Abstract
Background
Tic disorders, including Tourette syndrome, are complex, multi-symptom diseases, yet, the impact of these disorders on affected children, families, and communities is not well understood.
Methods
To improve the understanding of the impacts of Tourette syndrome, two research groups conducted independent cross-sectional studies using qualitative and quantitative measures. They focused on similar themes, but distinct scientific objectives, and the sites collaborated to align methods of independent research proposals with the aim of increasing the analyzable sample size.
Results
Site 1 (University of Rochester) was a Pediatric Neurology referral center. Site 2 (University of South Florida) was a Child Psychiatry referral center. A total of 205 children with tic disorders were enrolled from both studies. The University of Rochester also enrolled 100 control children in order to clearly isolate impacts of Tourette syndrome distinct from those occurring in the general population. The majority of children with tic disorders (n=191, 93.1%) had Tourette syndrome, the primary population targeted for these studies. Children with Tourette syndrome were similar across sites in terms of tic severity and the occurrence of co-morbid conditions. The occurrence of psychiatric comorbidities in the control group was comparable to that in the general pediatric population of the United States, making this a well-justified comparison group.
Conclusions
Through collaboration, two sites conducting independent research developed convergent research methods to enable pooling of data, and by extension increased power, for future analyses. This method of collaboration is a novel model for future epidemiological research of tic disorders.
Keywords: Tourette syndrome, tics, epidemiology, research methods, research design
Introduction
Tics are abnormal involuntary movements and sounds characterized by sudden, discrete, repetitive, stereotyped movements that wax and wane over time; tics are often preceded by a premonitory urge. Common tics include blinking, eye rolling, sniffing, and throat clearing. Tic disorders are classified by tic type (motor, phonic, or both) and symptom duration (less or greater than one year).1 The spectrum of tics is broad. Some tics are non-bothersome, some interfere with academic and social functioning, and still others result in direct self-injury or pain.2 As many as 20% of children in the United States experience tics at some time.3 Tourette syndrome (TS), the most clinically complex of the tic disorders, is defined by the presence of multiple motor tics and at least one vocal tic, occurring for more than one year, and beginning before age 18 years.1 Studies across several countries estimate that 0.2–0.9% of children have Tourette syndrome.4,5
Common comorbidities of Tourette syndrome include attention deficit/hyperactivity disorder (ADHD),6 anxiety, and obsessive-compulsive disorder (OCD).7,8 Tourette syndrome has also been linked with other behavioral health problems7,9–11 and impairments in school, home, and social functioning.12 Tourette syndrome and its associated conditions can have major social, emotional, and economic impacts during a child’s critical formative years and can impact the child’s family and community. These impacts have not been evaluated systematically. Understanding the impacts of Tourette syndrome is a prerequisite for the development of interventions and management approaches aimed at reducing the negative consequences of the condition.
We sought to improve the understanding of the ways that Tourette syndrome impacts children, families, and communities through a cross-sectional epidemiologic study. Herein, we outline the study design and methodological considerations, including multi-modal assessment and an approach to align methods across two independent research studies, enabling pooling of data to address new research questions with increased power. Results of our data analyses will be presented in subsequent manuscripts.
Methods
In 2009, the Centers for Disease Control and Prevention (CDC) released a funding opportunity announcement for proposals to examine the public health impact of pediatric tic disorders. The results of this research were anticipated to “aid in the development of programs and interventions [and local, state, and national policies] that will improve quality of life for individuals with tic disorders and their families.” Cooperative agreements with the CDC were competitively awarded to the University of Rochester (UR) and the University of South Florida (USF), who independently submitted applications with separate and distinct study aims and research plans. After the initial proposal development and funding, the sites collaborated to align ascertainment and assessment approaches for future collective data use across the sites. The characteristics of each site, study aims, recruitment strategies, and study activities are described below.
Study Site Characteristics
The UR and USF sites are tertiary care centers for the care of Tourette syndrome, tic disorders, and related conditions. The UR Tourette syndrome Clinic is based in Rochester, a mid-sized city in upstate New York. It serves a catchment of 1.5 million citizens from urban, suburban, and rural settings. Approximately 650 children and adolescents with Tourette syndrome receive ongoing care at the UR Tourette syndrome clinic. The USF Rothman Center for Pediatric Neuropsychiatry is located in St. Petersburg, a mid-sized city in Florida. It serves a catchment of 4 million individuals. Approximately 300 children and adolescents with tic disorders are actively followed.
Each site developed a multi-disciplinary team to conduct the study. The UR study team included two child neurologists who specialize in pediatric movement disorders, two clinical psychologists, a pediatric neurology nurse practitioner, an epidemiologist, and a biostatistician. The USF study team included two child and adolescent psychiatrists, four clinical psychologists, a speech-language pathologist, and a psychology trainee study coordinator.
Specific Aims
The primary objectives for the UR group were to assess the impacts of Tourette syndrome and to identify factors that were most closely associated with reduced quality of life in affected individuals and their families. To isolate impacts distinct from those occurring in the general population, UR established both Tourette syndrome and control groups and evaluated parent-child dyads from each group.
The primary objective of the USF group was to assess the impacts of tic disorders on children and their families, and the specific challenges faced by children with a tic disorder, in order to guide the development of interventions and community services. The specific aims of each research site are outlined in Table 1.
Table 1.
Research Aims by Site
| UR | USF | |
|---|---|---|
| Aim 1 | To establish the diagnosis and severity of TS and co-occurring neuropsychiatrie conditions | To examine characteristics and healthcare utilization of children receiving treatment for tic disorders from childhood to adolescence |
| Aim 2 | To examine individual school, social, and global functioning (comparing TS participants and controls) | To examine experiential components that enhanced or hindered adaptation of children and their families to their social networks |
| Aim 3 | To examine family functioning, including parent quality of life, socioeconomic, social, and global functioning (comparing TS participants and controls) | To assess acceptability, feasibility and perceived benefits of the intervention options identified within a qualitative research framework to supplement findings on experiences related to tics, support, resiliency, and coping mechanisms |
| Aim 4 | To examine community resource use, including educational, social, and health resource use (comparing TS participants and controls) | |
| Aim 5 | To identify targets for future intervention by assessing demographic and clinical features most closely correlating with quality of life |
Recruitment strategy
At UR, Tourette syndrome clinic patients were recruited in-person or by mail. Study information was also shared at local Tourette Association of America chapter events. The initial strategy for control recruitment was via peer nomination; participants with Tourette syndrome were asked to identify age- and gender-matched friends without Tourette syndrome. Most participants were unable to do so because non-family members were not privy to the TS diagnosis, or more commonly, because the child with Tourette syndrome lacked friends who could be approached for participation. The control recruitment strategy was modified to a community-based approach, distributing study recruitment materials at general pediatric practices, community organizations, and on family-oriented local websites.
At USF, individuals with tic disorders were recruited from the normal patient flow into the USF Rothman Center for Pediatric Neuropsychiatry. Information about the study was also made available at local Tourette Association of America chapter events.
Study activities
At UR, children ages 5–18 years with a confirmed diagnosis of Tourette syndrome and age- and sex-matched controls were invited to participate with a parent. Participation involved a single 3–5 hour research visit that included structured and semi-structured interviews, child and parent self-report forms, and parent-proxy report forms. The child’s history of legal or disciplinary problems was also sought by report from the parent-child dyad.
At USF, children ages 6–18 years with a confirmed diagnosis of Tourette syndrome, chronic tic disorder (CTD), or tic disorder-NOS were identified via phone screeners conducted by the study coordinator and were subsequently scheduled for a single study visit. The USF site used a multi-method study approach that combined quantitative and qualitative research methods. Participants were offered the choice to enroll in one or both of the quantitative/qualitative components of the study. Study participation involved a single 3–4 hour study visit that included several clinician-administered assessments and several child- and parent-report questionnaires. Tic and co-occurring psychiatric diagnoses were assessed using structured and semi-structured interviews, child and parent self-report forms, parent-proxy report forms, and a review of clinical interviews and medical records. Final diagnoses were assigned using all available data. For the qualitative portion of the study, parent-child dyads participated in focus groups to assess tic presentation, socio-demographic and parental characteristics, social relationships, and perceived stigma. Children were invited to complete a short, daily, experience-sampling questionnaire (for at least 10 days) on which they self-evaluated their day-to-day functioning and tic-related impairment. At both sites, school records were obtained for the most recently completed academic year, including state-based standardized tests of academic proficiency, educational classification and accommodations, prior grade retention and/or summer school, and school absenteeism. Participants identified a teacher to complete an assessment of classroom function and personal knowledge of features of Tourette syndrome. School records and teacher-reported data were not gathered for home-schooled children due to the lack of a consistent benchmark for academic attainment across the varied programs.
Table 2 lists inclusion and exclusion criteria for both sites. Low IQ and cognitive impairment were not specific UR exclusion criteria a priori. However, in the process of conducting the study, data from four parent-child dyads were excluded because either parent or child were not able to complete study-specific procedures due to cognitive limitations.
Table 2.
Inclusion/Exclusion Criteria
| University of Rochester | University of South Florida | |
|---|---|---|
| Tourette Syndrome Participants | Tic Disorder Participants | |
| Inclusion criteria | Physician confirmed diagnosis of Tourette Syndrome by DSM-IV-TR criteria | Clinician-diagnosed tic disorder for more than 6 months and confirmed diagnosis of a tic disorder by DSM-IV-TR criteria |
| Current tics as measured by the YGTSS | ||
| Score ≥ 80 Peabody Picture Vocabulary Test | ||
| Age 5–18 years | Age 6–18 years | |
| Parent and child willing to participate | Parent and child willing to participate | |
| Exclusion criteria | None | Comorbid active psychosis or mania, or current suicidal intent |
| A diagnosis that would limit ability to participate in study procedures | ||
| Control Participants | ||
| Inclusion criteria | Age 5–18 years | N/A |
| Parent and child willing to participate | ||
| Exclusion criteria | Immediate family member with Tourette syndrome |
Site Collaboration
Joint selection of measures
As part of the cooperative agreements with the CDC, the individual UR and USF sites collaborated to enable future pooling of data from their independent studies to maximize sample size for analysis of similar aims and new research questions. In the first year of the award, and prior to subject enrollment at either site, the UR and USF sites and CDC personnel developed a collaborative data collection approach. Wherever possible, identical case ascertainment methods and study measures were jointly agreed to and implemented for each independent study. Table 3 lists all study measures at each site and shows the extensive overlap that enabled each site to boost its sample size for independent analyses of the shared measures. The supplemental table outlines the characteristics of each study assessment, including the respondent, format, and disease or symptom domain. In concert with the alignment of assessments for the independent research programs, data capture and database design including variable naming conventions were developed.
Table 3.
Clinical measures
| DOMAIN | MEASURE | UR | USF |
|---|---|---|---|
|
| |||
| Tics | Yale Global Tic Severity Scale13 The Motor tic, | ✓ | ✓ |
| Obsessions and compulsions, Vocal tic Evaluation Survey14 | ✓ | ✓ | |
| Child TS Impairment Scale Parent Report12 | ✓ | ✓ | |
|
| |||
| ADHD | (DISC-IV)15 – ADHD module | ✓ | ✓ |
| Swanson, Nolan, and Pelham Questionnaire16 | ✓ | ✓ | |
|
| |||
| OCD | DISC-IV15 – OCD module | ✓ | ✓ |
| Children’s Yale-Brown Obsessive Compulsive Scale17 | ✓ | ✓ | |
| The Motor tic, Obsessions and compulsions, Vocal tic Evaluation Survey14 | ✓ | ✓ | |
|
| |||
| Depression | DISC-IV15 – Major Depressive Disorder module | ✓ | ✓ |
| Children’s Depression Inventory-short version18 | ✓ | ✓ | |
|
| |||
| Anxiety | DISC-IV15 – Generalized Anxiety Disorder module | ✓ | ✓ |
| Multidimensional Anxiety Scale for Children19 | ✓ | ✓ | |
|
| |||
| Anger, Rage | Measure of Anger, Violence, and Rage in Children20 | ✓ | ✓ |
| The Anger Expression Scale for Children21 | ✓ | ✓ | |
|
| |||
| Oppositional behaviors | DISC-IV15 – Oppositional Defiant Disorder and Conduct Disorder modules | ✓ | ✓ |
|
| |||
| Risk behaviors | DISC-IV15 – Substance Abuse Disorder module | ✓ | ✓ |
| Youth Risk Behavior Survey22 | ✓ | ||
|
| |||
| Global behavior | Child Behavior Check List23 | ✓ | ✓ |
| Youth Self Report23 | ✓ | ||
|
| |||
| Social skills and self-concept | Social Skills Rating System24 | ✓ | |
| Social Responsiveness Scale25 | ✓ | ||
| Friendship Qualities Scale26 | ✓ | ||
| Piers Harris Children’s Self-Concept Scale27 | ✓ | ||
| Children’s Coping Strategies Checklist28 | ✓ | ||
|
| |||
| Cognition | Peabody Picture Vocabulary Test-Third Edition29 | ✓ | |
| Behavior Rating Inventory of Executive Functioning30 | ✓ | ||
|
| |||
| School functioning | New York State standardized tests | ✓ | |
| Educational classification and accommodations | ✓ | ||
| Teacher Report Form23 | ✓ | ✓ | |
|
| |||
| Quality of life | Child Health Questionnaire31 | ✓ | ✓ |
| World Health Organization Quality of Life-BREF32 | ✓ | ||
|
| |||
| Family impacts | PedsQL Family Impact Module33 | ✓ | ✓ |
| Family Assessment Device34 | ✓ | ||
|
| |||
| Global functioning | Children’s Global Assessment Scale35 | ✓ | ✓ |
|
| |||
| Service use | Services Assessment for Children and Adolescents36 | ✓ | |
|
| |||
| Tourette Syndrome knowledge | Teacher Understanding of TS | ✓ | ✓ |
| Parent Understanding of TS | ✓ | ✓ | |
ADHD – Attention Deficit Hyperactivity Disorder, DISC-IV - Diagnostic Interview Schedule for Children-4th edition, OCD – Obsessive Compulsive Disorder, TS – Tourette Syndrome
Participants were enrolled from March 2010 to September 2012. Figure 1 outlines the participant flow into the study at each site.
Figure 1. Participant Recruitment and Eligibility.
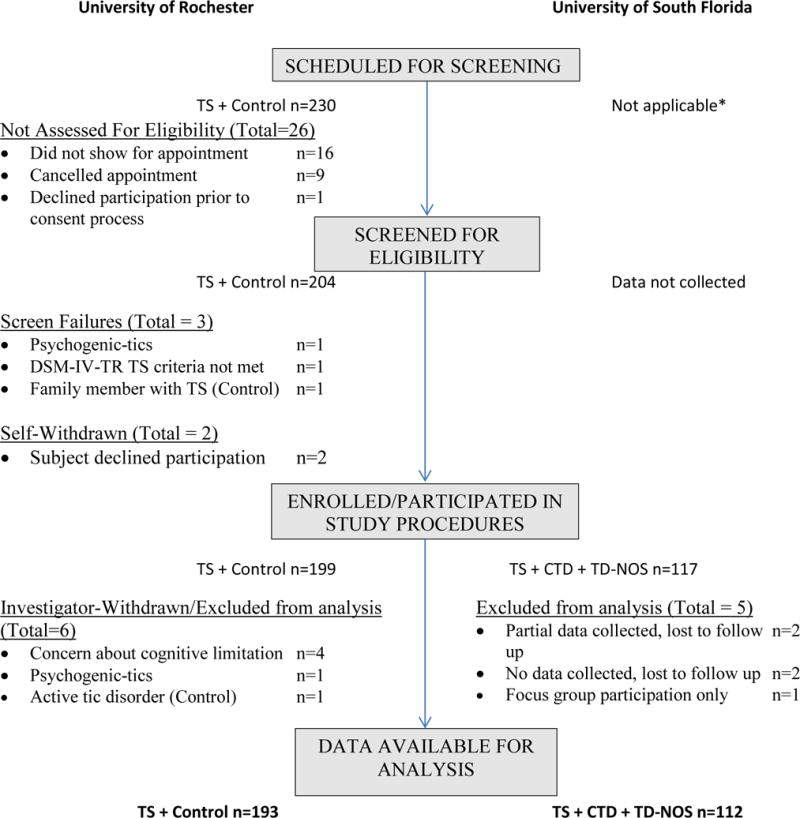
Abbreviations
CTD: chronic tic disorder
DSM-IV-TR: Diagnostic and Statistical Manual for Mental Disorders, 4th edition, text revision1
TD-NOS: Tic disorder not otherwise specified
TS: Tourette syndrome
Rater Training
Cross-site training sessions were conducted to ensure the integrity and compatibility of assessments across sites, particularly for the Yale Global Tic Severity Scale (YGTSS) and Child Diagnostic Interview Schedule for Children (C-DISC-IV). YGTSS training was provided by an experienced rater (L. Scahill) and included an initial didactic session with raters, scoring of a standardized YGTSS interview training video, scoring review with the experienced rater, then additional independent scoring of two additional YGTSS interview videos by the new raters, which were compared to the experienced rater. To be considered reliable, raters’ YGTSS scores had to fall within 15% of that obtained by the experienced rater for the Total Motor Tic score, the Total Vocal Tic score and the Total Tic Score, on all three recordings. Raters who did not meet criteria on the YGTSS received additional training and scored one or two additional YGTSS video recordings.
A licensed clinical psychologist (UR site) and a Bachelor’s or Master’s level clinician (USF site) provided C-DISC training and supervision to personnel with Bachelor’s or Master’s level education in Psychology or Nursing. Interviewers completed several supervised practice sessions in which they administered the C-DISC to another study team member. Following supervisor feedback on interview style, awareness of clinical phenomenology, and strategies to clarify participant responses, raters then administered the C-DISC to study participants with the supervisor present and available to assist. Once the supervisor was satisfied that a rater could administer the C-DISC on a consistent basis without additional support, the rater was approved to conduct the C-DISC interview independently.
Safety
Assessments included questions related to self-harm, suicidal ideation, and violence towards others. To ensure participant safety, each site instituted a safety triage process for those reporting these risk behaviors. If a participating child or parent answered a question that invoked triage, the participant was evaluated during the visit by a study team clinician to assess for safety and examine potential need for further referral or reporting. Referrals for mental health services were made if clinically indicated. Figure 2 represents a flow diagram of the triage process. A total of 19 youth with chronic tic disorders and 3 control youth had responses that triggered the triage process.
Figure 2. Triage Protocol.
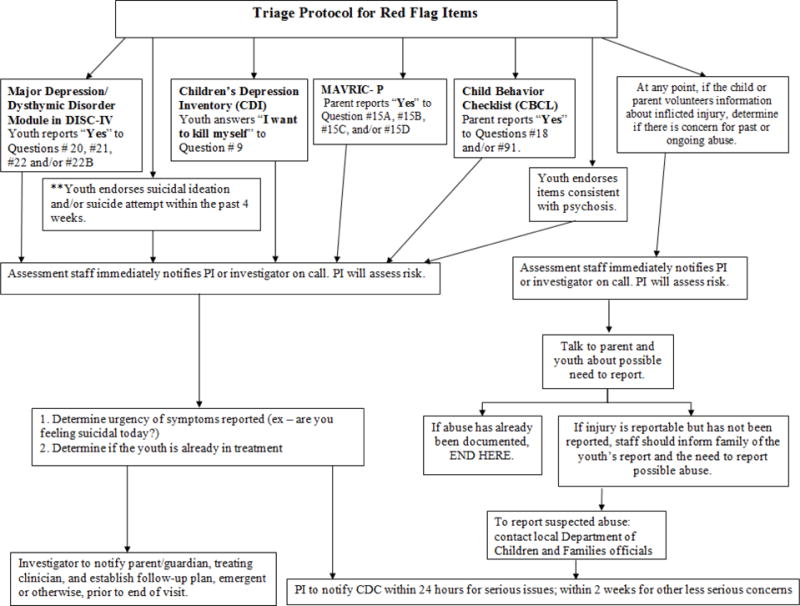
Abbreviations
DISC-IV: Diagnostic Interview Schedule for Children – Fourth edition (DISC-IV)15
MAVRIC-P: Measure of Anger, Violence, and Rage in Children, parent-report20
PI: Principal investigator
Local institutional review board approval was secured at both sites prior to enrollment of participants (UR RSRB# 30985, USF-ACH IRB# 09-0209). Parent permission for child’s participation, parent consent, and child assent were completed for each parent/child pair. A federal Certificate of Confidentiality was obtained to protect the privacy of study participants.
Statistical Analysis
For data presented in this manuscript, descriptive statistics were used to describe the data in aggregate. Due to small sample size in the chronic tic disorder and tic disorder-NOS groups (n=7, each), these data were not used in any group comparisons. One-way ANOVA tests were used for comparisons of age at study participation, age at tic onset, YGTSS score, and Clinician Global Assessment Scale (CGAS) score, by diagnostic group (UR Tourette syndrome group, USF Tourette syndrome group, or UR control group). Chi-square tests were used to compare demographic variables (sex, race, ethnicity, highest parent education level, and positive DISC diagnosis endorsed by parent or child) by diagnostic group. Analyses were completed using IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.
Results
Participant demographics are outlined in Table 4. Across sites, n=205 children with tic disorders were enrolled, and 100 control group children were enrolled at UR. A small number of children at USF had diagnoses other than Tourette syndrome, including Chronic Tic Disorder (CTD, n=7), and Tic Disorder Not Otherwise Specified (TD-NOS, n=7). Across both sites, participants were mostly male (70.5%, n=215), which was expected based on the known epidemiology of tic disorders.37 There were no group differences in child’s age at study participation or ethnicity between the Tourette syndrome groups (UR and USF) and UR controls. Demographic differences between UR and USF TS diagnostic groups were limited to the proportion endorsing they were more than one race, or reported their race was “unknown”, or did not report their race (χ2 =12.66, df=4, p=0.01). Between UR Tourette syndrome and UR control groups, we found the following differences: a higher percentage of males in the Tourette syndrome group (χ2=4.38, df=1, p=0.04), and a higher percentage of participants of Black race in the Control group (χ2=11.36, df=3, p=0.01).
Table 4.
Demographics by Site
| University of Rochester | University of South Florida | ||||
|---|---|---|---|---|---|
| TS (n=93) |
Controls (n=100) |
TS (n=98) |
CTD (n=7)ⱡ |
TD-NOS (n=7)ⱡ |
|
| Male n (%) | 69 (74.2) | 60 (60)* | 76 (77.6) | 6 (85.7) | 4 (57.1) |
| Mean age (years) (SD) | 11.5 (2.8) | 11.1 (2.8) | 11.2 (3.1) | 10.7 (2.6) | 8.0 (2) |
| Median age (years) (IQR) | 11 (5) | 11 (4) | 11 (5) | 10 (5) | 7 (4) |
| Race | |||||
| White n (%) | 77 (82.8) | 75 (75) | 90 (91.8) | 6 (85.7) | 7 (100) |
| Black n (%) | 1 (1.1) | 13 (13)* | 3 (3.1) | 0 | 0 |
| Asian n (%) | 0 | 0 | 2 (2) | 0 | 0 |
| More than one race n (%) | 10 (10.8) | 10 (10) | 3 (3.1)* | 1 (14.3) | 0 |
| Unknown or not reported n (%) | 5 (5.4) | 2 (2) | 0* | 0 | 0 |
| Ethnicity | |||||
| Non-Hispanic n (%) | 83 (89.2) | 90 (90) | 80 (81.6) | 6 (85.7) | 5 (71.4) |
| Hispanic n (%) | 8 (8.6) | 9 (9) | 18 (18.4) | 1 (14.3) | 2 (28.6) |
| Unknown or not reported n (%) | 2 (2.2) | 1 (1) | 0 | 0 | 0 |
| Highest Parent/Guardian Education | |||||
| Less than high school n (%) | 0 | 5 (5) | 0 | 1 (14.3) | 0 |
| High school graduate or GED® n (%) | 6 (6.5) | 6 (6) | 6 (6.1) | 0 | 0 |
| Some college, Associate’s degree, or Vocational school n (%) | 35 (37.6) | 25 (25) | 25 (25.5) | 1 (14.3) | 3 (42.9) |
| Bachelor’s, Master’s or professional degree n (%) | 50 (53.8) | 63 (63) | 63 (64.3) | 5 (71.4) | 4 (57.1) |
| Unknown or not reported n (%) | 2 (2.2) | 1 (1) | 4 (4.1) | 0 | 0 |
CTD - chronic tic disorder; GED® - General Educational Development Test; IQR - interquartile range; SD - standard deviation; TS - Tourette Syndrome; TDNOS - tic disorder not otherwise specified; UR - University of Rochester; USF - University of South Florida
Not included in group comparisons with UR TS group
Compared to UR TS group, χ2 p<0.05
Parent education (Table 4), was evaluated by the highest educational level reported for any of the child’s parents/primary caretakers. There were no differences between UR Tourette syndrome and UR control groups in educational attainment.
Clinical characteristics
Table 5 presents the clinical characteristics of child participants. In the Tourette syndrome group, three participants reported ages at tic onset younger than 2 years; these individuals were excluded from the age at onset analysis, based on the typical age of onset of tic disorders and likelihood that these children had other movement disorders seen in infancy (e.g. stereotypies). Of the 100 control children, n=5 had possible previously undiagnosed tics of low frequency. There were no differences between the UR and USF Tourette syndrome groups with respect to either parent-reported age at tic onset (retrospective) or tic severity as measured by the YGTSS. The YGTSS total tic severity scores (not including impairment) in the UR and USF Tourette syndrome groups spanned from minimal to severe tic symptoms (range 3–50). Based on C-DISC data, there were also no site differences in the frequency of other parent and/or child-endorsed specific clinical diagnoses. Similarly, there were no site differences in a measure of current clinician-rated global functioning (CGAS) between Tourette syndrome groups.
Table 5.
Clinical Characteristics by Site
| UR TS (n=93) |
UR Controls (n=100) |
USF TS (n=98) |
USF Other Tic Disorders (n=14) |
|
|---|---|---|---|---|
| Mean age at tic onset (SD) | 5.7 (2.3) | 7.2 (1.9) | 6.4 (2.9) | 7.1 (2.1) |
| Mean YGTSS total tic score (SD) | 21.1 (8.6) | 0.3 (1.2) | 23 (9.9) | 14.7 (8.4) |
| Mean GAS (SD) | 60.1 (14.7) | 77.1 (16.3) | 58 (7.5) | 62.6 (8.7) |
| C-DISC diagnosis modules %* (valid n)** | ||||
| ADHD | 46.2 (93) | 9.1 (99) | 39.8 (98) | 35.7 (14) |
| ODD | 39.8 (93) | 14.1 (99) | 33.7 (98) | 0 (14) |
| OCD | 37.6 (93) | 5.1 (99) | 42.9 (98) | 14.3 (14) |
| GAD | 14 (93) | 2 (99) | 19.4 (98) | 28.6 (14) |
| MDE | 7.5 (93) | 0 (99) | 9.2 (98) | 21.4 (14) |
| CD | 6.5 (93) | 5.1 (99) | 4.1 (98) | 0 (14) |
| SAD | 0.0 (50) | 8.3 (48) | 2.4 (42) | 0 (3) |
Represents % meeting criteria for a specified diagnosis based on C-DISC-parent or C-DISC-youth.
Number of participants who completed this C-DISC module
ADHD – Attention-Deficit/Hyperactivity Disorder
CD – Conduct Disorder
C-DISC - Diagnostic Interview Schedule for Children – Fourth edition, child report (DISC-IV)15
GAD – Generalized Anxiety Disorder
GAS - Clinician-rated global functioning
MDE – Major Depressive Episode
OCD – Obsessive Compulsive Disorder
ODD – Oppositional Defiant Disorder
SAD – Substance Abuse Disorder (completed for adolescents)
SD – standard deviation
TS – Tourette Syndrome
UR – University of Rochester
USF – University of South Florida
YGTSS – Yale Global Tic Severity Scale (YGTSS)13
Discussion
This study was unique for research on tic disorders in the composition of its research team, cross-site collaboration with independent projects, unified data collection methods to enable pooling of data, and a broad-based approach in terms of content and execution (e.g., multi-modal, multi-informant, and multi-setting). The approach was more comprehensive than typical approaches to epidemiologic research on tic disorders which involve prospective recruitment at a single center,38 retrospective use of a database,6,37 retrospective clinical chart review,39,40 or national survey data.4 With some exceptions,4,38,41–43 most approaches do not include a concurrent and well-matched control group, but instead use reported population-based norms or reference the extant literature. Similarly, such research is often framed by a neurologist, psychiatrist, or psychologist, but rarely all of these perspectives concurrently. Finally, most prior studies focus on either school, home, or social functioning, but in-depth assessments across a variety of functional domains and through multi-informant assessment of the same individual are limited. Informant discrepancies are not uncommon in child assessment, but each source (e.g., parent, teacher, child) may contribute valuable and distinct information about a child’s function; a multi-informant approach can boost validity of assessments and provide a more nuanced understanding of potentially context-dependent concerns.44
Our approach was also innovative in its parallel execution of two independent studies in a manner that enables pooling of data despite different aims. Typical approaches to multi-center research involve a single set of research aims, executed in the same manner by each center. In our research, investigators from independent research studies with distinct scientific questions were able to align data collection strategies in a unified operational approach to boost sample size and power for future analyses of new research questions. We have already used this pooled-data approach to address questions regarding suicidal ideation in children with tic disorders and the validity of the diagnostic interview schedule for children in the diagnosis of tic disorders.45,46 In the case of suicidal ideation, pooling data enabled more accurate assessment of an uncommon occurrence through larger sample size, advance alignment of data collection methods added to scientific rigor, and advance alignment of database development facilitated the feasibility of such an analysis. We anticipate that this could be a useful approach for future epidemiological studies, and an important consideration for funding agencies soliciting applications for targeted, disease-specific announcements. For instance, this kind of approach is underway for the National Institute of Environmental Health Sciences Environmental influences on Child Health Outcomes program, where standardized core data elements will be implemented in 35 independent cohort studies at sites across the United States (https://www.nih.gov/echo).
Through development of their respective, unique set of scientific questions, both sites sought to broadly improve understanding of the impacts of tic disorders, extending beyond the affected individual alone. The UR site focused on quantifying Tourette syndrome impacts on individuals, families, and communities; the USF site explored the qualitative experiences of children and families affected by Tourette syndrome to improve understanding of factors related to resiliency and coping.
The resulting samples enrolled by the independent sites did not differ on a core set of clinical characteristics (age at tic diagnosis, tic severity and co-morbid disorder occurrence), nor were there significantly different demographic characteristics, except for the proportion of individuals endorsing a background of more than one race. This suggests that although the Tourette syndrome groups were recruited from rather disparate settings in the U.S. (e.g., a Neurology clinic in a mid-sized northeastern city, and a Psychiatry clinic in a large southeastern metropolitan area), data from these groups are suitable for pooled analyses.
The UR control group differed from the UR Tourette syndrome group on two demographic factors: the proportion of individuals with male sex, and black race. To better understand the comparability of the UR control group, we evaluated how well the recruited controls reflected the clinical characteristics in terms of other neuropsychiatric diagnoses of the national population. The prevalence of other behavioral health disorders in the control cohort (Table 4) was similar to national estimates of ADHD (8.9%), major depressive episode (2.1%), generalized anxiety disorder (3%), OCD (3%), conduct disorder (2.1%), and substance abuse disorders (8.3%).47,48 Although there are some minor demographic differences between UR controls and the Tourette syndrome groups across sites, the control sample represents a valid comparison group based on age distribution and similarity to children nationwide in terms of psychiatric comorbidities, which form the critical backdrop for future comparative study of related factors of individual risk behaviors, family functioning, community resource use, and others. Given the similarity between the UR Tourette syndrome and USF Tourette syndrome groups, by extension, the UR control group can be an appropriate control group for the separately recruited USF Tourette syndrome group as well.
The Tourette syndrome groups under study were similar to previously published observational studies of patients with Tourette syndrome in terms of age at tic onset, tic severity and co-morbidities.4,49,50 This suggests that knowledge derived from the study of this cohort may be generalizable to at least a similar degree as prior landmark studies.
The collective approach had a number of strengths, including: use of a concurrent control group, recruitment from more than one geographic region, recruitment from both neurology-based and psychiatry-based clinic populations, and inclusion of a broad age range of participants. We anticipate that recruitment from both clinic populations will increase the generalizability of our results. Comprehensive, multi-modal assessment was completed, using observer-based, interview-based, and self-report data. In addition, the data sources were also expansive, including children, parents, teachers, and school districts. These data will allow expansion of the current state of knowledge of Tourette syndrome, particularly with a broader individual patient, family, and community resource use perspective. There were sufficient similarities between the UR and USF Tourette syndrome groups to suggest that pooling data for future analyses is appropriate. Despite some limited demographic differences, the control group well reflects the prevalence of non-Tourette syndrome neuropsychiatric disorders in the general population, and is reasonably well matched with our clinical groups for educational attainment. For select hypotheses, analyses utilizing the Tourette syndrome groups from both sites and the UR control group will be both fitting and a strength of the study designs.
There were some limitations of this study. It drew from a predominantly non-Hispanic Caucasian sample. Tic disorders in Hispanic, non-Hispanic Black, and other minority populations have not been well studied. This study does not add to the knowledge about these populations, and additional focused study of the epidemiology of Tourette syndrome and related disorders in minority populations is needed. The samples at both sites were highly educated, and may have more ready access to resources that provide resilience against negative impact compared to the population of children with Tourette syndrome at large. Both Tourette syndrome samples were predominantly male, and although this reflects the known epidemiology of Tourette syndrome, it is possible that there are sex-based differences in disease course and disease impact. Even when pooling data across the two sites, the sample size may be insufficient to examine these differences. Similarly, as a cross-sectional study, it will not be possible to ascertain the changing impacts of Tourette syndrome over time. It may be used to generate new hypotheses concerning risk or resiliency factors, but this will require direct study in future longitudinal projects. There is potential for recruitment bias; study visits were extensive, approximately 4 hours duration, at each site. Further, each site is a tertiary referral center for Tourette syndrome. It is possible that Tourette syndrome participants from these settings represent more severe or more complex cases. On the other hand, many may also be considered optimally treated, as their care is provided by clinicians considered expert in this diagnosis.
Understanding of the impacts of childhood tic disorders on individuals, families, and community resource use has been limited. Results from these combined multi-modal, multi-informant, and multi-setting cross-sectional studies will contribute significantly to this knowledge void. The results of our upcoming data analyses have the potential to lead to advancements in clinical care and public health policy for children and families affected by tic disorders. Of particular interest from these studies, however, is a model for observational studies employing academic-federal collaboration with advanced cross-site collaboration to enable expanded sample size for future questions of interest.
Acknowledgments
We thank the families and teachers who participated in these studies and the local chapters of the Tourette Association of America for their support in outreach to potential participants. We also acknowledge the contributions of Dr. Lawrence Scahill in YGTSS training.
This study was supported by CDC Cooperative Agreements #U01DD000509 (USF) and #U01DD000510 (UR) and NINDS NS066098 (K12).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th. Washington, D C: 2000. [Google Scholar]
- 2.Mathews CA, Waller J, Glidden D, et al. Self injurious behaviour in Tourette syndrome: correlates with impulsivity and impulse control. J neurology, neurosurgery, and psychiatry. 2004;75(8):1149–1155. doi: 10.1136/jnnp.2003.020693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Snider LA, Seligman LD, Ketchen BR, et al. Tics and problem behaviors in schoolchildren: prevalence, characterization, and associations. Pediatrics. 2002;110(2):331–336. doi: 10.1542/peds.110.2.331. [DOI] [PubMed] [Google Scholar]
- 4.Bitsko RH, Holbrook JR, Visser SN, et al. A national profile of Tourette syndrome, 2011–2012. J Dev Behav Pediatr. 2014;35(5):317–322. doi: 10.1097/DBP.0000000000000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robertson MM. The prevalence and epidemiology of Gilles de la Tourette syndrome. Part 1: the epidemiological and prevalence studies. J Psychosom Res. 2008;65(5):461–472. doi: 10.1016/j.jpsychores.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Freeman RD. Tic disorders and ADHD: answers from a world-wide clinical dataset on Tourette syndrome. Eur Child Adolesc Psychiatry. 2007;16(Suppl 1):15–23. doi: 10.1007/s00787-007-1003-7. [DOI] [PubMed] [Google Scholar]
- 7.Kurlan R, Como PG, Miller B, et al. The behavioral spectrum of tic disorders: a community-based study. Neurology. 2002;59(3):414–420. doi: 10.1212/wnl.59.3.414. [DOI] [PubMed] [Google Scholar]
- 8.Robertson MM, Trimble MR, Lees AJ. The psychopathology of the Gilles de la Tourette syndrome. A phenomenological analysis. The British journal of psychiatry : the journal of mental science. 1988;152:383–390. doi: 10.1192/bjp.152.3.383. [DOI] [PubMed] [Google Scholar]
- 9.Budman CL, Rockmore L, Stokes J, Sossin M. Clinical phenomenology of episodic rage in children with Tourette syndrome. J Psychosom Res. 2003;55(1):59–65. doi: 10.1016/s0022-3999(02)00584-6. [DOI] [PubMed] [Google Scholar]
- 10.Robertson MM. J Psychosom Res. Vol. 61. England: 2006. Mood disorders and Gilles de la Tourette’s syndrome: An update on prevalence, etiology, comorbidity, clinical associations, and implications; pp. 349–358. [DOI] [PubMed] [Google Scholar]
- 11.McGuire JF, Hanks C, Lewin AB, Storch EA, Murphy TK. Social deficits in children with chronic tic disorders: phenomenology, clinical correlates and quality of life. Comprehensive psychiatry. 2013;54(7):1023–1031. doi: 10.1016/j.comppsych.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 12.Storch EA, Lack CW, Simons LE, Goodman WK, Murphy TK, Geffken GR. A measure of functional impairment in youth with Tourette’s syndrome. Journal of pediatric psychology. 2007;32(8):950–959. doi: 10.1093/jpepsy/jsm034. [DOI] [PubMed] [Google Scholar]
- 13.Leckman JF, Riddle MA, Hardin MT, et al. The Yale Global Tic Severity Scale: initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry. 1989;28(4):566–573. doi: 10.1097/00004583-198907000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Gaffney GR, Sieg K, Hellings J. The MOVES: A self-rating scale for Tourette’s Syndrome. Journal of child and adolescent psychopharmacology. 1994;4(4):269–280. [Google Scholar]
- 15.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Bussing R, Fernandez M, Harwood M, et al. Parent and teacher SNAP-IV ratings of attention deficit hyperactivity disorder symptoms: psychometric properties and normative ratings from a school district sample. Assessment. 2008;15(3):317–328. doi: 10.1177/1073191107313888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scahill L, Riddle MA, McSwiggin-Hardin M, et al. Children’s Yale-Brown Obsessive Compulsive Scale: reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(6):844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- 18.Allgaier AK, Fruhe B, Pietsch K, Saravo B, Baethmann M, Schulte-Korne G. Is the Children’s Depression Inventory Short version a valid screening tool in pediatric care? A comparison to its full-length version. J Psychosom Res. 2012;73(5):369–374. doi: 10.1016/j.jpsychores.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 19.March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Goodman G, Bass JN, Geenens DL, Popper CW. The MAVRIC-C and MAVRIC-P: a preliminary reliability and validity study. Journal of personality assessment. 2006;86(3):273–290. doi: 10.1207/s15327752jpa8603_04. [DOI] [PubMed] [Google Scholar]
- 21.Steele RG, Legerski JP, Nelson TD, Phipps S. The Anger Expression Scale for Children: initial validation among healthy children and children with cancer. Journal of pediatric psychology. 2009;34(1):51–62. doi: 10.1093/jpepsy/jsn054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance System. http://www.cdc.gov/HealthyYouth/yrbs/index.htm. Accessed July 1, 2015.
- 23.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 24.Gresham FM, Elliott SN. The Social Skills Rating System. Circle Pines, MN: American Guidance Service; 1990. [Google Scholar]
- 25.Constantino JN. The Social Responsiveness Scale. Los Angeles, CA: Western Psychological Services; 2002. [Google Scholar]
- 26.Bukowski WM, Hoza B, Boivin M. Measuring friendship quality during pre- and early adolescence: the development and psychometric properties of the Friendship Qualities Scale. Journal of Social and Personal Relationships. 1994;11(3):471–484. [Google Scholar]
- 27.Piers EV. Manual for the Piers-Harris Children’s Self-Concept Scale. Nashville, TN: Counselor Recordings & Tests; 1969. [Google Scholar]
- 28.Ayers TS. Manual for the Children’s Coping Strategies Checklist & the How I Coped Under Pressure Scale. 2000 http://prc.asu.edu/docs/CCSC-fflCUPS%20%20Manual2.pdf. Accessed July 1, 2015.
- 29.Dunn LM, Dunn LM. Peabody Picture Vocabulary Test. 3rd. Circle Pines, MN: American Guidance Service; 1997. [Google Scholar]
- 30.Gioia G, Isquith P, Guy S, Kenworthy L. The Behavior Rating Inventory of Executive Function. Lutz, FL: Psychological Assessment Resources; 2000. [Google Scholar]
- 31.Landgraf JM, Abetz L, Ware JE. Child Health Questionnaire (CHQ): A user’s manual. Boston, MA: The Health Institute, New England Medical Center; 1996. [Google Scholar]
- 32.Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychological medicine. 1998;28(3):551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 33.Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P. The PedsQL Family Impact Module: preliminary reliability and validity. Health and quality of life outcomes. 2004;2:55. doi: 10.1186/1477-7525-2-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Epstein NB, Bishop DS. McMaster family assessment device. Journal of Family Therapy. 1983;9:171–180. [Google Scholar]
- 35.Shaffer D, Gould MS, Brasic J, et al. A children’s global assessment scale (CGAS) Arch Gen Psychiatry. 1983;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 36.Stiffman AR, Horwitz SM, Hoagwood K, et al. The Service Assessment for Children and Adolescents (SACA): adult and child reports. J Am Acad Child Adolesc Psychiatry. 2000;39(8):1032–1039. doi: 10.1097/00004583-200008000-00019. [DOI] [PubMed] [Google Scholar]
- 37.Freeman RD, Fast DK, Burd L, Kerbeshian J, Robertson MM, Sandor P. An international perspective on Tourette syndrome: selected findings from 3,500 individuals in 22 countries. Dev Med Child Neurol. 2000;42(7):436–447. doi: 10.1017/s0012162200000839. [DOI] [PubMed] [Google Scholar]
- 38.Termine C, Luoni C, Selvini C, et al. Mother-child agreement on behavioral ratings in Tourette Syndrome: a controlled study. J Child Neurol. 2014;29(1):79–83. doi: 10.1177/0883073812470003. [DOI] [PubMed] [Google Scholar]
- 39.Cheung MY, Shahed J, Jankovic J. Malignant Tourette syndrome. Movement disorders : official journal of the Movement Disorder Society. 2007;22(12):1743–1750. doi: 10.1002/mds.21599. [DOI] [PubMed] [Google Scholar]
- 40.Rizzo R, Gulisano M, Cali PV, Curatolo P. Long term clinical course of Tourette syndrome. Brain and Development. 2012;34(8):667–673. doi: 10.1016/j.braindev.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 41.Termine C, Selvini C, Balottin U, Luoni C, Eddy CM, Cavanna AE. Self-, parent-, and teacher-reported behavioral symptoms in youngsters with Tourette syndrome: a case-control study. Eur J Paediatr Neurol. 2011;15(2):95–100. doi: 10.1016/j.ejpn.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 42.Sukhodolsky DG, Landeros-Weisenberger A, Scahill L, Leckman JF, Schultz RT. Neuropsychological functioning in children with Tourette syndrome with and without attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2010;49(11):1155–1164. doi: 10.1016/j.jaac.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kurlan R, McDermott MP, Deeley C, et al. Prevalence of tics in schoolchildren and association with placement in special education. Neurology. 2001;57(8):1383–1388. doi: 10.1212/wnl.57.8.1383. [DOI] [PubMed] [Google Scholar]
- 44.De Los Reyes A, Augenstein TM, Wang M, et al. The validity of the multi-informant approach to assessing child and adolescent mental health. Psychol Bull. 2015;141(4):858–900. doi: 10.1037/a0038498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Storch EA, Hanks CE, Mink JW, et al. Suicidal Thoughts and Behaviors in Children and Adolescents with Chronic Tic Disorders. Depress Anxiety. 2015;32(10):744–753. doi: 10.1002/da.22357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lewin AB, Mink JW, Bitsko RH, et al. Utility of the diagnostic interview schedule for children for assessing Tourette syndrome in children. J Child Adolesc Psychopharmacol. 2014;24(5):275–284. doi: 10.1089/cap.2013.0128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Perou R, Bitsko RH, Blumberg SJ, et al. Mental health surveillance among children–United States, 2005–2011. Morbidity and mortality weekly report. Surveillance summaries (Washington, DC: 2002) 2013;62(Suppl 2):1–35. [PubMed] [Google Scholar]
- 48.Valleni-Basile LA, Garrison CZ, Jackson KL, et al. Frequency of obsessive-compulsive disorder in a community sample of young adolescents. J Am Acad Child Adolesc Psychiatry. 1994;33(6):782–791. doi: 10.1097/00004583-199407000-00002. [DOI] [PubMed] [Google Scholar]
- 49.Robertson MM. Tourette syndrome, associated conditions and the complexities of treatment. Brain. 2000;123(Pt 3):425–462. doi: 10.1093/brain/123.3.425. [DOI] [PubMed] [Google Scholar]
- 50.Specht MW, Woods DW, Piacentini J, et al. Clinical characteristics of children and adolescents with a primary tic disorder. J Dev Phys Disabil. 2011;23(1):15–31. doi: 10.1007/s10882-010-9223-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


