Highlights
-
•
We report here a case of a 62 years old patient with charcot arthropathy at her left knee developed one year after spinal stenosis surgery.
-
•
The patient’s knee joint was already beyond the fragmentation and coalescence stages at the moment of physical examination.
-
•
Unsuccessful spinal surgery affected polyneuropathy and migrated the level of the sensorineural loss proximally.
-
•
Elevated level of sensorineural loss resulted in Charcot knee joint in a short period of time.
Keywords: Charcot arthropathy, Charcot knee, Spinal stenosis, Case report
Abstract
Introduction
Charcot arthropathy was first described in 1868 by Jean Martin Charcot as a progressive and destructive joint disease. Diabetes, polyneuropathy, syphilis, syrengomyelia and chronic alcoholism are the main causes of the disease. In this study we present a Charcot arthropathy of the knee seen after unsuccessful spinal stenosis surgery.
Presentation of case
We report here a case of 62 years old patient with Charcot arthropathy at her left knee developed one year after spinal stenosis surgery. The patient’s knee joint was already beyond the fragmentation and coalescence stages at the moment of physical examination. Patient had already been treated for Charcot foot four years before spinal surgery. Because of an unsuccessful spinal surgery, proximal migration of the level of the sensorineural loss negatively affected the polyneuropathy and eventually resulted in Charcot knee joint in a short period of time.
Discussion
However, the etiology of the neuropathic arthropathy hasn’t been well described yet, it is usually seen at patients with diabetes mellitus as a long-term complication with or without polyneuropathy. In addition to the spinal canal pathologies, it is reported that Charcot arthropathy can be seen even after spinal anesthesia procedures.
Conclusion
In conclusion, spinal procedures should be applied with extra caution on the patients with polyneuropathy or any neuropathic arthropathy. It should be remembered that it is possible to encounter unexpected complications such as proximally migration of the level of sensorineural loss and progression of the actual disease after spinal procedures of these patients.
1. Charcot arthropathy of the knee after unsuccessful spinal stenosis surgery
Charcot arthropathy was first described in 1868 by Jean Martin Charcot as a progressive and destructive joint disease [1], [8]. Although in the years described neurosyphilis was the most frequent cause, at the present diabetes mellitus is the most common etiology for this disease [9]. Incidence among the patients with diabetes is 7.5% and the disease most commonly involves the feet and ankles [2]. It is known that the 6% of the Charcot arthropathy in diabetes affects knee joint [3], [10]. Its pathophysiology is explained with sensorineural, autonomic and motor dysfunction leading to instability, osteopenia, and micro trauma [1]. Polyneuropathy, syphilis, syrengomyelia and chronic alcoholism are the main causes of the disease in the literature [4]. However, Charcot arthropathy can be seen after some spinal cord pathologies, there is no literature known as Charcot knee arthropathy as a complication of spinal stenosis surgery [4].
In this study we present a Charcot arthropathy of the knee seen after a spinal stenosis surgery. This work has been reported in line with the SCARE criteria [15].
2. Case
A 62 years old women had a spinal stenosis surgery at 2010 with a posterior instrumentation (Figs. 1, 2 ). At the 1 year follow up an MRI of the patient’s left knee showed inflammatory changes compatible with a Charcot knee. Patient had been out of follow up for 4 years and did not receive any treatment. When patient first presented there were an increased varus and valgus instability with hyperextension laxity in her left knee joint. X-rays also showed excessive bone loss at the medial plateau of the tibia (Figs. 3, 4 ). There were no sings of oedema, swelling and erythema on inspection. According to the patient’s medical history it was obvious in hindsight that the patient had been Charcot arthropathy and the disease was already beyond the fragmentation and coalescence stages at that moment. Joint was at reconstruction phase at the time of diagnosis. An immediate EMG study showed us the L3-S1 roots had a severe chronic polyneuropathy with total sensorineural loss.
Fig. 1.
Lateral X-ray after posterior instrumentation.
Fig. 2.
Sagittal MRI image after posterior instrumentation.
Fig. 3.
Anteroposterior X-ray of the knee joint shows the excessive bone loss.
Fig. 4.
Lateral X-ray of the knee joint at the end stage of the disease.
Patient also had an ulcerative wound at the left heel which diagnosed as Charcot foot because of the polyneuropathy and that wound was treated at 2006 with surgery. Based on the medical history, orthopaedic and neurologic examination and the radiologic sings we believe that this patient developed a neuropathic arthropathy at her left knee after a spinal stenosis surgery.
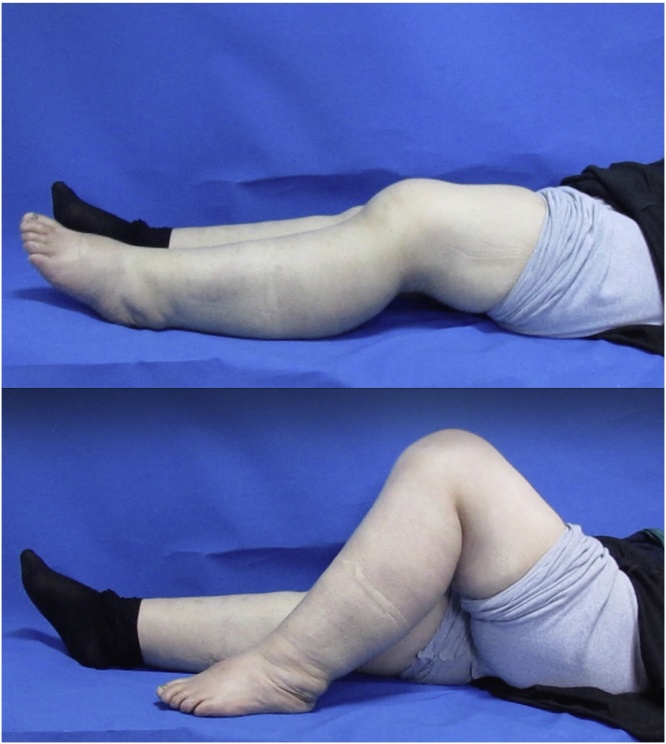
We preferred conservative treatment for the patient and suggested a custom made hinged knee brace for a daily use [12], [5], [6] (Fig. 5). In routine follow up we have seen that the patient was walking comfortably with crutches while using the brace [7]. Patient was consulted with the physical therapy and rehabilitation department for the use of bisphosphonates and medical treatment as well [11].
Fig. 5.
Clinic and functional pictures of the patient, at present.
3. Discussion
The etiology of the neuropathic arthropathy has not been well described yet. It is usually seen at patients with diabetes mellitus as a long-term complication with or without polyneuropathy [9]. Furthermore the literature shows us that after spinal canal pathology or even after spinal anaesthesia procedure Charcot arthropathy can be seen [4]. Charcot arthropathy of the knee joint also reported as a hereditary neuroarthropathy [13]. Incidence of the involvement of the knee is less than the distal joints such as foot and ankle [14]. Our patient had a polyneuropathy. After an unsuccessful spinal surgery, the level of the sensorineural loss moved proximally. Proximal migration of the polyneuropathy negatively affected a healthy knee joint. In conclusion we suggest that after spinal procedures Charcot arthropathy is a possible complication.
For that reason, spinal procedures should be applied with extra caution on the patients with polyneuropathy or any neuropathic arthropathy. It should be remembered that it is possible to encounter unexpected complications such as proximally migration of the level of sensorineural loss and progression of the actual disease after spinal procedures of these patients.
Conflicts of interest
The authors have none to declare.
Funding sources
The authors have none to declare.
Ethical approval
Ethics committee application has not been made because of the article.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Authors contribution
All authors contributed to this work.
Guarantor
The Guarantor is Dr. Melih Cıvan.
Contributor Information
Melih Cıvan, Email: melihcivan@gmail.com.
Önder Yazıcıoğlu, Email: oyazici@istanbul.edu.tr.
Mehmet Çakmak, Email: profcakmak@gmail.com.
Turgut Akgül, Email: trgtakgul@gmail.com.
References
- 1.Eichenholtz S.N. Charles C Thomas; Springfield: 1966. Charcot Joints. [Google Scholar]
- 2.Kucera Tomas, Urban Karel, Sponer Pavel. Charcot arthropathy of the knee. A case- based review. Clin. Rheumatol. 2011;30:425–428. doi: 10.1007/s10067-010-1617-x. [DOI] [PubMed] [Google Scholar]
- 3.Hideaki N., Kenzo U., Hisashi O., Takafumi Y., Erisa M., Yasuo K., Ryuichiro S., Shigeru K., Norbert O., Hisatoshi B. Rapidly progressive neuropathic arthropathy of the knee in possible association with a huge extruded cervical intervertebral disc herniation. Rheumatol. Int. 2010;30:811–815. doi: 10.1007/s00296-009-0999-z. [DOI] [PubMed] [Google Scholar]
- 4.Paliwal Vimal K., Sing Prabhat, Rahi S.K., Agarwal Vikas, Gupta Rakesh K. Charcot knee secondary to lumbar spinal cord syringomyelia complication of spinal anaesthesia. J. Clin. Rheumatol. 2012;18(June (4)):207–208. doi: 10.1097/RHU.0b013e3182598915. [DOI] [PubMed] [Google Scholar]
- 5.Parvizi J., Mars J., Morrey B.F. Total knee arthroplasty for neuropathic (Charcot) joints. Clin. Orthop. Relat. Res. 2003;416:145–150. doi: 10.1097/01.blo.0000081937.75404.ed. [DOI] [PubMed] [Google Scholar]
- 6.Kim Y.H., Kim J.S., Oh S.W. Total knee arthroplasty in neuropathic arthropathy. J. Bone Joint Surg. Br. 2002;84:216–219. doi: 10.1302/0301-620x.84b2.12312. [DOI] [PubMed] [Google Scholar]
- 7.Illgner U., Netten J., Droste C., Postema K., Meiners T., Wetz H. Diabetic Charcot neuroarthropathy of the knee: conservative treatment options as alternatives to surgery. Diabetes Care. 2014;37:129–130. doi: 10.2337/dc13-3045. [DOI] [PubMed] [Google Scholar]
- 8.Charcot J.M. Archives de Neurologie. 1883;6:305–319. [Google Scholar]
- 9.Wukich D.K., Sung W., Wipf S.A., Armstrong D.G. Diabet. Med. 2011;28(2):195–198. doi: 10.1111/j.1464-5491.2010.03141.x. [DOI] [PubMed] [Google Scholar]
- 10.Sinha S., Munichoodappa C.S., Kozak G.P. Medicine. 1972;51(3):191–210. doi: 10.1097/00005792-197205000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Al-Nammari S., Theologis T., Sabokbar A. A surgeon’s guide to advances in the pharmacological management of acute Charcot neuroarthropathy. Foot Ankle Surg. 2013;19:212–217. doi: 10.1016/j.fas.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 12.Ranawat C.S., Shine J.J. Duo-condylar total knee arthroplasty. Clin. Orthop. 1973;94:185–195. doi: 10.1097/00003086-197307000-00023. [DOI] [PubMed] [Google Scholar]
- 13.Meyer S. The pathogenesis of diabetic charcot joints. Iowa Orthop. J. 1992;12:63–70. [Google Scholar]
- 14.Kaynak G., Birsel O., Güven M.F., Öğüt T. An overview of the Charcot foot pathophysiology. Diabet. Foot Ankle. 2013;4:10. doi: 10.3402/dfa.v4i0.21117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]