Summary
Background
An adequate amount of prepaid resources for health is important to ensure access to health services and for the pursuit of universal health coverage. Previous studies on global health financing have described the relationship between economic development and health financing. In this study, we further explore global health financing trends and examine how the sources of funds used, types of services purchased, and development assistance for health disbursed change with economic development. We also identify countries that deviate from the trends.
Methods
We estimated national health spending by type of care and by source, including development assistance for health, based on a diverse set of data including programme reports, budget data, national estimates, and 964 National Health Accounts. These data represent health spending for 184 countries from 1995 through 2014. We converted these data into a common inflation-adjusted and purchasing power-adjusted currency, and used non-linear regression methods to model the relationship between health financing, time, and economic development.
Findings
Between 1995 and 2014, economic development was positively associated with total health spending and a shift away from a reliance on development assistance and out-of-pocket (OOP) towards government spending. The largest absolute increase in spending was in high-income countries, which increased to purchasing power-adjusted $5221 per capita based on an annual growth rate of 3·0%. The largest health spending growth rates were in upper-middle-income (5·9) and lower-middle-income groups (5·0), which both increased spending at more than 5% per year, and spent $914 and $267 per capita in 2014, respectively. Spending in low-income countries grew nearly as fast, at 4·6%, and health spending increased from $51 to $120 per capita. In 2014, 59·2% of all health spending was financed by the government, although in low-income and lower-middle-income countries, 29·1% and 58·0% of spending was OOP spending and 35·7% and 3·0% of spending was development assistance. Recent growth in development assistance for health has been tepid; between 2010 and 2016, it grew annually at 1·8%, and reached US$37·6 billion in 2016. Nonetheless, there is a great deal of variation revolving around these averages. 29 countries spend at least 50% more than expected per capita, based on their level of economic development alone, whereas 11 countries spend less than 50% their expected amount.
Interpretation
Health spending remains disparate, with low-income and lower-middle-income countries increasing spending in absolute terms the least, and relying heavily on OOP spending and development assistance. Moreover, tremendous variation shows that neither time nor economic development guarantee adequate prepaid health resources, which are vital for the pursuit of universal health coverage.
Funding
The Bill & Melinda Gates Foundation.
Introduction
Substantial disparities characterise the amount of resources spent on health globally.1 In many low-income countries, per capita spending remains less than $100 per year, and inadequate resources prevent people from accessing quality health care. By contrast, in many high-income countries, annual health spending has ballooned to higher than $5000 per capita. These divergent contexts are reflected in the thrust of public policy, with calls to rein in health spending growth in high-income countries, and appeals to mobilise more resources for health in low-income and middle-income countries.2, 3, 4, 5, 6, 7, 8
Notwithstanding these disparities, certain trends underpin health spending worldwide.9, 10, 11 The health financing transition is defined by changes in the level and composition of health spending. These changes are associated with economic development. More specifically, the health financing transition has two key features, observed across countries and across time: (1) as countries experience economic development, they spend more per capita on health; and (2) less of that spending is out-of-pocket (OOP).12, 13, 14 It has been theorised that both features of the health financing transition are driven by per capita income growth, technological advances, maturation of health financing system, greater government fiscal capacity, introduction of social health insurance, and population ageing, all associated with socioeconomic development. The first feature—increasing spending on health per capita—is important because it leads to more resources for health, which can lead to improved access to higher quality health services. The second feature—the declining share of health spending that is OOP—is important because high OOP payments can deter use of health-care services, which can lead to poor health outcomes and medical impoverishment.15, 16, 17, 18, 19, 20, 21
Research in context.
Evidence before this study
Understanding how national health spending in total, and disaggregated into government, prepaid private, out-of-pocket (OOP), and development assistance for health, is associated with economic development is important for assessing progress and determining fiscally appropriate financing targets. Deviation from these trends can be used to identify opportunities for increased focus and attention from development partners and domestic governments. Adequate health financing that is prepaid, rather than OOP, is crucial for the pursuit of universal health coverage.
Several studies have tracked national health spending patterns over time. Typically, these studies are descriptive (cross-sectional and time series) and focus on trends in growth in health spending and its determinants. A key piece of research on this topic was completed by Fan and Savedoff. They explored spending in 126 countries spanning 15 years and identified key patterns in how growth in health spending evolves over time, especially in relation to per capita income. They used the term “health financing transition” to characterise two observed patterns: as income rises, (1) health spending per capita tends to rise, and (2) the share of health payments that are OOP tends to decrease.
Added value of this study
This research expands what is known about the health financing transition and the availability of prepaid health resources in three distinct ways. First, this research provides a more comprehensive perspective on the health financing patterns associated with economic development. Previously our research on this topic has focused on development assistance for health. In this research we combine these data with domestic spending estimates to generate a panel of data spanning 20 years and 184 countries. Along with development assistance for health, this research measures government health spending that is domestically generated, prepaid private health spending, and out-of-pocket health spending. Second, we use non-linear methods to assess important non-linear variation across time and levels of economic development. These trends allow us to explore how health spending from development partners fit with the health financing transition framework. This addition is crucial to explore the effect that the transition away from a reliance on development assistance for health has on health-system financing. Relative to previous research, this work extends the analysis to use more comprehensive data that focuses on the source of the health spending, uses robust non-linear estimation methods, and highlights both trends and deviations from those trends for 184 countries. Third, we explore how the types of health-related goods and services purchased by each country evolve with economic development.
Implications of all the available evidence
The findings from this study expand the understanding of the health financing transition. We measure health financing trends associated with economic development: health spending increases exponentially, while the share of total health spending that is OOP declines, especially at the highest income levels. The share of financing from development assistance for health, on average, declines before government spending becomes the dominant funding source, leaving a period in the transition where countries often rely heavily on both OOP and government spending. The share of spending on each type of goods and service is relatively stable across the development spectrum with substantive emergence of long-term care spending at the highest income levels. Despite the health financing trends associated with economic development, tremendous variation exists and suggests that neither time nor economic development guarantee adequate prepaid health resources will be available. Deviations from the health spending trends can identify health financing opportunities. Furthermore, in view of the complexity of translating growth into health spending, proactive steps will be needed in some places to mobilise adequate prepaid resources for the pursuit of universal health coverage.
Changes in a country's reliance on development assistance for health is also related to economic development. Development assistance for health tends to be phased out as countries develop economically, especially when measured as a share of total health spending. Eligibility criteria set by donors, such as the Global Fund for AIDS, Tuberculosis, and Malaria (the Global Fund), the World Bank's International Development Association, and Gavi, the Vaccine Alliance (Gavi), are linked to gross national income thresholds.22 At a certain level of economic development, countries become ineligible to receive development assistance for health.
To explore the global health financing landscape and the patterns described by the health financing transition framework, this study examines spending on health in 184 countries over a 20-year period, 1995 to 2014. These data capture the distinct health spending trends of low-income, middle-income, and high-income countries. We track total health spending and health spending disaggregated by the source of the funds—spending originating from governments, development partners, OOP, and prepaid private pools, such as private insurance. To highlight changes in the mix of goods and services purchased, health spending has also been disaggregated by type of goods and services purchased, such as inpatient, outpatient, and pharmaceutical spending. Our analyses focus on patterns associated with economic development and, importantly, highlight deviations from observed trends. We also assess how development assistance for health is disbursed globally and discuss how development assistance for health is a part of and affects the health financing transition. These data span from 1990 to 2016, and highlight the sources and development agencies that provide development assistance for health. Primary health focus areas and recipient regions targeted by the development assistance is also tracked to show who is receiving development assistance for health and what focus areas are being prioritised.
Methods
Total health spending and government, prepaid private, and out-of-pocket health spending
Health spending stems from four sources: the government, which includes general government budgets and social health insurance; prepaid private spending, which includes private insurance and non-governmental organisation spending; OOP payments; and development assistance for health. The sum of these sources make up total health-care spending. Government, prepaid private, and OOP spending data were extracted from the WHO Global Health Observatory. These data measure the sum of all outlays for health maintenance, restoration, or enhancement paid for in cash or supplied in kind.23 This excludes indirect health spending, such as lost wages due to illness or transportation costs; spending on informal care, such as care provided by a family member; spending on traditional healers; and illegal so-called black market or under the table transactions, such as bribes. Spending estimates were extracted in national currency units and divided by gross domestic product (GDP), also reported in national currency units and reported by WHO. This fraction was multiplied by GDP per capita reported in inflation-adjusted 2015 PPP $.24
WHO data tracks spending by agent, such that it is unclear if government and prepaid private spending were sourced domestically. To differentiate between domestically and internationally financed spending, development assistance for health provided to the government was removed from WHO's government spending estimates and development assistance for health provided to non-government providers or organisations was removed from WHO's prepaid private estimates.25
For the 184 countries, between 1995 and 2014, 1·7%, 14·8%, and 1·7% of the government, prepaid private, and OOP health spending estimates were missing, respectively. These estimates were imputed in R using Amelia II: A program for missing data (version 1·7·4), and more information about these methods is provided in the appendix (p 19).26 The result of this approach is four mutually exclusive, collectively exhaustive spending estimates by source and time—government as source, prepaid private (excluding donor financing), OOP health spending, and development assistance for health. These four series were summed to form annual estimates of total health spending for each of the 184 countries, from 1995 through 2014.
Development assistance for health
Development assistance for health is the financial and in-kind resources transferred from development agencies to low-income and middle-income countries with the primary purpose of maintaining or improving health.27 Many of the methods used to estimate development assistance for health have been used and published previously, although the input data and some methods have been updated and improved for this study.25, 27, 28 These estimates are based on data from all publicly available databases tracking development assistance, including project-level records from the Organisation for Economic Co-operation and Development (OECD) and other development agencies, such as the World Bank, the Global Fund, Gavi, and the Bill & Melinda Gates Foundation. In addition, audited budget statements and annual reports are used to estimate development assistance for health through 2016. When disbursement data were not available, commitment data are adjusted to reflect disbursements. Disbursements are tracked comprehensively from source to disbursing agency, also known as the disbursing channel, to recipient to avoid double counting associated with development agencies transferring resources among themselves. These data are disaggregated based on the source of development assistance for health, disbursing channel, health focus area, and country recipient. Development assistance for health is disaggregated by health focus area—newborn and child health, maternal health, HIV/AIDS, malaria, tuberculosis, non-communicable diseases, other infectious diseases, health system strengthening, which includes discretionary grants to the health sector, and other and unallocable—and tracks disbursements from 1990 to 2016. Other includes projects that are for health projects that do not fit into any of the other health focus areas, while unallocable development assistance for health is that that does not have sufficient data to be disaggregated by health focus area. A more thorough presentation of these methods and explanation on how these methods defer from past research is provided in the appendix (p 41).
The Institute for Health Metrics and Evaluation's (IHME) development assistance for health database further disaggregates funds based on whether they are expected to be channelled to the recipient country's government, or are provided to non-governmental providers or organisations.29 Development assistance for health estimates are reported in 2015 US$, and were converted into 2015 purchasing-power-adjusted US$ to reflect the purchasing power of development assistance for health in the recipient country. Purchasing power parity exchange rates were based on data from the International Monetary Fund (IMF), World Bank, and WHO.
Health spending by types of goods and services
Total health spending was also disaggregated by type of goods and services, such as inpatient or outpatient care. For this purpose, we collected all available National Health Account (NHA) reports. NHAs track health spending using an agreed upon accounting framework developed by the OECD, WHO, and Eurostat. The standards were first codified in 2001, but then updated in 2011 to what is now known as the System of Health Accounts (SHA) 2011.30, 31 A systematic review located, extracted, and published data from 872 reports spanning 1996 to 2010.32 We added to this review by searching WHO, OECD, and Eurostat databases, and Google for search terms “National Health Account” and “System of Health Account”, which identified 178 additional NHAs. The newly collected reports are primarily from more recent years.
We mapped estimates based on NHA 2001 standards to SHA 2011 with methods described in the appendix (p 20). Because the NHA 2001 and SHA 2011 standards for tracking spending on some preventive health services were irreconcilable, we include only the spending on immunisations and early disease detection. Excluded categories contain spending on education and counselling programmes, epidemiological surveillance, and disaster preparedness.
Of the 1050 NHA reports identified for this research, only 964 NHA reports included the necessary data (specific information about the exclusion criterion used to determine the set of used NHAs outlined in the appendix [p 20]). These 964 reports span 108 countries and range from 1995 to 2014. From these, we extracted total and government health spending by type of goods and services, and aggregated spending into eight categories: inpatient curative and rehabilitative care; day and outpatient curative and rehabilitative care; long-term care; ancillary services; medical goods, which includes pharmaceuticals; governance and health-system and financing administration; immunisation and early disease detection programmes; and other care. Estimates by type of service were generated as a share of both total health spending and total government health spending. Other care is a residual category that includes all health spending not included in the other categories.
Gross domestic product data
GDP data spanning 1995 to 2015 were based on data collected from the International Monetary Fund, World Bank, the UN, the Maddison Project, and Penn World Tables database.33, 34, 35, 36 These data were combined using regression methods and previously developed for producing a complete GDP time series.24 GDP data were reported in inflation-adjusted 2015 PPP $.
Spending by income groups and geographic regions
We report estimates aggregated by FY2016 World Bank income groups and Global Burden of Disease (GBD) super regions.37, 38 World Bank income groups are four mutually exclusive categories assigned by the World Bank and based on gross national income. GBD super regions are seven mutually exclusive categories based on geography and cause of death patterns. Spending estimates were constructed to reflect the group or region as a whole. For example, the group's health spending per capita is the group's total spending divided by total population. Similarly, the group's government health spending as a share of total spending was the group's total government spending divided by the group's total health spending.
Statistical analyses
We completed three primary analyses. For all three analyses, we used multivariate penalised spline regression to allow for flexible and non-linear model fit across all 184 countries and 20 years of data.39 First, we regressed the natural log of total health spending per capita on the natural log of GDP per capita and time. Second, we regressed four health spending by source fractions—development assistance for health and government, prepaid private, and OOP health spending—on GDP per capita and time. Third, we regressed the eight health spending by type of goods and services fractions—inpatient curative and rehabilitative care, day and outpatient curative and rehabilitative care, long-term care, ancillary services, medical goods, governance and health-system and financing administration, immunisation and early disease detection programmes, and other care—on GDP per capita and time. For the second and third analyses, the spending fractions (by source and by type) were each measured as a share of total health spending and centre log-ratio transformed, while GDP per capita was natural log transformed.40 To estimate uncertainty, the underlying data was bootstrapped 1000 times, and all regressions were completed independently on each of the 1000 bootstrap samples.41, 42 Robustness checks included in the appendix (p 29) reinforce our qualitative conclusions, and use subsets of our data and also rely on the Socio-demographic Index and the Human Development Index, both of which track additional dimensions related to socioeconomic development, rather than simply GDP per capita which tracks economic development.
To measure countries' 2014 health spending relative to the expected value as determined by the fitted trend, we extracted the estimated country-year and year-specific residual (or error) from the regression analyses. The residuals measure the difference between the actual 2014 spending levels and the expected 2014 spending levels predicted by the model relative only to the country's GDP per capita. The residual measures the effect of country characteristics not included in the model, such as health burden, health-system policies, prices, and society's willingness to spend on health.
In addition to this, we tested whether health spending per capita grew exponentially with economic development. To test these we used ordinary least squares to regress the natural log of health spending per capita on the natural log of GDP per capita. More details on all estimation are included in the appendix (p 4).
Role of the funding source
The funder of this study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to the data in the study and JLD and CJLM had final responsibility for the decision to submit for publication.
Results
Health spending in 2014
Table 1 shows that in 2014 health spending per capita across all countries was $1279. This spending was concentrated in high-income countries, and ranged from $33 in Somalia to $9237 in the USA. These extremes, which are reported using 2015 PPP $ to account for inflation and different prices across countries, highlight the tremendous variation in how much is spent on health around the world. Disparate spending levels also exist within World Bank income groups. In 2014, health spending across low-income countries was $120 per capita, but range from $33 (Somalia) to $347 (Uganda). Spending per capita across lower-middle-income countries was $267, but ranged from $92 (Bangladesh) to $791 (Tunisia), while spending per capita in upper-middle-income countries was $914, but ranged from $228 (Angola) to $1980 (Maldives). Finally, health spending per capita was $5221 in high-income countries, and ranged from $853 (Seychelles) to $9237 (USA). Geographic variation is also present when examined using GBD super regions.
Table 1.
Health spending by source, 2014
| Total health spending per capita ($) | Total health expenditure per gross domestic product (%) | Domestic government health spending per total health spending (%) | Prepaid private spending per total health spending (%) | Out-of-pocket spending per total health spending (%) | Development assistance for health per total health spending (%) | Annualised rate of change in total health spending per capita, 1995–2014 (%) | |
|---|---|---|---|---|---|---|---|
| Global | |||||||
| Total | 1279 (33 to 9237) | 8·3% (1·9 to 39·3) | 59·2% (0·0 to 95·5) | 17·4% (0·0 to 64·8) | 22·8% (2·4 to 76·6) | 0·6% (0·0 to 92·3) | 3·3% (−3·0 to 19·7) |
| Income group | |||||||
| High income | 5221 (853 to 9237) | 11·7% (2·2 to 16·6) | 63·4% (42·4 to 93·9) | 22·7% (0·0 to 38·8) | 13·9% (2·4 to 55·7) | 0·0% (0·0 to 0·1) | 3·0% (−1·1 to 7·6) |
| Upper-middle income | 914 (228 to 1980) | 5·9% (2·3 to 17·2) | 57·2% (19·4 to 95·5) | 8·7% (0·0 to 44·2) | 33·8% (4·4 to 74·2) | 0·3% (0·0 to 23·2) | 5·9% (−3·0 to 17·0) |
| Lower-middle income | 267 (92 to 791) | 4·3% (1·9 to 16·1) | 35·9% (0·0 to 87·2) | 3·1% (0·0 to 10·2) | 58·0% (2·8 to 76·6) | 3·0% (0·2 to 92·3) | 5·0% (−1·4 to 9·4) |
| Low income | 120 (33 to 347) | 7·3% (3·6 to 39·3) | 18·0% (0·0 to 48·5) | 17·2% (0·0 to 64·8) | 29·1% (7·8 to 54·1) | 35·7% (12·9 to 92·2) | 4·6% (−3·0 to 19·7) |
| GBD super region | |||||||
| Central Europe, eastern Europe, and central Asia | 1364 (200 to 2845) | 6·7% (2·3 to 10·3) | 58·5% (19·4 to 84·8) | 2·8% (0·0 to 18·9) | 38·5% (11·2 to 74·2) | 0·3% (0·0 to 13·7) | 4·9% (1·4–9·6) |
| Global Burden of Disease high income | 5460 (1322 to 9237) | 12·3% (2·6 to 16·6) | 62·8 %(42·4 to 93·9) | 23·4% (0·0 to 38·8) | 13·8% (5·3 to 55·7) | 0·0% (0·0 to 0·0) | 2·9%(−0·6 to 7·6) |
| Latin America and Caribbean | 1082 (154 to 1996) | 7·3% (4·3 to 11·1) | 51·6% (0·0 to 95·5) | 16·1% (0·0 to 29·6) | 31·7% (4·4 to 64·3) | 0·7% (0·0 to 40·8) | 3·3% (−1·8 to 8·5) |
| North Africa and Middle East | 870 (159 to 2663) | 5·2% (2·2 to 9·7) | 60·1% (14·3 to 91·8) | 4·3% (0·0 to 14·9) | 34·9% (5·9 to 76·6) | 0·7% (0·0 to 30·9) | 4·9% (−1·4 to 9·0) |
| South Asia | 223 (92 to 279) | 4·2% (2·7 to 5·8) | 31·0% (22·7 to 70·7) | 2·6% (0·0 to 6·1) | 64·7% (25·1 to 65·6) | 1·7% (0·7 to 17·8) | 5·8% (2·0 to 6·4) |
| Southeast Asia, east Asia, and Oceania | 588 (105 to 1980) | 4·8% (1·9 to 17·2) | 58·6% (0·0 to 93·6) | 5·2% (0·0 to 10·2) | 35·7% (2·4 to 65·4) | 0·5% (0·0 to 92·3) | 8·9% (−3·0 to 11·0) |
| Sub-Saharan Africa | 218 (33 to 1411) | 5·9% (3·0 to 39·3) | 33·5% (0·0 to 80·7) | 20·8% (0·0 to 64·8) | 29·2% (5·1 to 70·1) | 16·6% (0·1 to 92·2) | 3·2% (−3·0 to 19·7) |
| Country | |||||||
| Afghanistan | 159 | 9·7% | 15·0% | 0·0% | 54·1% | 30·9% | 5·5% |
| Albania | 642 | 5·9% | 48·3% | 0·0% | 49·8% | 1·9% | 4·2% |
| Algeria | 1004 | 7·2% | 72·7% | 0·7% | 26·5% | 0·0% | 6·0% |
| Andorra | 5723 | 8·1% | 78·0% | 6·0% | 15·9% | 0·0% | 2·5% |
| Angola | 228 | 3·0% | 70·0% | 0·0% | 26·6% | 3·4% | 1·5%% |
| Antigua and Barbuda | 1213 | 5·5% | 68·3% | 8·0% | 23·7% | 0·0% | 3·0% |
| Argentina | 1322 | 4·8% | 55·8% | 13·2% | 30·9% | 0·0% | –0·6% |
| Armenia | 395 | 4·5% | 40·6% | 3·0% | 52·8% | 3·6% | 4·9% |
| Australia | 4032 | 9·0% | 70·4% | 9·9% | 19·7% | 0·0% | 3·3% |
| Austria | 5471 | 11·2% | 78·0% | 5·8% | 16·2% | 0·0% | 2·6% |
| Azerbaijan | 1030 | 5·9% | 20·9% | 4·3% | 74·2% | 0·6% | 9·6% |
| Bahrain | 2258 | 4·8% | 65·3% | 10·6% | 24·1% | 0·0% | 2·2% |
| Bangladesh | 92 | 2·9% | 22·7% | 0·0% | 65·6% | 11·7% | 3·2% |
| Barbados | 1116 | 7·5% | 63·5% | 6·6% | 29·9% | 0·0% | 2·0% |
| Belarus | 1093 | 5·6% | 66·9% | 0·1% | 32·6% | 0·4% | 4·0% |
| Belgium | 4751 | 10·6% | 77·9% | 4·3% | 17·8% | 0·0% | 3·3% |
| Belize | 503 | 5·8% | 64·7% | 9·5% | 23·0% | 2·9% | 2·8% |
| Benin | 105 | 5·1% | 35·0% | 0·0% | 35·5% | 29·6% | 2·0% |
| Bhutan | 279 | 3·6% | 70·7% | 0·0% | 25·1% | 4·2% | 4·0% |
| Bolivia | 404 | 6·3% | 70·2% | 3·4% | 23·1% | 3·3% | 5·2% |
| Bosnia and Herzegovina | 992 | 9·5% | 70·0% | 0·0% | 28·0% | 2·0% | 8·8% |
| Botswana | 903 | 5·5% | 49·9% | 35·0% | 5·1% | 10·0% | 5·1% |
| Brazil | 1357 | 8·3% | 45·9% | 28·5% | 25·5% | 0·1% | 3·3% |
| Brunei | 1811 | 2·6% | 93·9% | 0·1% | 6·0% | 0·0% | –0·4% |
| Bulgaria | 1490 | 8·4% | 54·7% | 0·9% | 44·3% | 0·2% | 6·3% |
| Burkina Faso | 83 | 5·0% | 35·8% | 0·0% | 38·6% | 25·6% | 2·8% |
| Burundi | 65 | 8·3% | 23·7% | 0·0% | 19·1% | 57·2% | 3·2% |
| Cambodia | 209 | 6·4% | 14·2% | 0·0% | 65·4% | 20·4% | 4·1% |
| Cameroon | 116 | 4·0% | 17·0% | 3·5% | 68·5% | 10·9% | 1·3% |
| Canada | 4576 | 10·3% | 72·1% | 14·1% | 13·8% | 0·0% | 2·4% |
| Cape Verde | 318 | 4·8% | 58·4% | 0·1% | 22·2% | 19·2% | 4·1% |
| Central African Republic | 35 | 5·7% | 9·0% | 0·0% | 34·2% | 56·7% | –1·3% |
| Chad | 89 | 3·8% | 48·5% | 1·3% | 37·2% | 12·9% | 0·6% |
| Chile | 1780 | 7·8% | 49·5% | 19·0% | 31·5% | 0·0% | 4·1% |
| China | 697 | 5·1% | 60·3% | 5·0% | 34·6% | 0·0% | 10·4% |
| Colombia | 975 | 7·2% | 71·9% | 9·5% | 15·3% | 3·2% | 2·7% |
| Comoros | 111 | 7·1% | 22·1% | 20·1% | 42·8% | 14·9% | –1·2% |
| Costa Rica | 1418 | 9·3% | 73·1% | 1·8% | 25·0% | 0·0% | 4·6% |
| Côte d'Ivoire | 179 | 5·3% | 22·1% | 8·2% | 54·6% | 15·1% | 0·2% |
| Croatia | 1734 | 7·8% | 81·9% | 6·9% | 11·2% | 0·0% | 3·5% |
| Cuba | 1706 | 11·1% | 95·5% | 0·0% | 4·4% | 0·2% | 8·5% |
| Cyprus | 2019 | 7·2% | 46·0% | 4·4% | 49·6% | 0·0% | 3·0% |
| Czech Republic | 2384 | 7·4% | 84·8% | 0·8% | 14·4% | 0·0% | 2·8% |
| DR Congo | 46 | 4·5% | 21·3% | 0·0% | 37·4% | 41·3% | 2·9% |
| Denmark | 5075 | 10·8% | 84·8% | 1·9% | 13·4% | 0·0% | 2·8% |
| Djibouti | 357 | 10·9% | 58·3% | 0·0% | 34·6% | 7·1% | 5·3% |
| Dominica | 599 | 5·5% | 68·7% | 3·0% | 28·3% | 0·0% | 1·1% |
| Dominican Republic | 601 | 4·4% | 63·4% | 11·4% | 21·0% | 4·2% | 3·0% |
| Ecuador | 1071 | 9·2% | 48·8% | 2·2% | 48·5% | 0·5% | 8·0% |
| Egypt | 581 | 5·4% | 39·9% | 1·5% | 58·3% | 0·2% | 5·5% |
| El Salvador | 567 | 6·8% | 64·7% | 4·9% | 28·8% | 1·6% | 3·3% |
| Equatorial Guinea | 1411 | 3·7% | 79·2% | 0·0% | 20·7% | 0·1% | 17·0% |
| Eritrea | 59 | 5·1% | 23·4% | 0·0% | 35·2% | 41·4% | –1·1% |
| Estonia | 1830 | 6·4% | 79·0% | 0·3% | 20·8% | 0·0% | 5·1% |
| Ethiopia | 85 | 5·5% | 26·9% | 0·0% | 28·4% | 44·7% | 7·6% |
| Federated States of Micronesia | 490 | 16·1% | 0·0% | 0·0% | 7·7% | 92·3% | 2·9% |
| Fiji | 399 | 4·5% | 63·8% | 7·5% | 23·0% | 5·7% | 3·3% |
| Finland | 3935 | 9·3% | 78·0% | 3·1% | 18·9% | 0·0% | 3·1% |
| France | 4589 | 11·3% | 79·9% | 13·6% | 6·5% | 0·0% | 2·0% |
| Gabon | 612 | 3·4% | 67·4% | 8·8% | 22·0% | 1·8% | 0·0% |
| Georgia | 700 | 7·3% | 19·4% | 18·9% | 59·1% | 2·6% | 9·3% |
| Germany | 5356 | 11·2% | 77·3% | 9·4% | 13·3% | 0·0% | 2·6% |
| Ghana | 146 | 3·5% | 52·8% | 3·1% | 27·1% | 17·0% | 4·3% |
| Greece | 2170 | 8·1% | 61·7% | 3·4% | 34·9% | 0·0% | 0·9% |
| Grenada | 737 | 6·1% | 46·6% | 2·0% | 51·2% | 0·2% | 2·0% |
| Guatemala | 466 | 6·2% | 36·9% | 8·2% | 52·1% | 2·8% | 3·9% |
| Guinea | 101 | 7·4% | 20·4% | 0·0% | 34·5% | 45·1% | 3·5% |
| Guinea-Bissau | 77 | 5·3% | 6·0% | 0·0% | 52·1% | 41·9% | –3·0% |
| Guyana | 438 | 5·4% | 53·5% | 2·9% | 36·5% | 7·1% | 3·2% |
| Haiti | 154 | 8·9% | 0·0% | 29·6% | 29·6% | 40·8% | –1·8% |
| Honduras | 420 | 8·8% | 47·2% | 5·0% | 43·3% | 4·6% | 4·4% |
| Hungary | 1855 | 7·2% | 68·1% | 4·4% | 27·5% | 0·0% | 2·5% |
| Iceland | 3959 | 8·7% | 82·3% | 0·0% | 17·7% | 0·0% | 2·3% |
| India | 253 | 4·5% | 31·3% | 2·4% | 65·6% | 0·7% | 6·4% |
| Indonesia | 265 | 2·5% | 42·7% | 2·7% | 53·5% | 1·1% | 5·2% |
| Iran | 1073 | 6·5% | 43·8% | 5·3% | 50·8% | 0·0% | 6·2% |
| Iraq | 828 | 5·7% | 58·2% | 3·0% | 38·4% | 0·5% | 7·5% |
| Ireland | 4006 | 7·6% | 67·6% | 14·3% | 18·1% | 0·0% | 4·6% |
| Israel | 2722 | 7·7% | 61·5% | 11·2% | 27·3% | 0·0% | 1·9% |
| Italy | 3311 | 9·0% | 77·4% | 0·9% | 21·7% | 0·0% | 1·8% |
| Jamaica | 477 | 5·4% | 50·5% | 19·4% | 27·8% | 2·3% | 1·7% |
| Japan | 3816 | 10·2% | 83·6% | 2·4% | 13·9% | 0·0% | 3·0% |
| Jordan | 839 | 7·4% | 66·8% | 8·0% | 21·1% | 4·1% | 2·7% |
| Kazakhstan | 1143 | 4·3% | 54·4% | 0·0% | 45·3% | 0·3% | 5·8% |
| Kenya | 197 | 6·4% | 37·8% | 3·8% | 23·4% | 35·0% | 3·4% |
| Kiribati | 168 | 9·6% | 79·3% | 0·0% | 2·8% | 17·9% | 0·3% |
| Kuwait | 2075 | 3·0% | 85·9% | 1·3% | 12·7% | 0·0% | –1·1% |
| Kyrgyzstan | 236 | 6·9% | 47·7% | 1·3% | 37·3% | 13·7% | 3·1% |
| Laos | 113 | 2·0% | 28·3% | 0·4% | 36·6% | 34·7% | 1·8% |
| Latvia | 1427 | 5·9% | 63·2% | 1·7% | 35·1% | 0·0% | 5·5% |
| Lebanon | 1060 | 6·4% | 47·6% | 14·9% | 36·4% | 1·1% | –1·2% |
| Lesotho | 319 | 11·6% | 63·4% | 0·3% | 15·0% | 21·3% | 6·1% |
| Liberia | 345 | 39·3% | 0·0% | 0·0% | 7·8% | 92·2% | 19·7% |
| Libya | 751 | 5·0% | 73·5% | 0·0% | 26·5% | 0·0% | 0·0% |
| Lithuania | 1830 | 6·5% | 67·9% | 0·8% | 31·3% | 0·0% | 7·2% |
| Luxembourg | 7105 | 6·9% | 83·9% | 5·5% | 10·6% | 0·0% | 3·2% |
| Macedonia | 887 | 6·5% | 63·1% | 0·0% | 36·6% | 0·3% | 1·4% |
| Madagascar | 52 | 3·7% | 29·5% | 0·0% | 34·3% | 36·2% | –0·4% |
| Malawi | 148 | 12·9% | 33·5% | 14·0% | 9·3% | 43·1% | 5·5% |
| Malaysia | 1047 | 4·1% | 56·0% | 8·1% | 35·8% | 0·0% | 5·1% |
| Maldives | 1980 | 13·5% | 79·4% | 2·0% | 18·5% | 0·0% | 11·0% |
| Mali | 162 | 7·4% | 22·0% | 10·9% | 43·6% | 23·5% | 4·0% |
| Malta | 3058 | 9·7% | 69·2% | 2·0% | 28·9% | 0·0% | 5·5% |
| Marshall Islands | 599 | 17·2% | 62·9% | 2·1% | 11·8% | 23·2% | –3·0% |
| Mauritania | 153 | 3·7% | 44·5% | 1·4% | 44·7% | 9·3% | 0·7% |
| Mauritius | 880 | 4·6% | 50·8% | 0·7% | 48·0% | 0·4% | 4·8% |
| Mexico | 1088 | 6·3% | 51·7% | 4·2% | 44·0% | 0·1% | 2·9% |
| Moldova | 527 | 10·3% | 47·2% | 8·2% | 38·3% | 6·3% | 3·4% |
| Mongolia | 575 | 4·7% | 51·4% | 0·9% | 41·9% | 5·8% | 8·4% |
| Montenegro | 1015 | 6·6% | 55·3% | 2·7% | 41·4% | 0·6% | 3·4% |
| Morocco | 505 | 5·9% | 33·1% | 7·6% | 58·4% | 0·9% | 5·6% |
| Mozambique | 92 | 7·8% | 10·6% | 0·6% | 8·5% | 80·2% | 7·4% |
| Myanmar | 121 | 2·5% | 36·2% | 0·0% | 45·6% | 18·2% | 9·4% |
| Namibia | 936 | 9·3% | 53·5% | 31·2% | 6·9% | 8·4% | 5·2% |
| Nepal | 138 | 5·8% | 28·6% | 5·9% | 47·7% | 17·8% | 3·1% |
| Netherlands | 5234 | 10·7% | 88·4% | 6·3% | 5·3% | 0·0% | 3·9% |
| New Zealand | 4050 | 11·0% | 82·3% | 6·6% | 11·0% | 0·0% | 4·2% |
| Nicaragua | 450 | 9·1% | 50·9% | 3·8% | 37·3% | 8·0% | 3·6% |
| Niger | 66 | 6·7% | 26·3% | 0·0% | 49·5% | 24·2% | 0·6% |
| Nigeria | 225 | 3·7% | 22·1% | 0·8% | 70·1% | 7·0% | 7·5% |
| Norway | 6537 | 10·0% | 83·1% | 3·7% | 13·2% | 0·0% | 3·3% |
| Oman | 1467 | 3·5% | 91·8% | 2·3% | 5·9% | 0·0% | 1·6% |
| Pakistan | 132 | 2·7% | 32·1% | 6·1% | 55·4% | 6·4% | 2·0% |
| Panama | 1743 | 8·0% | 72·5% | 4·5% | 22·3% | 0·8% | 4·8% |
| Papua New Guinea | 108 | 4·4% | 60·1% | 3·9% | 10·1% | 25·9% | 3·5% |
| Paraguay | 863 | 9·8% | 45·6% | 4·6% | 49·3% | 0·5% | 4·7% |
| Peru | 626 | 5·2% | 63·3% | 6·3% | 30·0% | 0·4% | 4·4% |
| Philippines | 330 | 4·7% | 33·6% | 10·2% | 54·3% | 1·9% | 4·4% |
| Poland | 1629 | 6·3% | 71·4% | 5·0% | 23·6% | 0·0% | 5·0% |
| Portugal | 2697 | 9·3% | 66·6% | 5·9% | 27·6% | 0·0% | 3·3% |
| Qatar | 2663 | 2·2% | 85·7% | 7·4% | 6·9% | 0·0% | 0·7% |
| Congo (Brazzaville) | 312 | 5·2% | 80·7% | 0·3% | 17·4% | 1·7% | 4·5% |
| Romania | 1077 | 5·5% | 79·1% | 0·4% | 18·9% | 1·6% | 7·2% |
| Russia | 1877 | 7·1% | 51·8% | 2·8% | 45·5% | 0·0% | 5·4% |
| Rwanda | 158 | 9·4% | 0·0% | 22·4% | 22·6% | 55·0% | 7·9% |
| Saint Lucia | 755 | 6·7% | 49·2% | 0·8% | 45·6% | 4·4% | 1·4% |
| Saint Vincent and the Grenadines | 917 | 8·8% | 46·1% | 2·0% | 48·2% | 3·6% | 3·4% |
| Samoa | 365 | 7·2% | 87·2% | 0·0% | 5·9% | 6·9% | 4·5% |
| São Tomé and Príncipe | 251 | 7·9% | 31·1% | 8·0% | 11·9% | 49·0% | 1·9% |
| Saudi Arabia | 2320 | 4·4% | 78·7% | 6·2% | 15·1% | 0·0% | 5·0% |
| Senegal | 121 | 5·2% | 39·4% | 0·0% | 33·8% | 26·9% | 2·1% |
| Serbia | 1392 | 10·3% | 62·5% | 0·3% | 37·0% | 0·1% | 6·9% |
| Seychelles | 853 | 3·3% | 93·6% | 4·0% | 2·4% | 0·1% | –0·2% |
| Sierra Leone | 255 | 13·5% | 5·1% | 9·2% | 50·1% | 35·6% | 3·0% |
| Singapore | 3981 | 4·8% | 42·4% | 1·9% | 55·7% | 0·0% | 6·5% |
| Slovakia | 2203 | 7·7% | 76·3% | 0·0% | 23·7% | 0·0% | 5·1% |
| Slovenia | 2845 | 9·1% | 73·2% | 14·5% | 12·3% | 0·0% | 3·5% |
| Solomon Islands | 107 | 5·8% | 67·0% | 0·0% | 4·0% | 29·1% | 2·7% |
| Somalia | 33 | 6·9% | 25·0% | 1·2% | 28·5% | 45·2% | 1·9% |
| South Africa | 1172 | 8·9% | 47·0% | 44·2% | 6·4% | 2·4% | 2·1% |
| South Korea | 2507 | 7·1% | 56·0% | 6·6% | 37·4% | 0·0% | 7·6% |
| South Sudan | 94 | 3·6% | 21·0% | 0·0% | 40·7% | 38·3% | 1·8% |
| Spain | 3096 | 9·0% | 71·1% | 4·8% | 24·1% | 0·0% | 2·6% |
| Sri Lanka | 402 | 3·5% | 54·5% | 1·0% | 42·3% | 2·1% | 5·2% |
| Sudan | 334 | 8·3% | 20·4% | 0·9% | 76·6% | 2·2% | 9·0% |
| Suriname | 731 | 4·3% | 67·6% | 15·5% | 15·2% | 1·7% | 2·0% |
| Swaziland | 745 | 9·5% | 66·6% | 8·4% | 10·0% | 15·0% | 4·7% |
| Sweden | 5446 | 11·8% | 85·1% | 0·6% | 14·2% | 0·0% | 4·0% |
| Switzerland | 7831 | 12·8% | 60·3% | 15·2% | 24·5% | 0·0% | 3·2% |
| Syria | 562 | 3·4% | 44·5% | 3·3% | 51·6% | 0·6% | –1·4% |
| Tajikistan | 200 | 7·3% | 22·9% | 8·7% | 57·9% | 10·6% | 7·3% |
| Tanzania | 166 | 6·4% | 20·3% | 17·1% | 20·2% | 42·4% | 7·2% |
| Thailand | 633 | 4·1% | 78·7% | 8·6% | 12·1% | 0·7% | 3·7% |
| The Bahamas | 1996 | 7·7% | 45·9% | 24·9% | 29·2% | 0·0% | 1·2% |
| The Gambia | 151 | 9·2% | 47·4% | 0·0% | 13·6% | 39·0% | 5·8% |
| Timor-Leste | 105 | 1·9% | 51·6% | 0·0% | 7·4% | 41·0% | 8·3% |
| Togo | 81 | 5·5% | 29·7% | 7·8% | 44·3% | 18·3% | 1·9% |
| Tonga | 253 | 5·3% | 69·5% | 0·4% | 11·7% | 18·5% | 1·7% |
| Trinidad and Tobago | 1823 | 5·8% | 54·5% | 6·8% | 38·7% | 0·0% | 6·2% |
| Tunisia | 791 | 6·9% | 57·2% | 4·5% | 38·1% | 0·2% | 3·5% |
| Turkey | 1040 | 5·3% | 78·4% | 3·5% | 18·0% | 0·1% | 6·6% |
| Turkmenistan | 396 | 2·3% | 59·2% | 8·7% | 31·6% | 0·6% | 5·3% |
| Uganda | 347 | 18·1% | 0·9% | 64·8% | 16·4% | 18·0% | 9·3% |
| Ukraine | 659 | 7·0% | 51·3% | 0·9% | 46·8% | 0·9% | 2·9% |
| United Arab Emirates | 2561 | 3·6% | 72·3% | 9·9% | 17·8% | 0·0% | –0·4% |
| UK | 3749 | 9·1% | 83·1% | 7·1% | 9·7% | 0·0% | 3·4% |
| USA | 9237 | 16·6% | 49·8% | 38·8% | 11·4% | 0·0% | 2·9% |
| Uruguay | 1837 | 8·6% | 71·2% | 13·2% | 15·6% | 0·0% | 2·9% |
| Uzbekistan | 397 | 5·9% | 51·9% | 2·6% | 43·7% | 1·7% | 3·6% |
| Vanuatu | 149 | 5·4% | 56·7% | 0·0% | 5·4% | 37·9% | 4·1% |
| Venezuela | 1010 | 5·3% | 29·3% | 6·3% | 64·3% | 0·0% | 1·0% |
| Vietnam | 398 | 7·0% | 53·0% | 6·9% | 37·4% | 2·7% | 7·0% |
| Yemen | 233 | 5·8% | 14·3% | 1·7% | 74·7% | 9·3% | 3·0% |
| Zambia | 216 | 5·4% | 32·6% | 0·0% | 27·7% | 39·7% | 4·8% |
Data in parenthesis are range within aggregate. Currency are 2015 purchasing power parity US$. GBD=Global Burden of Disease.
Table 1 also highlights the sources of health financing in 2014. Globally, governments provided 59·2% of health spending, while 17·4% of total health financing was prepaid private, 22·8% was OOP, and 0·6% was development assistance for health. In low-income countries, health spending was predominately financed by development assistance for health and OOP, constituting 35·7% and 29·1% of total health spending, respectively. However, the share of health financing sourced from OOP is largest in lower-middle-income countries, at 58·0%, where development assistance for health makes up a smaller share of total health spending than in low-income countries. Governments in upper-middle-income and high-income countries, by contrast, finance the bulk of health care and related activities, at 57·2% and 63·4%, respectively. Across all income groups, prepaid private health spending remained quite low. Within income groups, and also GBD super regions, the composition of sources financing the health system varied dramatically.
Health spending trends across time
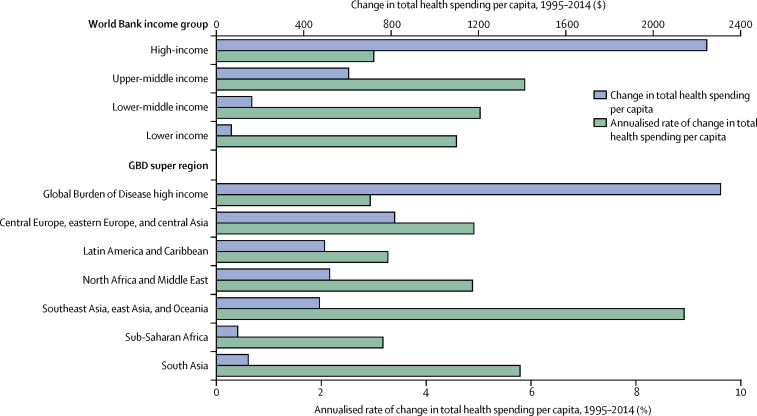
Figure 1 highlights how total health spending per capita has changed between 1995 and 2014. Upper-middle and lower-middle-income country groups have increased per capita health spending the fastest, with annualised growth rates of 5·9% and 5·0%, respectively. Over the course of 20 years, this has led to a near tripling of health spending per capita in upper-middle-income countries, from $309 to $914 per capita. Spending in low-income countries grew at 4·6%, while the slowest growth was observed in high-income countries, which grew collectively at 3·0% per year. Despite this slower rate, the largest health spending increases in terms of dollar per capita increase was in high-income countries, which added $2244 per capita in spending. Upper-income and lower-income countries added $605 and $162 per capita respectively. Low-income countries, which spent very little in 1995, increased health spending by $69 per capita between 1995 and 2014. Liberia, Equatorial Guinea, and Maldives had the fastest per capita growth rates between 1995 and 2014 (table 1).
Figure 1.
Changes in health spending by income group and Global Burden of Disease (GBD) super region, 1995–2014
Currency reported in 2015 purchasing power parity adjusted $.
For high-income and middle-income countries, the growth in spending was driven by increases in government spending. For example, in high-income countries, 64·5% of the $2244 increase was due to increases in government spending. Conversely, the growth in low-income countries was driven by increases in development assistance for health (51·0% of absolute increase).
Although we observed increases in spending per capita between 1995 and 2014 in 170 of 184 countries, the multivariate penalised spline analysis shows that when controlling on GDP per capita, there was essentially no change in health spending across time at the median health spending per capita value (appendix p 36 illustrates this null finding).
Health spending trends and economic development
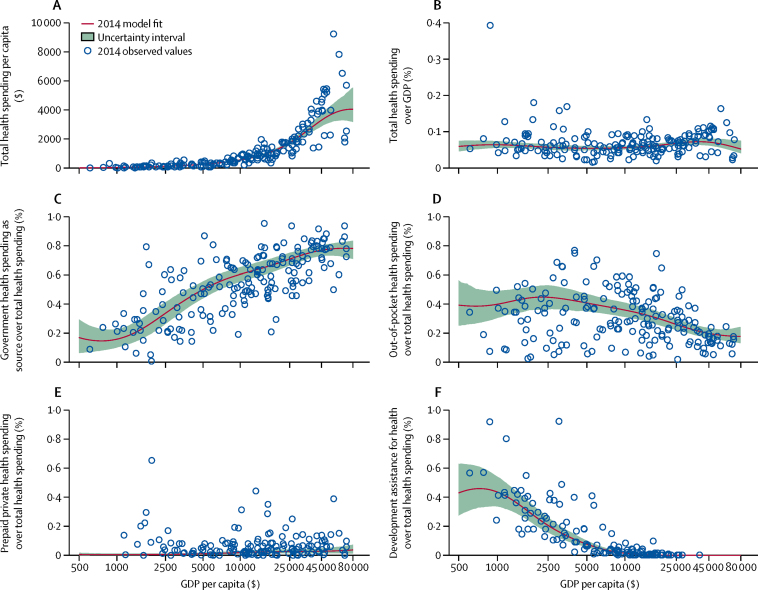
Although time does not seem to be associated with health spending per capita, our trend analyses confirm the relationship between economic development and health financing—total health spending increases with economic development, while the share of OOP financing decreases. These associations are represented in figure 2. Across countries, growth in GDP per capita was associated with exponential growth in total health spending per capita (figure 2A; appendix p 40; p<0·000).
Figure 2.
Health spending by source (total health spending [A, B], government health spending [C]; out-of-pocket health spending [D]; prepaid private health spending [E], and development assistance for health [F]), 2014
Health spending relative to gross domestic product (GDP) per capita (reported in 2015 purchasing-power-parity [PPP] adjusted $). Although all countries and years of data were used for this analysis, the trend line reflects the 2014 model fit.
Figure 2B shows that when measured as a share of GDP, there is not a robust relationship connecting economic development and spending. The estimated fit is nearly flat and there are countries with similar GDP per capita with disparate spending levels.
Figure 2C and 2D show that the share of health spending from the government increases with economic development, while the share that is OOP decreases. Prepaid private spending as a share of total spending is very small, on average, across all levels of economic development (figure 2E), while the share of health spending that is development assistance for health increases at the very lowest levels of GDP per capita and peaks at GDP per capita of $801 (figure 2F).
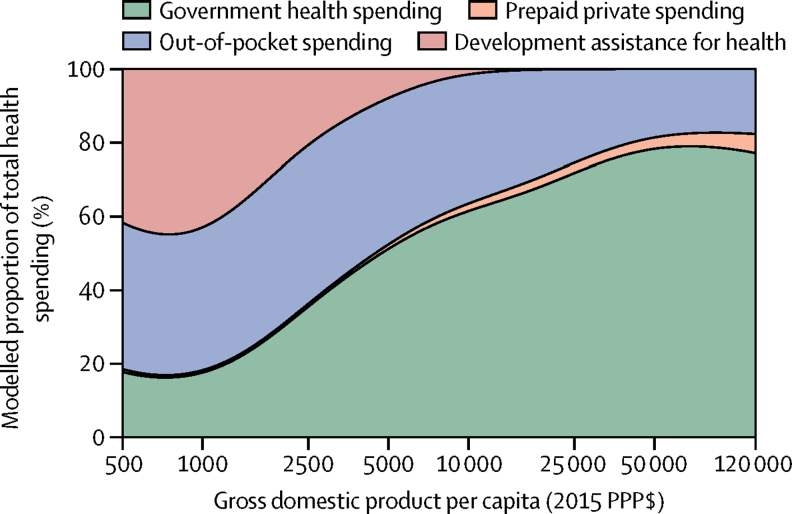
Figure 3 shows how the fraction of total health spending from governments, prepaid private, OOP, and development assistance for health evolve, on average, with economic development. On average, the proportion of total health spending sourced from governments rise as GDP per capita increases. At the 80th wealth percentile (GDP per capita of $27 617), trend analysis estimates that health spending is financed by the governments (72·2%), with only 24·9% sourced from OOP. At the 20th wealth percentile (GDP per capita of $2267), trend analysis estimates that OOP financing is 44·8% of total spending, while development assistance for health is 23·1%.
Figure 3.
Composition of health-care spending by source, 2014
PPP=purchasing-power-parity.
Deviation from the health financing trends
Table 2 measures health spending relative to the modelled amount, which is based on country-specific and year-specific GDP per capita. The first column reports total health spending for 2014, which, as figure 2A shows, increases exponentially with GDP per capita. Countries such as Afghanistan, Brazil, France, Liberia, Uganda, and the USA spent more in 2014 than the modelled average, based on each country's GDP per capita. On the other hand, countries such as Timor-Leste, Laos, and Turkmenistan spend 33·0%, 34·7%, and 35·6% of the expected amount.
Table 2.
Health spending relative to expected health spending, 2014
| Total health spending relative to modelled total health spending (%) | Share of total health spending that is from the government, relative to the modelled share (%) | Share of total health spending that is prepaid private, relative to the modelled share (%) | Share of total health spending that is out-of-pocket, relative to the modelled share (%) | Share of total health spending that is development assistance, relative to the modelled share (%) | |
|---|---|---|---|---|---|
| Afghanistan | 153·8% | 64·0% | 0·3% | 123·7% | 96·3% |
| Albania | 99·5% | 78·6% | 0·6% | 141·5% | 170·3% |
| Algeria | 118·0% | 113·8% | 30·3% | 80·0% | 8·8% |
| Andorra | 141·7% | 99·6% | 167·6% | 88·2% | 0·0% |
| Angola | 52·0% | 122·2% | 0·0% | 70·3% | 109·7% |
| Antigua and Barbuda | 81·1% | 98·7% | 293·5% | 84·8% | 9·6% |
| Argentina | 65·2% | 77·2% | 475·9% | 124·3% | 30·8% |
| Armenia | 78·7% | 69·0% | 158·5% | 142·9% | 162·4% |
| Australia | 121·3% | 91·4% | 333·2% | 98·6% | 0·0% |
| Austria | 154·6% | 100·6% | 191·4% | 83·2% | 0·0% |
| Azerbaijan | 91·3% | 31·4% | 164·4% | 242·1% | 263·9% |
| Bahrain | 66·0% | 84·5% | 354·1% | 121·9% | 0·0% |
| Bangladesh | 49·2% | 56·7% | 0·0% | 149·9% | 76·7% |
| Barbados | 120·6% | 98·2% | 264·0% | 92·2% | 0·0% |
| Belarus | 84·3% | 98·7% | 5·5% | 111·0% | 232·0% |
| Belgium | 142·9% | 101·2% | 144·0% | 88·9% | 0·0% |
| Belize | 100·1% | 109·7% | 498·3% | 62·2% | 131·1% |
| Benin | 82·8% | 120·8% | 0·0% | 79·3% | 115·9% |
| Bhutan | 62·9% | 123·3% | 0·0% | 66·3% | 137·8% |
| Bolivia | 110·7% | 128·8% | 225·1% | 59·0% | 68·2% |
| Bosnia and Herzegovina | 162·4% | 114·9% | 0·0% | 78·6% | 154·6% |
| Botswana | 86·4% | 75·9% | 1352·6% | 16·4% | 3595·7% |
| Brazil | 131·4% | 70·0% | 1104·9% | 81·0% | 33·1% |
| Brunei | 45·0% | 119·9% | 2·8% | 33·1% | 0·0% |
| Bulgaria | 130·6% | 82·1% | 33·2% | 145·0% | 72·0% |
| Burkina Faso | 80·1% | 152·7% | 0·0% | 88·2% | 80·0% |
| Burundi | 119·3% | 161·9% | 0·0% | 49·3% | 124·5% |
| Cambodia | 109·2% | 35·0% | 0·0% | 149·9% | 137·0% |
| Cameroon | 67·3% | 45·1% | 404·5% | 155·1% | 63·6% |
| Canada | 138·7% | 93·8% | 475·0% | 68·8% | 0·0% |
| Cape Verde | 83·0% | 105·6% | 9·4% | 57·3% | 446·0% |
| Central African Republic | 77·4% | 59·1% | 0·0% | 88·4% | 125·3% |
| Chad | 63·1% | 151·3% | 168·8% | 83·1% | 57·9% |
| Chile | 111·6% | 70·8% | 693·3% | 115·4% | 3·3% |
| China | 83·9% | 94·7% | 208·7% | 103·9% | 5·9% |
| Colombia | 118·8% | 113·1% | 394·1% | 46·0% | 586·2% |
| Comoros | 111·9% | 99·1% | 2797·1% | 98·6% | 44·5% |
| Congo | 90·7% | 150·8% | 17·6% | 44·0% | 31·0% |
| Costa Rica | 147·8% | 112·5% | 71·1% | 78·0% | 8·3% |
| Côte d'Ivoire | 90·7% | 53·6% | 869·3% | 125·5% | 105·6% |
| Croatia | 113·0% | 117·9% | 253·3% | 40·5% | 0·0% |
| Cuba | 177·8% | 146·9% | 0·0% | 13·7% | 44·9% |
| Cyprus | 98·4% | 63·6% | 157·4% | 200·1% | 0·0% |
| Czech Republic | 98·4% | 114·6% | 28·1% | 62·2% | 0·0% |
| Congo (Brazzaville) | 66·9% | 134·1% | 0·0% | 93·5% | 95·1% |
| Denmark | 147·3% | 109·7% | 62·3% | 67·9% | 0·0% |
| Djibouti | 186·7% | 143·9% | 0·0% | 79·4% | 47·5% |
| Dominica | 92·9% | 111·7% | 135·8% | 80·5% | 3·5% |
| Dominican Republic | 72·4% | 99·4% | 472·1% | 63·1% | 789·2% |
| Ecuador | 153·4% | 78·5% | 96·8% | 139·9% | 59·0% |
| Egypt | 91·0% | 65·1% | 68·6% | 165·3% | 20·8% |
| El Salvador | 117·8% | 110·7% | 262·7% | 77·3% | 66·3% |
| Equatorial Guinea | 48·7% | 104·6% | 0·0% | 96·9% | 480·8% |
| Eritrea | 78·2% | 136·8% | 0·0% | 86·0% | 100·3% |
| Estonia | 86·0% | 108·6% | 9·6% | 85·0% | 0·0% |
| Ethiopia | 87·6% | 122·7% | 0·0% | 65·6% | 131·3% |
| Federated States of Micronesia | 273·0% | 0·0% | 0·0% | 17·5% | 566·3% |
| Fiji | 77·8% | 107·8% | 390·3% | 62·4% | 277·3% |
| Finland | 124·2% | 101·9% | 105·6% | 92·2% | 0·0% |
| France | 150·0% | 104·9% | 467·6% | 31·1% | 0·0% |
| Gabon | 52·9% | 101·1% | 332·0% | 72·4% | 853·0% |
| Georgia | 126·5% | 32·3% | 941·1% | 162·8% | 151·8% |
| Germany | 154·4% | 100·0% | 311·0% | 67·6% | 0·0% |
| Ghana | 61·0% | 114·5% | 286·3% | 64·4% | 159·6% |
| Greece | 111·0% | 85·8% | 124·1% | 138·0% | 0·0% |
| Grenada | 102·0% | 74·5% | 88·4% | 148·8% | 27·3% |
| Guatemala | 108·6% | 64·7% | 477·2% | 137·2% | 85·3% |
| Guinea | 115·4% | 103·8% | 0·0% | 81·5% | 120·9% |
| Guinea-Bissau | 83·7% | 29·2% | 0·0% | 121·8% | 116·5% |
| Guyana | 92·9% | 92·0% | 155·8% | 97·7% | 275·7% |
| Haiti | 142·4% | 0·0% | 4032·0% | 67·1% | 133·3% |
| Honduras | 153·3% | 96·0% | 413·0% | 105·1% | 54·1% |
| Hungary | 99·8% | 95·4% | 159·5% | 106·5% | 0·0% |
| Iceland | 118·2% | 106·8% | 0·0% | 88·9% | 0·0% |
| India | 77·6% | 59·5% | 175·1% | 164·5% | 10·8% |
| Indonesia | 42·5% | 69·8% | 124·6% | 151·0% | 93·9% |
| Iran | 102·6% | 66·6% | 204·4% | 162·2% | 15·6% |
| Iraq | 92·8% | 90·4% | 121·4% | 117·3% | 105·0% |
| Ireland | 108·8% | 86·9% | 457·8% | 94·9% | 0·0% |
| Israel | 101·9% | 82·1% | 393·6% | 123·1% | 0·0% |
| Italy | 119·0% | 102·7% | 32·4% | 99·7% | 0·0% |
| Jamaica | 92·9% | 85·4% | 1005·4% | 75·5% | 112·7% |
| Japan | 134·4% | 110·7% | 84·7% | 64·6% | 0·0% |
| Jordan | 124·4% | 107·9% | 358·9% | 60·6% | 422·4% |
| Kazakhstan | 60·0% | 75·9% | 1·2% | 177·3% | 649·7% |
| Kenya | 108·6% | 96·8% | 428·7% | 53·2% | 217·6% |
| Kiribati | 154·9% | 323·3% | 0·0% | 6·4% | 58·3% |
| Kuwait | 51·6% | 109·7% | 37·6% | 70·3% | 0·0% |
| Kyrgyzstan | 117·6% | 114·4% | 139·3% | 86·0% | 98·0% |
| Laos | 34·7% | 53·7% | 30·4% | 91·8% | 570·8% |
| Latvia | 82·8% | 89·5% | 61·3% | 132·4% | 0·0% |
| Lebanon | 100·1% | 72·2% | 574·1% | 116·6% | 422·6% |
| Lesotho | 194·8% | 175·0% | 30·2% | 33·8% | 115·3% |
| Liberia | 575·9% | 0·0% | 0·0% | 20·0% | 203·9% |
| Libya | 80·2% | 113·5% | 0·2% | 81·9% | 8·3% |
| Lithuania | 89·1% | 93·8% | 28·9% | 126·3% | 0·0% |
| Luxembourg | 182·2% | 108·5% | 116·6% | 59·1% | 0·0% |
| Macedonia | 106·8% | 99·0% | 0·0% | 109·8% | 63·2% |
| Madagascar | 57·3% | 146·3% | 0·0% | 80·4% | 99·2% |
| Malawi | 197·6% | 197·2% | 2043·1% | 22·9% | 104·1% |
| Malaysia | 57·0% | 78·6% | 293·6% | 138·4% | 59·1% |
| Maldives | 219·3% | 123·2% | 81·5% | 56·8% | 2·9% |
| Mali | 121·0% | 72·1% | 1399·1% | 97·2% | 98·4% |
| Malta | 130·7% | 93·9% | 70·4% | 123·0% | 0·0% |
| Marshall Islands | 293·5% | 149·1% | 220·6% | 27·2% | 170·7% |
| Mauritania | 64·0% | 96·6% | 128·7% | 106·2% | 87·6% |
| Mauritius | 70·5% | 75·4% | 27·0% | 161·6% | 242·8% |
| Mexico | 97·7% | 77·9% | 161·4% | 142·9% | 45·1% |
| Moldova | 179·8% | 93·3% | 641·7% | 94·2% | 84·3% |
| Mongolia | 78·7% | 82·1% | 37·5% | 122·3% | 752·2% |
| Montenegro | 105·8% | 85·0% | 105·8% | 129·1% | 177·0% |
| Morocco | 102·8% | 56·4% | 405·2% | 157·4% | 37·8% |
| Mozambique | 119·0% | 61·0% | 93·7% | 20·7% | 196·6% |
| Myanmar | 44·2% | 73·7% | 0·0% | 110·7% | 215·1% |
| Namibia | 158·4% | 88·2% | 1495·1% | 19·2% | 600·0% |
| Nepal | 95·9% | 87·8% | 732·5% | 106·5% | 81·7% |
| Netherlands | 147·9% | 114·1% | 206·3% | 27·3% | 0·0% |
| New Zealand | 145·5% | 109·3% | 231·1% | 50·8% | 0·0% |
| Nicaragua | 157·9% | 101·8% | 306·9% | 91·3% | 101·0% |
| Niger | 99·0% | 168·1% | 0·0% | 124·4% | 55·2% |
| Nigeria | 65·6% | 41·3% | 53·1% | 177·4% | 127·5% |
| Norway | 163·8% | 106·1% | 107·2% | 72·6% | 0·0% |
| Oman | 46·3% | 120·0% | 76·9% | 28·9% | 0·0% |
| Pakistan | 46·3% | 64·2% | 486·2% | 135·6% | 81·2% |
| Panama | 116·5% | 104·8% | 163·9% | 79·6% | 758·5% |
| Papua New Guinea | 73·5% | 181·5% | 488·4% | 22·5% | 121·6% |
| Paraguay | 169·9% | 77·2% | 239·1% | 133·7% | 25·0% |
| Peru | 87·6% | 101·4% | 276·0% | 87·0% | 48·7% |
| Philippines | 80·9% | 59·8% | 614·9% | 141·5% | 50·7% |
| Poland | 87·6% | 100·0% | 180·6% | 91·6% | 0·0% |
| Portugal | 125·1% | 91·4% | 210·2% | 113·5% | 0·0% |
| Qatar | 72·6% | 112·2% | 137·1% | 37·8% | 0·0% |
| Romania | 84·1% | 116·9% | 15·1% | 64·2% | 1012·3% |
| Russia | 98·5% | 72·3% | 100·0% | 178·1% | 0·0% |
| Rwanda | 149·8% | 0·0% | 3072·2% | 51·5% | 174·6% |
| Saint Lucia | 113·2% | 79·7% | 37·3% | 130·3% | 441·0% |
| Saint Vincent and the Grenadines | 150·1% | 75·7% | 95·9% | 135·3% | 284·7% |
| Samoa | 125·8% | 173·2% | 0·0% | 14·5% | 90·4% |
| Sao Tome and Principe | 133·8% | 77·6% | 874·5% | 27·2% | 320·8% |
| Saudi Arabia | 63·0% | 101·2% | 197·0% | 79·4% | 0·0% |
| Senegal | 85·6% | 122·7% | 0·0% | 75·3% | 120·5% |
| Serbia | 167·5% | 98·1% | 13·4% | 111·2% | 23·9% |
| Seychelles | 46·5% | 131·3% | 143·3% | 9·2% | 181·7% |
| Sierra Leone | 218·9% | 19·2% | 1235·0% | 112·7% | 125·6% |
| Singapore | 98·1% | 54·3% | 47·7% | 311·5% | 0·0% |
| Slovakia | 103·5% | 104·9% | 0·0% | 97·1% | 0·0% |
| Slovenia | 120·2% | 99·2% | 516·1% | 52·7% | 0·0% |
| Solomon Islands | 94·2% | 260·3% | 0·0% | 9·0% | 99·6% |
| Somalia | 87·6% | 142·7% | 164·2% | 72·2% | 107·2% |
| South Africa | 146·2% | 74·0% | 1850·3% | 19·2% | 411·3% |
| South Korea | 93·9% | 74·7% | 233·0% | 168·7% | 0·0% |
| South Sudan | 61·1% | 61·1% | 0·0% | 91·1% | 190·8% |
| Spain | 118·4% | 95·1% | 170·8% | 107·6% | 0·0% |
| Sri Lanka | 58·9% | 88·0% | 45·8% | 121·5% | 229·0% |
| Sudan | 143·6% | 44·8% | 80·1% | 180·9% | 19·7% |
| Suriname | 66·5% | 102·1% | 592·7% | 49·1% | 716·5% |
| Swaziland | 164·8% | 115·5% | 473·5% | 26·6% | 519·4% |
| Sweden | 160·3% | 110·3% | 20·8% | 71·9% | 0·0% |
| Switzerland | 199·2% | 77·1% | 452·0% | 133·2% | 0·0% |
| Syria | 53·1% | 67·6% | 127·1% | 165·3% | 216·1% |
| Tajikistan | 123·6% | 63·6% | 1024·3% | 130·3% | 56·5% |
| Tanzania | 107·3% | 58·5% | 2069·5% | 45·2% | 213·9% |
| Thailand | 65·2% | 120·9% | 337·4% | 37·7% | 195·2% |
| The Bahamas | 107·4% | 64·3% | 899·4% | 113·4% | 0·0% |
| The Gambia | 145·7% | 202·4% | 0·0% | 31·1% | 121·6% |
| Timor-Leste | 33·0% | 99·1% | 0·0% | 18·6% | 634·8% |
| Togo | 86·0% | 140·6% | 1091·4% | 103·0% | 51·9% |
| Tonga | 92·3% | 141·4% | 32·8% | 28·4% | 217·7% |
| Trinidad and Tobago | 77·9% | 74·0% | 242·1% | 164·9% | 0·0% |
| Tunisia | 117·2% | 92·4% | 202·5% | 109·3% | 18·0% |
| Turkey | 80·2% | 115·7% | 130·9% | 61·3% | 35·7% |
| Turkmenistan | 35·6% | 89·2% | 331·7% | 102·5% | 238·5% |
| Uganda | 293·2% | 3·3% | 8624·8% | 36·7% | 64·8% |
| Ukraine | 120·5% | 85·8% | 45·9% | 128·7% | 53·6% |
| United Arab Emirates | 63·4% | 92·4% | 273·9% | 98·6% | 0·0% |
| UK | 121·4% | 109·0% | 244·6% | 46·9% | 0·0% |
| USA | 243·7% | 63·8% | 1211·9% | 60·7% | 0·0% |
| Uruguay | 126·1% | 103·3% | 485·1% | 55·2% | 6·8% |
| Uzbekistan | 102·4% | 93·5% | 165·1% | 113·0% | 41·6% |
| Vanuatu | 90·0% | 155·2% | 0·0% | 12·2% | 208·0% |
| Venezuela | 79·9% | 43·4% | 236·0% | 217·4% | 1·5% |
| Vietnam | 121·9% | 100·8% | 494·6% | 93·7% | 44·3% |
| Yemen | 100·2% | 31·5% | 161·1% | 176·4% | 83·5% |
| Zambia | 93·7% | 72·1% | 0·0% | 65·3% | 351·9% |
Columns 2 to 5 of table 2 report the share of health spending financed by different sources relative to the expected amount. The results show that some countries deviate substantially from average trends. For government health spending, Rwanda, Liberia, and Federated States of Micronesia stand out as countries that finance a smaller share than expected relative to respective GDP per capita. On the other hand, Kiribati, Solomon Islands, and The Gambia have governments that finance a greater share than expected. By contrast with the government health financing share, the OOP share of total health spending declines with economic development. Surrounding the modelled average, however, is a great deal of variation. Countries such as Afghanistan, Sudan, and Nigeria, spend more through OOP than expected. Conversely, countries such as Congo (Brazzaville), Algeria, South Africa, and France have a disproportionally smaller OOP share of total health spending.
Column 5 of table 2 reports the share of health spending that is from development partners, in this case measured relative to expected spending. As shown in figure 2F, development assistance for health as a share of total health spending actually increases with GDP per capita for the countries with the smallest GDP per capita; a number of countries, such as Niger, which has a very low GDP per capita, receive very little development assistance for health. Relative to the expected amount, countries such as Botswana, Romania, and Gabon finance a greater share of their health spending using development assistance funds than would otherwise be expected. On the other hand, countries such as Cameroon and Sudan finance their health spending with less development assistance funds than would be expected based on their GDP per capita.
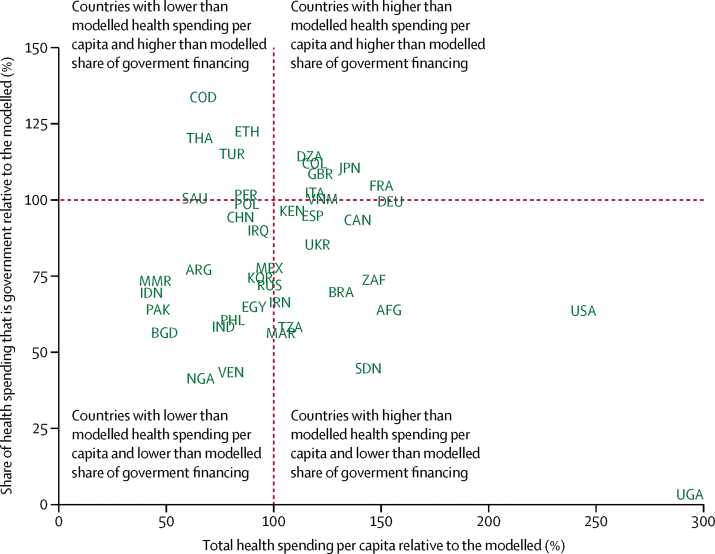
Figure 4 shows total health spending and the share that is government health spending, both relative to the modelled amount, based solely on GDP per capita. Countries such as Algeria and Japan have greater than modelled health spending per capita and greater than modelled share of financing from government. Countries such as Uganda and the USA have greater than modelled health spending per capita, but less than modelled share of financing from government. Conversely, countries such as Ethiopia and Thailand, have less health spending per capita than modelled, but higher than modelled share of financing from government, and countries such as India, Indonesia, and Philippines have less health spending per capita than modelled and lower than modelled share of financing from government.
Figure 4.
Observed government and total health spending relative to modelled spending, 2014
The figure shows the total health spending relative to modelled spending, and the share of health spending that is from the government relative to the modelled share. The vertical and horizontal red lines indicate where the observed spending is equal to the modelled spending (100%). Although all countries and years of data were used for this analysis, the deviations reflects the 2014 model fit. Only countries with a population higher than 30 million and 2014 data are included as points to avoid too many markers. A version with all countries included a dots is included in the appendix (p 68). AFG=Afghanistan. ARG=Argentina. BGD=Bangladesh. BRA=Brazil. CAN=Canada. CHN=China. COD=Democratic Republic of the Congo. COL=Colombia. DEU=Germany. DZA=Algeria. EGY=Egypt. ESP=Spain. ETH=Ethiopia. FRA=France. GBR=UK. IDN=Indonesia. IND=India. IRN=Iran. IRQ=Iraq. ITA=Italy. JPN=Japan. KEN=Kenya. KOR=South Korea. MAR=Morocco. MEX=Mexico. MMR=Myanmar. NGA=Nigeria. PAK=Pakistan. PER=Peru. PHL=Philippines. POL=Poland. RUS=Russia. SAU=Saudi Arabia. SDN=Sudan. THA=Thailand. TUR=Turkey. TZA=Tanzania. UGA=Uganda. UKR=Ukraine. USA=USA. VEN=Venezuela. VNM=Vietnam. ZAF=South Africa.
Trends in development assistance for health
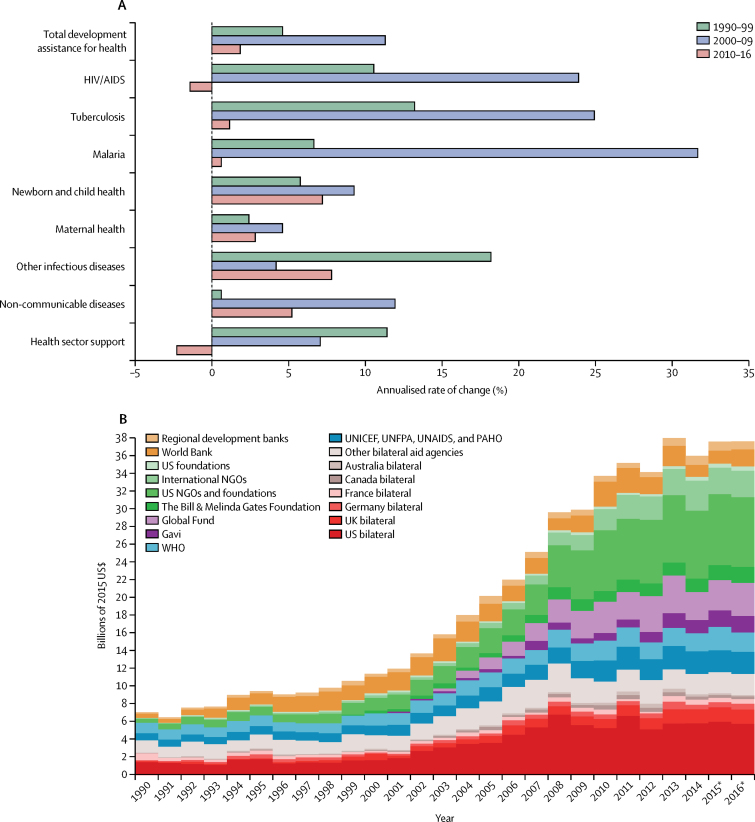
Figure 5, Figure 6 highlight important trends related to development assistance for health, reported in 2015 US $. In 2016, total development assistance for health amounted to US$37·6 billion. Figure 5 shows the most recent growth rates in the disbursement of development assistance for health (figure 5A), and recent disbursements disaggregated by channel of assistance (figure 5B). In the 1990s, total development assistance for health grew at an annualised rate of 4·6%. During the first decade of the millennium, development assistance for health grew at an annualised rate of 11·3%, with especially large annualised growth for target areas associated with the Millennium Development Goals. Annualised growth between 2000 and 2009 was the highest for malaria, tuberculosis, and HIV/AIDS. Since 2010, total development assistance for health has grown at an annualised growth rate of 1·8%, with reductions in spending (−1·4%) for the largest health focus area, which is HIV/AIDS.
Figure 5.
Changes in development assistance for health disbursements, 1990–2016
Development assistance for health as annualised growth rates (A) and disaggregated by channel (B). (A) Growth rates are shown for 1990–99, 2000–09, and 2010–16. (B) Estimates are shown from 1990 to 2016, all in billions of 2015 US$. World Bank includes the International Development Association and the International Bank for Reconstruction and Development; and regional development banks include the Inter-American Development Bank, the African Development Bank, and the Asian Development Bank. NGOs=non-governmental organisations. Global Fund=The Global Fund to Fight AIDS, Tuberculosis and Malaria. Gavi=Gavi, the Vaccine Alliance. UNICEF=United Nations Children's Fund. UNFPA=United Nations Population Fund. UNAIDS=Joint United Nations Programme on HIV/AIDS. PAHO=Pan American Health Organization. *Data for 2015 and 2016 are preliminary estimates based on budget data and estimation.
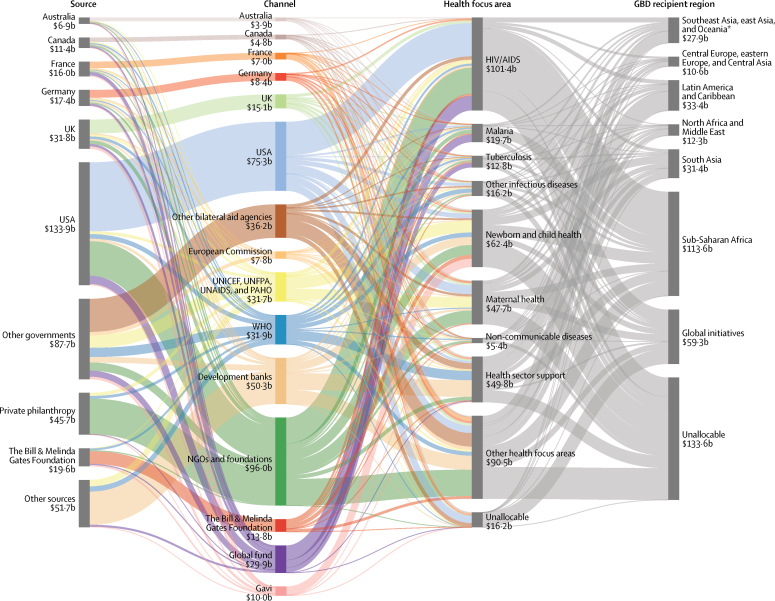
Figure 6.
Flow of developmental assistance for health for all funds dispersed, 1995–2014
The figures shows the flow of development assistance for health from sources, through intermediary channels, to health focus areas and the region where the development assistance was ultimately received. Data are cumulative developmental assistance for health from 1995 to the end of 2014 in billions of 2015 US$. Each column disaggregates the total developmental assistance for health disbursed from 1995 through to 2014, which was US$423·0 billion. Funding sources are shown on the left, channels in the middle left, health focus areas on the middle right, and Global Burden of Disease (GBD) recipient super-regions are on the right. Private philanthropy includes corporate donations among other private philanthropy. Other sources include debt repayments and funds whose sources are unallocable. NGOs and foundations include non-governmental organisations and US foundations. UN Agencies include the UN Children's Fund, UN Population Fund, Joint UN Programme on HIV/AIDS, Pan American Health Organization, and WHO. Development banks include the World Bank International Development Association, the World Bank International Bank for Reconstruction and Development, the Inter-American Development Bank, the African Development Bank, and the Asian Development Bank. Other health focus areas correspond to developmental assistance for health for which we have project-level information but which is not identified as funding any of the health focus areas we tracked. Unallocable in terms of health focus area corresponds to developmental assistance for health for which we do not have project-level information and cannot parse across health focus areas. Latin America and the Caribbean includes Argentina, Chile, and Uruguay, which are now high-income countries when they were each middle-income countries. Southeast Asia, east Asia, and Oceania includes South Korea, which is also now a high-income country when it was a middle-income country. Unallocable in recipient region also corresponds to development assistance for health for which we do not have project-level information and thus, cannot parse across recipients. UNICEF=United Nations Children's Fund. UNFPA=United Nations Population Fund. UNAIDS=Joint United Nations Programme on HIV/AIDS. PAHO=Pan American Health Organization. Global Fund=The Global Fund to Fight AIDS, Tuberculosis and Malaria. Gavi=Gavi, the Vaccine Alliance.
Between 1995 and 2014, $423·0 billion of development assistance for health was disbursed to low-income and middle-income countries (figure 6). 27·0% of development assistance for health went to sub-Saharan Africa, whereas 7·9% flowed to Latin America and the Caribbean. Across health focus areas, 24·0% of development assistance for health focused on HIV/AIDS, while child and maternal health projects received 14·8% and 11·3% of funding, respectively. The majority of the resources were provided by national treasuries, including the USA at 34·0% and the UK at 10·9%, of total development assistance for health in 2016. Major shares of development assistance for health also flowed through multilateral development agencies, such as the World Bank and WHO, which disbursed 5·1% and 5·8%, respectively, and private-public partnerships, such as the Global Fund and Gavi, who disbursed 9·9% and 4·9%, respectively, in 2016.
Health spending by type of goods and service
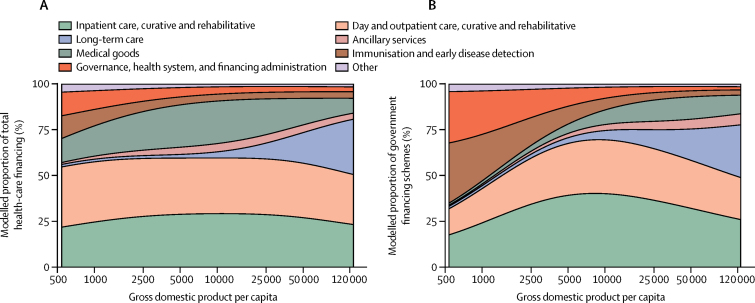
Figure 7 shows that spending by type of goods and service was relatively constant across different levels of economic development. At the median GDP per capita ($8346), 29·0% of total spending was on inpatient curative and rehabilitative care, 30·6% is on day and outpatient curative and rehabilitative care, and 23·5% is on medical goods, which include pharmaceuticals, in 2014 (figure 7A). These values drop marginally at the highest values of GDP per capita, where long-term care is more prominent.
Figure 7.
Composition of health spending by type of goods and services, 2014
The modelled proportion of total (A) and government (B) health spending across gross domestic product per capita by types of goods and services. Other health spending includes all other health spending that is not otherwise classified in this taxonomy. Spending on education and counselling programs, epidemiological surveillance, and disaster preparedness was excluded.
Government spending by type of goods and service is very similar to total spending (figure 7B), although the government spends less on medical goods, in particular above the median GDP capita, and slightly more on immunisations and early disease detection at the very lowest levels of GDP per capita.
Discussion
This study identifies health spending trends and country-specific deviations for 184 nations from 1995 to 2014. The findings show that, on average, economic development is associated with increases in health spending per person and decreases in the share of spending that is financed OOP. In addition to this, we show that development assistance for health also fits neatly into the framework outlined in the health financing transition—like OOP health spending, the share of health financing from development partners decreases precipitously with economic development.
Figure 3 highlights three distinct health financing stages that emerge along the spectrum of economic development. In the first stage, health financing is dominated by development assistance for health and OOP. In the second stage, development assistance for health subsides, and the primary sources of health-care financing are OOP and domestic government spending. Finally, the third stage includes countries with the highest GDP per capita, which tend to finance health care using government spending. While these stages are conceptually clear, and are neatly shown in figure 3, it is important to note the great deal of variation that exists around these trends. While the empirical evidence supporting the health financing transition is robust on average, many counter-examples exists. Some upper-middle-income countries such as Angola and Turkmenistan spent only $228 and $396, respectively, per capita on health in 2014. Similarly, some lower-middle-income countries such as Sudan and Federated States of Micronesia rely heavily on OOP and development assistance for health. Despite the clear and intuitive trends articulated by the health financing transition, an important conclusion of this research is that country-specific characteristics are central to health financing, and that time and economic development do not guarantee a transition towards adequate prepaid spending needed to support universal health coverage. The trends shown here are encouraging, although substantive deviation from the trends are in some cases worrisome.
At the nexus of economic development and health financing are concerns related to what some have called the missing middle. This missing middle concept, which has been debated, asserts that in the process of transitioning from low-income to middle-income status, countries receive less development assistance for health although they are not yet able to domestically raise sufficient government resources to replace the lost external resources.43, 44 Identifying, understanding, and managing this potential is of crucial importance because more than 70% of the world's poor live in middle-income-countries.45 A result of a premature transition from development assistance for health would be a reduction in prepaid, pooled resources, and an increase in OOP financing. Our estimates provide some evidence of this occurrence, because lower-middle-income countries finance more of their health spending OOP than any other income group.
Trends in development assistance for health disbursement draw even more attention to the missing middle concern, because the growth rates of development assistance for health disbursement have slowed substantially since 2010, causing some donors to re-evaluate their own development assistance for health allocation policies.46 Along with this, some key health focus areas have recently experienced tepid growth, and funds for HIV/AIDS, which for the past 15 years has been the largest development assistance health focus area, have contracted since 2010. In some cases this comes after major gains have been made.47, 48, 49 For many low-income countries and some missing middle-income countries, these trends could have crucial impacts on the provision of essential health services, unless the trends reverse or domestic funds are identified.
Development assistance for health disbursements grew substantially between 2000 and 2010. Although this period, referred to as the so-called golden age of development assistance for health growth, saw annual disbursement more than triple, how these disbursements affected total health spending in low-income and middle-income countries remains unclear.50 In some cases, this disbursement might prop up domestic spending and hide the true amount of spending that is being financed domestically. In other cases, development assistance could have crowded out or replaced government spending that would have otherwise exsisted.51, 52 Because development assistance for health is not always predicable and sustainable, ongoing maturation of domestic prepaid financing is important.
While a shift from a reliance on development assistance for health can be externally imposed upon some countries, the shift from a reliance on OOP must be driven by internal, institutional forces. Political efforts and health-system reform have encouraged movement away from OOP financing in countries such as Mexico and Thailand. While these countries reduced the share of health spending that was OOP as middle-income countries, this transition occurs, on average, later in the process of economic development. Our estimates (Figure 2, Figure 3) show that while the share of health spending from OOP peaks at GDP per capita of $2456, it remains a major source of spending for many countries beyond this point. The modelled trends do not show an accelerated decline in spending from OOP till above GDP per capita of $20 000. This threshold is crucial because OOP financing has been linked to less access to prescribed medicines, less access to care, more adverse health outcomes, and impoverishment.15, 16, 20, 53
In addition to tracking total health spending and health spending by source, this study also highlights how the type of health-care services purchased is relatively stable across the spectrum of economic development. While these trends are quite stable in relative terms, the exponential growth of total health spending means that in absolute terms, much more is being spent on each type of goods and service in high-income countries than in low-income countries. In relative terms, trends do show that countries with the lower GDP per capita spent more proportionally on medical goods, which includes pharmaceuticals, and their governments spend relatively more on immunisation and early disease detection. Most clear is that spending on long-term care is minimal in low-income countries, whereas it grows to 20% in high-income countries. In many low-income countries, long-term care remains informal and relies on volunteers and community care.54
Long-term care is only one type of service associated with the epidemiological transition and the shift from a health burden dominated by infectious and childhood diseases to a health burden dominated non-communicable, chronic conditions. While many middle-income countries are dealing with this double burden simultaneously, planning within low-income countries should revolve around ensuring progress along this epidemiological transition, while also anticipating the additional financing challenges associated with this transition.55 In many cases, these challenges include caring for an older population with chronic conditions and in many cases complex comorbidities. Recent US research shows that in the USA, 70% of personal health spending is on non-communicable diseases.56 This research shows that a dramatic shift in how resources are allocated across types of goods and services is not the norm, although, in most cases, considerably more resources are used to care for these populations.
Sufficient supply of prepaid, pooled health resources, such as government spending, is crucial in the pursuit of universal health coverage.57 If, like the health financing transition describes, this health spending is encouraged by economic development, then economic growth is a catalyst for progress towards universal health coverage. This research affirms these trends on average, but also highlights substantial deviations from these trends. The reality is that many factors determine a country's health spending level, including factors related to the population's age pattern and health burden, the supply and demand of health care, prices, adaptation of new medical technology, and many health-system characteristics, including health-system efficiency.58, 59, 60 These same factors might also be integral in transitioning from reliance on OOP financing to prepaid financing. While national income can constrain health spending, these shifts in financing might be more connected to comprehensive socioeconomic development. Moreover, health-system reform is generally a political process that is affected, but not purely determined, by any one of these additional factors. Ongoing assessment of these factors is crucial for informed pursuit of universal health coverage.
This research has several limitations that revolve around the data availability and data quality. The WHO Global Health Observatory is the only curator of some of the estimates used in this study: government, prepaid private, and OOP health spending estimates that span worldwide. These data are intended to be comparable, although estimates across time and release versions can vary substantially. The estimates of private spending, including OOP and prepaid private spending, are particularly concerning because the underlying input data are sparse and vary in quality. In addition, these data are reported as spending agent, rather than as the source of the financing. Spending estimates fluctuate drastically across time for many countries and might hint at inconsistency in tracking across time rather than dramatic spending shifts. Moving forward, more effort is needed to evaluate and validate these health financing data.
An additional data limitation is that NHA reports are sparse and contain gaps.61 These issues prevent analysis at a more granular level. Although the framework for completing NHAs is standardised, the actual methods used to complete an NHA report vary across countries and time. This is particularly the case in many low-income and middle-income settings, where generation of an NHA relies less on routinely collected data and more heavily on approximation. Like the data from the WHO Global Health Observatory, these data are tremendously powerful, although scarcity and quality suggest additional assessment, validation, and correcting of any discovered biases is necessary.
Furthermore, like the spending by source data from the WHO and the spending by type data from the NHAs, IHME's development assistance for health data relies on estimation and approximation to fill in incomplete data. In particular, estimates of development assistance for health rely on modelling of disbursement data when only commitment data are available and keyword searches of project level data when health focus areas are not clearly identified. In addition, these data capture development assistance for health from the bilateral aid agencies from high-income countries only, missing any so-called South–South cooperation in the health sector. In addition to these, some development assistance for health is not allocable to a specific country because the development agency does not report project level information. When development assistance for health can be allocated to a specific country, it might remain unclear if all the development assistance for health was actually disbursed within that country. Because country-specific development assistance for health estimates are used to estimate domestic government and private health spending, development assistance for health measurement error might cause measurement error in these other metrics. Measurement error and misalignment of government spending and development assistance for health even lead to domestic government spending estimates for some countries falling below zero, after development assistance for health provided to the government is removed. More transparency and complete reporting of development assistance for health, including precise information about where resources are spent and who was the primary recipient, would lead to improved development assistance for health tracking.
Two final data limitations are that many of the estimates reported in this study are reported using PPP $ and none of the data sources used for this study provide subnational spending estimates. The empirical basis for some purchasing power parity adjustments is weak, despite ongoing efforts to improve them.62 In addition, the absence of subnational data prevented the examination of within-country heterogeneity in health financing. GDP per capita does not capture income equality, and health spending within many countries varies substantially, and many cases substantial health spending inequalities exist.63, 64 Spending levels and the share prepaid can vary greatly, particularly in countries with a small government share of health spending. Many key dimensions, such as income, wealth, race, geography, age, sex, and economic status, are glossed over when estimates are reported in national, per capita terms only. Because this study focuses on national spending, it abstracts from these critical variations. Future analyses should aim to assess the health financing transition within countries, while globally more efforts need to be made to collect subnational health financing data.
In addition to these data concerns, it is also important to recognise that this research has not tracked health spending in relation to health outcomes. More spending on health does not guarantee better health outcomes. A recent report from the OECD have shown that a substantial share of health spending in high-income countries is wasted.65 Coupled with efforts to ensure adequate prepaid resources for health must be efforts to ensure that health services are provided efficiently and equitably.
In conclusion, the availability of prepaid resources for health, such as government spending, is one of many determinants of access to health care, and can lead to population health gains. Economic development is associated with an increase in spending and specifically an increase in prepaid resources. This is at the core of the pursuit for universal health coverage. This research also points to countries that deviate from the trends, spending more or less than expected, based on their level of economic development. This information is valuable to planners assessing funding gaps and financing opportunities, and can be used to provide insight into what future health financing challenges are likely. Tracking changes in health financing patterns across time and benchmarking against global trends is vital to addressing missed opportunities, ensuring access to medicines and high quality services, and the pursuit of universal health coverage.
Correspondence to: Dr Joseph L Dieleman, 2301 Fifth Avenue, Suite 600, Seattle, WA 98121, USA dieleman@uw.edu
For WHO global health expenditure database see http://apps.who.int/nha/database
For WHO Global Health Observatory see http://www.who.int/gho/en/
For the International Monetary Fund world economic outlook database see https://www.imf.org/external/pubs/ft/weo/2016/02/weodata/index.aspx
For the World Bank Databank see http://databank.worldbank.org/data/home.aspx
This online publication has been corrected. The corrected version first appeared at thelancet.com on May 18, 2017
Acknowledgments
Acknowledgments
We would like to acknowledge George Schieber for his review of preliminary drafts of this report. We thank the countless individuals who have contributed to the Financing Global Health Study 2016 in various capacities. Lastly, we extend out thanks to the editorial team at IHME for their efforts specifically Joan Williams, Adrienne Chew, Kate Muller, Dawn Shepard, Katherine Leach-Kemon, Margot Case, and Sean McKee. We also thank the remainder of the IHME Financial Resources for Health research team for their support—specifically Cody Horst, Zhiyin Li, and Ellen Squires.
Contributors
Joseph L Dieleman prepared the first draft and was responsible for the conception of this study. Erica Eldrenkamp, Joseph L Dieleman, and Matthew T Schneider were responsible for methods development. Yingying Liu, Alex Reynolds, Madeline Campbell, Erika Eldrenkamp, Nafis Sadat, Ajay Tandon, Christoph Kurowski, and Taylor Matyasz all contributed to data analysis. Victoria Fan, Annie Haakenstad, Jennifer Kates, Joseph Dieleman, Angela Micah, Ajay Tandon, Christoph Kurowski, David Evans, Christopher J L Murray, and Matthew Schneider all contributed to subsequent iterations of the draft. Abigail Chapin and Joseph L Dieleman provided project management. All other authors provided data or developed models, reviewed results, initiated modelling infrastructure, or reviewed and contributed to this report.
Global Burden of Disease Health Financing Collaborator Network
Joseph Dieleman, Madeline Campbell, Abigail Chapin, Erika Eldrenkamp, Victoria Y Fan, Annie Haakenstad, Jennifer Kates, Yingying Liu, Taylor Matyasz, Angela Micah, Alex Reynolds, Nafis Sadat, Matthew T Schneider, Reed Sorensen, Tim Evans, David Evans, Christoph Kurowski, Ajay Tandon, Kaja M Abbas, Semaw Ferede Abera, Aliasghar Ahmad Kiadaliri, Kedir Yimam Ahmed, Muktar Beshir Ahmed, Khurshid Alam, Reza Alizadeh-Navaei, Ala'a Alkerwi, Erfan Amini, Walid Ammar, Stephen Marc Amrock, Carl Abelardo T Antonio, Tesfay Mehari Atey, Leticia Avila-Burgos, Ashish Awasthi, Aleksandra Barac, Oscar Alberto Bernal, Addisu Shunu Beyene, Tariku Jibat Beyene, Charles Birungi, Habtamu Mellie Bizuayehu, Nicholas J K Breitborde, Lucero Cahuana-Hurtado, Ruben Estanislao Castro, Ferran Catalia-Lopez, Koustuv Dalal, Lalit Dandona, Rakhi Dandona, Pieter de Jager, Samath D Dharmaratne, Manisha Dubey, Carla Sofia e Sa Farinha, Andre Faro, Andrea B Feigl, Florian Fischer, Joseph Robert Anderson Fitchett, Nataliya Foigt, Ababi Zergaw Giref, Rahul Gupta, Samer Hamidi, Hilda L Harb, Simon I Hay, Delia Hendrie, Masako Horino, Mikk Jürisson, Mihajlo B Jakovljevic, Mehdi Javanbakht, Denny John, Jost B Jonas, Seyed M. Karimi, Young-Ho Khang, Jagdish Khubchandani, Yun Jin Kim, Jonas M Kinge, Kristopher J Krohn, G Anil Kumar, Hassan Magdy Abd El Razek, Mohammed Magdy Abd El Razek, Azeem Majeed, Reza Malekzadeh, Felix Masiye, Toni Meier, Atte Meretoja, Ted R Miller, Erkin M Mirrakhimov, Shafiu Mohammed, Vinay Nangia, Stefano Olgiati, Abdalla Sidahmed Osman, Mayowa O Owolabi, Tejas Patel, Angel J Paternina Caicedo, David M Pereira, Julian Perelman, Suzanne Polinder, Anwar Rafay, Vafa Rahimi-Movaghar, Rajesh Kumar Rai, Usha Ram, Chhabi Lal Ranabhat, Hirbo Shore Roba, Joseph Salama, Miloje Savic, Sadaf G Sepanlou, Mark G Shrime, Roberto Tchio Talongwa, Braden J Te Ao, Fabrizio Tediosi, Azeb Gebresilassie Tesema, Alan J Thomson, Ruoyan Tobe-Gai, Roman Topor-Madry, Eduardo A Undurraga, Tommi Vasankari, Francesco S Violante, Andrea Werdecker, Tissa Wijeratne, Gelin Xu, Naohiro Yonemoto, Mustafa Z Younis, Chuanhua Yu, Zoubida Zaidi, Maysaa El Sayed Zaki, Christopher J L Murray.
Affiliations
Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA, USA; (Prof J Dieleman PhD, M Campbell BS, A Chapin BA, E Eldrenkamp BA, A Haakenstad MA, T Matyasz MS, A Micah PhD, N Sadat MA, M T Schneider MPH, R Sorensen MPH, Y Liu MS, A Reynolds BA, Prof S I Hay DSc, K J Krohn BA, J Salama, Prof C J L Murray DPhil, L Dandona MD, R Dandona PhD); University of Hawaii at Manoa, Honolulu, HI, USA (V Y Fan ScD); François-Xavier Bagnoud Center for Health and Human Rights (V Y Fan ScD), Department of Global Health and Population, TH Chan School of Public Health (A B Feigl ScD), Harvard University, Boston, MA, USA (J R A Fitchett MD); Center for Global Development, Washington, DC, USA (V Y Fan ScD); Kaiser Family Foundation, Washington, DC, USA (J Kates PhD); World Bank, Washington, DC, USA (T Evans DPhil, D Evans PhD, C Kurowski MD, A Tandon PhD); Virginia Tech, Blacksburg, VA, USA (Prof K M Abbas PhD); School of Public Health, College of Health Sciences (S F Abera MSc), Mekelle University, Mekelle, Ethiopia (T M Atey MS, A G Tesema MPH); Food Security and Institute for Biological Chemistry and Nutrition, University of Hohenheim, Stuttgart, Germany (S F Abera MSc); Department of Clinical Sciences Lund, Orthopedics, Clinical Epidemiology Unit, Lund University, Lund, Sweden (A Ahmad Kiadaliri PhD); Debre Markos University, Debre Markos, Ethiopia (K Y Ahmed MPH); College of Health Sciences, Department of Epidemiology, ICT and e-Learning Coordinator, Jimma University, Jimma, Ethiopia (M B Ahmed MPH); Murdoch Childrens Research Institute (K Alam PhD), The University of Melbourne, Melbourne, VIC, Australia (K Alam PhD); The University of Sydney, Sydney, NSW, Australia (K Alam PhD); Gastrointestinal Cancer Research Center, Mazandaran University of Medical Sciences, Sari, Iran (R Alizadeh-Navaei PhD); Luxembourg Institute of Health (LIH), Strassen, Luxembourg (A Alkerwi PhD); Uro-Oncology Research Center (E Amini MD), Endocrinology and Metabolism Research Institute (E Amini MD) Digestive Diseases Research Institute (Prof R Malekzadeh MD, S G Sepanlou PhD), Sina Trauma and Surgery Research Center (Prof V Rahimi-Movaghar MD), Tehran University of Medical Sciences, Tehran, Iran; Ministry of Public Health, Beirut, Lebanon (W Ammar PhD, H L Harb MPH); Oregon Health & Science University, Portland, OR, USA (S M Amrock MD); Department of Health Policy and Administration, College of Public Health, University of the Philippines Manila, Manila, Philippines (C A T Antonio MD); National Institute of Public Health, Cuernavaca, Mexico (L Avila-Burgos PhD, L Cahuana-Hurtado PhD); Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India (A Awasthi MSc); Faculty of Medicine, University of Belgrade, Belgrade, Serbia (A Barac PhD); University Andes, Bogota, Colombia (O A Bernal PhD); College of Health and Medical Science (A S Beyene MPH), College of Health and Medical Sciences (H S Roba MPH), Haramaya University, Harar, Ethiopia; Addis Ababa University, Addis Ababa, Ethiopia (T J Beyene MS, A Z Giref PhD); Wageningen University, Wageningen, Netherlands (T J Beyene MS); University College London, London, UK (C Birungi MS); Debre Markos University, Debre Markos Town, Ethiopia (H M Bizuayehu MPH); Ohio State University, Columbus, OH, USA (Prof N J K Breitborde PhD); Universidad Diego Portales, Santiago, Chile (R E Castro PhD); Department of Medicine, University of Valencia/INCLIVA Health Research Institute and CIBERSAM, Valencia, Spain (F Catalá-López PhD); Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, ON, Canada (F Catalá-López PhD); Centre for Injury Prevention and Safety Promotion, School of Health and Medical Sciences, Orebro University, Orebro, Sweden (Prof K Dalal PhD); Public Health Foundation of India, New Delhi, India (L Dandona, R Dandona, G A Kumar PhD); School of Public Health, University of the Witwatersrand, Johannesburg, South Africa (P de Jager FCPHM(SA)); National Health Laboratory Service, National Institute for Occupational Health, Johannesburg, South Africa (P de Jager FCPHM(SA)); Department of Community Medicine, Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka (S D Dharmaratne MD); International Institute for Population Sciences, Mumbai, India (M Dubey MPhil, Prof U Ram PhD); DGS Directorate General of Health, Lisboa, Portugal (C S E S Farinha MSc); Universidade Aberta, Lisboa, Portugal (C S E S Farinha MSc); Federal University of Sergipe, Aracaju, Brazil (Prof A Faro PhD); School of Public Health, Bielefeld University, Bielefeld, Germany (F Fischer PhD); Institute of Gerontology, Academy of Medical Science, Kyiv, Ukraine (N Foigt PhD); West Virginia Bureau for Public Health, Charleston, WV, USA (R Gupta MD); Hamdan Bin Mohammed Smart University, Dubai, United Arab Emirates (S Hamidi DrPH); Oxford Big Data Institute, Li Ka Shing Centre for Health Information and Discovery, University of Oxford, Oxford, UK (Prof S I Hay DSc); Centre for Population Health Research (D Hendrie MA), Curtin University, Bentley, WA, Australia; Department of Health and Human Services, Nevada Division of Public and Behavioral Health, Carson City, NV, USA (M Horino MPH); Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia (Prof M B Jakovljevic PhD); University of Aberdeen, Aberdeen, UK (M Javanbakht PhD); International Center for Research on Women, New Delhi, India (D John MPH); Department of Ophthalmology, Medical Faculty Mannheim, Ruprecht-Karls-University Heidelberg, Mannheim, Germany (Prof J B Jonas MD); Institute of Family Medicine and Public Health, University of Tartu, Tartu, Estonia (M Jürisson MD); University of Washington Tacoma, Tacoma, WA, USA (S M Karimi PhD); College of Medicine, Seoul National University, Seoul, South Korea (Prof Y Khang MD); Ball State University, Muncie, IN, USA (J Khubchandani PhD); Southern University College, Skudai, Malaysia (Y J Kim PhD); Norwegian Institute of Public Health, Oslo, Norway (J M Kinge PhD, M Savic PhD); Mansoura Faculty of Medicine, Mansoura, Egypt (H Magdy Abd El Razek MBBCH); Aswan University Hospital, Aswan Faculty of Medicine, Aswan, Egypt (M Magdy Abd El Razek MBBCh); Imperial College London, London, UK (Prof A Majeed MD); University of Zambia, Lusaka, Zambia (F Masiye); Martin Luther University Halle-Wittenberg, Halle (Saale), Germany (T Meier PhD); Department of Medicine (A Meretoja PhD), University of Melbourne, Footscray, VIC, Australia (Prof T Wijeratne MD); Department of Neurology, Helsinki University Hospital, Helsinki, Finland (A Meretoja PhD); Pacific Institute for Research & Evaluation, Calverton, MD, USA (T R Miller PhD); Centre for Population Health (T R Miller PhD), Curtin University, Perth, WA, Australia; Kyrgyz State Medical Academy, Bishkek, Kyrgyzstan (Prof E M Mirrakhimov PhD); National Center of Cardiology and Internal Disease, Bishkek, Kyrgyzstan (Prof E M Mirrakhimov PhD); Health Systems and Policy Research Unit, Ahmadu Bello University, Zaria, Nigeria (S Mohammed PhD); Institute of Public Health, Heidelberg University, Heidelberg, Germany (S Mohammed PhD); Suraj Eye Institute, Nagpur, India (V Nangia MD); State University of Bergamo, Bergamo, Italy (S Olgiati PhD); Public Health Institute Sudan, Khartoum, Sudan (A S Osman); Department of Medicine, Ibadan, Nigeria (M O Owolabi MD); Blossom Specialist Medical Center, Ibadan, Nigeria (M O Owolabi MD); Mount Sinai Health System, New York, NY, USA (T Patel MD); Universidad de Cartagena, Cartagena, Colombia (A J Paternina Caicedo MD); Public Health Dynamics Laboratory, University of Pittsburgh, Pittsburgh, PA, USA (A J Paternina Caicedo MD); REQUIMTE/LAQV, Laboratorio de Farmacognosia, Departamento de QuÃmica, Faculdade de FarmÃicia, Universidade do Porto, Porto, Portugal (Prof D M Pereira PhD); National School of Public Health, Lisbon, Portugal (Prof J Perelman PhD); Department of Public Health, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands (S Polinder PhD); Contech International Health Consultants, Lahore, Pakistan (A Rafay MS); Contech School of Public Health, Lahore, Pakistan (A Rafay MS); Society for Health and Demographic Surveillance, Suri, India (R K Rai MPH); Institute for Poverty Alleviation and International Development (C L Ranabhat PhD), Wonju College of Medicine (C L Ranabhat PhD), Yonsei University, Wonju, South Korea; Harvard Medical School, Boston, MA, USA (M G Shrime MD); Ministry of Health, MINSANTE, Yaounde, Cameroon (R T Talongwa MD); Auckland University of Technology, Auckland, new zealand (B J Te Ao MPH); Swiss Tropical and Public Health Institute, University of Basel, Basel, Switzerland (F Tediosi PhD); Adaptive Knowledge Management, Victoria, BC, Canada (A J Thomson PhD); National Center for Child Health and Development, Tokyo, Japan (R Tobe-Gai PhD); Institute of Public Health, Faculty of Health Sciences, Jagiellonian University Medical College, Krakow, Poland (R Topor-Madry PhD); Faculty of Health Sciences, Wroclaw Medical University, Wroclaw, Poland (R Topor-Madry PhD); Brandeis University, Waltham, MA, USA (E A Undurraga PhD); UKK Institute for Health Promotion Research, Tampere, Finland (Prof T Vasankari PhD); University of Bologna, Bologna, Italy (Prof F S Violante MD); Competence Center Mortality-Follow-Up of the German National Cohort, Federal Institute for Population Research, Wiesbaden, Germany (A Werdecker PhD); Western Health, Footscray, VIC, Australia (Prof T Wijeratne MD); Department of Neurology, Jinling Hospital, Nanjing University School of Medicine, Nanjing, China (Prof G Xu PhD); Department of Biostatistics, School of Public Health, Kyoto University, Kyoto, Japan (N Yonemoto MPH); Jackson State University, Jackson, MS, USA (Prof M Z Younis DrPH); Department of Epidemiology and Biostatistics, School of Public Health, Wuhan University, Wuhan, China (Prof C Yu PhD), Global Health Institute, Wuhan University, Wuhan, China (Prof C Yu PhD); University Hospital, Setif, Algeria (Prof Z Zaidi PhD); and Faculty of Medicine, Mansoura University, Mansoura, Egypt (Prof M E Zaki PhD).
Declaration of interests
SIH is funded by a Senior Research Fellowship from the Wellcome Trust [095066], and grants from the Bill & Melinda Gates Foundation (OPP1119467, OPP1093011, OPP1106023 and OPP1132415). MBJ acknowledges contributions on Serbia and Western Balkans/former Yugoslavia countries were co-funded with Grant OI 175 014 financed by the Ministry of Science Education and Technological Development of Serbia. MOO is supported by U54 HG007479 from the National Institutes of Health and H3Africa. MGS reports grants from GE Foundation Safe Surgery 2020, grants from Steven C and Carmella Kletjian Foundation outside of the the submitted work. BJTA reports other from Health Research Council of New Zealand, outside of the submitted work.
Contributor Information
Global Burden of Disease Health Financing Collaborator Network:
Joseph Dieleman, Madeline Campbell, Abigail Chapin, Erika Eldrenkamp, Victoria Y Fan, Annie Haakenstad, Jennifer Kates, Yingying Liu, Taylor Matyasz, Angela Micah, Alex Reynolds, Nafis Sadat, Matthew T Schneider, Reed Sorensen, Tim Evans, David Evans, Christoph Kurowski, Ajay Tandon, Kaja M Abbas, Semaw Ferede Abera, Aliasghar Ahmad Kiadaliri, Kedir Yimam Ahmed, Muktar Beshir Ahmed, Khurshid Alam, Reza Alizadeh-Navaei, Ala'a Alkerwi, Erfan Amini, Walid Ammar, Stephen Marc Amrock, Carl Abelardo T Antonio, Tesfay Mehari Atey, Leticia Avila-Burgos, Ashish Awasthi, Aleksandra Barac, Oscar Alberto Bernal, Addisu Shunu Beyene, Tariku Jibat Beyene, Charles Birungi, Habtamu Mellie Bizuayehu, Nicholas J K Breitborde, Lucero Cahuana-Hurtado, Ruben Estanislao Castro, Ferran Catalia-Lopez, Koustuv Dalal, Lalit Dandona, Rakhi Dandona, Pieter de Jager, Samath D Dharmaratne, Manisha Dubey, Carla Sofia e Sa Farinha, Andre Faro, Andrea B Feigl, Florian Fischer, Joseph Robert Anderson Fitchett, Nataliya Foigt, Ababi Zergaw Giref, Rahul Gupta, Samer Hamidi, Hilda L Harb, Simon I Hay, Delia Hendrie, Masako Horino, Mikk Jürisson, Mihajlo B Jakovljevic, Mehdi Javanbakht, Denny John, Jost B Jonas, Seyed M. Karimi, Young-Ho Khang, Jagdish Khubchandani, Yun Jin Kim, Jonas M Kinge, Kristopher J Krohn, G Anil Kumar, Hassan Magdy Abd El Razek, Mohammed Magdy Abd El Razek, Azeem Majeed, Reza Malekzadeh, Felix Masiye, Toni Meier, Atte Meretoja, Ted R Miller, Erkin M Mirrakhimov, Shafiu Mohammed, Vinay Nangia, Stefano Olgiati, Abdalla Sidahmed Osman, Mayowa O Owolabi, Tejas Patel, Angel J Paternina Caicedo, David M Pereira, Julian Perelman, Suzanne Polinder, Anwar Rafay, Vafa Rahimi-Movaghar, Rajesh Kumar Rai, Usha Ram, Chhabi Lal Ranabhat, Hirbo Shore Roba, Joseph Salama, Miloje Savic, Sadaf G Sepanlou, Mark G Shrime, Roberto Tchio Talongwa, Braden J Te Ao, Fabrizio Tediosi, Azeb Gebresilassie Tesema, Alan J Thomson, Ruoyan Tobe-Gai, Roman Topor-Madry, Eduardo A Undurraga, Tommi Vasankari, Francesco S Violante, Andrea Werdecker, Tissa Wijeratne, Gelin Xu, Naohiro Yonemoto, Mustafa Z Younis, Chuanhua Yu, Zoubida Zaidi, Maysaa El Sayed Zaki, and Christopher J L Murray
Supplementary Material
References
- 1.Gottret P, Schieber G. Health financing revisited. A practitioner's guide. The World Bank; Washington DC: 2006. [Google Scholar]
- 2.Emanuel E, Tanden N, Altman S. A systemic approach to containing health care spending. N Engl J Med. 2012;367:949–954. doi: 10.1056/NEJMsb1205901. [DOI] [PubMed] [Google Scholar]
- 3.Center for American Progress Cutting health care costs. Leading experts propose bold solutions. 2012. https://www.americanprogress.org/issues/healthcare/news/2012/08/02/11970/cutting-health-care-costs/ (accessed Dec 5, 2016).
- 4.Herman B. Healthcare spending growth rate rises again in 2015. Mod. Healthc. 2016. http://www.modernhealthcare.com/article/20160713/news/160719963 (accessed Dec 5, 2016).
- 5.United Nations Population Fund The Prime Minister of Tanzania calls on regional leaders to increase health spending to 15 per cent of national budgets and to strive for achieving health MDGs. 2007. http://www.unfpa.org/press/prime-minister-tanzania-calls-regional-leaders-increase-health-spending-15-cent-national (accessed Dec 6, 2016).
- 6.The Center for Global Health and Diplomacy Increasing domestic health funding in Africa. http://www.cghd.org/index.php/publication/global-health-partnerships-and-solutions/expert-spotlight/164-increasing-domestic-health-funding-in-africa (accessed Dec 6, 2016).
- 7.Bill & Melinda Gates Foundation . Bill Gates, Bono call on leaders at World Economic Forum to increase global health spending. Bill & Melinda Gates Foundation; 2002. http://www.gatesfoundation.org/Media-Center/Press-Releases/2002/02/Call-For-Global-Health-Funding (accessed Dec 6, 2016). [Google Scholar]
- 8.National Commission on Fiscal Responsibility and Reform The moment of truth: report of the National Commission on Fiscal Responsibility and Reform. 2010. https://www.fiscalcommission.gov/sites/fiscalcommission.gov/files/documents/TheMomentofTruth12_1_2010.pdf (accessed Jan 7, 2017).
- 9.Fan VY, Savedoff WD. The health financing transition: a conceptual framework and empirical evidence. Soc Sci Med. 2014;105:112–121. doi: 10.1016/j.socscimed.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 10.Savedoff WD, Bitran R, de Ferranti D. Transitions in health financing and policies for universal health coverage: final report of the transitions in Health Financing Project. Results for Development Institute. 2012. http://www.resultsfordevelopment.org/sites/resultsfordevelopment.org/files/THF%20Summary%20-%20Transitions%20in%20Health%20Financing%20and%20Policies%20for%20Universal%20Health%20Coverage.pdf (accessed Jan 7, 2017).)
- 11.Savedoff WD, de Ferranti D, Smith AL, Fan V. Political and economic aspects of the transition to universal health coverage. Lancet. 2012;380:924–932. doi: 10.1016/S0140-6736(12)61083-6. [DOI] [PubMed] [Google Scholar]
- 12.Fan VY, Savedoff WD. The health financing transition: a conceptual framework and empirical evidence. Soc Sci Med. 2014;105:112–121. doi: 10.1016/j.socscimed.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 13.Schieber G, Maeda A. Health care financing and delivery in developing countries. Health Aff (Millwood) 1999;18:193–205. doi: 10.1377/hlthaff.18.3.193. [DOI] [PubMed] [Google Scholar]
- 14.Musgrove P, Zeramdini R, Carrin G. Basic patterns in national health expenditure. Bull World Health Organ. 2002;80:134–142. [PMC free article] [PubMed] [Google Scholar]
- 15.Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff (Millwood) 2007;26:972–983. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]
- 16.Falkingham J. Poverty, out-of-pocket payments and access to health care: evidence from Tajikistan. Soc Sci Med. 2004;58:247–258. doi: 10.1016/s0277-9536(03)00008-x. [DOI] [PubMed] [Google Scholar]
- 17.Piette JD, Heisler M, Wagner TH. Problems paying out-of-pocket medication costs among older adults with diabetes. Diabetes Care. 2004;27:384–391. doi: 10.2337/diacare.27.2.384. [DOI] [PubMed] [Google Scholar]
- 18.Damme WV, Leemput LV, Por I, Hardeman W, Meessen B. Out-of-pocket health expenditure and debt in poor households: evidence from Cambodia. Trop Med Int Health. 2004;9:273–280. doi: 10.1046/j.1365-3156.2003.01194.x. [DOI] [PubMed] [Google Scholar]
- 19.Galbraith AA, Wong ST, Kim SE, Newacheck PW. Out-of-pocket financial burden for low-Income families with children: socioeconomic disparities and effects of insurance. Health Serv Res. 2005;40:1722–1736. doi: 10.1111/j.1475-6773.2004.00421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gotsadze G, Bennett S, Ranson K, Gzirishvili D. Health care-seeking behaviour and out-of-pocket payments in Tbilisi, Georgia. Health Policy Plan. 2005;20:232–242. doi: 10.1093/heapol/czi029. [DOI] [PubMed] [Google Scholar]
- 21.van Doorslaer E, O'Donnell O, Rannan-Eliya RP. Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. Lancet. 2006;368:1357–1364. doi: 10.1016/S0140-6736(06)69560-3. [DOI] [PubMed] [Google Scholar]
- 22.Ottersen T, Kamath A, Moon S, Martinsen L, Rottingen J. Development assistance for health: what criteria do multi- and bilateral funders use? Health Econ Policy Law. 2017;12:223–244. doi: 10.1017/S1744133116000475. [DOI] [PubMed] [Google Scholar]
- 23.WHO . Indicator code book. National health accounts. World Health Organization; Geneva, Switzerland: 2015. apps.who.int/nha/database/DocumentationCentre/GetFile/52869001/en (accessed Jan 7, 2017). [Google Scholar]
- 24.James SL, Gubbins P, Murray CJ, Gakidou E. Developing a comprehensive time series of GDP per capita for 210 countries from 1950 to 2015. Popul Health Metr. 2012;10:12. doi: 10.1186/1478-7954-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dieleman JL, Schneider MT, Haakenstad A. Development assistance for health: past trends, associations, and the future of international financial flows for health. Lancet. 2016;387:2536–2544. doi: 10.1016/S0140-6736(16)30168-4. [DOI] [PubMed] [Google Scholar]
- 26.Honaker J, King G, Blackwell M. Amelia II: a program for missing data. J Stat Softw; 45: 1–47.
- 27.Ravishankar N, Gubbins P, Cooley RJ. Financing of global health: tracking development assistance for health from 1990 to 2007. Lancet. 2009;373:2113–2124. doi: 10.1016/S0140-6736(09)60881-3. [DOI] [PubMed] [Google Scholar]
- 28.Dieleman JL, Graves C, Johnson E. Sources and focus of health development assistance, 1990–2014. JAMA. 2015;313:2359–2368. doi: 10.1001/jama.2015.5825. [DOI] [PubMed] [Google Scholar]
- 29.Dieleman JL, Graves CM, Hanlon M. The fungibility of health aid: reconsidering the reconsidered. J Dev Stud. 2013;49:1755–1762. [Google Scholar]
- 30.OECD. Eurostat. WHO A system of health accounts. 2011 (accessed Jan 7, 2017). [Google Scholar]
- 31.OECD A System of Health Accounts. Version 1.0. Organization for Economic Co-Operation and Development. 2000. http://www.who.int/health-accounts/documentation/EnglishSHA.pdf?ua=1 (accessed Jan 7, 2017).
- 32.WHO National health accounts data from 1996 to 2010: a systematic review. WHO. http://www.who.int/bulletin/volumes/93/8/14-145235/en/ (accessed Dec 5, 2016). [DOI] [PMC free article] [PubMed]
- 33.World Economic Outlook Database. April 2016. https://www.imf.org/external/pubs/ft/weo/2016/01/weodata/index.aspx (accessed Dec 15, 2016).
- 34.United Nations Statistics Division-National Accounts http://unstats.un.org/unsd/snaama/Introduction.asp (accessed Dec 15, 2016).
- 35.Maddison Project http://www.ggdc.net/maddison/maddison-project/home.htm (accessed Dec 15, 2016).
- 36.Feenstra RC, Inklaar R, Timmer MP. The next generation of the Penn World Table. Am Econ Rev. 2015;105:3150–3182. [Google Scholar]
- 37.The World Bank World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed Feb 25, 2017).
- 38.Wang H, Naghavi M, Allen C. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jann B, Gutierrez RG. PSPLINE: Stata module providing a penalized spline scatterplot smoother based on linear mixed model technology. Boston College Department of Economics. 2009. https://ideas.repec.org/c/boc/bocode/s456972.html (accessed Dec 29, 2016).
- 40.Muriithi FK. Centerd log-ratio (clr) transformation and robust principal component analysis of long-term NDVI data reveal vegetation activity linked to climate processes. Climate. 2015;3:135–149. [Google Scholar]
- 41.Carpenter J, Bithell J. Bootstrap confidence intervals: when, which, what? A practical guide for medical statisticians. Stat Med. 2000;19:1141–1164. doi: 10.1002/(sici)1097-0258(20000515)19:9<1141::aid-sim479>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 42.Chernick MR. Bootstrap methods: a guide for practitioners and researchers. John Wiley & Sons; 2011. [Google Scholar]
- 43.Dercon S, Lea N. The missing middle - or is there an obvious resource gap for LMICS? 2015. http://users.ox.ac.uk/∼econstd/2015-30-05%20-%20The%20Missing%20Middle_web.pdf (accessed (accessed Jan 7, 2017).
- 44.Kharas H, Prizzon A, Rogerson A. Financing the post-2015 sustainable development goals-a rough roadmap. Overseas Development Institute; London, UK: 2014. [Google Scholar]
- 45.Sumner A. Global poverty and the ‘New Bottom Billion’: what if three-quarters of the world's poor live in middle-income countries? Institute of Development Studies; Brighton, UK: 2010. [Google Scholar]
- 46.The Equitable Access Initiative Expert Panel and Technical Working Group . The equitable access initiative report. The Equitable Access Initiative; Geneva, Switzerland: 2016. http://www.theglobalfund.org/en/equitableaccessinitiative/ (accessed Jan 7, 2017). [Google Scholar]
- 47.Gething PW, Casey DC, Weiss DJ. Mapping Plasmodium falciparum mortality in Africa between 1990 and 2015. N Engl J Med. 2016;375:2435–2445. doi: 10.1056/NEJMoa1606701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bhatt S, Weiss DJ, Cameron E. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015;526:207–211. doi: 10.1038/nature15535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bor J, Herbst AJ, Newell M-L, Bärnighausen T. Increases in adult life expectancy in rural South Africa: valuing the scale-up of HIV treatment. Science. 2013;339 doi: 10.1126/science.1230413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Institute for Health Metrics and Evaluation . Financing global health 2012: the end of the global age? IHME; Seattle, WA: 2012. [Google Scholar]
- 51.Lu C, Schneider MT, Gubbins P, Leach-Kemon K, Jamison D, Murray CJ. Public financing of health in developing countries: a cross-national systematic analysis. Lancet. 2010;375:1375–1387. doi: 10.1016/S0140-6736(10)60233-4. [DOI] [PubMed] [Google Scholar]
- 52.Dieleman JL, Hanlon M. Measuring the displacement and replacement of government health expenditure. Health Econ. 2014;23:129–140. doi: 10.1002/hec.3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Piette JD, Wagner TH, Potter MB, Schillinger D. Health insurance status, cost-related medication underuse, and outcomes among diabetes patients in three systems of care. Med Care. 2004;42:102–109. doi: 10.1097/01.mlr.0000108742.26446.17. [DOI] [PubMed] [Google Scholar]
- 54.WHO . Long-term care in developing countries: ten case-studies. World Health Organization; Geneva, Switzerland: 2002. http://www.who.int/chp/knowledge/publications/Case_studies/en/ (accessed Feb 26, 2017). [Google Scholar]
- 55.Kassebaum NJ, Arora M, Barber RM. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1603–1658. doi: 10.1016/S0140-6736(16)31460-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dieleman JL, Baral R, Birger M. US spending on personal health care and public health, 1996-2013. JAMA. 2016;316:2627–2646. doi: 10.1001/jama.2016.16885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.WHO . The World Health Report. Health systems financing. The path to universal coverage. World Health Organization; Geneva, Switzerland: 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zweifel P, Felder S, Meiers M. Ageing of population and health care expenditure: a red herring? Health Econ. 1999;8:485–496. doi: 10.1002/(sici)1099-1050(199909)8:6<485::aid-hec461>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 59.Savedoff WD. What should a country spend on health care? Health Aff (Millwood) 2007;26:962–970. doi: 10.1377/hlthaff.26.4.962. [DOI] [PubMed] [Google Scholar]
- 60.Sorenson C, Drummond M, Bhuiyan Khan B. Medical technology as a key driver of rising health expenditure: disentangling the relationship. Clin Outcomes Res CEOR. 2013;5:223–234. doi: 10.2147/CEOR.S39634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bui AL, Lavado RL, Johnson EK. National health accounts data from 1996 to 2010: a systematic review. Bull World Health Organ. 2015;93:566–576. doi: 10.2471/BLT.14.145235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Deaton A, Aten B. Trying to understand the PPPs in ICP2011:why are the results so different? National Bureau of Economic Research; Cambridge MA: 2014. [Google Scholar]
- 63.Pannarunothai S, Mills A. The poor pay more: health-related inequality in Thailand. Soc Sci Med. 1997;44:1781–1790. doi: 10.1016/s0277-9536(96)00287-0. [DOI] [PubMed] [Google Scholar]
- 64.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder ÉL. The implications of regional variations in medicare spending. part 2: Health outcomes and satisfaction with care. Ann Intern Med. 2003;138:288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 65.OECD . Tackling wasteful spending on health. OECD Publishing; Paris: 2017. http://dx.doi.org/10.1787/9789264266414-en (accessed Feb 25, 2017). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.