebrafish embryos. J Immunol. 2013;190(4):1631–1645. doi: 10.4049/jimmunol.1200551. [DOI] [PubMed] [Google Scholar]
- 19.Xiao W, et al. Phospholipase C-β3 regulates FcɛRI-mediated mast cell activation by recruiting the protein phosphatase SHP-1. Immunity. 2011;34(6):893–904. doi: 10.1016/j.immuni.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eriksen KW, et al. Deficient SOCS3 and SHP-1 expression in psoriatic T cells. J Invest Dermatol. 2010;130(6):1590–1597. doi: 10.1038/jid.2010.6. [DOI] [PubMed] [Google Scholar]
- 21.Christophi GP, et al. SHP-1 deficiency and increased inflammatory gene expression in PBMCs of multiple sclerosis patients. Lab Invest. 2008;88(3):243–255. doi: 10.1038/labinvest.3700720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhu Z, et al. Tyrosine phosphatase SHP-1 in allergic and anaphylactic inflammation. Immunol Res. 2010;47(1–3):3–13. doi: 10.1007/s12026-009-8134-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu E, et al. Hepatocyte-specific Ptpn6 deletion protects from obesity-linked hepatic insulin resistance. Diabetes. 2012;61(8):1949–1958. doi: 10.2337/db11-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu E, et al. Hepatocyte-specific Ptpn6 deletion promotes hepatic lipid accretion, but reduces NAFLD in diet-induced obesity: potential role of PPARγ. Hepatology. 2014;59(5):1803–1815. doi: 10.1002/hep.26957. [DOI] [PubMed] [Google Scholar]
- 25.Robinson MW, Harmon C, O’Farrelly C. Liver immunology and its role in inflammation and homeostasis. Cell Mol Immunol. 2016;13(3):267–276. doi: 10.1038/cmi.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Minter RM, et al. LPS-binding protein mediates LPS-induced liver injury and mortality in the setting of biliary obstruction. Am J Physiol Gastrointest Liver Physiol. 2009;296(1):45–54. doi: 10.1152/ajpgi.00041.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vels L, Røntved CM, Bjerring M, Ingvartsen KL. Cytokine and acute phase protein gene expression in repeated liver biopsies of dairy cows with a lipopolysaccharide-induced mastitis. J Dairy Sci. 2009;92(3):922–934. doi: 10.3168/jds.2008-1209. [DOI] [PubMed] [Google Scholar]
- 28.Chuang K, Elford EL, Tseng J, Leung B, Harris HW. An expanding role for apolipoprotein E in sepsis and inflammation. Am J Surg. 2010;200(3):391–397. doi: 10.1016/j.amjsurg.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miyazaki S, Ishikawa F, Fujikawa T, Nagata S, Yamaguchi K. Intraperitoneal injection of lipopolysaccharide induces dynamic migration of Gr-1high polymorphonuclear neutrophils in the murine abdominal cavity. Clin Diagn Lab Immunol. 2004;11(3):452–457. doi: 10.1128/CDLI.11.3.452-457.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walley KR, Lukacs NW, Standiford TJ, Strieter RM, Kunkel SL. Balance of inflammatory cytokines related to severity and mortality of murine sepsis. Infect Immun. 1996;64(11):4733–4738. doi: 10.1128/iai.64.11.4733-4738.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nesseler N, et al. Clinical review: The liver in sepsis. Crit Care. 2012;16(5):235. doi: 10.1186/cc11381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.He L, et al. Protective effects of the SEPS1 gene on lipopolysaccharide-induced sepsis. Mol Med Rep. 2014;9(5):1869–1876. doi: 10.3892/mmr.2014.1991. [DOI] [PubMed] [Google Scholar]
- 33.Kontoyiannis D, Pasparakis M, Pizarro TT, Cominelli F, Kollias G. Impaired on/off regulation of TNF biosynthesis in mice lacking TNF AU-rich elements: implications for joint and gut-associated immunopathologies. Immunity. 1999;10(3):387–398. doi: 10.1016/S1074-7613(00)80038-2. [DOI] [PubMed] [Google Scholar]
- 34.Steinmüller M, et al. Endotoxin induced peritonitis elicits monocyte immigration into the lung: implications on alveolar space inflammatory responsiveness. Respir Res. 2006;7:30. doi: 10.1186/1465-9921-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scott MJ, Liu S, Su GL, Vodovotz Y, Billiar TR. Hepatocytes enhance effects of lipopolysaccharide on liver nonparenchymal cells through close cell interactions. Shock. 2005;23(5):453–458. doi: 10.1097/01.shk.0000160939.08385.f1. [DOI] [PubMed] [Google Scholar]
- 36.Liu S, et al. Role of toll-like receptors in changes in gene expression and NF-kappa B activation in mouse hepatocytes stimulated with lipopolysaccharide. Infect Immun. 2002;70(7):3433–3442. doi: 10.1128/IAI.70.7.3433-3442.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Spooner CE, Markowitz NP, Saravolatz LD. The role of tumor necrosis factor in sepsis. Clin Immunol Immunopathol. 1992;62(1 Pt 2):S11–7. doi: 10.1016/0090-1229(92)90036-N. [DOI] [PubMed] [Google Scholar]
- 38.Svenungsson E, et al. Increased levels of proinflammatory cytokines and nitric oxide metabolites in neuropsychiatric lupus erythematosus. Ann Rheum Dis. 2001;60(4):372–379. doi: 10.1136/ard.60.4.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pao LI, et al. B cell-specific deletion of protein-tyrosine phosphatase Shp1 promotes B-1a cell development and causes systemic autoimmunity. Immunity. 2007;27(1):35–48. doi: 10.1016/j.immuni.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 40.Wang W, et al. Pentoxifylline protects against endotoxin-induced acute renal failure in mice. Am J Physiol Renal Physiol. 2006;291(5):1090–1095. doi: 10.1152/ajprenal.00517.2005. [DOI] [PubMed] [Google Scholar]
- 41.Matte C, et al. Peroxovanadium-mediated protection against murine leishmaniasis: role of the modulation of nitric oxide. Eur J Immunol. 2000;30(9):2555–2564. doi: 10.1002/1521-4141(200009)30:9<2555::AID-IMMU2555>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 42.Qiu W, et al. Hepatic PTP-1B expression regulates the assembly and secretion of apolipoprotein B-containing lipoproteins: evidence from protein tyrosine phosphatase-1B overexpression, knockout, and RNAi studies. Diabetes. 2004;53(12):3057–3066. doi: 10.2337/diabetes.53.12.3057. [DOI] [PubMed] [Google Scholar]
- 43.Zhang, X., Goncalves, R. & Mosser, D. M. The isolation and characterization of murine macrophages. Curr Protoc Immunol Chapter 14, Unit 14, 1 (2008). [DOI] [PMC free article] [PubMed]
- 44.Olivier M, et al. Modulation of interferon-gamma-induced macrophage activation by phosphotyrosine phosphatases inhibition. Effect on murine Leishmaniasis progression. J Biol Chem. 1998;273(22):13944–13949. doi: 10.1074/jbc.273.22.13944. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


