Abstract
Acne vulgaris is one of the top three most commonly encountered dermatological problems worldwide in both primary and secondary care. Acne diagnosis and treatment date back to ancient Greek and Egyptian times. This article explores acne through the ages and discusses past theories on etiology and treatment with particular focus on the discovery of retinoids and their impact on women’s health.
Keywords: Acne, Treatment, History, Retinoid, Pregnancy
Introduction
Acne vulgaris is a disorder of the pilosebaceous unit that is characterized by comedones, papules, cysts, nodules, and scarring. It is one of the top three most commonly encountered dermatological problems in both primary and secondary care (Rea et al., 1976). While the condition is not life threatening, it can cause significant psychological morbidity and lead to lifelong scarring and some cases of facial disfigurement if left untreated. Acne vulgaris typically starts around the age of 12 to 14 years but tends to manifest earlier in female patients. Patients’ peak age for severity is 16 to 17 years in female and 17 to 19 years in male patients.
There is much debate over the gender distribution of acne vulgaris. Simpson (1991) states that 95% of boys and 83% of girls are affected during their adolescent and young adult life. Hunter et al. (2002) concluded that acne has no gender predilection and affects both sexes equally.
This article examines acne through the ages and discusses the myths and theories that surround its etiology as well as developments in acne treatments with a focus on isotretinoin and its impact on women’s health (Fig. 1).
Fig. 1.
Woman with acne on her face
Source: Burgess TH. Eruptions of the face, head, and hands: with the latest improvements in the treatment of diseases of the skin [Internet]. 1849 [cited 2015 October 6]. Available from: https://commons.wikimedia.org/wiki/File:Illustration_of_a_woman_with_acne_on_her_face_Wellcome_L0037455.jpg
Acne through the ages
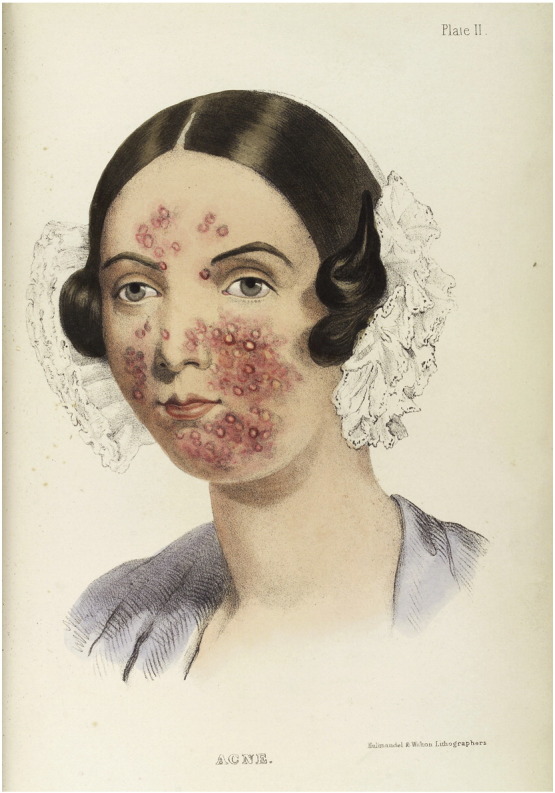
Greek physicians Aristotle and Hippocrates used the Greek words ionthoi and varus to describe acne as a condition that is strongly associated with puberty (Grant, 1951). In fact, the singular form of ionthoi translates to the onset of beard growth. In the Ebers Papyrus (Fig. 2), ancient Egyptians used the term aku-t, which means boils, blains, sore, pustules, or any inflamed swelling (Grant, 1951). Given its phonetic resemblance to the term we use today, this likely represents the root word of acne. The term acne vulgaris (vulgaris means common) was first used by Fuchs in 1840 and has persisted to the present day (Grant, 1951).
Fig. 2.
Excerpt from the Ebers Papyrus wherein one passage mentions a prescription dating from the first dynasty (circa 3400 BC). The papyrus was discovered at Thebes in 1862.
Source: Wellcome collection [Internet]. 2015 [cited 2015 October 6]. Available from: https://commons.wikimedia.org/wiki/File:A_page_from_the_Ebers_Papyrus,_written_circa_1500_B.C._Wellcome_M0008455.jpg?uselang=en-gb
Skin disease was historically seen as a manifestation of internal problems and thought to represent the need to balance the four humors defined in ancient Greek medicine. Humors existed as liquids within the body and were identified as blood, phlegm, black bile, and yellow bile. Pores in the skin were regarded as orifices through which humors could pass. In the 16th Century, Sir Thomas Elyot (Fig. 3) in his “Castell of Health” described a condition due to an abundance of melancholy blood. Elyot may have seen acne as part of a wider endocrinological syndrome because he describes obesity of the upper body that is associated with boils, increased urine, and black pouches (Grant, 1951). In 1638, Riolanus associated acne with menstruation-related disorders (Grant, 1951). Ten years later, Johnston linked acne with a pattern of heterosexual behavior. His words, translated by Culpepper, state “vari are little hard tumours on the skin of the face curdled up of a hard thick juice. They are known easily. They are of the bigness of hemp seed, and they infect young people that are inclined to venery and fruitful, but chast withal and continent” (Grant, 1951; Fig. 4).
Fig. 3.

Portrait of Sir Thomas Elyot (1532-1533) by Hans Holbein the Younger
Source: Royal Collection at Windsor Castle [Internet]. 2015 [cited 2015 October 6]. Available from: https://commons.wikimedia.org/wiki/File:Holbein_Sir_Thomas_Elyot.jpg?uselang=en-gb
Fig. 4.
Hemp seeds (left rule divisions in mm)
Source: Photo by Erik Fenderson [Internet]. 2015 [cited 2015 October 6]. Available from: https://commons.wikimedia.org/wiki/File:Hempseed.jpg?uselang=en-gb
It was not until the invention of microscopes that skin glands were identified and allowed for advancements in dermatology. Italian researcher Marcello Malphigi discussed pores as the opening of glands in the skin in his book Opera Postuma (Zouboulis et al., 2014). Hermann Boerhaave, a Dutch Professor of Medicine and Botanics, also supported this view (Zouboulis et al., 2014). The term sebaceous gland was coined by Giovanni Battista Morgagni (Fig. 5) who described them in his book De Sedibus et cause morborum per anatomen indagatis (Zouboulis et al., 2014).
Fig. 5.
Engraving of Giambattista Morgagni (1682-1771) by G. Simoncelli
Source: Burgess R. Portraits of doctors and scientists in the Wellcome Institute. [Internet]. 1973 [cited 2015 October 6]. Available from: https://commons.wikimedia.org/wiki/File:Giovanni_Battista_Morgagni_(1682_-_1771),_Italian_anatomist_Wellcome_V0004121.jpg?uselang=en-gb
German physician Karl Gustav Theodor Simon was a hobbyist microscopist based in Berlin who, in 1842, saw a living, moving creature when examining tissue that was affected with acne. He remarked that “postulation became certainty when I pressed the object under observation very gently between two glass plates and saw very clearly that it moved” (Plewig and Kligman, 2012). This was the first described observation of the Demodex mite. As the Chief of Dermatology at the Charite Hospital in Berlin, Dr. Simon published his observations in 1848 in his work Die Hautkrankheiten durch Anatomische Untersuchungen Erlautert (Skin conditions explained through anatomical investigation; Plewig and Kligman, 2012).
English dermatologist Samuel Plumbe published A practical treatise on the diseases of the skin in 1837 (Fig. 6). He described blockage of the sebaceous glands as follows: “it has been constantly observed, that persons of sanguine temperament and florid complexion have been most subject to follicular inflammation; and among these, that young men between the ages of 20 and 25 have been the greatest sufferers from it. Females, at the same age, are also subjects in whom its visitations are not infrequently manifested, but, in the latter, it rarely proceeds with such rapidity to suppuration, or produces such unpleasant appearances as to extent” (Plumbe, 1937).
Fig. 6.
Excerpt from A practical treatise on the diseases of the skin (electronic resource)- arranged with a view to their constitutional causes and local characters (1838) demonstrating the skin “papillae” of the heel
Source: Samuel Plumbe, engraver E.W. Mumford [Internet]. 1838 [cited 2015 October 6]. Available from: https://commons.wikimedia.org/wiki/File:A_practical_treatise_on_the_diseases_of_the_skin_(electronic_resource)-_arranged_with_a_view_to_their_constitutional_causes_and_local_characters_(1838)_(14783479905).jpg?uselang=en-gb
In the 19th Century, Robert Willan (Fig. 7) and Thomas Bateman, who are regarded by some as the fathers of modern dermatology, divided acne into four types based on the associated lesions: simplex, punctate, indurate, and rosacea (McCaw, 1944). The first three types were identified as local lesions that require local remedies; however, rosacea was deemed a cutaneous manifestation of underlying stomach or liver problems.
Fig. 7.

Robert Willan, English physician and possible founder of dermatology
Source: Wikepedia [Internet]. 2016 [cited 2016 August 16]. Available from: https://en.wikipedia.org/wiki/Robert_Willan
In 1903, the etiology of acne remained uncertain. Eduard Von Jacobi (1903) wrote in Atlas der Hautkrankheiten that “many morbid processes conspire to favour the existence of the disease,” “a peculiar seborrhoeic condition is frequently present, which gives rise to the formation of comedones.” He continued that “specific significance attributed to various bacteria found in the pus of acne pustules is contestable.”
Over the centuries, our understanding of the multifactorial pathophysiology of acne vulgaris has improved. There is a genetic component with acne vulgaris that is thought to be familial in half of the cases. Studies of monozygotic twins, for example, show a high concordance of the sebum excretion rate in acne; however, dizygotic twins do not show the same concordance. In the past, acne vulgaris was regarded as an infectious disease but today, it is recognized as an inflammatory process in which Propionibacterium acnes and innate immunity trigger a cascade of events at the level of the pilosebaceous unit that break down triglycerides to release free fatty acids, produce substances that are chemotactic for inflammatory cells, and induce the ductal epithelium to secrete pro-inflammatory cytokines (interleukin [IL]-1, IL-6, IL-8, IL-10, IL-12 and tumor necrosis factor alpha [TNFα]). The inflammatory reaction continues by means of a type IV immune reaction to one or more antigens in the follicle. It was previously thought that abnormal keratinization occurred first but current understanding is that inflammation, namely the expression of IL-α from the open comedones, precedes abnormal hyperkeratinization (Das and Reynolds, 2014).
A keratin plug forms at the follicular infundibulum from follicular epithelial hyperproliferation and retention of keratinocytes. A complex interplay that involves increased sensitivity to androgens and increased androgen levels, sebum lipid composition, P. acnes overgrowth, and local pro-inflammatory cytokines drive epithelial hyperproliferation. The biofilm that is produced by P. acnes perpetuates comedone formation and the hyperkeratinization process by propagating the infundibular plug (Das and Reynolds, 2014).
Acne treatments through time
While Greeks preferred vegetable-based treatments for acne, Egyptians typically opted for animal-based products (Zouboulis et al., 2014). The one common treatment they used was honey; however, given its popularity with both civilizations to treat a wide range of ailments, this may be a mere coincidence. Throughout the Middle Ages, the four humors that underpinned medical treatment and research was stifled by religious control. Treatment development stagnated and was based on balancing humors, diets, herbal remedies, and prayers.
Botanical and herbal treatments were still used in 1936 as seen in Cosmetic Dermatology, a good guide on historical treatments (Goodman, 1936). Goodman first stated the importance of a good history that includes information about diet, cathartics, periods, urine, blood sugar, ingestion of bromide or iodine drugs, blood purifiers, headache medicine, nerve tonics, and sleep potions. Topical treatments were classified into keratolytic, antiseptic, astringent, emollient, and keratoplastic therapies. Some examples of keratolytic therapies that were championed by Goodman are outlined in Box 1.
Box 1. Keratolytic Therapy.
-
•
Vleminckx solution (16 parts lime, 24 parts sublimed sulfur, and 100 parts water)
-
•
Lotio alba nascent gas (50 parts zinc sulfate and 50 parts potassium sulfate)
-
•
Injections of salt solution
-
•
Kummerfield’s lotion (1 part camphor, 2 parts acacia, 4 parts glycerin, 10 parts precipitated sulfur, and 100 parts of rose water)
-
•
ergot ointment (0.8 part phenol, 8 parts ergot, 8 parts chalk, 8 parts zinc oxide, 24 parts cold cream, and 100 parts lanolin).
Alt-text: Box 1.
Goodman also discussed peels and recommended an initial application for 1 to 3 hours and, if the patient had no adverse reaction, to extended the peel for a full treatment lasting 12 hours. The peels he described contained (a) 40 parts resoricin, 10 parts zinc oxide, 6 parts kaolin, 100 parts benzoinate lard, and (b) 32 parts resoricin, 20 parts potash soap, 20 parts sulfur lotum, and 100 parts spirits of lavender. Antiseptic therapy as recommended by Goodman were iodine, picric acid, sodium carbonate, camphor, alcohol, and boric or oleic acids. Of note, he wrote “do large pores ever disappear? The answer is ‘yes’. Many matrons who grieved in their youth over the structural defects of the skin leading to enlarged pores are the envy of their daughters who are now passing through the same cycle” (Goodman, 1936). Goodman recommended the following astringents to shrink pores: alcohol, tannins (in almond, cinnamon, rose, lavender, or lemon oils), alum, bismuth, acetic/boric/citric/lactic acid, balsam of Peru, active beta-naphthol, resoricin, sulfur, lecithin, and metal salts (Goodman, 1936).
Canadian dermatologist William E. Pace was the first to recognize the usefulness of benzoyl peroxide to treat acne when he identified it as the active ingredient of Squibb’s antiseptic Quinolor compound ointment (Pace, 1965).
Throughout history, much focus has been placed on dietary avoidance as a treatment of acne. MacKee and his team advised in 1922 that “avoiding candy, pastry, soda water, ice cream, chocolate, rich foods, fried foods, cocoa and gravy as a bare minimum plus or minus tea, coffee, alcohol and spices” (Smith and Mann, 2011). In addition, Goodman (1936) advised to avoid starchy foods, bread rolls, noodles, spaghetti, potatoes, oily nuts, chop suey, chow mein, and waffles. Goodman praised the following foods as suitable to cure acne: cooked and raw fruit, farina, rice, wheat, oatmeal, green vegetables, boiled or broiled meat and poultry, clear soup, vegetable soup, and an abundance of water. Conversely, Fulton et al. (1969) showed that excessive intake of chocolate had no bearing on the composition or output of sebum production. MacKee also stressed the importance of a daily bowel movement in the prevention of acne by stating that “if there is indigestion or intestinal troubles the alimentary canal must be attacked” (Smith and Mann, 2011). Avoidance of excess sexual activity was also cited as a potential therapy in treating acne and “masturbation and sexual excess must be avoided” (Smith and Mann, 2011). Furthermore, the “menstrual functions and genito-urinary tract should receive attention” when treating for acne (Smith and Mann, 2011).
From 1895, when Wilhelm Roentgen discovered the use of X-rays in medicine, the spectra were used to treat a variety of conditions including acne (Cleveland and Pirie, 1938). In 1902, American researcher W.A. Pusay first published on the use of X-rays as a novel therapeutic agent in the treatment of acne (Pusay, 1902). In the 1930s, researchers calibrated X-ray equipment to allow it to be widely used in the 1940s. MacKee and Cipollaro (1946) described X-rays as the most useful and important single agent in the armamentarium of dermatology. MacKee and his research team believed that if relapses occurred post–X-ray treatment, an internal factor was to blame citing “masturbation, intestinal auto-intoxication, faulty diet” as potential precipitants (Smith and Mann, 2011). However, public perception toward the use of X-rays in medicine changed in the 1960s as the effects of the bombing of Hiroshima, Japan created wide mistrust of radiation. Karagas et al. (1996) researched non-melanoma skin cancers that occurred in patients who were treated with ionizing radiation for a variety of conditions. Of the 259 patients who received treatment for acne vulgaris, 62 patients (24%) developed basal cell carcinomas compared with 8 of 23 patients (35%) who received radiotherapy for cancer treatment (Karagas et al., 1996).
In the first half of the 20th Century, phototherapy was a popular treatment for acne and quartz mercury vapor lamps in particular were used (Armstrong, 1992). One example of an air-cooled lamp was the Emesay-Hanovia quart mercury vapor lamp.
Isotretinoin and its impact on women’s health
In 1947, Otto Isler with pharmaceutical company Hoffman-La Roche developed a commercial synthetic vitamin A. However, it was not until 1959 that dermatologist Gunter Stüttgen worked with retinols for the treatment of dyskeratosis disorders and discovered that retinol was effective after metabolic activation. Dr. Stüttgen’s work with Hoffman-La Roche on tretinoin showed that it worked in the treatment of certain skin conditions (Stüttgen, 1962).
Albert Montgomery Kligman, Professor of Dermatology at the University of Pennsylvania and a trained botanist, also investigated acne and published the first paper on the use of topical retinoids (Kligman et al., 1969). Treatment with isotretinoin was thought to be more effective and safer than tretinoin and revolutionized the treatment of acne vulgaris as 9 of 10 patients saw a significant improvement in their skin after only a single course (1-2 mg/kg/day) for 16 to 24 weeks (Zouboulis et al., 2014). It should be noted that interest in acne treatment with tretinoin has resurged. Oral isotretinoin is reserved for acne that is more refractory rather than conventional therapies. Tretinoin reduces the size of the pilosebaceous unit and dramatically suppresses sebum production, resulting in altered skin surface lipid composition. This mechanism results in the frequently reported side effects of mucocutaneous dryness, grittiness of the eyes, and epistaxis. Side effects are dose dependent and occur in up to 95% of patients. Diffuse hair loss and myalgia are less commonly reported side effects and resolve on discontinuation of the drug.
In 1953, Sidney Q. Cohlan (1953) observed that high doses of vitamin A had teratogenic effects on pregnant rats. G. L. Peck was initially researching vitamin A for the treatment of Darier’s disease, ichthyosis, and pityriasis rubra pilaris and discovered its therapeutic effects on acne vulgaris. Peck et al. (1979) also counseled on contraception, as isotretinoin is contraindicated during pregnancy even at doses under 0.5 mg/kg for short treatment periods. Women of reproductive age (i.e., 15 to 44 years) account for 90% of isotretinoin prescriptions to female patients (Honein et al., 2001). Isotretinoin fetal exposure results in congenital malformations and on rare occasions in intrauterine death, even with conception up to 5 weeks after taking the drug (Honein et al., 2001). Despite widespread knowledge of the drug’s teratogenicity, more than 80 cases of isotretinoin embryopathy were reported between 1982 and 1990 (Honein et al., 2001). Malformations that were observed include microtia or anotia (i.e., small or absent ears), micrognathia, cleft palate, auditory canal defects, thymic hypoplasia, retina or optic nerve abnormalities, and functional impairment (Lynberg et al., 1990). The U.K. National Tetratology Information Service estimates that with fetal exposure to isotretinoin, 30% of infants with no gross malformations have learning difficulties and up to 60% have impaired neuropsychological function (Sladden and Harman, 2007).
Fetal exposure to isotretinoin continued even after the implementation of a pregnancy prevention program (i.e., signed agreement between clinician and patient) that was introduced in 1988 (Sladden and Harman, 2007). Despite the pregnancy prevention program, 1019 of 177,216 pregnancies were identified with fetal exposure to isotretinoin in The Slone Survey, an independent follow-up survey of women of childbearing age in the United States who were prescribed isotretinoin between 1989 and June 2000 (Lee et al., 2009). Of these pregnancies with fetal exposure to isotretinoin, records show that 117 resulted in live births, 681 in elective terminations, 177 in spontaneous abortions, and 29 in ectopic pregnancies. Records were examined for 63 pregnancies that resulted in live births and 13% showed documented major malformations and 30% some degree of malformation. Ten percent of the live births were recorded as occurring within 30 days after isotretinoin discontinuation (Lee et al., 2009).
In reaction to these numbers, the iPLEDGE program was introduced in the United States in 2007, which required a negative pregnancy test before treatment with isotretinoin, every month during treatment, at the end of treatment, and 1 month after discontinuation of treatment. Similar guidelines and protocols exist in many other countries across the world. One culprit for the continued reporting of isotretinoin pregnancies is the prescription-sharing phenomenon, which has swept the United States over the last decade. Of the 700 patients surveyed by Goldsworthy et al. (2008), 22.9% admitted to loaning medications to others and 6.4% to sharing isotretinoin with people who had not been formally prescribed the treatment by a dermatologist. This prescription-sharing behavior has put females of childbearing age at risk of teratogen exposure without the recommended treatment education and monitoring.
Teratogenic risk is not absolute; however, it is perceived to persist on completion of the course as described in an example by Lee et al. (2009) who reported a case of a 24-year old female patient who conceived 5 weeks after treatment discontinuation. The patient had been taking 10 mg isotretinoin for nearly 2 years to treat severe acne and used an intrauterine contraceptive device while taking the drug. Regular antenatal care that included ultrasound scans at 10 and 20 weeks showed no definite fetal malformations but the baby boy was noted to have a right ear microtic deformity with a visible opening of the ear canal. The area on the left side showed a skin tag-like remnant of the lower part of the ear lobe with no visible opening. Both vestibules were dilated and the ossicle with surrounding hemorrhage was fused. Sladden and Harman (2007) describe the case of a patient who became pregnant while treated with isotretinoin even with appropriate counseling, concomitant oral contraceptive pill therapy, and a negative pregnancy test. She was 6 to 7 weeks pregnant and immediately stopped taking isotretinoin. The patient was counseled on the risks of fetal exposure to isotretinoin but opted to proceed with the pregnancy. Regular ultrasound scans were normal and she delivered a healthy baby girl with no apparent birth defects. At 18 months, the child was reported to be developing normally (Sladden and Harman, 2007).
Birth defects are the leading cause of mortality and morbidity in children. The psychosocial impact on mothers who have a child with birth defects is astounding and studies report that the worse a child’s symptoms are, the more a parent’s psychosocial functioning deteriorates over time (Lemacks et al., 2013). During their pregnancy, expectant mothers become preoccupied with medical visits and fears of caring for a sick child haunt their pregnancy. They may forgo baby showers or other celebrations because they feel undeserving or fearful of postnatal outcomes (Lemacks et al., 2013). Mothers of children with birth defects experience significant depression, marital upset, fear, anxiety, isolation, and feelings of guilt, embarrassment, and shame. If the birth defect requires medical procedures, hospital stays, surgeries, and other interventions, the mother’s quality of life is much more likely to be adversely affected. Mothers may experience feelings of inadequacy in caring for their child and worry how they will manage financially and logistically since many mothers are forced to give up their careers to become full time care takers.
The stages of grief that are experienced when receiving the news of expecting a child with a birth defect is comparable with those of losing a child. The mourning process is thought to stem from the realization that the previous hopes and visions of life with their child are now drastically changed. Grief counseling in these instances may be beneficial for mothers.
Conclusions
Acne vulgaris is a serious disorder that can disfigure patients and affect the psychosocial health of teenagers and young adults. Although understanding of the disease has progressed well since the time of the Renaissance, research still continues. Isotretinoin has been a major life-changing advance in the treatment of this disease but its teratogenic effects means it must be prescribed with education and care.
Footnotes
Disclosures: This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Armstrong RB. Photobiology of ultraviolet radiation. In: Abel EA, editor. Photochemotherapy in Dermatology. 2nd ed. Medical Publishers/Igaku-Shoin; New York/Tokyo: 1992. p. 17. [Google Scholar]
- Cleveland DE, Pirie AH. The treatment of chronic acne by X-ray. Can Med Assoc J. 1938;39:499–500. [PMC free article] [PubMed] [Google Scholar]
- Cohlan SQ. Excessive intake of vitamin A as a cause of congenital anomalies in the rat. Science. 1953;117:535–536. doi: 10.1126/science.117.3046.535. [DOI] [PubMed] [Google Scholar]
- Das S, Reynolds RV. Recent advances in acne pathogenesis. Am J Dermatol. 2014;15:479–488. doi: 10.1007/s40257-014-0099-z. [DOI] [PubMed] [Google Scholar]
- Fulton JE, Jr., Plewig G, Kligman AM. Effect of chocolate on acne vulgaris. JAMA. 1969;210:2071–2074. [PubMed] [Google Scholar]
- Goldsworthy RC, Schwartz NC, Mayhorn CB. Beyond abuse and exposure: Framing the impact of prescription-medication sharing. Am J Public Health. 2008;98:1115–1121. doi: 10.2105/AJPH.2007.123257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman H. 1st ed. McGraw-Hill; New York: 1936. Cosmetic dermatology. [Google Scholar]
- Grant RN. The history of acne. Proc R Soc Med. 1951;44:647–652. doi: 10.1177/003591575104400802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honein MA, Paulozzi LJ, Erickson JD. Continued occurrence of accutane-exposed pregnancies. Teratology. 2001;64:142–147. doi: 10.1002/tera.1057. [DOI] [PubMed] [Google Scholar]
- Hunter J, Savin J, Dahl M. 3rd ed. Wiley-Blackwell; Oxford: 2002. Clinical dermatology. [Google Scholar]
- Karagas MR, McDonald JA, Greenberg ER, Stukel TA, Weiss JE, Baron JA. Risk of basal cell and squamous cell skin cancers after ionizing radiation therapy. J Natl Cancer Inst. 1996;88:1848–1853. doi: 10.1093/jnci/88.24.1848. [DOI] [PubMed] [Google Scholar]
- Kligman AM, Fulton JE, Jr., Plewing G. Topical vitamin A in acne vulgaris. Arch Dermatol. 1969;99:469–476. [PubMed] [Google Scholar]
- Lee SM, Kim HM, Lee JS, Yoon CS, Park MS, Park KI. A case of suspected isotretinoin-induced malformation in a baby of a mother who became pregnant one month after discontinuation of the drug. Yonsei Med J. 2009;50:445–447. doi: 10.3349/ymj.2009.50.3.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemacks J, Fowles K, Mateus A, Thomas K. Insights from parents about caring for a child with birth defects. Int J Environ Res Public Health. 2013;10:3465–3482. doi: 10.3390/ijerph10083465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynberg MC, Khoury MJ, Lammer EJ, Waller KO, Cordero JF, Erickson JD. Sensitivity, specificity, and positive predictive value of multiple malformations in isotretinoin embryopathy surveillance. Tetrology. 1990;42:513–519. doi: 10.1002/tera.1420420508. [DOI] [PubMed] [Google Scholar]
- MacKee GM, Cipollaro AC. 4th ed. Lea and Fehiger; Philadelphia: 1946. X-rays and radium in the treatment of disease of the skin. [Google Scholar]
- McCaw IH. A synopsis of the history of dermatology. Ulster Med J. 1944;13:109–122. [PMC free article] [PubMed] [Google Scholar]
- Pace WE. A benzoyl peroxide-sulfur cream for acne vulgaris. Can Med Assoc J. 1965;93:252–254. [PMC free article] [PubMed] [Google Scholar]
- Peck GL, Olsen TG, Yoder FW, Strauss JS, Downing DT, Pandya M. Prolonged remissions of cystic and conglobate acne with 13-cis-retinoic acid. N Engl J Med. 1979;300:329–333. doi: 10.1056/NEJM197902153000701. [DOI] [PubMed] [Google Scholar]
- Plewig G, Kligman AM. Springer-Verlag; Berlin: 2012. Acne and rosacea 3rd ed. [Google Scholar]
- Plumbe S. 4th ed. Sherwood, Gilbert, & Piper; London: 1937. A practical treatise on the diseases of the skin: Arranged with a view to their constitutional causes and local characters: Including the substance of the essay to which the Royal College of Surgeons awarded the Jacksonian Prize, and all such valuable facts as have been recorded by continental authors on these subjects to the present time. [Google Scholar]
- Pusay WA. Acne and sycosis treated by exposure to roentgen rays. J Cutan Dis. 1902;20:204–210. [Google Scholar]
- Rea JN, Newhouse ML, Halil T. Skin disease in Lambeth. A community study of prevalence and use of medical care. Br J Prev Soc Med. 1976;30:107–114. doi: 10.1136/jech.30.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson NB. Science Press; London: 1991. Acne and the mature woman. [Google Scholar]
- Smith R, Mann N. Glycemic load and acne. In: Pappas A, editor. Nutrition and skin lessons for anti-aging, beauty and healthy skin. 1st ed. Springer; New York: 2011. p. 147. [Google Scholar]
- Sladden MJ, Harman KE. What is the chance of a normal pregnancy in a woman whose fetus has been exposed to isotretinoin? Arch Dermatol. 2007;143:1187–1188. doi: 10.1001/archderm.143.9.1187. [DOI] [PubMed] [Google Scholar]
- Stüttgen G. Zur lokal behandlung von keratosen mit vitamen A saure. Dermatologia. 1962;124:65–80. [PubMed] [Google Scholar]
- Von Jacobi E. 1st ed. Urban and Schwartzenberg; Berlin: 1903. Atlas der hautkrankheiten. [Google Scholar]
- Zouboulis CC, Katsambas AD, Kligman AM. Springer-Verlag; Berlin: 2014. Pathogenesis and treatment of acne and rosacea. [Google Scholar]