Abstract
Background
The congenital granular cell tumour of the newborn, also known as congenital epulis or Neumann's tumor, is rare. It occurs on the gingiva of the anterior alveolar ridge of the jaws. This lesion behaves in a benign manner and no recurrent or metastatic lesions have been reported.
Case Report
We are reporting a 2-day-old female neonate, who came to our unit with a well defined, solitary, firm mass arising from the maxillary anterior region measuring about 3.5 cms in diameter and causing difficulty in breast feeding but no hindrance to the airway. The mass was surgically excised under general anesthesia. Postoperative wound healing was uneventful.
Conclusion
We have shared our experience in handling this rare type of tumor. We have presented the clinical features and the different modalities of its treatment to spread awareness among clinicians for better management of similar tumors.
Keywords: Neumann's tumor, Congenital Epulis, Congenital Granular Cell Tumor (cgct)
Introduction
Congenital granular cell tumor (CGCT), first described by Neumann in 1871, is a benign soft tissue lesion of the neonate that almost always arises from the alveolar mucosa. It is also known as congenital epulis or Neumann's tumor (1). They are seen 3 times more frequently in the maxillary alveolus than in the mandibular alveolus (2, 3). Females are affected from 8 to 10 times more frequently than males, perhaps indicating a hormonal component in its development (4,5). The typical location is the alveolar ridge of the maxilla near the canine, but the mandibular region can also be involved. Usually, it is presented as a single lesion; however, multiple lesions have been reported in some cases (6,7). This lesion is seen as a mass protruding from the mouth of a newborn and it may interfere with feeding and respiration.
The recommended treatment plan involves prompt surgical resection of the mass under GA or LA, since spontaneous regression is rare. There are no reports showing CGCT recurrence or malignant transformation (2,5). Electrocautery and use of carbon dioxide laser (8) have also been advocated. Some authors have also advocated gingivoperiosteoplasty with excision for Primary alveolar reconstruction in cases of defects in the alveolar ridge. It helps in achieving proper alignment and promotes normal tooth development (9).This case report intends to document the clinical presentation and its management of the Neumann's tumor in the maxillary arch of a 2-day-old female neonate.
Case Report
An otherwise healthy 2-day-old neonate was referred to our Oral and Maxillofacial Surgery Unit from the Neonatal ICU of our hospital for diagnosis and treatment of a large mass protruding from her mouth. The mother was fit and well gravida 2 para 1, with no remarkable medical history to note. The infant was born by normal vaginal delivery. The baby was born at term plus eight days weighing 2.85 kg, pink and breathing spontaneously (Apgar: 9–10). As the mother was from a remote rural area, she did not have access to any antenatal ultrasonogram. At birth, a firm pedunculated mass was observed protruding from the oral cavity.
On examination, there was a solitary, firm, pedunculated mass, measuring about 3.5cms in diameter. It was arising from the upper alveolar ridge over the right lateral and central incisor area (Figure 1). There was no difficulty in respiration, but the mass interfered while breast feeding. Therefore, a nasogastric tube was passed due to concerns over feeding.
Figure 1.

Pre-op view of 5th day neonate's congenital granular cell tumor
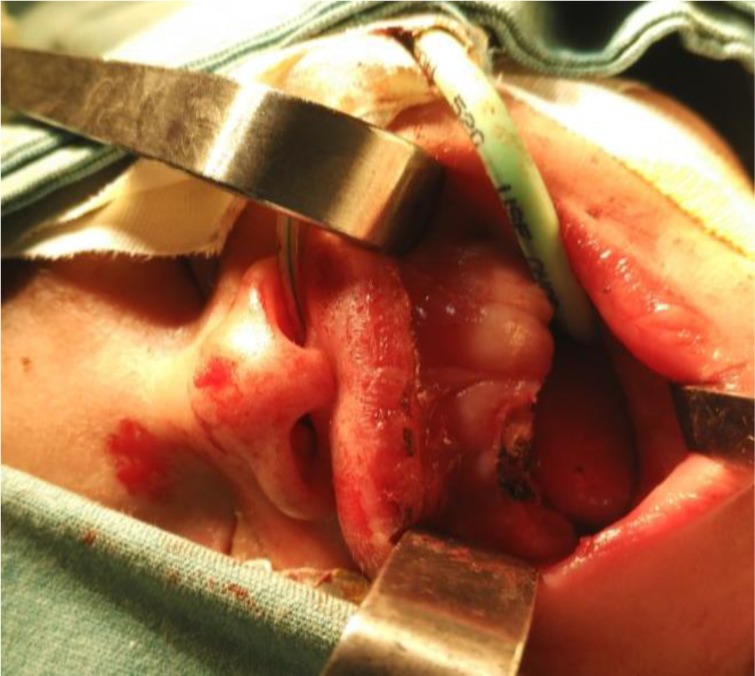
She was scheduled for surgery on the 5th day after birth. The excision of this mass was done under general anaesthesia with oral endotracheal intubation. Monopolar electrocautery was used, and there was very minimal blood loss (Figure 2). In postexcision, any kind of alveolar defect was not noted (Figure 3). Postoperative recovery was uneventful. Nasogastric tube feeding was intiated 3 hours after surgery. The child was breastfeeding 48 hours after surgery, and she was discharged the following day. Healing was uneventful, and the gingival reepithelised in 10days. Histopathology revealed focal ulceration with underlying stroma demonstrating large sheets of closely packed, polygonal cells with round, regular nuclei and inconspicuous nucleoli. It also showed abundant granular cytoplasm consistent with the diagnosis of congenital epulis, or congenital granular cell tumor (Figure 4).
Figure 2.

Excised congenital granular cell tumor
Figure 3.
Post-op view of the 5th day neonate after excision congenital granular cell tumor with cautery
Figure 4.

Histopathology of excised congenital granular cell tumor
Discussion
Congenital epulis, also known as granular cell tumour of the gingiva, congenital granular cell myoblastoma, or Newmann's tumour, following the first published case (1), is encountered exclusively in newborns. The etiology remains unknown and controversial. Congenital epulis differs from other granular cell tumours encountered in adults by its exclusive origin from the neonatal gingiva, the scattered presence of odontogenic epithelium, the more elaborate vasculature and the lack of interstitial cells with angulate bodies (10, 11) different entity from other GCTs. The tumor has a marked female preponderance of 8:1. The tumor usually arises at the future site of the maxillary canine or the lateral incisors, but the unerupted teeth are not involved. It has been described as arising from the mandibular gingiva as well as from several other locations simultaneously. The reported size varies from several millimeters to 7.5 cm (8).
The clinical presentation consists of a lobular or ovoid, sessile or pedunculated swelling covered by a smooth mucosal surface, usually in the maxilla. A provisional diagnosis is often made clinically at birth and is confirmed histologically. The differential diagnosis of a large mass in the fetal or neonatal oral cavity should include such congenital malformations as encephalocoele, dermoid cysts orteratoma and benign and malignant neoplasms including hemangioma, lymphatic malformations, melanotic or pigmented neurectodermal tumours of infancy and rhadomyosarcoma (10).
The treatment of choice is surgical excision to be performed as soon as possible (12). The use of general anesthesia seems to be the recommended procedure in such cases . There are reports of lesion removal without the use of anesthesia. However, this kind of procedure is not justified since these surgical interventions are elective. The CGCT removal under local anesthesia is also an alternative (7,8,11) when intubation is not possible or in cases of small lesions. Some wait for spontaneous regression of small lesions. There is also the possibility of removal during the delivery in cases where the lesion was detected during pregnancy (12). This approach may eliminate additional procedures such as anesthesia and intubation, and it provides the newborn with a free airway and an unobstructed oral cavity immediately after birth (7). Recurrence after removal is not seen, infact recurrence is not seen even after incomplete excision (13). Excision of these masses can leave a notch in the alveolus that may result in an incomplete dental arch.
Gingivoperioseptoplasty is performed early to correct it so that it can restore physiological continuity across the premaxilla and allow osteogenic hematoma formation between the anterior maxillary cleft. It is thought that the union of the mucoperiosteum across an alveolar and anterior hard palate defect creates a periosteal tunnel conducive to bone formation and normal tooth eruption along the cleft region (9,14).
In conclusion, Neumann's tumor or congenital epulis is a very imposing tumor of the oral cavity in neonates. It can be alarming for parents and clinicians. The tumor is often misdiagnosed before surgery because of its rarity and lack of awareness among clinicians (15).
Neumann's tumors rarely cause compromise in the airway, but most of them do hamper breast feeding. It does not harm the future dentition. It is ultimately a benign lesion and does not recur postsurgical excision. Therefore, radical resection is not warranted.
References
- 1.Neumann E, Elin Fall von. Congenitaler Epulis. Arch Heilk. 1871;(12):189. [Google Scholar]
- 2.Chami RG, Wang HS. Large congenital epulis of newborn. J Pediatr Surg. 1986;21(11):929–930. doi: 10.1016/s0022-3468(86)80091-4. [DOI] [PubMed] [Google Scholar]
- 3.Inan M, Yalcin O, Pul M. Congenital fibrous epulis in the infant. Yonsei Med J. 2002;43(5):675–677. doi: 10.3349/ymj.2002.43.5.675. [DOI] [PubMed] [Google Scholar]
- 4.Fuhr AH, Krogh PH. Congenital epulis of the newborn: centennial review of the literature and a report of case. J Oral Surg. 1972;30(1):30–35. [PubMed] [Google Scholar]
- 5.Loyola AM, Gatti AF, Pinto DS, Jr, Mesquita RA. Alveolar and extra-alveolar granular cell lesions of the newborn: report of case and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997 Dec;84(6):668–671. doi: 10.1016/s1079-2104(97)90370-x. [DOI] [PubMed] [Google Scholar]
- 6.Bernhoft CH, Gilhuus-Moe O, Bang G. Congenital epulis in the newborn. Int J Pediatr Otorhinolaryngol. 1987;13(1):25. doi: 10.1016/0165-5876(87)90004-8. [DOI] [PubMed] [Google Scholar]
- 7.Guilherme CCS, Tainah CV. Congenital granular cell tumor (congenital epulis): A lesion of multidisciplinary interest. Med Oral Patol Oral Cir Bucal. 2007 Jan;12(6):E428–E430. [PubMed] [Google Scholar]
- 8.Lapid Oren. Ruthy Shaco-Levy. Congenital Epulis. Pediatrics. 2001;107(2):22–25. doi: 10.1542/peds.107.2.e22. [DOI] [PubMed] [Google Scholar]
- 9.Narasimhan K, Arneja JS, Rabah R. Treatment of congenital epulis (granular cell tumour) with excision and gingivoperiosteoplasty. Can J Plast Surg. 2007;15(4):215–218. doi: 10.1177/229255030701500411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bork M, Hoede N, Korting GW, Burgdorf WH, Young SK. Diseases of the oral mucosa and the lips. Philadelphia, PA: WB Saunders; 1996. p. 293. [Google Scholar]
- 11.Taylor P, McGuire, Petrus P G. Congenital Epulis: A Surprise in the Neonate. J Can Dent Assoc. 2006;72(8):747–750. [PubMed] [Google Scholar]
- 12.Kumar P, Kim HH, Zahtz GD, Valderrama E, Steele AM. Obstructive congenital epulis: prenatal diagnosis and perinatal management. Laryngoscope. 2002;112(11):1935–1939. doi: 10.1097/00005537-200211000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Eppley BL, Sadove AM, Campbell A. Obstructive congenital epulis in a newborn. Ann Plast Surg. 1991;27:152–155. doi: 10.1097/00000637-199108000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Millard DR, Jr, Latham RA. Improved primary surgical and dental treatment of clefts. Plast Reconstr Surg. 1990;(86):856–871. doi: 10.1097/00006534-199011000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Zuker RM, Buenecha R. Congenital epulis: review of the literature and case report. J Oral Maxillofac Surg. 1993;(51):1040–1043. doi: 10.1016/s0278-2391(10)80053-9. [DOI] [PubMed] [Google Scholar]


