Abstract
Objective
The purpose of this case report was to describe the use of dry needling in conjunction with auricular acupuncture, core exercises, and light aerobic activity for treating chronic tendinopathy of the biceps femoris.
Clinical Features
A 30-year-old white female presented with chronic biceps femoris tendinopathy. The injury had occurred 18 months prior while training for a triathlon. Active stretching of her right biceps femoris while standing with her feet 6 inches apart aggravated the pain at the origin in the right tendon of the biceps femoris at 0 degrees of movement.
Intervention/Outcome
The combination of dry needling and auricular acupuncture with core rehabilitation exercises and light activity was employed. Alleviation of pain with full range of motion was achieved during hip extension, knee flexion, and standing biceps femoris stretch at the 11th, 16th, and 18th treatments. In addition, the patient also reported improvement in her symptoms, including night sweats, insomnia, anxiety, tension, and constipation.
Conclusions
This patient’s symptoms and function improved after 18 treatments of multimodal care. Dry needling employed simultaneously with auricular acupuncture, core exercises, and light activity could be considered a possible strategy for treating chronic tendinopathy.
Key Indexing Terms: Tendinopathy, Acupuncture, Chronic Pain
Introduction
The American Academy of Pain Medicine estimated that 100 million people experience chronic pain.1 In 2011, the treatment of chronic pain cost between $261 billion and $300 billion in the United States.1 According to the Centers for Disease Control, doctors prescribed 259 million pain medications in 2012.2
An array of treatment strategies is available for patients with chronic pain, and these range from conservative therapies, including dry needling, auricular acupuncture, massage, or physical therapy, to more invasive options, such as surgery or injections. Several acupuncture techniques and dry needling have demonstrated efficacy for the treatment of certain types of chronic pain.3, 4, 5 These modalities may be used in combination with exercises to supplement therapy. A case report described treatment of 2 runners with proximal biceps femoris tendinopathy with the use of a combination of eccentric loading and lumbopelvic stabilization exercises and dry needling. The therapy was administered once a week for 8 to 10 weeks, and clinical improvements were noted in pain, tenderness, and range of motion (ROM).6 Another example was the use of dry needling with stretching and strengthening exercises to treat chronic pain of the hip and thigh. Pain and functionality were improved according to the Lower Extremity Functional Scale and the Visual Analog Scale.7 The combination of these therapies was determined to be effective for treating chronic pain.7
The physiological effects of dry needling may manifest locally in tissues. Puncturing the epidermis with these minimally invasive needles has been shown to prevent collagen degradation by inhibiting matrix metalloproteinase activity. Matrix metalloproteinase is involved in the degradation of tissue resulting from damage. Inhibiting the activity of matrix metalloproteinase promotes tissue healing and repair.5 Evidence suggests that dry needling may downregulate the inflammatory cascade. It has the ability to inhibit the expression of nuclear-factor KB, which disrupts the production of arachidonic acid, thus preventing the generation of inflammatory prostaglandins, leukotrienes, and thromboxanes.8 In addition, penetration of the tissue reduces inflammatory mediators tumor necrosis factor-α and interleukin-6.8
Available research data emphasize the potential benefit of dry needling for treating chronic pain. However, most studies utilizing dry needling for treating chronic pain were focused on musculoskeletal conditions. Information pertaining to the effectiveness of dry needling for tendinopathies is limited. In addition, only a minimal amount of information exists to validate the use of auricular therapy for pain management. In a study including 38 patients, true or sham auricular therapy was provided while patients were riding in an ambulance after a hip fracture. In patients receiving true auriculotherapy, less pain was observed in conjunction with lower levels of anxiety and a reduced heart rate, as well as overall satisfaction with treatment.4
The purpose of this case report is to describe the combination of dry needling and auricular acupuncture in conjunction with core exercises and light aerobic activity for the treatment of chronic tendinopathy of the right biceps femoris muscle.
Case Study
History
A 30-year-old white female sought treatment for pain of her right biceps femoris muscle at its origin on the ischium. She noted that the pain had begun 18 months earlier. The onset of the pain was gradual. Pain would start during training, after running, or after cycling for a prolonged period. No trauma was associated with her injury. The pain intensified and eventually became constant during activity. The patient continued her training regimen and competed in the triathlon despite the nociceptive sensations, which were rated at 6 out of 10 on a numeric pain scale (NPS) with any activity requiring movement of the right lower extremity. The NPS ranged from 1 to 10 with 10 being the worst pain. However, the movements that generated the greatest exacerbation of pain were experienced during running and when riding a bicycle, activities that the patient continued to participate in on a weekly basis regardless of the pain. Pain was also noted during stretching of her biceps femoris tendon while standing with forward flexion of the trunk with feet apart and the legs extended and when seated for several hours in a car or at work.
The patient had previously tried several different treatment modalities. Active rehabilitation exercises, which consisted mainly of light cycling, stretching, and postisometric relaxation, in conjunction with ultrasonic therapy over the tendon of the biceps femoris, reduced her pain. However, the patient was not able to receive continuous care because of time constraints. Graston instrument–assisted soft tissue mobilization was applied to the tendon, and relief of pain did occur, but the patient discontinued care because of acute exacerbation of pain for 1 or 2 days after each treatment.
To aid in the selection of the auricular acupuncture points, history taking was performed according to Traditional Chinese Medicine. The patient stated that she typically felt hot but preferred drinks at warm temperatures. She tended to experience constipation frequently and was often hypersomnolent, sleeping for 8 to 10 hours a night, but she woke up feeling unrefreshed and fatigued. She had been experiencing disturbed sleep for over 2 years. She also had night sweats about 3 times a week sporadically in the past 2 years. Her demeanor was tense and anxious, and she felt “wired” most of the time and had for years prior to the onset of her chronic pain. She experienced polydipsia and craved sweet foods. Her pulse was wiry and rapid on the right side and choppy and rapid on the left. Her tongue was swollen and flaccid and had a thick, dry, yellow coating. From the perspective of Traditional Chinese Medicine, the patient was diagnosed with trauma bi syndrome complicated by spleen qi and kidney yin deficiency, resulting in deficiency heat.
Examination
Upon examination, no pain was elicited with unloaded active ROM. The patient had full active ROM of her right hip during extension while prone, which was 20 degrees, and right knee during flexion while prone, which was 130 degrees without pain. However, active stretching of her right biceps femoris while standing with feet 6 inches apart aggravated the pain at the origin in the right tendon of the biceps femoris at 0 degrees of movement. Full ROM with pain was 130 degrees. Nociceptive perception was 6 out of 10 on the NPS for active standing stretch of her biceps femoris. Right-sided hip extension and knee flexion against resistance were isolated to determine the quantity of pain produced by each movement. Resistance to both activities induced pain at 0 degrees upon initiation of movement, and she experienced a pain intensity of 5 out of 10 on the NPS.
Ischial tuberosity bursitis, biceps femoris tendinopathy, and an avulsion fracture were considered as potential differential diagnoses. The Erichsen test generated a minimal amount of pain in her sacroiliac joints bilaterally, and straight leg raise, Hibb, Yeoman, Mennell, and Laseque differentials, all tested on the right lower extremity, failed to reproduce pain. Palpation of the biceps femoris tendon at the ischium, and muscle body revealed hypertonicity and tenderness, as did palpation of the tensor fascia lata (TFL) and the iliotibial (IT) band.
On the basis of the information collected via evaluation and through history, the condition was not consistent with the signs and symptoms typically characteristic of ischial tuberosity bursitis or an avulsion fracture. Ischial tuberosity tendonitis typically manifests as localized pain in the hip or the buttock exacerbated by movement, which was the case in this patient.9 However, in this case, the pain was extending into the muscle body of the biceps femoris, reducing the probability that the pain generator was the bursal sac. Avulsion fractures are rare injuries that produce intense pain often prohibiting movement and are most commonly observed in adolescents, as the secondary ossification center begins to fuse.10 Because of the gradual onset, the extent of pain, and the age of the patient, an avulsion fracture seemed unlikely. The evaluation led to the diagnosis of biceps femoris tendinopathy in conjunction with strain of the TFL and the IT band and sacroiliac dysfunction. The mechanism of injury for a tendinopathy, which is a repetitive loading injury, is consistent with the literature.
Treatment
The treatment strategy employed auricular acupuncture in combination with localized dry needling. Acupuncture treatment and dry needling were provided twice a week for 8 weeks and once a week for 3 additional weeks. The auricular points consisted of the kidney, liver, and spleen points, shen men, and the sympathetic point bilaterally, and the liver yang, ear apex, and hip unilaterally on the right side (Fig 1). Dry needling consisted of 7 to 10 points that were subjectively painful or objectively hypertonic and typically differed for each treatment in the biceps femoris, semitendinosis, TFL and IT band, gluteus medius, and gluteus maximus. The final aspect of the treatment protocol was to have the patient perform core muscle strengthening exercises and participate in light aerobic activity, such as riding a bicycle without resistance, swimming, or using the elliptical machine. Swimming was the preferred activity of the practitioner for the patient to participate in. Her goal was to run 2 miles without pain.
Fig 1.

Auricular acupuncture points chosen for treatment.
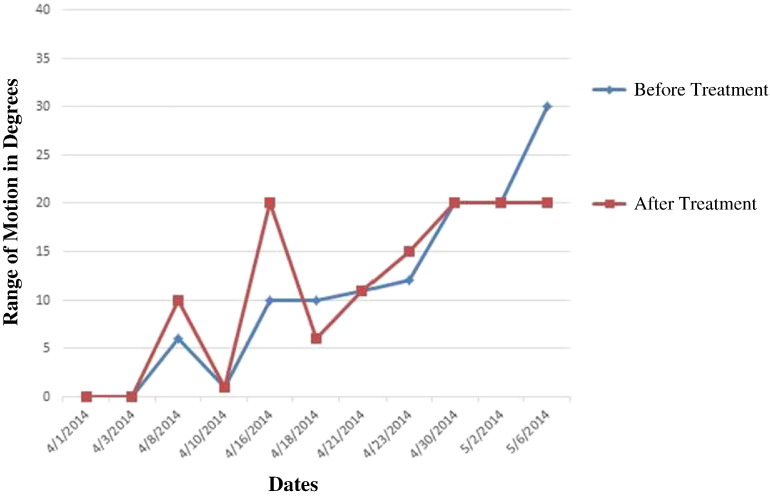
Nociceptive improvements and the ability to perform aerobic activity, consisting of riding a bicycle without resistance, swimming, or using the elliptical machine, were observed throughout the treatment period. After continuous pain during activity for 18 months, pain during resisted hip extension, knee flexion, and active biceps femoris stretch was resolved after 11, 16, and 18 treatments, respectively. The patient’s progress can be observed in Fig 2, Fig 3, Fig 4. At the patient’s 12th-week appointment, resolution of pain had been achieved.
Fig 2.
Range of motion before and after treatment for standing biceps femoris stretch.
Fig 3.
Range of motion before and after treatment for prone hip flexion.
Fig 4.
Range of motion before and after treatement for prone knee flexion.
By the fifth treatment, the patient noticed that she was experiencing less fatigue, her sleep quality had improved, and she woke up feeling more refreshed. Constipation was less frequent, symptoms such as anxiety and general tension were less intense, and her night sweats had ceased.
At approximately 4, 5, and 6 treatments, the pain experienced during resisted hip extension, knee flexion, and active standing stretch of the biceps femoris had decreased to a score of 1 out of 10 on a NPS and remained at that level for almost the entirety of the treatment, with the exception of an acute exacerbation on May 15, 2014.
After 10 treatments, pain experienced with both resisted hip extension and knee flexion were resolved. However, on May 15, 2014, the patient was moving from her house to an apartment, and the exertion created an acute exacerbation of the injury. In spite of this, pain experienced during resisted extension of the hip remained alleviated, whereas pain caused by knee flexion and standing stretch were increased to a 1 out of 10 and 4 out of 10, respectively. Yet after the treatment on May 16, 2014, the pain subsided from a 1 out of 10 and 4 out of 10 to a 0 out of 10 and 1 out of 10 for resisted knee flexion and standing biceps femoris stretch, respectively. After 1 additional treatment, pain with resisted knee flexion was again relieved, whereas pain with standing stretch was sustained at 1 out of 10 and abated at the 18th treatment.
The patient did not experience pain in the 3-week follow-up period, and she did not receive treatment during this time. She was able to run 2 miles, which was her goal and an activity that she was not able to accomplish without pain for a 18 months. The patient was consulted in November 2015 and reported that she was still pain free. The patient also reported that her symptoms, including night sweats, insomnia, anxiety, tension, and constipation, remained improved. The patient gave consent for the publication of this report.
Discussion
There is limited data from research pertaining to the treatment of a tendinopathy of the biceps femoris using dry needling. One published study had analyzed the treatment of biceps femoris tendinopathy utilizing dry needling. The study reported by Jayaseelan et al. consisted of 2 case reports, which were discussed in the introduction section of the paper. The overall results of the case reports by Jayaseelan et al. and this case report have similar findings that demonstrate the effectiveness of dry needling and exercises for the alleviation of symptoms of tendinopathy.6
Several factors distinguish the present case report from others. One factor is that the patient in this report had a tendinopathy for 18 months compared with 4 and 7 months in the reports conducted by Jayaseelan et al.6 This case report also followed the progress of the treatment of the patient throughout the treatment period recording the improvement in ROM and the response of the patient to pain, which did not always improve immediately after treatment. In addition, there are no studies at present that are related to the use of auricular therapy for any type of injury to the biceps femoris, including tendinopathy. Although we cannot assert that auricular therapy made a positive contribution to the outcome observed in this case, it may have acted as an adjunct therapy for reduction of pain and concurrent symptoms.
The biceps femoris muscle possesses a short head and a long head, which originate on the ischial tuberosity and linea aspera and lateral supracondylar line of the femur, respectively.11 The 2 heads join together to form the muscle body, which gives rise to the tendon that inserts onto the fibular head, fibular collateral ligament, and lateral tibial condyle.11 Inflammation of the origin or insertion of the biceps femoris tendon results in tendonitis. Tendonitis is most commonly derived from repetitive loading, causing the partial tears observed in acute injuries.12 Improper management or absence of treatment may result in chronicity of the condition, characterized by degenerative changes to the tendon or its sheath, more appropriately defined as tendinopathy.12
Research suggests that dry needling techniques can help alleviate chronic musculoskeletal pain.7, 13, 14 Our data reinforce this assertion and indicate that dry needling may be effective in the treatment of tendinopathy as well. In our patient, the pain experienced with resisted hip extension and knee flexion and active stretching of the legs was resolved at the end of the treatment period and relief was maintained without treatment for the 3-week follow-up period. In addition, the patient was able to sit for prolonged periods without discomfort, and consultation over a year later revealed that she was still pain free.
This case demonstrates the progressive healing process of chronic tendinopathy with the use of a multimodal approach. The treatment protocol allowed the patient to continue to engage in physical activity. She was encouraged to participate within her limits, especially in swimming, which produces a minimal amount of resistance from the movement. It should be noted that performing light exercise may have delayed the healing process, and yet the activities that the patient engaged in were less strenuous and less likely to exacerbate her condition.
Another important aspect observed in this study was that the pain before and immediately after treatment was sometimes the same or slightly exacerbated. Generally, after a dry needling session, pain had declined. However, as this study demonstrates, that may not always be the case. One of the potential side effects of dry needling is muscle soreness after therapy. In this case, the patient experienced no improvement or reduction in pain-free ROM after treatment about 30% of the time, which constitutes a minority. Regardless of this observation, the patient reported an increase in pain-free ROM the day after treatment and her pain-free ROM gradually increased throughout the treatment period.
It is impossible to determine the extent to which auricular acupuncture assisted in the mitigation of pain in our patient. However, she experienced improvements in her symptoms, including fatigue, sleep quality, anxiety, and night sweats, which all had existed even prior to the onset of her chronic pain. The mitigation of these symptoms occurred after 5 treatments, and the auricular acupuncture points may have assisted in the process. However, psychosomatic symptoms can manifest from pain, and any reduction in pain can reduce the symptoms of insomnia and anxiety.15, 16 Therefore, in our patient, the alleviation of pain from dry needling and exercise may have been responsible for the relief of the symptoms noted previously; yet, the auricular spleen, shen men, and sympathetic points are classically used for relaxation, and their potential effects cannot be diminished, especially since the patient experienced her psychosomatic symptoms prior to the onset of her chronic pain.17
The calming effects of auricular acupuncture were demonstrated in a study utilizing 10 medical students prior to an examination. In this study, all of these students noted improvements in their level of anxiety by almost 20%.18 In another study, investigators found that auricular acupuncture improved sleep quality in war veterans.19 Unfortunately, there are no studies supporting the effectiveness of auricular acupuncture for treating night sweats. However, since in our case the selection of all of the dry needling points was based on subjective or objective symptoms and these points did not correspond to actual acupuncture points with physiologic functions, and since exercise in the absence of hormone therapy did not reduce the incidence of night sweats, auricular acupuncture may be said to have a positive benefit in alleviating these symptoms.20
Another consideration is that the patient’s demeanor was tense, and she felt stressed and anxious most of the day. The combination of these attributes may predispose her to sleep disturbances, which was a symptom that had manifested prior to the onset of her chronic pain. Auricular acupuncture studies have demonstrated a reduction in stress and anxiety and an improvement in general well-being, as well as improvement in the quality sleep.21
In addition, poor sleep quality and anxiety have been established as possible comorbidities of chronic pain.22, 23 Research has demonstrated that chronic pain is associated with sensitization of the central nucleus of the amygdala and is involved in pain-related anxiety. GABAergic inhibition has been observed in chronic pain conditions as well.24 Evidence suggests that treatment with medications for anxiety and insomnia can help alleviate chronic pain.23, 24
Data from this case do not adequately explain the impact of auricular acupuncture on chronic tendinopathy. The alleviation of pain as a result of exercise and dry needling may have accounted for the reduction in psychosomatic symptoms. However, since these symptoms occurred prior to the onset of the patient’s pain and since this study has shown that auricular acupuncture can improve psychosomatic symptoms, it is possible that auricular acupuncture may have acted as an adjunct to dry needling, exercises, and light activity in the therapy for our patient’s pain. Consequently, auricular acupuncture could have contributed to the mitigation of anxiety, tension, and insomnia, which, in turn, may have helped reduce the patient’s chronic pain.
Limitations
The therapy consisted of a combination of therapeutic modalities. Consequently, the combined efficacy of all of the treatments makes it impossible to distinguish between the positive effects of dry needling, auricular acupuncture, and core exercises with light aerobic activity. It is also possible that the patient’s symptoms improved spontaneously, and thus it is not possible to say with certainty that the treatment caused the improvement in this patient. As well, it must be kept in mind that this is a single case report, and that other patients may not necessarily have the same response to treatment.
The direct physiological augmentation of tissue from dry needling and exercise cannot be discounted, and auricular acupuncture may have assisted with pain reduction by decreasing tension and anxiety and improving sleep quality. However, reducing pain by utilizing dry needling, exercises, and light activity could have been responsible for the improvement in these symptoms. It is the opinion of the author that the combination of auricular acupuncture and dry needling in conjunction with core exercises and light activity may be an effective treatment plan for the relief of chronic pain caused by tendinopathy.
Conclusions
This patient responded positively to treatment of chronic tendinopathy with dry needling in combination with auricular acupuncture, core exercises, and light aerobic activity. This therapeutic approach may help to alleviate pain and could be helpful in other cases of tendinopathy. However, with this treatment strategy, the exact impact of each individual treatment modality is difficult to ascertain.
Funding Sources and Potential Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): B.R.M.
Design (planned the methods to generate the results): B.R.M.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): B.R.M.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): B.R.M.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): B.R.M.
Literature search (performed the literature search): B.R.M.
Writing (responsible for writing a substantive part of the manuscript): B.R.M.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): B.R.M.
Practical Applications
-
•
Multimodal care consisting of dry needling in conjunction with core exercises, light activity, and auricular acupuncture was selected to address this case of chronic biceps femoris tendinopathy.
-
•
After a course of 18 weeks of treatment, the patient was able to run 2 miles without pain.
-
•
The treatment strategy also eliminated concurrent symptoms, such as night sweats, insomnia, anxiety, tension, and constipation.
Alt-text: Image 1
References
- 1.CHP Group The cost of chronic pain: how complementary and alternative medicine can provide relief. 2014. http://www.chpgroup.com/wp-content/uploads/2014/12/CHP-WP_CAM-Chronic-Pain_Sls_12.12.2014.pdf Available at: Accessed August 20, 2015.
- 2.Centers for Disease Control and Prevention Opioid painkiller prescribing. 2014. http://www.cdc.gov/vitalsigns/opioid-prescribing/ Available at: Accessed August 20, 2015.
- 3.Llamas-Ramos R, Pecos-Martin D, Gallego-Izquierdo T, Llamas-Ramos I. Comparison of the short-term outcomes between trigger point dry needling and trigger point manual therapy for the management of chronic mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2014;44(11):852–861. doi: 10.2519/jospt.2014.5229. [DOI] [PubMed] [Google Scholar]
- 4.Barker R, Kober A, Hoerauf K, Latzke D. Out-of-hospital auricular acupressure in elder patients with hip fracture: a randomized double-blinded trial. Acad Emerg Med. 2006;13(1):19–23. doi: 10.1197/j.aem.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Kessler M, Barr J, Greenwald R, Lane L, Dines J. Enhancement of Achilles tendon repair mediated by matrix metalloproteinase inhibition via systemic administration of doxycycline. J Orthop Res. 2014;32(4):500–506. doi: 10.1002/jor.22564. [DOI] [PubMed] [Google Scholar]
- 6.Jayaseelan DJ, Moats N, Ricardo CR. Rehabilitation of proximal hamstring tendinopathy utilizing eccentric training, lumbopelvic stabilization and trigger point dry needling: 2 case reports. J Orthop Sports Phys Ther. 2014;44(3):198–205. doi: 10.2519/jospt.2014.4905. [DOI] [PubMed] [Google Scholar]
- 7.Pavkovich R. Effectiveness of dry needling, stretching and strengthening to reduce pain and improve function in subjects with chronic lateral hip and thigh pain: a retrospective case series. Int J Sports Phys Ther. 2015;10(4):540–551. [PMC free article] [PubMed] [Google Scholar]
- 8.Xue Q, Pan H, Huang L, Li N. Effects of acupuncture at ST25 on inflammatory mediators and nuclear factor KB in a rat model of severe acute pancreatitis. Acupunct Med. 2015;33(4):299–304. doi: 10.1136/acupmed-2014-010609. [DOI] [PubMed] [Google Scholar]
- 9.Guanche CA. Hamstring injuries. J Hip Preserv Surg. 2015;2(2):116–122. doi: 10.1093/jhps/hnv026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gidwani S, Jakub J, Bircher M. Avulsion fracture of the ischial tuberosity in adolescents—an easy missed diagnosis. BMJ. 2004;329(7457):99–100. doi: 10.1136/bmj.329.7457.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cramer GD, Darby SA. 3rd ed. Elsevier Mosby; St. Louis, MO: 2014. Basic and Clinical Anatomy of the Spine, Spinal Cord and ANS. [Google Scholar]
- 12.Magee DJ, Zachazewski JE, Quillen WS. Saunders Elsevier; St. Louis, MO: 2007. Scientific Foundations and Principles of Practice in Musculoskeletal Rehabilitation. [Google Scholar]
- 13.Campa-Moran I, Rey-Gudin E, Fernandez-Carnero J. Comparison of dry needling versus orthopedic manual therapy in patients with myofascial chronic neck pain: a single-blind, randomized pilot study. Pain Res Treat. 2015;2015:327307. doi: 10.1155/2015/327307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gerber LH, Shah J, Rosenberger W. Dry needling alters trigger points in upper trapezius muscle and reduces pain in subjects with chronic myofascial pain. PMR. 2015;7(7):711–718. doi: 10.1016/j.pmrj.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Woo AKM. Depression and anxiety in pain. Rev Pain. 2010;4(1):8–12. doi: 10.1177/204946371000400103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agmon M, Armon G. Increased insomnia symptoms predict the onset of back pain among employed adults. PLoS One. 2014;9(8):e103591. doi: 10.1371/journal.pone.0103591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xinnong C. 3rd ed. Foreign Languages Press; Beijing, China: 2009. Chinese Acupuncture and Moxibustion. [Google Scholar]
- 18.Klausenitz C, Hesse T, Hacker H, Hahnenkamp K, Usichenko T. Auricular acupuncture for pre-exam anxiety in medical students: a prospective observational pilot investigation. Acupunct Med. 2016;34(2):90–94. doi: 10.1136/acupmed-2015-010887. [DOI] [PubMed] [Google Scholar]
- 19.King HC, Spence DL, Hickey AH, Sargent P, Elesh R, Connelly CD. Auricular acupuncture for sleep disturbance in veterans with post-traumatic stress disorder: a feasibility study. Mil Med. 2015;180(5):582–590. doi: 10.7205/MILMED-D-14-00451. [DOI] [PubMed] [Google Scholar]
- 20.Daley A, Stokes-Lampard H, Thomas A. The effectiveness of exercise as treatment for vasomotor menopausal symptoms: randomised controlled trial. BJOG. 2015;122(4):565–575. doi: 10.1111/1471-0528.13193. [DOI] [PubMed] [Google Scholar]
- 21.De Valois B, Degun T. Using the NADA protocol to improve wellbeing for prostate cancer survivors: five case studies. EJOM. 2015;8(1):8–18. [Google Scholar]
- 22.Tegethoff M, Belardi A, Stalujanis E, Meinlschmidt G. Comorbidity of mental disorders and chronic pain: chronology of onset in adolescents of a national representative cohort. J Pain. 2015;16(10):1054–1064. doi: 10.1016/j.jpain.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 23.Tang N, Lereya S, Boulton H, Miller MA, Wolke D, Cappuccio FP. Nonpharmacological treatments of insomnia for long-term painful conditions: a systemic review and meta-analysis of patient-reported outcomes in randomized controlled trials. Sleep. 2015;38(11):1751–1764. doi: 10.5665/sleep.5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiang H, Fang D, Kong L. Sensitization of neurons in the central nucleus of the amygdala via the decreased GABAergic inhibition contributes to the development of neuropathic pain-related anxiety-like behaviors in rats. Mol Brain. 2014;7:72. doi: 10.1186/s13041-014-0072-z. [DOI] [PMC free article] [PubMed] [Google Scholar]